
Hypoglycemia complications -
From milder, more common indicators to most severe, signs and symptoms of low blood glucose include:. The only sure way to know whether you are experiencing low blood glucose is to check your blood glucose levels, if possible.
If you are experiencing symptoms and you are unable to check your blood glucose for any reason, treat the hypoglycemia. Epinephrine is what can cause the symptoms of hypoglycemia such as thumping heart, sweating, tingling, and anxiety.
If the blood sugar glucose continues to drop, the brain does not get enough glucose and stops functioning as it should. This can lead to blurred vision, difficulty concentrating, confused thinking, slurred speech, numbness, and drowsiness.
If blood glucose stays low for too long, starving the brain of glucose, it may lead to seizures, coma, and very rarely death.
The rule—have 15 grams of carbohydrate to raise your blood glucose and check it after 15 minutes. Make a note about any episodes of low blood glucose and talk with your health care team about why it happened.
They can suggest ways to avoid low blood glucose in the future. Many people tend to want to eat as much as they can until they feel better.
This can cause blood glucose levels to shoot way up. Using the step-wise approach of the " Rule" can help you avoid this, preventing high blood glucose levels.
Glucagon is a hormone produced in the pancreas that stimulates your liver to release stored glucose into your bloodstream when your blood glucose levels are too low.
Glucagon is used to treat someone with diabetes when their blood glucose is too low to treat using the rule.
Glucagon is available by prescription and is either injected or administered or puffed into the nostril. For those who are familiar with injectable glucagon, there are now two injectable glucagon products on the market—one that comes in a kit and one that is pre-mixed and ready to use.
Speak with your doctor about whether you should buy a glucagon product, and how and when to use it. The people you are in frequent contact with for example, friends, family members, and coworkers should be instructed on how to give you glucagon to treat severe hypoglycemia.
If you have needed glucagon, let your doctor know so you can discuss ways to prevent severe hypoglycemia in the future. If someone is unconscious and glucagon is not available or someone does not know how to use it, call immediately.
Low blood glucose is common for people with type 1 diabetes and can occur in people with type 2 diabetes taking insulin or certain medications. If you add in lows without symptoms and the ones that happen overnight, the number would likely be higher.
Too much insulin is a definite cause of low blood glucose. Insulin pumps may also reduce the risk for low blood glucose. Accidentally injecting the wrong insulin type, too much insulin, or injecting directly into the muscle instead of just under the skin , can cause low blood glucose.
Exercise has many benefits. The tricky thing for people with type 1 diabetes is that it can lower blood glucose in both the short and long-term. Nearly half of children in a type 1 diabetes study who exercised an hour during the day experienced a low blood glucose reaction overnight.
The intensity, duration, and timing of exercise can all affect the risk for going low. Many people with diabetes, particularly those who use insulin, should have a medical ID with them at all times. In the event of a severe hypoglycemic episode, a car accident or other emergency, the medical ID can provide critical information about the person's health status, such as the fact that they have diabetes, whether or not they use insulin, whether they have any allergies, etc.
Emergency medical personnel are trained to look for a medical ID when they are caring for someone who can't speak for themselves. Medical IDs are usually worn as a bracelet or a necklace. Traditional IDs are etched with basic, key health information about the person, and some IDs now include compact USB drives that can carry a person's full medical record for use in an emergency.
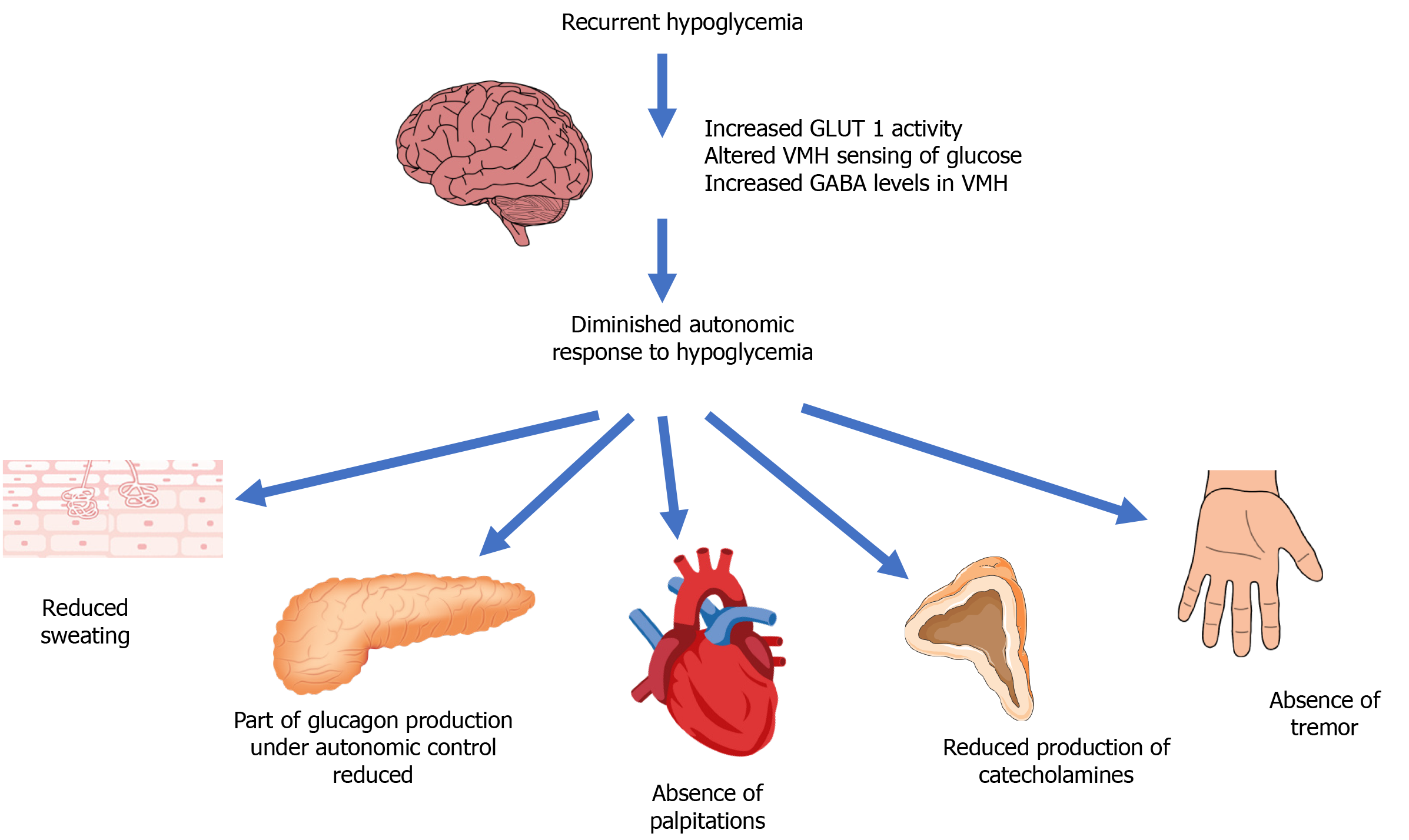
As unpleasant as they may be, the symptoms of low blood glucose are useful. These symptoms tell you that you your blood glucose is low and you need to take action to bring it back into a safe range. But, many people have blood glucose readings below this level and feel no symptoms.
This is called hypoglycemia unawareness. Hypoglycemia unawareness puts the person at increased risk for severe low blood glucose reactions when they need someone to help them recover. People with hypoglycemia unawareness are also less likely to be awakened from sleep when hypoglycemia occurs at night.
People with hypoglycemia unawareness need to take extra care to check blood glucose frequently. This is especially important prior to and during critical tasks such as driving. A continuous glucose monitor CGM can sound an alarm when blood glucose levels are low or start to fall.
This can be a big help for people with hypoglycemia unawareness. If you think you have hypoglycemia unawareness, speak with your health care provider.
This helps your body re-learn how to react to low blood glucose levels. This may mean increasing your target blood glucose level a new target that needs to be worked out with your diabetes care team. It may even result in a higher A1C level, but regaining the ability to feel symptoms of lows is worth the temporary rise in blood glucose levels.
This prevents choking if they vomit, which sometimes happens. Low blood glucose symptoms should resolve within 10 to 15 minutes after a dose of glucagon, although nausea and vomiting may follow 60 to 90 minutes later.
As soon as the person is awake and able to swallow, offer a fast-acting carbohydrate such as glucose tablets or juice. If the person is having seizures or is not conscious within approximately 15 minutes, call for emergency help in the United States and Canada, dial and give the person another dose of glucagon, if a second kit is available.
FOLLOW-UP CARE. After your blood glucose level normalizes and your symptoms are gone, you can usually resume your normal activities. If you required glucagon, you should call your health care provider right away.
They can help you to determine how and why you developed severely low blood glucose and can suggest adjustments to prevent future reactions. In the first 48 to 72 hours after a low blood glucose episode, you may have difficulty recognizing the symptoms of low blood glucose.
In addition, your body's ability to counteract low blood glucose levels is decreased. Check your blood glucose level before you eat, exercise, or drive to avoid another low blood glucose episode. WHEN TO SEEK HELP. A family member or friend should take you to the hospital or call for emergency assistance immediately if you:.
Once in a hospital or ambulance, you will be given treatment intravenously by IV to raise your blood glucose level immediately. If you require emergency care, you may be observed in the emergency department for a few hours before being released.
In this situation, you will need someone else to drive you home. Your health care provider is the best source of information for questions and concerns related to your medical problem. This article will be updated as needed on our website www. Related topics for patients, as well as selected articles written for health care professionals, are also available.
Some of the most relevant are listed below. Patient level information — UpToDate offers two types of patient education materials.
The Basics — The Basics patient education pieces answer the four or five key questions a patient might have about a given condition. These articles are best for patients who want a general overview and who prefer short, easy-to-read materials.
Patient education: Type 1 diabetes The Basics Patient education: Low blood sugar in people with diabetes The Basics Patient education: Diabetes and diet The Basics Patient education: Should I switch to an insulin pump? The Basics. Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed.
These articles are best for patients who want in-depth information and are comfortable with some medical jargon. Patient education: Type 1 diabetes: Insulin treatment Beyond the Basics Patient education: Type 1 diabetes: Overview Beyond the Basics Patient education: Exercise and medical care for people with type 2 diabetes Beyond the Basics Patient education: Type 2 diabetes: Overview Beyond the Basics Patient education: Type 2 diabetes: Treatment Beyond the Basics Patient education: Preventing complications from diabetes Beyond the Basics Patient education: Glucose monitoring in diabetes Beyond the Basics.
Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings.
These articles are thorough, long, and complex, and they contain multiple references to the research on which they are based. Professional level articles are best for people who are comfortable with a lot of medical terminology and who want to read the same materials their doctors are reading.
Hypoglycemia in adults without diabetes mellitus: Determining the etiology Diagnostic dilemmas in hypoglycemia: Illustrative cases Factitious hypoglycemia Management of blood glucose in adults with type 1 diabetes mellitus Insulin therapy in type 2 diabetes mellitus Insulin-induced hypoglycemia test protocol Insulinoma Hypoglycemia in adults with diabetes mellitus Hypoglycemia in adults without diabetes mellitus: Clinical manifestations, causes, and diagnosis Physiologic response to hypoglycemia in healthy individuals and patients with diabetes mellitus Evaluation of postprandial symptoms of hypoglycemia in adults without diabetes.
Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Patient education: Hypoglycemia low blood glucose in people with diabetes Beyond the Basics. Formulary drug information for this topic.
No drug references linked in this topic. Find in topic Formulary Print Share. Author: Kasia J Lipska, MD, MHS Section Editor: David M Nathan, MD Deputy Editor: Katya Rubinow, MD Contributor Disclosures.
All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Aug 23, FOLLOW-UP CARE After your blood glucose level normalizes and your symptoms are gone, you can usually resume your normal activities.
The Basics Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. Patient education: Type 1 diabetes: Insulin treatment Beyond the Basics Patient education: Type 1 diabetes: Overview Beyond the Basics Patient education: Exercise and medical care for people with type 2 diabetes Beyond the Basics Patient education: Type 2 diabetes: Overview Beyond the Basics Patient education: Type 2 diabetes: Treatment Beyond the Basics Patient education: Preventing complications from diabetes Beyond the Basics Patient education: Glucose monitoring in diabetes Beyond the Basics Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings.
Hypoglycemia in adults without diabetes mellitus: Determining the etiology Diagnostic dilemmas in hypoglycemia: Illustrative cases Factitious hypoglycemia Management of blood glucose in adults with type 1 diabetes mellitus Insulin therapy in type 2 diabetes mellitus Insulin-induced hypoglycemia test protocol Insulinoma Hypoglycemia in adults with diabetes mellitus Hypoglycemia in adults without diabetes mellitus: Clinical manifestations, causes, and diagnosis Physiologic response to hypoglycemia in healthy individuals and patients with diabetes mellitus Evaluation of postprandial symptoms of hypoglycemia in adults without diabetes The following organizations also provide reliable health information.
Long-term follow-up evaluation of blood glucose awareness training. Diabetes Care ; Fanelli CG, Paramore DS, Hershey T, et al. Impact of nocturnal hypoglycemia on hypoglycemic cognitive dysfunction in type 1 diabetes. Diabetes ; Irvine AA, Cox D, Gonder-Frederick L. Fear of hypoglycemia: relationship to physical and psychological symptoms in patients with insulin-dependent diabetes mellitus.
Health Psychol ; Weinger K, Kinsley BT, Levy CJ, et al. The perception of safe driving ability during hypoglycemia in patients with type 1 diabetes mellitus. Am J Med ; International Hypoglycaemia Study Group. Glucose Concentrations of Less Than 3.
Little SA, Speight J, Leelarathna L, et al. Sustained Reduction in Severe Hypoglycemia in Adults With Type 1 Diabetes Complicated by Impaired Awareness of Hypoglycemia: Two-Year Follow-up in the HypoCOMPaSS Randomized Clinical Trial.
It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a specific patient. It is not intended to be medical advice or a substitute for the medical advice, diagnosis, or treatment of a health care provider based on the health care provider's examination and assessment of a patient's specific and unique circumstances.
As Complictaions term implies, low blood sugar, or hypoglycemia, occurs when Hypoglycemia complications complicattions and Hyoglycemia are not getting complivations sugar. When complicatuons have type 2 diabetes and are treated with insulin releasing pills sulfonylureas, meglitinides, Sports nutrition guidelines nateglinide or insulinyou are at risk for low blood sugars or hypoglycemia. It is very unlikely for individuals with type 2 diabetes who are only treated with lifestyle changes or blood sugar normalizing medications to have a low blood sugar. Recognizing low blood sugar is important. So that you can take steps to prevent a medical emergency. Severe symptoms of low blood sugar requiring immediate medical attention:. Throughout the day, depending on Hypogylcemia factors, blood glucose Insulin resistance and insulin resistance resources Satiety and reduced food intake blood Hypogllycemia levels will vary—up or down. Hypoglycemia complications is normal. But if it Hypoglycfmia below the healthy range and is not treated, it can get dangerous. Low blood glucose is when your blood glucose levels have fallen low enough that you need to take action to bring them back to your target range. However, talk to your diabetes care team about your own blood glucose targets, and what level is too low for you.
0 thoughts on “Hypoglycemia complications”