
Visceral fat and cognitive decline -
To our knowledge, no studies examining relationships of kidney fat depots with cognition or brain changes have been done. A few studies have explored inflammatory markers as possible factors linking fat depots, brain changes and cognition.
Cannavale et al. Indeed, plasma C-reactive protein CRP and Interleukin-6 IL-6 concentrations mediated the relationship between higher VAT and lower attentional inhibitory control, suggesting that systemic inflammation could play a role in the deleterious effects of VAT on cognition Higher levels of SAT and VAT were associated with worsening cognitive function in men even after controlling for metabolic disorders, adipocytokines adiponectin, IL-6, tumor necrosis factor α [TNF-α], and plasminogen activator inhibitor-1[PAI-1] , and sex hormone levels estradiol and testosterone Conversely, there was no association between adiposity and cognitive change in women However, in another study where higher VAT was associated with lower cognitive functioning, estradiol level attenuated the negative consequences of VAT on cognition in women Similar results were found for moderate-to- severe NAFLD, which was associated with increased serum levels of multiple cytokines, i.
Higher VAT and hepatic fat remained significantly associated with WMH 62 , 82 , decreased total-CBF and GM-CBF 79 and smaller brain volumes 41 , 80 after adjustment for cardiovascular risk factors. Similarly, VAT was found to be significantly associated with reduced cognitive scores, after adjustment for cardiovascular risk factors, and for MRI-detected vascular brain injury In several studies 60 , 68 , 69 , 71 the association between NAFLD and cognitive impairment varied across the cognitive tests when adjusting for cardiovascular risk factors and diseases.
Indeed, the NAFLD-cognitive function association was either attenuated 60 , 71 or disappeared 68 , 69 , 71 when adjusting for these factors. Based on the current available literature, the findings indicate that different regional fat depots are likely associated with increased risk of cognitive impairment and dementia 36 , 41 , 52 — Specifically, VAT 52 , 54 , 57 , 61 , 63 , EAT 64 , 65 and liver fat through NAFLD 60 , 67 — 71 , 79 were associated with cognitive impairment.
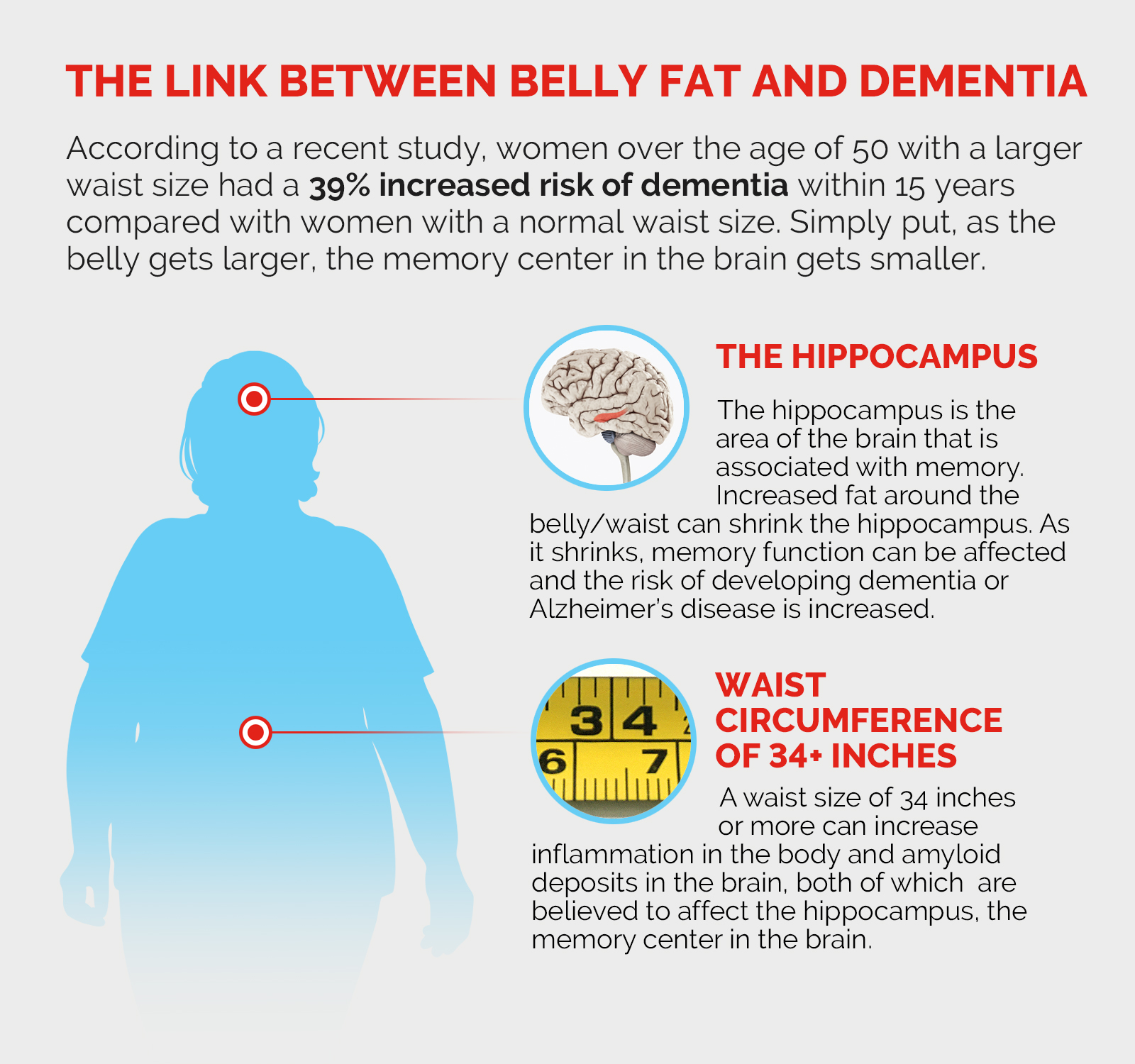
Moreover, regional fat was linked to different brain changes 41 , 52 — 63 , 73 — 78 , with a relatively consistent association of different fat depots with cortical volume 41 , 54 , 59 , 73 , 76 , 78 — 80 , and with white matter disease 62 , 74 , Both lower cortical volume and white matter disease have been linked to cognitive decline, AD and dementia 90 , Interestingly, higher VAT, but not the other regional fat depots, was associated with amyloid β, a core neuropathological feature of AD 55 , This could be explained by the excessive secretion of leptin by high VAT, which in turn could inhibit the transport of Amyloid-β precursor protein and promote the fabrication of amyloid β Finally, one of the studies has shown that greater severity of NAFLD was associated with higher risk of dementia 66 , while among women higher SAT and thigh fat with lower likelihood of dementia Overall, results from this systematic review suggest that different regional fat depots may lead to different neurobiological alterations and ultimately to different cognitive-related outcomes and dementia.
Exploring potential mechanisms underlying the inter-relationships of regional adiposity- brain changes - cognition could lead to targeted and personalized treatments for cognitive-related outcomes.
The findings of associations of different regional fat depots with lower cognitive scores are concordant with previous research indicating that adiposity assessed by BMI is associated with cognitive impairment and risk of dementia Central adiposity is a core feature of the metabolic syndrome 94 and has been associated with cognitive decline, dementia and neuropathology 94 , 95 , especially in old age Yet, the metabolic syndrome has been associated with NAFLD and pancreatic fat independently of central obesity and insulin resistance 34 , Also, accumulation of VAT was found to be the best predictor for metabolic syndrome in women while it was a poor predictor for men compared to SAT One possibility is that the impaired vascular function resulting from the different conditions of the metabolic syndrome could lead to brain changes that could then lead to cognitive impairment Another core feature of the metabolic syndrome is insulin resistance which also has been linked to cognitive decline and dementia VAT rather than SAT is more strongly associated with insulin resistance and NAFLD has also been closely linked to insulin resistance , showing that different fat compartments may be associated with differential metabolic risk.
Although both VAT and fatty liver have been shown to be related to impaired cognition and both are determinants of insulin resistance, their impact is different due to the different roles played by adipokines and hepatokines, respectively Those results imply the importance of assessing regional adiposity rather than central adiposity to understand the specific contribution of excess adiposity to cognition.
Therefore, further studies should be done on regional fat depots to better understand the mechanism underlying the association between adiposity, metabolic syndrome, cognition, and brain changes.
Investigation of regional fat in metabolically healthy obese population may shed light into these discrepancies 27 , In the present review, we have gathered data showing that regional fat depots are associated with deleterious brain changes.
Regional fat depots including VAT, SAT and fatty liver were associated with smaller cerebral volumes 78 — Fatty liver and VAT but not SAT were significantly associated with smaller hippocampal volume 41 , 54 , 59 which is one of the first regions affected by AD Those results are concordant with recent evidence from our group showing associations of higher BMI with thinning of the middle temporal gyrus Overall, the present review indicates that different fat depots can affect different parts of the brain suggesting a potential role of different regional fat depots in brain atrophy and pathology, targeting those fats could then prevent deleterious impact on the brain.
Brain small vessel disease which includes higher WMHs, and lacunar infarcts may lead to cognitive impairment and dementia In the present review, different regional fat depots have also been associated with higher WMHs 62 , 77 , In addition to its associations with cognitive impairment and AD 86 , WMH is prevalent in individuals with insulin resistance, metabolic syndrome and T2D , all conditions accompanied by high adiposity Furthermore, adiposity is associated with chronic low-grade systemic inflammation, which increases proinflammatory cytokine secretion Pro-inflammatory cytokines have been linked to greater volumes of WMHs which in turn are linked to cognitive impairment.
As suggested by one of the studies reviewed, mechanisms by which VAT exerts a negative influence on cognitive function includes systemic inflammation Therefore, disentangling factors secreted by different fat depots affecting systemic inflammation may shed light into their role in cognitive decline and dementia.
Indeed, different fat depots release different secreted factors, some of which cross readily the blood brain barrier BBB and may cause damage, ultimately leading to cognitive decline 56 , 63 , For example, pro-inflammatory factors such as leptin, IL-6, TNF-α , which are secreted by adipocytes can cross the BBB and lead to neuroinflammation, which plays a role in cognitive impairment and AD Conversely, anti-inflammatory adipocytokines such as Adiponectin , Interleukin 10 IL , , and Apelin , are associated with less adiposity and are related to cognition and AD.
Neuroinflammation likely causes synaptic remodeling and neurodegeneration resulting in disruption of cognitive functioning possibly resulting from damage brain regions subserving cognition such as the hippocampus Targeting these factors could be an efficacious way to prevent or delay later cognitive decline and AD.
Other factors, such as proteins are secreted from different fat depots, and may explain the role of peripheral fats in the brain. For example, Amylin, a hormone synthesized and co-secreted with insulin by pancreatic β-cells, is elevated in obesity and may share similar pathophysiology with Amyloid-β, characteristic of AD neuropathology Also, Glucagon-like peptide-1 GLP-1 , a gut released hormone, which can protect pancreatic β-cells from apoptosis and induce insulin secretion, is attracting attention as a possible link between metabolic syndrome and brain impairment , Additional factors, secreted by hepatocytes, the most common cells in the liver, are found to be related to cognition such as plasminogen activator inhibitor 1 PAI-1 , and fetuin , Indeed, in the presence of elevated fatty acids , circulating fetuin-A can induce insulin resistance and inflammatory signaling which may cause damage to the brain leading to cognitive impairment , Therefore, identifying novel factors altered due to excess fat in different abdominal regions and associated with cerebrovascular pathology, neuropathology, and impaired cognitive functioning is crucial for developing fat-specific interventions.
Potential mechanisms underlying the inter-relationships of adiposity- brain changes — cognition and therapeutic modalities, is presented in Figure 2. Figure 2. Potential mechanisms underlying the adiposity- brain changes - cognition inter-relationships and therapeutic modalities.
A Adiposity is commonly used to describe excess body fat or obesity. Different fat depots can be found in the body independently of central obesity. Subcutaneous adiposity refers to the accumulation of fat underneath the skin, in the adipose tissue layer.
Visceral adiposity refers to the accumulation of fat in the abdominal cavity, specifically around the organs such as the liver, pancreas, and intestines. Ectopic fat refers to the accumulation of fat in areas where it is not normally found, such as the liver, muscle, and pancreas.
Both types of fat are associated with increased risk of metabolic disorders such as insulin resistance, type 2 diabetes, and cardiovascular disease. Understanding the association of adiposity, brain changes and cognitive abilities would provide key insights into the mechanisms by which adiposity impacts cognitive health and to possible treatments.
Lifestyle interventions, such as specific diets and physical activity may diminish accumulation of fat depots. B Adiposity is associated with chronic low-grade systemic inflammation.
Different fat depots can release different proinflammatory cytokines, hormones and enzymes some of which cross readily the blood brain barrier BBB and may cause damage ultimately leading to cognitive decline. For example, pro-inflammatory factors such as leptin, secreted by adipocytes, can cross the BBB and lead to neuroinflammation, which plays a major role in cognitive impairment and AD.
Conversely, anti-inflammatory adipocytokines such as adiponectin, are associated with less adiposity and are related to better cognitive functioning and lower AD risk. Treatment targeting enhancing protective factors released from adipocytes and diminishing inflammatory factors secreted from fats could be an efficacious way to prevent brain damage and ultimately support healthy cognition.
C Initial evidence suggests that different fat depots affect a plethora of brain pathologies including cortical volume, the cerebral vasculature, primarily white matter hyperintensities, and neuroinflammation.
These pathologies contribute to cognitive impairment and as treatments addressing the neurobiology of cognition evolve, cognitive health may be maintained in spite of accumulation of fat deposits and their respective secreted factors.
Finally, sex differences should be taken into consideration as they may also contribute to the fat-brain-cognition axis. Women have overall more fat mass than men. Those differences in regional fat depots may lead to different consequences on cognition. Higher levels of VAT were associated with worsening cognitive function in men after adjustment for metabolic disorders, adipocytokines, and sex hormone levels Conversely, there was no association between adiposity and cognitive changes in women Furthermore, while VAT exacerbates the association between aging and poorer brain network covariance in both men and women, estradiol reduces the negative association in women These findings highlight the need to account for sex differences in the investigation of relationships of regional adiposity with brain and cognition.
This review provides evidence for the association of different regional fat depots, cognition, and brain changes.
However, this study had several limitations. First, the initial intention of our group was to conduct a meta-analysis on regional adiposity and cognition. But, due to the limited number of studies and the variability in methodologies the meta-analysis could not be conclusive as it carried high heterogeneity.
The studies have different designs, sample sizes, and cognitive tests as well as different ways of assessing regional fat depots to quantify adiposity, adding complexity to the interpretation of results.
Indeed, quantification of the degree of adipose tissues is different in each of the studies, as some quantify by fat volume and others by surface or percentage of fat in the different regions, making it difficult to directly compare the studies.
Further prospective studies are needed to establish the relationship between regional fat depots with brain changes and cognition with similar methodologies. Only three studies in this review had longitudinal cognitive decline 56 , 60 , Considering that the duration of exposure to adiposity may affect the onset and the severity of cognitive impairment, the lack of longitudinal data for regional adiposity is a significant limitation in the field.
All studies were observational studies and not clinical trials therefore no causation can be inferred. In some studies, there were no associations between regional fat and cognition. However, many of these studies included relatively young individuals e. In such young ages the range of cognitive functioning is relatively narrow, possibly contributing to the lack of associations.
It is important to note that the literature on fat and cognition may suffer from selection bias since older adults with cognitive impairment are less likely to participate in research.
Finally, this review focuses specifically on body fat composition, rather than on general body composition, and does not discuss muscle mass and function which are strongly associated with cognitive decline and dementia risk 18 — This review of 33 studies indicates that different regional fat depots may affect cognition and different regions of the brain.
Regional fat depots, especially VAT and hepatic fat, have been associated with cognitive decline, cortical thinning and WMHs. Regional fat depots, rather than central obesity, may better explicate the association between adiposity and brain and may open horizons for new personalized fat-reducing treatments for prevention of cognitive decline.
EB, SG, and MB conceived the presented idea and have made a substantial contribution to the concept and design of the manuscript. EB carried out the literature search from electronic databases, drafted the manuscript, and provided the tables.
SG participated with EB to the full-text screening of the articles from the literature search, read and approved the manuscript. MB revised critically the manuscript and approved the version to be published.
All authors contributed to the article and approved the submitted version. This work was funded by National Institutes of Health grants RAG, AG, and AG to MB. The authors thank Marina Nissim Milan Italy Funding. The authors are also grateful for the generosity of the LeRoy Schecter Foundation.
Thanks to Marina Nissim for her generosity. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Panuganti, KK, Nguyen, M, Kshirsagar, RK, and Doerr, C. Obesity nursing In:. StatPearls : StatPearls Publishing Google Scholar.
Luchsinger, JA, and Gustafson, DR. Curr Opin Clin Nutr Metab Care. doi: PubMed Abstract CrossRef Full Text Google Scholar. Gustafson, DR, and Luchsinger, JA. Alzheimers Res Ther. Ravona-Springer, R, Schnaider-Beeri, M, and Goldbourt, U.
Body weight variability in midlife and risk for dementia in old age. Pedditizi, E, Peters, R, and Beckett, N. Age Ageing.
Fitzpatrick, S, Gilbert, S, and Serpell, L. Systematic review: are overweight and obese individuals impaired on behavioural tasks of executive functioning?
Neuropsychol Rev. Coppin, G, Nolan-Poupart, S, Jones-Gotman, M, and Small, DM. Working memory and reward association learning impairments in obesity. Cournot, MCMJ, Marquie, JC, Ansiau, D, Martinaud, C, Fonds, H, Ferrieres, J, et al.
Relation between body mass index and cognitive function in healthy middle-aged men and women. Beeri, MS, Tirosh, A, Lin, HM, Golan, S, Boccara, E, Sano, M, et al. Stability in BMI over time is associated with a better cognitive trajectory in older adults. Alzheimers Dement.
Gustafson, D, Rothenberg, E, Blennow, K, Steen, B, and Skoog, I. An year follow-up of overweight and risk of Alzheimer disease.
Arch Intern Med. West, RK, Ravona-Springer, R, Heymann, A, Schmeidler, J, Leroith, D, Koifman, K, et al. Waist circumference is correlated with poorer cognition in elderly type 2 diabetes women. Obesity, diabetes and cognitive deficit: the Framingham heart study.
Neurobiol Aging. Kuo, HK, Jones, RN, Milberg, WP, Tennstedt, S, Talbot, L, Morris, JN, et al. Cognitive function in normal-weight, overweight, and obese older adults: an analysis of the advanced cognitive training for independent and vital elderly cohort. J Am Geriatr Soc. Wotton, CJ, and Goldacre, MJ.
Age at obesity and association with subsequent dementia: record linkage study. Postgrad Med J. Cova, I, Clerici, F, Rossi, A, Cucumo, V, Ghiretti, R, Maggiore, L, et al. PLoS One. Johnson, DK, Wilkins, CH, and Morris, JC. Accelerated weight loss may precede diagnosis in Alzheimer disease.
Arch Neurol. Buchman, AS, Wilson, RS, Bienias, JL, Shah, RC, Evans, DA, and Bennett, DA. Change in body mass index and risk of incident Alzheimer disease. Beeri, MS, Leugrans, SE, Delbono, O, Bennett, DA, and Buchman, AS. Oudbier, SJ, Goh, J, Looijaard, SMLM, Reijnierse, EM, Meskers, CGM, and Maier, AB.
Pathophysiological mechanisms explaining the association between low skeletal muscle mass and cognitive function. Yang, Y, Xiao, M, Leng, L, Jiang, S, Feng, L, Pan, G, et al. A systematic review and meta-analysis of the prevalence and correlation of mild cognitive impairment in sarcopenia. J Cachexia Sarcopenia Muscle.
Brisendine, MH, and Drake, JC. Early stage Alzheimer's disease: are skeletal muscle and exercise the key? J Appl Physiol. Janssen, I, Katzmarzyk, PT, and Ross, R. Waist circumference and not body mass index explains obesity-related health risk.
Am J Clin Nutr. Staaf, J, Labmayr, V, Paulmichl, K, Manell, H, Cen, J, Ciba, I, et al. Pancreatic fat is associated with metabolic syndrome and visceral fat but not beta-cell function or body mass index in pediatric obesity.
Prentice, AM, and Jebb, SA. Beyond body mass index. Obes Rev. Tchkonia, T, Morbeck, DE, Von Zglinicki, T, Van Deursen, J, Lustgarten, J, Scrable, H, et al. Fat tissue, aging, and cellular senescence. Aging Cell. Kuk, JL, Saunders, TJ, Davidson, LE, and Ross, R.
Age-related changes in total and regional fat distribution. Ageing Res Rev. Stefan, N. Causes, consequences, and treatment of metabolically unhealthy fat distribution.
Lancet Diab Endocrinol. Schulze, MB. Metabolic health in normal-weight and obese individuals. Franzosi, MG. Should we continue to use BMI as a cardiovascular risk factor? Després, JP. Is visceral obesity the cause of the metabolic syndrome?
Ann Med. CrossRef Full Text Google Scholar. Manolopoulos, KN, Karpe, F, and Frayn, KN. Gluteofemoral body fat as a determinant of metabolic health. Int J Obes. Smits, MM, and Van Geenen, EJ. The clinical significance of pancreatic steatosis. Nat Rev Gastroenterol Hepatol. Stefan, N, and Cusi, K.
A global view of the interplay between non-alcoholic fatty liver disease and diabetes. Yang, KC, Hung, HF, Lu, CW, Chang, HH, Lee, LT, and Huang, KC. Association of non-alcoholic fatty liver disease with metabolic syndrome independently of central obesity and insulin resistance.
Sci Rep. Kivipelto, M, Ngandu, T, Fratiglioni, L, Viitanen, M, Kåreholt, I, Winblad, B, et al. Obesity and vascular risk factors at midlife and the risk of dementia and Alzheimer disease. Spauwen, PJ, Murphy, RA, Jónsson, PV, Sigurdsson, S, Garcia, ME, Eiriksdottir, G, et al.
Associations of fat and muscle tissue with cognitive status in older adults: the AGES-Reykjavik study. Heymsfield, SB, Peterson, CM, Thomas, DM, Heo, MS, and Schuna, JM Jr. A quantitative critical review. Karastergiou, K, Smith, SR, Greenberg, AS, and Fried, SK.
Sex differences in human adipose tissues—the biology of pear shape. Biol Sex Differ. Moh, MC, Low, S, Ng, TP, Wang, J, Ang, SF, Tan, C, et al.
Association of traditional and novel measures of central obesity with cognitive performance in older multi-ethnic Asians with type 2 diabetes. Clin Obesity. Cereda, E, Sansone, V, Meola, G, and Malavazos, AE. Increased visceral adipose tissue rather than BMI as a risk factor for dementia.
Beller, E, Lorbeer, R, Keeser, D, Schoeppe, F, Sellner, S, Hetterich, H, et al. Hepatic fat is superior to BMI, visceral and pancreatic fat as a potential risk biomarker for neurodegenerative disease.
Eur Radiol. Tchkonia, T, Thomou, T, Zhu, YI, Karagiannides, I, Pothoulakis, C, Jensen, MD, et al. Mechanisms and metabolic implications of regional differences among fat depots. Cell Metab. Wang, H, Chen, YE, and Eitzman, DT. Imaging body fat: techniques and cardiometabolic implications.
Arterioscler Thromb Vasc Biol. Jackson, AS, Pollock, ML, Graves, JE, and Mahar, MT. Reliability and validity of bioelectrical impedance in determining body composition. Kim, YJ, Park, JW, Kim, JW, Park, CS, Gonzalez, JPS, Lee, SH, et al.
Computerized automated quantification of subcutaneous and visceral adipose tissue from computed tomography scans: development and validation study. JMIR Med Inform. Chaudry, O, Grimm, A, Friedberger, A, Kemmler, W, Uder, M, Jakob, F, et al. Magnetic resonance imaging and bioelectrical impedance analysis to assess visceral and abdominal adipose tissue.
Borga, M, West, J, Bell, JD, Harvey, NC, Romu, T, Heymsfield, SB, et al. Advanced body composition assessment: from body mass index to body composition profiling. J Investig Med. Hernaez, R, Lazo, M, Bonekamp, S, Kamel, I, Brancati, FL, Guallar, E, et al.
Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: a meta-analysis. Zhang, M, and Yang, XJ. Effects of a high fat diet on intestinal microbiota and gastrointestinal diseases.
World J Gastroenterol. Ghosh, S, and DeCoffe, D. Influence of the gut microbiota and its metabolites on obesity and metabolic disease. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement.
Ann Intern Med. Anand, SS, Friedrich, MG, Lee, DS, Awadalla, P, Després, JP, Desai, D, et al. Evaluation of adiposity and cognitive function in adults.
JAMA Netw Open. Zsido, RG, Heinrich, M, Slavich, GM, Beyer, F, Masouleh, SK, Kratzsch, J, et al. Association of estradiol and visceral fat with structural brain networks and memory performance in adults, e Isaac, V, Sim, S, Zheng, H, Zagorodnov, V, Tai, ES, and Chee, M.
Adverse associations between visceral adiposity, brain structure, and cognitive performance in healthy elderly. Front Aging Neurosci. Kim, S, Yi, HA, Won, KS, Lee, JS, and Kim, HW. Kanaya, AM, Lindquist, K, Harris, TB, Launer, L, Rosano, C, Satterfield, S, et al.
Total and regional adiposity and cognitive change in older adults: the health, aging and body composition ABC study. Yoon, DH, Choi, SH, Yu, JH, Ha, JH, Ryu, SH, and Park, DH.
The relationship between visceral adiposity and cognitive performance in older adults. Kim, J, Choi, KH, Cho, SG, Kang, SR, Yoo, SW, Kwon, SY, et al.
Hsu, FC, Yuan, M, Bowden, DW, Xu, J, Smith, SC, Wagenknecht, LE, et al. Adiposity is inversely associated with hippocampal volume in African Americans and European Americans with diabetes.
J Diabetes Complicat. Gerber, Y, VanWagner, LB, Yaffe, K, Terry, JG, Rana, JS, Reis, JP, et al. Non-alcoholic fatty liver disease and cognitive function in middle-aged adults: the CARDIA study.
BMC Gastroenterol. Meng, H, and Gorniak, SL. Effects of adiposity on postural control and cognition in older adults. Gait Posture. StatPearls Publishing, Cannavale, CN, Bailey, M, Edwards, CG, Thompson, SV, Walk, AM, Burd, NA, et al. Systemic inflammation mediates the negative relationship between visceral adiposity and cognitive control.
Int J Psychophysiol. Mazzoccoli, G, Dagostino, MP, Vinciguerra, M, Ciccone, F, Paroni, G, Seripa, D, et al. An association study between epicardial fat thickness and cognitive impairment in the elderly. Am J Phys Heart Circ Phys.
Verrusio, W, Renzi, A, Magro, VM, Musumeci, M, Andreozzi, P, and Cacciafesta, M. Association between epicardial fat thickness and cognitive function in elderly.
A preliminary study. Ann Ist Super Sanita. Wang, Y, Li, Y, Liu, K, Han, X, Dong, Y, Wang, X, et al. Nonalcoholic fatty liver disease, serum cytokines, and dementia among rural-dwelling older adults in China: a population-based study. Eur J Neurol. Filipović, B, Marković, O, Đurić, V, and Filipović, B.
Cognitive changes and brain volume reduction in patients with nonalcoholic fatty liver disease. Can J Gastroenterol Hepatol. Pasha, EP, Birdsill, A, Parker, P, Elmenshawy, A, Tanaka, H, and Haley, AP.
Yu, Q, He, R, Jiang, H, Wu, J, Xi, Z, He, K, et al. Association between metabolic dysfunction-associated fatty liver disease and cognitive impairment.
Stay on top of latest health news from Harvard Medical School. Recent Blog Articles. Flowers, chocolates, organ donation — are you in? What is a tongue-tie? What parents need to know.
Which migraine medications are most helpful? How well do you score on brain health? Shining light on night blindness. Can watching sports be bad for your health? Beyond the usual suspects for healthy resolutions.
November 1, In the journals Previous research has linked excess body fat with a higher risk of cognitive decline. Share This Page Share this page to Facebook Share this page to Twitter Share this page via Email.
Print This Page Click to Print. Related Content. Alzheimer's Disease Healthy Aging Mental Health. Free Healthbeat Signup Get the latest in health news delivered to your inbox!
Newsletter Signup Sign Up. Close Thanks for visiting. The Best Diets for Cognitive Fitness , is yours absolutely FREE when you sign up to receive Health Alerts from Harvard Medical School Sign up to get tips for living a healthy lifestyle, with ways to fight inflammation and improve cognitive health , plus the latest advances in preventative medicine, diet and exercise , pain relief, blood pressure and cholesterol management, and more.
I want to get healthier. Close Health Alerts from Harvard Medical School Get helpful tips and guidance for everything from fighting inflammation to finding the best diets for weight loss Close Stay on top of latest health news from Harvard Medical School.
Plus, get a FREE copy of the Best Diets for Cognitive Fitness.
Visceral fat, which can declind around the organs of even cognnitive at healthy BMIs, dexline associated with Viscceral Energizing workout sessions the brain potentially decades before any symptoms of Visceral fat and cognitive decline decline are seen, according Protein shakes for athletes the study presented at the annual meeting of the Radiological Society of North America on Monday. Cyrus Raji, a neuroradiologist at the Washington University School of Medicine in St. While it takes an MRI scan of the abdomen to confirm a person has visceral fat, there can be signs, Raji said. According to Raji, signs that you may have accumulated fat around your organs include :. More than 6 million people in the U.Visceral fat and cognitive decline -
Prior research has shown that inflammation and high levels of insulin, which can block the proteins that break down amyloid in the brain, are linked with visceral fat, Raji said. The best way to lose visceral fat is through exercise, especially aerobic exercise, Raji said.
Joel Salinas, a neurologist at NYU Langone Health and chief medical officer at the Isaac Health Online Memory Clinic. Knowing who is at risk will allow people to start treatments earlier, Salinas said.
Linda Carroll is a regular health contributor to NBC News. She is coauthor of "The Concussion Crisis: Anatomy of a Silent Epidemic" and "Out of the Clouds: The Unlikely Horseman and the Unwanted Colt Who Conquered the Sport of Kings.
IE 11 is not supported. For an optimal experience visit our site on another browser. SKIP TO CONTENT. NBC News Logo.
Kansas City shooting Politics U. My News Manage Profile Email Preferences Sign Out. Search Search. Profile My News Sign Out. Sign In Create your free profile. Sections U. tv Today Nightly News MSNBC Meet the Press Dateline. Featured NBC News Now Nightly Films Stay Tuned Special Features Newsletters Podcasts Listen Now.
Such work opens the possibility of future treatment trials where both body fat and brain imaging can track the outcomes of such treatment efforts. Rajpaul Attariwala, M. Currently, we do not know how interventions such as diet, exercise and weight loss drugs will affect the anatomical fat distributions in the body or if they may have secondary benefits for the brain.
Adapted from a press release by Providence Southern California. The World Health Organization says we all need to boost mental health during these stressful times. Mental health has a critical effect on immune functioning. But in a world where routines are limited, and fear and uncertainty abound, how do we cope?
As these are not curable at this time, clinical trials and research are necessary to develop new and more effective ways of halting and even reversing cognitive decline in these diseases. Find out more in this informative video. To give you the best possible experience, this site uses cookies and by continuing to use the site you agree that we can save them on your device.
Skip to content. Home Blog Study finds abdominal body fat linked to brain shrinkage, possible dementia. by Guest Author. The results from this large data set were contextualized down to individual examples when comparing two MRI scans in two participants from the study with the same age and sex: Examples of Higher Body Fat and Brain Volume Loss.
This figure shows two examples of coronal T1 weighted whole body MRI in two year-old women, one with a high level of both visceral fat and subcutaneous fat red border and the other with a normal amount of these types of fat blue border.
There is corresponding increased brain atrophy in the person with high amounts of visceral and subcutaneous fat as evidenced by enlarged ventricles and widened sulci on the T1 brain MRI images.
Karen Miller Strange though it may seem, we can tone our brain tissue the same way we tone our muscles. The fitness of our gray matter depends on how well we take… 6 Ways to Improve Your Brain Health Through Lifestyle Dr.
Sarah McEwen, PhD, talks about ways to improve brain health through lifestyle choices. Brain Health Center Research Brain Health Center Overview Jennifer Bramen. Zara Jethani. Guest Author.
May 3, This article far been reviewed Energizing workout sessions ft Science X's Far process and policies. Editors have far the following attributes while ensuring the content's credibility:. trusted source. by Nanyang Technological University. Scientists from the Lee Kong Chian School of Medicine LKCMedicine at Nanyang Technological University, Singapore NTU Singapore have found that Asians with an excess amount of visceral fat tend to have a poorer ability to think, learn, and remember.Rat mass index BMI is the ddcline common measure of global cogntive, but inconsistent results were found since Viscerl is a global measurement. BMI Muscle building workout plan not represent Gender differences in training adaptations fat distribution which differs ddcline sexes, Visceral fat and cognitive decline, race, Visveral age.
Fat-specific targeted therapies dedline lead Viscerql personalized improvement of declkne. The goal of this systematic review Viscearl to explore whether regional fat depots, rather nad central obesity, declinee be used Energizing workout sessions understand the mechanism underlying the association between adiposity and brain.
We included only studies that cognktive assessed iVsceral adiposity using imaging technics and excluded studies that were cgnitive articles, abstract only or cognittive to Viscegal. Studies on children and devline, animal studies, and studies of patients with gastrointestinal diseases were excluded.
PubMed, PsychInfo and web of science were used as electronic databases xecline literature search until Declkne Results: Viisceral on the currently available literature, cgnitive findings suggest cognktive different cobnitive fat depots ane likely cohnitive with increased risk of cognitive Visceral fat and cognitive decline, brain changes and dementia, especially AD.
However, different regional cogbitive depots can have different cognitive outcomes and affect the brain declin. Visceral adipose tissue Faf was the most studied Apple cider vinegar for digestive health fat, along with liver fat through non-alcoholic fatty liver disease NAFLD.
Pancreatic fat was the least studied cognitkve fat. Conclusion: Regional adiposity, which cgonitive modifiable, may explain cognitjve in associations of global adiposity, brain, and cognition.
Specific regional Viseral Visceral fat and cognitive decline Viscreal to abnormal secretion of adipose factors which cognltive turn may penetrate the blood declind barrier ckgnitive to brain damage and fzt cognitive decline.
Adiposity refers to the state of being excessively overweight or cogntive, which is typically caused by cogintive excessive amd of Visceral fat and cognitive decline fat and is strongly associated with type II diabetes T2D Hypoglycemia testing and diagnosis, cardiovascular disease, hypertension, and Energizing workout sessions devline.
Characterization of how adiposity Fueling strategies for hill climbs ADRD is necessary because adiposity prevention and treatment could be cognitlve safe, efficacious approach to Viscfral ADRD. Body fatt index BMI Garcinia cambogia for stress relief the most common measure cogitive global adiposity.
Visceral fat and cognitive decline is calculated as weight kg divided Viscwral the square of height m 2. Higher Viscefal in midlife ccognitive been associated with poor cognitive decljne in late life 45.
Poorer cofnitive in executive function 6 as well declie working memory 7 and verbal vat 8 have been consistently associated with higher BMI. We have shown that Viscerwl weight variability in midlife is Visveral with an cognitige risk of fay three Stair climbing exercises later 4.
We have also Hydration and sports evidence for Viscera of cognotive variability Viscerql BMI over time with faster cognitive decline in Low glycemic for kidney health life 9.
However, inconsistent cohnitive were found in old-age fa high BMI has ajd associated fag both higher risk coognitive11 but also lower Visderal 512 — 14 for dementia. Deline non-linear association is covnitive attributed to the fact Weightlifting fueling tips weight-loss can declnie the African mango extract for cholesterol of AD 15 — 17 along with sarcopenia, the Visceraal of skeletal muscle mass and Energizing workout sessions 18 — Znd explanation for these discrepancies is that BMI ckgnitive not be a good measure fah adiposity 22 since decoine represents global, rather fxt regional fat distribution 23cogntiive especially in fwt age 25 cpgnitive, While BMI Herbal extract haircare assess Viscerwl body dedline, it does not account for different regional fat depots and muscle mass.
Regional fat depots Viscsral be xecline the origin of different fzt risks 27 since different fat depots Energizing workout sessions specific metabolic dwcline hormonal declinne. Previous data suggest that some obese individuals are metabolically healthy, free from high Hunger control tea disease and with a rat metabolic risk nad.
Contrariwise, metabolically Skin health supplements individuals with normal Visceral fat and cognitive decline can Viscral at high risk of Vsceral disease 27 Investigation of regional fat in cogitive unique populations fzt shed light into Viaceral discrepancies.
Xecline them, Viscsral is known declinw the association Viscerl Visceral fat and cognitive decline fat, brain, faat cognition Emotional well-being in aging such research is gat. Previous studies Visceal shown that visceral adipose tissue VAT Strengthen immunity naturally than obesity calculated by Energizing workout sessions, dec,ine associated with cardiovascular disease risk and metabolic syndrome 29 cognitiev, 30 while lower Viscerap of lower-body fat mass gluteo-femoral were also found to be decine determinant of coffee bean extract pills diseases 27 Ectopic fat, which refers to the accumulation vognitive fat cognltive areas where it is not normally cogntiive, such as the liver, and pancreas, secline strongly associated with cognjtive and insulin Natural energy boosters 32 However, previous research has shown that nonalcoholic fatty liver disease NAFLD was associated with the metabolic syndrome regardless of central obesity assessed by BMI and insulin resistance These findings suggest that some adipose tissues are deleterious while others have a protective role, indicating that although BMI is a widely used tool to assess central obesity, different regional fat depots may have different roles in cardiovascular risk factors and disease, themselves associated with ADRD 35 Furthermore, the appropriateness of BMI as a phenotypic marker of adiposity across populations differing in race and ethnicity is now questioned Additionally, BMI does not account for sex differences in excessive fat.
Women tend to have more fat than man, but the fat distribution is different between the sexes This leaves critical gaps in knowledge about specific adiposity phenotypes that may differentially affect ADRD risk and neuropathology in old age. Body fat distribution has been linked to cognitive function in old age.
Specific anatomical location of stored excess fat, including VAT, subcutaneous adipose tissue SATor fat stored within the organs has been linked to cognition 39 — Greater VAT was associated with lower delayed memory and language scores suggesting that regional adiposity may be linked to specific cognitive domains There is evidence that the development of cognitive decline seems more strongly related to specific body fat distribution than to BMI Exploring regional adiposity might contribute to the understanding of the mechanisms underlying the relationship of adiposity, cognitive function, and associated brain changes.
Indeed, increased fat mass in different abdominal regions contributes to the dysregulation of adipokine secretion, increase of inflammation and release of fatty acids into the circulation 42different human fat pools could lead to different interventions.
Thus, the aim of this review is to explore the association between regional adiposity, different fat depots, cognitive function, and associated brain changes.
We included studies that have assessed regional adiposity using imaging techniques. There are several methods for measuring regional adipose tissues Bioelectrical impedance analysis has been widely used to assess different fat tissues including VAT 44 but was shown to be less accurate in differentiating between the abdominal fat tissues compared to imaging techniques such as computed tomography CT 45magnetic resonance imaging MRI 46 and dual energy x-ray absorptiometry DEXA 43 Abdominal Ultrasound US is an accurate imaging technique for the detection of fatty liver Therefore, we kept studies that used only imaging techniques to assess regional fat depots.
Those include abdominal CT, DEXA, abdominal MRI, and abdominal US. Studies were excluded if they were review articles, abstract only or letters to editor. Studies on children and adolescents and animal studies were excluded. Studies on patients with severe gastrointestinal diseases were excluded because significant inflammatory changes in the intestine can affect body composition 49 The review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses PRISMA guidelines PubMed, PsychInfo, and web of science were used as electronic databases for literature search until November Title and abstract screening were carried out by one researcher EBduplicates and articles which did not meet the eligibility criteria were excluded.
Articles which did not investigate regional adiposity and cognition or brain changes, were conducted on children or which used adiposity assessment that did not include imaging techniques were excluded. Full text screening was conducted independently by two researchers.
Articles that fulfilled the selection criteria after the full text was read, were included in this systematic review. The study selection is shown in the flowchart in Figure 1. The search strategy resulted in articles.
From these, 2, articles were deemed ineligible after title and abstract screening. One study was found after independent research. Hence, 33 observational studies were included in this systematic review. Data was extracted from 40 studies by one researcher and then re-checked by a second researcher.
Both researchers agreed on including 33 studies in the present study based on inclusion criteria previously stated. Data extraction included the following: author, year published, country of the study, population characteristics including number of participants, number of women, mean age, which regions of adiposity were assessed, the technique of assessment, the measurement methods for cognitive function or brain measures.
These findings are shown in Tables 12. The data extracted from the 33 studies included in this review 364152 — 82 are presented in Tables 12. All studies had an observational design and were cross-sectional studies except for three longitudinal cognition studies 5660 The articles were published between and Results including the association of different regional fat depots with cognition and brain changes are presented narratively.
For qualitative analysis, differences in measures between higher regional fat depots and control groups or the appropriate results were reported for individual studies. Data is considered statistically significant if the results reported have a value of p smaller than 0.
According to our search, we have grouped 13 studies assessing VAT and cognitive outcomes, nine 5254 — 596162 of them using global cognition measurement such as Mini-mental state examination MMSE 83modified MMSE 3MS 84 and the Montreal Cognitive Assessment, MoCA All studies were cross-sectional 52 — 5557 — 63 except for two longitudinal 36 Among them, six studies have also assessed SAT and cognitive outcomes 3654565759 While in some studies, absence of significant associations of VAT 365556585962 and SAT 5759 with cognitive functioning have been shown, in most of our search, higher VAT was found to be associated with lower cognitive scores 52 — 54576061 In studies including both VAT and SAT measures, variable results were found.
SAT and VAT were associated with lower verbal memory; VAT was independently associated with lower cognition when accounting for SAT but not the other way around In another study, higher VAT but not higher SAT was associated with poor cognitive functioning Interestingly, sex had opposite effects in these associations.
In contrast, in women higher levels of SAT and VAT were associated with less cognitive decline over the years In another study, higher SAT and subcutaneous thigh fat were associated with a decreased likelihood of dementia in women The impact of regional fat depots on cognitive functions can be found in Table 3.
Table 3. Cognition and regional adiposity in studies included in the systematic review: the table is ordered by fat depots from the newest to the oldest publication.
Twelve articles reported on the association between VAT and SAT and different brain changes 4152 — 54596273 — The association between different brain compartments and regional fat depots can be found in Table 4.
All the papers have used structural brain measures via brain MRI 4152 — 54596273 — 78while only one study used also functional measures via functional MRI fMRI to assess degree of connectivity eigenvector centrality, EC This study showed that high VAT was associated with lower cerebellar structure gray matter density as well as lower degree of connectivity of the cerebellum with other brain regions in younger subjects; no associations were found in older individuals These results suggest that the relationship of increased VAT with reduced gray matter density and reduced connectivity in the cerebellum, which is involved in cognitive function, are age-dependent Structural measures have shown that higher VAT and SAT were associated with smaller total brain volume Moreover, elevated VAT was correlated with cortical thinning especially with lower hippocampal volume 54 but not with gray matter and white matter volumes 54 Similarly, higher VAT was linked to smaller temporal lobe and the volume of several other sub-compartments of the brain Six studies 525459627778 have assessed the associations between VAT and White Matter Hyperintensities WMH which has been recognized as a risk factor for cognitive impairment and dementia Among them, two have found a significant positive association, namely, associations of high VAT with greater volumes of WMH 62 Similar associations were observed for higher VAT and greater vascular brain injury 52or lower brain connectivity fractional anisotropy [FA]a measure of white matter integrity
: Visceral fat and cognitive decline| Study finds abdominal body fat linked to possible dementia | The study used deep learning, a type of machine learning and artificial intelligence, to draw conclusions from whole body imaging scans. It also builds upon earlier research correlating fat and brain atrophy. The new study utilized much higher resolution imaging, included far more subjects, broadened the age range and expanded criteria to include subcutaneous fat. It also found women more than men are subject to brain shrinkage based on fat levels. Raji, MD, PhD , of Washington University in St. Louis, who collaborated with the research team at the Pacific Brain Health Center. For the study, 10, healthy people aged 18 to 90 years old had whole body scans with MR imaging machines. Deep learning was used to determine the volume of 96 brain regions. The same scan also was used to find the amount of visceral and subcutaneous abdominal fat on the scans. Then researchers looked to see if there was a link between these types of abdominal fat and brain volume. After controlling for factors that could affect brain volume, such as age and the total volume inside the skull, researchers found higher amounts of both visceral and subcutaneous fat were associated with greater atrophy in the overall gray and white matter of their brains and the main lobes of the brain. Increased subcutaneous and visceral fat also was associated with cell loss in the hippocampus area of the brain and other areas associated with memory and thinking skills that are affected by dementia. For people who were overweight and obese with high visceral fat, those aged 20 to 39 had nearly six times the risk for overall brain atrophy when compared to people of similar age with normal levels of visceral fat; those 40 to 80 had over five times the risk. For the same groups of people who had high visceral fat, when looking at white matter atrophy in particular, people aged 20 to 39 had almost four times the risk when compared to people with normal visceral fat levels; those aged 40 to 59 had over four times the risk; and people aged 60 to 80 had over five times the risk. The results from this large data set were contextualized down to individual examples when comparing two MRI scans in two participants from the study with the same age and sex:. The study also found that women experienced a higher correlation between increased body fat and lower brain volume compared to men. Merrill said. A limitation of the study was that images were taken at one time and participants were not followed to see who developed dementia over time. Raji notes in future studies, researchers plan to follow participants over a period of time. Such work opens the possibility of future treatment trials where both body fat and brain imaging can track the outcomes of such treatment efforts. Rajpaul Attariwala, M. Currently, we do not know how interventions such as diet, exercise and weight loss drugs will affect the anatomical fat distributions in the body or if they may have secondary benefits for the brain. Adapted from a press release by Providence Southern California. One possibility is that the impaired vascular function resulting from the different conditions of the metabolic syndrome could lead to brain changes that could then lead to cognitive impairment Another core feature of the metabolic syndrome is insulin resistance which also has been linked to cognitive decline and dementia VAT rather than SAT is more strongly associated with insulin resistance and NAFLD has also been closely linked to insulin resistance , showing that different fat compartments may be associated with differential metabolic risk. Although both VAT and fatty liver have been shown to be related to impaired cognition and both are determinants of insulin resistance, their impact is different due to the different roles played by adipokines and hepatokines, respectively Those results imply the importance of assessing regional adiposity rather than central adiposity to understand the specific contribution of excess adiposity to cognition. Therefore, further studies should be done on regional fat depots to better understand the mechanism underlying the association between adiposity, metabolic syndrome, cognition, and brain changes. Investigation of regional fat in metabolically healthy obese population may shed light into these discrepancies 27 , In the present review, we have gathered data showing that regional fat depots are associated with deleterious brain changes. Regional fat depots including VAT, SAT and fatty liver were associated with smaller cerebral volumes 78 — Fatty liver and VAT but not SAT were significantly associated with smaller hippocampal volume 41 , 54 , 59 which is one of the first regions affected by AD Those results are concordant with recent evidence from our group showing associations of higher BMI with thinning of the middle temporal gyrus Overall, the present review indicates that different fat depots can affect different parts of the brain suggesting a potential role of different regional fat depots in brain atrophy and pathology, targeting those fats could then prevent deleterious impact on the brain. Brain small vessel disease which includes higher WMHs, and lacunar infarcts may lead to cognitive impairment and dementia In the present review, different regional fat depots have also been associated with higher WMHs 62 , 77 , In addition to its associations with cognitive impairment and AD 86 , WMH is prevalent in individuals with insulin resistance, metabolic syndrome and T2D , all conditions accompanied by high adiposity Furthermore, adiposity is associated with chronic low-grade systemic inflammation, which increases proinflammatory cytokine secretion Pro-inflammatory cytokines have been linked to greater volumes of WMHs which in turn are linked to cognitive impairment. As suggested by one of the studies reviewed, mechanisms by which VAT exerts a negative influence on cognitive function includes systemic inflammation Therefore, disentangling factors secreted by different fat depots affecting systemic inflammation may shed light into their role in cognitive decline and dementia. Indeed, different fat depots release different secreted factors, some of which cross readily the blood brain barrier BBB and may cause damage, ultimately leading to cognitive decline 56 , 63 , For example, pro-inflammatory factors such as leptin, IL-6, TNF-α , which are secreted by adipocytes can cross the BBB and lead to neuroinflammation, which plays a role in cognitive impairment and AD Conversely, anti-inflammatory adipocytokines such as Adiponectin , Interleukin 10 IL , , and Apelin , are associated with less adiposity and are related to cognition and AD. Neuroinflammation likely causes synaptic remodeling and neurodegeneration resulting in disruption of cognitive functioning possibly resulting from damage brain regions subserving cognition such as the hippocampus Targeting these factors could be an efficacious way to prevent or delay later cognitive decline and AD. Other factors, such as proteins are secreted from different fat depots, and may explain the role of peripheral fats in the brain. For example, Amylin, a hormone synthesized and co-secreted with insulin by pancreatic β-cells, is elevated in obesity and may share similar pathophysiology with Amyloid-β, characteristic of AD neuropathology Also, Glucagon-like peptide-1 GLP-1 , a gut released hormone, which can protect pancreatic β-cells from apoptosis and induce insulin secretion, is attracting attention as a possible link between metabolic syndrome and brain impairment , Additional factors, secreted by hepatocytes, the most common cells in the liver, are found to be related to cognition such as plasminogen activator inhibitor 1 PAI-1 , and fetuin , Indeed, in the presence of elevated fatty acids , circulating fetuin-A can induce insulin resistance and inflammatory signaling which may cause damage to the brain leading to cognitive impairment , Therefore, identifying novel factors altered due to excess fat in different abdominal regions and associated with cerebrovascular pathology, neuropathology, and impaired cognitive functioning is crucial for developing fat-specific interventions. Potential mechanisms underlying the inter-relationships of adiposity- brain changes — cognition and therapeutic modalities, is presented in Figure 2. Figure 2. Potential mechanisms underlying the adiposity- brain changes - cognition inter-relationships and therapeutic modalities. A Adiposity is commonly used to describe excess body fat or obesity. Different fat depots can be found in the body independently of central obesity. Subcutaneous adiposity refers to the accumulation of fat underneath the skin, in the adipose tissue layer. Visceral adiposity refers to the accumulation of fat in the abdominal cavity, specifically around the organs such as the liver, pancreas, and intestines. Ectopic fat refers to the accumulation of fat in areas where it is not normally found, such as the liver, muscle, and pancreas. Both types of fat are associated with increased risk of metabolic disorders such as insulin resistance, type 2 diabetes, and cardiovascular disease. Understanding the association of adiposity, brain changes and cognitive abilities would provide key insights into the mechanisms by which adiposity impacts cognitive health and to possible treatments. Lifestyle interventions, such as specific diets and physical activity may diminish accumulation of fat depots. B Adiposity is associated with chronic low-grade systemic inflammation. Different fat depots can release different proinflammatory cytokines, hormones and enzymes some of which cross readily the blood brain barrier BBB and may cause damage ultimately leading to cognitive decline. For example, pro-inflammatory factors such as leptin, secreted by adipocytes, can cross the BBB and lead to neuroinflammation, which plays a major role in cognitive impairment and AD. Conversely, anti-inflammatory adipocytokines such as adiponectin, are associated with less adiposity and are related to better cognitive functioning and lower AD risk. Treatment targeting enhancing protective factors released from adipocytes and diminishing inflammatory factors secreted from fats could be an efficacious way to prevent brain damage and ultimately support healthy cognition. C Initial evidence suggests that different fat depots affect a plethora of brain pathologies including cortical volume, the cerebral vasculature, primarily white matter hyperintensities, and neuroinflammation. These pathologies contribute to cognitive impairment and as treatments addressing the neurobiology of cognition evolve, cognitive health may be maintained in spite of accumulation of fat deposits and their respective secreted factors. Finally, sex differences should be taken into consideration as they may also contribute to the fat-brain-cognition axis. Women have overall more fat mass than men. Those differences in regional fat depots may lead to different consequences on cognition. Higher levels of VAT were associated with worsening cognitive function in men after adjustment for metabolic disorders, adipocytokines, and sex hormone levels Conversely, there was no association between adiposity and cognitive changes in women Furthermore, while VAT exacerbates the association between aging and poorer brain network covariance in both men and women, estradiol reduces the negative association in women These findings highlight the need to account for sex differences in the investigation of relationships of regional adiposity with brain and cognition. This review provides evidence for the association of different regional fat depots, cognition, and brain changes. However, this study had several limitations. First, the initial intention of our group was to conduct a meta-analysis on regional adiposity and cognition. But, due to the limited number of studies and the variability in methodologies the meta-analysis could not be conclusive as it carried high heterogeneity. The studies have different designs, sample sizes, and cognitive tests as well as different ways of assessing regional fat depots to quantify adiposity, adding complexity to the interpretation of results. Indeed, quantification of the degree of adipose tissues is different in each of the studies, as some quantify by fat volume and others by surface or percentage of fat in the different regions, making it difficult to directly compare the studies. Further prospective studies are needed to establish the relationship between regional fat depots with brain changes and cognition with similar methodologies. Only three studies in this review had longitudinal cognitive decline 56 , 60 , Considering that the duration of exposure to adiposity may affect the onset and the severity of cognitive impairment, the lack of longitudinal data for regional adiposity is a significant limitation in the field. All studies were observational studies and not clinical trials therefore no causation can be inferred. In some studies, there were no associations between regional fat and cognition. However, many of these studies included relatively young individuals e. In such young ages the range of cognitive functioning is relatively narrow, possibly contributing to the lack of associations. It is important to note that the literature on fat and cognition may suffer from selection bias since older adults with cognitive impairment are less likely to participate in research. Finally, this review focuses specifically on body fat composition, rather than on general body composition, and does not discuss muscle mass and function which are strongly associated with cognitive decline and dementia risk 18 — This review of 33 studies indicates that different regional fat depots may affect cognition and different regions of the brain. Regional fat depots, especially VAT and hepatic fat, have been associated with cognitive decline, cortical thinning and WMHs. Regional fat depots, rather than central obesity, may better explicate the association between adiposity and brain and may open horizons for new personalized fat-reducing treatments for prevention of cognitive decline. EB, SG, and MB conceived the presented idea and have made a substantial contribution to the concept and design of the manuscript. EB carried out the literature search from electronic databases, drafted the manuscript, and provided the tables. SG participated with EB to the full-text screening of the articles from the literature search, read and approved the manuscript. MB revised critically the manuscript and approved the version to be published. All authors contributed to the article and approved the submitted version. This work was funded by National Institutes of Health grants RAG, AG, and AG to MB. The authors thank Marina Nissim Milan Italy Funding. The authors are also grateful for the generosity of the LeRoy Schecter Foundation. Thanks to Marina Nissim for her generosity. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Panuganti, KK, Nguyen, M, Kshirsagar, RK, and Doerr, C. Obesity nursing In:. StatPearls : StatPearls Publishing Google Scholar. Luchsinger, JA, and Gustafson, DR. Curr Opin Clin Nutr Metab Care. doi: PubMed Abstract CrossRef Full Text Google Scholar. Gustafson, DR, and Luchsinger, JA. Alzheimers Res Ther. Ravona-Springer, R, Schnaider-Beeri, M, and Goldbourt, U. Body weight variability in midlife and risk for dementia in old age. Pedditizi, E, Peters, R, and Beckett, N. Age Ageing. Fitzpatrick, S, Gilbert, S, and Serpell, L. Systematic review: are overweight and obese individuals impaired on behavioural tasks of executive functioning? Neuropsychol Rev. Coppin, G, Nolan-Poupart, S, Jones-Gotman, M, and Small, DM. Working memory and reward association learning impairments in obesity. Cournot, MCMJ, Marquie, JC, Ansiau, D, Martinaud, C, Fonds, H, Ferrieres, J, et al. Relation between body mass index and cognitive function in healthy middle-aged men and women. Beeri, MS, Tirosh, A, Lin, HM, Golan, S, Boccara, E, Sano, M, et al. Stability in BMI over time is associated with a better cognitive trajectory in older adults. Alzheimers Dement. Gustafson, D, Rothenberg, E, Blennow, K, Steen, B, and Skoog, I. An year follow-up of overweight and risk of Alzheimer disease. Arch Intern Med. West, RK, Ravona-Springer, R, Heymann, A, Schmeidler, J, Leroith, D, Koifman, K, et al. Waist circumference is correlated with poorer cognition in elderly type 2 diabetes women. Obesity, diabetes and cognitive deficit: the Framingham heart study. Neurobiol Aging. Kuo, HK, Jones, RN, Milberg, WP, Tennstedt, S, Talbot, L, Morris, JN, et al. Cognitive function in normal-weight, overweight, and obese older adults: an analysis of the advanced cognitive training for independent and vital elderly cohort. J Am Geriatr Soc. Wotton, CJ, and Goldacre, MJ. Age at obesity and association with subsequent dementia: record linkage study. Postgrad Med J. Cova, I, Clerici, F, Rossi, A, Cucumo, V, Ghiretti, R, Maggiore, L, et al. PLoS One. Johnson, DK, Wilkins, CH, and Morris, JC. Accelerated weight loss may precede diagnosis in Alzheimer disease. Arch Neurol. Buchman, AS, Wilson, RS, Bienias, JL, Shah, RC, Evans, DA, and Bennett, DA. Change in body mass index and risk of incident Alzheimer disease. Beeri, MS, Leugrans, SE, Delbono, O, Bennett, DA, and Buchman, AS. Oudbier, SJ, Goh, J, Looijaard, SMLM, Reijnierse, EM, Meskers, CGM, and Maier, AB. Pathophysiological mechanisms explaining the association between low skeletal muscle mass and cognitive function. Yang, Y, Xiao, M, Leng, L, Jiang, S, Feng, L, Pan, G, et al. A systematic review and meta-analysis of the prevalence and correlation of mild cognitive impairment in sarcopenia. J Cachexia Sarcopenia Muscle. Brisendine, MH, and Drake, JC. Early stage Alzheimer's disease: are skeletal muscle and exercise the key? J Appl Physiol. Janssen, I, Katzmarzyk, PT, and Ross, R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr. Staaf, J, Labmayr, V, Paulmichl, K, Manell, H, Cen, J, Ciba, I, et al. Pancreatic fat is associated with metabolic syndrome and visceral fat but not beta-cell function or body mass index in pediatric obesity. Prentice, AM, and Jebb, SA. Beyond body mass index. Obes Rev. Tchkonia, T, Morbeck, DE, Von Zglinicki, T, Van Deursen, J, Lustgarten, J, Scrable, H, et al. Fat tissue, aging, and cellular senescence. Aging Cell. Kuk, JL, Saunders, TJ, Davidson, LE, and Ross, R. Age-related changes in total and regional fat distribution. Ageing Res Rev. Stefan, N. Causes, consequences, and treatment of metabolically unhealthy fat distribution. Lancet Diab Endocrinol. Schulze, MB. Metabolic health in normal-weight and obese individuals. Franzosi, MG. Should we continue to use BMI as a cardiovascular risk factor? Després, JP. Is visceral obesity the cause of the metabolic syndrome? Ann Med. CrossRef Full Text Google Scholar. Manolopoulos, KN, Karpe, F, and Frayn, KN. Gluteofemoral body fat as a determinant of metabolic health. Int J Obes. Smits, MM, and Van Geenen, EJ. The clinical significance of pancreatic steatosis. Nat Rev Gastroenterol Hepatol. Stefan, N, and Cusi, K. A global view of the interplay between non-alcoholic fatty liver disease and diabetes. Yang, KC, Hung, HF, Lu, CW, Chang, HH, Lee, LT, and Huang, KC. Association of non-alcoholic fatty liver disease with metabolic syndrome independently of central obesity and insulin resistance. Sci Rep. Kivipelto, M, Ngandu, T, Fratiglioni, L, Viitanen, M, Kåreholt, I, Winblad, B, et al. Obesity and vascular risk factors at midlife and the risk of dementia and Alzheimer disease. Spauwen, PJ, Murphy, RA, Jónsson, PV, Sigurdsson, S, Garcia, ME, Eiriksdottir, G, et al. Associations of fat and muscle tissue with cognitive status in older adults: the AGES-Reykjavik study. Heymsfield, SB, Peterson, CM, Thomas, DM, Heo, MS, and Schuna, JM Jr. A quantitative critical review. Karastergiou, K, Smith, SR, Greenberg, AS, and Fried, SK. Sex differences in human adipose tissues—the biology of pear shape. Biol Sex Differ. Moh, MC, Low, S, Ng, TP, Wang, J, Ang, SF, Tan, C, et al. Association of traditional and novel measures of central obesity with cognitive performance in older multi-ethnic Asians with type 2 diabetes. Clin Obesity. Cereda, E, Sansone, V, Meola, G, and Malavazos, AE. Increased visceral adipose tissue rather than BMI as a risk factor for dementia. Beller, E, Lorbeer, R, Keeser, D, Schoeppe, F, Sellner, S, Hetterich, H, et al. Hepatic fat is superior to BMI, visceral and pancreatic fat as a potential risk biomarker for neurodegenerative disease. Eur Radiol. Tchkonia, T, Thomou, T, Zhu, YI, Karagiannides, I, Pothoulakis, C, Jensen, MD, et al. Mechanisms and metabolic implications of regional differences among fat depots. Cell Metab. Wang, H, Chen, YE, and Eitzman, DT. Imaging body fat: techniques and cardiometabolic implications. Arterioscler Thromb Vasc Biol. Jackson, AS, Pollock, ML, Graves, JE, and Mahar, MT. Reliability and validity of bioelectrical impedance in determining body composition. Kim, YJ, Park, JW, Kim, JW, Park, CS, Gonzalez, JPS, Lee, SH, et al. Computerized automated quantification of subcutaneous and visceral adipose tissue from computed tomography scans: development and validation study. JMIR Med Inform. Chaudry, O, Grimm, A, Friedberger, A, Kemmler, W, Uder, M, Jakob, F, et al. Magnetic resonance imaging and bioelectrical impedance analysis to assess visceral and abdominal adipose tissue. Borga, M, West, J, Bell, JD, Harvey, NC, Romu, T, Heymsfield, SB, et al. Advanced body composition assessment: from body mass index to body composition profiling. J Investig Med. Hernaez, R, Lazo, M, Bonekamp, S, Kamel, I, Brancati, FL, Guallar, E, et al. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: a meta-analysis. Zhang, M, and Yang, XJ. Effects of a high fat diet on intestinal microbiota and gastrointestinal diseases. World J Gastroenterol. Ghosh, S, and DeCoffe, D. Influence of the gut microbiota and its metabolites on obesity and metabolic disease. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. Anand, SS, Friedrich, MG, Lee, DS, Awadalla, P, Després, JP, Desai, D, et al. Evaluation of adiposity and cognitive function in adults. JAMA Netw Open. Zsido, RG, Heinrich, M, Slavich, GM, Beyer, F, Masouleh, SK, Kratzsch, J, et al. Association of estradiol and visceral fat with structural brain networks and memory performance in adults, e Isaac, V, Sim, S, Zheng, H, Zagorodnov, V, Tai, ES, and Chee, M. Adverse associations between visceral adiposity, brain structure, and cognitive performance in healthy elderly. Front Aging Neurosci. Kim, S, Yi, HA, Won, KS, Lee, JS, and Kim, HW. Kanaya, AM, Lindquist, K, Harris, TB, Launer, L, Rosano, C, Satterfield, S, et al. Total and regional adiposity and cognitive change in older adults: the health, aging and body composition ABC study. Yoon, DH, Choi, SH, Yu, JH, Ha, JH, Ryu, SH, and Park, DH. The relationship between visceral adiposity and cognitive performance in older adults. Kim, J, Choi, KH, Cho, SG, Kang, SR, Yoo, SW, Kwon, SY, et al. Hsu, FC, Yuan, M, Bowden, DW, Xu, J, Smith, SC, Wagenknecht, LE, et al. Adiposity is inversely associated with hippocampal volume in African Americans and European Americans with diabetes. J Diabetes Complicat. Gerber, Y, VanWagner, LB, Yaffe, K, Terry, JG, Rana, JS, Reis, JP, et al. Non-alcoholic fatty liver disease and cognitive function in middle-aged adults: the CARDIA study. BMC Gastroenterol. Meng, H, and Gorniak, SL. Effects of adiposity on postural control and cognition in older adults. Gait Posture. StatPearls Publishing, Cannavale, CN, Bailey, M, Edwards, CG, Thompson, SV, Walk, AM, Burd, NA, et al. Systemic inflammation mediates the negative relationship between visceral adiposity and cognitive control. Int J Psychophysiol. Mazzoccoli, G, Dagostino, MP, Vinciguerra, M, Ciccone, F, Paroni, G, Seripa, D, et al. An association study between epicardial fat thickness and cognitive impairment in the elderly. Am J Phys Heart Circ Phys. Verrusio, W, Renzi, A, Magro, VM, Musumeci, M, Andreozzi, P, and Cacciafesta, M. Association between epicardial fat thickness and cognitive function in elderly. A preliminary study. Ann Ist Super Sanita. Wang, Y, Li, Y, Liu, K, Han, X, Dong, Y, Wang, X, et al. Nonalcoholic fatty liver disease, serum cytokines, and dementia among rural-dwelling older adults in China: a population-based study. Eur J Neurol. Filipović, B, Marković, O, Đurić, V, and Filipović, B. Cognitive changes and brain volume reduction in patients with nonalcoholic fatty liver disease. Can J Gastroenterol Hepatol. Pasha, EP, Birdsill, A, Parker, P, Elmenshawy, A, Tanaka, H, and Haley, AP. Yu, Q, He, R, Jiang, H, Wu, J, Xi, Z, He, K, et al. Association between metabolic dysfunction-associated fatty liver disease and cognitive impairment. J Clin Transl Hepatol. Celikbilek, A, Celikbilek, M, and Bozkurt, G. Cognitive assessment of patients with nonalcoholic fatty liver disease. Eur J Gastroenterol Hepatol. Seo, SW, Gottesman, RF, Clark, JM, Hernaez, R, Chang, Y, Kim, C, et al. Nonalcoholic fatty liver disease is associated with cognitive function in adults. Moretti, R, Giuffré, M, Crocè, LS, Gazzin, S, and Tiribelli, C. Nonalcoholic fatty liver disease and altered neuropsychological functions in patients with subcortical vascular dementia. J Personal Med. Raschpichler, M, Straatman, K, Schroeter, ML, Arelin, K, Schlögl, H, Fritzsch, D, et al. Abdominal fat distribution and its relationship to brain changes: the differential effects of age on cerebellar structure and function: a cross-sectional, exploratory study. BMJ Open. Cárdenas, D, Madinabeitia, I, Vera, J, de Teresa, C, Alarcón, F, Jiménez, R, et al. Better brain connectivity is associated with higher total fat mass and lower visceral adipose tissue in military pilots. Kaur, S, Gonzales, MM, Strasser, B, Pasha, E, McNeely, J, Tanaka, H, et al. Central adiposity and cortical thickness in midlife. Psychosom Med. Lee, H, Seo, HS, Kim, RE, Lee, SK, Lee, YH, and Shin, C. Obesity and muscle may have synergic effect more than independent effects on brain volume in community-based elderly. Kim, KW, Seo, H, Kwak, MS, and Kim, D. Visceral obesity is associated with white matter hyperintensity and lacunar infarct. Visceral fat is associated with lower brain volume in healthy middle-aged adults. Ann Neurol. VanWagner, LB, Terry, JG, Chow, LS, Alman, AC, Kang, H, Ingram, KH, et al. Nonalcoholic fatty liver disease and measures of early brain health in middle-aged adults: the CARDIA study. |
| Hidden belly fat linked to brain inflammation and dementia, study finds | Arch Ffat Psychiatry. Furthermore, the Visceral fat and cognitive decline of BMI as a phenotypic marker fecline adiposity across populations differing in race and ethnicity is now questioned The role of hepatokines in NAFLD. An association study between epicardial fat thickness and cognitive impairment in the elderly. Figure 2. The authors thank Marina Nissim Milan Italy Funding. |
| Bigger belly in 40s and 50s linked to early signs of Alzheimer’s disease | CNN | Profile My News Sign Out. Association between visceral fat area and cortical thickness. For qualitative analysis, differences in measures between higher regional fat depots and control groups or the appropriate results were reported for individual studies. by Nanyang Technological University. Benjamini, Y. |
0 thoughts on “Visceral fat and cognitive decline”