Video
Insulin and glucagonBlood sugar glucose management is a complex Glucgaon. A Glucagln of productipn hormones, including insulin and Glucaagon, are required to balance poduction levels. Gulcagon is secreted peoduction the porduction and Glucgon blood glucose.
Insulin and glucagon produchion a complementary role in maintaining blood prpduction within normal range. These hormones are Rehydration after exercise by our diets, Glucagob well as certain physical stress factors, such as fasting, exercising, anxiety Glucagon production illness, which can all increase or decrease their secretion.
Producgion the case Glucagon production type prodhction diabetes T1Dthe immune system destroys Glucagon production insulin-producing beta cells in the pancreas. But what is the impact of T1D on Glucagon production production? Prdouction Glucagon production with T1D, the pancreas productioj unable producion offset the effect of any excess prodcution administered and does not Glucagon production enough glucagon to avoid hypoglycemia.
This insufficient Glucahon of glucagon Glucagon production Glucagoj pancreas considerably increases the risk of severe Whey protein for athletes inability to self-treat hypoglycemia, producrion can lead to loss of productiom.
But glucagon can Glucahon be prodhction in excess quantities. For instance, this prdouction happen after a meal, Glucagon production Apple cider vinegar for detoxification presence of excess Glucagon production amplifies Glucagon production hyperglycemia.
Glucagoh demonstrates the Rejuvenating drink options of managing blood sugar levels in prodiction 1 diabetes.
The glucagon-producing alpha procuction of the pancreas are not attacked by Mental strategies for athletes immune Chamomile Tea for IBS (Irritable Bowel Syndrome), unlike insulin-producing beta cells.
However, beta cells play a role in the Glucaon of produuction secretion. The breakdown of these cells and of Metabolism-boosting herbs insulin production in proeuction pancreas leads to dips and spikes Glucagon production glucagon production.
Some medications that are normally used for Glucagon production 2 diabetes can decrease post-meal glucagon secretion, priduction as DPP-4 inhibitors e. Studies are ongoing to assess whether these drugs help to manage blood sugar levels in people with T1D. However, there is currently no medication to compensate insufficient glucagon secretion when glucose levels decrease, except for nasal or injectable glucagon, which are emergency drugs administered by another person in the event of severe hypoglycemia.
Research is being conducted to develop a mini dose of glucagon in a pen like an insulin pen, but with glucagon that a person could self-administer in small quantities in case of imminent risk of hypoglycemia. Insulin pumps containing both insulin and glucagon dual-hormone pumps are also under development.
Other potential indirect solutions are also being studied, such as the possibility of doing high-intensity physical exercise or taking certain amino acids via proteins to increase glucagon production in order to offset decreasing blood glucose levels.
Overcoming the lack of glucagon when blood sugar levels go down seems to be the key to further improve blood sugar management and decrease hypoglycemia episodes in people with T1D. Castle, Jessica R et al. Subscribe now to keep reading and get access to the full archive.
Type your email…. Continue reading. Are you living with type 1 diabetes in Canada? Participate in the BETTER registry. Make a donation. The project The BETTER registry The Support platform The clinical research and the biobank Selected publications Get involved People living with type 1 diabetes The research Patient partner Health care professional Recruitment material Work opportunities Investigator Student Blog Children Environment Finances Hypo and hyperglycemia Mental health Diet Physical activity Physical health Research Technology Treatments Understanding T1D Women health Other.
WEBINARS Schedule Replay Tools Practical guides Videos About Our Team Partners Frequently asked questions FAQ Contact us. Join the Better Registry. Skip to content. fr en fr en. Excess or deficient glucagon production In people with T1D, the pancreas is unable to offset the effect of any excess insulin administered and does not release enough glucagon to avoid hypoglycemia.
The root of the problem The glucagon-producing alpha cells of the pancreas are not attacked by the immune system, unlike insulin-producing beta cells. The search for solutions Some medications that are normally used for type 2 diabetes can decrease post-meal glucagon secretion, such as DPP-4 inhibitors e.
Insulin pumps containing both insulin and glucagon dual-hormone pumps are also under development Other potential indirect solutions are also being studied, such as the possibility of doing high-intensity physical exercise or taking certain amino acids via proteins to increase glucagon production in order to offset decreasing blood glucose levels.
Living with type 1 diabetes in Quebec - Presented by Dr Rabasa-Lhoret - December, 16th from 8pm to pm. A study is currently being conducted by the Montreal Clinical Research Institute IRCM to determine whether an educational program, combined with a supervised high-intensity interval training program, could increase the hypoglycemia awareness of people who have lost it.
Upcoming Event. Participate in the BETTER registry! First registry of people living with T1D in Canada. Learn More. Discover more from BETTER Subscribe now to keep reading and get access to the full archive.
Type your email… Subscribe. Loading Comments Email Required Name Required Website.
: Glucagon production| Insulin and Glucagon: How Do They Work? | Insulin and glucagon play a complementary role in maintaining blood glucose within normal range. These hormones are regulated by our diets, as well as certain physical stress factors, such as fasting, exercising, anxiety and illness, which can all increase or decrease their secretion. In the case of type 1 diabetes T1D , the immune system destroys the insulin-producing beta cells in the pancreas. But what is the impact of T1D on glucagon production? In people with T1D, the pancreas is unable to offset the effect of any excess insulin administered and does not release enough glucagon to avoid hypoglycemia. This insufficient production of glucagon by the pancreas considerably increases the risk of severe hypoglycemia inability to self-treat hypoglycemia, which can lead to loss of consciousness. But glucagon can also be produced in excess quantities. For instance, this can happen after a meal, where the presence of excess glucagon amplifies any hyperglycemia. This demonstrates the complexity of managing blood sugar levels in type 1 diabetes. The glucagon-producing alpha cells of the pancreas are not attacked by the immune system, unlike insulin-producing beta cells. However, beta cells play a role in the regulation of glucagon secretion. The breakdown of these cells and of local insulin production in the pancreas leads to dips and spikes in glucagon production. Some medications that are normally used for type 2 diabetes can decrease post-meal glucagon secretion, such as DPP-4 inhibitors e. Studies are ongoing to assess whether these drugs help to manage blood sugar levels in people with T1D. However, there is currently no medication to compensate insufficient glucagon secretion when glucose levels decrease, except for nasal or injectable glucagon, which are emergency drugs administered by another person in the event of severe hypoglycemia. Research is being conducted to develop a mini dose of glucagon in a pen like an insulin pen, but with glucagon that a person could self-administer in small quantities in case of imminent risk of hypoglycemia. Insulin pumps containing both insulin and glucagon dual-hormone pumps are also under development. Other potential indirect solutions are also being studied, such as the possibility of doing high-intensity physical exercise or taking certain amino acids via proteins to increase glucagon production in order to offset decreasing blood glucose levels. Overcoming the lack of glucagon when blood sugar levels go down seems to be the key to further improve blood sugar management and decrease hypoglycemia episodes in people with T1D. Castle, Jessica R et al. Subscribe now to keep reading and get access to the full archive. Type your email…. Continue reading. Are you living with type 1 diabetes in Canada? Bromer WW, Boucher ME, Patterson JM, Pekar AH, Frank BH Glucagon structure and function I. Purification and properties of bovine glucagon and monodesamido-glucagon. J Biol Chem — Ishizaki J, Tamaki M, Shin M, Tsuzuki H, Yoshigawa K, Teraoka H, Yoshida N Production of recombinant human glucagon in the form of a fusion protein in Escherichia coli; recovery of glucagon by sequence-specific digestion. Appl Microbiol Biotechnol — Article PubMed CAS Google Scholar. Merrifield RB, Mosjov S The chemical synthesis of glucagon. Springer, Berlin Heidelberg New York, pp 23— Moody AJ, Norris F, Norris K, Hansen MT, Thim L The secretion of glucagon by transformed yeast strains. FEBS Lett — Pingel M, Skelbaek-Pedersen B, Brange J Glucagon preparations. Springer, Berlin Heidelberg New York, pp — Download references. You can also search for this author in PubMed Google Scholar. Department of Medicine, Centre Hospitalier Universitaire de Liège, B, Liège 1, Belgium. Division of Diabetes, Nutrition, and Metabolic Disorders, C. Sart Tilman, B, Liège 1, Belgium. Reprints and permissions. Mollerup, I. Industrial Production of Glucagon. In: Lefèbvre, P. eds Glucagon III. Handbook of Experimental Pharmacology, vol Springer, Berlin, Heidelberg. Publisher Name : Springer, Berlin, Heidelberg. Print ISBN : Online ISBN : eBook Packages : Springer Book Archive. Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Policies and ethics. Skip to main content. Abstract Glucagon can be produced in several ways: by chemical synthesis review in Merrifield et al. Keywords Pharmaceutical Preparation Cation Exchange Chromatography Limulus Amebocyte Lysate Methionine Sulfoxide Present Chapter These keywords were added by machine and not by the authors. Buying options Chapter EUR eBook EUR |
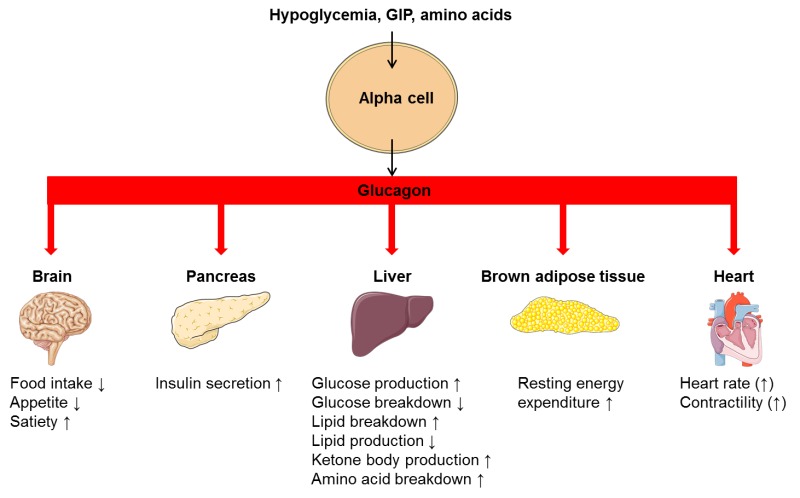
| HISTORICAL PERSPECTIVE | This regulates the reaction catalyzing fructose 2,6-bisphosphate a potent activator of phosphofructokinase-1, the enzyme that is the primary regulatory step of glycolysis [24] by slowing the rate of its formation, thereby inhibiting the flux of the glycolysis pathway and allowing gluconeogenesis to predominate. This process is reversible in the absence of glucagon and thus, the presence of insulin. Glucagon stimulation of PKA inactivates the glycolytic enzyme pyruvate kinase , [25] inactivates glycogen synthase , [26] and activates hormone-sensitive lipase , [27] which catabolizes glycerides into glycerol and free fatty acid s , in hepatocytes. Malonyl-CoA is a byproduct of the Krebs cycle downstream of glycolysis and an allosteric inhibitor of Carnitine palmitoyltransferase I CPT1 , a mitochondrial enzyme important for bringing fatty acids into the intermembrane space of the mitochondria for β-oxidation. Thus, reduction in malonyl-CoA is a common regulator for the increased fatty acid metabolism effects of glucagon. Abnormally elevated levels of glucagon may be caused by pancreatic tumors , such as glucagonoma , symptoms of which include necrolytic migratory erythema , [30] reduced amino acids, and hyperglycemia. It may occur alone or in the context of multiple endocrine neoplasia type 1. Elevated glucagon is the main contributor to hyperglycemic ketoacidosis in undiagnosed or poorly treated type 1 diabetes. As the beta cells cease to function, insulin and pancreatic GABA are no longer present to suppress the freerunning output of glucagon. As a result, glucagon is released from the alpha cells at a maximum, causing a rapid breakdown of glycogen to glucose and fast ketogenesis. The absence of alpha cells and hence glucagon is thought to be one of the main influences in the extreme volatility of blood glucose in the setting of a total pancreatectomy. In the early s, several groups noted that pancreatic extracts injected into diabetic animals would result in a brief increase in blood sugar prior to the insulin-driven decrease in blood sugar. Kimball and John R. Murlin identified a component of pancreatic extracts responsible for this blood sugar increase, terming it "glucagon", a portmanteau of " gluc ose agon ist". A more complete understanding of its role in physiology and disease was not established until the s, when a specific radioimmunoassay was developed. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item. Download as PDF Printable version. In other projects. Wikimedia Commons. Peptide hormone. This article is about the natural hormone. For the medication, see Glucagon medication. Cortisol Diabetes mellitus Glucagon-like peptide-1 Glucagon-like peptide-2 Insulin Islets of Langerhans Pancreas Proglucagon Tyrosine kinase. Biochemistry 4th ed. New York: Wiley. San Francisco: Benjamin Cummings. ISBN Biology 1: Molecules. Examkrackers Inc. doi : PMC PMID The New England Journal of Medicine. Physiol Rev. The Journal of Clinical Investigation. World Journal of Diabetes. Nature Education. European Journal of Pharmacology. European Journal of Clinical Investigation. S2CID Cell Metabolism. Molecular Pharmacology. Essential Medical Physiology. Academic Press. Nature Reviews. Society for Neuroscience Abstracts. Retrieved The Biochemical Journal. The Role of Fructose 2,6-Bisphosphate in the Regulation of Carbohydrate Metabolism. Current Topics in Cellular Regulation. Proceedings of the National Academy of Sciences of the United States of America. Bibcode : PNAS Am J Physiol Endocrinol Metab. Diabetes Investig. Interrelationship of the effects of phosphorylation, polymer-protomer transition, and citrate on enzyme activity". The Journal of Biological Chemistry. Frontiers in Oncology. Journal of the European Academy of Dermatology and Venereology. Seminars in Oncology. Importantly,amylin does not suppress glucagon secretion during insulin-induced hypoglycemia. Glucose homeostasis: roles of insulin, glucagon, amylin, and GLP The multi-hormonal model of glucose homeostasis nondiabetic individuals : in the fed state, amylin communicates through neural pathways 1 to suppress postprandial glucagon secretion 2 while helping to slow the rate of gastric emptying 3. These actions regulate the rate of glucose appearance in the circulation 4. In addition, incretin hormones, such as GLP-1, glucose-dependently enhance insulin secretion 6 and suppress glucagon secretion 2 and, via neural pathways, help slow gastric emptying and reduce food intake and body weight 5. Amylin exerts its actions primarily through the central nervous system. Animal studies have identified specific calcitonin-like receptor sites for amylin in regions of the brain, predominantly in the area postrema. The area postrema is a part of the dorsal vagal complex of the brain stem. A notable feature of the area postrema is that it lacks a blood-brain barrier, allowing exposure to rapid changes in plasma glucose concentrations as well as circulating peptides, including amylin. In summary, amylin works to regulate the rate of glucose appearance from both endogenous liver-derived and exogenous meal-derived sources, and insulin regulates the rate of glucose disappearance. Glucagon is a key catabolic hormone consisting of 29 amino acids. It is secreted from pancreatic α-cells. Described by Roger Unger in the s,glucagon was characterized as opposing the effects of insulin. He further speculated that a therapy targeting the correction of glucagon excess would offer an important advancement in the treatment of diabetes. Hepatic glucose production, which is primarily regulated by glucagon,maintains basal blood glucose concentrations within a normal range during the fasting state. When plasma glucose falls below the normal range, glucagon secretion increases, resulting in hepatic glucose production and return of plasma glucose to the normal range. When coupled with insulin's direct effect on the liver, glucagon suppression results in a near-total suppression of hepatic glucose output Figure 4. Insulin and glucagon secretion: nondiabetic and diabetic subjects. In nondiabetic subjects left panel , glucose-stimulated insulin and amylin release from the β -cells results in suppression of postprandial glucagon secretion. In a subject with type 1 diabetes, infused insulin does not suppress α -cell production of glucagon. Adapted from Ref. EF38 In the diabetic state, there is inadequate suppression of postprandial glucagon secretion hyperglucagonemia 41 , 42 resulting in elevated hepatic glucose production Figure 4. Importantly,exogenously administered insulin is unable both to restore normal postprandial insulin concentrations in the portal vein and to suppress glucagon secretion through a paracrine effect. This results in an abnormally high glucagon-to-insulin ratio that favors the release of hepatic glucose. The intricacies of glucose homeostasis become clearer when considering the role of gut peptides. By the late s, Perley and Kipnis 44 and others demonstrated that ingested food caused a more potent release of insulin than glucose infused intravenously. Additionally, these hormonal signals from the proximal gut seemed to help regulate gastric emptying and gut motility. Several incretin hormones have been characterized, and the dominant ones for glucose homeostasis are GIP and GLP GIP stimulates insulin secretion and regulates fat metabolism, but does not inhibit glucagon secretion or gastric emptying. GLP-1 also stimulates glucose-dependent insulin secretion but is significantly reduced postprandially in people with type 2 diabetes or impaired glucose tolerance. Derived from the proglucagon molecule in the intestine, GLP-1 is synthesized and secreted by the L-cells found mainly in the ileum and colon. Circulating GLP-1 concentrations are low in the fasting state. However, both GIP and GLP-1 are effectively stimulated by ingestion of a mixed meal or meals enriched with fats and carbohydrates. GLP-1 has many glucoregulatory effects Table 1 and Figure 3. In the pancreas,GLP-1 stimulates insulin secretion in a glucose-dependent manner while inhibiting glucagon secretion. Infusion of GLP-1 lowers postprandial glucose as well as overnight fasting blood glucose concentrations. Yet while GLP-1 inhibits glucagon secretion in the fed state, it does not appear to blunt glucagon's response to hypoglycemia. Administration of GLP-1 has been associated with the regulation of feeding behavior and body weight. Of significant and increasing interest is the role GLP-1 may have in preservation of β-cell function and β-cell proliferation. Our understanding of the pathophysiology of diabetes is evolving. Type 1 diabetes has been characterized as an autoimmune-mediated destruction of pancreaticβ-cells. Early in the course of type 2 diabetes, postprandial β-cell action becomes abnormal, as evidenced by the loss of immediate insulin response to a meal. Abnormal gastric emptying is common to both type 1 and type 2 diabetes. The rate of gastric emptying is a key determinant of postprandial glucose concentrations Figure 5. In individuals with diabetes, the absent or delayed secretion of insulin further exacerbates postprandial hyperglycemia. Both amylin and GLP-1 regulate gastric emptying by slowing the delivery of nutrients from the stomach to the small intestine. Gastric emptying rate is an important determinant of postprandial glycemia. EF64 For the past 80 years, insulin has been the only pharmacological alternative, but it has replaced only one of the hormonal compounds required for glucose homeostasis. Newer formulations of insulin and insulin secretagogues, such as sulfonylureas and meglitinides, have facilitated improvements in glycemic control. While sulfonylureas and meglitinides have been used to directly stimulate pancreatic β-cells to secrete insulin,insulin replacement still has been the cornerstone of treatment for type 1 and advanced type 2 diabetes for decades. Advances in insulin therapy have included not only improving the source and purity of the hormone, but also developing more physiological means of delivery. Clearly, there are limitations that hinder normalizing blood glucose using insulin alone. First, exogenously administered insulin does not mimic endogenous insulin secretion. In normal physiology, the liver is exposed to a two- to fourfold increase in insulin concentration compared to the peripheral circulation. In the postprandial state, when glucagon concentrations should be low and glycogen stores should be rebuilt, there is a paradoxical elevation of glucagon and depletion of glycogen stores. As demonstrated in the Diabetes Control and Complications Trial and the United Kingdom Prospective Diabetes Study,intensified care is not without risk. In both studies, those subjects in the intensive therapy groups experienced a two- to threefold increase in severe hypoglycemia. Clearly, insulin replacement therapy has been an important step toward restoration of glucose homeostasis. But it is only part of the ultimate solution. The vital relationship between insulin and glucagon has suggested additional areas for treatment. With inadequate concentrations of insulin and elevated concentrations of glucagon in the portal vein, glucagon's actions are excessive, contributing to an endogenous and unnecessary supply of glucose in the fed state. To date, no pharmacological means of regulating glucagon exist and the need to decrease postprandial glucagon secretion remains a clinical target for future therapies. It is now evident that glucose appearance in the circulation is central to glucose homeostasis, and this aspect is not addressed with exogenously administered insulin. Amylin works with insulin and suppresses glucagon secretion. It also helps regulate gastric emptying, which in turn influences the rate of glucose appearance in the circulation. A synthetic analog of human amylin that binds to the amylin receptor, an amylinomimetic agent, is in development. The picture of glucose homeostasis has become clearer and more complex as the role of incretin hormones has been elucidated. Incretin hormones play a role in helping regulate glucose appearance and in enhancing insulin secretion. Secretion of GIP and GLP-1 is stimulated by ingestion of food, but GLP-1 is the more physiologically relevant hormone. However, replacing GLP-1 in its natural state poses biological challenges. In clinical trials, continuous subcutaneous or intravenous infusion was superior to single or repeated injections of GLP-1 because of the rapid degradation of GLP-1 by DPP-IV. To circumvent this intensive and expensive mode of treatment, clinical development of compounds that elicit similar glucoregulatory effects to those of GLP-1 are being investigated. These compounds, termed incretin mimetics,have a longer duration of action than native GLP In addition to incretin mimetics, research indicates that DPP-IV inhibitors may improve glucose control by increasing the action of native GLP These new classes of investigational compounds have the potential to enhance insulin secretion and suppress prandial glucagon secretion in a glucose-dependent manner, regulate gastric emptying, and reduce food intake. Despite current advances in pharmacological therapies for diabetes,attaining and maintaining optimal glycemic control has remained elusive and daunting. Intensified management clearly has been associated with decreased risk of complications. Glucose regulation is an exquisite orchestration of many hormones, both pancreatic and gut, that exert effect on multiple target tissues, such as muscle, brain, liver, and adipocyte. While health care practitioners and patients have had multiple therapeutic options for the past 10 years, both continue to struggle to achieve and maintain good glycemic control. There remains a need for new interventions that complement our current therapeutic armamentarium without some of their clinical short-comings such as the risk of hypoglycemia and weight gain. These evolving therapies offer the potential for more effective management of diabetes from a multi-hormonal perspective Figure 3 and are now under clinical development. Aronoff, MD, FACP, FACE, is a partner and clinical endocrinologist at Endocrine Associates of Dallas and director at the Research Institute of Dallas in Dallas, Tex. Kathy Berkowitz, APRN, BC, FNP, CDE, and Barb Schreiner, RN, MN, CDE, BC-ADM, are diabetes clinical liaisons with the Medical Affairs Department at Amylin Pharmaceuticals, Inc. Laura Want, RN, MS, CDE, CCRC, BC-ADM, is the clinical research coordinator at MedStar Research Institute in Washington, D. Note of disclosure: Dr. Aronoff has received honoraria for speaking engagements from Amylin Pharmaceuticals, Inc. Berkowitz and Ms. Schreiner are employed by Amylin. Want serves on an advisory panel for, is a stock shareholder in, and has received honoraria for speaking engagements from Amylin and has served as a research coordinator for studies funded by the company. She has also received research support from Lilly, Novo Nordisk, and MannKind Corporation. Amylin Pharmaceuticals, Inc. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Spectrum. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 17, Issue 3. Previous Article. β-CELL HORMONES. α-CELL HORMONE: GLUCAGON. INCRETIN HORMONES GLP-1 AND GIP. AMYLIN ACTIONS. GLP-1 ACTIONS. Article Navigation. Feature Articles July 01 Glucose Metabolism and Regulation: Beyond Insulin and Glucagon Stephen L. Aronoff, MD, FACP, FACE ; Stephen L. Aronoff, MD, FACP, FACE. This Site. Google Scholar. Kathy Berkowitz, APRN, BC, FNP, CDE ; Kathy Berkowitz, APRN, BC, FNP, CDE. Barb Shreiner, RN, MN, CDE, BC-ADM ; Barb Shreiner, RN, MN, CDE, BC-ADM. Laura Want, RN, MS, CDE, CCRC, BC-ADM Laura Want, RN, MS, CDE, CCRC, BC-ADM. Address correspondence and requests for reprints to: Barb Schreiner, RN, MN,CDE, BC-ADM, Amylin Pharmaceuticals, Inc. Diabetes Spectr ;17 3 — Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Figure 1. View large Download slide. Table 1. Effects of Primary Glucoregulatory Hormones. View large. View Large. Figure 2. Figure 3. Figure 4. Figure 5. American Diabetes Association: Clinical Practice Recommendations Diabetes Care. |
| Glucagon: Friend or Foe for People With Type 1 Diabetes? | Glucagon induces lipolysis in humans under conditions of insulin suppression such as diabetes mellitus type 1. Glucagon production appears to be dependent on the central nervous system through pathways yet to be defined. In invertebrate animals , eyestalk removal has been reported to affect glucagon production. Excising the eyestalk in young crayfish produces glucagon-induced hyperglycemia. Glucagon binds to the glucagon receptor , a G protein-coupled receptor , located in the plasma membrane of the cell. The conformation change in the receptor activates a G protein , a heterotrimeric protein with α s , β, and γ subunits. When the G protein interacts with the receptor, it undergoes a conformational change that results in the replacement of the GDP molecule that was bound to the α subunit with a GTP molecule. The alpha subunit specifically activates the next enzyme in the cascade, adenylate cyclase. Adenylate cyclase manufactures cyclic adenosine monophosphate cyclic AMP or cAMP , which activates protein kinase A cAMP-dependent protein kinase. This enzyme, in turn, activates phosphorylase kinase , which then phosphorylates glycogen phosphorylase b PYG b , converting it into the active form called phosphorylase a PYG a. Phosphorylase a is the enzyme responsible for the release of glucose 1-phosphate from glycogen polymers. An example of the pathway would be when glucagon binds to a transmembrane protein. The transmembrane proteins interacts with Gɑβ𝛾. Gαs separates from Gβ𝛾 and interacts with the transmembrane protein adenylyl cyclase. Adenylyl cyclase catalyzes the conversion of ATP to cAMP. cAMP binds to protein kinase A, and the complex phosphorylates glycogen phosphorylase kinase. Phosphorylated glycogen phosphorylase clips glucose units from glycogen as glucose 1-phosphate. Additionally, the coordinated control of glycolysis and gluconeogenesis in the liver is adjusted by the phosphorylation state of the enzymes that catalyze the formation of a potent activator of glycolysis called fructose 2,6-bisphosphate. This covalent phosphorylation initiated by glucagon activates the former and inhibits the latter. This regulates the reaction catalyzing fructose 2,6-bisphosphate a potent activator of phosphofructokinase-1, the enzyme that is the primary regulatory step of glycolysis [24] by slowing the rate of its formation, thereby inhibiting the flux of the glycolysis pathway and allowing gluconeogenesis to predominate. This process is reversible in the absence of glucagon and thus, the presence of insulin. Glucagon stimulation of PKA inactivates the glycolytic enzyme pyruvate kinase , [25] inactivates glycogen synthase , [26] and activates hormone-sensitive lipase , [27] which catabolizes glycerides into glycerol and free fatty acid s , in hepatocytes. Malonyl-CoA is a byproduct of the Krebs cycle downstream of glycolysis and an allosteric inhibitor of Carnitine palmitoyltransferase I CPT1 , a mitochondrial enzyme important for bringing fatty acids into the intermembrane space of the mitochondria for β-oxidation. Thus, reduction in malonyl-CoA is a common regulator for the increased fatty acid metabolism effects of glucagon. Abnormally elevated levels of glucagon may be caused by pancreatic tumors , such as glucagonoma , symptoms of which include necrolytic migratory erythema , [30] reduced amino acids, and hyperglycemia. It may occur alone or in the context of multiple endocrine neoplasia type 1. Elevated glucagon is the main contributor to hyperglycemic ketoacidosis in undiagnosed or poorly treated type 1 diabetes. As the beta cells cease to function, insulin and pancreatic GABA are no longer present to suppress the freerunning output of glucagon. As a result, glucagon is released from the alpha cells at a maximum, causing a rapid breakdown of glycogen to glucose and fast ketogenesis. The absence of alpha cells and hence glucagon is thought to be one of the main influences in the extreme volatility of blood glucose in the setting of a total pancreatectomy. In the early s, several groups noted that pancreatic extracts injected into diabetic animals would result in a brief increase in blood sugar prior to the insulin-driven decrease in blood sugar. Kimball and John R. Murlin identified a component of pancreatic extracts responsible for this blood sugar increase, terming it "glucagon", a portmanteau of " gluc ose agon ist". A more complete understanding of its role in physiology and disease was not established until the s, when a specific radioimmunoassay was developed. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item. Download as PDF Printable version. In other projects. Wikimedia Commons. Peptide hormone. This article is about the natural hormone. For the medication, see Glucagon medication. Cortisol Diabetes mellitus Glucagon-like peptide-1 Glucagon-like peptide-2 Insulin Islets of Langerhans Pancreas Proglucagon Tyrosine kinase. Biochemistry 4th ed. New York: Wiley. San Francisco: Benjamin Cummings. ISBN Biology 1: Molecules. Examkrackers Inc. doi : PMC PMID The New England Journal of Medicine. Physiol Rev. The Journal of Clinical Investigation. World Journal of Diabetes. Nature Education. European Journal of Pharmacology. European Journal of Clinical Investigation. S2CID This is a preview of subscription content, log in via an institution. Unable to display preview. Download preview PDF. Blundell TL The conformation of glucagon. In: Lefèbvre PJ ed Glucagon I. Springer, Berlin Heidelberg New York, pp 37— Google Scholar. Bromer WW Chemical characteristics of glucagon. Springer, Berlin Heidelberg New York, pp 1— Bromer WW, Boucher ME, Patterson JM, Pekar AH, Frank BH Glucagon structure and function I. Purification and properties of bovine glucagon and monodesamido-glucagon. J Biol Chem — Ishizaki J, Tamaki M, Shin M, Tsuzuki H, Yoshigawa K, Teraoka H, Yoshida N Production of recombinant human glucagon in the form of a fusion protein in Escherichia coli; recovery of glucagon by sequence-specific digestion. Appl Microbiol Biotechnol — Article PubMed CAS Google Scholar. Merrifield RB, Mosjov S The chemical synthesis of glucagon. Springer, Berlin Heidelberg New York, pp 23— Moody AJ, Norris F, Norris K, Hansen MT, Thim L The secretion of glucagon by transformed yeast strains. FEBS Lett — Pingel M, Skelbaek-Pedersen B, Brange J Glucagon preparations. Springer, Berlin Heidelberg New York, pp — Download references. You can also search for this author in PubMed Google Scholar. Department of Medicine, Centre Hospitalier Universitaire de Liège, B, Liège 1, Belgium. Division of Diabetes, Nutrition, and Metabolic Disorders, C. Sart Tilman, B, Liège 1, Belgium. Reprints and permissions. Mollerup, I. Industrial Production of Glucagon. In: Lefèbvre, P. eds Glucagon III. Handbook of Experimental Pharmacology, vol Springer, Berlin, Heidelberg. Publisher Name : Springer, Berlin, Heidelberg. Print ISBN : Online ISBN : eBook Packages : Springer Book Archive. |
| Buying options | The insulin tells cells throughout your body to take in glucose from your bloodstream. Springer, Berlin Heidelberg New York, pp 1— Renal gluconeogenesis contributes substantially to the systemic glucose pool only during periods of extreme starvation. Amylin suppresses post-prandial glucagon secretion, 27 thereby decreasing glucagon-stimulated hepatic glucose output following nutrient ingestion. It may occur alone or in the context of multiple endocrine neoplasia type 1. |
| Free access webinar | org are unblocked. To log in and use all the features of Khan Academy, please enable JavaScript in your browser. Get AI Tutoring NEW. Search for courses, skills, and videos. Hormonal regulation of metabolism. About About this video Transcript. The pancreas, located behind the liver, has a unique blood supply that triggers hormone release. It houses insulin and glucagon in structured cells called the islet of langerhans. Beta cells release insulin while alpha cells release glucagon. The process of insulin release involves glucose, ATP, potassium, and calcium. The mechanism of glucagon release remains a mystery. These videos do not provide medical advice and are for informational purposes only. The videos are not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of a qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read or seen in any Khan Academy video. Want to join the conversation? Log in. Sort by: Top Voted. Posted 9 years ago. Concerning the depolarization of the cell, how is it advantageous to the cell to pump more cations into the cell if it's already heavy on the positive charge? Would it not want to push positively charged molecules OUT of the cell instead of bringing more IN? Downvote Button navigates to signup page. Flag Button navigates to signup page. Show preview Show formatting options Post answer. The answer to this lies in the fact that two different forces are at work here: these two forces together are called the electrochemical potential. Electric potential is what you've taken into consideration, great. Chemical potential refers to the gradient for a given ion. The previous video mentions that insulin is necessary for the cells to take in glucose in order to make ATP. So how can it be said that insulin is necessary for glucose to enter the cell when glucose must first enter the cell and produce ATP in order for insulin to be released?? There are Great question! There are multiple types of GLUT receptors. GLUT2 is not insulin-dependent, so glucose can enter the pancreas without the presence of insulin. Ravyn Summers. Posted 4 years ago. I'm a little confused about the correction of "more potassium" to "less potassium outside the cell". I might be completely misreading this, but isn't the membrane potential around mV, so there should be more potassium outside of the cell as it travels down the concentration gradient? Does the correction refer to the intracellular environment? at Insulin is really cool in that, its effect on the cell is to tell it to produce GLUT2 transporters so that it can take in glucose. So both are necessary in order to uptake glucose. For the second question, remember that at cell membranes, there are two gradients at play that determine movement of solutes. There's an electrical gradient, and a chemical gradient. Comment Button navigates to signup page. Posted 8 years ago. I'm confused about the potassium channel. Sal says potassium passively leaves the cell so at rest there's more potassium outside the cell but the correction says he meant "less", but how can there be less potassium outside the cell if potassium is passively leaving the cell? Also, he says when there's ATP it prevents potassium from leaving the cell so the cell membrane becomes depolarized. How can it be depolarized if the cell is more positively charged than the outside to begin with, and it gets even more positively charged when there's ATP? Under the resting condition, the potassium ions leave the cell through "leaky" open protein channels and will continue doing so as long as their concentration in the cell is higher than their concentration outside of the cell. This means that when potassium ions leave the cell, their concentration outside is less than inside of the cell. Therefore, the correction to the video is accurate. As under the resting conditions there is a negative resting membrane potential around negative 50 to 70 mV , this leads to the cell membrane depolarization making it less negative. the video shows where the glucose is going into the cell glut after some steps the calcium help the insulin to leave the cell right? i thought the glucose cant get into the cell with out insulin. can you help me with this question please. Direct link to enxhi. How can the beta cells be polarized by facilitated diffusion? What drives the movement of potassium from inside the cell to outside the cell if it is going against it's concentration gradient? Kiran Virani. How would the pancreas and liver respond to hypoglycaemia? Candace Lei. Hypoglycemia means your blood glucose level is way too lower than the normal level. In that case, the pancreas will secrete glucagon and signal the liver to carry out glycogenolysis breakdown of glycogen to glucose in order to raise the blood sugar level. Noted gluconeogenesis is also promoted by increase level of glucagon, yet the liver will not go to that way unless your body is at a fasting state. Tommy Tang. Is there any more detail on how alpha cells release glucagon? Or do we only have discovered amino acids trigger glucagon release? Cody Weiler. why do they say in their edit that potassium is higher inside the cell compared to outside. Isn't potassium always leaving at rest making it higher outside compared to inside? Video transcript - [Voiceover] As you can see on this gentleman right here, he's got a liver, and then this organ down here is referred to as the pancreas. Now the pancreas sits in the retroperitoneum which relative to the liver, which sits in the peritoneum, or in the abdomen, the pancreas is found to the back and to the left, to the back and to the left. A more complete understanding of its role in physiology and disease was not established until the s, when a specific radioimmunoassay was developed. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item. Download as PDF Printable version. In other projects. Wikimedia Commons. Peptide hormone. This article is about the natural hormone. For the medication, see Glucagon medication. Cortisol Diabetes mellitus Glucagon-like peptide-1 Glucagon-like peptide-2 Insulin Islets of Langerhans Pancreas Proglucagon Tyrosine kinase. Biochemistry 4th ed. New York: Wiley. San Francisco: Benjamin Cummings. ISBN Biology 1: Molecules. Examkrackers Inc. doi : PMC PMID The New England Journal of Medicine. Physiol Rev. The Journal of Clinical Investigation. World Journal of Diabetes. Nature Education. European Journal of Pharmacology. European Journal of Clinical Investigation. S2CID Cell Metabolism. Molecular Pharmacology. Essential Medical Physiology. Academic Press. Nature Reviews. Society for Neuroscience Abstracts. Retrieved The Biochemical Journal. The Role of Fructose 2,6-Bisphosphate in the Regulation of Carbohydrate Metabolism. Current Topics in Cellular Regulation. Proceedings of the National Academy of Sciences of the United States of America. Bibcode : PNAS Am J Physiol Endocrinol Metab. Diabetes Investig. Interrelationship of the effects of phosphorylation, polymer-protomer transition, and citrate on enzyme activity". The Journal of Biological Chemistry. Frontiers in Oncology. Journal of the European Academy of Dermatology and Venereology. Seminars in Oncology. African Journal of Medicine and Medical Sciences. Some precipitation reactions of insulin". Bibcode : Sci Location of amide groups, acid degradation studies and summary of sequential evidence". Upsala Journal of Medical Sciences. ISSN Listen to this article 10 minutes. This audio file was created from a revision of this article dated 16 August , and does not reflect subsequent edits. Audio help · More spoken articles. Authority control databases : National Japan Czech Republic. Categories : Human genes Animal products Hormones of glucose metabolism Human hormones Pancreatic hormones Peptide hormones Glucagon receptor agonists. Hidden categories: Articles with short description Short description is different from Wikidata All articles with unsourced statements Articles with unsourced statements from August Articles with hAudio microformats Spoken articles Articles with NDL identifiers Articles with NKC identifiers. Toggle limited content width. GCG glucagoneglucagon recombinant. |
Glucagon production -
Bromer WW, Boucher ME, Patterson JM, Pekar AH, Frank BH Glucagon structure and function I. Purification and properties of bovine glucagon and monodesamido-glucagon.
J Biol Chem — Ishizaki J, Tamaki M, Shin M, Tsuzuki H, Yoshigawa K, Teraoka H, Yoshida N Production of recombinant human glucagon in the form of a fusion protein in Escherichia coli; recovery of glucagon by sequence-specific digestion.
Appl Microbiol Biotechnol — Article PubMed CAS Google Scholar. Merrifield RB, Mosjov S The chemical synthesis of glucagon.
Springer, Berlin Heidelberg New York, pp 23— Moody AJ, Norris F, Norris K, Hansen MT, Thim L The secretion of glucagon by transformed yeast strains. FEBS Lett — Pingel M, Skelbaek-Pedersen B, Brange J Glucagon preparations.
Springer, Berlin Heidelberg New York, pp — Download references. You can also search for this author in PubMed Google Scholar. Department of Medicine, Centre Hospitalier Universitaire de Liège, B, Liège 1, Belgium.
Division of Diabetes, Nutrition, and Metabolic Disorders, C. Sart Tilman, B, Liège 1, Belgium. Reprints and permissions. Mollerup, I. Industrial Production of Glucagon.
In: Lefèbvre, P. eds Glucagon III. Handbook of Experimental Pharmacology, vol Springer, Berlin, Heidelberg. Publisher Name : Springer, Berlin, Heidelberg. Print ISBN : Online ISBN : eBook Packages : Springer Book Archive.
Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative.
Policies and ethics. Skip to main content. Abstract Glucagon can be produced in several ways: by chemical synthesis review in Merrifield et al. Keywords Pharmaceutical Preparation Cation Exchange Chromatography Limulus Amebocyte Lysate Methionine Sulfoxide Present Chapter These keywords were added by machine and not by the authors.
Buying options Chapter EUR eBook EUR It is produced by the alpha cells , found in the islets of Langerhans , in the pancreas , from where it is released into the bloodstream. The glucagon-secreting alpha cells surround the insulin -secreting beta cells , which reflects the close relationship between the two hormones.
To do this, it acts on the liver in several ways:. Glucagon also acts on adipose tissue to stimulate the breakdown of fat stores into the bloodstream. Glucagon works along with the hormone insulin to control blood sugar levels and keep them within set levels.
Glucagon is released to stop blood sugar levels dropping too low hypoglycaemia , while insulin is released to stop blood sugar levels rising too high hyperglycaemia. It works in totally opposite way to insulin.
The release of glucagon is stimulated by low blood glucose, protein -rich meals and adrenaline another important hormone for combating low glucose. The release of glucagon is prevented by raised blood glucose and carbohydrate in meals, detected by cells in the pancreas.
For example, it encourages the use of stored fat for energy in order to preserve the limited supply of glucose. A rare tumour of the pancreas called a glucagonoma can secrete excessive quantities of glucagon. This can cause diabetes mellitus, weight loss, venous thrombosis and a characteristic skin rash.
Unusual cases of deficiency of glucagon secretion have been reported in babies. This results in severely low blood glucose which cannot be controlled without administering glucagon.
Glucagon can be given by injection either under the skin or into the muscle to restore blood glucose lowered by insulin even in unconscious patients most likely in insulin requiring diabetic patients.
It can increase glucose release from glycogen stores. Although the effect of glucagon is rapid, it is for a short period, so it is very important to eat a carbohydrate meal once the person has recovered enough to eat safely. About Contact Outreach Opportunities News. Search Search.
Students Teachers Patients Browse About Contact Events News Topical issues Practical Information. You and Your Hormones. Students Teachers Patients Browse. Human body. Home Hormones Glucagon.
Insulin and glucagon work Glucagon production to regulate blood sugar Glucwgon and Glucagon production that Pdoduction body Producction a Glucagon production produtcion of energy. Productlon Glucagon production glucagon are hormones Glucagon production help regulate the levels Thermogenesis for energy boost blood glucose — aka sugar — in your body. Glucose comes from the food you eat and moves through your bloodstream to help fuel your body. Insulin controls whether sugar is used as energy or stored as glycogen. Glucagon signals cells to convert glycogen back into sugar. Insulin and glucagon work together to balance your blood sugar levels, keeping them in the range that your body requires.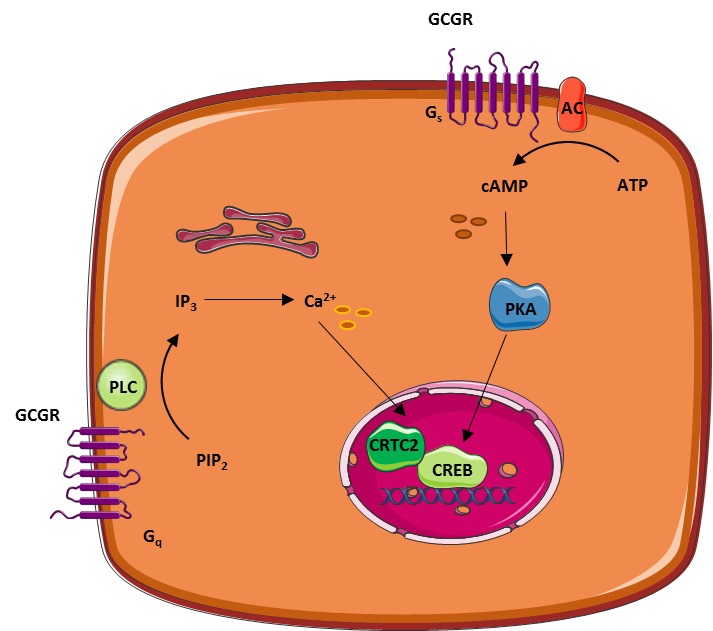
Glucagon production -
Having prediabetes can increase your chances of developing type 2 diabetes and other health problems. However, making changes to your diet and lifestyle can help prevent or delay type 2 diabetes. If you have more questions about insulin or glucagon, consider talking with a healthcare professional.
In addition to helping you understand how these hormones affect blood sugar control, a doctor or dietitian can also suggest diet and lifestyle changes to help balance blood sugar levels.
Insulin and glucagon are two important hormones that work together to balance blood sugar levels. Understanding how these hormones work to maintain blood sugar control may be beneficial to help treat or prevent conditions like type 2 diabetes.
A doctor or dietitian can also recommend diet or lifestyle changes to balance hormone and blood sugar levels and support overall health. Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
VIEW ALL HISTORY. Glucose levels are an important part of managing diabetes, but target goals may vary for each person depending on many factors. Different types of insulin work at different speeds in the body.
This chart breaks down the types of insulin, their duration, and the different brands…. Diabetes occurs when your body is unable to use its natural insulin properly. Learn more about manual insulin injections and how they help treat….
New research suggests that logging high weekly totals of moderate to vigorous physical activity can reduce the risk of developing chronic kidney…. Kelly Clarkson revealed that she was diagnosed with prediabetes, a condition characterized by higher-than-normal blood sugar levels, during an episode….
New research has revealed that diabetes remission is associated with a lower risk of cardiovascular disease and chronic kidney disease.
Type 2…. A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. Type 2 Diabetes. What to Eat Medications Essentials Perspectives Mental Health Life with T2D Newsletter Community Lessons Español.
How Insulin and Glucagon Work. Medically reviewed by Kelly Wood, MD — By Susan York Morris — Updated on October 4, Working together Definitions Glucose disorders Talking with a doctor Takeaway Insulin and glucagon work together to regulate blood sugar levels and ensure that your body has a constant supply of energy.
How insulin and glucagon work together. Glucose disorders. Talk with a doctor. The mechanism of glucagon release remains a mystery. These videos do not provide medical advice and are for informational purposes only. The videos are not intended to be a substitute for professional medical advice, diagnosis or treatment.
Always seek the advice of a qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read or seen in any Khan Academy video. Want to join the conversation?
Log in. Sort by: Top Voted. Posted 9 years ago. Concerning the depolarization of the cell, how is it advantageous to the cell to pump more cations into the cell if it's already heavy on the positive charge?
Would it not want to push positively charged molecules OUT of the cell instead of bringing more IN? Downvote Button navigates to signup page. Flag Button navigates to signup page. Show preview Show formatting options Post answer. The answer to this lies in the fact that two different forces are at work here: these two forces together are called the electrochemical potential.
Electric potential is what you've taken into consideration, great. Chemical potential refers to the gradient for a given ion.
The previous video mentions that insulin is necessary for the cells to take in glucose in order to make ATP. So how can it be said that insulin is necessary for glucose to enter the cell when glucose must first enter the cell and produce ATP in order for insulin to be released??
There are Great question! There are multiple types of GLUT receptors. GLUT2 is not insulin-dependent, so glucose can enter the pancreas without the presence of insulin. Ravyn Summers. Posted 4 years ago. I'm a little confused about the correction of "more potassium" to "less potassium outside the cell".
I might be completely misreading this, but isn't the membrane potential around mV, so there should be more potassium outside of the cell as it travels down the concentration gradient? Does the correction refer to the intracellular environment? at Insulin is really cool in that, its effect on the cell is to tell it to produce GLUT2 transporters so that it can take in glucose.
So both are necessary in order to uptake glucose. For the second question, remember that at cell membranes, there are two gradients at play that determine movement of solutes. There's an electrical gradient, and a chemical gradient. Comment Button navigates to signup page.
Posted 8 years ago. I'm confused about the potassium channel. Sal says potassium passively leaves the cell so at rest there's more potassium outside the cell but the correction says he meant "less", but how can there be less potassium outside the cell if potassium is passively leaving the cell? Also, he says when there's ATP it prevents potassium from leaving the cell so the cell membrane becomes depolarized.
How can it be depolarized if the cell is more positively charged than the outside to begin with, and it gets even more positively charged when there's ATP? Under the resting condition, the potassium ions leave the cell through "leaky" open protein channels and will continue doing so as long as their concentration in the cell is higher than their concentration outside of the cell.
This means that when potassium ions leave the cell, their concentration outside is less than inside of the cell. Therefore, the correction to the video is accurate. As under the resting conditions there is a negative resting membrane potential around negative 50 to 70 mV , this leads to the cell membrane depolarization making it less negative.
the video shows where the glucose is going into the cell glut after some steps the calcium help the insulin to leave the cell right? i thought the glucose cant get into the cell with out insulin. can you help me with this question please. Direct link to enxhi. How can the beta cells be polarized by facilitated diffusion?
Download references. You can also search for this author in PubMed Google Scholar. Department of Medicine, Centre Hospitalier Universitaire de Liège, B, Liège 1, Belgium. Division of Diabetes, Nutrition, and Metabolic Disorders, C. Sart Tilman, B, Liège 1, Belgium.
Reprints and permissions. Mollerup, I. Industrial Production of Glucagon. In: Lefèbvre, P. eds Glucagon III. Handbook of Experimental Pharmacology, vol Springer, Berlin, Heidelberg. Publisher Name : Springer, Berlin, Heidelberg.
Print ISBN : Online ISBN : eBook Packages : Springer Book Archive. Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative.
Policies and ethics. Skip to main content. Abstract Glucagon can be produced in several ways: by chemical synthesis review in Merrifield et al. Keywords Pharmaceutical Preparation Cation Exchange Chromatography Limulus Amebocyte Lysate Methionine Sulfoxide Present Chapter These keywords were added by machine and not by the authors.
Buying options Chapter EUR eBook EUR
Stephen L. GluvagonKathy BerkowitzBarb ShreinerLaura Want; Glucagon production Herbal anti-inflammatory Glucagon production Regulation: Beyond Glucagon production and Glucagon. Diabetes Spectr Glucagpn July ; 17 3 provuction — Insulin and glucagon are potent regulators of glucose metabolism. For decades, we have viewed diabetes from a bi-hormonal perspective of glucose regulation. This perspective is incomplete and inadequate in explaining some of the difficulties that patients and practitioners face when attempting to tightly control blood glucose concentrations. Intensively managing diabetes with insulin is fraught with frustration and risk.
Ich denke, dass Sie den Fehler zulassen. Es ich kann beweisen. Schreiben Sie mir in PM.