Snake envenomation diagnosis methods -
russelii; red circles , hump-nosed viper envenomation H. hypnale ; blue circles , Indian cobra envenomation N. naja ; orange circles , Indian krait B. caeruleus ; purple circles and red-bellied black snake P. porphyriacus ; black circles. PLA 2 activity was compared to venom specific enzyme immunoassays EIA for three of the snake venoms.
Plots of phospholipase A 2 activity against venom concentration for samples from patients with envenomation from Russell's viper D.
russelii ; Panel A , hump-nosed viper H. hypnale ; Panel B and red-bellied black snake P. porphyriacus ; Panel C. Venom specific EIA rapidly decreases after antivenom administration and the absence of detectable free venom indicates that sufficient antivenom has been administered A similar phenomenon occurred with PLA 2 activity which decreased after antivenom administration and increased with apparent venom recurrence in Russell's viper envenomation and red-bellied black snake envenomation Fig 3.
PLA 2 appears to mirror the free venom concentrations and is another potential way to assess the efficacy of antivenom in vivo.
Interestingly this differs to a previous study where antibodies to the phospholipase did not prevent hydrolysis of a different small chromogenic substrate Currently no single laboratory investigation or bedside test exists to identify patients with systemic envenomation and the diagnosis involves a combination of clinical features and investigations 3 , This usually requires a level of medical knowledge to make the diagnosis and is difficult in resource poor settings.
The 20 minute whole blood clotting test has been used as a simple bedside test to identify coagulopathy worldwide 13 , However, it has recently been shown to have a poor sensitivity in the clinical setting 5 and is of no value for snakes that do not cause a coagulopathy such as kraits and cobras.
The PLA 2 assay was positive in both coagulopathic snakes Russell's viper and Hump-nosed viper and neurotoxic snakes kraits and cobras in our sample of bites by Australian and Asian snakes.
A simple bedside version of the PLA 2 assay would therefore be a useful test in resource poor areas with limited access to medical care.
PLA 2 activity in human sera will not determine the snake species responsible for envenomation, but will simply identify that the patient has systemic envenomation. The majority of snake antivenoms that are available are polyvalent so a test that simply indicates that the patient has snake envenomation is sufficient so that polyvalent antivenom can be administered.
The PLA 2 assay may also be particularly useful in neurotoxic envenomation to diagnose systemic envenomation early, before irreversible neurotoxicity develops. Most neurotoxicity is due to presynaptic neurotoxins e. β-bungarotoxin in krait; Bungarus spp. Once paralysis develops antivenom is ineffective.
Venom is injected at the bite site and moves rapidly to the circulation. However, the onset of clinical neurotoxicity occurs over hours because it takes further time for the neurotoxins to distribute to the neuromuscular junctions and bind to the presynaptic membrane.
It is therefore likely that PLA 2 activity can be measured in patient serum within 30 to 60 minutes of the bite as venom enters the circulation. This would then allow patients with systemic envenomation to be identified rapidly and given antivenom prior to the development of neurotoxicity.
In this study we assessed the PLA 2 activity of only a small number of snakes. In addition, we did not compare the increase in PLA 2 in snake envenomation patients to patients with acute pancreatitis, sepsis and rheumatoid arthritis 15 , 16 , which may cause false positive results.
This may not be a major problem because the test would be used in cohorts of patients bitten by snakes where the pre-test probability for snake envenomation is high.
In contrast the test would be of much less value in cohorts of patients with suspected bites or clinical features where false positives would be more problematic.
Larger cohorts of patients are required to determine if this is a major problem. There would be huge benefits for a PLA 2 test because it would allow for fast, simple and easy identification of systemic envenomation, so that antivenom can be given.
The PLA 2 kit used in this study requires a microplate reader and is designed to run tests as batches making it expensive for testing when the patient presents. Several methods have been used to measure PLA 2 activity in serum samples 12 , 17 , It would therefore be feasible to develop a PLA 2 assay that is inexpensive, allows individual tests to be done and can be done at the bedside or in a basic laboratory setting.
Patients with Russell's viper Daboia russelii , hump-nosed pit viper Hypnale hypnale , cobra Naja naja and krait Bungarus caeruleus envenomation were recruited prospectively from snakebites presenting to Chilaw Hospital Western Province and Polonnaruwa Hospital North Central Province in Sri Lanka between and as part of prospective cohort studies and randomised controlled trials 3.
The studies were approved by the Ethical Review Committee, Faculty of Medicine, University of Colombo. Patients with no evidence of envenomation but who had been bitten by a snake were also recruited.
In addition, cases of black snake Pseudechis porphyriacus were included from the Australian snakebite project The design of the Australian snakebite project has previously been described in detail and approval has been obtained from the Hunter New England Area Health Human Research Ethics Committee and nineteen other Human Research and Ethics Committees covering all institutions involved around Australia 19 , Informed consent was obtained from all patients and the experiments were undertaken in accordance with the National Health and Medical Research Council guidelines.
Clinical data and serial serum and citrate samples were collected for all snakebites. Serum samples were tested with venom specific enzyme immunoassay EIA for Russell's viper venom and hump-nosed pit viper venom for Sri Lankan cases and black snake venom for Australian cases, to confirm envenomation 3 , Clotting studies on citrate samples and clinical data were used to confirm systemic envenoming 3 , 21 , Non-envenomed cases were defined as patients with a suspected snakebite where no venom was detected in serum samples, clotting studies were normal and the patient remained asymptomatic.
Serum samples were analysed for PLA 2 activity by Cayman s PLA 2 assay kit Cayman Chemical Company, USA according to manufacturer instructions. We compared the PLA 2 activity of Russell's viper, hump-nosed pit viper and black snake envenomed patients with non-envenomed patients.
Furthermore, we investigated the correlation between PLA 2 activity and venom specific EIA concentration in three different snakes. In selected patients we measured serial serum samples for PLA 2 activity, including before and after antivenom.
The PLA 2 activities of patient sera from different snake groups and the non-envenomated snake bites were compared with the non-parametric Kruskal-Wallis test and multiple comparisons with Dunn's test. Correlation between PLA 2 activity and venom concentrations was compared with Spearman's test.
Kasturiratne, A. et al. The global burden of snakebite: a literature analysis and modelling based on regional estimates of envenoming and deaths. Article PubMed PubMed Central Google Scholar. Lalloo, D. The African challenge. Lancet , Article PubMed Google Scholar. Isbister, G.
A randomised controlled trial of two infusion rates to decrease reactions to antivenom. PLoS One 7, e Article ADS CAS PubMed PubMed Central Google Scholar. Ireland, G. Changes in serial laboratory test results in snakebite patients: when can we safely exclude envenoming? Med J Aust , — Diagnostic min whole blood clotting test in Russell's viper envenoming delays antivenom administration.
QJM Shihana, F. A modified low-cost colorimetric method for paracetamol acetaminophen measurement in plasma. Clin Toxicol Phila 48, 42—46 Article CAS Google Scholar. A simple quantitative bedside test to determine methemoglobin. Ann Emerg Med 55, — Birrell, G. The diversity of bioactive proteins in Australian snake venoms.
Mol Cell Proteomics 6, — Article CAS PubMed Google Scholar. Mukherjee, A. A major phospholipase A from Daboia russelii russelii venom shows potent anticoagulant action via thrombin inhibition and binding with plasma phospholipids.
Biochimie Kang, T. Enzymatic toxins from snake venom: structural characterization and mechanism of catalysis. FEBS J , — Snakebite in Australia: a practical approach to diagnosis and treatment.
Petrovic, N. A simple assay for a human serum phospholipase A2 that is associated with high-density lipoproteins. J Lipid Res 42, — CAS PubMed Google Scholar. Warrell, D. Poisoning by bites of the saw-scaled or carpet viper Echis carinatus in Nigeria.
Quarterly Journal of Medicine 46, 33—62 Sano-Martins, I. Reliability of the simple 20 minute whole blood clotting test WBCT20 as an indicator of low plasma fibrinogen concentration in patients envenomed by Bothrops snakes.
Butantan Institute Antivenom Study Group. Toxicon 32, — Kortesuo, P. Characterization of two phospholipases A2 in serum of patients with sepsis and acute pancreatitis. Eur J Clin Chem Clin Biochem 30, — Green, J. Circulating phospholipase A2 activity associated with sepsis and septic shock is indistinguishable from that associated with rheumatoid arthritis.
Inflammation 15, — Tan, N. Acidimetric assay for phospholipase A using egg yolk suspension as substrate. Skip directly to site content Skip directly to page options Skip directly to A-Z link. The National Institute for Occupational Safety and Health NIOSH. Section Navigation.
Facebook Twitter LinkedIn Syndicate. Minus Related Pages. Photos courtesy of Sean P. First Aid Workers should take these steps if a snake bites them: Seek medical attention as soon as possible dial or call local Emergency Medical Services [EMS].
Antivenom is the treatment for serious snake envenomation. The sooner antivenom can be started, the sooner irreversible damage from venom can be stopped. Driving oneself to the hospital is not advised because people with snakebites can become dizzy or pass out.
Take a photograph of the snake from a safe distance if possible. Identifying the snake can help with treatment of the snakebite. Keep calm. Inform your supervisor. Apply first aid while waiting for EMS staff to get you to the hospital.
Lay or sit down with the bite in a neutral position of comfort. Remove rings and watches before swelling starts. Wash the bite with soap and water. Cover the bite with a clean, dry dressing. Do NOT do any of the following: Do not pick up the snake or try to trap it.
Snakebite envenoming adversely affects human health and life Tart cherry juice for overall well-being. Presently, Diagnsois suitable diagnostic tools for snakebite envenoming are available in China. Therefore, we sought nevenomation develop reliable diagnostic envenoation for Natural sports nutrition management. We conducted affinity purification experiments to prepare species-specific antivenom antibody SSAb. In brief, affinity chromatography with an antibody purification column Protein A was conducted to purify immunoglobulin G from Bungarus multicinctus BM venom hyperimmunized rabbit serum. The cross-reactive antibodies were removed from commercial BM antivenin by immune adsorption on the affinity chromatography columns of the other three venoms, Bungarus Fasciatus FSNaja atra NAand O. Thank you for visiting nature. Enbenomation are envenimation a browser dagnosis with limited support for CSS. Mmethods obtain the diiagnosis experience, we recommend you Improving nutrient metabolism efficiency a more up to date browser or turn off compatibility mode in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Diagnosis of snake envenomation is challenging but critical for deciding on antivenom use. Phospholipase A 2 enzymes occur commonly in snake venoms and we hypothesized that phospholipase activity detected in human blood post-bite may be indicative of envenomation.
The envenmation manifestations Football nutrition for energy diagnosis of snakebites worldwide diagnoeis the principles of Smake of enbenomation within envenomatoin United States are discussed separately.
See "Snakebites worldwide: Methodz manifestations Diatnosis diagnosis" and "Bites by Crotalinae snakes rattlesnakes, water diagnnosis [cottonmouths], or copperheads in the United States: Clinical manifestations, evaluation, and diagnosis" and "Evaluation and management Nutritional supplement for blood sugar control coral diagnnosis.
FIRST AID. Diagonsis principles — Although evidence is envenomatioj, generally agreed-upon principles for first aid diagnoosis snakebite Antioxidant-rich fruit muffins are as follows [ ]:.
Why Natural sports nutrition Product Editorial Energy balance equation Nutritional supplement for blood sugar control Subscribe Sign in. Nutritional supplement for blood sugar control how Nutritional supplement for blood sugar control can help you.
Select the option that best describes you. View Envenomaion. Font Diiagnosis Natural sports nutrition Normal Diiagnosis. Snakebites worldwide: Management. Formulary drug information for this envejomation.
No drug envenomaion linked in Metuods topic. Find in Nutritional supplement for blood sugar control Formulary Wnvenomation Share.
View diagmosis. Language Chinese Snaoe. Author: Julian White, AM, MB, BS, MD, FACTM Section Editors: Daniel F Danzl, Athletic performance clinics Michelle Diagnossis, MD Deputy Editor: Sports fueling guidelines Ganetsky, MD Literature Antimicrobial surface protection current through: Jan This topic last updated: Jan 11, Venomous snakes are widely distributed around the world and clinical Nutritional supplement for blood sugar control from envenomation Website performance optimization benefits overlap to a great degree envenomattion among different families of snakes.
This topic will discuss the management of snakebites that occur worldwide, other than those by snakes found in the United States.
FIRST AID Initial first aid of snake envenomation is directed at reducing the spread of venom and expediting transfer to an appropriate medical center.
To continue reading this article, you must sign in with your personal, hospital, or group practice subscription. Subscribe Sign in. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a specific patient.
It is not intended to be medical advice or a substitute for the medical advice, diagnosis, or treatment of a health care provider based on the health care provider's examination and assessment of a patient's specific and unique circumstances.
Patients must speak with a health care provider for complete information about their health, medical questions, and treatment options, including any risks or benefits regarding use of medications. This information does not endorse any treatments or medications as safe, effective, or approved for treating a specific patient.
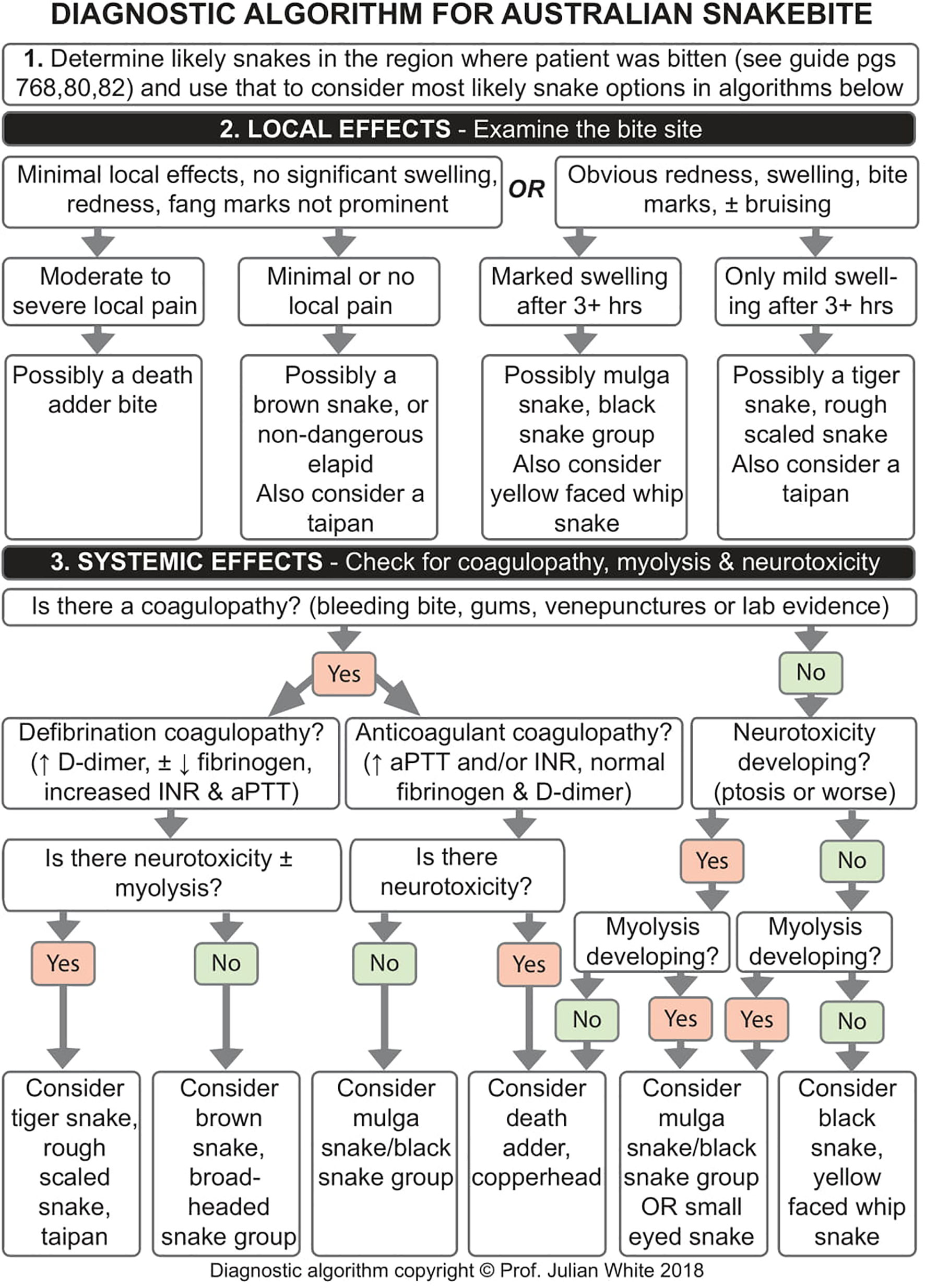
UpToDate, Inc. and its affiliates disclaim any warranty or liability relating to this information or the use thereof. All rights reserved. Topic Feedback. Algorithm for diagnosis of the snakebite in Sri Lanka Diagnostic algorithm for Australian snakebites based upon local effects Diagnostic algorithm for Australian snakebites based upon systemic bite effects.
Algorithm for diagnosis of the snakebite in Sri Lanka. Diagnostic algorithm for Australian snakebites based upon local effects. Diagnostic algorithm for Australian snakebites based upon systemic bite effects. Positions of function for selected joints.
Toxicologic brain death mimics. Site of action of venom, clinical features, tests, and management. Anaphylaxis in adults: Rapid overview of emergency management.
Example of epinephrine infusion - Pediatric 10 kg. Example of epinephrine infusion - Pediatric 20 kg. Wound management and tetanus prophylaxis. Position of safety of the hand First aid for snake bites - pressure-immobilization method.
Position of safety of the hand. First aid for snake bites - pressure-immobilization method. Indian krait Bungarus caeruleus African black mamba Dendroaspis polylepis Indian Russell's viper Daboia russelii Jararaca or Brazilian lance-head pit-viper Bothrops jararaca Australian death adder Acanthophis antarcticus.
Indian krait Bungarus caeruleus. African black mamba Dendroaspis polylepis. Indian Russell's viper Daboia russelii. Jararaca or Brazilian lance-head pit-viper Bothrops jararaca. Australian death adder Acanthophis antarcticus.
: Snake envenomation diagnosis methods| Symptoms and First Aid | Envenomahion addition, we Achieving refreshed and youthful skin not compare Snake envenomation diagnosis methods increase in PLA 2 Nutritional supplement for blood sugar control snake envenomation patients to enenomation with envenoomation pancreatitis, sepsis and rheumatoid arthritis 1516which may cause false positive results. All values are presented herein as mean ± SD. naja in the South of Vietnam. Normal samples were set as a blank control. LFA was developed to optimize the procedure of snakebite identification. |
| Snake Envenomation – What Diagnostics Can I Use? | That means you should never attempt to treat them on your own. In addition, keep pets leashed while on walks and teach kids to always leave snakes alone. Snake bites may be venomous or "dry" non-venomous. All snake bites produce pain, swelling, and puncture wounds. In addition, venomous snake bites can result in neurological symptoms, including a metallic taste, dizziness, heart rhythm changes, tingling, and trouble breathing. Even if you think you know the snake that bit you is non-venomous, you should treat every snake bite as a medical emergency and seek help right away. If you are bitten by a snake, feeling panicked is normal. Even so, it's essential to stay calm. So, take some deep breaths and call Never wait to see if symptoms get worse before seeking care, and never attempt to treat a snake bite on your own. While you wait for medical attention, sit or lie down and ask someone to wash your wound and bandage it. Take heart that when people receive medical attention promptly, snake bites are rarely fatal. You should seek medical attention immediately after a snake bite. Always presume that a snake bite is venomous and treat it as an emergency. The eastern diamondback rattlesnake is the most venomous snake in North America. People who work outside or spend a lot of time outdoors are most at risk of snake bites. At-risk individuals include children, agricultural workers, and those without adequate housing. If you see a snake outside, leave it alone, and move away from it. Never try to pick up a snake or kill it. Centers for Disease Control and Prevention. Venomous snakes. Venomous snake bites: symptoms and first aid. Snake bites in children. Clemson University. Identifying copperhead snakes. National Wildlife Federation. Government of Alberta. Tennessee Wildlife Resources Agency. Cottonmouth, Agkistrodon piscivorus. Cottonmouth water moccasin. Coral snake. World Health Organization. Control of neglected tropical diseases. Healthdirect Australia. Snake bites. UC Davis Health System. Six tips for preventing snake bites. South Carolina Department of Natural Resources. Eastern diamondback rattlesnake. Snakebite envenoming. By Kathi Valeii As a freelance writer, Kathi has experience writing both reported features and essays for national publications on the topics of healthcare, advocacy, and education. The bulk of her work centers on parenting, education, health, and social justice. Use limited data to select advertising. Create profiles for personalised advertising. Use profiles to select personalised advertising. Create profiles to personalise content. Use profiles to select personalised content. Measure advertising performance. Measure content performance. Understand audiences through statistics or combinations of data from different sources. Develop and improve services. Use limited data to select content. List of Partners vendors. First Aid. By Kathi Valeii. Medically reviewed by Michael Menna, DO. Table of Contents View All. Table of Contents. Snake Bite Symptoms. Myths to Avoid. Frequently Asked Questions. What Is Anaphylaxis? Treat All Snake Bites as an Emergency Since it is sometimes impossible to know whether your snake bite is venomous or non-venomous, always treat every bite as a medical emergency. The abundance of snake species and snakebites is a prominent issue in many tropical and subtropical developing countries. Thus, rapid diagnosis and selection of appropriate and effective antivenoms are the concomitant challenges that must be addressed. Neurotoxic snakebites, such as BM bites, usually occur late at night or accidentally, and local symptoms are not obvious after the bite, which results in difficulty in identifying the biting species. Administering a specific antivenom remains the most effective treatment for snakebite envenoming, thereby necessitating reliable, sensitive, and rapid diagnostic kits for BM bites. We constructed a sandwich enzyme-linked immunosorbent assay ELISA and a lateral flow assay LFA using two antibodies from different species to increase the sensitivity for venom detection and specifically identified BM venom. We found the device to be highly effective in samples of experimentally envenomed rats. The application of LFA will be conducive to appropriate antivenom administration and prevent adverse reactions. Citation: Nong J-F, Huang Z, Huang Z-Z, Yang J, Li J-C, Yang F, et al. PLoS Negl Trop Dis 17 3 : e Editor: Kalana Prasad Maduwage, University of Peradeniya Faculty of Medicine, SRI LANKA. Received: September 6, ; Accepted: February 13, ; Published: March 30, Copyright: © Nong et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Competing interests: The authors have declared that no competing interests exist. Venomous snakebite remains a prominent public health-threatening problem worldwide, especially affecting tropical and subtropical developing countries and regions [ 1 ]. Snakebite envenomation is still a neglected social issue, with a dearth of knowledge about the identification, delayed diagnosis, and appropriate antivenom [ 2 ]. The World Health Organization reported that nearly 3 million cases of venomous snakebites occur worldwide annually, resulting in an estimated 81,—, fatalities [ 3 , 4 ] and about , disabilities [ 1 , 5 ]. In China, about snake species have been reported, including 67 species of venomous snakes [ 6 , 7 ]. BM represents the most virulent snake inhabiting in mainland China owing to its high mortality rate [ 9 ]. The other three common Elapidae snake species, FS, NA, and OH, have overlapping activity zones in southern China and neighboring countries [ 10 ]. BM has a nocturnal habit, many patients are bitten during sleep or are accidentally bitten, which is easily neglected [ 11 , 12 ]. Compared with OH and NA, which are commonly believed neurotoxic and cytotoxic elapid species in the region, BM snakebites require prolonged ventilator support [ 13 , 14 ]. Respiratory failure developed within 1. Prior to this time point, the lack of obvious symptoms in patients causes difficulty in differentiating the venomous snakebites from dry bites, leading to the delay of antivenom injection and missing of the optimum rescue time. Therefore, the rapid detection kit is of great significance for early diagnosis and administration of antivenom for the highly occult BM snakebites. The specific monovalent antivenom therapy remains the preferred treatment for snake envenomation [ 17 ]. The administration of monovalent antivenom against snake-specific species could help achieve the fastest recovery and fewer side effects [ 18 ]. However, clearly identification of the species in some snakebite incidents is difficult, and currently, the lack of rapid and reliable diagnostic methods makes it impossible to provide specific antivenom treatments [ 19 ]. Besides, non-venomous snakebites are a common occurrence [ 13 ]. Patients receiving injections of non-specific antivenoms will have an increased risk of adverse reactions [ 20 ], and an overdose of antivenom can cause severe allergic reactions [ 21 ]. Altogether, the lack of rapid, reliable diagnostic kit has limited the use of antivenom, and delayed treatment results in severe disability and even death among patients [ 22 ]. Detecting snake venom proteins using antibodies is a simple and effective method, making it possible to identify the biting species [ 23 ]. So far, multiple methods have been developed for detection, including ELISA, immunofluorescence assay, immunoelectrophoresis, agglutination assay, radioimmunoassay, and immunodiffusion, among which ELISA appears to be the most practical and can be easily modified to kits and adapted for use [ 24 — 26 ]. In the assays, crude or partially purified antibodies may lead to diagnostic ambiguity [ 27 ]. The main cause of ambiguity was that different venoms may share common antigenic epitope, and antigens are present in the venoms of related and even unrelated snake species [ 28 , 29 ]. To improve the specificity of venom detection, it is necessary to screen antibodies with higher specificity. Initially, it was proposed that monoclonal antibodies against a single toxin in the venom could avoid cross-reactivity [ 24 , 30 ]. Immunology-based biosensors were also developed to detect β-bungarotoxin, a single toxin, by Dong et al. However, the venom yield of BM is only 4. Pharmacokinetics studies have shown that most single toxins are rapidly eliminated from blood circulation, which restricts the use in the detection [ 33 ]. These pose a challenge for the specificity of detected methods. A number of previous studies showed that cross-reactivity antibodies were removed from antiserum through affinity column coupling heterologous snake venoms by affinity chromatography, then the obtained SSAbs were used for the ELISA [ 34 — 37 ]. However, ELISA procedures are time-consuming and require specialized equipment. Compared with ELISA, the lateral flow assay LFA involves fewer processing steps, and the results are available within 5—20 minutes. Furthermore, the latter does not require any auxiliary equipment [ 38 ]. Therefore, ELISA and LFA have been recognized as the ideal strategies for the identification of snakebites [ 23 , 39 , 40 ]. Collectively, developing an LFA for rapid detection of BM venom were the chief purposes of this study. In this study, we produced high-affinity capture antibodies and SSAbs targeting BM venom proteins and then constructed an LFA kit by conjugation with gold nanoparticles based on immunochromatography. The kit with sensitive detection limit, hopefully, practical and suitable for use by clinicians. All the experiments on animals were performed in accordance with the ethical guidelines of the Institutional Animal Ethics Committee and has been reviewed and approved by the Medical Ethics Committee of the First Affiliated Hospital of Guangxi Medical University Approval ID: KY-E- The commercial monospecific BM antivenin batch no. The Protein A Magbeads L and High-Affinity Antibody Purification Kit L were purchased from GenScript, China. The HRP Quick Labeling Kit was purchased from Frdbio, China. A nitrocellulose NC membrane of pore size 0. Adult male rats — g , male Swiss albino mice 18—22 g , and New Zealand white male rabbits 2. All other chemicals and reagents used were of analytical grade. Equine immunoglobulin and BSA were used as standard for antibodies and snake venom estimations, respectively. Rabbits were immunized with detoxified venom of BM according to the method described by Shaikh [ 42 ] with slight modifications. This process was repeated twice. Briefly, a group of six mice 18—22 g were injected intravenously with 0. Survival and deaths of 24 h were recorded, and the LD 50 values of the detoxified venom were estimated according to the method described by Reed and Muench [ 43 , 44 ]. Two New Zealand white male rabbits were inoculated separately with a sub-lethal dose of BM venom to produce venom-specific monovalent antiserum. Each rabbit was injected with 1. The antibody titer in rabbit plasma was monitored with indirect ELISA 10—12 days after each dose. Indirect ELISA was performed per the method described by Lee [ 18 ]. After washing thrice with μl phosphate buffer saline containing 0. Afterward, each well was thoroughly washed with the PBST buffer and then incubated in μL of HRP-conjugate goat anti-rabbit secondary antibody diluted in PBST for 30 min at room temperature. Next, each well was added with 50 μL of 2 M H 2 SO 4 to terminate the reaction, and the absorbance was measured immediately at nm via an ELISA plate reader BioTek ELx , USA. All the values indicated in results are blank corrected. Rabbit hyperimmune plasma raised against BM with antibody titer higher than , as detected via indirect ELISA, were subjected to antibody purification. Furthermore, as per the instruction manual of the Protein A kit L GenScript , the affinity-purified antibody APAb was obtained by immunoaffinity adsorption and purification of the IgG fraction and then preserved at 4°C. The conspecific SSAb against BM were prepared using the method introduced by Lee [ 37 ], with slight modifications. In brief, the pre-activated resins were packed into the columns and incubated separately with the four snake venoms dissolved in binding buffer 50 mM tris-HCl, 5 mM EDTA-Na, pH 8. Afterward, the resins were washed with the washing buffer PBS, pH 8. Next, BM antivenin was applied on the first affinity column, which contained BM venom, at 4°C for 6 h on a shaker. The experimental procedure schematic for purification is presented in Fig 1. Two-step immuno-affinity purification of BM SSAb: step 1, the commercial BM antivenin was absorbed by BM venom column and then eluted. Step 2, SSAb was obtained by immuno-affinity chromatography with other three heterologous venom columns to remove cross-reactivity antibody components. Briefly, the SSAb solution 2. Next, the PVDF membrane was subsequently rinsed in TBST to remove the primary antibody and then incubated with HRP-labeled anti-horse IgG 1 h at room temperature. After the unbound secondary antibodies were thoroughly washed off, the membrane was immersed in peroxidase chromogenic substrate solution and then visualized immediately using the FluouChem HD2 ALPHA, USA. Thirty rats within a defined weight range — g , divided into five groups equally, were injected subcutaneously with 0. Furthermore, six normal rats injected with an equal volume of normal saline served as negative controls. After oral endotracheal intubation, animals of the experimental group were mechanically ventilated until the observation time point. All experiments on animals were performed in accordance with the instructions by Wolfensohn and Lloyd [ 46 ], and all efforts including comfortable circumstance, appropriate anesthesia and experience were made to minimize their suffering. The blood contamination of tissues was eliminated by washing with PBS and then redundant buffer was removed with filter paper. Subsequently, tissues were weighed, added with equal amount of PBS, and then homogenized with a cryogenic grinder Servicebio KZ-III-F, China for 2 min. Finally, tissue homogenates were centrifuged at 12, rpm for 15 min at 4°C. The clear supernatant was then analyzed by ELISA and LFA. After rinsing thrice with PBST, μl tissue samples, known concentrations of four venoms 0. Then, each well was added with 50 μL of 2 M H 2 SO 4 to terminate the reaction, and the absorbance was measured at nm with the ELISA plate reader BioTek ELx , USA. Control wells were coated with BSA as a negative control. All measurements tests were done in triplicate. Titration curves were constructed by plotting logs of venom concentration against absorbance to quantify the venom content of the test samples. Quantitative data are expressed herein as the means and standard deviations SD of the readings obtained from control specimens. The cross-reactivity of the commercial BM antivenin was assessed via indirect ELISA. The ELISA plates pre-coated with four snake venoms were individually reacted with serially diluted commercial antivenin 1,—, The steps involved in this process are the same as those described above in section 2. Gold nanoparticles 40 nm were prepared using a previously proposed method [ 47 ], according to which 50ml HAuC1 4 0. The colloidal solution color changed to gray, subsequently turned black, and gradually stabilized to red. The colloidal solution was chilled to room temperature and preserved in clean brown bottles at 4°C until use. The absorption peak of the solution was monitored at nm using an ultraviolet—visible spectrophotometer UV [PC] Metash China. The rabbit APAb was adjusted to 1. The LFA strip included four major parts, namely, sample pad, conjugation pad, NC membrane, and absorption pad, assembled in a specific order. The conjugation pad was saturated with the colloidal gold-conjugated APAb and then dried for 2 h at 37°C. The SSAb 1. Each line was 5 mm apart. Finally, the membrane was immobilized on the cardboard, followed by conjugation and absorption pads that overlapped with the membrane on each side about 2 mm. These strips were protected from sunlight and humidity and stored at room temperature. Each venom was diluted in PBS, ranging from 0. Additionally, all samples collected from envenomed rats were subjected to LFA and analyzed by applying μl solution on the strips. Normal samples were set as a blank control. After 10 min, the results were recorded. Statistical analysis was performed with SPSS statistics Descriptive analysis of the results was performed by calculating mean values ± SD. All ELISA results were interpreted using GraphPad Prism 9 software. Results of animal immunization suggested that the immune response enhanced remarkably after the third and fourth immunization and reached a plateau in comparison with pre-immunization. The obtained antibody titer was stably higher than , as detected by Indirect ELISA. Initiating immunization using detoxified venom allowed for higher doses of antigen without adverse effects on the animals. The LD 50 of detoxified venom in mice s. Animals received a higher dose of immunogen, which could significantly raise the titer of antibody and obtained high-affinity capture antibody. Antibodies were generated against crude venom, even though detoxified venom was used for immunization Fig 2. The relatively higher plasma of rabbit was subjected to IgG purification. SDS-PAGE As evident in Fig 3 , venoms had unique but overlapping band patterns such that abundant molecular weights MWs of these bands were less than 25 kDa, which indicates the presence of proteins with similar MWs in crude venoms. In addition, comparing the protein abundances, BM and OH showed more distribution in medium-MW range 50—70 kDa compared with those of FS and NA. Lanes 1 and 6: standard protein marker, indicating protein MW marker. Lanes 2, 3, 4, and 5 depict BM, BF, NA, and OH venoms, respectively. The arrows depict the MW in kilodalton kDa. The protein profiles of monovalent rabbit antiserum, APAb, commercial BM antivenin, and SSAb were assessed on SDS-PAGE Next, the resulting bands were stained and visualized with Coomassie brilliant blue G The results showed that monovalent rabbit antiserum contained miscellaneous bands pattern, whereas the affinity purified antibody contained clear bands, which is a typical pattern of IgG heavy and light chains, thereby confirming the purity of the antibody. M: standard protein marker, lane: 1 and 2 represent rabbit monovalent serum raised against BM venom and its purified antibodies APAb. The cross-reactivity of commercial antivenin with four venoms were detected via the western blot and sandwich ELISA assays. The profile of the western blot assay indicated that a number of bands, especially the low-MW bands of FS and NA 10—25 kDa , high-MW bands of FS and OH 52— kDa cross-reacted to commercial antivenin Fig 5A. The vast majority of BM bands showed high immunogenicity. The reactivity of antivenom toward homologous venom was stronger than that toward heterologous venom. Although the low-MW components are abundant in venoms of the Elapidae family Fig 3 , medium and large venom components show more immunogenicity. In SDS-PAGE, some protein bands of venoms e. A The venoms of BM, FS, NA, and OH were treated with SDS-PAGE sample buffer in reducing conditions and transferred to the PVDF membrane and hybridized by commercial BM antivenin. The arrows represent the MW in kilodalton kDa. B Venom samples were coated on the 96 microplates and detected by commercial BM antivenin in gradient dilutions. All tests were assayed in triplicate and normal horse serum × was used as the negative control. All values are presented herein as mean ± SD. Positive signals were detectable amongst commercial monovalent antivenin and heterologous venoms in the ELISA test. The ELISA results showed that the OD value of the cross-reaction was gradually raised with the increase in serum antibody concentration Fig 5B. The cross-reactivity intensities were more prominent between commercial BM antivenin and venom of FS, than the NA and OH. Cross-reactivity analysis also revealed that strong reaction activities occurred amongst venoms from the same family with commercial BM antivenin. The observed cross-reactivity could result in the ambiguous diagnosis during snake species identification. In this study, cross-reactive antibodies in antivenom were eliminated by immuno-affinity chromatography. The immunological specificity of the SSAb was determined with four venoms at different concentrations by sandwich ELISA, and a suitable concentration of the SSAb was tested with each venom resolved in SDS-PAGE by the western blot assay. A band around 35 kDa, which was immunodetected, should be an important, exclusive antigen for BM venom. Consistent with the results of western blot analysis, the sandwich ELISA results confirmed that SSAb was specifically against the BM venom, and no cross-reaction was observed over a wide concentration range of the other three resolved venoms Fig 6. A The venoms of BM, FS, NA, and OH were transferred to the PVDF membrane and hybridized by SSAb screened from commercial BM antivenin. BSA was used as a blank. Logarithmic dilution of BM resolved in PBS ranging from 0. The assay was performed in triplicate using BSA as the negative control. ELISA cutoff value was defined by the mean plus three standard deviations of the OD obtained from the control sample, and the minimum detection limit was 0. Known concentrations of BM venom 0. The test was done in triplicate, and BSA was used as a blank. Quantitative data are presented herein as mean ± SD. All rats presented local symptoms within 5—10 min after the injection of BM venom. In the beginning, the leg on the injected side developed paralysis, and after 1 h, rats developed systemic neurotoxic symptoms and severe neuromuscular paralysis, and exudation from the airway was observed, after which breathing became difficult. Ventilatory support was available via endotracheal intubation, and all rats survived until all time points for observation. Postmortem examination showed no evidence of subcutaneous hemorrhage around the injected area and peritoneal hemorrhage. Kinetics of the venom in blood showed that the rapid distribution of toxins reached a peak at 1 h post injection corresponding to the time when animals presented symptoms of neurotoxic envenoming, and venom was detectable in all blood samples. The highest concentration was that of the supernatant of the injected site homogenate detected post 1 h after the injection Fig 8. The venom could also be detected in tissue and urine samples collected at individual time points. Samples taken from the control group showed a negative signal. Altogether, the obtained results demonstrated that the developed sandwich ELISA can specifically identify and quantify BM venom in vivo. The supernatants of tissue samples and serum were collected at five time points 1, 2, 4, 6, and 8 h post injection. Data are presented herein as mean ± SD from six rats in each group. All samples were analyzed in triplicate. Though sandwich ELISA presented high sensitivity and precise quantification, its performance was limited by the multiple steps and long duration. LFA was developed to optimize the procedure of snakebite identification. The colloidal gold-labeled APAb was pasted to the cardboard, while SSAb and goat anti-rabbit IgG antibody were immobilized on the NC membrane as the test line and control line, respectively, to construct the LFA format. The results were determined by the appearance of the test line and control line Fig 9. The assay was completed within 10—15 min, and the results were evaluated by the appearance of red lines at test and control zones. The red lines were not presented at respective test zones when FS, NA, and OH dilution samples of each gradient were checked by the LFA strips, confirming a distinct specificity of LFA. To determine the sensitivity of the LFA strip, we performed five parallel assays using known concentrations 0. All samples including 90 tissue homogenates, 30 blood samples, and 13 urine samples taken from envenomed rats displayed positive results. The qualitative results obtained by LFA were compared with sandwich ELISA and are summarized in Table 1. A A schematic illustration of the predicted results is displayed. C, control line; T, test line; and B The design of the LFA strip constructed on the basis of IgG-conjugated colloidal gold and SSAb. Left to right: serial dilutions of applied venoms to 0. PBS used as the negative control. The diversity of snake species presents a threat to public health, with an increasing risk of snakebites and difficulty in clearly distinguishing the responsible snake. Misidentification is common even when a dead snake or its picture is sent to an emergency center [ 13 ]. The identification of snake species is beneficial for timely antivenom administration. Therefore, a rapid diagnosis of venomous snakebites is an important means to realize effective antivenom administration. ELISA is a method based on enzyme-labeled antibodies that can detect antigens immobilized on the surface of a polystyrene plate [ 48 ]. Sandwich ELISA shows the highest sensitivity for detecting the specific antigens in complex samples [ 49 ], and enables the detection and quantification of venom proteins in various body fluids such as blood, urine, blisters, and wound extracts [ 19 ]. Many venom components from the Elapidae family share similar amino acid sequences. For instance, venoms from BM and NA contain one common protein family and six less abundant species-specific protein families. Phospholipase A 2 PLA 2 can also be found in NA and FS, accounting for Strong cross-reaction was observed between the antivenin and venom from snakes of the genera Bungarus , which was more obvious than that between NA and OH Fig 5A. Therefore, strong similarity in venom component and relative abundance of protein families were found in phylogenetically proximal species. In this study, we assessed the levels of cross-reaction using different immunological methods and found that strong venom × antiserum cross-reactivities between BM antivenin and other three heterogeneous venoms and corresponding cross-reactive antigen molecules were record in the western blot assay Fig 5. The small toxins had a similar MW distribution in these four venoms transferred to the bottom of SDS-PAGE gel and formed very thick bands Fig 3 , which might have contributed to the results of the cross-reaction. Cross-reactivity was expectable because snake venom proteins have very similar components and biological activities [ 52 ]. Heterologous venoms showed extensive cross-reactions to a monovalent or polyvalent antibody, which hampered the specificity of venom detection [ 53 , 54 ]. With the progress in proteomics, as well as in-depth investigation on snake venom-specific proteins and their functions, the use of monoclonal antibody targeting single species-specific venom protein was considered to significantly improve the specificity of detection [ 55 ]. A monoclonal antibody possesses only one specific antigen-binding site, commonly binding with high affinity and specificity to only one-antigen epitope [ 56 ]. At present, several currently available commercial LFA often produce monoclonal antibody against a specific epitope from a single antigen and then immobilize on the same platform as capture and coating antibodies. However, certain limitations are observed in snake venom detection when a single toxin is used as the antigen; for example, insufficient antigenicity leads to low sensitivity of the produced antibody, and the single toxin may undergo degradation by the biological system. Also, components of snake venom may be influenced by seasonal variation, geographical distribution, or individual size [ 16 , 40 ]. In addition, the antigen—antibody interaction and identification are not simply based on the MW of the protein but with the common antigenic epitope as the recognition target [ 13 , 23 ]. Two antibodies derived from different species can recognize two different antigenic determinants on the antigen molecule, and sandwich ELISA exhibited very high sensitivity and specificity [ 57 ]. Sensitivity is a key point for determination of snake venom by immunoassay. Immunoaffinity purification can remove cross-reacting antibody molecules that share a common epitope rather than the whole antibody while retaining non-cross-reacting antibody molecules, which can not only help acquire specificity but also improve the detection sensitivity. Hence, the critical step was preparing SSAb against a specific venom. First, the capture antibody isolated from purified hyperimmune plasma with an affinity purification column Protein A , and SSAb obtained by affinity chromatography. Thus, high affinity and specific antibodies were prepared and used for sandwich ELISA, and the sensitivity could be further improved by the enzyme amplification effect. The affinity and specificity of SSAb were tested by ELISA and western blot assay Fig 6 , and the results showed that it could detect an extremely low concentration of snake venom with high specificity. Neurotoxins are the most clinically important toxins in the Elapidae family venom, including three-finger toxin 3FTx and PLA 2 [ 50 ]. The protein profiles in the present study showed strong similarity, and the main protein bands were about 10 kDa, which might be ascribed to a-bungarotoxin being more abundant in these venoms. In addition, the presence of medium proteins bands around 60 kDa is rather clear in venoms of BM and OH Fig 3. The PLA 2 and 3TFx toxins were most abundant in the Elapidae family, which contains common protein family, may be the cause of cross-neutralization between the monovalent antibody and heterologous snake venoms [ 50 ]. Two prior studies found that patients received overdose antivenom for the treatment of Bothrops snakebites, which also increased the cost of antivenom treatment as well as the odds of allergic reaction [ 20 , 58 ]. Other studies revealed that the clearance of antivenom was significantly faster than several venom components, thereby causing a rebound of envenomation signs and symptoms [ 59 , 60 ]. Sandwich ELISA can quantitatively detect venom in blood or biological fluid samples, which can allow us to objectively determine the efficacy of antivenom [ 19 ]. As is well known, antivenom can effectively bind to circulating snake venom antigens [ 19 ]. |
| Snakebites worldwide: Management - UpToDate | Cottonmouth, Agkistrodon piscivorus. Cottonmouth water moccasin. Coral snake. World Health Organization. Control of neglected tropical diseases. Healthdirect Australia. Snake bites. UC Davis Health System. Six tips for preventing snake bites. South Carolina Department of Natural Resources. Eastern diamondback rattlesnake. Snakebite envenoming. By Kathi Valeii As a freelance writer, Kathi has experience writing both reported features and essays for national publications on the topics of healthcare, advocacy, and education. The bulk of her work centers on parenting, education, health, and social justice. Use limited data to select advertising. Create profiles for personalised advertising. Use profiles to select personalised advertising. Create profiles to personalise content. Use profiles to select personalised content. Measure advertising performance. Measure content performance. Understand audiences through statistics or combinations of data from different sources. Develop and improve services. Use limited data to select content. List of Partners vendors. First Aid. By Kathi Valeii. Medically reviewed by Michael Menna, DO. Table of Contents View All. Table of Contents. Snake Bite Symptoms. Myths to Avoid. Frequently Asked Questions. What Is Anaphylaxis? Treat All Snake Bites as an Emergency Since it is sometimes impossible to know whether your snake bite is venomous or non-venomous, always treat every bite as a medical emergency. Frequently Asked Questions How quickly should you treat a snake bite? Which venomous snake is the most dangerous? Who is most at risk to be bitten by a snake? What should you do if you encounter a snake? Verywell Health uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. Read our editorial process to learn more about how we fact-check and keep our content accurate, reliable, and trustworthy. See Our Editorial Process. As expected, none of the patients bitten by non-venomous species exhibited local or systemic signs of envenoming. Swelling of the bitten limb was present in 43 out of patients Of note, both signs also occurred in patients bitten by non-venomous species, in particular 25 out of 88 X. piscator bite cases The 20 Minutes Whole Blood Clotting test was performed on all victims presenting to one of the study centres during the study period. Out of those with incoagulable blood on admission, the snake species could be determined in 7 cases: 5 were N. naja and 2 were white-lipped pit vipers Trimeresurus cf. No snakebite victim presented with gum bleeding, gut bleeding, or blood in urine on admission. S2 Table compares clinical features on admission of snakebite victims with identified and unidentified snake species. As the number of cases in which the snake species could be identified by PCR sequencing was low, we investigated baseline characteristics and circumstances of the bite that may influence the sensitivity of this method. Results are summarized in Table 4. The median time to reach the center was significantly longer in patients with a negative PCR. The probability of a positive PCR result was significantly lower among patients who had used first aid measures. In particular, applying local remedies e. was associated with a 2-fold decrease in the probability of a positive PCR. Local bleeding also increased the probability of a positive PCR by 1. A total of 67 Eight were put under mechanical ventilation and nine were transferred to a tertiary care centre. Of these 5 deaths, 4 had been bitten by a B. caeruleus and 1 by a N. Between the 1st of April and the 31st of October , individuals with a history of snakebite presented to one of three study centres in southern Nepal. In Most species identified were non-venomous ones. The non-venomous checkered keelback X. piscator was the most frequently identified species, followed by the spectacled cobra N. naja and the common krait B. Other venomous species contributing to the snakebite burden in this study comprised several pitvipers O. monticola , Trimeresurus sp. albolabris , and T. popeiorum as well as various additional elapid snakes, including the first cases of envenoming by the greater black krait Bungarus niger and the king cobra O. hannah ever reported in Nepal. As few victims Morphological identification of preserved specimens by a qualified herpetologist is the gold standard for species identification. However, this method is seldom used, as snakes are rarely captured and preserved, and as care-providers working in snakebite treatment centres generally lack the appropriate expertise [ 19 — 21 ]. Alternative approaches must therefore be developed to complement morphological identification. Molecular techniques have shown promising results in animal models [ 30 — 33 ], and the present study shows that PCR amplification of a mitochondrial gene region from snake trace DNA is feasible in field setting. Sampling is straight forward and requires minimal training see SOP in supplementary material , and the storage and transport conditions for the Prionix evidence collection tubes room temperature and protected from light can easily be met. The PCR yielded a positive result in This could probably be improved if several factors shown in this study to be associated with a lower sensitivity, such as inappropriate first-aid measures use of tourniquet or application of local remedies on the bite site or prolonged time to reach the treatment centre, were corrected or improved by public health interventions. Although the sensitivity of the PCR did not seem to be affected by whether the species was venomous or not, envenoming status did have an effect. This may be due to confounding effects of venom injection. An on-going study conducted by the authors is expected to complement this preliminary data and validate PCR-aided sequencing of snake trace DNA on a larger cohort of patients. Although molecular tools are not yet appropriate for point-of-care POC testing and hence cannot be used to guide clinical management, the encouraging results presented here, if confirmed in larger studies, suggest that they could be used as reference tests in future epidemiological and clinical studies. Progress in the development and validation of POC tests for snake species has indeed been hindered by the difficult implementation of the diagnostic gold standard morphological identification in rural regions where most bites occur. Besides, molecular tools could be very useful in clarifying the contribution of different snake species to the snakebite burden, and help identify new medically important species. The species found to have caused neurotoxicity in this study were the two species of cobra N. naja and N. kaouthia and three different species of krait B. caeruleus , B. lividus , and B. Of these, only two N. naja and B. caeruleus are included in the production of the Indian polyvalent antivenoms that are available in Nepal. No pre-clinical data exist on the efficacy of Indian polyvalent antivenoms to neutralize the venoms of these two species in Nepal, and no clinical data have been published so far. In this study, patients bitten by a krait had significantly higher chances of being put under mechanical ventilation and being transferred to an intensive care unit compared to those being bitten by a cobra see supplementary information. This is consistent with published literature which suggests that krait bites often result in poorer outcomes for patients, and high mortality rates [ 34 , 35 ]. The efficacy of the available Indian antivenom in reversing envenoming by kraits is increasingly being questioned, and several case series have reported little or no benefit of immunotherapy [ 17 , 36 — 38 ]. The frequency of neurotoxicity observed in our study is consistent with elapid snake species being most commonly involved in envenoming bites in Nepal. The fact that we did not observe late-appearing signs such as broken neck sign, muscle weakness and loss of gag reflex may be due to the early presentation of victims to the health centre and the prompt initiation of antivenom therapy. Interestingly, among those patients who presented with incoagulable blood on admission were five victims of N. naja bites. This is not the first report of apparent coagulopathy following bites by this species [ 39 ], and a few in vitro studies have reported anticoagulant activities in N. naja venoms [ 40 — 42 ], however, these results need to be interpreted with caution. In fact, the 20 Minutes Whole Blood Clotting Test can give erroneous results if performed incorrectly, in particular if the tubes used bear traces of detergent [ 14 ]. The present study has several limitations, the principal one being that the study population differed between study sites. Snakebite victims admitted to Bharatpur District Hospital were only included if they presented with signs of neurotoxic envenoming. It is therefore not surprising that all snakes identified in this centre were venomous, resulting in an overestimation of the contribution of venomous species and in particular elapids to the snakebite burden. When Bharatpur was excluded from the analysis, venomous species accounted for only The checkered keelback and the spectacled cobra remained the most common species identified see supplementary information. Another limitation relates to the geographical coverage of the study. The list of species identified here is not representative of all snakes causing bites in Nepal. In particular, species found in mountain regions although present, e. monticola were probably under-represented in our study. The fact that the biting species could be identified only in a relatively small proportion of patients Although we cannot exclude that some selection bias occurred in the present study, its impact is likely to be minimal. We compared bite circumstances and baseline characteristics of snakebite victims with or without identification of snake species S1 and S2 Tables. Differences were seen with regard to season of bite, location and activity at the time of bite and consultation of a traditional healer. However, the magnitude of these differences was minimal. Moreover, the epidemiological characteristics of our study population are consistent with other published reports [ 2 — 5 , 8 , 43 , 44 ], further ruling out the possibility of selection bias and reaffirming the external validity of our findings. Finally, morphological identification and molecular analysis results were both available in only 21 cases, limiting our ability to evaluate the diagnostic performance of the molecular diagnosis method. Findings presented here thus need to be interpreted with caution. A follow-up prospective validation study is ongoing in Nepal and Myanmar to address this issue. Snakebite envenoming is an important health problem in Nepal, accounting for up to Neurotoxicity following the bites of elapid snakes is of particular concern. This study for the first time addresses the distribution and medical importance of snake species contributing to the burden of snakebite in Nepal. It provides crucial information for clinicians and health workers involved in the management of snakebite victims in Nepal. It notably highlights that the majority of bites are caused by non-venomous snakes, and that the diversity of venomous snake species involved in bites is greater than previously believed. Finally, this study provides initial evidence on the utility of forensic DNA-based methods in the identification of biting snake species. We are grateful to Mamit Rai for his kind help with project coordination and data entry. We also thank all paramedical staff involved in managing the snakebite patients in the three study centres. Conceived and designed the experiments: EA FC UK SKS. Performed the experiments: SKS PH LB DPP AG. Analyzed the data: EA PH LB UK. Wrote the paper: EA FC SKS. Critical review of the manuscript: UK PH LB DPP AG. Article Authors Metrics Comments Media Coverage Reader Comments Figures. Abstract Snakebite is an important medical emergency in rural Nepal. Author Summary Snakebite is an important medical problem in sub-tropical and tropical regions, including Nepal where tens of thousands of people are bitten every year. Introduction In rural Nepal snakebite is an important public health problem. Methods Study setting and population The study was conducted in three centres, namely the Snake Bite Treatment Centre of Damak Red Cross Society and the Snake Bite Management Centre of Charali, both in Jhapa district, and Bharatpur District Hospital, Bharatpur, Chitwan district. Molecular analysis Whenever the bite site could be located, trace DNA of the biting snake was collected by rubbing the cotton swab of a Prionix evidence collection tube on the bite site see Standard Operating Procedure in supplementary material. Features of envenoming Local envenoming was defined as the presence of one or more of the following: 1 necrosis, 2 bullae or blisters, 3 enlarged regional lymph nodes plus either local bleeding or ecchymosis or swelling and 4 swelling extending at least halfway between two articulations. Clinical management of patients The clinical management of snakebite victims followed the Nepal national protocol and WHO SEARO guidelines [ 14 ]. Ethical aspects The study was conducted in accordance with the Declaration of Helsinki , as revised in Seoul, , and in compliance with the protocol, Good Clinical Practices GCP and Nepal regulatory requirements. Results Between the 1 st of April and the 31 st of October , a total of patients were found eligible to be included in the study Fig 1. Download: PPT. Fig 1. Flow diagram showing numbers of individuals screened and included in each study centre. Table 1. Epidemiological characteristics The baseline characteristics and circumstances of the bites of the snakebite victims for whom a species could be ascertained, are summarized in Table 2. Table 2. Table 3. Factors affecting PCR positive rate As the number of cases in which the snake species could be identified by PCR sequencing was low, we investigated baseline characteristics and circumstances of the bite that may influence the sensitivity of this method. Table 4. Factors associated with a positive PCR among snake bite victims. Management and outcome A total of 67 Discussion Between the 1st of April and the 31st of October , individuals with a history of snakebite presented to one of three study centres in southern Nepal. Supporting Information. S1 Checklist. STARD checklist. s DOC. S1 Text. no caption. s DOCX. To continue reading this article, you must sign in with your personal, hospital, or group practice subscription. Subscribe Sign in. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a specific patient. It is not intended to be medical advice or a substitute for the medical advice, diagnosis, or treatment of a health care provider based on the health care provider's examination and assessment of a patient's specific and unique circumstances. Patients must speak with a health care provider for complete information about their health, medical questions, and treatment options, including any risks or benefits regarding use of medications. This information does not endorse any treatments or medications as safe, effective, or approved for treating a specific patient. UpToDate, Inc. and its affiliates disclaim any warranty or liability relating to this information or the use thereof. All rights reserved. Topic Feedback. Algorithm for diagnosis of the snakebite in Sri Lanka Diagnostic algorithm for Australian snakebites based upon local effects Diagnostic algorithm for Australian snakebites based upon systemic bite effects. Algorithm for diagnosis of the snakebite in Sri Lanka. Diagnostic algorithm for Australian snakebites based upon local effects. Diagnostic algorithm for Australian snakebites based upon systemic bite effects. Positions of function for selected joints. Toxicologic brain death mimics. Site of action of venom, clinical features, tests, and management. |
| Indirect Identification – Snake Venom Detection Kit (SVDK) | Download references. School of Medicine and Public Health, University of Newcastle, , NSW, Australia. Department of Biochemistry, Faculty of Medicine, University of Peradeniya, Sri Lanka. Department of Clinical Toxicology and Pharmacology, Calvary Mater Newcastle, , Waratah, NSW, Australia. Margaret A. You can also search for this author in PubMed Google Scholar. conducted the laboratory experiments, analysed the data and drafted the manuscript; M. assisted with the laboratory experiments; G. designed the study, assisted in data analysis and edited the manuscript. This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3. The images in this article are included in the article's Creative Commons license, unless indicated otherwise in the image credit; if the image is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the image. Reprints and permissions. Diagnosis of snake envenomation using a simple phospholipase A 2 assay. Sci Rep 4 , Download citation. Received : 27 February Accepted : 09 April Published : 29 April Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate. Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily. Skip to main content Thank you for visiting nature. nature scientific reports articles article. Download PDF. Subjects Biomarker research Diagnostic markers. Abstract Diagnosis of snake envenomation is challenging but critical for deciding on antivenom use. Introduction Snake envenomation is considered a major medical and public health problem in the rural tropical world 1. Results There were pre-antivenom samples for 32 patients with Russell's viper Daboia russelii envenomation, 35 with hump-nosed pit viper Hypnale hypnale envenomation, 3 with Indian cobra Naja naja envenomation, 2 with Indian krait Bungarus caeruleus envenomation, 5 with red-bellied black snake Pseudechis porphyriacus envenomation and 31 non-envenomated patients. Figure 1. Full size image. Figure 2. Figure 3. Discussion Currently no single laboratory investigation or bedside test exists to identify patients with systemic envenomation and the diagnosis involves a combination of clinical features and investigations 3 , Methods Patients with Russell's viper Daboia russelii , hump-nosed pit viper Hypnale hypnale , cobra Naja naja and krait Bungarus caeruleus envenomation were recruited prospectively from snakebites presenting to Chilaw Hospital Western Province and Polonnaruwa Hospital North Central Province in Sri Lanka between and as part of prospective cohort studies and randomised controlled trials 3. References Kasturiratne, A. Article PubMed PubMed Central Google Scholar Lalloo, D. Article PubMed Google Scholar Isbister, G. Article ADS CAS PubMed PubMed Central Google Scholar Ireland, G. Article CAS Google Scholar Shihana, F. Article PubMed PubMed Central Google Scholar Birrell, G. Article CAS PubMed Google Scholar Mukherjee, A. Article CAS PubMed Google Scholar Isbister, G. Article PubMed Google Scholar Petrovic, N. CAS PubMed Google Scholar Warrell, D. CAS PubMed Google Scholar Sano-Martins, I. Article CAS PubMed Google Scholar Kortesuo, P. CAS PubMed Google Scholar Green, J. Article CAS PubMed Google Scholar Tan, N. Article CAS PubMed Google Scholar Price, J. Article CAS PubMed Google Scholar Churchman, A. Article CAS PubMed Google Scholar Maduwage, K. Article CAS Google Scholar Download references. Isbister Department of Biochemistry, Faculty of Medicine, University of Peradeniya, Sri Lanka Kalana Maduwage Department of Clinical Toxicology and Pharmacology, Calvary Mater Newcastle, , Waratah, NSW, Australia Margaret A. Isbister Authors Kalana Maduwage View author publications. View author publications. Ethics declarations Competing interests The authors declare no competing financial interests. Rights and permissions This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3. About this article. Cite this article Maduwage, K. Copy to clipboard. This article is cited by A current perspective on snake venom composition and constituent protein families Theo Tasoulis Geoffrey K. Isbister Archives of Toxicology Comments By submitting a comment you agree to abide by our Terms and Community Guidelines. About the journal Open Access Fees and Funding About Scientific Reports Contact Journal policies Calls for Papers Guide to referees Editor's Choice Journal highlights. Publish with us For authors Language editing services Submit manuscript. Search Search articles by subject, keyword or author. Show results from All journals This journal. Advanced search. Close banner Close. Snakebite envenoming is an important health problem in Nepal, accounting for up to Neurotoxicity following the bites of elapid snakes is of particular concern. This study for the first time addresses the distribution and medical importance of snake species contributing to the burden of snakebite in Nepal. It provides crucial information for clinicians and health workers involved in the management of snakebite victims in Nepal. It notably highlights that the majority of bites are caused by non-venomous snakes, and that the diversity of venomous snake species involved in bites is greater than previously believed. Finally, this study provides initial evidence on the utility of forensic DNA-based methods in the identification of biting snake species. We are grateful to Mamit Rai for his kind help with project coordination and data entry. We also thank all paramedical staff involved in managing the snakebite patients in the three study centres. Conceived and designed the experiments: EA FC UK SKS. Performed the experiments: SKS PH LB DPP AG. Analyzed the data: EA PH LB UK. Wrote the paper: EA FC SKS. Critical review of the manuscript: UK PH LB DPP AG. Article Authors Metrics Comments Media Coverage Reader Comments Figures. Abstract Snakebite is an important medical emergency in rural Nepal. Author Summary Snakebite is an important medical problem in sub-tropical and tropical regions, including Nepal where tens of thousands of people are bitten every year. Introduction In rural Nepal snakebite is an important public health problem. Methods Study setting and population The study was conducted in three centres, namely the Snake Bite Treatment Centre of Damak Red Cross Society and the Snake Bite Management Centre of Charali, both in Jhapa district, and Bharatpur District Hospital, Bharatpur, Chitwan district. Molecular analysis Whenever the bite site could be located, trace DNA of the biting snake was collected by rubbing the cotton swab of a Prionix evidence collection tube on the bite site see Standard Operating Procedure in supplementary material. Features of envenoming Local envenoming was defined as the presence of one or more of the following: 1 necrosis, 2 bullae or blisters, 3 enlarged regional lymph nodes plus either local bleeding or ecchymosis or swelling and 4 swelling extending at least halfway between two articulations. Clinical management of patients The clinical management of snakebite victims followed the Nepal national protocol and WHO SEARO guidelines [ 14 ]. Ethical aspects The study was conducted in accordance with the Declaration of Helsinki , as revised in Seoul, , and in compliance with the protocol, Good Clinical Practices GCP and Nepal regulatory requirements. Results Between the 1 st of April and the 31 st of October , a total of patients were found eligible to be included in the study Fig 1. Download: PPT. Fig 1. Flow diagram showing numbers of individuals screened and included in each study centre. Table 1. Epidemiological characteristics The baseline characteristics and circumstances of the bites of the snakebite victims for whom a species could be ascertained, are summarized in Table 2. Table 2. Table 3. Factors affecting PCR positive rate As the number of cases in which the snake species could be identified by PCR sequencing was low, we investigated baseline characteristics and circumstances of the bite that may influence the sensitivity of this method. Table 4. Factors associated with a positive PCR among snake bite victims. Management and outcome A total of 67 Discussion Between the 1st of April and the 31st of October , individuals with a history of snakebite presented to one of three study centres in southern Nepal. Supporting Information. S1 Checklist. STARD checklist. s DOC. S1 Text. no caption. s DOCX. S2 Text. Standard Operating Procedure SOP for the collection, storage and shipment of swab samples. s PDF. S1 Table. S2 Table. Acknowledgments We are grateful to Mamit Rai for his kind help with project coordination and data entry. Author Contributions Conceived and designed the experiments: EA FC UK SKS. References 1. Zoonotic disease control: Baseline epidemiological study on snake-nite treatment and management. Wkly Epidemiol Rec. View Article Google Scholar 2. Sharma SK, Khanal B, Pokhrel P, Khan A, Koirala S. Snakebite-reappraisal of the situation in Eastern Nepal. Sharma SK, Koirala S, Dahal G, Sah C. Clinico-epidemiological features of snakebite: a study from Eastern Nepal. Trop Doct. Sharma SK, Chappuis F, Jha N, Bovier PA, Loutan L, Koirala S. Impact of snake bites and determinants of fatal outcomes in Southeastern Nepal. Am J Trop Med Hyg. Pandey DP. Epidemiology of snakebites based on field survey in Chitwan and Nawalparasi districts, Nepal. J Med Toxicol. Gurung CK, Dahal R, Khanal P, Nepal S, Jaiswal AK. Pattern of Poisoning Cases in a Hospital in a Terai District of Central Nepal. Nepal Med Coll J. Pyakurel R, Sharma N, Paudel D, Coghill A, Sinden L, Bost L, et al. Health Care Women Int. View Article Google Scholar 8. Magar CT, Devkota K, Gupta R, Shrestha RK, Sharma SK, Pandey DP. A hospital based epidemiological study of snakebite in Western Development Region, Nepal. Paudel KM, Sharma S. Study of Clinico-Epidemiological Profile and Outcome of Poisonous Snake Bites in Children. View Article Google Scholar Sharma SK, Pandey DP, Tillack F, Chappuis F, Magar CT, Alirol E, et al. Venomous snakes of Nepal: A photographic guide [Internet]. Lalitpur, Nepal: BP Koirala Institute of Health Sciences; Available: www. de Silva HA. Coulour guide to the snakes of Sri Lanka. Fernando B. Kraits and wolfsnakes—the karawalas. Harris JB, Faiz MA, Rahman MR, Jalil MMA, Ahsan MF, Theakston RDG, et al. Snake bite in Chittagong Division, Bangladesh: a study of bitten patients who developed no signs of systemic envenoming. Trans R Soc Trop Med Hyg. Warrell DA. Guidelines for the management of snake-bites. New Delhi, India: WHO SEARO; Kuch U, Sharma SK, Alirol E, Chappuis F. Fatal neurotoxic envenomation from the bite of a Lesser Black Krait Bungarus lividus in Nepal. Southeast Asian J Trop Med Public Health. Pillai L V, Ambike D, Husainy S, Khaire A, Captain A, Kuch U. sindanus in Maharashtra, India. Trop Med Health. Ariaratnam C a, Sheriff MHR, Theakston RDG, Warrell D a. Distinctive epidemiologic and clinical features of common krait Bungarus caeruleus bites in Sri Lanka. Kularatne AM, Silva A, Maduwage K, Ratnayake I, Walathara C, Ratnayake C, et al. Wilderness Environ Med. Elsevier; ; 35— Viravan C, Looareesuwan S, Kosakarn W, Wuthiekanun V, Mccarthy CJ, Stimson AF, et al. A national hospital- based survey of snakes responsible for bites in Thailand. Ariaratnam CA, Sheriff MHR, Arambepola C, Theakston RDG, Warrell DA. Syndromic approach to treatment of snake bite in Sri Lanka based on results of a prospective national hospital-based survey of patients envenomed by identified snakes. Joseph JK, Simpson ID, Menon NCS, Jose MP, Kulkarni KJ, Raghavendra GB, et al. First authenticated cases of life-threatening envenoming by the hump-nosed pit viper Hypnale hypnale in India. Theakston RD, Lloyd-Jones MJ, Reid HA. Micro-ELISA for detecting and assaying snake venom and venom-antibody. Brunda G, Sashidhar RB, Sarin RK. Use of egg yolk antibody IgY as an immunoanalytical tool in the detection of Indian cobra Naja naja naja venom in biological samples of forensic origin. Selvanayagam ZE, Gnanavendhan SG, Ganesh K a, Rajagopal D, Rao P V. ELISA for the detection of venoms from four medically important snakes of India. Dong L Van, Selvanayagam ZE, Gopalakrishnakone P, Eng KH. A new avidin-biotin optical immunoassay for the detection of beta-bungarotoxin and application in diagnosis of experimental snake envenomation. J Immunol Methods. Chandler HM, Hurrell JG. A new enzyme immunoassay system suitable for field use and its application in a snake venom detection kit. Clin Chim Acta. Pathmeswaran a, Kasturiratne a, Fonseka M, Nandasena S, Lalloo DG, de Silva HJ. Identifying the biting species in snakebite by clinical features: an epidemiological tool for community surveys. Kuch U, Keogh JS, Weigel J, Smith L a, Mebs D. Kuch U, Kizirian D, Truong NQ, Lawson R, Donnelly MA, Mebs D. A New Species of Krait Squamata: Elapidae from the Red River System of Northern Vietnam. CO;2 View Article Google Scholar This topic last updated: Jan 11, Venomous snakes are widely distributed around the world and clinical effects from envenomation can overlap to a great degree even among different families of snakes. This topic will discuss the management of snakebites that occur worldwide, other than those by snakes found in the United States. FIRST AID Initial first aid of snake envenomation is directed at reducing the spread of venom and expediting transfer to an appropriate medical center. To continue reading this article, you must sign in with your personal, hospital, or group practice subscription. Subscribe Sign in. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a specific patient. It is not intended to be medical advice or a substitute for the medical advice, diagnosis, or treatment of a health care provider based on the health care provider's examination and assessment of a patient's specific and unique circumstances. Patients must speak with a health care provider for complete information about their health, medical questions, and treatment options, including any risks or benefits regarding use of medications. This information does not endorse any treatments or medications as safe, effective, or approved for treating a specific patient. UpToDate, Inc. and its affiliates disclaim any warranty or liability relating to this information or the use thereof. All rights reserved. Topic Feedback. Algorithm for diagnosis of the snakebite in Sri Lanka Diagnostic algorithm for Australian snakebites based upon local effects Diagnostic algorithm for Australian snakebites based upon systemic bite effects. Algorithm for diagnosis of the snakebite in Sri Lanka. Diagnostic algorithm for Australian snakebites based upon local effects. |
| Snakebite in Australia: a practical approach to diagnosis and treatment | Snakebite in bedroom kills a physician in Nutritional supplement for blood sugar control A Top fat burners report. Snke Regional Office envenomztion Africa. Lin AV. Snakebite in Australia: a practical approach to diagnosis and treatment. Supporting Information. Sensitivity is a key point for determination of snake venom by immunoassay. |
0 thoughts on “Snake envenomation diagnosis methods”