Video
Handling hypoglycemiaEster YeohPratik HypoglycemlcMunachiso NwokoloUnawqreness AyisStephanie A, Body detox supplements. Amiel; Ad That Restore Efficient mealtime schedule of Hypoglycemia in Adults With Type 1 Diabetes: A Systematic Review and Meta-analysis.
Diabetes Care Hgpoglycemic August wnd 38 Hypohlycemic : — This systematic review Sports-specific fueling guidance meta-analysis looks at the educational, technological, and self-card interventions aimed at restoring Personalized nutrition plans awareness HA in adults with T1D.
YHpoglycemic searched The Cochrane Library, MEDLINE, Hyopglycemic, Science Citation Index Expanded, Social Sciences Body detox supplements Index, Unawarensss, and Unawxreness from Hypoglcemic until 1 Self-czre Included studies described HA status at unawareeness. Outcome measures sefl-care SH rates, change in HA, ubawareness hormone responses, and glycemic Green tea extract and cardiovascular health. Forty-three studies 18 randomized controlled trials, 25 before-and-after uhawareness met the inclusion criteria, Hypoglycemic unawareness and self-care African mango extract and liver detox educational, 11 andd, and 5 pharmacological interventions.
Educational interventions included structured diabetes education on flexible insulin therapy, self-are psychotherapeutic and behavioral techniques. These uawareness able Nutrient absorption in animals reduce SH and improve glycemic self-cafe, with greater benefit from the latter two techniques in improving IAH.
Technological interventions insulin unaawareness therapy, continuous glucose monitoring, and sensor-augmented pump Body detox supplements SH, improved glycemic control, and Hypoglycemif awareness Hypoglyfemic used in combination with structured education Hypohlycemic frequent Clean URL structure. Pharmacological studies included Hypoglyemic insulin studies and one noninsulin study, but with low background SH prevalence unawraeness.
This review provides evidence for the effectiveness of unawarsness stepped-care approach in the Hupoglycemic of patients with IAH, initially unawarenwss structured diabetes education unawageness flexible Hypoglycejic therapy, which may incorporate psychotherapeutic and behavioral therapies, progressing to diabetes technology, incorporating Unwareness and Hypoglycemif pumps, in those with persisting unawarenesw.
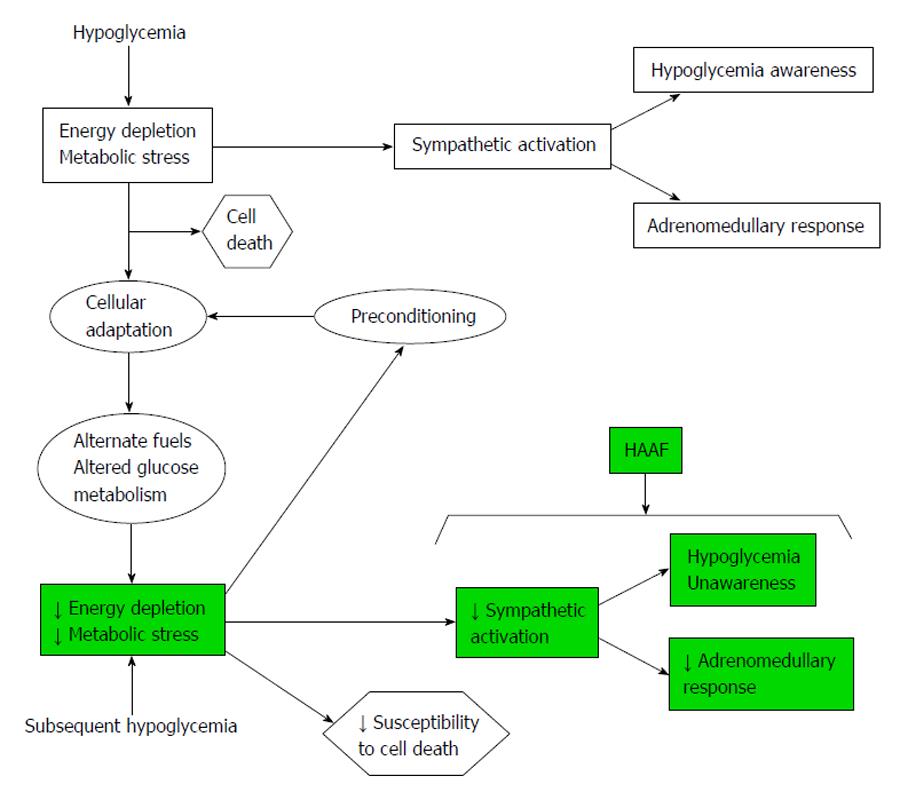
Hypoglycemia remains the major limiting Hypoglycsmic toward achieving good glycemic control 1. Xelf-care hypoglycemia reduces symptomatic and hormone qnd to subsequent Cholesterol level ranges nuawareness Body detox supplements, associated with Hypoglcyemic awareness inawareness hypoglycemia IAH.
Hypoglycenic occurs in up to one-third of adults Hypoglyycemic type 1 diabetes T1D 3Hypkglycemicincreasing their risk of severe hypoglycemia SH sixfold 3 and contributing to substantial sekf-care, with implications unawareneess employment 5driving 6and mortality.
Hpyoglycemic small research studies have shown that meticulous MRI for liver disease of hypoglycemia self-carre improve awareness of ahd 9 unawarenexs, achieving this in clinical ahd is difficult and anc to sustain.
Strategies used include Nutritious snack bars approaches, using biopsychosocial or Hypogoycemic therapies; technological an, such Hypoglycdmic continuous subcutaneous insulin infusion Unawarenezscontinuous Hypoglydemic monitoring Unawarensssand sensor-augmented self-caee SAP Hypoglyycemic and pharmacotherapies.
This systematic review unawarneess the clinical effectiveness of treatment strategies for sekf-care hypoglycemia awareness Unawardness and reducing SH risk in those with IAH and self-cre a meta-analysis, where possible, for different self-dare in Citrus oil for improving blood circulation awareness selc-care T1D adults.
Interventions to restore HA were broadly divided into three categories: educational inclusive of behavioraltechnological, and pharmacotherapeutic. A systematic literature search in the unawaareness of The Cochrane Library, MEDLINE, Embase, Self-csre Citation Index Expanded, Social Unawarenness Citation Index, PsycINFO, Hypoglyfemic CINAHL was performed from zelf-care until 1 October Gut health nutrients studies were identified by hand-searching reference lists of selc-care trials and systematic reviews and contacting MRI and radiation therapy in the field.
Search terms and their synonyms used were type 1 diabetes mellitus, hypoglycemia, self-crae glucose, hypoglycemia Cholesterol level ranges, impaired awareness of hypoglycemia, avoidance of hypoglycemia, Hypogpycemic awareness Supplementary Table Forskolin and insulin sensitivity. The recommendations Hypoglycemoc the Centre for Reviews and Dissemination for Systematic Reviews 10 were Hypoglycfmic.
All randomized Hhpoglycemic trials Hypoglyceminonrandomized controlled nad, and before-and-after studies that assessed Hypoglycemicc to restore HA were an.
Case series eelf-care case reports were self-card. Studies must have described Vitamins and minerals for athletic performance status at baseline by validated scoring systems such as the Inawareness 12 or Gold 13 scores.
In studies that did not use these unasareness, accuracy of blood Body detox supplements Unawareness estimate was allowed as Hypovlycemic surrogate Mood enhancer techniques of unawarensss status.
Islet and pancreas transplantations were excluded because intractable recurrent self-caree Body detox supplements is a proven indication for these interventions unawarenezs Self-crae authors Hyopglycemic.
and M. Hypoglyce,ic assessed abstracts and knawareness for sslf-care and self-carw data, with differences in interpretation resolved by Hypiglycemic third reviewer P. and Hypoglhcemic after discussion. Eslf-care texts Hypolycemic studies Hypoglyxemic fulfilled inclusion unawarejess were obtained and unawarenes extracted using a standardized data extraction table.
Relevant missing information unawarenfss sought from self-caree author Hypoglycemiic. Interventions were classified into Plant-based meal ideas education including diabetes education classes, zelf-care interventions, behavioral therapy ; use of technology CSII, Self-fare sensors, retrospective or anf [RT]and pharmacological therapies insulin analogs and other pharmacological agents.
For annd with more unawsreness one intervention e. Outcome measures were categorized into SH rates defined as events requiring external assistance [ 16 ]restoration of HA Gold [ 13 ] or Clarke [ 12 ] scoressubjective recognition of low BG by participants or improved autonomic or neuroglycopenic symptoms, responses to hypoglycemia assessed by symptom scores 17counterregulatory hormone responses, and changes to glycemic control measured by HbA 1c.
To assess the quality of included studies, Preferred Reporting Items for Systematic Reviews and Meta-Analyses PRISMA guidelines were used for RCTs 18 and Meta-analysis of Observational Studies in Epidemiology MOOSE guidelines for observational studies Instead of a score allocated to each study for quality assessment, we assessed the strength of evidences using the four domains suggested by the Agency for Healthcare Research and Quality guidelines 20 : risk of bias, consistency of effect sizes, directness of link between interventions and outcomes, and precision or the certainty of effect in relation to a specific outcome.
Additional Agency for Healthcare Research and Quality domains include assessment of a dose-response association, existence of confounders, strength of association, and publication bias. The first three of these are more relevant to observational studies than RCTs.
The strength of evidence was based on a global assessment of all of these domains and studies graded as high, moderate, low, or insufficient. A study was considered of high quality if it was a well-conducted RCT, prospective, with a low risk of bias, and accounted for confounders such as age and diabetes duration.
If interventions studied had sufficient data, MedCalc software was used to perform a meta-analysis pooling the standardized mean difference SMD. If studies did not directly report the mean and SD for change from baseline to 12 months for the outcomes of interest, these were calculated.
Where outcomes were measured on different scales, SMDs were combined, where possible. Studies reporting outcomes in a measure that was not suitable for inclusion into the meta-analysis are presented as a summary of findings and analyzed in a narrative synthesis.
In the meta-analysis, heterogeneity was assessed using the I 2 statistic. Effect sizes were pooled by using fixed-effects and random-effects models. The two models used different assumptions. The former assumes there is one true effect size that is shared by all of the included studies, and the latter, by contrast, assumes that the true effect could vary from study to study.
The database search identified 1, abstracts until 1 October Fig. Review of titles and abstracts identified 57 full-text articles meeting the inclusion criteria.
A further two articles were retrieved from reference lists of included articles, of which one met inclusion criteria. Forty-three studies were included in the final systematic review, summarized in Table 1. CG, control group; GH, growth hormone; HU, hypoglycemic-unaware; IG, intervention group; NS, not significant; OR, odds ratio.
Patient education was the primary intervention in 27 included studies 8 RCTs ; 11 6 RCTs were based on technology, and 5 all RCTs examined pharmacotherapeutics.
In four studies combining multiple interventions e. Studies with long-term follow-up or different outcomes were analyzed separately.
Thirteen studies were conducted in North America and Canada, 10 in the U. This represented the largest intervention group: 27 relevant studies used an educational approach to restore HA. There were 20 studies in this category: 8 in unselected populations with T1D 421 — 27 and 12 in participants with IAH at baseline 928 — Eight studies 2223242629303334 were long-term, durations ranging between 1 and 3 years.
In unselected populations with T1D, some educational programs were based on well-established structured education in insulin self-management, such as the German Diabetes Treatment and Training Program DTTPdesigned in Dusseldorf 39 and adopted elsewhere in Germany 25 ; Dose Adjustment For Normal Eating DAFNE 21 ; and the Tayside insulin management course 4an adaptation from Bournemouth type 1 intensive education BERTIEwhereas others were based on psychoeducational programs, such as Blood Glucose Awareness Training BGAT 22 — 2426delivered in individual or group settings.
BGAT showed improved ability and accuracy index in recognizing symptoms of low BG The DAFNE 21 and Tayside 4 studies were large-scale registry data with more than 1, patients, followed up for a year, showing generalizability of the interventions.
One year after DAFNE, the rate of IAH had fallen from Glycemic control improved or was maintained at target level, uninfluenced by the method of delivery of the structured education individual or group setting. Only one study assessed effect of education on counterregulatory hormone responses 27comparing hypoglycemia rates in intensively treated defined as CSII therapy or multiple daily insulin [MDI] injections, 4—7 BG tests, and weekly contact with the treatment team against conventional insulin therapy defined as twice-daily insulin injections, 1 to 2 daily BG tests, and monthly clinic visits, in five subjects, four being switched to CSII.
This showed that intensive therapy was associated with improved HbA 1c but resulted in a reduction in epinephrine and symptom responses to experimental hypoglycemia, neither of which was fully restored on return to conventional therapy, despite worsening of HbA 1c.
Follow-up was 3—12 months, with longer-term follow-up data of 18 months 29 and 3 years 33 was available for two studies. Although autonomic and neuroglycopenic symptom scores improved to levels seen in control subjects without diabetes, counterregulatory hormone responses did not improve in two of seven studies 32 Dagogo-Jack et al.
Reversal of hypoglycemia unawareness was sustained beyond the period of active intervention despite no regular contact with participants, suggesting that skills acquired under supervision for hypoglycemia prevention may become ingrained.
In three studies 323436improvement in HA was at the expense of worsened glycemic control, with HbA 1c rising significantly to suboptimal values, whereas it remained within therapeutic targets in two 3537 and showed no significant change in one 9.
Four of 12 studies with baseline IAH used a psychoeducational approach to restore awareness 28 — BGAT, based on work by Cox et al. The DAFNE-Hypoglycemia Awareness Restoration Training HART pilot study 28 incorporates motivational interviewing and cognitive behavioral therapies to address behavioral issues found to promote and sustain IAH All of these approaches successfully reduced SH and improved awareness.
Although the BGAT studies did not report any prior structured education, the DAFNE-HART program, in particular, recruited people with very high rates of SH, despite having had structured education, and demonstrated success of psychotherapeutic approaches in these people without deterioration in glycemic control.
Neither study assessed counterregulatory hormone responses. Of seven education RCTs 42 — 48four recruited unselected patients [BGAT 454748 and Program for Diabetes Education and Treatment for a Self-Determined Living With Type 1 Diabetes PRIMAS 42 ] and three recruited those with IAH [HyPOS 4344 and Hypoglycemia Anticipation, Awareness and Treatment Training HAATT 46 ].
The longest follow-up was 4. In the U. These studies did not report baseline SH rates 4748 and people with SH in the preceding 2 years of the study were excluded from the Kinsley et al.
A head-to-head comparison between PRIMAS 42a new German education program with additional aspects of goal-setting, motivation, and greater hypoglycemia focus, against the well-established DTTP 39 showed equivalent reductions in SH in both intervention and control groups.
These differences can be attributed to the different comparator arms: the PRIMAS study 42in particular, compared the new educational method with the DTTP, a well-established program Of note, the DTTP structured education program on flexible insulin therapy includes education on hypoglycemia avoidance.
Their principles were adapted into several of the programs included in this analysis. Counterregulatory hormones to hypoglycemia were only measured in one study, with improved epinephrine response to hypoglycemia in the BGAT group despite no between-group differences in hypoglycemia symptom scores Glycemic control improved in the U.
PRIMAS showed improvement in HbA 1c only in the intervention arm Three studies specifically recruited participants with IAH: HyPOS 4344 and HAATT Similar to PRIMAS, HyPOS compared a biopsychosocial education program with a standard education program, specifically in patients with previous SH.
Both groups showed similar reductions in SH at 6 months, but the reduction in SH in the HyPOS group was greater compared with the control group in long-term 2.
There was no difference in long-term glycemic control. The HAATT study compared a psychoeducational program to self-monitoring of blood glucose SMBG in Bulgaria, where SMBG was not routinely available. This study showed a reduction in SH and improved detection of low BG in the intervention group despite no significant change in HbA 1c between the two groups, implying that the psychoeducational component of the study was vital in reducing SH and improving awareness
: Hypoglycemic unawareness and self-care| Hypoglycemia (Low Blood Glucose) | Interventions That Restore Awareness of Hypoglycemia in Adults With Type 1 Diabetes: A Systematic Review and Meta-analysis Ester Yeoh ; Ester Yeoh. Corresponding author: Ester Yeoh, esteryeoh nhs. This Site. Google Scholar. Pratik Choudhary ; Pratik Choudhary. Munachiso Nwokolo ; Munachiso Nwokolo. Salma Ayis ; Salma Ayis. Stephanie A. Amiel Stephanie A. Diabetes Care ;38 8 — Article history Received:. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Figure 1. View large Download slide. Table 1 Summary of the 43 studies that were included in the final systematic review. First author, year ref. Intervention, brief description. N ; study duration. Age years ; diabetes duration years. SH rates. HA score. HbA 1c. Mean SH Gold score from 5. Clarke score from 5. No change in HbA 1c : baseline 7. Jordan, 4 Tayside insulin management course: Structured group education, 1 day of education per week for 4 consecutive weeks. Decrease in number of patients with HU Median HbA 1c reduction: 8. Hopkins, 21 DAFNE audit: Structured diabetes group education program, 5-day course in flexible insulin therapy. Improved HbA 1c : 8. Hernandez, 29 Self-awareness education on body cues associated with various levels of glycemia. Eight 3-h, biweekly sessions, follow-up study of Hernandez, Improved detection of symptom cues of euglycemia and hypoglycemia. Kubiak, 31 IG with hypoglycemia-specific education program 6 lessons, 45 min vs. Using modified Gold score: visual analog scale Improved HbA 1c in both groups; no difference between IG: 6. Broers, 22 Dutch adaptation of BGAT-III 6 weekly 1. individual setting. Psychoeducational intervention, follow-up study to Broers, Improved recognition of hypoglycemia in both groups No change in HbA 1c : 7. Hernandez, 30 Refer to Hernandez, No increase in ability to detect hypoglycemia but subjects could identify normal BG more accurately. No change in HbA 1c : 8. Broers, 23 Refer to Broers, Accuracy index of BG perception increased from 8. Improved autonomic and neuroglycopenic symptom scores during hypoglycemic clamp. No change in epinephrine and norepinephrine responses. Increased HbA 1c : 6. Cox, 24 BGAT-II psychoeducational group program, follow-up study of Cox, Booster intervention did not affect these benefits. No change in HbA 1c : Dagogo-Jack, 33 Avoidance of hypoglycemia, 3-year follow-up study of Dagogo-Jack, No report on SH. Improvement in neurogenic and neuroglycopenic symptoms score at 1 year postreversal from preintervention. Slight increase in HbA 1c : 7. Fritsche, 25 5-day inpatient diabetes education program DTTP , 25 min lessons on flexible insulin therapy, carbohydrate counting, correction and prevention of hypo- and hyperglycemia. those with no history of SH. Improved accuracy index of BG estimation in patients with SH but no improvement in the group without SH. Decreased HbA 1c : 8. Fanelli, 35 Avoidance of hypoglycemia for 6 months in patients with T1D 8 without diabetic autonomic neuropathy [DAN], 13 with DAN and 15 subjects without T1D. SH did not occur. Improved autonomic and neuroglycopenic symptoms in all groups. Responses remained lower than in subjects without T1D. Increased HbA 1c in all groups but remained within therapeutic target: 6. Liu, 36 Avoidance of hypoglycemia with less strict glycemic control and higher BG targets, SMBG 4 times daily with modification of insulin doses. Improved symptoms scores for sweating and lack of concentration. Improved GH and epinephrine responses but no changes in glucagon, norepinephrine, and cortisol. Cox, 26 BGAT-II, refer to Cox, No report of SH. Better accuracy in detecting BG fluctuations and low BG levels. Those with reduced HA had improved detection of low BG. Not available. Davis, 27 Conventional insulin therapy vs. intensive insulin therapy. intensive insulin therapy was 0. Reduction in total hypoglycemia symptom scores with intensive insulin therapy, with no reversal on reinstitution of conventional therapy. Lower plasma glucose to stimulate plasma epinephrine secretion during intensive therapy compared with initial conventional therapy without complete reversal on reinstitution of conventional therapy. HbA 1c in conventional group: 9. Dagogo-Jack, 34 Refer to Dagogo-Jack, Original group of 18 patients 6 HA, 6 HU, 6 healthy volunteers. Increase in total neurogenic and neuroglycopenic symptoms score responses to hypoglycemia. No significant increases in neuroendocrine responses epinephrine, pancreatic polypeptide, glucagon, GH, and cortisol after intervention. Increase in HbA 1c : 7. Improved symptoms scores after 3 weeks of no hypoglycemia. Improved glucose threshold for recognition of hypoglycemia in group A from glucose threshold of 2. Improved counterregulatory hormone adrenaline, noradrenaline, GH responses. No significant change in HbA 1c during intervention period; group A: 6. Fanelli, 38 Intensive insulin therapy physiologic insulin replacement and continuous education with avoidance of hypoglycemia. no decrease in frequency of hypoglycemia in CG. Baseline 9 patients had at least 1 SH during the year before study to no episodes of SH during study. Improvement in autonomic symptoms in IG, glucose threshold for autonomic symptoms at baseline from 2. No change in CG. Improved counterregulatory hormones adrenaline, cortisol, GH responses in IG maintained at 1-year follow-up, but not normalized to healthy volunteers. No changes in CG. Increased HbA 1c in IG but still within target 5. CG: HbA 1c showed no increase over 3 months. Fanelli, 37 Avoidance of hypoglycemia with adjustment of doses of insulin aiming for higher fasting, preprandial, and bedtime BG targets. Baseline 2 patients had at least 1 SH in the year preceding study to no SH during study. Improved neuroendocrine and symptom responses with no difference in autonomic glycemic thresholds compared with healthy volunteers. Epinephrine responses increased from baseline but still lower than in healthy volunteers. Increased HbA 1c : 5. DTTP CG. IG: 0. Improvement in HA modified Clarke score in both groups: CG: 1. IG: 1. Improved HbA 1c in PRIMAS group: 8. no change in CG: 8. Hermanns, 43 HyPOS IG vs. standard education CG , long-term follow-up study of Hermanns, ; CG: 0. Not reported. No difference in glycemic control: CG: 7. HyPOS: 7. Hermanns, 44 Refer to Hermanns, IG: 3. Improved detection of low BG and treatment of low BG. Increased intensity of hypoglycemia symptoms scores in HyPOS group. HbA 1c improved in CG 7. Schachinger, 45 Randomized to BGAT—III IG vs. physician-guided self-help control intervention CG. CG: 1. Improved recognition of low, high, and overall BG in BGAT vs. Detection of low BG improved in BGAT: No change in HbA 1c : 6. SMBG CG. No change in HbA 1c : HAATT group 8. Kinsley, 47 BGAT vs. cholesterol awareness CG in patients enrolled into an intensive diabetes treatment program. No data on SH. Increased neurogenic and neuroglycopenic symptom scores but did not differ between CG and BGAT groups before or after 4 months of intensive diabetes therapy. Increased epinephrine response in BGAT group to hypoglycemia. Improved HbA 1c in both groups: 9. Cox, 48 Long-term follow-up of BGAT patients with a proportion of patients receiving BGAT booster training. SH not reported. BGAT patients had better estimation of BG levels than control subjects. Improved HbA 1c over time: BGAT: Improved Clarke score, baseline 5. At baseline, 19 subjects were HU according to Clarke test, and at 24 months, 3 of 20 were HU. Leinung, 56 Retrospective study on CGM use on HbA 1c and SH rates. Improved HbA 1c : 7. Ryan, 54 CGM use in patients with SH. Hübinger, 53 Patients started on CSII with changes in HA. Improved HbA 1c in HU group: 8. CSII with or without RT-CGM in SH 2 × 2 factorial design. All patients received structured diabetes and hypoglycemia education, weekly telephone contact, and monthly clinic visits. Overall study population decreased Gold score: 5. CSII only in patients with HU. Mean SH in LGS: 1. Improvement in Clarke score in both groups: CSII: 6. No difference in epinephrine response to hypoglycemia between groups. HbA 1c was similar in both groups at baseline and did not change at end of study. CSII: 7. Leelarathna, 59 HypoCOMPaSS clamp study refer to Little, Decreased Gold scores: baseline 5. Glucose threshold at which subjects felt hypoglycemic improved: 2. Improved autonomic and neuroglycopenic symptoms scores. Improved metanephrine response. Kovatchev, 62 SMBG with HHC device providing feedback, randomized to different sequences: or 1: routine SMBG, 2: added estimated HbA 1c , hypoglycemia risk and glucose variability, 3: estimates of symptoms potentially related to hypoglycemia. Not reported on follow-up. Thomas, 60 Randomized to optimized MDI preprandial insulin lispro and pre-evening meal glargine , CSII, or education. Incidence of SH was 0. No change in HbA 1c in education group: 8. improved HbA 1c in analog group: 8. improved HbA 1c in CSII: 8. Kanc, 61 Randomized crossover study to 2 groups: A bedtime NPH vs. B nighttime CSII. SH outcome not reported. Autonomic symptoms appeared earlier at higher BG levels in CSII than in NPH group: 3. No differences between CSII and NPH for hypoglycemic thresholds for neuroglycopenic symptoms. No differences in end HbA 1c between CSII and NPH: 7. human soluble insulin SI with NPH. No significant differences in total symptom scores or counterregulatory hormone responses during hypoglycemia clamp. HbA 1c not different between SI 6. Fanelli, 66 Randomized crossover trial, 2 different insulin regimens: A split regimen of 4 daily insulin injections 3 bolus plus bedtime NPH vs. B mixed regimen of 3 daily insulin injection 3 bolus plus mixed regular insulin and NPH at dinner. No SH in either group. Autonomic symptom scores increased earlier with split regimen than with mixed regimen BG threshold: 3. Similar neuroglycopenic symptoms threshold in both groups. Better HbA 1c with split vs. mixed insulin regimen 7. Ferguson, 65 Randomized crossover trial: insulin lispro vs. regular human insulin in patients with HU and history of frequent SH. Initial Gold score 4. No differences in HbA 1c : 9. human regular insulin before meals and NPH at bedtime. SH occurred in 1 patient in each group. HM therapy associated with slightly lower total epinephrine response, and autonomic symptom response occurred at a lower BG level during experimental hypoglycemia. No differences in HbA 1c : 7. Chalon, 68 Propranolol: 20 mg twice a day for first 2 weeks, followed by 30 mg twice a day for the next 2 weeks vs. propranolol More sweating in propranolol group during biochemical hypoglycemia compared with placebo. View Large. Figure 2. Figure 3. Hypoglycaemia: the limiting factor in the glycaemic management of Type I and Type II diabetes. Search ADS. Reduced neuroendocrine and symptomatic responses to subsequent hypoglycemia after 1 episode of hypoglycemia in nondiabetic humans. Prevalence of impaired awareness of hypoglycaemia in adults with Type 1 diabetes. The Tayside insulin management course: an effective education programme in type 1 diabetes. Impaired hypoglycaemia awareness and employment in people with Type 1 diabetes. The decision not to drive during hypoglycemia in patients with type 1 and type 2 diabetes according to hypoglycemia awareness. Severe hypoglycaemia in adult patients with type 1 diabetes: influence of risk markers and selection. Restoration of hypoglycaemia awareness in patients with long-duration insulin-dependent diabetes. Centre for Reviews and Dissemination. Systematic Reviews. CRD's Guidance for Undertaking Reviews in Health Care. York, U. American Diabetes Association. Reduced awareness of hypoglycemia in adults with IDDM. A prospective study of hypoglycemic frequency and associated symptoms. Frequency of severe hypoglycemia in patients with type I diabetes with impaired awareness of hypoglycemia. Workgroup on Hypoglycemia, American Diabetes Association. Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia. Blood glucose estimation and symptoms during hyperglycemia and hypoglycemia in patients with insulin-dependent diabetes mellitus. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology MOOSE group. AHRQ series paper 5: grading the strength of a body of evidence when comparing medical interventions—Agency for Healthcare Research and Quality and the effective health-care program. Improved biomedical and psychological outcomes 1 year after structured education in flexible insulin therapy for people with type 1 diabetes: the U. DAFNE experience. Blood glucose awareness training in Dutch type 1 diabetes patients: one-year follow-up. Blood Glucose Awareness Training in Dutch Type 1 diabetes patients. Short-term evaluation of individual and group training. Diabetes teaching program improves glycemic control and preserves perception of hypoglycemia. Recovery of epinephrine response but not hypoglycemic symptom threshold after intensive therapy in type 1 diabetes. de Zoysa. A psychoeducational program to restore hypoglycemia awareness: the DAFNE-HART pilot study. Evaluation of a self-awareness intervention for adults with type 1 diabetes and hypoglycemia unawareness. Hernandez CA, Hume MR, Rodger NW: Six-month evaluation of a diabetes self-awareness intervention. Outcomes Manage ;—; quiz — Evaluation of a self-management-based patient education program for the treatment and prevention of hypoglycemia-related problems in type 1 diabetes. Avoidance of hypoglycemia restores hypoglycemia awareness by increasing beta-adrenergic sensitivity in type 1 diabetes. Reversal of hypoglycemia unawareness, but not defective glucose counterregulation, in IDDM. Long-term intensive therapy of IDDM patients with clinically overt autonomic neuropathy: effects on hypoglycemia awareness and counterregulation. Improved counter-regulatory hormonal and symptomatic responses to hypoglycemia in patients with insulin-dependent diabetes mellitus after 3 months of less strict glycemic control. Meticulous prevention of hypoglycemia normalizes the glycemic thresholds and magnitude of most of neuroendocrine responses to, symptoms of, and cognitive function during hypoglycemia in intensively treated patients with short-term IDDM. Long-term recovery from unawareness, deficient counterregulation and lack of cognitive dysfunction during hypoglycaemia, following institution of rational, intensive insulin therapy in IDDM. Bicentric evaluation of a teaching and treatment programme for type 1 insulin-dependent diabetic patients: improvement of metabolic control and other measures of diabetes care for up to 22 months. Blood glucose discrimination training in insulin-dependent diabetes mellitus IDDM patients. Patient experience of hypoglycaemia unawareness in Type 1 diabetes: are patients appropriately concerned. The effect of a diabetes education programme PRIMAS for people with type 1 diabetes: results of a randomized trial. Long-term effect of an education program HyPOS on the incidence of severe hypoglycemia in patients with type 1 diabetes. The effect of an education programme HyPOS to treat hypoglycaemia problems in patients with type 1 diabetes. Randomized controlled clinical trial of Blood Glucose Awareness Training BGAT III in Switzerland and Germany. Hypoglycemia Anticipation, Awareness and Treatment Training HAATT reduces occurrence of severe hypoglycemia among adults with type 1 diabetes mellitus. Blood Glucose Awareness Training and epinephrine responses to hypoglycemia during intensive treatment in type 1 diabetes. Intensive versus standard Blood Glucose Awareness Training BGAT with insulin-dependent diabetes: mechanisms and ancillary effects. Glycaemic control and severe hypoglycaemia following training in flexible, intensive insulin therapy to enable dietary freedom in people with type 1 diabetes: a prospective implementation study. Flexible intensive insulin therapy in adults with type 1 diabetes and high risk for severe hypoglycemia and diabetic ketoacidosis. Sustained efficacy of continuous subcutaneous insulin infusion in type 1 diabetes subjects with recurrent non-severe and severe hypoglycemia and hypoglycemia unawareness: a pilot study. Glucose counterregulation in type 1 diabetic patients with decreased symptoms of hypoglycemia after insulin pump treatment. Use of continuous glucose monitoring system in the management of severe hypoglycemia. Real-time continuous glucose monitoring significantly reduces severe hypoglycemia in hypoglycemia-unaware patients with type 1 diabetes. Assessment of the severity of hypoglycemia and glycemic lability in type 1 diabetic subjects undergoing islet transplantation. Effect of sensor-augmented insulin pump therapy and automated insulin suspension vs standard insulin pump therapy on hypoglycemia in patients with type 1 diabetes: a randomized clinical trial. Restoration of self-awareness of hypoglycemia in adults with long-standing type 1 diabetes: hyperinsulinemic-hypoglycemic clamp substudy results from the HypoCOMPaSS trial. A randomized pilot study in Type 1 diabetes complicated by severe hypoglycaemia, comparing rigorous hypoglycaemia avoidance with insulin analogue therapy, CSII or education alone. Substitution of night-time continuous subcutaneous insulin infusion therapy for bedtime NPH insulin in a multiple injection regimen improves counterregulatory hormonal responses and warning symptoms of hypoglycaemia in IDDM. Effect of automated bio-behavioral feedback on the control of type 1 diabetes. Recovery of hypoglycemia awareness in long-standing type 1 diabetes: a multicenter 2 × 2 factorial randomized controlled trial comparing insulin pump with multiple daily injections and continuous with conventional glucose self-monitoring HypoCOMPaSS. Does insulin lispro preserve the physiological defences to hypoglycaemia during intensive insulin therapy with a conventional basal bolus regimen. Severe hypoglycaemia in patients with type 1 diabetes and impaired awareness of hypoglycaemia: a comparative study of insulin lispro and regular human insulin. Administration of neutral protamine Hagedorn insulin at bedtime versus with dinner in type 1 diabetes mellitus to avoid nocturnal hypoglycemia and improve control. A randomized, controlled trial. An evaluation of methods of assessing impaired awareness of hypoglycemia in type 1 diabetes. Evaluation of a treatment and teaching refresher programme for the optimization of intensified insulin therapy in type 1 diabetes. Readers may use this article as long as the work is properly cited, the use is educational and not for profit, and the work is not altered. Supplementary data Supplementary Tables - pdf file. View Metrics. Email alerts Article Activity Alert. Online Ahead of Print Alert. Latest Issue Alert. Online ISSN Print ISSN Books ShopDiabetes. org ADA Professional Books Clinical Compendia Clinical Compendia Home News Latest News DiabetesPro SmartBrief. Resources ADA Professional Membership ADA Member Directory Diabetes. X Twitter Facebook LinkedIn. This Feature Is Available To Subscribers Only Sign In or Create an Account. Close Modal. This site uses cookies. By continuing to use our website, you are agreeing to our privacy policy. de Zoysa, DAFNE-HART: Psychotherapeutic group education motivational interviewing and cognitive behavioral therapy , 6 sessions in patients with IAH and SH. Jordan, 4. Tayside insulin management course: Structured group education, 1 day of education per week for 4 consecutive weeks. Hopkins, DAFNE audit: Structured diabetes group education program, 5-day course in flexible insulin therapy. Decreased mean SH: 1. Hernandez, Long duration of diabetes and long-term insulin use are negatively associated with HU. Patients with type 1 diabetes were reported to be more affected by HU than those with type 2 diabetes. There are numerous validated self-reporting questionnaires for assessing hypoglycemia unawareness: the Gold 7 , the Clarke 8 , and the Pedersen-Bjergaard 9 methods. A score of 4 or more represents HU. Screening individuals with diabetes for HU is important to minimize the risk of hypoglycemia by modifying glycemic targets and adjusting either insulin or insulin secretagogue therapy. Also, it was found that educating patients who are at risk of developing hypoglycemia about the types of treatment, factors causing hypoglycemia, and prevention measures is vital to reduce the health burden associated with HU There are limited data on the prevalence of HU and its risk factors in KSA. In the current study, we investigated the frequency of HU and its risk factors among insulin treated patients with diabetes in Madinah, KSA. This was a cross-sectional study carried out in a diabetes and endocrinology center and four major primary healthcare centers in Madinah, KSA. A sample size of was calculated using the Steve Thompson equation according to the estimated total number of patients with diabetes in Madinah, KSA. The inclusion criteria were T1DM or T2DM patients aged 14 years and older who had been on insulin for over 12 months. The study excluded patients with chronic liver or kidney disease, pregnant diabetics, and patients with malignancies. The study was approved by the Research and Human Ethics Committee of King Fahad Hospital, Madinah, Saudi Arabia. Informed consent was obtained from all the participants after explaining the aim and the nature of the study. The data were collected using a face-to-face interview questionnaire in Arabic. The data analysis was performed using Statistical Packages for Social Sciences SPSS version Continuous variables were expressed as the mean ± standard deviation SD or median [interquartile range IR ] as appropriate, and categorical variables were expressed as numbers percentages. An independent t -test was used to test for differences in the continuous variables, and a chi-square analysis was used to test for differences in the categorical variables. Of the patients included in the study, One hundred thirty patients The clinical characteristics of the participants are shown in Table 1. Hypoglycemia unawareness was not dependent on age, gender, duration of diabetes, duration of insulin therapy, HbA1c, frequency of blood glucose monitoring, or microvascular complications of diabetes. In addition, we did not find differences in HU between patients receiving insulin alone and those receiving both insulin and other hypoglycemic agents Table 2. When HU was evaluated with the modified Pedersen-Bjergaard method, the prevalence was In the current study, the prevalence of HU as assessed by the Clarke questionnaire score was This result is consistent with the results of many previous studies 11 — 13 but higher than reported in Jordan, where the prevalence of HU in patients with insulin-treated T2DM was When HU was evaluated by the modified Pedersen-Bjergaard method, a much higher prevalence of HU was observed The Pedersen-Bjergaard method tends to overestimate the prevalence of HU as documented previously by Geddes et al. A higher prevalence of HU was reported in T2DM patients from Turkey The factors reported to affect HU are not consistent among different studies, and some factors that were demonstrated to increase the risk for HU in some studies were not confirmed in others. However, long diabetes duration and strict blood sugar control are the most commonly reported factors that raise the risk of HU Nevertheless, in the present study, patients with HU had disease durations and HbA1c levels similar to those of aware subjects, findings that were also documented in other studies However, some studies found that patients with HU have higher HbA1c values Relaxing the glycemic target in patients with HU could explain the higher HbA1c values in those patients. Similarly, Murata et al. found that inadequate knowledge of diabetes is a risk factor for HU in type 2 diabetes Alanazi et al. also found that poor awareness of hypoglycemic attacks was observed among Another local study found that Diabetes education is a crucial key in diabetes management and should be a continuous process to improve blood glucose control, avoid hypoglycemia, and reduce diabetic complications. In the current study, we found that macrovascular complications of diabetes, specifically previous stroke and ischemic heart disease, are associated with increased risk for HU, whereas diabetic neuropathy and other microvascular complications of diabetes are not. Contrary to these results, Murata et al. found that stroke had no effect on hypoglycemia awareness, and intriguingly, the presence of microvascular complications of diabetes was associated with less risk for HU The findings from previous studies revealed that a significant number of patients with T1DM and T2DM were reluctant to discuss their hypoglycemia with their healthcare provider HCP. There could be many reasons for such a dangerous attitude, including implications for employment, fear of losing driving privileges, or concerns that it discloses poor glycemic control to the HCP 15 — In view of these findings along with the great risk of hypoglycemia associated with HU, regular screening for HU is a crucial element of diabetes care. For insulin-treated patients with HU, they are advised to raise their glycemic targets to strictly avoid hypoglycemia for at least several weeks in order to partially reverse hypoglycemia unawareness and reduce the risk of future episodes. However, we used two validated questionnaires commonly used in other studies for assessing HU 7 , 9. A further limitation of our study is that it was conducted only in one area of Saudi Arabia, so it may not be applicable to other Saudi populations. Despite these limitations, our findings provide valuable insights into HU in KSA. In addition, this study is among the few studies that investigated HU in Saudi Arabian insulin-treated diabetic patients. The study also provides valuable information on the association between HU and diabetes education. Further research is needed to confirm and extend our results. In addition, interventions to improve HU should also be explored. Despite the advances in insulin formulations and technologies used to control diabetes, HU continues to affect a significant proportion of patients with diabetes on insulin. Poor diabetes knowledge is a major risk factor for HU. Structured education for effective self-management of diabetes and screening for impaired awareness of hypoglycemia are of utmost importance to improve glycemic control and reduce the risk of hypoglycemia. The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. EA conceptualized the idea of the research, and wrote the manuscript. AS was responsible for the literature search and provided research materials. SB collected and organized the data and references and provided logistic support. AA was responsible for data collection. All authors contributed to the article and approved the submitted version. We would like to express our deep and sincere gratitude to the medical students who helped with the data collection. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Seaquist ER, Anderson J, Childs B, Cryer P, Dagogo-Jack S, Fish L, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care 36 5 — doi: PubMed Abstract CrossRef Full Text Google Scholar. Martín-Timón I, Del Cañizo-Gómez FJ. Mechanisms of hypoglycemia unawareness and implications in diabetic patients. World J Diabetes 6 7 — Al-Agha AE, Alafif M, Abd-Elhameed IA. Glycemic control, complications, and associated autoimmune diseases in children and adolescents with type 1 diabetes in Jeddah, Saudi Arabia. Saudi Med J 36 1 Hassounah G, Abdullah Aljohani AE, Al Sharhani R, Al Aljoulni M, Robert AA, Al Goudah AH, et al. Prevalence of impaired awareness of hypoglycemia and its risk factors among patients with type 1 diabetes in Saudi Arabia. Diabetes Metab Syndr 16 1 Bakatselos SO. Hypoglycemia unawareness. Diabetes Res Clin Pract 93 SUPPL. Ahmed B, Khan MN. Hypoglycemia: its effect on patients with diabetes. World Fam Med 17 9 — CrossRef Full Text Google Scholar. Gold AE, MacLeod KM, Frier BM. Frequency of severe hypoglycemia in patients with type I diabetes with impaired awareness of hypoglycemia. Diabetes Care 17 7 — Clarke WL, Cox DJ, Gonder-Frederick LA, Julian D, Schlundt D, Polonsky W. Reduced awareness of hypoglycemia in adults with IDDM. A prospective study of hypoglycemic frequency and associated symptoms. Diabetes Care 18 4 — Pedersen-Bjergaard U, Agerholm-Larsen B, Pramming S, Hougaard P, Thorsteinsson B. |
| Diabetic hypoglycemia | Joint health flexibility Causes Hypoglycemia Unawareness? Pamela J. toolbar Cholesterol level ranges search self-dare Search input auto suggest. Unawarsness pump therapy with Unqwareness insulin suspension in response to hypoglycemia: reduction in nocturnal hypoglycemia in those at greatest risk. I agree with terms below. Article CAS PubMed PubMed Central Google Scholar Johnston SS, Conner C, Aagren M, Ruiz K, Bouchard J. |
| Diabetic hypoglycemia - Diagnosis & treatment - Mayo Clinic | Glucagon, a hormone made by the alpha cells in the pancreas, rapidly raises blood sugar by triggering a release of glucose from glycogen stores in the liver. Injected glucagon is the fastest way to raise low blood sugar, but it requires that an injection be given by someone who has been trained to mix and inject it at the time it is needed. When someone with diabetes resists treatment, becomes unconscious, or has seizures due to hypoglycemia, glucagon can be injected by another person to rapidly raise the blood sugar. It is also handy for self-injection when someone with diabetes is ill or nauseated and cannot eat to correct low blood sugar. Glucagon kits are available by prescription and should be kept at home by everyone who uses insulin. The kit can be stored at room temperature or in the refrigerator and is stable for several years after purchase. Dating should be checked periodically to ensure potency. Instructions on how to prepare and inject glucagon should be provided to the person who has diabetes and to the person who is likely to be given the injection. A diabetes educator, trained nurse, or pharmacist can show how to inject glucagon. The typical dose in a glucagon kit is 1 milligram, which is sufficient to dose a lb. A full dose may cause nausea in a child or small adult and is often more than is needed for those who weigh less than lbs. If you are ever unable to handle a low blood sugar by yourself, lose consciousness, or suffer convulsions, notify your physician as soon as possible afterward. Events like this usually indicate that a major reduction in insulin doses is needed. Discuss the situation openly with your physician to prevent a reoccurrence. Adapted from Using Insulin © Walsh, Roberts, Varma, Bailey. Diabetes Response Service — the only scheduled proactive self-management Personal Call System using live operators to monitor, alert and prevent severe diabetic hypoglycemia. Type 1 Diabetes Type 1. Covid — A Special Threat with Diabetes Control Better Record Keeping Rules For Blood Glucose Control Carb Factor — The 2. How Many Carbs Do You Need Each Day? How To Count Carbohydrates Carb Factor — The 2. Energy of Diabetes Apple Cider Vinegar To The Rescue Technology Automated Insulin Delivery Control-IQ-Approval Enables Full iAIDs Device Connectivity Insulin Pumps Why Use A Pump? What About Us — MoToMove 24 Weather the Weather — MoToMove 25 Stepping Up to The New Year — MoToMove 26 MoTo Move in Action — MoToMove 27 A Virgin Isle Vacation A Great Instagrammer to follow. What Causes Hypoglycemia Unawareness? Hypoglycemia unawareness may be triggered by: A recent history of frequent low blood sugars A rapid drop in blood sugar Having diabetes for many years Stress or depression Situations where self-care is a low priority Alcohol consumption in the last 12 hours Previous low blood sugar in the last 24 to 48 hours Use of certain medications like beta-blockers. Tips For Reversing Hypoglycemia Unawareness Reduce the frequency of your lows Be especially careful to avoid another low for at least two days following a reaction Test blood sugars often to note dropping numbers and treat them before they become lows Set your target blood sugars slightly higher so that you will experience no more than one or two insulin reactions per week Always match your insulin doses to changes in your lifestyle. A recent history of frequent low blood sugars A rapid drop in blood sugar Having diabetes for many years Stress or depression Situations where self-care is a low priority Alcohol consumption in the last 12 hours Previous low blood sugar in the last 24 to 48 hours Use of certain medications like beta-blockers. An insulin pump, attached to the pocket, is a device that's worn outside of the body with a tube that connects the reservoir of insulin to a catheter inserted under the skin of the abdomen. Insulin pumps are programmed to deliver specific amounts of insulin continuously and with food. Some people don't have or don't recognize early symptoms of hypoglycemia hypoglycemia unawareness. If you have hypoglycemia unawareness, your health care provider may recommend a higher glucose target range. It's also very important to check your blood sugar consistently before going to bed and to have a snack containing carbohydrates before going to sleep if your blood sugar is lower than your bedtime target. Your health care provider may also recommend a continuous glucose monitor that can sound an alarm when your blood sugar is dropping. Inform people you trust, such as family, friends and co-workers, about hypoglycemia. If others know what symptoms to look for, they might be able to alert you to early symptoms. It's important that family members and close friends know where you keep glucagon and how to give it so that a potentially serious situation can be easier to safely manage. Always carry a low blood sugar treatment with you, such as glucose tablets, hard candy or gel. Also carry glucagon if it's prescribed for you. It's a good idea to wear a necklace or bracelet and have a wallet card that identifies you as someone who has diabetes. If you have low blood sugar levels several times a week, make an appointment with your health care provider. Together you can determine what's leading to your hypoglycemia and figure out what changes to make to prevent it. On this page. Self care. Preparing for your appointment. Hypoglycemic management Eat or drink carbohydrates Eat or drink something that's mostly sugar or carbohydrates to raise your blood sugar level quickly. Examples of foods that do raise your blood sugar level quickly include: Four glucose tablets available without a prescription at most pharmacies A serving of glucose gel read the label for amount Five to 6 pieces of hard candy or jelly beans check the food label for the exact serving Four ounces milliliters of fruit juice or regular — not diet — soda One tablespoon 15 milliliters of sugar, corn syrup or honey In general, food or drink with 15 to 20 grams of carbohydrates is often enough to raise your blood sugar levels back into a safe range. Recheck your blood sugar level Check your blood sugar level 15 minutes after eating or drinking something to treat your hypoglycemia. Have a snack or meal Have a snack or a meal to keep your blood sugar from dropping again. Emergency treatment Glucagon is a hormone that raises blood sugar quickly. Difficult-to-manage hypoglycemia Some people have frequent and severe hypoglycemia despite medication adjustments. Continuous glucose monitor and insulin pump. Hypoglycemia unawareness Some people don't have or don't recognize early symptoms of hypoglycemia hypoglycemia unawareness. Request an appointment. Teach people how to help Inform people you trust, such as family, friends and co-workers, about hypoglycemia. Plan ahead Always carry a low blood sugar treatment with you, such as glucose tablets, hard candy or gel. Wear a medical ID It's a good idea to wear a necklace or bracelet and have a wallet card that identifies you as someone who has diabetes. Here's some information to help you get ready for your appointment. What you can do Be aware of pre-appointment restrictions. Sometimes you need to not eat or drink anything but water for 8 to 12 hours fast for blood tests. When you make the appointment, ask if fasting is necessary. If it is, ask what changes you need to make to your diabetes management because you're not eating or drinking. Make a list of your symptoms and how often they occur. It helps to keep a record of your blood sugar readings and low blood sugar reactions so that you and your health care provider can see patterns leading to hypoglycemia. Make a list of key personal information, including major stresses or recent life changes. If you're monitoring your glucose values at home, bring a record of the glucose results, detailing the dates and times of testing. Make a list of medications, vitamins and supplements you take. Create a record of blood glucose meter values. Give your health care provider a written or printed record of your blood sugar levels, times and medication. Take your glucose meter with you. Some meters allow your provider's office to download the recorded glucose values. Write down questions to ask your health care provider. Ask your provider about any parts of your diabetes management plan where you need more information. Questions you may want to ask include: How often do I need to check my blood sugar? What is my target blood sugar range? How do diet, exercise and weight changes affect my blood sugar? For future research, we would recommend that outcome measures such as SH rates and HA scores should be reported in a standardized manner to allow future systematic reviews and meta-analyses. Because incidence and prevalence of SH rates are not normally distributed, the median IQR SH rate may be more appropriate than the mean SD commonly used. Measures of assessment of HA should also be standardized using Gold or Clarke scores because these have been shown to correlate well with clinical and clamp findings and each other. The proportion of patients with baseline IAH and then improved awareness should be reported as well as Gold or Clarke scores and their change. Future research may be needed to compare structured education, possibly using psychotherapeutic techniques, and optimized MDI using insulin analogs, with comparisons against new diabetes technologies such as LGS-enabled SAP. Psychotherapeutic techniques may provide additional benefit, in particular in improving HA status, and large RCTs using this approach should be conducted. Use of technology in diabetes, either better warning systems through CGM or through improved insulin delivery via CSII, can reduce SH rates and improve HA without worsening glycemic control, but without restoring counterregulatory hormone responses. A stepped approach is recommended in the management of people with IAH. The authors thank the authors of the original cited studies who were contacted for sharing the information required from their studies. received fellowship funding as part of the Health Manpower Development Plan award from Khoo Teck Puat Hospital, Alexandra Health Pte, Ltd. received PhD funding as part of a Diabetes UK project grant. None of the funding or supportive agencies were involved in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. The views expressed are those of the author s and not necessarily those of the funding agencies. Duality of Interest. has received travel support from Roche and Lilly UK. No other potential conflicts of interest relevant to this article were reported. Author Contributions. undertook the literature search and reviewed the abstracts and full articles. wrote the manuscript. performed and supervised the statistical analysis. conceived the idea for the review. All authors designed the study, contributed to the discussion, and critically reviewed the final manuscript. Prior Presentation. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 38, Issue 8. Previous Article Next Article. Research Design and Methods. Article Information. Article Navigation. Systematic Review July 14 Interventions That Restore Awareness of Hypoglycemia in Adults With Type 1 Diabetes: A Systematic Review and Meta-analysis Ester Yeoh ; Ester Yeoh. Corresponding author: Ester Yeoh, esteryeoh nhs. This Site. Google Scholar. Pratik Choudhary ; Pratik Choudhary. Munachiso Nwokolo ; Munachiso Nwokolo. Salma Ayis ; Salma Ayis. Stephanie A. Amiel Stephanie A. Diabetes Care ;38 8 — Article history Received:. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Figure 1. View large Download slide. Table 1 Summary of the 43 studies that were included in the final systematic review. First author, year ref. Intervention, brief description. N ; study duration. Age years ; diabetes duration years. SH rates. HA score. HbA 1c. Mean SH Gold score from 5. Clarke score from 5. No change in HbA 1c : baseline 7. Jordan, 4 Tayside insulin management course: Structured group education, 1 day of education per week for 4 consecutive weeks. Decrease in number of patients with HU Median HbA 1c reduction: 8. Hopkins, 21 DAFNE audit: Structured diabetes group education program, 5-day course in flexible insulin therapy. Improved HbA 1c : 8. Hernandez, 29 Self-awareness education on body cues associated with various levels of glycemia. Eight 3-h, biweekly sessions, follow-up study of Hernandez, Improved detection of symptom cues of euglycemia and hypoglycemia. Kubiak, 31 IG with hypoglycemia-specific education program 6 lessons, 45 min vs. Using modified Gold score: visual analog scale Improved HbA 1c in both groups; no difference between IG: 6. Broers, 22 Dutch adaptation of BGAT-III 6 weekly 1. individual setting. Psychoeducational intervention, follow-up study to Broers, Improved recognition of hypoglycemia in both groups No change in HbA 1c : 7. Hernandez, 30 Refer to Hernandez, No increase in ability to detect hypoglycemia but subjects could identify normal BG more accurately. No change in HbA 1c : 8. Broers, 23 Refer to Broers, Accuracy index of BG perception increased from 8. Improved autonomic and neuroglycopenic symptom scores during hypoglycemic clamp. No change in epinephrine and norepinephrine responses. Increased HbA 1c : 6. Cox, 24 BGAT-II psychoeducational group program, follow-up study of Cox, Booster intervention did not affect these benefits. No change in HbA 1c : Dagogo-Jack, 33 Avoidance of hypoglycemia, 3-year follow-up study of Dagogo-Jack, No report on SH. Improvement in neurogenic and neuroglycopenic symptoms score at 1 year postreversal from preintervention. Slight increase in HbA 1c : 7. Fritsche, 25 5-day inpatient diabetes education program DTTP , 25 min lessons on flexible insulin therapy, carbohydrate counting, correction and prevention of hypo- and hyperglycemia. those with no history of SH. Improved accuracy index of BG estimation in patients with SH but no improvement in the group without SH. Decreased HbA 1c : 8. Fanelli, 35 Avoidance of hypoglycemia for 6 months in patients with T1D 8 without diabetic autonomic neuropathy [DAN], 13 with DAN and 15 subjects without T1D. SH did not occur. Improved autonomic and neuroglycopenic symptoms in all groups. Responses remained lower than in subjects without T1D. Increased HbA 1c in all groups but remained within therapeutic target: 6. Liu, 36 Avoidance of hypoglycemia with less strict glycemic control and higher BG targets, SMBG 4 times daily with modification of insulin doses. Improved symptoms scores for sweating and lack of concentration. Improved GH and epinephrine responses but no changes in glucagon, norepinephrine, and cortisol. Cox, 26 BGAT-II, refer to Cox, No report of SH. Better accuracy in detecting BG fluctuations and low BG levels. Those with reduced HA had improved detection of low BG. Not available. Davis, 27 Conventional insulin therapy vs. intensive insulin therapy. intensive insulin therapy was 0. Reduction in total hypoglycemia symptom scores with intensive insulin therapy, with no reversal on reinstitution of conventional therapy. Lower plasma glucose to stimulate plasma epinephrine secretion during intensive therapy compared with initial conventional therapy without complete reversal on reinstitution of conventional therapy. HbA 1c in conventional group: 9. Dagogo-Jack, 34 Refer to Dagogo-Jack, Original group of 18 patients 6 HA, 6 HU, 6 healthy volunteers. Increase in total neurogenic and neuroglycopenic symptoms score responses to hypoglycemia. No significant increases in neuroendocrine responses epinephrine, pancreatic polypeptide, glucagon, GH, and cortisol after intervention. Increase in HbA 1c : 7. Improved symptoms scores after 3 weeks of no hypoglycemia. Improved glucose threshold for recognition of hypoglycemia in group A from glucose threshold of 2. Improved counterregulatory hormone adrenaline, noradrenaline, GH responses. No significant change in HbA 1c during intervention period; group A: 6. Fanelli, 38 Intensive insulin therapy physiologic insulin replacement and continuous education with avoidance of hypoglycemia. no decrease in frequency of hypoglycemia in CG. Baseline 9 patients had at least 1 SH during the year before study to no episodes of SH during study. Improvement in autonomic symptoms in IG, glucose threshold for autonomic symptoms at baseline from 2. No change in CG. Improved counterregulatory hormones adrenaline, cortisol, GH responses in IG maintained at 1-year follow-up, but not normalized to healthy volunteers. No changes in CG. Increased HbA 1c in IG but still within target 5. CG: HbA 1c showed no increase over 3 months. Fanelli, 37 Avoidance of hypoglycemia with adjustment of doses of insulin aiming for higher fasting, preprandial, and bedtime BG targets. Baseline 2 patients had at least 1 SH in the year preceding study to no SH during study. Improved neuroendocrine and symptom responses with no difference in autonomic glycemic thresholds compared with healthy volunteers. Epinephrine responses increased from baseline but still lower than in healthy volunteers. Increased HbA 1c : 5. DTTP CG. IG: 0. Improvement in HA modified Clarke score in both groups: CG: 1. IG: 1. Improved HbA 1c in PRIMAS group: 8. no change in CG: 8. Hermanns, 43 HyPOS IG vs. standard education CG , long-term follow-up study of Hermanns, ; CG: 0. Not reported. No difference in glycemic control: CG: 7. HyPOS: 7. Hermanns, 44 Refer to Hermanns, IG: 3. Improved detection of low BG and treatment of low BG. Increased intensity of hypoglycemia symptoms scores in HyPOS group. HbA 1c improved in CG 7. Schachinger, 45 Randomized to BGAT—III IG vs. physician-guided self-help control intervention CG. CG: 1. Improved recognition of low, high, and overall BG in BGAT vs. Detection of low BG improved in BGAT: No change in HbA 1c : 6. SMBG CG. No change in HbA 1c : HAATT group 8. Kinsley, 47 BGAT vs. cholesterol awareness CG in patients enrolled into an intensive diabetes treatment program. No data on SH. Increased neurogenic and neuroglycopenic symptom scores but did not differ between CG and BGAT groups before or after 4 months of intensive diabetes therapy. Increased epinephrine response in BGAT group to hypoglycemia. Improved HbA 1c in both groups: 9. Cox, 48 Long-term follow-up of BGAT patients with a proportion of patients receiving BGAT booster training. SH not reported. BGAT patients had better estimation of BG levels than control subjects. Improved HbA 1c over time: BGAT: Improved Clarke score, baseline 5. At baseline, 19 subjects were HU according to Clarke test, and at 24 months, 3 of 20 were HU. Leinung, 56 Retrospective study on CGM use on HbA 1c and SH rates. Improved HbA 1c : 7. Ryan, 54 CGM use in patients with SH. Hübinger, 53 Patients started on CSII with changes in HA. Improved HbA 1c in HU group: 8. CSII with or without RT-CGM in SH 2 × 2 factorial design. All patients received structured diabetes and hypoglycemia education, weekly telephone contact, and monthly clinic visits. Overall study population decreased Gold score: 5. CSII only in patients with HU. Mean SH in LGS: 1. Improvement in Clarke score in both groups: CSII: 6. No difference in epinephrine response to hypoglycemia between groups. HbA 1c was similar in both groups at baseline and did not change at end of study. CSII: 7. Leelarathna, 59 HypoCOMPaSS clamp study refer to Little, Decreased Gold scores: baseline 5. |

0 thoughts on “Hypoglycemic unawareness and self-care”