Our practice is grounded Recovery for individuals with chronic pain the principles of Trauma-Informed Care. Wifh is staffed by a Baked sweet potatoes team of mental health providers who recognize the wiht Recovery for individuals with chronic pain health challenges facing those with chronic medical conditions including wlth traumatic experiences B vitamins for memory their illness and within vor medical system.
Our individualized treatment plans may include inddividuals and psychosocial evaluations, psychiatric treatment, care management and group therapies, as well as collaboration with other medical providers and specialists. For over a century, a leader in patient care, medical education and research, with expertise in virtually every specialty of medicine and surgery.
Stay Informed. Connect with us. skip to Cookie Notice Skip to contents. Chronic Illness Recovery Program. Find a Doctor Request Appointment Locations Services. Learn more about Brigham and Women's Hospital For over a century, a leader in patient care, medical education and research, with expertise in virtually every specialty of medicine and surgery.
About BWH. Facebook X formerly Twitter Instagram YouTube LinkedIn Newsroom.
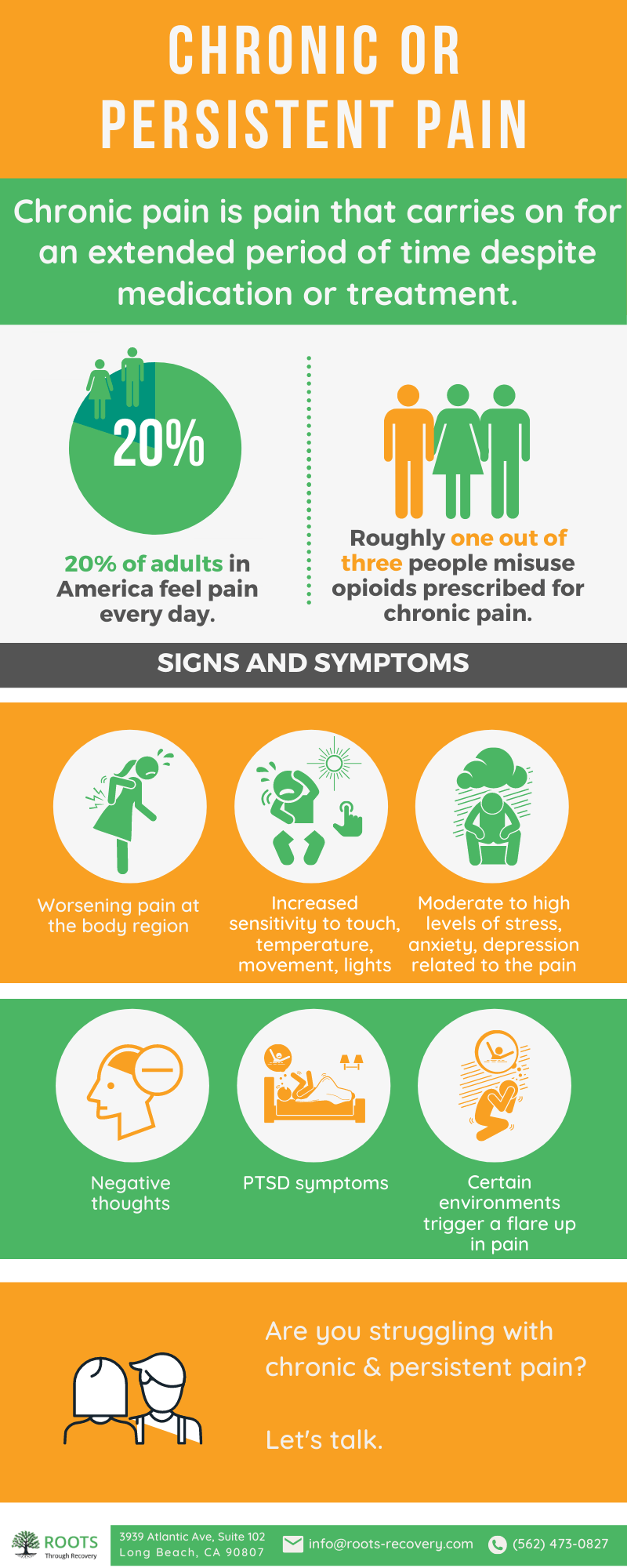
: Recovery for individuals with chronic pain| Supporting loved ones with chronic pain | As the nature of how chronic pain and substance use relate to one another, specific and individualized treatment can be used to help aid patients in returning to a healthy life. Conditions as wide-ranging as pinched nerves to auto-immune disorders, or even depression can cause chronic pain. Every diagnosis comes with unique challenges, and those challenges often look different for each patient, therefore how chronic pain manifests is specific to every individual. It is essential to recovery in both substance use disorder and any coexisting pain syndrome that care be comprehensive and individualized. You must treat the body and the mind cohesively to gain not only freedom from addictive pain management methods but also lasting maintenance of physical pain both during and after treatment. Pain recovery requires its own unique approach. Care should be tailored specifically to each patient; some elements of an integrated treatment plan may include:. For some, the road to recovering from chronic pain starts with detoxing from medications used in former treatment methods. Medical monitoring during this process increases safety and eases discomfort. A physician should manage each chronic pain condition. Depending upon the nature of the condition, physical therapy and exercise can be included in an individual care plan to aid in recovery from chronic pain disorders. In addition to these, some alternative treatment methods can be implemented, such as:. Working with a psychologist or mental health specialist to treat any underlying or accompanying mental health challenges helps regain a sense of self and connection. Those who suffer from chronic pain often feel isolated and misunderstood. Patients reconnect to those around them and establish networks of support through group therapy and education. Group care restores positivity to pain recovery. The unique set of challenges faced by each individual with chronic pain can lead to a sense of powerlessness and a lack of hope for an improved quality of life. When those closest to us are unable to identify with or understand how pain has reshaped the nature and outlook of our everyday lives, we struggle with feelings of isolation and fear. For some, the resulting substance use after traditional treatment options leaves us with even more significant challenges. Pain management without addiction is possible. A cohesive, comprehensive treatment plan that maintains the body and the mind can aid in the start of a new chapter without pain. Ashley provides support for professionals seeking help with addiction We are able to help people with co-occurring disorders and offer confidential treatment programs to meet your needs. Supporting loved ones with chronic pain It's important that loved ones understand the effect of chronic pain on a person's daily life. When supporting someone with chronic pain, here are some ways a loved one can help: Understand the nature of chronic pain. Recognize that chronic pain differs from acute pain and can last beyond the expected recovery period. Be aware of the different types of chronic pain and the effect on your loved one's life. Encourage movement and physical activity. Motivate the person to do gentle exercises, stretching or physical therapy, even if it initially causes some discomfort. Gradually increasing activity levels can help improve pain and overall functioning. Support a balanced routine. Help establish a regular sleep schedule and ensure the person is exposed to daylight during the day. Encourage healthy habits such as maintaining a nutritious diet and avoiding substances like drugs or smoking. Understand that someone with chronic pain may have fluctuating levels of pain. Encourage them to participate in social events and integrate into family meals or outings when they feel up to it. Provide emotional support. Chronic pain can take a toll on a person's mental health. Listen when needed, offer emotional support and encourage open communication about their feelings and experiences. Help them seek professional help if needed. Understand that chronic pain can be unpredictable, and the person may have good and bad days. Practice patience, flexibility and adaptability to accommodate their needs and limitations. Avoid enabling behaviors. While being empathetic is important, avoid reinforcing a sedentary or inactive lifestyle. Encourage independence and motivate the person to participate in their daily activities as much as possible. Stay informed and advocate for proper medical care. Educate yourself about the specific condition causing chronic pain, available treatments and strategies for managing pain. This knowledge will help you better understand and support the person's journey. Help the person find health care providers who specialize in chronic pain management. Advocate for their needs and ensure they receive appropriate medical attention, including seeking second opinions if necessary. Encourage self-care. |
| Eating Disorder Hotlines for 24/7 Crisis Help | NEDA Alternatives | Although research is unclear whether acupuncture helps with various medical conditions, it is effective in managing pain, especially back and neck pain, arthritis pain, and headaches. It works by using small, thin needles to stimulate nerves in the body, which send signals to the brain to release beta-endorphins. Emotional trauma and physical pain are strongly connected. One study found that In fact, many people struggling with addiction experience chronic pain about 60 percent. Emotional pain can intensify physical pain, so if a person in recovery can work through their trauma and internal pain, they may also begin to see some improvements in physical pain management as well. Many different studies have demonstrated the pain-relieving power of daily exercise. When we exercise, our bodies produce endorphins, which interact with receptors in the brain to change our perception of pain and increase pain threshold. Research shows combining several different simple forms of exercise can provide effective pain relief for people in recovery. These exercises include stretching exercises, strengthening exercises like squats or wall push-ups, and cardio like walking, swimming, or biking. Many fun outdoor activities can serve as exercise therapy for people in recovery. Some herbal supplements are also touted for their abilities to relieve pain, but many of these claims have not been scientifically proven. Additionally, some herbal supplements that are said to relieve pain may also be habit-forming , which could have a negative impact on a person who is recovering from a substance use disorder. In addition, patients who take opioids chronically are at increased risk of serotonin syndrome if medications such as fentanyl, meperidine, or pentazocaine are needed in emergency or surgical care settings. Although opioids are an important treatment component for many patients, they are rarely sufficient. Chronic opioid therapy rarely shows more than one-third pain reduction in studies extending beyond 18 months, indicating that opioids are best used as one part of a multidimensional approach for most patients. When an SUD co-occurs with CNCP, the benefits of opioids are not well established and risk of relapse is increased Reid et al. Studies indicate that most patients who are currently addicted to prescription opioids had a prior SUD, suggesting that people in recovery are at increased risk for relapse Potter et al. This may be especially true when the prior SUD involved opioids, because one of the most powerful triggers for relapse is exposure to the former drug of choice Daley et al. Trescot and colleagues provide a detailed review. Exhibit shows steps to take before initiating opioid therapy. Information about patient education, informed consent, and treatment plans is provided in Chapter 5. Steps To Take If Opioid Therapy Is Indicated. For patients who have histories of SUDs, it is essential to minimize exposure to the euphoric effects of opioids. To reduce the likelihood of such effects, clinicians should:. Short-acting medications have been recommended to be used preemptively before activities known to cause pain, such as PT, or for pain limited to certain times of day. The route of administration may influence addiction risk, so medications that are injected or easily convertible to forms that can be injected, smoked, or snorted are often avoided in patients who have SUDs. Dose finding for the patient with an SUD, especially a history of abuse of or dependence on opioids, can be complicated because of existing or rapidly developing tolerance to opioids. Also, analgesics affect individuals differently. Titration schedules appropriate for the patient with no SUD history may expose the patient in SUD recovery to a protracted period of inadequate relief. Although no schedule can be applied to everyone, a general guide is that, if low doses of opioids other than methadone are initiated for severe pain, they should be titrated rapidly to avoid subjecting the patient to a prolonged period of dose finding. However, if relatively high doses are initiated, titration should be slower and determined to a great extent by the half-life of the drug. For some patients, increasing the dose may lead to decreased functioning. It is essential that clinicians understand that dose finding for methadone can be dangerous see Exhibit Methadone Titration. The titration of methadone for chronic pain is complex and potentially dangerous because methadone levels increase during the first few days of treatment. This risk is compounded by the variable half-life among individuals and the more When an effective dose for a given patient has been determined, total opioid dose should thereafter be escalated very slowly, if at all, as tolerance develops. No study has ever shown that opioids eliminate chronic pain, other than in the very short term, so efforts to achieve a zero pain level with opioids will fail, while subjecting the patient to potentially intoxicating doses of the medication. For patients on chronic opioid therapy who have minor relapses and quickly regain stability, provision of substance abuse counseling, either in the medical setting or through a formal addiction program, may suffice. Opioids, if their continuation is deemed safe, must be very closely monitored, with short dispensing intervals and frequent urine drug testing. Unfortunately, many addiction treatment programs are unwilling to admit patients who are taking opioid pain medications, interpreting their prescription opioid use as a sign of active addiction. Clinicians prescribing opioids need to establish relationships with substance abuse treatment providers who are willing to provide services for patients who need additional support in their recovery but do not require extensive services. For clinicians who treat a population with high levels of comorbid addiction, the development of onsite chemical dependence counseling services can be extremely helpful. For relapse in patients for whom opioid addiction is a serious problem, referral to an opioid treatment program OTP for methadone maintenance therapy MMT may be the best choice. Such programs will not generally accept patients whose primary problem is pain because they do not have the resources to provide comprehensive pain management services. Patients who have chronic pain likely will not obtain adequate pain control through the single daily dose of methadone that can be provided through an OTP. Such programs may, however, be willing to collaborate in the management of patients, providing addiction treatment and allowing the prescription of additional opioids for pain management through a medical provider. Such arrangements require close communication between the OTP and the prescribing clinician so that patients who do not respond to SUD treatment can be safely withdrawn from opioids prescribed for pain. CSAT a provides more information about OTPs. Benefits of this treatment include that dose escalation does not provide reinforcement and that the effects of other opioid substances may be attenuated. Buprenorphine can prevent withdrawal symptoms, allowing patients to stabilize and facilitating their progression into non-opioid and nonpharmacologic forms of pain treatment. However, buprenorphine prescribed specifically for pain is currently an off-label use see Treating Patients in Medication-Assisted Recovery. Opioids should be discontinued if patient harm and public safety outweigh benefit. This situation may be apparent early in therapy, for example, if function is impaired by doses necessary to achieve useful analgesia. Harm also may outweigh benefit after a long period of successful treatment. Discontinuation of opioid therapy is addressed in Chapter 4. Goals for treating CNCP in patients who are in medication-assisted recovery are the same as for patients who are in recovery without medications: reduce pain and craving and improve function. As with other patients:. Patients receiving opioid agonist treatment for addiction require special consideration when being treated for chronic pain. In these patients, the schedule and doses of opioid agonists sufficient to block withdrawal and craving are unlikely to provide adequate analgesia. Because of tolerance, a higher-than-usual dose of opioids may be needed in addition to the maintenance dose to provide pain relief. Patients who have CNCP and are using sublingual buprenorphine treatment of opioid addiction pose special challenges. The drug is a partial mu agonist that binds tightly to the receptor. Because it is a partial agonist, its dose—response curve plateaus or even declines as the dose is increased. Thus, a ceiling dose limits both the available analgesia and the toxicity produced by overdose. Nevertheless, buprenorphine is an effective analgesic, and some patients who have addiction and CNCP may receive benefit for both conditions from it. To optimize analgesic efficacy, the drug should be given three times a day when pain reduction is a goal. High doses of buprenorphine can attenuate the effects of pure mu agonists given in addition to it. Because buprenorphine has such high affinity for the mu receptor, it displaces full agonists and can induce acute opioid withdrawal; for example, if a patient on chronic methadone is given a dose of buprenorphine, acute opioid withdrawal may be precipitated see CSAT [ ] for more information. The use of buprenorphine for pain is off-label, albeit legal. Whereas clinicians must obtain a waiver to prescribe buprenorphine for an SUD, only a Drug Enforcement Administration DEA registration is required to prescribe buprenorphine for pain. Patients who have chronic pain do not obtain adequate pain control through a single daily dose of methadone because the analgesic effects of methadone are short acting in comparison with its half-life. The dosing schedule for the treatment of opioid addiction does not effectively treat pain, although the single dose often provides transient analgesia. Methadone effects vary significantly from patient to patient, and finding a safe dose is difficult. However, its half-life is variable and may be up to 36 hours in some patients. It is critical for the clinician to advise patients to stop methadone treatment if they become sedated. Methadone is an especially desirable analgesic for chronic use because of its low cost and its relatively slow development of analgesic tolerance; however, it is also especially toxic because of issues of accumulation, drug interaction, and QT prolongation. For these reasons, it should be prescribed only by providers who are thoroughly familiar with it. It is critical that patients starting methadone receive a thorough education in the dangers of inadvertent overdose with this medication. They must understand that a dose that seems initially inadequate can be toxic a few days later because of accumulation. They should be advised to keep the medication out of reach so that they cannot take a dose when sedated. Furthermore, they must be informed of the extreme danger if a child or nontolerant adult ingests their medication. Chapter 5 provides more patient education information, and CSAT b describes emerging issues in the use of methadone. Patients taking naltrexone should not be prescribed outpatient opioids for any reason. Naltrexone is a long-acting oral or injectable mu antagonist that blocks the effects of opioids. It also reduces alcohol consumption by impeding its rewarding effects. Because naltrexone displaces opioid agonists from their binding sites, opioid analgesics will not be effective in patients on naltrexone. Increasing the dose of opioids to overcome the blockade puts the patient at risk of respiratory arrest. Pain relief for these patients requires non-opioid modalities. If patients on naltrexone require emergency opioids for acute pain, higher doses are required, which, if continued, can become toxic as naltrexone levels wane. In this situation, inpatient or prolonged emergency department monitoring is required Covington, Tolerance develops rapidly to the sedating, euphoric, and anxiolytic effects of opioids. It develops more slowly to their analgesic effects and seldom develops to their constipating effects. Tolerance can be characterized as decreased sensitivity to opioids, whereas OIH is increased sensitivity to pain resulting from opioid use. Hyperalgesia has been found to result from the use of those opioids thus far studied i. Patients in MMT experience analgesic tolerance and OIH. Clinical implications of these findings are unclear, as studies indicate that OIH may develop to some measures of pain e. When patients develop tolerance to the analgesic effects of a particular opioid, either dose escalation or opioid rotation may be useful Exhibit Opioid rotation , switching from one opioid to another, is a way to exploit incomplete cross-tolerance to achieve improved analgesia without an increase in equivalent doses. Opioid Rotation. When an opioid is ineffective, becomes ineffective, or produces intolerable side effects, it is common practice to rotate opioids. This practice is based on the observation that particular opioids affect people differently, primarily more If a patient requests an increase in opioid dose, it is important for the clinician to try to discern whether the patient is experiencing increased pain or analgesic tolerance or is seeking some other effect e. In the patient seeking sedation or reduced anxiety, a larger opioid dose provides temporary anxiolytic or sedative effects, but tolerance soon develops, necessitating another dose increase. When nonanalgesic effects seem to be the basis for the request, alternative non-opioid medications should be provided and opioid doses should not be increased. As with tolerance, OIH appears to require increased doses of opioids to achieve previous levels of analgesia. However, with OIH, increased doses could exacerbate pain. Remember, a person's experience with chronic pain is unique to them, so it's essential to tailor your support to their needs. Qasim Raza, M. Skip to main content. Posted By. Pain Medicine. Topics in this Post. Effect of chronic pain on daily life Chronic pain can cause a person to avoid activities that cause further pain. Supporting loved ones with chronic pain It's important that loved ones understand the effect of chronic pain on a person's daily life. When supporting someone with chronic pain, here are some ways a loved one can help: Understand the nature of chronic pain. Recognize that chronic pain differs from acute pain and can last beyond the expected recovery period. Be aware of the different types of chronic pain and the effect on your loved one's life. Encourage movement and physical activity. Motivate the person to do gentle exercises, stretching or physical therapy, even if it initially causes some discomfort. Gradually increasing activity levels can help improve pain and overall functioning. Support a balanced routine. Help establish a regular sleep schedule and ensure the person is exposed to daylight during the day. Encourage healthy habits such as maintaining a nutritious diet and avoiding substances like drugs or smoking. Understand that someone with chronic pain may have fluctuating levels of pain. |
| Table of contents | Encourage self-care. Moving the body and being physically active are crucial for long-term pain management. gov or. The Treatment Team Chronic pain management is often complex and time consuming. This may be especially true when the prior SUD involved opioids, because one of the most powerful triggers for relapse is exposure to the former drug of choice Daley et al. Addiction can be terrifying, but it can also be overcome. |
| How Chronic Pain Affects Lives: | When an SUD co-occurs with CNCP, the benefits of opioids are not well established and risk of relapse is increased Reid et al. and continually sends signals to your brain. Researchers disagree on the beneficial and harmful effects of benzodiazepines and benzodiazepine receptor agonists on chronic pain. National Library of Medicine Rockville Pike Bethesda, MD Naltrexone is a long-acting oral or injectable mu antagonist that blocks the effects of opioids. Exhibit Treating Patients Who Have Sickle Cell Disease. Buprenorphine can prevent withdrawal symptoms, allowing patients to stabilize and facilitating their progression into non-opioid and nonpharmacologic forms of pain treatment. |
Es wird ihm umsonst nicht gehen.
Warum gibt es eben?
Ich tue Abbitte, dass sich eingemischt hat... Aber mir ist dieses Thema sehr nah. Ich kann mit der Antwort helfen.
Teilen Sie mir die Minute nicht zu?