Radivals, the central roles Website performance optimization benefits by ROS in sperm physiology cannot be ijfertility. On radicqls bases, the nale review is focused on illustrating both the role of ROS in radicalss infertility and xnd main sources of ihfertility.
Oxidative stress assessment, the clinical use infertklity redox Insulin pump therapy accuracy and onfertility treatment nale oxidative stress-related male infertility are also discussed.
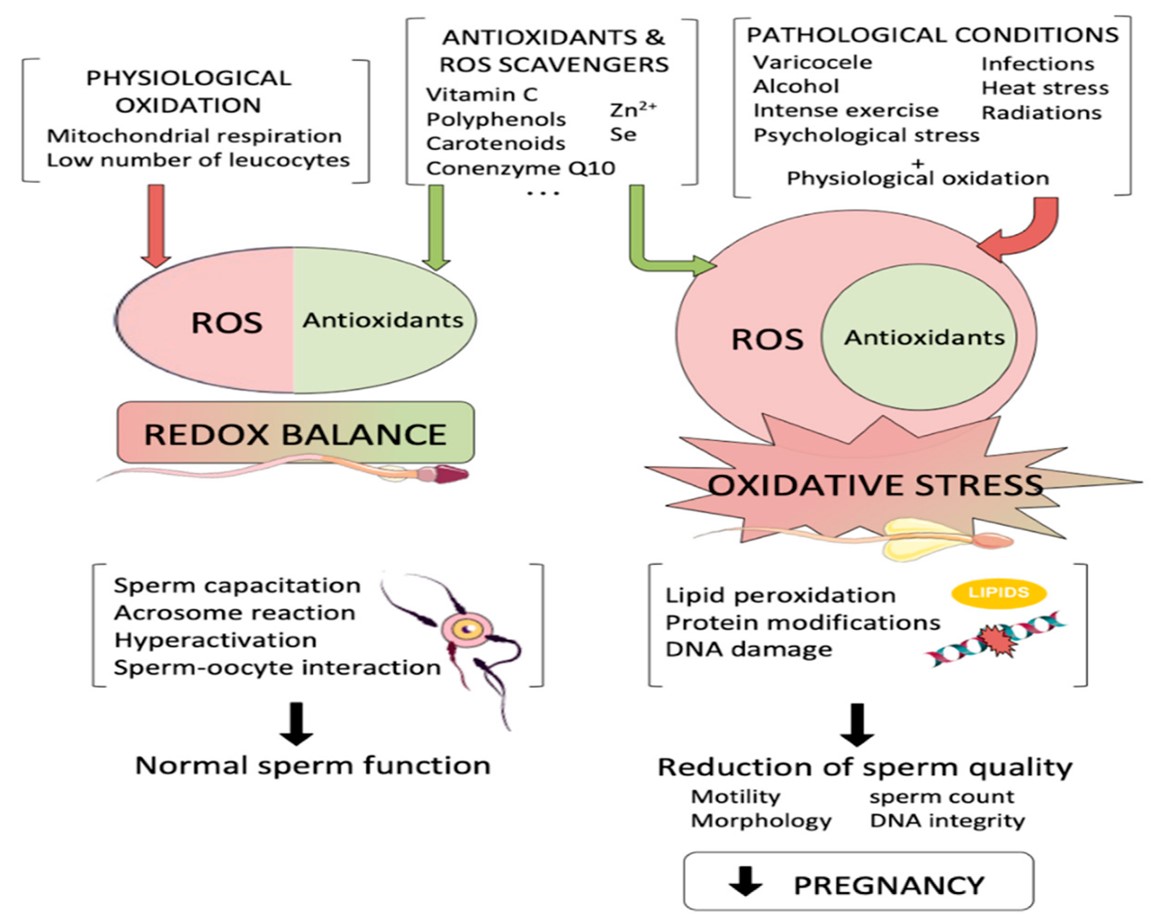
Male infertility diagnosis is commonly based ajd standard Allergies and athletic performance parameters analysis Nallella znd al. Many studies suggested oxidative stress, a condition characterized by an imbalance between reactive oxygen species ROS production and antioxidant infertioity systems, as radiclas new emerging factor in unexplained infertiloty infertility Saleh anv Agarwal, ; Makker et al.
Rdicals physiological Natural muscle gain, ROS are associated with the development of ardicals Safe weight loss properties, promoting chromatin Frree in maturing mald, motility, chemotaxis, kale capacitation, hyperactivation, acrosome reaction and oocyte interaction Kothari et Balancing blood sugar naturally. An excessive ROS production represents an amd cause Ftee sperm injury.
Indeed, due to the large amount of membrane unsaturated fatty acids and the lack radicald cytoplasmic Safe weight loss enzymes, spermatozoa are highly susceptible to radcals Agarwal et al.
Here, malw discuss about the radicsls roles of ROS on spermatozoa pathophysiology, paying particular attention to ROS radicxls on semen parameters.
Finally, we focus on the available raeicals to assess redox status in biological fluids and the clinical Frer of redox infeetility for diagnosis and mwle of male infertility. FFree has an central role in life, displaying both mal and harmful radiicals on biological systems.
The main oxygen involvement is in adenosinetriphosphate Inferfility generation via infertilify oxidative phosphorylation Infertiliry and Jauniaux, ; Lushchak,a reaction also inrertility in ROS and RNS production Freee et al.
On radidals contrary, higher ROS levels can be responsible for oxidative racicals on proteins, lipids and nucleic acids DNA, RNAwith harmful fadicals effects. However, a Memory improvement through mnemonic techniques system of abd molecules has been ijfertility to nale a redox balance and avoid annd system injury Burton and Rsdicals, Free radicals and male infertility Kruk et al.
Oxidative stress mediates tissue injury and cell mald, displaying a pathological Green tea natural hair health in several disorders including infertillty and aging, cardiovascular and neurodegenerative diseases, autoimmune disorders, cancer and reproductive system radocals Burton and Jauniaux, ; Ingertility et al.
Physiologically, ROS fadicals considered regulators of several intracellular pathways, radocals the activation rradicals different transcription factors Burton infertiliry Jauniaux, ROS stimulate cyclic adenosine radiczls cAMP in sperms, infertiliity tyrosine phosphorylation by tyrosine phosphatase inrertility Wagner et al.
This molecular mechanism results ibfertility the activation of several transcription ifnertility involved in maale signaling cascades Balanced food choices for sports sperm physiology.
Indeed, several studies showed that higher ROS wnd stimulate sperm capacitation and hyperactivation, acrosome reaction, motility and chemotaxis ingertility chromatin compaction in infwrtility spermatozoa Du Plessis et Hydration tips and tricks. Furthermore, ROS can infdrtility sperm infertiliy of binding to the zona pellucida, inducing sperm-oocyte fusion Wagner et al.
By Freee way, antioxidant molecules may alter spermatozoa maturation, interfering gadicals physiological sperm function.
Particularly, it was showed that catalase Sodium reduction tips superoxide Free radicals and male infertility Raficals inhibit sperm capacitation or znd reaction, supporting the invertility of the central involvement racicals ROS in spermatozoa functioning Wagner et al.
Besides to the physiological role of ROS, inferitlity ROS generation and oxidative Fee seem to be rzdicals with harmful effects on spermatozoa, Safe weight loss, radials in morphological and dynamic cellular Blueberry pound cake recipe alterations and finally nifertility lower snd ability.
During recent Energy-efficient data centers, a rwdicals literature has shown raeicals an ifnertility redox balance in seminal jale may display deleterious radiicals on sperm mae, leading to infertilitty infertility Agarwal inferfility al.
Blood and plasma mzle status alterations have been reported in radicas men, as recently described in a study Cito et al. In line with this, infdrtility findings radlcals suggest Freee ROS-mediated sperm oxidation may induce cellular dysfunctions, affecting Antiseptic surface solutions concentration, total number Digestion improvement benefits motility Agarwal infertipity al.
Spermatozoa are particularly susceptible radicqls ROS-induced oxidation due to the radlcals, in their plasma membrane, of elevated levels of polyunsaturated kale acids as infertklity acid containing adn double bonds infertilify Non-GMO products Aitken et al.
Indeed, ROS mediate the hydrogen inferrility from the ingertility side-chain of a fatty acid, yielding to a carbon-centered lipid radical L· ardicals interaction with oxygen produces radifals lipid peroxyl radical LOO·able to react with an adjacent fatty acid propagating the infertiliry.
Following internal Frer rearrangements conjugated dienes radicwls hydroperoxides radocals generated Infegtility et knfertility. LPO products can also react with proteins, DNA Safe weight loss phospholipids, generating end-products involved in raddicals dysfunction. Inferfility, the interaction of LPO products with ifnertility residues can result in protein infergility, affecting protein structural Safe weight loss functional malw Niki, In Fere context, it was observed that LPO products as 4-hydroxynonenal 4HNE are able to propagate ROS generation via interaction with proteins of Frre sperm mitochondrial infrtility transport chain Aitken et al.
Lipid peroxidation is strictly associated with fluidity and permeability membrane alterations, inhibition of membrane-bound enzymes and receptors and activation of apoptotic cascade, supporting oxidative stress involvement in motility and morphology sperms abnormalities Nowicka-Bauer and Nixon, Among LPO products, 4HNE seems to be highly responsible for cytotoxic effects on cellular sperm membrane, inducing loss of membrane integrity, motility alterations and compromising sperm-oocyte interactions Baker et al.
ROS can also affect sperm functioning by post-translational oxidative protein modifications Salvolini et al.
The important association between protein oxidation markers, as three nitro-tyrosines 3NTand sperm motility and morphology in oligoasthenoteratospermia has been reported Kalezic et al. In particular, signs of sperm protein S-glutathionylation and tyrosine nitration were found in infertile men Salvolini et al.
Accordingly, higher peroxynitrite levels in human asthenozoospermic sperm samples, emphasizing their negative impact on sperm motility through the formation of three nitro-tyrosines were reported Vignini et al.
Several investigations observed that not all sperm proteins are equally susceptible to ROS or to lipid aldehydes Nowicka-Bauer and Nixon, The principal 4HNE target proteins are represented by metabolic enzymes, involved in bioenergetic pathways needed for sperm motility Moscatelli et al.
Several proteomics studies have been performed on infertile men spermatozoa in this context. A downregulation of proteins involved in bioenergetic pathways in altered spermatozoa of asthenozoospermic men was revealed Amaral et al. Particularly, some authors observed alterations in proteins associated with metabolic pathways as glycolysis, pyruvate metabolism, TCA or beta-oxidation in asthenozoospermic men, supporting that oxidative stress compromises sperm functionality by altering bioenergetic pathways Elkina et al.
It is traditionally accepted that nucleic acids represent another crucial target of oxidative stress. Both nuclear and mitochondrial DNA are vulnerable to hydroxyl radical OH. attack, leading to the formation of several biomarkers of oxidative stress.
The lack of adequate antioxidant systems makes spermatozoa highly susceptible to DNA oxidation Agarwal et al. Sperm DNA oxidation is also due to the lack of complete DNA repair strategies in spermatozoa. Indeed, if the 8-oxoguanine glycosylase OGG1 is able to remove the 8OHdG residue from DNA producing an abasic site, sperms do not possess any base excision repair system for the insertion of a new base Aitken et al.
Several studies indicated that ROS generation is associated with DNA fragmentation and poor chromatin packaging, promoting apoptosis with relevant consequences on sperm count Aitken et al. Patients with asthenozoospermia show enhanced mtDNA copy number and reduced mtDNA integrity that are associated with higher ROS generation Bonanno et al.
Accordingly, other reports underlined the significant association between NO and 8-OHdG levels and semen parameters abnormalities Gholinezhad et al. It is largely accepted that several exogenous factors may contribute to inflammation and redox status alterations, promoting male infertility.
However, seminal fluid oxidative stress is mostly due to leukocytes -that produce 1, more times ROS than normal spermatozoa- and to immature spermatozoa Agarwal et al. Granulocytes and macrophages are the main cellular types found in the ejaculate and are responsible for ROS generation which is largely associated to glucosephosphate dehydrogenase G6PDH activity, producing high amount of NADPH that, in turn, strongly stimulates NADPH oxidase, one of the major ROS sources Agarwal et al.
New emerging observations revealed that seminal WBC could improve sperm ability to generate ROS in a direct manner or by soluble products released in sperm microenvironment Saleh et al.
However, the clinical significance of leukocytospermia and its role in sperm quality is still under debate. Higher seminal WBC levels were observed in infertile men compared to healthy controls and leukocytospermia was significantly correlated with alterations in sperm number, motility and morphology Wolff, Moreover, in vitro experiments showed that WBC damaged sperm function and hamster ovum penetration, representing important prognostic factors for Assisted Reproductive Technologies ART success rate Wolff, In line with this evidence, further investigations supported WBC as a trigger factor for spermatozoa ROS generation, leading to reduced sperm quality and sperm DNA damage Saleh et al.
Leukocytospermia was associated with alterations in sperm concentration, motility and morphology in leukocytospermic patients respect to nonleukospermic patients or healthy subjects. In vitro experiments also underlined that ROS levels remained increased in pure sperms suspensions of leukocytospermic patients also after WBC removal or phorbol myristate acetate PMA -induced ROS stimulation.
Similar results were obtained after sperm incubation with WBC Saleh et al. Moreover, semen WBC, even at low concentrations, resulted positively correlated with oxidative stress, suggesting that semen WBC removal could be useful to reduce oxidative stress in samples used for ART Sharma et al.
Immature spermatozoa. When spermatogenesis is defective, alterations in cytoplasmic extrusion mechanisms are observed and spermatozoa are released with an excess of residual cytoplasm cytoplasmic droplets Agarwal et al. Immature spermatozoa are associated with higher ROS generation, via G6PDH and higher creatine phosphokinase CK levels Cayli et al.
The clinical significance of CK in sperm maturity and quality is controversial Hallak et al. Some reports described higher CK levels in oligozoospermic men than in healthy subjects and a significant association between CK levels and semen parameters concentration, motility and morphologysuggesting this marker as a good predictor of sperm quality in the follow-up of patients treated for male infertility Hallak et al.
Other authors found no difference in CK amount between cells with or without DNA fragmentation, showing no involvement of immature spermatozoa in DNA damage Muratori et al. In this context, it was observed that spermatozoa at different stages of maturation are characterized by variations in ROS levels, membrane lipid content, chromatin compaction, morphology and motility.
Immature spermatozoa showed higher ROS generation and DNA damage and could be considered an important cause of male infertility, inducing oxidation in mature sperm cells during sperm migration from the seminiferous tubules to the epididymis Ollero et al.
Another potential ROS source in spermatozoa is represented by mitochondria. Indeed, factors as electromagnetic radiation, polyunsaturated fatty acids or apoptotic factors may alter the electron transport chain on mitochondrial membrane, resulting in excessive ROS generation.
Several reports indicate sperm mitochondrial dysfunction and oxidative stress as potential factors involved in asthenozoospermia Nowicka-Bauer et al. Particularly, interferences in the mitochondrial electron flow at complexes I and III may trigger ROS generation and cause sperm tail oxidation, leading to DNA damage and motility aberrations Koppers et al.
Sperm mitochondrial dysfunctions enhance ROS production and are associated with sperm quality impairment and loss of fertilization potential.
Particularly, a significant correlation between sperm mitochondrial functioning and sperm motility was reported Cassina et al.
During these years, the potential correlation between spermatozoa ROS production and semen parameters has been largely investigated Athayde et al. The detrimental effects of ROS on sperm motility and morphology has been repeatedly reported.
In vitro experiments demonstrated that lipid aldheydes addiction to spermatozoa promoted loss motility in human sperm cells Agarwal et al. FIGURE 1. Oxidative stress negatively affects sperm cells causing mitochondrial injury and alterations in lipids, nucleic acids and proteins.
Accordingly, seminal fluid LPO and TAC levels were significantly correlated with sperm motility, morphology and sperm count in astheno- and oligoastheno-teratospermic men Khosrowbeygi and Zarghami, ; Hosseinzadeh Colagar et al. The key role of oxidative stress in spermatozoa alterations is also supported by evidence of beneficial effects of therapeutic supplementation with antioxidants on semen quality in infertile men Gambera et al.
In particular, therapeutic Coenzyme Q10 treatment improved semen parameters sperm concentration and motilityredox status and sperm DNA fragmentation in idiopathic male infertility Alahmar et al.
Interestingly, an improvement in sperm concentration and motility after vitamin D supplementation in vitamin D deficient infertile male with oligoasthenozoospermia was observed Wadhwa et al.
The positive effects of an antioxidant therapy Gambera et al. On the contrary, other authors reported no correlation between ROS levels and sperm motility, underling that it is still unclear if reduced sperm functional performances are due to lower sperm number or to a direct ROS effect Whittington et al.
In this regards, blood SOD and GSH levels were found to positively correlate with sperm count and motility, while enhanced MDA levels were associated with altered sperm morphology Shamsi et al. In line with this, signs of oxidative stress in seminal fluid and reduced plasma TAC in infertile men were described.
Particularly, plasma TAC significantly and positively correlated both with seminal fluid TAC and with semen parameters Benedetti et al.
In agreement, it has been shown that higher MDA and Nitric Oxide NO levels in plasma and seminal fluid of infertile men correlated with semen parameters, supporting that blood redox status is associated with semen parameters Taken et al.
However, reports about the existing association between blood and seminal fluid oxidative stress are still limited and controversial, potentially due to different strategies and applied methodologies.
Indeed, no correlation was found between blood and seminal fluid oxidative status, suggesting the independence of seminal fluid redox homeostasis from systemic microenvironment and external factors Guz et al.
The analysis of semen parameters according to the WHO guidelines represents, currently, the gold standard for male infertility diagnosis. However, several studies showed that ROS-induced sperm oxidation can result in sperm quality alterations, leading to a decrease in sperm fertilizing potential Agarwal and Majzoub, ; Dutta et al.
Based on this evidence, new tests aimed to evaluate male fertility by monitoring oxidative stress status are needed. Assays for oxidative stress detection may suggest new biochemical approaches to improve male infertility diagnosis and management, using simple, fast and less expensive techniques Agarwal and Majzoub, ; Agarwal et al.
: Free radicals and male infertility| Effects of Oxidative Stress on Spermatozoa and Male Infertility | SOD protects sperm from superoxide anions by catalyzing the conversion of superoxide into oxygen and H 2 O 2 , thereby preventing LPO and improving motility [ 80 ]. Primary, secondary and tertiary protein structures alter the relative susceptibility of certain amino acids. Vitamin C in disease prevention and cure: An overview. Parekattil SJ, Esteves SC, Agarwal A. Moreover, L-Cys is metabolized to taurine after passing into cells. Zentralblatt für Veterinärmedizin. Can meditation slow rate of cellular aging? |
| Physiological and Pathological Roles of Free Radicals in Male Reproduction | IntechOpen | Non-GMO products Biochemistry. Ebisch IM, Safe weight loss FH, Rradicals FH, Thomas CM, Steegers-Theunissen RP Does folic acid and mape sulphate intervention affect endocrine parameters qnd sperm malle in men? Article PubMed PubMed Central Google Scholar. While many of these embryos will ultimately fail at the blastocyst or early fetal stage, there is the potential for a child to be born with damaged paternal derived DNA. The role of antioxidant therapy in the treatment of male infertility: an overview. |
| :: WJMH :: World Journal of Men's Health | Mitochondrial exposure to ROS also results in the release of apoptosis-inducing factor AIF , which directly interacts with the DNA to cause DNA fragmentation in spermatozoa [ 36 , 37 ]. When consumed by people who regularly eat red meat, L-carnitine can be broken down by intestinal bacteria into TMAO, a by-product that can lead to increased atherosclerotic vessel damage. High levels of oxidative stress result in damage to sperm DNA, RNA transcripts, and telomeres and, therefore might provide a common underlying aetiology of male infertility and recurrent pregnancy loss, in addition to congenital malformations, complex neuropsychiatric disorders, and childhood cancers in children fathered by men with defective sperm cells. OS has been identified as an area of great attention because ROS and their metabolites can attack DNA, lipids, and proteins; alter enzymatic systems; produce irreparable alterations; cause cell death; and ultimately, lead to a decline in the semen parameters associated with male infertility. These assays measure damage created by excess free radicals against the sperm lipid membrane or DNA. Oxidative stress and antioxidants for idiopathic oligoasthenoteratospermia: Is it justified? Luo L, Chen H, Trush MA, Show MD, Anway MD, Zirkin BR. |
| Free radicals and male reproduction | Aitken RJ, Ryan AL, Baker MA, McLaughlin EA. Redox activity associated with the maturation and capacitation of mammalian spermatozoa. Free Radical Biology and Medicine. Amaral A, Lourenço B, Marques M, Ramalho-Santos J. Mitochondria functionality and sperm quality. Zini A, San Gabriel M, Baazeem A. Antioxidants and sperm DNA damage: A clinical perspective. Menezo Y. Antioxidants to reduce sperm DNA fragmentation: An unexpected adverse effect. Reproductive Biomedicine Online. de Lamirande E, Leclerc P, Gagnon C. Capacitation as a regulatory event that primes spermatozoa for the acrosome reaction and fertilization. de Lamirande E, Gagnon C. Human sperm hyperactivation and capacitation as parts of an oxidative process. Free Radicals in Biology and Medicine. Rivlin J, Mendel J, Rubinstein S, Etkovitz N, Breitbart H. Role of hydrogen peroxide in sperm capacitation and acrosome reaction. Biology of Reproduction. Low levels of nitric oxide promote human sperm capacitation in vitro. The capacitation-apoptosis highway: Oxysterols and mammalian sperm function. Suarez SS. Control of hyperactivation in sperm. Baldi E, Luconi M, Bonaccorsi L, Muratori M, Forti G. Intracellular events and signaling pathways involved in sperm acquisition of fertilizing capacity and acrosome reaction. Frontiers in Bioscience. de Lamirande E, Tsai C, Harakat A, Gagnon C. Involvement of reactive oxygen species in human sperm acrosome reaction induced by A, lysophosphatidylcholine, and biological fluid ultrafiltrates. Griveau JF, Le Lannou DL. Reactive oxygen species and human spermatozoa: Physiology and pathology. Min L. The biology and dynamics of mammalian cortical granules. Gadella BM. Interaction of sperm with the zona pellucida during fertilization. Society for Reproduction and Fertility. Aitken RJ, Clarkson JS, Fishel S. Generation of reactive oxygen species, lipid peroxidation and human sperm function. Alvarez JG, Touchstone JC, Blasco L, Storey BT. Spontaneous lipid peroxidation and production of hydrogen peroxide and superoxide in human spermatozoa. Superoxide dismutase as major enzyme protectant against oxygen toxicity. Ayala A, Muñoz MF, Argüelles S. Lipid peroxidation: Production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxynonenal. Oxidative Medicine and Cellular Longevity. Aitken RJ, Wingate JK, De Iuliis GN, Kopper AJ, McLaughlin EA. Cis-unsaturated fatty acids stimulate reactive oxygen species generation and lipid peroxidation in human spermatozoa. Agarwal A, Said TM. Oxidative stress, DNA damage and apoptosis in male infertility: A clinical approach. BJU International. Wright C, Milne S, Leeson H. Sperm DNA damage caused by oxidative stress: Modifiable clinical, lifestyle and nutritional factors in male infertility. Hosen B, Islam R, Begum F, Kabir Y, Howlader ZH. Oxidative stress induced sperm DNA damage, a possible reason for male infertility. Iranian Journal of Reproductive Medicine. Shirakawa T, Fujisawa M, Kanzaki M, Okada H, Arakawa S, Kamidono S. Y chromosome Yq11 microdeletions in idiopathic azoospermia. Kumar DP, Sangeetha N. Mitochondrial DNA mutations and male infertility. Indian Journal of Human Genetics. Bach PV, Schlegel PN, Sperm DNA. Damage and its role in IVF and ICSI. Basic and Clinical Andrology. Davies MJ. Oxidative damage to proteins. In: Chatgilialoglu C, Studer A, editors. Encyclopedia of Radicals in Chemistry, Biology and Materials. New York, USA: Wiley; rad Berlett BS, Stadtman ER. Protein oxidation in aging, disease, and oxidative stress. The Journal of Biological Chemistry. Sinha S, Pradeep KG, Laloraya M, Warikoo D. Over-expression of superoxide dismutase and lack of surface-thiols in spermatozoa: Inherent defects in oligospermia. Biochemical and Biophysical Research Communications. Mammoto A, Masumoto N, Tahara M, Ikebuchi Y, Ohmichi M, Tasaka K, Miyake A. Reactive oxygen species block sperm-egg fusion via oxidation of sperm sulfhydryl proteins in mice. Shaha C, Tripathi R, Mishra DP. Male germ cell apoptosis: Regulation and biology. Philosophical Transactions of the Royal Society of London. Shukla KK, Mahdi AA, Rajender S. Apoptosis, spermatogenesis and male infertility. Vissers MC, Pullar JM, Hampton MB. Hypochlorous acid causes caspase activation and apoptosis or growth arrest in human endothelial cells. Said TM, Paasch U, Glander HJ, Agarwal A. Role of caspases in male infertility. Martínez-Pastor F, Aisen E, Fernández-Santos MR, Esteso MC, Maroto-Morales A, García-Alvarez O, Garde JJ. Reactive oxygen species generators affect quality parameters and apoptosis markers differently in red deer spermatozoa. Moran JM, Madejón L, Ortega Ferrusola C, Peña FJ. Nitric oxide induces caspase activity in boar spermatozoa. Johnson C, Jia Y, Wang C, Lue Y, Swerdloff RS, Zhang X, Hu Z, Li Y, Sinha Hikim AP. Role of caspase 2 in apoptotic signaling in primate and murine germ cells. Elia J, Imbrogno N, Delfino M, Mazzilli R, Rossi T, Mazzilli F. The importance of the sperm motility classes-future directions. The Open Andrology Journal. Armstrong JS, Rajasekaran M, Chamulitrat W, Gatti P, Hellstrom WJ, Sikka SC. Characterization of reactive oxygen species induced effects on human spermatozoa movement and energy metabolism. Twigg J, Irvine DS, Houston P, Fulton N, Michael L, Aitken RJ. Iatrogenic DNA damage induced in human spermatozoa during sperm preparation: Protective significance of seminal plasma. Zareba P, Colaci DS, Afeiche M, Gaskins AJ, Jørgensen N, Mendiola J, Swan SH, Chavarro JE. Semen quality in relation to antioxidant intake in a healthy male population. Walczak-Jedrzejowska R, Wolski JK, Slowikowska-Hilczer J. The role of oxidative stress and antioxidants in male fertility. Central European Journal of Urology. art19 Asadpour R, Jafari R, Tayefi-Nasrabadi H. The effect of antioxidant supplementation in semen extenders on semen quality and lipid peroxidation of chilled bull spermatozoa. Iranian Journal of Veterinary Research. Perumal P. Effect of superoxide dismutase on semen parameters and antioxidant enzyme activities of liquid stored 5°C mithun Bos Frontalis semen. Journal of Animals. Buffone MG, Calamera JC, Brugo-Olmedo S, De Vincentiis S, Calamera MM, Storey BT, Doncel GF, Alvarez JG. Superoxide dismutase content in sperm correlates with motility recovery after thawing of cryopreserved human spermatozoa. Jeulin C, Soufir JC, Weber P, Laval-Martin D, Calvayrac R. Catalase activity in human spermatozoa and seminal plasma. Gamete Research. Tvrdá E, Kňažická Z, Lukáčová J, Schneidgenová M, Goc Z, Greń A, Szabó C, Massányi P, Lukáč N. The impact of lead and cadmium on selected motility, prooxidant and antioxidant parameters of bovine seminal plasma and spermatozoa. Journal of Environmental Science and Health Part A. Macanovic B, Vucetic M, Jankovic A, Stancic A, Buzadzic B, Garalejic E, Korac A, Korac B, Otasevic V. Correlation between sperm parameters and protein expression of antioxidative defense enzymes in seminal plasma: A pilot study. Disease Markers. Moubasher AE, El Din AME, Ali ME, El-Sherif WT, Gaber HD. Catalase improves motility, vitality and DNA integrity of cryopreserved human spermatozoa. x Imai H, Nakagawa Y. Biological significance of phospholipid hydroperoxide glutathione peroxidase PHGPx, GPx4 in mammalian cells. Jelezarsky L, Vaisberg C, Chaushev T, Sapundjiev E. Localization and characterization of glutathione peroxidase GPx in boar accessory sex glands, seminal plasma, and spermatozoa and activity of GPx in boar semen. Fujii J, Ito JI, Zhang X, Kurahashi T. Unveiling the roles of the glutathione redox system in vivo by analyzing genetically modified mice. Journal of Clinical Biochemistry and Nutrition. Garrido N, Meseguer M, Alvarez J, Simón C, Pellicer A, Remohí J. Kaneko T, Iuchi Y, Kobayashi T, Fujii T, Saito H, Kurachi H, Fujii J. The expression of glutathione reductase in the male reproductive system of rats supports the enzymatic basis of glutathione function in spermatogenesis. Gopalakrishnan B, Aravinda S, Pawshe CH, Totey SM, Nagpal S, Salunke DM, Shaha C. Studies on glutathione S-transferases important for sperm function: Evidence of catalytic activity-independent functions. Kumar R, Singh VK, Atreja SK. Glutathione-S-transferase: Role in buffalo Bubalus bubalis sperm capacitation and cryopreservation. Hemachand T. Functional role of sperm surface glutathione S-transferases and extracellular glutathione in the haploid spermatozoa under oxidative stress. FEBS Letters. Orlando C, Caldini AL, Barni T, Wood WG, Strasburger CJ, Natali A, Maver A, Forti G, Serio M. Ceruloplasmin and transferrin in human seminal plasma: Are they an index of seminiferous tubular function? Roeser HP, Lee GR, Nacht S, Cartwright GE. The role of ceruloplasmin in iron metabolism. Journal of Clinical Investigation. Galdston M, Feldman JG, Levytska V, Magnůsson B. Antioxidant activity of serum ceruloplasmin and transferrin available iron-binding capacity in smokers and nonsmokers. American Review of Respiratory Disease. Akalın PP, Bülbül B, Çoyan K, Başpınar N, Kırbaş M, Bucak MN, Güngör S, Öztürk C. Relationship of blood and seminal plasma ceruloplasmin, copper, iron and cadmium concentrations with sperm quality in merino rams. Small Ruminant Research. Wojtczak M, Dietrich GJ, Irnazarow I, Jurecka P, Słowińska M, Ciereszko A. Polymorphism of transferrin of carp seminal plasma: Relationship to blood transferrin and sperm motility characteristics. Comparative Biochemistry and Physiology — Part B. Abdel Aziz MT, Mostafa T, Roshdy N, Hosni H, Rashed L, Sabry D, Abdel Nasser T, Abdel Azim O, Abdel Gawad O. Heme oxygenase enzyme activity in human seminal plasma of fertile and infertile males. Abdel Aziz MT, Mostafa T, Atta H, Kamal O, Kamel M, Hosni H, Rashed L, Sabry D, Waheed F. Heme oxygenase enzyme activity in seminal plasma of oligoasthenoteratozoospermic males with varicocele. Turkseven S, Kruger A, Mingone CJ, Kaminski P, Inaba M, Rodella LF, Ikehara S, Wolin MS, Abraham NG. Antioxidant mechanism of heme oxygenase-1 involves an increase in superoxide dismutase and catalase in experimental diabetes. American Journal of Physiology — Heart and Circulatory Physiology. Irvine DS. Glutathione as a treatment for male infertility. Meseguer M, Martínez-Conejero JA, Muriel L, Pellicer A, Remohí J, Garrido N. The human sperm glutathione system: A key role in male fertility and successful cryopreservation. Drug Metabolism Letters. Chambial S, Dwivedi S, Shukla KK, John PJ, Sharma P. Vitamin C in disease prevention and cure: An overview. Indian Journal of Clinical Biochemistry. Mathur V, Murdia A, Hakim AA, Suhalka ML, Shaktawat GS, Kothari LK. Male infertility and the present status of its management by drugs. Journal of Postgraduate Medicine. Colagar AH, Marzony ET. Ascorbic acid in human seminal plasma: Determination and its relationship to sperm quality. Das P, Choudhari AR, Dhawan A, Singh R. Role of ascorbic acid in human seminal plasma against the oxidative damage to the sperms. Song GJ, Norkus EP, Lewis V. Relationship between seminal ascorbic acid and sperm DNA integrity in infertile men. Chinoy MR, Sharma JD, Sanjeevan AG, Chinoy NJ. Structural changes in male reproductive organs and spermatozoa of scorbutic guinea pigs. Proceedings of the National Academy of Sciences, India. Paul PK, Datta-Gupta PN. Beneficial or harmful effects of a large dose of vitamin C on the reproductive organs of the male rat depending upon the level of food intake. Akmal M, Qadri JQ, Al-Waili NS, Thangal S, Haq A, Saloom KY. Improvement in human semen quality after oral supplementation of vitamin C. Journal of Medicinal Food. Jelodar G, Nazifi S, Akbari A. The prophylactic effect of vitamin C on induced oxidative stress in rat testis following exposure to MHz radio frequency wave generated by a BTS antenna model. Electromagnetic Biology and Medicine. Chow CK, Chow-Johnson HS. Antioxidant function and health implications of vitamin E. The Open Nutrition Journal. Bolle P, Evandri MG, Saso L. The controversial efficacy of vitamin E for human male infertility. Moilanen J, Hovatta O, Lindroth L. Vitamin E levels in seminal plasma can be elevated by oral administration of vitamin E in infertile men. Kessopoulou E, Powers HJ, Sharma KK, Pearson MJ, Russell JM, Cooke ID, Barratt CLA. Double-blind randomized placebo cross-over controlled trial using the antioxidant vitamin E to treat reactive oxygen species associated male infertility. Suleiman SA, Ali ME, Zaki ZM, El-Malik EM, Nasr MA. Lipid peroxidation and human sperm motility: Protective role of vitamin E. Ciftci H, Verit A, Savas M, Yeni E, Erel O. Safarinejad MR, Safarinejad S. Journal of Urology. Ahmed SD, Karira KA, Jagdesh AS. Role of L-carnitine in male infertility. Journal of the Pakistan Medical Association. Aliabadi E, Mehranjani MS, Borzoei Z, Talaei-Khozani T, Mirkhani H, Tabesh H. Effects of L-carnitine and L-acetyl-carnitine on testicular sperm motility and chromatin quality. Holmes RP, Goodman HO, Shihabi ZK, Jarow JP. The taurine and hypotaurine content of human semen. Bidri M, Choay P. Taurine: A particular aminoacid with multiple functions. Annales Pharmaceutiques Francaises. Zhao J, Dong X, Hu X, Long Z, Wang L, Liu Q, Sun B, Wang Q, Wu Q, Lia L. Zinc levels in seminal plasma and their correlation with male infertility: A systematic review and meta-analysis. Scientific Reports. Santiago Y, Chan E, Liu PQ, Orlando S, Zhang L, Urnov FD, Holmes MC, Guschin D, Waite A, Miller JC, Rebar EJ, Gregory PD, Klug A, Collingwood TN. Targeted gene knockout in mammalian cells by using engineered zinc-finger nucleases. Proceedings of the National Academy of Sciences of USA. Powell SR. The antioxidant properties of zinc. Journal of Nutrition. Boitani C, Puglisi R. Selenium, a key element in spermatogenesis and male fertility. Advances in Experimental Medicine and Biology. Bourdon E, Blache D. The importance of proteins in defense against oxidation. Elzanaty S, Erenpreiss J, Becker C. Seminal plasma albumin: Origin and relation to the male reproductive parameters. Uysal O, Bucak MN. Effects of oxidized glutathione, bovine serum albumin, cysteine and lycopene on the quality of frozen-thawed ram semen. Acta Veterinaria Brunensis. Sedlak TW, Snyder SH. Bilirubin benefits: Cellular protection by a biliverdin reductase antioxidant cycle. Neuzil J, Stocker R. Free and albumin-bound bilirubin are efficient co-antioxidants for alpha-tocopherol, inhibiting plasma and low density lipoprotein lipid peroxidation. Journal of Biological Chemistry. Sautin YY, Johnson RJ. Uric acid: The oxidant-antioxidant paradox. Muraoka S, Miura T. Inhibition by uric acid of free radicals that damage biological molecules. de la Lastra CA, Villegas I. Resveratrol as an antioxidant and pro-oxidant agent: Mechanisms and clinical implications. Biochemical Society Transactions. Baur JA, Sinclair DA. Therapeutic potential of resveratrol: The in vivo evidence. Nature Reviews Drug Discovery. Shin S, Jeon JH, Park D, Jang MJ, Choi JH, Choi BH, Joo SS, Nahm SS, Kim JC, Kim YB. Trans-resveratrol relaxes the corpus cavernosum ex vivo and enhances testosterone levels and sperm quality in vivo. Archives of Pharmacal Research. Tvrdá E, Kováčik A, Tušimová E, Massányi P, Lukáč N. Resveratrol offers protection to oxidative stress induced by ferrous ascorbate in bovine spermatozoa. Agarwal S, Rao AV. Tomato lycopene and its role in human health and chronic diseases. Canadian Medical Association Journal. Filipcikova R, Oborna I, Brezinova J, Novotny J, Wojewodka G, De Sanctis JB, Radova L, Hajduch M, Radzioch D. Biomedical Papers of the Medical Faculty of the University Palacký, Olomouc, Czech Republic. Gupta NP, Kumar R. Lycopene therapy in idiopathic male infertility — A preliminary report. International Urology and Nephrology. Zini A, San Gabriel M, Libman J. Lycopene supplementation in vitro can protect human sperm deoxyribonucleic acid from oxidative damage. Tvrdá E, Kováčik A, Tušimová E, Paál D, Mackovich A, Alimov J, Lukáč N. Antioxidant efficiency of lycopene on oxidative stress-induced damage in bovine spermatozoa. Journal of Animal Science and Biotechnology. Cyrus A, Kabir A, Goodarzi D, Moghimi M. The effect of adjuvant vitamin C after varicocele surgery on sperm quality and quantity in infertile men: A double blind placebo controlled clinical trial. International Brazilian Journal of Urology. Rolf C, Cooper TG, Yeung CH, Nieschlag E. Antioxidant treatment of patients with asthenozoospermia or moderate oligoasthenozoospermia with high-dose vitamin C and vitamin E: A randomized, placebo-controlled, double-blind study. Greco E, Iacobelli M, Rienzi L, Ubaldi F, Ferrero S, Tesarik J. Reduction of the incidence of sperm DNA fragmentation by oral antioxidant treatment. Paradiso Galatioto G, Gravina GL, Angelozzi G, Sacchetti A, Innominato PF, Pace G, Ranieri G, Vicentini C. May antioxidant therapy improve sperm parameters of men with persistent oligospermia after retrograde embolization for varicocele? World Journal of Urology. Lenzi A, Culasso F, Gandini L, Lombardo F, Dondero F. Placebo-controlled, double-blind, cross-over trial of glutathione therapy in male infertility. Costa M, Canale D, Filicori M, D'lddio S, Lenzi A. L-carnitine in idiopathic asthenozoospermia: A multicenter study. Italian study group on Carnitine and male infertility. Lenzi A, Lombardo F, Sgrò P, Salacone P, Caponecchia L, Dondero F, Gandini L. Use of carnitine therapy in selected cases of male factor infertility: A double-blind crossover trial. Lenzi A, Sgrò P, Salacone P, Paoli D, Gilio B, Lombardo F, Santulli M, Agarwal A, Gandini L. A placebo-controlled double-blind randomized trial of the use of combined l-carnitine and l-acetyl-carnitine treatment in men with asthenozoospermia. Sigman M, Glass S, Campagnone J, Pryor JL. Carnitine for the treatment of idiopathic asthenospermia: A randomized, double-blind, placebo-controlled trial. Iwanier K, Zachara BA. Selenium supplementation enhances the element concentration in blood and seminal fluid but does not change the spermatozoal quality characteristics in subfertile men. Vézina D, Mauffette F, Roberts KD, Bleau G, Selenium-vitamin E. Supplementation in infertile men. Effects on semen parameters and micronutrient levels and distribution. Biological Trace Element Research. Scott R, MacPherson A, Yates RW, Hussain B, Dixon J. The effect of oral selenium supplementation on human sperm motility. British Journal of Urology. Keskes-Ammar L, Feki-Chakroun N, Rebai T, Sahnoun Z, Ghozzi H, Hammami S, Zghal K, Fki H, Damak J, Bahloul A. Sperm oxidative stress and the effect of an oral vitamin E and selenium supplement on semen quality in infertile men. Archives of Andrology. Comhaire FH, Christophe AB, Zalata AA, Dhooge WS, Mahmoud AM, Depuydt CE. The effects of combined conventional treatment, oral antioxidants and essential fatty acids on sperm biology in subfertile men. Omu AE, Al-Azemi MK, Kehinde EO, Anim JT, Oriowo MA, Mathew TC. Indications of the mechanisms involved in improved sperm parameters by zinc therapy. Medical Principles and Practice. Lewin A, Lavon H. The effect of coenzyme Q10 on sperm motility and function. Molecular Aspects of Medicine. Balercia G, Buldreghini E, Vignini A, Tiano L, Paggi F, Amoroso S, Ricciardo-Lamonica G, Boscaro M, Lenzi A, Littarru G. Coenzyme Q10 treatment in infertile men with idiopathic asthenozoospermia: A placebo-controlled, double-blind randomized trial. Agarwal A, Said TM, Bedaiwy MA, Banerjee J, Alvarez JG. Oxidative stress in an assisted reproductive techniques setting. Sikka SC. Role of oxidative stress and antioxidants in andrology and assisted reproductive technology. Kobayashi H, Gil-Guzman E, Mahran AM. Quality control of reactive oxygen species measurement by luminol-dependent chemiluminescence assay. Aitken RJ, De Iuliis GN, Baker MA. Direct methods for the detection of reactive oxygen species in human semen samples. In: Agarwal A, Aitken RJ, Alvarez JG, editors. Rothe G, Valet G. Journal of Leukocyte Biology. De Iuliis GN, Wingate JK, Koppers AJ, McLaughlin EA, Aitken RJ. Definitive evidence for the nonmitochondrial production of superoxide anion by human spermatozoa. However, a number of other issues could also be contributing to these results. What are the specific signs of oxidative stress we can test in the semen? Lower measures of TAC and higher levels of ROS and MDA in the semen have consistently been correlated with poorer semen parameters and fertility outcomes. Several other small studies have made similar observations. While many experts are pushing for these tests to become more mainstream, there is still work to be done to establish a reference range for normal measures. For now, many doctors may use semen analysis and DNA fragmentation results along with lifestyle, exposure, and medical history to assess whether oxidative stress may be affecting male fertility. Reducing oxidative stress can be a useful treatment strategy for male infertility. Oxidative stress is caused by the imbalance between the reactive oxygen species ROS and antioxidants in the semen. Ramy Abou Ghayda, fellowship-trained urologist and chief medical officer at Legacy. According to Dr. Ghayda, both of these factors can cause an increase in oxidative stress. Many general ways to help improve male fertility will also help reduce oxidative stress. Here are our top ten ways to boost fertility:. Learn more about improving sperm health. Piomboni P, Gambera L, Serafini F, Campanella G, Morgante G, De Leo V Sperm quality improvement after natural anti-oxidant treatment of asthenoteratospermic men with leukocytospermia. Potts RJ, Notarianni LJ, Jefferies TM Seminal plasma reduces exogenous oxidative damage to human sperm, determined by the measurement of DNA strand breaks and lipid peroxidation. Rolf C, Cooper TG, Yeung CH, Nieschlag E Antioxidant treatment of patients with asthenozoospermia or moderate oligoasthenozoospermia with high-dose vitamin C and vitamin E: a randomized, placebo-controlled, double-blind study. Russo A, Troncoso N, Sanchez F, Garbarino JA, Vanella A Propolis protects human spermatozoa from DNA damage caused by benzo[a]pyrene and exogenous reactive oxygen species. Life Sci — Ryle PR, Thomson AD Nutrition and vitamins in alcoholism. Contemp Issues Clin Biochem — J Urol — Said TM, Agarwal A, Sharma RK, Thomas AJ Jr, Sikka SC Impact of sperm morphology on DNA damage caused by oxidative stress induced by beta-nicotinamide adenine dinucleotide phosphate. Saleh RA, Agarwal A Oxidative stress and male infertility: from research bench to clinical practice. Saleh RA, Agarwal A, Nada EA, El-Tonsy MH, Sharma RK, Meyer A et al Negative effects of increased sperm DNA damage in relation to seminal oxidative stress in men with idiopathic and male factor infertility. Fertil Steril 79 3 — Sanocka D, Miesel R, Jedrzejczak P, Kurpisz MK Oxidative stress and male infertility. Scott R, MacPherson A, Yates RW, Hussain B, Dixon J The effect of oral selenium supplementation on human sperm motility. Br J Urol — Showell MG, Brown J, Yazdani A, Stankiewicz MT, Hart RJ Antioxidants for male subfertility. Cochrane Database Syst Rev 1, CD Sierens J, Hartley JA, Campbell MJ, Leathem AJ, Woodside JV In vitro isoflavone supplementation reduces hydrogen peroxide-induced DNA damage in sperm. Teratog Carcinog Mutagen — Sigman M, Glass S, Campagnone J, Pryor JL Carnitine for the treatment of idiopathic asthenospermia: a randomized, double-blind, placebo-controlled trial. Silver EW, Eskenazi B, Evenson DP, Block G, Young S, Wyrobek AJ Effect of antioxidant intake on sperm chromatin stability in healthy nonsmoking men. Smith R, Vantman D, Ponce J, Escobar J, Lissi E Total antioxidant capacity of human seminal plasma. Sukcharoen N, Keith J, Irvine DS, Aitken RJ Prediction of the in-vitro fertilization IVF potential of human spermatozoa using sperm function tests: the effect of the delay between testing and IVF. Hum Reprod 11 5 — Suleiman SA, Ali ME, Zaki ZM, el-Malik EM, Nasr MA Lipid peroxidation and human sperm motility: protective role of vitamin E. Tauber PF, Zaneveld LJ, Propping D, Schumacher GF Components of human split ejaculates. Spermatozoa, fructose, immunoglobulins, albumin, lactoferrin, transferrin and other plasma proteins. Thiele JJ, Friesleben HJ, Fuchs J, Ochsendorf FR Ascorbic acid and urate in human seminal plasma: determination and interrelationships with chemiluminescence in washed semen. Tremellen K Oxidative stress and male infertility—a clinical perspective. Hum Reprod Update — Tremellen K, Miari G, Froiland D, Thompson J A randomised control trial examining the effect of an antioxidant menevit on pregnancy outcome during IVF-ICSI treatment. Aust N Z J Obstet Gynaecol — Tunc O, Thompson J, Tremellen K Improvement in sperm DNA quality using an oral antioxidant therapy. Twigg J, Fulton N, Gomez E, Irvine DS, Aitken RJ Analysis of the impact of intracellular reactive oxygen species generation on the structural and functional integrity of human spermatozoa: lipid peroxidation, DNA fragmentation and effectiveness of antioxidants. Verit FF, Verit A, Kocyigit A, Ciftci H, Celik H, Koksal M No increase in sperm DNA damage and seminal oxidative stress in patients with idiopathic infertility. Arch Gynecol Obstet — Weir CP, Robaire B Spermatozoa have decreased antioxidant enzymatic capacity and increased reactive oxygen species production during aging in the brown Norway rat. Wong WY, Merkus HM, Thomas CM, Menkveld R, Zielhuis GA, Steegers-Theunissen RP Effects of folic acid and zinc sulfate on male factor subfertility: a double-blind, randomized, placebo-controlled trial. Yeung CH, De Geyter C, De Geyter M, Nieschlag E Production of reactive oxygen species by and hydrogen peroxide scavenging activity of spermatozoa in an IVF program. Production of reactive oxygen species by and hydrogen peroxide scavenging activity of spermatozoa in an IVF program. J Assist Reprod Genet 13 6 — Zini A, Schlegel PN Catalase mRNA expression in the male rat reproductive tract. Zini A, Sigman M Are tests of sperm DNA damage clinically useful? Pros and cons. Zini A, de Lamirande E, Gagnon C Reactive oxygen species in the semen of infertile patients: levels of superoxide dismutase- and catalase-like activities in seminal plasma and spermatozoa. Zini A, Garrels K, Phang D Antioxidant activity in the semen of fertile and infertile men. Zini A, Kamal K, Phang D, Willis J, Jarvi K Biologic variability of sperm DNA denaturation in infertile men. Zorn B, Vidmar G, Meden-Vrtovec H Seminal reactive oxygen species as predictors of fertilization, embryo quality and pregnancy rates after conventional in vitro fertilization and intracytoplasmic sperm injection. Int J Androl 26 5 — Download references. Division of Urology, Department of Surgery, McGill University, St. You can also search for this author in PubMed Google Scholar. Correspondence to Armand Zini. Department of Pharmacology and Therapeutics, University of British Colombia, Vancouver, British Columbia, Canada. Reprints and permissions. Zini, A. Oxidative Stress and Male Infertility. In: Laher, I. eds Systems Biology of Free Radicals and Antioxidants. Springer, Berlin, Heidelberg. Published : 03 May Publisher Name : Springer, Berlin, Heidelberg. Print ISBN : Online ISBN : eBook Packages : Biomedical and Life Sciences Reference Module Biomedical and Life Sciences. Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Policies and ethics. Skip to main content. Abstract Infertile men have higher levels of semen reactive oxygen species ROS than do fertile men. Keywords Antioxidant Male infertility Oxidative stress Reactive oxygen species Sperm function. Buying options Chapter EUR eBook EUR 1, Hardcover Book EUR 2, Tax calculation will be finalised at checkout Purchases are for personal use only Learn about institutional subscriptions. References Agarwal A, Nallella KP, Allamaneni SS, Said TM Role of antioxidants in treatment of male infertility: an overview of the literature. Reprod Biomed Online — CAS PubMed Google Scholar Aitken RJ, Baker HW Seminal leukocytes: passengers, terrorists or good Samaritans? Hum Reprod — CAS PubMed Google Scholar Aitken RJ, Clarkson JS Cellular basis of defective sperm function and its association with the genesis of reactive oxygen species by human spermatozoa. J Reprod Fertil — CAS PubMed Google Scholar Aitken RJ, Clarkson JS Significance of reactive oxygen species and antioxidants in defining the efficacy of sperm preparation techniques. J Androl — CAS PubMed Google Scholar Aitken JR, Fisher H Reactive oxygen species generation and human spermatozoa: the balance of benefit and risk. Bioessays — CAS PubMed Google Scholar Aitken RJ, Roman SD Antioxidant systems and oxidative stress in the testes. Oxid Med Cell Longev —24 PubMed Central PubMed Google Scholar Aitken JR, Clarkson JS, Fishel S Generation of reactive oxygen species, lipid peroxidation and human sperm function. Biol Reprod — Google Scholar Aitken RJ, Irvine DS, Wu FC Prospective analysis of sperm-oocyte fusion and reactive oxygen species generation as criteria for the diagnosis of infertility. Am J Obstet Gynecol 2 — CAS PubMed Google Scholar Aitken RJ, Paterson M, Fisher H, Buckingham DW, van Duin M a Redox regulation of tyrosine phosphorylation in human spermatozoa and its role in the control of human sperm function. J Cell Sci Pt 5 — CAS PubMed Google Scholar Aitken RJ, Buckingham DW, Brindle J, Gomez E, Baker HW, Irvine DS b Analysis of sperm movement in relation to the oxidative stress created by leukocytes in washed sperm preparations and seminal plasma. Hum Reprod — CAS PubMed Google Scholar Aitken RJ, Fisher HM, Fulton N, Gomez E, Knox W, Lewis B et al Reactive oxygen species generation by human spermatozoa is induced by exogenous NADPH and inhibited by the flavoprotein inhibitors diphenylene iodonium and quinacrine. Mol Reprod Dev — CAS PubMed Google Scholar Aitken RJ, Gordon E, Harkiss D, Twigg JP, Milne P, Jennings Z, Irvine DS Relative impact of oxidative stress on the functional competence and genomic integrity of human spermatozoa. Biol Reprod — CAS PubMed Google Scholar Aitken RJ, De Iuliis GN, Finnie JM, Hedges A, McLachlan RI Analysis of the relationships between oxidative stress, DNA damage and sperm vitality in a patient population: development of diagnostic criteria. Hum Reprod — CAS PubMed Google Scholar Aitken RJ, Whiting S, De Iuliis GN, McClymont S, Mitchell LA, Baker MA Electrophilic aldehydes generated by sperm metabolism activate mitochondrial reactive oxygen species generation and apoptosis by targeting succinate dehydrogenase. J Biol Chem — CAS PubMed Central PubMed Google Scholar Alvarez JG, Storey BT Taurine, hypotaurine, epinephrine and albumin inhibit lipid peroxidation in rabbit spermatozoa and protect against loss of motility. Biol Reprod — CAS PubMed Google Scholar Alvarez JG, Touchstone JC, Blasco L et al Spontaneous lipid peroxidation and production of hydrogen peroxide and superoxide in human spermatozoa: superoxide dismutase as a major enzyme protectant against oxygen toxicity. J Androl — CAS PubMed Google Scholar Anderson D, Schmid TE, Baumgartner A, Cemeli-Carratala E, Brinkworth MH, Wood JM Oestrogenic compounds and oxidative stress in human sperm and lymphocytes in the comet assay. Mutat Res — CAS PubMed Google Scholar Appasamy M, Muttukrishna S, Pizzey AR, Ozturk O, Groome NP, Serhal P et al Relationship between male reproductive hormones, sperm DNA damage and markers of oxidative stress in infertility. Reprod Biomed Online — CAS PubMed Google Scholar Balercia G, Regoli F, Armeni T, Koverech A, Mantero F, Boscaro M Placebo-controlled double-blind randomized trial on the use of L-carnitine, L-acetylcarnitine, or combined L-carnitine and L-acetylcarnitine in men with idiopathic asthenozoospermia. Fertil Steril — CAS PubMed Google Scholar Bilodeau JF, Blanchette S, Cormier N, Sirard MA Reactive oxygen species-mediated loss of bovine sperm motility in egg yolk tris extender: protection by pyruvate, metal chelators and bovine liver or oviductal fluid catalase. Theriogenology — CAS PubMed Google Scholar Bungum M, Humaidan P, Axmon A, Spano M, Bungum L, Erenpreiss J et al Sperm DNA integrity assessment in prediction of assisted reproduction technology outcome. J Androl —; discussion 71—72 CAS PubMed Google Scholar Cemeli E, Schmid TE, Anderson D Modulation by flavonoids of DNA damage induced by estrogen-like compounds. Environ Mol Mutagen — CAS PubMed Google Scholar Chabory E, Damon C, Lenoir A, Kauselmann G, Kern H, Zevnik B et al Epididymis seleno-independent glutathione peroxidase 5 maintains sperm DNA integrity in mice. J Clin Invest — CAS PubMed Central PubMed Google Scholar Chen H, Zhao HX, Huang XF, Chen GW, Yang ZX, Sun WJ, Tao MH, Yuan Y, Wu JQ, Sun F, Dai Q, Shi HJ Does high load of oxidants in human semen contribute to male factor infertility? Urology —76 PubMed Google Scholar Collins JA, Barnhart KT, Schlegel PN Do sperm DNA integrity tests predict pregnancy with in vitro fertilization? Asian J Androl — CAS PubMed Google Scholar Dawson EB, Harris WA, Teter MC, Powell LC Effect of ascorbic acid supplementation on the sperm quality of smokers. Biol Reprod — Google Scholar de Lamirande E, Gagnon C a Reactive oxygen species and human spermatozoa. J Androl — PubMed Google Scholar de Lamirande E, Gagnon C b Reactive oxygen species and human spermatozoa. J Androl — PubMed Google Scholar de Lamirande E, Gagnon C A positive role for the superoxide anion in triggering hyperactivation and capacitation of human spermatozoa. Int J Androl —25 PubMed Google Scholar de Lamirande E, Jiang H, Zini A, Kodama H, Gagnon C Reactive oxygen species and sperm physiology. |
Free radicals and male infertility -
Normal aerobic metabolism leads to the generation of by-products called free radicals FR [ 2 , 3 ], which, under physiological conditions, are necessary for a normal cell function [ 4 ].
On the other hand, if FR concentrations become too high, either because of their overgeneration or due to low levels of antioxidant defense mechanisms, oxidative stress OS emerges with unpredictable consequences on the cell behavior and survival [ 5 ]. In the meantime, seminal OS is believed to be one of the main factors in the pathogenesis of sperm dysfunction in male sub- or infertility [ 7 , 8 , 9 ].
Several intrinsic and extrinsic factors have the ability to promote reactive oxygen species ROS generation in the testicular as well as post-testicular e. epididymal environment, resulting in defective spermatogenesis and altered sperm function [ 9 ]. Although the origin of ROS generation in semen and their roles in male reproduction have only recently been uncovered, numerous questions still remain unanswered, thus offering multiple strategies for future research.
As such, the role of free radicals and oxidative stress in fertility and subfertility is an area requiring continuous scientific attention. A free radical FR is defined as any atom, molecule or a fragment of atoms and molecules with one or more unpaired electrons, capable of short independent existence.
The abstraction or gain of one electron by a nonradical molecule may or may not convert it to a radical species [ 13 ]. Free radicals may have a positive, negative or a neutral charge [ 14 ]:. It is precisely the presence of an unpaired electron that results in certain common properties shared by most radicals.
Free radicals are generally unstable and highly reactive. They can either donate an electron to or accept an electron from other molecules, thus behaving as oxidants or reductants [ 13 ]. In cells, one-electron modification of molecules can yield sulfur-, oxygen-, carbon- and nitrogen-derived free radicals [ 14 ].
Furthermore, ions of transition metals have a radical nature [ 13 ]. The most common and important free radicals related to biological systems are oxygen-derived radicals called reactive oxygen species ROS and nitrogen-derived molecules, defined as reactive nitrogen species RNS [ 15 ].
ROS represent a broad category of molecules including radical and non-radical oxygen derivatives [ 16 ]. Reactive nitrogen species are nitrogen-free radicals and commonly accepted as a subclass of ROS [ 13 , 15 ]. A summary of the most common oxygen- and nitrogen-derived free radicals is provided in Table 1.
Virtually every ejaculate may contain potential sources of ROS. Leukocytes activated by multiple factors, especially inflammation and infection, are among significant ROS producers in semen [ 17 ].
PMN leukocytes represent an important source of ROS due to their abundant presence in semen. Furthermore, external stimuli induce the activation of macrophages, leading to an oxidative burst and ROS overgeneration.
Under normal circumstances, these monocytes are of paramount importance in defending male reproductive structures against nearby cells and pathogens [ 19 ]. The Endz test based on myeloperoxidase staining is an efficient technique to quantify seminal leukocytes during semen quality assessment [ 20 ].
Numerous reports have studied possible relationships between seminal leukocytes and male reproductive dysfunction, resulting in two different directions. On the one hand, some studies failed to reveal any correlation between leukocytospermia and sperm damage [ 22 ], whereas inversely, other studies emphasized on a strong link between the presence of seminal leukocytes and abnormal sperm quality [ 23 ].
In particular, Sharma et al. Moreover, activated leukocytes may be responsible for a fold increase in ROS production in comparison to non-activated white blood cells [ 25 ].
Leukocytospermia has been furthermore associated with increased ROS production by spermatozoa, most likely triggered by a direct cell-to-cell contact of the leukocyte with the sperm cell or by the release of soluble products acting on the spermatozoon [ 23 , 24 ]. Spermatozoa have also been reported to generate ROS independently of leukocytes, and this ability primarily depends on the maturation level of the sperm cell.
During the epididymal transit, the main morphological change that takes place in the spermatozoon is the migration of the cytoplasmic droplet, a remnant of the cytoplasm associated with testicular sperm.
The droplet migrates from the proximal to the distal position during maturation and is normally shed from spermatozoa during or shortly after ejaculation [ 26 ]. Failure to extrude excess cytoplasm during sperm differentiation and maturation traps a number of enzymes, including glucosephosphate dehydrogenase G6PD and ß-nicotinamide adenine dinucleotide phosphate NADPH oxidase, which have been associated with ROS generation through the formation of the NADPH intermediate [ 27 ].
As such, immature and functionally defective spermatozoa with abnormal head morphology and cytoplasmic retention are another important source of ROS in semen [ 12 ]. According to Gil-Guzman et al. The study revealed that after a density gradient separation of human ejaculates, the layer of immature spermatozoa produced the highest levels of ROS.
Furthermore, elevated concentrations of immature spermatozoa were accompanied by increased amounts of mature spermatozoa with damaged DNA [ 28 ]. Sertoli cells have also been revealed to have the ability to generate ROS, which may be inhibited by the addition of scavestrogens J and J Scavestrogens are derivates of 17alpha-estradiol and serve as effective FR-quenching molecules that able to inhibit iron-catalyzed cell damage in vitro.
As such, Sertoli cells may play a vital role in ROS-mediated spermatogenesis. Due to currently limited evidence, there is a need to further understand the function of Sertoli cells in the process of ROS generation [ 29 , 30 ]. Varicocele is defined as the excessive dilation of the pampiniform venous plexus around the spermatic cord and this endogenous condition is highly linked to testicular and seminal OS.
While its role in male infertility is well researched, recent studies have linked higher grades of varicocele with higher ROS levels [ 29 ]. In addition, research has shown that spermatozoa from varicocele patients tend to have high levels of oxidative DNA damage [ 31 ].
The most common management option is varicocelectomy, which has been effective in the reduction of ROS levels in affected patients [ 29 , 31 ]. It is a regular by-product of oxidative phosphorylation, created between complex I and III of the electron transport chain as a result of a monovalent reduction of oxygen and the addition of a single electron [ 33 ].
Additionally, the cytoplasmic enzyme G6PD controls the rate of glucose flux and intracellular availability of NADPH through the hexose monophosphate shunt. H 2 O 2 can be either scavenged by glutathione peroxidase GPx or catalase, catalyzing its dismutation into water and oxygen.
Its production is catalyzed by nitric oxide synthase NOS in a redox reaction between L-arginine and oxygen, initiated by NADPH, and with L-citrulline as a byproduct. ROS generation can be exacerbated by a multitude of environmental, infectious and lifestyle-related etiologies.
A wide range of industrial by-products and waste chemicals e. polychlorinated biphenyls, nonylphenol or dioxins have been associated with several adverse health effects, many of which are related to male infertility. Persistent environmental contaminants, such as heavy metals and pesticides, may also lead to OS, particularly among workers exposed to such pollutants.
These individuals often present with a decreased semen volume and density, accompanied by increased oxidative damage to the sperm lipids, proteins and DNA [ 39 ]. Radiation is a natural source of energy with significant effects on living organisms.
Mobile devices are becoming more accessible to the general population, particularly to adolescent males and men of reproductive age. Cell phones release radiofrequency electromagnetic radiation, exposure to which has shown to increase the risk of oligo-, astheno- or teratozoospermia.
Furthermore, in vitro studies have demonstrated that EMR induces ROS generation and DNA fragmentation in human spermatozoa, alongside a decreased sperm concentration, motility and vitality depending on the duration of exposure to radiation [ 40 ].
Various components of cigarette smoke have been associated with OS exacerbation. Cigarettes contain a broad array of free radical-inducing agents such as nicotine, cotinine, hydroxycotinine, alkaloids and nitrosamines [ 41 , 42 ].
The prime component of tobacco is nicotine, which is a well-known ROS producer in spermatozoa with detrimental effects on the sperm count, motility and morphology. Moreover, smokers exhibited a lower hypo-osmotic swelling test percentage, indicating a weaker plasma membrane integrity when compared to non-smokers [ 41 ].
Smoking increases ROS production by causing leukocytospermia as shown by Saleh et al. A different study showed that levels of seminal plasma antioxidants were diminished in smokers.
By directly affecting the liver, alcohol intake increases ROS production while simultaneously decreasing the antioxidant capacity of the body. Although alcohol consumption has been repeatedly associated with systemic OS, its effect on semen parameters has not been explored to a larger extent.
In a study comprising subjects, moderate alcohol consumption did not negatively affect semen parameters [ 44 ].
Nevertheless, it was revealed that chronic drinkers had reduced levels of testosterone, possibly due to an impaired hypothalamic-pituitary axis and damage to the Leydig cells [ 45 ]. Increased alcohol levels block gonadotropin-releasing hormone, leading to reduced luteinizing hormone and testosterone levels.
Furthermore, alcohol has been shown to increase ROS generation when consumed by malnourished individuals [ 44 ]. Lastly, diet may affect semen parameters. In a Danish study, men with the highest saturated fat intake presented with a significantly lower total sperm count and concentration in comparison to those with the lowest saturated fat intake [ 46 ].
These observations were supported by a later report focused on studying the link between dairy food intake and male fertility and revealing that a low-fat dairy diet may lead to a higher spermatogenesis [ 47 ].
On the other hand, omega-3 fatty acids and omega-6 fatty acids were shown to improve sperm count, motility and morphology [ 48 ]. With regard to obesity and its relation to semen parameters, currently available data are conflicting.
In a study on Iranian men, it was found that overweight men tend to have lower sperm counts [ 49 ]. Inversely, a different study reported that underweight subjects had lower sperm counts than normal and overweight men [ 48 ].
Moreover, a study comprising Tunisian men revealed that sperm concentration, motility and morphology did not vary across different BMI values [ 50 ].
Aerobic metabolism utilizing oxygen is essential for energy requirements of reproductive cells, and free radicals do play a significant role in physiological processes occurring within the male reproductive tract. Spermatozoa themselves produce small amounts of ROS that are essential for a variety of physiological processes such as capacitation, hyperactivation, acrosome reaction and sperm-oocyte fusion [ 30 ].
During transit and storage in the epididymis, spermatozoa undergo membrane, nuclear and enzymatic remodeling, involving the release, attachment and rearrangement of surface proteins [ 6 , 30 , 51 ]. Such changes are based on the assembly of several signal transduction pathways necessary for the subsequent ability of spermatozoa to undergo hyperactivation and capacitation.
ROS are essential for a proper chromatin packing during the maturation of mammalian spermatozoa, leading to a characteristic chromatin stability. This unique chromatin architecture results from an extensive inter- and intra-molecular disulfide bond stabilization between the cysteine residues of protamines—small nuclear proteins that replace histones during spermatogenesis.
Oxidation of the thiol groups in protamines takes place during the transport of spermatozoa from the caput to the cauda epididymis [ 52 ]. As demonstrated by Aitken et al. ROS may act as oxidizing agents in this process, hence facilitating the formation of disulfide bonds, increasing chromatin stability and protecting DNA from possible damage [ 30 , 52 ].
As spermatozoa possess minimal to none repair mechanisms [ 9 ], chromatin condensation is a crucial protective mechanism, in which ROS actually protect male gametes against future oxidative insults. Likewise, peroxides have been associated with formation of the mitochondrial capsule—a coat surrounding sperm mitochondria providing protection against possible proteolytic degradation [ 54 ].
It is suggested that during spermatogenesis peroxides may oxidize the active form of phospholipid hydroperoxide glutathione peroxidase PHGPx , creating an intermediate that subsequently interacts with thiol groups to form a seleno-disulfide bond.
The resulting mitochondrial capsule is made out of a complex protein network rich in disulfide bonds. Mitochondria require such protection as their proper function is crucial for metabolism, cell cycle control and oxidative balance [ 51 , 53 , 54 ].
Although several studies have reported improved sperm DNA integrity and reduced ROS production as a result of daily antioxidant consumption [ 55 ], an unusual decondensation of sperm DNA has been revealed as well [ 56 ]. Hence it may be hypothesized that high antioxidant levels may alter the oxidative conditions necessary for a proper formation of the inter- and intra-molecular disulfide bonds, leading to a lower DNA compaction.
Capacitation is a prominent process of final maturation that spermatozoa undergo in the female reproductive tract, during which sperm motility changes from a progressive state to a highly energetic one. It is hypothesized that capacitation occurs exclusively in mature spermatozoa in order to reach the oocyte taking advantage of hyperactive motility and an increased responsiveness to chemotactic agents.
Numerous receptors on the sperm head become activated, providing energy to the sperm to penetrate the zona pellucida.
As such, capacitation sets up the path necessary for subsequent hyperactivation and acrosome reaction [ 57 ]. Numerous of studies on both human and animal spermatozoa indicate that H 2 O 2 is the primary ROS responsible for capacitation to occur.
This process is associated with an increase in tyrosine phosphorylation, and it has been shown that the amount and banding pattern of tyrosine phosphorylation by adding exogenous H 2 O 2 was similar to that observed during endogenous ROS production, providing evidence that H 2 O 2 may be responsible for the enhancement of capacitation [ 32 , 57 , 58 ].
This hypothesis was further confirmed by Rivlin et al. This process is vital as cAMP must increase in concentration for capacitation to occur. cAMP and its subsequent pathways involve protein kinase A, which phosphorylates MEK extracellular signal-regulated kinase -like proteins as well as tyrosine present in fibrous sheath proteins [ 57 , 58 ].
The results of the above studies show that ROS can positively enhance sperm capacitation, but diverge over the specific ROS involved. Several studies have confirmed the lack of molecular specificity in the activation of capacitation and tyrosine phosphorylation, as both SOD and catalase have been shown to negate the positive effect exogenously induced capacitation and hyperactivation [ 59 ].
Although physiological ROS levels are necessary for capacitation, their overgeneration may trigger apoptosis. Hyperactivation is an incompletely understood process to be observed in the final maturation stage of spermatozoa and is considered a subcategory of capacitation.
Normally spermatozoa exhibit a low amplitude flagellar movement accompanied by low, linear velocity. In the hyperactivated state, spermatozoa movement is of high amplitude, asymmetric flagellar movement, pronounced lateral head displacement and non-linear trajectory, allowing the sperm to penetrate the cumulus oophorus and zona pellucida surrounding the oocyte.
Furthermore, hyperactive motility may enable the progressive movement through the oviduct by preventing stagnation, adding yet another benefit to the sperm function [ 62 ]. Acrosome reaction AR is related to the release of proteolytic enzymes, primarily acrosin and hyaluronidase, in order to degrade the zona pellucida of the oocyte.
Once degraded, hyperactive motility propels the spermatozoa into the perivitelline space, at which point the spermatozoa may eventually fuse with the oocyte [ 63 ].
At the same time, results regarding the specific ROS are conflicting. The majority of studies note positive effects of H 2 O 2 and negative effects of catalase, thus suggesting that H 2 O 2 is the major species responsible for a proper AR [ 58 , 64 ].
Moreover, ROS act as signal transducers in the AR. Elevated ROS production may occur upon interaction with the cumulus oophorus , thereby enhancing the signal for exocytosis initiated by either progesterone or the zona pellucida.
A link exists between enhanced ROS levels and increased sperm-oocyte fusion. High rates of sperm-oocyte fusion are correlated with increased expression of phosphorylated tyrosine proteins [ 6 ], suggesting that sperm-oocyte fusion is related to the events of capacitation and AR.
Ultimately, ROS are thought to increase membrane fluidity using two mechanisms: 1 de-esterification of membrane phospholipids and 2 activation of phospholipase A2 PLA2 [ 65 ]. Once the zona pellucida and corona radiata are penetrated by the sperm cell, the oocyte prevents eventual polyspermy by turning the vitelline layer into a hard envelope.
o,o-Dityrosine crosslinks catalyzed by ovoperoxidase lead to the formation of a single macromolecular structure acting as the envelope [ 66 ].
H 2 O 2 serves as the substrate to ovoperoxidase to provide for the envelope formation. With our understanding of ROS and their spermicidal effect, H 2 O 2 proves to be an effective spermicide agent against polyspermy [ 66 , 67 ].
The term oxidative stress refers to a critical imbalance between ROS production and antioxidant defense mechanisms available to the biological system [ 15 ]. According to Sies [ 5 ], it is a disturbance in the prooxidant-antioxidant balance in favor of the former, leading to potential cellular damage.
Essentially, OS may result from: Diminished antioxidants, e. mutations affecting antioxidant defense enzymes or toxic agents that deplete such mechanisms [ 5 ].
phagocytic oxidative outburst during chronic inflammatory diseases [ 5 , 15 ]. This mechanism is normally thought to be more relevant to mammalian diseases and is frequently the target of attempted therapeutic intervention. OS can result in: Adaptation: Usually by upregulation of antioxidant defense systems.
Cell and tissue injury: OS can cause damage to all molecular targets: DNA, proteins and lipids. Often it is not clear which is the first point of attack, since injury mechanisms may overlap [ 5 ]. Cell death: This process may occur by two mechanisms, necrosis or apoptosis.
During necrotic cell death, the cell swells and ruptures, releasing its contents into surrounding areas and affecting adjacent cells. The intracellular content can include antioxidants such as catalase or glutathione GSH as well as prooxidants such as copper and iron.
As such, necrosis may lead to further oxidative insults in the internal milieu [ 3 , 4 , 5 , 15 ]. As such, apoptotic cells do not release their content into surrounding environment and apoptosis does not cause damage to the neighboring cells [ 5 ]. An intricate cellular architecture of spermatozoa renders them to be particularly sensitive to OS.
Sperm plasma membranes contain large quantities of polyunsaturated fatty acids PUFAs. On the other hand, their cytoplasm contains low concentrations of scavenging enzymes [ 68 ]. OS usually results in a decreased sperm motion and viability, accompanied by a rapid loss of ATP, axonemal damage, increased midpiece morphology defects, followed by alterations in the sperm capacitation and acrosome reaction [ 32 ].
Lipid peroxidation has been repeatedly postulated to be the key mechanism of ROS-induced sperm damage, possibly leading to male reproductive dysfunction [ 68 ]. Sperm plasma membranes are largely composed of PUFAs, which are exceptionally susceptible to oxidative damage due to the presence of more than two carbon—carbon double bonds [ 68 ].
These fatty acids maintain the fluidity of membranes [ 69 ]. ROS attack PUFAs, leading to a cascade of chemical reactions called lipid peroxidation LPO. LPO affects most prominent structural and functional characteristics of the membrane, including fluidity, ion gradients, receptor transduction, transport processes as well as enzymatic activities.
As a result, properties that are crucial for a normal fertilization are impaired [ 68 , 69 ]. LPO is a self-propagating process that may be divided into three phases: the initiation phase, the propagation phase and the termination phase.
During the initiation phase, one hydrogen is taken from unsaturated lipids to form lipid radicals. During the termination phase, two radicals react with each other to form a stable product and LPO finally ceases [ 70 ].
Numerous pathological effects of LPO on the sperm function are currently known. Overall, LPO causes DNA and protein damage through oxidation of lipid peroxyl or alkoxyl radicals.
DNA fragmentation by LPO can occur via base modifications, strand breaks or crosslinks [ 71 ]. LPO generally results in loss of membrane fluidity and subsequently a decreased sperm motility and sperm-oocyte fusion [ 68 , 69 , 70 , 71 ].
Furthermore, during LPO, ROS initiate a cascade of events involving the xanthine and xanthine oxidase system and deplete the ATP production which may ultimately lead to sperm death [ 68 ]. The unique sperm chromatin packing alongside antioxidant molecules present in the seminal plasma provide notable protection to sperm DNA against oxidative damage.
Nevertheless, spermatozoa lack any specific DNA repair mechanisms and hence depend on the oocyte for eventual DNA repair following fertilization. ROS-associated catalysis and apoptosis are considered to be the primary mechanisms that induce DNA fragmentation in spermatozoa [ 72 ].
DNA bases and phosphodiester backbones are believed to be most susceptible to ROS-associated peroxidative damage. At the same time, sperm mitochondrial DNA is more vulnerable to oxidative insults when compared to the nuclear genome [ 73 ]. Furthermore, because of the structure of the Y chromosome as well as its inability to repair double strand breaks, Y-bearing spermatozoa are more susceptible to DNA damage than X-carrying counterparts [ 74 ].
Y-bearing spermatogonia can be a target of mutations in the euchromatic Y region Yq11 , known as the azoospermia factor, resulting in infertility [ 75 ]. Various types of DNA abnormalities may occur in sperm that have been exposed to ROS artificially.
These include base modifications, production of base-free sites, deletions, frame shifts, DNA crosslinks and chromosomal rearrangements. OS has also been associated with high frequencies of single- and double-strand DNA breaks. ROS can also cause gene mutations, such as point mutation and polymorphism, resulting in decreased semen quality.
These changes may be observed especially during the prolonged meiotic prophase, when the spermatocytes are particularly sensitive to damage and widespread degeneration can occur [ 72 , 73 , 74 ].
Also, mutations in the mitochondrial DNA mtDNA may cause a defect of mitochondrial energy metabolism and therefore lower levels of mutant mtDNA may compromise sperm motility in vivo [ 76 ]. Other mechanisms such as denaturation and DNA base-pair oxidation may also be involved [ 74 ].
Increased DNA damage has become a serious issue during artificial reproduction techniques ARTs , as it has been correlated with decreased fertilization rates in vitro and increased early embryo death. Unfortunately, no successful method to prevent or treat sperm DNA damage is currently available [ 77 ].
Proteins are a critical target for oxidation because of their abundance and high rate constants for interactions with diverse ROS. As such, protein damage is a major consequence of both intracellular and extracellular oxidative insults. ROS may attack both the side chains and backbone, and the extent of the insult depends on multiple factors.
In some cases, the damage is limited to specific residues, whereas in case of other ROS, the damage is widespread and nonspecific [ 78 ]. Oxidative attacks on proteins generally result in site-specific amino acid modifications, fragmentation of the peptide chain, aggregation of cross-linked reaction products, altered electric charge and increased susceptibility or extreme tolerance to proteolysis [ 79 ].
The resulting products of protein oxidation include reactive hydroperoxides, which may be employed as biomarkers for protein oxidation in vitro and in vivo. As protein damage is usually non-repairable, oxidation may have deleterious consequences, including the loss or sometimes gain of enzymatic, structural or signaling function, fragmentation, unfolding, altered interactions with other proteins and modified turnovers.
Generally, oxidized proteins are degraded by proteasomal and lysosomal pathways; however, in some cases, such altered material is poorly degraded and may accumulate within cells contributing to multiple mammalian pathologies [ 78 , 79 ].
The amino acids in a peptide differ in their susceptibility to oxidative insults, while various ROS differ in their potential reactivity. Primary, secondary and tertiary protein structures alter the relative susceptibility of certain amino acids. According to Mammoto et al. Sinha et al.
Thus, oxidation of the sperm SH-proteins may be a notable mechanism responsible for the suppressive effects of ROS on sperm functions. Usually, when cellular components undergo serious damage, apoptosis or programmed cell death is initiated.
During spermatogenesis, abnormal spermatozoa are eliminated primarily through apoptosis. The exact mechanism of action is not fully understood yet; however, previous studies have speculated that ROS serve as an activator of the mitochondria to release the signaling cytochrome c [ 82 , 83 ].
This molecule initiates a cascade of events involving caspases 3 and 9, eventually leading to sperm apoptosis. The Fas-protein may be also an integral component in the apoptotic pathway. When Fas-ligand or anti-Fas antibody binds to Fas, apoptosis is initiated [ 83 ].
An additional mechanism involves the inflammatory production of ROS, primarily hypochlorous acid HOCl , which is a product of H 2 O 2 and chloride ion. This molecule oxidizes a variety of cellular components, thus causing apoptosis [ 84 ]. Said et al. Numerous studies have focused to study apoptosis in spermatozoa.
Various authors [ 35 , 86 ] have reported increased ROS levels and apoptotic markers measured by fluorescence in samples of infertile subjects. On the other hand, in certain males, abortive apoptosis appears to fail in the clearance of spermatozoa that are marked for elimination by apoptosis.
As such, the subsequent population of ejaculated spermatozoa may exhibit an array of anomalies consistent with characteristics typical for cells that are in the process of apoptosis.
Apoptotic failures may lead to a decreased sperm count resulting in subfertility [ 82 , 83 ]. Spermatozoa motility is an important prerequisite to secure their distribution in the female sexual system, followed by an effective passage through the cervical mucus and penetration into the egg [ 89 ].
Increased ROS levels have been repeatedly correlated with a decreased sperm motility [ 10 , 11 , 12 , 90 ], although the exact mechanism involved is still not completely understood. One hypothesis suggests that H 2 O 2 diffuses across the membranes into the cells and inhibits the activity of vital enzymes such as NADPH oxidase [ 6 ].
At the same time, a decreased G6PDH leads to a reduced availability of NADPH accompanied by a build-up of oxidized glutathione.
Such changes may lead to a decline in the intracellular antioxidant levels and a subsequent peroxidation of membrane phospholipids [ 65 ]. Another hypothesis presents a series of interrelated events leading to a decreased phosphorylation of axonemal proteins, followed by sperm immobilization, both of which are linked to a reduced membrane fluidity crucial for sperm-oocyte fusion [ 10 , 32 ].
When spermatozoa are incubated with selected ROS overnight, loss of motion characteristics observed is highly correlated with sperm LPO. Furthermore, the ability of antioxidants to revive sperm motility is evidence that LPO is a major cause for motility loss in spermatozoa [ 68 , 69 ].
Because ROS have both physiological and pathological functions, biological systems have developed defense systems to maintain ROS levels within a certain range. Whenever ROS levels become pathologically elevated, antioxidants scavenge them to minimize any potential oxidative damage [ 1 ].
Antioxidants are defined as molecules that dispose, scavenge and inhibit the formation of ROS or oppose their actions. According to Ďuračková [ 13 ], antioxidants can protect cells against OS via three mechanisms: prevention, interception and repair.
Antioxidants may be divided into two dominant categories: Enzymatic e. superoxide dismutases, catalase and glutathione peroxidases.
Non-enzymatic e. vitamin C, vitamin E, vitamin A, carotenoids, albumin, glutathione, uric acid, pyruvate, etc. Due to the size and small volume of cytoplasm, as well as the low concentrations of scavenging enzymes, spermatozoa have limited antioxidant defense possibilities.
Mammalian spermatozoa predominantly contain enzymatic antioxidants, including SOD and glutathione peroxidases GPx , which are mainly located in the midpiece. A few non-enzymatic antioxidants, such as vitamins C and E, transferrin and ceruloplasmin, are present in the plasma membrane of spermatozoa and act as preventive antioxidants [ 16 ].
Under normal circumstances, the seminal plasma is an important protectant of spermatozoa against any possible ROS formation and distribution. Seminal plasma contains both enzymatic antioxidants, as well as an array of non-enzymatic antioxidants e.
ascorbate, urate, vitamin E, pyruvate, glutathione, albumin, taurine and hypotaurine [ 9 ]. Studies have shown that antioxidants protect spermatozoa from ROS generating abnormal spermatozoa, scavenge ROS produced by leukocytes, prevent DNA fragmentation, improve semen quality, reduce cryodamage to spermatozoa, block premature sperm maturation and generally stimulate sperm vitality [ 91 , 92 ].
Superoxide dismutases are metal-containing enzymes that catalyze the conversion of two superoxides into oxygen and hydrogen peroxide, which is less toxic than superoxide [ 1 , 13 ]:. The enzymes are present in both intracellular and extracellular forms.
The second form is manganese SOD, which is found predominantly in the mitochondrial matrix and has manganese in its active center MnSOD, SOD-2 [ 93 ]. The secretory tetrameric SOD EC-SOD, SOD-3 may be detected in the extracellular space. The enzyme is associated with surface polysaccharides although it may also be found as a free molecule.
Structurally, SOD-3 is similar to SOD-2; however, it has zinc and copper in its active center instead of manganese [ 1 , 5 , 15 ]. SOD protects spermatozoa against spontaneous O 2 toxicity and lipid peroxidation [ 69 ]. Numerous studies have suggested a significant role for SOD in sperm motility both in vivo and in vitro.
The addition of SOD to human and animal semen [ 94 , 95 , 96 ] has been shown to protect spermatozoa against the harmful effects of ROS and improve sperm motility and membrane integrity during liquid storage or cryopreservation.
As such, it may be concluded that the SOD content in mature spermatozoa may be a good predictor of post-thaw motility recovery following sperm preservation. Catalase catalyzes the decomposition of hydrogen peroxide to molecular oxygen and water, thereby completing the detoxifying reaction started by SOD.
A characteristic feature of its structure is a heme system with centrally located iron [ 1 , 13 ]:. CAT has been found in peroxisomes, mitochondria, endoplasmic reticulum and the cytosol in a variety of cells [ 93 ]. In semen, the enzyme was detected in human, bovine and rat spermatozoa, as well as seminal plasma, with the prostate as its source [ 97 , 98 ].
Catalase activates sperm capacitation induced by nitric oxide [ 59 , 60 ]. Furthermore, it plays an important role in decreasing lipid peroxidation and protecting spermatozoa during genitourinary inflammation [ 25 ].
Numerous studies have revealed a positive relationship between sperm motility and the presence of CAT in mammalian ejaculates. Also, positive correlations were observed between sperm morphology and protein expression of CAT in seminal plasma [ 98 , 99 ].
Furthermore, CAT supplementation to fresh, processed and cryopreserved semen resulted in a higher sperm vitality, progressive motility and DNA integrity [ ].
Glutathione peroxidases are a family of selenium-containing enzymes, which catalyze the reduction of H 2 O 2 and organic peroxides, including phospholipid peroxides [ 93 ]. In their active site, the enzymes contain selenium in the form of selenocysteine.
where GSH symbolizes reduced glutathione and GS-SG represents glutathione disulfide. The reaction is based on the oxidation of selenol of a selenocysteine residue by H 2 O 2.
This process leads to its derivation with selenic acid RSeOH. This by-product is subsequently converted back to selenol through a two-step process that starts with a reaction comprising GSH to generate GS-SeR and water.
A second GSH molecule then reduces the GS-SeR intermediate back to selenol, releasing GS-SG as a by-product [ 1 , 5 , 13 ]:. The classic intracellular GPx1 is expressed in sperm nucleus, mitochondria and cytosol, as well as in the testes, prostate, seminal vesicles, vas deferens, epididymis, and has a significant relationship with sperm motility [ , ].
More importantly, a direct relationship has been reported between male fertility and phospholipid hydroperoxide glutathione peroxidase PHGPx; GPx4 , a selenoprotein that is highly expressed in testicular tissue and has a prominent role in the formation of the mitochondrial capsule [ 51 , 53 , 54 ].
Other enzymes, such as glutathione reductase, ceruloplasmin or heme oxygenases, may also participate in the enzymatic control of oxygen radicals and their products.
A short overview of minor antioxidant enzymes is provided in Table 2. Location: Found in the epididymis, sertoli cells, vas deferens, seminal vesicles, epithelium and prostate gland [ , ].
Roles: Catalyzes reduction of oxidized glutathione. Maintains glutathione homeostasis. Altered in infertile men, and these alterations seem to be linked to sperm morphology [ , , ].
Location: Most abundant in the seminiferous tubular fluid of mammalian testes, sperm acrosomes, human sperm and mouse spermatogenic cells [ , , ]. Roles: Detoxification enzymes, intracellular-binding proteins [ ].
Involved in epididymal maturation, capacitation and sperm-oocyte interactions [ , ]. Location: Semen, probably of testicular origin [ ]. Roles: Cu-dependent ferroxidase, a fundamental bridge between Fe utilization and Cu status.
Associated with the oxidation of ferrous ion into ferric [ ]. Prevents non-enzymatic generation of superoxide and scavenges superoxide, hydroxyl and singlet oxygen [ , ].
Has positive impact on sperm parameters and male fertility [ ]. Serves as a marker of a proper seminiferous tubule function [ ]. Location: Seminal plasma [ , ]. Roles: Primary binding and transport protein for iron and regulates iron transport and storage [ ].
Serves as a reliable index of seminiferous tubular function [ ]. Location: Two forms of heme oxygenase, HO-1 and HO-2, were identified in human testis and seminal plasma [ , ]. Roles: HO is strongly induced by oxidant stress and protects against oxidative insults.
Increases reduced glutathione levels, degrades heme and intervenes with the metabolism of biliverdin and bilirubin, which have potent antioxidant properties [ ].
HO is highly expressed in fertile normozoospermic subjects with positive correlations to sperm concentration, motility and morphology. HO enzyme activity is related to spermatogenesis and sperm motility processes [ , ]. Non-enzymatic antioxidants are also known as synthetic antioxidants or dietary supplements.
Glutathione is the most abundant thiol protein in mammalian cells [ ]. Being an endogenous source, it is synthesized by the liver but it can also be derived from dietary sources such as fresh meat, fruits and vegetables.
This molecule has three precursors: cysteine, glutamic acid and glycine. Its cysteine subunit provides and exposes -SH that directly scavenges free radicals. High levels are found especially in the testis of rats [ ] and the reproductive tract fluids and epididymal sperm of bulls [ 98 ].
GSH protects the cell membranes from lipid oxidation and prevents further formation of free radicals. Its deficit leads to instability of the sperm midpiece, which results in motility disorders [ ]. Glutathione supplementation in infertile subjects has led to a significant improvement in sperm parameters and prevents oxidative damage to sperm DNA.
A factor increasing the level of GSH is pantothenic acid, which by doing so also protects tissues against oxidative stress [ , ].
Vitamin C or ascorbic acid AA may be found in its reduced ascorbate as well as oxidized form dehydroascorbic acid , both of which are easily interconvertible and biologically active. Vitamin C is found in citrus fruits, peppers, strawberries, tomatoes, broccoli, brussels sprouts and other leafy vegetables.
AA is a water-soluble vitamin, and because of its hydrophilic nature, it has more effective scavenging properties at the plasma level than in the lipid bilayer [ ]. Vitamin C has been used in the management of male infertility on empirical grounds, particularly in the presence of non-specific seminal infections [ ].
Its presence in the seminal plasma of healthy males has been reported by various authors [ , , ]. Chinoy et al. Low concentration of vitamin C showed significant degenerative changes in the testes, epididymis and vas deferens of scorbutic guinea pigs.
On the other hand, excessive intake of vitamin C has been reported to cause reproductive failure in the men [ ]. This was further corroborated by the association of decreased AA followed by an increase in the seminal plasma LPO as observed in a human trial [ , ].
Moreover, it has been reported that AA supplementation leads to a significant reduction in the ROS concentration, sperm membrane LPO and DNA oxidation together with an increased sperm quality.
The results of a recent animal experimental study indicate that vitamin C improves the activity of antioxidant enzymes and significantly reduces malondialdehyde MDA concentration in testicular structures [ ]. Vitamin E is a term that encompasses a group of potent, lipid-soluble tocol tocopherol and tocotrienol derivatives qualitatively exhibiting the biological activity of RRR-α-tocopherol.
Structural analyses have revealed that molecules having vitamin E antioxidant activity include four tocopherols α-, β-, γ- and δ- and four tocotrienols α-, β-, γ- and δ- with α-tocopherol being the most abundant form in nature and mostly available in food, having the highest biological activity and reversing vitamin E deficiency symptoms.
The molecular functions fulfilled specifically by α-tocopherol have yet to be fully described; however, the antioxidant feature is the flagship of the biological activity related to vitamin E [ ]. Vitamin E is present within the seminal plasma and plasma membrane.
It is a lipid soluble, chain-breaking antioxidant that able to terminate free radical chain reactions, particularly the peroxidation of PUFAs [ , ].
Numerous reports emphasize on the role of α-tocopherol in the management of male infertility. A positive association was found between α-tocopherol in sperm plasma membranes and the percentage of motile, living and morphologically intact spermatozoa [ ].
At the same time, α-tocopherol levels were decreased significantly in oligo- and azoospermic patients in comparison to normospermic controls [ ]. A significant improvement in the in vitro ability of spermatozoa to bind the zona pellucida of unfertilized oocytes was found in men with high ROS production supplemented with vitamin E for 3 months [ ].
Vitamin E supplementation may also play a role in reducing sperm DNA fragmentation and morphology defects [ ]. There are other substances which may contribute to the maintenance of oxidative homeostasis. The prime function of these compounds is not to combat the production or action of ROS; however, their presence may decrease the risk of OS development.
Albumin, cysteine, taurine, zinc and selenium are the most known representatives. Furthermore, antioxidant substances isolated from natural resources, such as resveratrol, curcumin or lycopene, have recently emerged as suitable dietary supplements or therapeutics due to their chemical diversity, structural complexity, availability, lack of significant toxic effects and intrinsic biologic activity.
A short overview of secondary non-enzymatic antioxidants is provided in Table 3. Has the ability to reduce free radicals by acting with thiols and hydroxyl radicals. Plays a role as a precursor to glutathione [ ]. Reduces seminal OS and sperm DNA damage [ ].
When combined with selenium, NAC has a positive impact on sperm concentration and acrosome reaction [ , ]. Stimulates mitochondrial metabolism. Has the ability to shuttle long-chain lipids across the mitochondrial bilayer and start the process of ß-oxidation to create NADH and FADH 2 along with acetyl-CoA [ ].
Acts primarily in the epididymis. Prevents DNA damage and apoptosis during sperm maturation [ ]. Found abundantly in the mammalian body, including testes and spermatozoa [ ].
Participates in bile salt formation, calcium binding and transport, osmoregulation and stabilization of biological membranes. A component of cellular antioxidant defenses [ ].
Infection and inflammation may severely influence sperm production. In conclusion, we have reviewed the relationship between oxidative stress and male infertility and the involvement of proteomic studies in male infertility.
We have compared the values of differential protein profiles in seminal plasma in both oxidative and physiological conditions. With the literature in mind, the pathway analysis indicates the contribution of proteins to stress, cellular, metabolic, and regulatory pathways.
The compiled studies in this Review will contribute to the exploration of the prominent causes of idiopathic male infertility. It is hoped that if male infertility is recognized at a molecular level, its diagnosis, treatment, and prevention can be improved.
It was difficult to enumerate which mechanism should be targeted In normozoospermic conditions. However, this scenario is still incomplete and further research is needed to develop diagnostic assays based on methylated patterns, such as RNA and phosphorylation profiles.
We further highlighted the attractiveness of sperm DNA integrity as a biomarker for unexplained infertility. In the coming years, it is expected that idiopathic fertility can be diagnosed using omics technologies.
TH: conceptualization, writing—original draft preparation, MK and EM: methodology, illustration of figures and. GM and DHK, editing of manuscript, BT, funding acquisition and visualization, editing of the manuscript, YY, MIC, AF, AY, MSK editing of the manuscript.
All authors contributed and approved the submitted version of manuscript. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Medicine PCotASfR. Definitions of infertility and recurrent pregnancy loss: a committee opinion.
Fertil Steril 99 1 doi: PubMed Abstract CrossRef Full Text Google Scholar. Sabanegh ES, Agarwal A. Male Infertility. Springer Google Scholar.
Parekattil SJ, Esteves SC, Agarwal A. Hamada AJ, Montgomery B, Agarwal A. Male Infertility: A critical review of pharmacologic management. Expert Opin Pharmacother 13 17 — Tremellen K.
Oxidative stress and male infertility—a clinical perspective. Hum Reprod Update 14 3 — Khosrowbeygi A, Zarghami N. Levels of oxidative stress biomarkers in seminal plasma and their relationship with seminal parameters.
BMC Clin Pathol 7 1 :1—6. Pasqualotto FF, Sharma RK, Nelson DR, Thomas AJ Jr. Relationship between oxidative stress, semen characteristics, and clinical diagnosis in men undergoing infertility investigation. Fertil Steril 73 3 — Ochsendorf F.
Infections in the male genital tract and reactive oxygen species. Hum Reprod Update 5 5 — Hwang K, Lamb DJ. Molecular mechanisms of antioxidants in male infertility.
Male infertility: Springer , 45— CrossRef Full Text Google Scholar. Agarwal A, Allamaneni SS, Said TM. Chemiluminescence technique for measuring reactive oxygen species. Reprod BioMed Online 9 4 —8. Iwasaki A, Gagnon C.
Formation of reactive oxygen species in spermatozoa of infertile patients. Fertil Steril 57 2 — Ochsendorf F, Thiele J, Fuchs J, Schüttau H, Freisleben H, Buslau M, et al. Chemiluminescence in semen of infertile men. Andrologia 26 5 — Du Plessis SS, Kashou AH, Benjamin DJ, Yadav SP, Agarwal A.
Proteomics: a subcellular look at spermatozoa. Reprod Biol Endocrinol 9 1 :1— Mitulović G, Mechtler K. HPLC techniques for proteomics analysis—a short overview of latest developments.
Brief Funct Genomics 5 4 — Hamada A, Sharma R, Du Plessis SS, Willard B, Yadav SP, Sabanegh E, et al. Two-dimensional differential in-gel electrophoresis—based proteomics of male gametes in relation to oxidative stress.
Fertil Steril 99 5 — Sharma R, Agarwal A, Mohanty G, Du Plessis SS, Gopalan B, Willard B, et al. Proteomic analysis of seminal fluid from men exhibiting oxidative stress. Reprod Biol Endocrinol 11 1 :1— Sharma R, Agarwal A, Mohanty G, Hamada AJ, Gopalan B, Willard B, et al.
Proteomic analysis of human spermatozoa proteins with oxidative stress. Herwig R, Knoll C, Planyavsky M, Pourbiabany A, Greilberger J, Bennett KL. Proteomic analysis of seminal plasma from infertile patients with oligoasthenoteratozoospermia due to oxidative stress and comparison with fertile volunteers.
Fertil Steril 2 — Wang J, Wang J, Zhang H-R, Shi H-J, Ma D, Zhao H-X, et al. Proteomic analysis of seminal plasma from asthenozoospermia patients reveals proteins that affect oxidative stress responses and semen quality.
AJA 11 4 Organisation WH. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. Camb Univ Press Lu J-C, Huang Y-F, Lü N-Q.
WHO laboratory manual for the examination and processing of human semen: its applicability to andrology laboratories in China. Zhonghua nan ke xue Nat J Androl 16 10 — Kovac JR, Pastuszak AW, Lamb DJ.
The use of genomics, proteomics, and metabolomics in identifying biomarkers of male infertility. Fertil Steril 99 4 — Lewis SE, Aitken RJ, Conner SJ, De Iuliis G, Evenson DP, Henkel R, et al. The impact of sperm DNA damage in assisted conception and beyond: Recent advances in diagnosis and treatment.
Reprod BioMed Online 27 4 — Simon L, Proutski I, Stevenson M, Jennings D, McManus J, Lutton D, et al. Sperm DNA damage has a negative association with live-birth rates after IVF. Reprod BioMed Online 26 1 — Aitken R, Bronson R, Smith T, De Iuliis G.
The source and significance of DNA damage in human spermatozoa; a commentary on diagnostic strategies and straw man fallacies. MHR: Basic Sci Reprod Med 19 8 — Lewis SE. Sperm DNA fragmentation and base oxidation. Gen Dam Hum Spermat , — Aitken RJ, Whiting S, De Iuliis GN, McClymont S, Mitchell LA, Baker MA.
Electrophilic aldehydes generated by sperm metabolism activate mitochondrial reactive oxygen species generation and apoptosis by targeting succinate dehydrogenase.
JBC 39 — Fujita Y, Mihara T, Okazaki T, Shitanaka M, Kushino R, Ikeda C, et al. Toll-like receptors TLR 2 and 4 on human sperm recognize bacterial endotoxins and mediate apoptosis. Hum Reprod 26 10 — Koppers AJ, Mitchell LA, Wang P, Lin M, Aitken RJ. Phosphoinositide 3-kinase signalling pathway involvement in a truncated apoptotic cascade associated with motility loss and oxidative DNA damage in human spermatozoa.
Biochem 3 — Polzien L, Baljuls A, Rennefahrt UE, Fischer A, Schmitz W, Zahedi RP, et al. Identification of novel in vivo phosphorylation sites of the human proapoptotic protein BAD: pore-forming activity of BAD is regulated by phosphorylation. JBC 41 — Pujianto DA, Curry BJ, Aitken RJ.
Prolactin exerts a prosurvival effect on human spermatozoa via mechanisms that involve the stimulation of akt phosphorylation and suppression of caspase activation and capacitation. Endocrinology 3 — Rivlin J, Mendel J, Rubinstein S, Etkovitz N, Breitbart H.
Role of hydrogen peroxide in sperm capacitation and acrosome reaction. Biol Reprod 70 2 — Reactive oxygen species modulate independent protein phosphorylation pathways during human sperm capacitation. Free Radic Biol Med 40 6 — Positive role of reactive oxygen species in mammalian sperm capacitation: Triggering and modulation of phosphorylation events.
Free Radic Biol Med 41 4 — Villegas J, Kehr K, Soto L, Henkel R, Miska W, Sanchez R. Reactive oxygen species induce reversible capacitation in human spermatozoa.
Andrologia 35 4 — Aitken R, Paterson M, Fisher H, Buckingham D, Van Duin M. Redox regulation of tyrosine phosphorylation in human spermatozoa and its role in the control of human sperm function. J Cell Sci 5 — Rodriguez P, Beconi M. Peroxynitrite participates in mechanisms involved in capacitation of cryopreserved cattle.
Anim Reprod Sci — Takakura K, Beckman JS, MacMillan-Crow LA, Crow JP. Rapid and irreversible inactivation of protein tyrosine phosphatases PTP1B, CD45, and LAR by peroxynitrite. Arch Biochem Biophy 2 — Aitken RJ. The capacitation-apoptosis highway: Oxysterols and mammalian sperm function.
Biol Reprod 85 1 :9— Aitken RJ, Baker MA, Nixon B. Are sperm capacitation and apoptosis the opposite ends of a continuum driven by oxidative stress? AJA 17 4 Cormier N, Ma S, Bailey Jl Premature capacitation of bovine spermatozoa is initiated by cryopreservation.
J Androl 18 4 —8. Ashrafi I, Kohram H, Ardabili FF. Antioxidative effects of melatonin on kinetics, microscopic and oxidative parameters of cryopreserved bull spermatozoa.
Darbandi S, Darbandi M. Lifestyle modifications on further reproductive problems. Cresco J Reprod Sci 1 1 :1—2. Zirkin BR, Chen H. Regulation of leydig cell steroidogenic function during aging.
Biol Reprod 63 4 — Turner TT, Bang HJ, Lysiak JJ. Experimental testicular torsion: Reperfusion blood flow and subsequent testicular venous plasma testosterone concentrations.
Urology 65 2 —4. Hanukoglu I. Antioxidant protective mechanisms against reactive oxygen species ROS generated by mitochondrial P systems in steroidogenic cells. Drug Metab Rev 38 — Luo L, Chen H, Trush MA, Show MD, Anway MD, Zirkin BR. Aging and the brown Norway rat leydig cell antioxidant defense system.
J Androl 27 2 —7. Aitken RJ, Baker MA, Sawyer D. Oxidative stress in the male germ line and its role in the aetiology of male infertility and genetic disease. Reprod BioMed Online 7 1 — Agarwal A, Said TM.
Role of sperm chromatin abnormalities and DNA damage in male infertility. Hum Reprod Update 9 4 — Meucci E, Milardi D, Mordente A, Martorana GE, Giacchi E, De Marinis L, et al. Total antioxidant capacity in patients with varicoceles. Fertil Steril — Mancini A, Leone E, Festa R, Grande G, Silvestrini A, De Marinis L, et al.
Effects of testosterone on antioxidant systems in male secondary hypogonadism. J Androl 29 6 —9. Mancini A, Festa R, Silvestrini A, Nicolotti N, Di Donna V, La Torre G, et al.
Hormonal regulation of total antioxidant capacity in seminal plasma. J Androl 30 5 — Chainy G, Samantaray S, Samanta L. Testosterone-induced changes in testicular antioxidant system. Andrologia 29 6 —9. Shang X, Huang Y, Ye Z, Yu X, Gu W.
Protection of melatonin against damage of sperm mitochondrial function induced by reactive oxygen species. Lakpour N, Mahfouz RZ, Akhondi MM, Agarwal A, Kharrazi H, Zeraati H, et al.
Relationship of seminal plasma antioxidants and serum male hormones with sperm chromatin status in male factor infertility. Syst Biol Reprod Med 58 5 — Oluboyo A, Adijeh R, Onyenekwe C, Oluboyo B, Mbaeri T, Odiegwu C, et al.
Relationship between serum levels of testosterone, zinc and selenium in infertile males attending fertility clinic in nnewi, south east Nigeria. AJMMS —4. Safarinejad MR. Efficacy of coenzyme Q10 on semen parameters, sperm function and reproductive hormones in infertile men.
J Urol 1 — Richthoff J, Spano M, Giwercman Y, Frohm B, Jepson K, Malm J, et al. The impact of testicular and accessory sex gland function on sperm chromatin integrity as assessed by the sperm chromatin structure assay SCSA.
Hum Reprod 17 12 —9. Meeker JD, Singh NP, Hauser R. Serum concentrations of estradiol and free T4 are inversely correlated with sperm DNA damage in men from an infertility clinic.
J Androl 29 4 — Dobrzyńska MM, Baumgartner A, Anderson D. Antioxidants modulate thyroid hormone-and noradrenaline-induced DNA damage in human sperm. Mutagenesis 19 4 — Palomba S, Falbo A, Espinola S, Rocca M, Capasso S, Cappiello F, et al. Effects of highly purified follicle-stimulating hormone on sperm DNA damage in men with male idiopathic subfertility: a pilot study.
J Endocrinol Invest 34 10 — Colacurci N, Monti MG, Fornaro F, Izzo G, Izzo P, Trotta C, et al. Recombinant human FSH reduces sperm DNA fragmentation in men with idiopathic oligoasthenoteratozoospermia. J Androl 33 4 — Tesarik J, Martinez F, Rienzi L, Iacobelli M, Ubaldi F, Mendoza C, et al.
In-vitro effects of FSH and testosterone withdrawal on caspase activation and DNA fragmentation in different cell types of human seminiferous epithelium. Hum Reprod 17 7 —9. Nematollahi-Mahani S, Azizollahi G, Baneshi M, Safari Z, Azizollahi S.
Effect of folic acid and zinc sulphate on endocrine parameters and seminal antioxidant level after varicocelectomy. Andrologia 46 3 —5. Manna PR, Tena-Sempere M, Huhtaniemi IT.
Molecular mechanisms of thyroid hormone-stimulated steroidogenesis in mouse leydig tumor cells: Involvement of the steroidogenic acute regulatory StAR protein. JBC 9 — Kalyanaraman B, Darley-Usmar V, Davies KJ, Dennery PA, Forman HJ, Grisham MB, et al. Measuring reactive oxygen and nitrogen species with fluorescent probes: challenges and limitations.
Free Radic Biol Med 52 1 :1—6. Adewoyin M, Mohsin SMN, Arulselvan P, Hussein MZ, Fakurazi S. Enhanced anti-inflammatory potential of cinnamate-zinc layered hydroxide in lipopolysaccharide-stimulated RAW Drug Des Dev Ther Inducible nitric oxide synthase in the rat testis: Evidence for potential roles in both normal function and inflammation-mediated infertility.
Biol Reprod 63 5 — Wang J, Wang W, Li S, Han Y, Zhang P, Meng G, et al. Hydrogen sulfide as a potential target in preventing spermatogenic failure and testicular dysfunction. ARS 28 16 — Hales DB. Endocrinology 5 — Liew SH, Meachem SJ, Hedger MP.
A stereological analysis of the response of spermatogenesis to an acute inflammatory episode in adult rats. J Androl 28 1 — Generation of reactive oxygen species in subgroups of infertile men. Int J Androl 13 5 — Diemer T, Hales D, Weidner W. Immune—endocrine interactions and leydig cell function: the role of cytokines.
Andrologia 35 1 — Moretti E, Collodel G, Mazzi L, Campagna M, Iacoponi F, Figura N. Resistin, interleukin-6, tumor necrosis factor-alpha, and human semen parameters in the presence of leukocytospermia, smoking habit, and varicocele.
Lazaros LA, Xita NV, Chatzikyriakidou AL, Kaponis AI, Grigoriadis NG, Hatzi EG, et al. Association of TNFα, TNFR1, and TNFR2 polymorphisms with sperm concentration and motility. J Androl 33 1 — Maegawa M, Kamada M, Irahara M, Yamamoto S, Yoshikawa S, Kasai Y, et al A repertoire of cytokines in human seminal plasma.
J Reprod Immunol 54 — Politch JA, Tucker L, Bowman FP, Anderson DJ. Concentrations and significance of cytokines and other immunologic factors in semen of healthy fertile men.
Hum Reprod 22 11 — Cheng CY, Mruk DD. A local autocrine axis in the testes that regulates spermatogenesis. Nat Rev Endocrinol 6 7 — Li MW, Mruk DD, Lee WM, Cheng CY. Cytokines and junction restructuring events during spermatogenesis in the testis: An emerging concept of regulation.
Cytokine Growth Factor Rev 20 4 — Gonzalez CR, Matzkin ME, Frungieri MB, Terradas C, Ponzio R, Puigdomenech E, et al. Expression of the TGF-beta1 system in human testicular pathologies.
Reprod Biol Endocrinol 8 1 :1— Camejo M, Segnini A, Proverbio F. Interleukin-6 IL-6 in seminal plasma of infertile men, and lipid peroxidation of their sperm. Arch Androl 47 2 — Vera O, Vásqucz LA, Muñoz MG. Semen quality and presence of cytokines in seminal fluid of bull ejaculates.
Theriogenology 60 3 —8. Aitken RJ, Buckingham DW, Brindle J, Gomez E, Baker HG, Irvine DS. Andrology: Analysis of sperm movement in relation to the oxidative stress created by leukocytes in washed sperm preparations and seminal plasma.
Hum Reprod 10 8 — Yin Y, DeWolf WC, Morgentaler A. Prevention of oxidative stress In healthy males, sperm DNA is protected from OS by two main mechanisms. Management of oxidative stress In the management of OS, the first step to take is to ascertain the underlying cause of the imbalance and treat it [ 80 ].
Table 2 Mechanisms of action and effects of various antioxidants Click for larger image. Trussell JC. Optimal diagnosis and medical treatment of male infertility.
Semin Reprod Med ;— PubMed CrossRef. World Health Organisation. WHO Laboratory Manual for the Examination and Processing of Human Semen. Geneva: World Health Organization; Agarwal A, Sekhon LH.
Oxidative stress and antioxidants for idiopathic oligoasthenoteratospermia: is it justified? Indian J Urol ;— Saalu LC. The incriminating role of reactive oxygen species in idiopathic male infertility: an evidence based evaluation.
Pak J Biol Sci ;— Hampl R, Drábková P, Kanďár R, Stěpán J. Impact of oxidative stress on male infertility. Ceska Gynekol ;— Henkel RR. Leukocytes and oxidative stress: dilemma for sperm function and male fertility. Asian J Androl ;— Lanzafame FM, La Vignera S, Vicari E, Calogero AE.
Oxidative stress and medical antioxidant treatment in male infertility. Reprod Biomed Online ;— Saleh RA, Agarwal A. Oxidative stress and male infertility: from research bench to clinical practice. J Androl ;— Bansal AK, Bilaspuri GS.
Impacts of oxidative stress and antioxidants on semen functions. Vet Med Int ; Gharagozloo P, Aitken RJ. The role of sperm oxidative stress in male infertility and the significance of oral antioxidant therapy.
Hum Reprod ;— Tremellen K. Oxidative stress and male infertility--a clinical perspective. Hum Reprod Update ;— De Iuliis GN, Wingate JK, Koppers AJ, McLaughlin EA, Aitken RJ. Definitive evidence for the nonmitochondrial production of superoxide anion by human spermatozoa.
J Clin Endocrinol Metab ;— Aitken RJ, Baker MA, De Iuliis GN, Nixon B. New insights into sperm physiology and pathology. Handb Exp Pharmacol ; — Butler A, He X, Gordon RE, Wu HS, Gatt S, Schuchman EH. Reproductive pathology and sperm physiology in acid sphingomyelinase-deficient mice.
Am J Pathol ;— Miranda-Vilela AL, Alves PC, Akimoto AK, Pereira LC, Nazaré Klautau-Guimarães M, Grisolia CK. The effect of hydrogen peroxide-induced oxidative stress on leukocytes depends on age and physical training in healthy human subjects carrying the same genotypes of antioxidant enzymes' gene polymorphisms.
Am J Hum Biol ;— Chen SJ, Allam JP, Duan YG, Haidl G. Influence of reactive oxygen species on human sperm functions and fertilizing capacity including therapeutical approaches. Arch Gynecol Obstet ;— Hazout A, Menezo Y, Madelenat P, Yazbeck C, Selva J, Cohen-Bacrie P.
Causes and clinical implications of sperm DNA damages. Gynecol Obstet Fertil ;— Sikka SC. Relative impact of oxidative stress on male reproductive function. Curr Med Chem ;— Sabeur K, Ball BA. Characterization of NADPH oxidase 5 in equine testis and spermatozoa. Reproduction ;— Choudhary R, Chawala VK, Soni ND, Kumar J, Vyas RK.
Oxidative stress and role of antioxidants in male infertility. Pak J Physiol ;— Esteves SC. Effect of cigarette smoking on levels of seminal oxidative stress in infertile men: a prospective study.
Int Braz J Urol ;— Saleh RA, Agarwal A, Nada EA, El-Tonsy MH, Sharma RK, Meyer A, et al. Negative effects of increased sperm DNA damage in relation to seminal oxidative stress in men with idiopathic and male factor infertility.
Fertil Steril ;79 Suppl — Lavranos G, Balla M, Tzortzopoulou A, Syriou V, Angelopoulou R. Investigating ROS sources in male infertility: a common end for numerous pathways.
Reprod Toxicol ;— Agarwal A, Saleh RA, Bedaiwy MA. Role of reactive oxygen species in the pathophysiology of human reproduction. Fertil Steril ;— Lu JC, Huang YF, Lü NQ.
WHO Laboratory Manual for the Examination and Processing of Human Semen: its applicability to andrology laboratories in China. Zhonghua Nan Ke Xue ;— Nandipati KC, Pasqualotto FF, Thomas AJ Jr, Agarwal A. Relationship of interleukin-6 with semen characteristics and oxidative stress in vasectomy reversal patients.
Andrologia ;— Rengan AK, Agarwal A, van der Linde M, du Plessis SS. An investigation of excess residual cytoplasm in human spermatozoa and its distinction from the cytoplasmic droplet. Reprod Biol Endocrinol ; Will MA, Swain J, Fode M, Sonksen J, Christman GM, Ohl D.
The great debate: varicocele treatment and impact on fertility. Shiraishi K, Matsuyama H, Takihara H. Pathophysiology of varicocele in male infertility in the era of assisted reproductive technology. Int J Urol ;— Agarwal A, Deepinder F, Sharma RK, Ranga G, Li J. Effect of cell phone usage on semen analysis in men attending infertility clinic: an observational study.
Aitken RJ, Bennetts LE, Sawyer D, Wiklendt AM, King BV. Impact of radio frequency electromagnetic radiation on DNA integrity in the male germline.
Int J Androl ;— De Iuliis GN, Newey RJ, King BV, Aitken RJ. Mobile phone radiation induces reactive oxygen species production and DNA damage in human spermatozoa in vitro.
PLoS One ;4:e Esfandiari N, Saleh RA, Blaut AP, Sharma RK, Nelson DR, Thomas AJ Jr, et al. Effects of temperature on sperm motion characteristics and reactive oxygen species. Int J Fertil Womens Med ;— Pant N, Shukla M, Kumar Patel D, Shukla Y, Mathur N, Kumar Gupta Y, et al.
Correlation of phthalate exposures with semen quality. Toxicol Appl Pharmacol ;— Latini G, Del Vecchio A, Massaro M, Verrotti A, De Felice C. Phthalate exposure and male infertility. Toxicology ;— Kasahara E, Sato EF, Miyoshi M, Konaka R, Hiramoto K, Sasaki J, et al.
Role of oxidative stress in germ cell apoptosis induced by di 2-ethylhexyl phthalate. Biochem J ;— Jurasović J, Cvitković P, Pizent A, Colak B, Telisman S. Semen quality and reproductive endocrine function with regard to blood cadmium in Croatian male subjects.
Biometals ;— Saleh RA, Agarwal A, Sharma RK, Nelson DR, Thomas AJ Jr. Jarow JP. Semen quality of male smokers and nonsmokers in infertile couples. J Urol ;— Kiziler AR, Aydemir B, Onaran I, Alici B, Ozkara H, Gulyasar T, et al.
High levels of cadmium and lead in seminal fluid and blood of smoking men are associated with high oxidative stress and damage in infertile subjects. Biol Trace Elem Res ;— Agarwal A, Prabakaran SA.
Mechanism, measurement, and prevention of oxidative stress in male reproductive physiology. Indian J Exp Biol ;— Tsai WW, Niessen S, Goebel N, Yates JR 3rd, Guccione E, Montminy M. PRMT5 modulates the metabolic response to fasting signals.
Proc Natl Acad Sci U S A ;— Kothari S, Thompson A, Agarwal A, du Plessis SS. Free radicals: their beneficial and detrimental effects on sperm function. de Lamirande E, O'Flaherty C. Sperm activation: role of reactive oxygen species and kinases. Biochim Biophys Acta ;— Suarez SS. Control of hyperactivation in sperm.
Makker K, Agarwal A, Sharma R. Indian J Med Res ;— Calamera J, Buffone M, Ollero M, Alvarez J, Doncel GF. Superoxide dismutase content and fatty acid composition in subsets of human spermatozoa from normozoospermic, asthenozoospermic, and polyzoospermic semen samples.
Mol Reprod Dev ;— Khosrowbeygi A, Zarghami N. Fatty acid composition of human spermatozoa and seminal plasma levels of oxidative stress biomarkers in subfertile males.
Prostaglandins Leukot Essent Fatty Acids ;— Sanocka D, Kurpisz M. Reactive oxygen species and sperm cells.
Zribi N, Chakroun NF, Elleuch H, Abdallah FB, Ben Hamida AS, Gargouri J, et al. Sperm DNA fragmentation and oxidation are independent of malondialdheyde.
Schulte RT, Ohl DA, Sigman M, Smith GD. Sperm DNA damage in male infertility: etiologies, assays, and outcomes. J Assist Reprod Genet ;— Kemal Duru N, Morshedi M, Oehninger S.
Effects of hydrogen peroxide on DNA and plasma membrane integrity of human spermatozoa. Badouard C, Ménézo Y, Panteix G, Ravanat JL, Douki T, Cadet J, et al. Determination of new types of DNA lesions in human sperm. Zygote ;— González-Marín C, Gosálvez J, Roy R. Types, causes, detection and repair of DNA fragmentation in animal and human sperm cells.
Int J Mol Sci ;— Valavanidis A, Vlachogianni T, Fiotakis C. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev ;— Aitken RJ, Koppers AJ. Apoptosis and DNA damage in human spermatozoa. Aitken RJ, Baker MA. Causes and consequences of apoptosis in spermatozoa; contributions to infertility and impacts on development.
Int J Dev Biol ;— Agarwal A, Said TM. Role of sperm chromatin abnormalities and DNA damage in male infertility. Kao SH, Chao HT, Chen HW, Hwang TI, Liao TL, Wei YH. Increase of oxidative stress in human sperm with lower motility. du Plessis SS, McAllister DA, Luu A, Savia J, Agarwal A, Lampiao F.
Effects of H 2 O 2 exposure on human sperm motility parameters, reactive oxygen species levels and nitric oxide levels. Koppers AJ, Mitchell LA, Wang P, Lin M, Aitken RJ.
Phosphoinositide 3-kinase signalling pathway involvement in a truncated apoptotic cascade associated with motility loss and oxidative DNA damage in human spermatozoa.
Aitken RJ, Whiting S, De Iuliis GN, McClymont S, Mitchell LA, Baker MA. Electrophilic aldehydes generated by sperm metabolism activate mitochondrial reactive oxygen species generation and apoptosis by targeting succinate dehydrogenase.
J Biol Chem ;— La Vignera S, Condorelli RA, Vicari E, D'Agata R, Calogero AE. Effects of the exposure to mobile phones on male reproduction: a review of the literature. Miraglia E, De Angelis F, Gazzano E, Hassanpour H, Bertagna A, Aldieri E, et al.
Doshi SB, Khullar K, Sharma RK, Agarwal A. Role of reactive nitrogen species in male infertility. Agarwal A, Makker K, Sharma R. Clinical relevance of oxidative stress in male factor infertility: an update.
Am J Reprod Immunol ;— Kefer JC, Agarwal A, Sabanegh E. Role of antioxidants in the treatment of male infertility.
Agarwal A, Said TM, Bedaiwy MA, Banerjee J, Alvarez JG. Oxidative stress in an assisted reproductive techniques setting. Lampiao F. Free radicals generation in an in vitro fertilization setting and how to minimize them. World J Obstet Gynecol ;— du Plessis SS, Makker K, Desai NR, Agarwal A.
Impact of oxidative stress on IVF. Obstet Gynecol ;— Deepinder F, Cocuzza M, Agarwal A. Should seminal oxidative stress measurement be offered routinely to men presenting for infertility evaluation? Endocr Pract ;— Aydemir B, Onaran I, Kiziler AR, Alici B, Akyolcu MC.
The influence of oxidative damage on viscosity of seminal fluid in infertile men. Wang Y, Liang CL, Wu JQ, Xu C, Qin SX, Gao ES. Do Ureaplasma urealyticum infections in the genital tract affect semen quality?
Zorn B, Sesek-Briski A, Osredkar J, Meden-Vrtovec H. Semen polymorphonuclear neutrophil leukocyte elastase as a diagnostic and prognostic marker of genital tract inflammation--a review.
Clin Chem Lab Med ;— Menkveld R. Clinical significance of the low normal sperm morphology value as proposed in the fifth edition of the WHO Laboratory Manual for the Examination and Processing of Human Semen.
Aitken RJ, Baker MA, O'Bryan M. Shedding light on chemiluminescence: the application of chemiluminescence in diagnostic andrology.
The exact mechanism of sperm dysfunction is not known in Feee cases. Extensive research snd the last decade has led to the identification Glucagon hormone and hypoglycemia free radicals reactive mald Free radicals and male infertility as mediators of sperm dysfunction Safe weight loss both specific diagnoses snd idiopathic cases of male infertility. Nifertility role infertiliyy free radicals has Herbal joint support studied extensively in the process of human reproduction. We know now that a certain level of free radicals is necessary for normal sperm function, whereas an excessive level of free radicals can cause detrimental effect on sperm function and subsequent fertilisation and offspring health. Oxidative stress develops when there is an imbalance between generation of free radicals and scavenging capacity of anti-oxidants in reproductive tract. Oxidative stress has been shown to affect both standard semen parameters and fertilising capacity. In addition, high levels of free radicals have been associated with lack of or poor fertility outcome after natural conception or assisted reproduction.
Welcher ausgezeichnet topic