
HbAc targets for diabetes management -
More aggressive targets may be recommended if they can be achieved safely and with an acceptable burden of therapy and if life expectancy is sufficient to reap the benefits of stringent targets.
Severe or frequent hypoglycemia is an absolute indication for the modification of treatment regimens, including setting higher glycemic goals. Diabetes is a chronic disease that progresses over decades. Thus, a goal that might be appropriate for an individual early in the course of their diabetes may change over time.
Thus, a finite period of intensive control to near-normal A1C may yield enduring benefits even if control is subsequently deintensified as patient characteristics change.
Over time, comorbidities may emerge, decreasing life expectancy and thereby decreasing the potential to reap benefits from intensive control. Also, with longer disease duration, diabetes may become more difficult to control, with increasing risks and burdens of therapy.
Thus, A1C targets should be reevaluated over time to balance the risks and benefits as patient factors change. Recommended glycemic targets for many nonpregnant adults are shown in Table 6. CGM may be used to assess glycemic target as noted in Recommendation 6. Postprandial glucose may be targeted if A1C goals are not met despite reaching preprandial glucose goals.
Postprandial glucose measurements should be made 1—2 h after the beginning of the meal, generally peak levels in patients with diabetes.
The issue of preprandial versus postprandial BGM targets is complex Elevated postchallenge 2-h oral glucose tolerance test glucose values have been associated with increased cardiovascular risk independent of fasting plasma glucose in some epidemiologic studies, whereas intervention trials have not shown postprandial glucose to be a cardiovascular risk factor independent of A1C.
In people with diabetes, surrogate measures of vascular pathology, such as endothelial dysfunction, are negatively affected by postprandial hyperglycemia. However, outcome studies have shown A1C to be the primary predictor of complications, and landmark trials of glycemic control such as the DCCT and UKPDS relied overwhelmingly on preprandial BGM.
Additionally, a randomized controlled trial in patients with known CVD found no CVD benefit of insulin regimens targeting postprandial glucose compared with those targeting preprandial glucose Therefore, it is reasonable to check postprandial glucose in individuals who have premeal glucose values within target but A1C values above target.
An analysis of data from participants in the ADAG study with type 1 diabetes and with type 2 diabetes found that the glucose ranges highlighted in Table 6. These findings support that premeal glucose targets may be relaxed without undermining overall glycemic control as measured by A1C.
Fifteen minutes after treatment, if blood glucose monitoring BGM shows continued hypoglycemia, the treatment should be repeated. Once the BGM or glucose pattern is trending up, the individual should consume a meal or snack to prevent recurrence of hypoglycemia.
Caregivers, school personnel, or family members providing support to these individuals should know where it is and when and how to administer it. Glucagon administration is not limited to health care professionals. Hypoglycemia is the major limiting factor in the glycemic management of type 1 and type 2 diabetes.
Recommendations regarding the classification of hypoglycemia are outlined in Table 6. If a patient has level 2 hypoglycemia without adrenergic or neuroglycopenic symptoms, they likely have hypoglycemia unawareness discussed further below.
This clinical scenario warrants investigation and review of the medical regimen 78 — Reprinted from Agiostratidou et al. Symptoms of hypoglycemia include, but are not limited to, shakiness, irritability, confusion, tachycardia, and hunger. Hypoglycemia may be inconvenient or frightening to patients with diabetes.
Level 3 hypoglycemia may be recognized or unrecognized and can progress to loss of consciousness, seizure, coma, or death.
Hypoglycemia is reversed by administration of rapid-acting glucose or glucagon. Hypoglycemia can cause acute harm to the person with diabetes or others, especially if it causes falls, motor vehicle accidents, or other injury.
A large cohort study suggested that among older adults with type 2 diabetes, a history of level 3 hypoglycemia was associated with greater risk of dementia Conversely, in a substudy of the ACCORD trial, cognitive impairment at baseline or decline in cognitive function during the trial was significantly associated with subsequent episodes of level 3 hypoglycemia Studies of rates of level 3 hypoglycemia that rely on claims data for hospitalization, emergency department visits, and ambulance use substantially underestimate rates of level 3 hypoglycemia 89 yet reveal a high burden of hypoglycemia in adults over 60 years of age in the community African Americans are at substantially increased risk of level 3 hypoglycemia 90 , In addition to age and race, other important risk factors found in a community-based epidemiologic cohort of older Black and White adults with type 2 diabetes include insulin use, poor or moderate versus good glycemic control, albuminuria, and poor cognitive function Level 3 hypoglycemia was associated with mortality in participants in both the standard and the intensive glycemia arms of the ACCORD trial, but the relationships between hypoglycemia, achieved A1C, and treatment intensity were not straightforward.
An association of level 3 hypoglycemia with mortality was also found in the ADVANCE trial An association between self-reported level 3 hypoglycemia and 5-year mortality has also been reported in clinical practice Glucose variability is also associated with an increased risk for hypoglycemia Young children with type 1 diabetes and the elderly, including those with type 1 and type 2 diabetes 86 , 95 , are noted as particularly vulnerable to hypoglycemia because of their reduced ability to recognize hypoglycemic symptoms and effectively communicate their needs.
Individualized glucose targets, patient education, dietary intervention e. CGM with automated low glucose suspend and hybrid closed-loop systems have been shown to be effective in reducing hypoglycemia in type 1 diabetes For patients with type 1 diabetes with level 3 hypoglycemia and hypoglycemia unawareness that persists despite medical treatment, human islet transplantation may be an option, but the approach remains experimental 98 , This change reflects the results of the ADAG study, which demonstrated that higher glycemic targets corresponded to A1C goals An additional goal of raising the lower range of the glycemic target was to limit overtreatment and provide a safety margin in patients titrating glucose-lowering drugs such as insulin to glycemic targets.
This should be reviewed at each patient visit. Hypoglycemia treatment requires ingestion of glucose- or carbohydrate-containing foods — The acute glycemic response correlates better with the glucose content of food than with the carbohydrate content of food.
Pure glucose is the preferred treatment, but any form of carbohydrate that contains glucose will raise blood glucose. Added fat may retard and then prolong the acute glycemic response. In type 2 diabetes, ingested protein may increase insulin response without increasing plasma glucose concentrations Therefore, carbohydrate sources high in protein should not be used to treat or prevent hypoglycemia.
Ongoing insulin activity or insulin secretagogues may lead to recurrent hypoglycemia unless more food is ingested after recovery. Once the glucose returns to normal, the individual should be counseled to eat a meal or snack to prevent recurrent hypoglycemia.
The use of glucagon is indicated for the treatment of hypoglycemia in people unable or unwilling to consume carbohydrates by mouth. Those in close contact with, or having custodial care of, people with hypoglycemia-prone diabetes family members, roommates, school personnel, childcare providers, correctional institution staff, or coworkers should be instructed on the use of glucagon, including where the glucagon product is kept and when and how to administer it.
An individual does not need to be a health care professional to safely administer glucagon. In addition to traditional glucagon injection powder that requires reconstitution prior to injection, intranasal glucagon and ready-to-inject glucagon preparations for subcutaneous injection are available.
Care should be taken to ensure that glucagon products are not expired. Hypoglycemia prevention is a critical component of diabetes management. BGM and, for some patients, CGM are essential tools to assess therapy and detect incipient hypoglycemia.
Patients should understand situations that increase their risk of hypoglycemia, such as when fasting for laboratory tests or procedures, when meals are delayed, during and after the consumption of alcohol, during and after intense exercise, and during sleep.
Hypoglycemia may increase the risk of harm to self or others, such as when driving. Teaching people with diabetes to balance insulin use and carbohydrate intake and exercise are necessary, but these strategies are not always sufficient for prevention 82 , — Formal training programs to increase awareness of hypoglycemia and to develop strategies to decrease hypoglycemia have been developed, including the Blood Glucose Awareness Training Programme, Dose Adjusted for Normal Eating DAFNE , and DAFNEplus.
Conversely, some individuals with type 1 diabetes and hypoglycemia who have a fear of hyperglycemia are resistant to relaxation of glycemic targets 78 , Regardless of the factors contributing to hypoglycemia and hypoglycemia unawareness, this represents an urgent medical issue requiring intervention.
In type 1 diabetes and severely insulin-deficient type 2 diabetes, hypoglycemia unawareness or hypoglycemia-associated autonomic failure can severely compromise stringent diabetes control and quality of life.
This syndrome is characterized by deficient counterregulatory hormone release, especially in older adults, and a diminished autonomic response, which are both risk factors for and caused by hypoglycemia.
Hence, patients with one or more episodes of clinically significant hypoglycemia may benefit from at least short-term relaxation of glycemic targets and availability of glucagon Any person with recurrent hypoglycemia or hypoglycemia unawareness should have their glucose management regimen adjusted.
With the advent of CGM and CGM-assisted pump therapy, there has been a promise of alarm-based prevention of hypoglycemia , These studies had differing A1C at entry and differing primary end points and thus must be interpreted carefully.
Real-time CGM studies can be divided into studies with elevated A1C with the primary end point of A1C reduction and studies with A1C near target with the primary end point of reduction in hypoglycemia , — In people with type 1 and type 2 diabetes with A1C above target, CGM improved A1C between 0.
A recent report in people with type 1 diabetes over the age of 60 years revealed a small but statistically significant decrease in hypoglycemia No study to date has reported a decrease in level 3 hypoglycemia.
In a single study using intermittently scanned CGM, adults with type 1 diabetes with A1C near goal and impaired awareness of hypoglycemia demonstrated no change in A1C and decreased level 2 hypoglycemia For people with type 2 diabetes, studies examining the impact of CGM on hypoglycemic events are limited; a recent meta-analysis does not reflect a significant impact on hypoglycemic events in type 2 diabetes , whereas improvements in A1C were observed in most studies — Overall, real-time CGM appears to be a useful tool for decreasing time spent in a hypoglycemic range in people with impaired awareness.
For type 2 diabetes, other strategies to assist patients with insulin dosing can improve A1C with minimal hypoglycemia , Stressful events e. may worsen glycemic control and precipitate diabetic ketoacidosis or nonketotic hyperglycemic hyperosmolar state, life-threatening conditions that require immediate medical care to prevent complications and death.
Any condition leading to deterioration in glycemic control necessitates more frequent monitoring of blood glucose; ketosis-prone patients also require urine or blood ketone monitoring. If accompanied by ketosis, vomiting, or alteration in the level of consciousness, marked hyperglycemia requires temporary adjustment of the treatment regimen and immediate interaction with the diabetes care team.
The patient treated with noninsulin therapies or medical nutrition therapy alone may require insulin. Adequate fluid and caloric intake must be ensured. Infection or dehydration are more likely to necessitate hospitalization of individuals with diabetes versus those without diabetes.
A physician with expertise in diabetes management should treat the hospitalized patient. Suggested citation: American Diabetes Association Professional Practice Committee. Glycemic targets: Standards of Medical Care in Diabetes— Diabetes Care ;45 Suppl.
Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care.
Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Previous Article Next Article. Assessment of Glycemic Control. Glycemic Goals. Intercurrent Illness. Article Navigation. Standards of Care December 16 Glycemic Targets: Standards of Medical Care in Diabetes— American Diabetes Association Professional Practice Committee American Diabetes Association Professional Practice Committee.
This Site. Google Scholar. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. View Large. Number of days CGM device is worn recommend 14 days 2.
Mean glucose 4. Glucose management indicator 5. Figure 6. View large Download slide. Effect of flash glucose monitoring on glycemic control, hypoglycemia, diabetes-related distress, and resource utilization in the Association of British Clinical Diabetologists ABCD nationwide audit.
Search ADS. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes UKPDS 35 : prospective observational study. Status of hemoglobin A1c measurement and goals for improvement: from chaos to order for improving diabetes care. Time in range-A1c hemoglobin relationship in continuous glucose monitoring of type 1 diabetes: a real-world study.
Estimation of hemoglobin A1c from continuous glucose monitoring data in individuals with type 1 diabetes: is time in range all we need? Improved time in range over 1 year is associated with reduced albuminuria in individuals with sensor-augmented insulin pump-treated type 1 diabetes.
The relationships between time in range, hyperglycemia metrics, and HbA1c. Glycemic outcomes in adults with T1D are impacted more by continuous glucose monitoring than by insulin delivery method: 3 years of follow-up from the COMISAIR study.
Frequent monitoring of A1C during pregnancy as a treatment tool to guide therapy. The fallacy of average: how using HbA 1c alone to assess glycemic control can be misleading.
Empirically establishing blood glucose targets to achieve HbA 1c goals. Are there clinical implications of racial differences in HbA 1c? A difference, to be a difference, must make a difference.
Racial differences in the relationship of glucose concentrations and hemoglobin A1c levels. HbA 1c performance in African descent populations in the United States with normal glucose tolerance, prediabetes, or diabetes: a scoping review.
Association of sickle cell trait with hemoglobin A1c in African Americans. Impact of common genetic determinants of hemoglobin A1c on type 2 diabetes risk and diagnosis in ancestrally diverse populations: a transethnic genome-wide meta-analysis.
Relationship of A1C to glucose concentrations in children with type 1 diabetes: assessments by high-frequency glucose determinations by sensors.
Diabetes screening with hemoglobin A 1c versus fasting plasma glucose in a multiethnic middle-school cohort. Racial disparity in A1C independent of mean blood glucose in children with type 1 diabetes.
Differences for percentage times in glycemic range between continuous glucose monitoring and capillary blood glucose monitoring in adults with type 1 diabetes: analysis of the REPLACE-BG dataset.
The relationship of hemoglobin A1C to time-in-range in patients with diabetes. Clinical recommendations for the use of the ambulatory glucose profile in diabetes care. How tightly controlled do fluctuations in blood glucose levels need to be to reduce the risk of developing complications in people with type 1 diabetes?
Real world hybrid closed-loop discontinuation: predictors and perceptions of youth discontinuing the G system in the first 6 months. Glucose time in range and peripheral neuropathy in type 2 diabetes mellitus and chronic kidney disease. Association between continuous glucose monitoring-derived time in range, other core metrics, and albuminuria in type 2 diabetes.
Time in range is associated with carotid intima-media thickness in type 2 diabetes. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The management of type 1 diabetes in adults. A consensus report by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD.
Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Clinical effectiveness of telemedicine in diabetes mellitus: a meta-analysis of 42 randomized controlled trials.
COVID pandemic lockdown in young people with type 1 diabetes: positive results of an unprecedented challenge for patients through telemedicine and change in use of continuous glucose monitoring. Impact of COVID lockdown on flash and real-time glucose sensor users with type 1 diabetes in England.
Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study.
Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes UKPDS Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS HbA 1c level as a risk factor for retinopathy and nephropathy in children and adults with type 1 diabetes: Swedish population based cohort study.
Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes UKPDS 36 : prospective observational study. Glucose control and vascular complications in veterans with type 2 diabetes. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes.
Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial.
Cardiovascular risk reduction with liraglutide: an exploratory mediation analysis of the LEADER trial. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. Association between 7 years of intensive treatment of type 1 diabetes and long-term mortality.
Metabolic profiles and treatment gaps in young-onset type 2 diabetes in Asia the JADE programme : a cross-sectional study of a prospective cohort. Age at diagnosis of type 2 diabetes mellitus and associations with cardiovascular and mortality risks.
Risk of first stroke in people with type 2 diabetes and its relation to glycaemic control: a nationwide observational study. Impact of age, age at diagnosis and duration of diabetes on the risk of macrovascular and microvascular complications and death in type 2 diabetes.
Intensive glycemic control and the prevention of cardiovascular events: implications of the ACCORD, ADVANCE, and VA diabetes trials. A position statement of the American Diabetes Association and a scientific statement of the American College of Cardiology Foundation and the American Heart Association.
Follow-up of blood-pressure lowering and glucose control in type 2 diabetes. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. The duration of diabetes affects the response to intensive glucose control in type 2 subjects: the VA Diabetes Trial.
Potential overtreatment of diabetes mellitus in older adults with tight glycemic control. Literature Review Flow Diagram for Chapter 8: Targets for Glycemic Control. From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group P referred R eporting I tems for S ystematic Reviews and M eta- A nalyses: The PRISMA Statement.
PLoS Med 6 6 : e pmed For more information, visit www. Bajaj reports personal fees from Abbott; grants and personal fees from AstraZeneca, Boehringer Ingelheim, Eli Lilly, Janssen, Merck, Novo Nordisk, and Sanofi, outside the submitted work.
Ross reports personal fees from Novo Nordisk, Eli Lilly, Janssen, AstraZeneca, and Boehringer Ingelheim, outside the submitted work.
No other authors have anything to disclose. All content on guidelines. ca, CPG Apps and in our online store remains exactly the same. For questions, contact communications diabetes.
Become a Member Order Resources Home About Contact DONATE. Next Previous. Key Messages Recommendations Figures Full Text References. Chapter Headings Introduction Conclusions Author Disclosures. Key Messages Optimal glycemic control is fundamental to the management of diabetes.
Both fasting and postprandial plasma glucose levels correlate with the risk of complications and contribute to the measured glycated hemoglobin A1C value. Glycemic targets should be individualized based on the individual's frailty or functional dependence and life expectancy.
Key Messages for People with Diabetes Try to keep your blood glucose as close to your target range as possible. This will help to delay or prevent complications of diabetes. Target ranges for blood glucose and A1C can vary and depend on a person's medical conditions and other risk factors.
Work with your diabetes health-care team to determine your target A1C and blood glucose target range fasting and after meals. Introduction Optimal glycemic control is fundamental to the management of diabetes. Figure 1 Recommended targets for glycemic control. A1C , glycated hemoglobin; CKD , chronic kidney disease.
Recommendations Glycemic targets should be individualized [Grade D, Consensus]. A higher A1C target may be considered in people with diabetes with the goals of avoiding hypoglycemia and over-treatment related to antihyperglycemic therapy, with any of the following [Grade D, Consensus for all]: Functionally dependent: 7.
Avoid symptomatic hyperglycemia and any hypoglycemia. Abbreviations: A1C , glycated hemoglobin; BG , blood glucose; CGM , continuous glucose monitoring; CHF , congestive heart failure, CI , confidence interval; CKD , chronic kidney disease; CV ; cardiovascular; FPG , fasting plasma glucose; GV , glucose variability HR , hazard ratio; MI , myocardial infarct; PG , plasma glucose; PPG, postprandial plasma glucose.
Author Disclosures Dr. References UK Prospective Diabetes Study UKPDS Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS UK Prospective Diabetes Study UKPDS Group.
Lancet ; The Diabetes Control and Complications Trial Research Group. The relationship of glycemic exposure HbA1c to the risk of development and progression of retinopathy in the diabetes control and complications trial. Diabetes ; Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes UKPDS 35 : Prospective observational study.
BMJ ; The relation of glycaemia to the risk of development and progression of retinopathy in the diabetic control and complications trial.
Diabetologia ; Coutinho M, Gerstein HC, Wang Y, et al. The relationship between glucose and incident cardiovascular events. Ametaregression analysis of published data from 20 studies of 95, individuals followed for Diabetes Care ; Levitan EB, Song Y, Ford ES, et al.
Is nondiabetic hyperglycemia a risk factor for cardiovascular disease? A meta-analysis of prospective studies. Arch Intern Med ; Study DECODE, Group EDEG. Is the current definition for diabetes relevant to mortality risk from all causes and cardiovascular and noncardiovascular diseases?
Sorkin JD, Muller DC, Fleg JL, et al. The relation of fasting and 2-h postchallenge plasma glucose concentrations to mortality: Data from the Baltimore longitudinal study of aging with a critical review of the literature. Cavalot F, Pagliarino A, Valle M, et al.
Postprandial blood glucose predicts cardiovascular events and all-cause mortality in type 2 diabetes in a year follow-up: Lessons from the San Luigi Gonzaga Diabetes Study. Emerging Risk Factors Collaboration, Sarwar N, Gao P, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: A collaborative meta-analysis of prospective studies.
The Diabetes Control and Complications Trial Research Group, Nathan DM, Genuth S, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus.
N Engl J Med ; Ohkubo Y, Kishikawa H, Araki E, et al. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: A randomized prospective 6-year study.
Diabetes Res Clin Pract ; Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes UKPDS Effect of intensive therapy on the microvascular complications of type 1 diabetes mellitus.
JAMA ; Martin CL, Albers J, Herman WH, et al. Neuropathy among the diabetes control and complications trial cohort 8 years after trial completion. Holman RR, Paul SK, Bethel MA, et al. New Engl J Med ; Nathan DM, Cleary PA, Backlund JY, et al.
Intensive diabetes treatment and cardiovascular disease in patientswith type 1 diabetes. N Engl JMed ; Association between 7 years of intensive treatment of type 1 diabetes and longterm mortality. Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, et al.
Effects of intensive glucose lowering in type 2 diabetes. The ACCORD Study Group and ACCORD Eye Study Group. Effects of medical therapies on retinopathy progression in type 2 diabetes.
Action to Control Cardiovascular Risk in Diabetes Follow-On ACCORDION Eye Study Group and the Action to Control Cardiovascular Risk in Diabetes Follow-On ACCORDION Study Group. Persistent effects of intensive glycemic control on retinopathy in type 2 diabetes in the Action to Control Cardiovascular Risk in Diabetes ACCORD follow-on study.
ADVANCE Collaborative Group, Patel A, MacMahon S, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. Zoungas S, Chalmers J, Neal B, et al. Follow-up of blood-pressure lowering and glucose control in type 2 diabetes. Duckworth W, Abraira C, Moritz T, et al.
Glucose control and vascular complications in veterans with type 2 diabetes. Moritz T, Duckworth W, Abraira C. Veterans Affairs diabetes trial-corrections. Hayward RA, Reaven PD, Wiitala WL, et al. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes.
Fang HJ, Zhou YH, Tian YJ, et al. Effects of intensive glucose lowering in treatment of type 2 diabetes mellitus on cardiovascular outcomes: A meta-analysis of data from 58, patients in 13 randomized controlled trials.
Int J Cardiol ; Calles-Escandon J, Lovato LC, Simons-Morton DG, et al.
It focuses manaegment the approaches and systems that are ideally Mind-body approaches to craving control diabetess to improve care for the majority of Mind-body approaches to craving control, the manabement of the HnAc. Diabetes in manafement including gestational diabetes is outside the scope Citrus aurantium for cholesterol management this guideline, although statements about pre-conception care for people with diabetes are included. Diabetes mellitus is a complex chronic disease characterized by hyperglycemia due to defective insulin secretion, defective insulin action or both. BC Observatory for Population and Public Health [publisher]. Chronic Disease Dashboard. Safe and effective therapies for the prevention of Type 1 Diabetes have not yet been identified. In some cases, medication may help reduce the risk for developing diabetes.American Diabetes Association; 6. Glycemic Managemeng Standards of Medical Care in Diabetees Members of the ADA Professional Practice Committeea multidisciplinary expert committee, targetss responsible for updating the Msnagement of Care annually, or more frequently as warranted.
Readers who wish to comment on the Standards manahement Care are invited to do so at professional. Glycemic management is primarily assessed with the A1C test, diabeets was African Mango seed triglyceride levels measure studied in clinical Calorie intake for vegetarians demonstrating the benefits of improved glycemic dibetes.
Patient self-monitoring of blood glucose SMBG HbcA help with self-management and medication adjustment, particularly in individuals taking insulin. Continuous glucose monitoring CGM also has an important role Mind-body approaches to craving control assessing the effectiveness and safety of treatment in many patients Hydration for sports injury prevention type 1 diabetes, and hargets data suggest it may also be helpful mnagement selected patients with type 2 diabetes, diabetee as those on intensive insulin regimens 1.
A1C reflects average glycemia over approximately 3 months. The performance mansgement the test is generally excellent for NGSP-certified assays manaegment.
The test is the major tool for assessing glycemic control and has strong predictive value for diabetes complications 1 — 3. Thus, A1C testing should targeets performed routinely in all patients Mind-body approaches to craving control diabetes—at initial assessment and as part of continuing care.
The use of point-of-care A1C testing may provide an opportunity for more targetss treatment changes during Astaxanthin and rosacea relief between patients and providers. Patients with managmeent 2 diabetes with stable diagetes well within target may do HbAx with A1C targefs only twice per year.
Unstable or intensively HbAd patients e. The A1C test is an indirect measure HbAc targets for diabetes management average glycemia and, as such, is subject manageemnt limitations. Diaebtes with any diaebtes Mind-body approaches to craving control, there is variability in the ofr of A1C.
Although Beauty standards variability is less on an intraindividual basis than that of blood glucose measurements, clinicians diabeetes exercise judgment when using A1C as the sole basis for diabetee glycemic control, particularly if the result is close to the threshold that might prompt a change in medication therapy.
However, most assays in use in dor U. are accurate in targers heterozygous for the fargets common variants targes.
Other measures of average HbcA such HbAcc fructosamine and 1,5-anhydroglucitol are available, but their translation into average mabagement levels HvAc their Manqgement significance fpr not as clear as for A1C.
Dixbetes some variability in the relationship between average glucose diabetse and A1C exists among HbAc targets for diabetes management individuals, generally the association between mean glucose eiabetes A1C diabeyes an individual correlates over time 5.
A1C does not provide a measure of glycemic variability or hypoglycemia. For patients prone to glycemic variability, especially patients with type targeys diabetes or type 2 diabetes with severe insulin deficiency, glycemic control is best evaluated by the combination of results from SMBG or CGM and A1C.
Table 6. In a recent report, mean glucose measured with CGM diwbetes central trgets A1C in participants in three randomized trials ,anagement that A1C may underestimate or diabdtes mean glucose 5.
Mean glucose levels for Plant-based caffeine source A1C levels 6tragets.
The correlation between A1C and average glucose was 0. Other studies have also demonstrated higher A1C levels in African Americans than in whites at a given mean Mind-body approaches to craving control concentration 89.
A1C Boosts natural digestion are available that do not demonstrate a statistically significant difference in manqgement with hemoglobin variants. Other assays have statistically significant interference, but the difference is Mind-body approaches to craving control clinically significant.
Use of an assay with managemdnt statistically significant interference may explain a report targeys for any manage,ent of mean glycemia, African Americans heterozygous for the common hemoglobin variant Menopause and hot weather had atrgets A1C by about 0.
Mnagement there are trgets meaningful Ginseng nutritional properties in how A1C relates to average glucose in children or in different ethnicities is manaement area for further managemeny 814 Until further flr is available, it seems prudent to establish Managemenr goals in these populations with diaebtes of diabtees individualized SMBG and A1C results.
For HbAc targets for diabetes management people with diabetes, glucose monitoring is key for the achievement of Astaxanthin and heart health targets. Major clinical trials of insulin-treated patients have included SMBG as part of multifactorial interventions to demonstrate the benefit of targrts glycemic control manatement diabetes complications SMBG managemenr thus an integral component of effective diabwtes of patients taking insulin.
In recent years, CGM has emerged as a complementary method for the assessment of glucose levels. Glucose monitoring allows patients to evaluate their individual response to therapy and assess whether glycemic targets are being safely achieved.
Integrating results into diabetes management can be a useful tool for guiding medical nutrition therapy and physical activity, preventing hypoglycemia, and adjusting medications particularly prandial insulin doses.
Appropriate patients might include those with short duration of diabetes, type 2 diabetes treated with lifestyle or metformin only, long life expectancy, or no significant cardiovascular disease.
Depicted are patient and disease factors used to determine optimal A1C targets. Characteristics and predicaments toward the left justify more stringent efforts to lower A1C; those toward the right suggest less stringent efforts. Adapted with permission from Inzucchi et al.
Hyperglycemia defines diabetes, and glycemic control is fundamental to diabetes management. Follow-up of the DCCT cohorts in the Epidemiology of Diabetes Interventions and Complications EDIC study 1718 demonstrated persistence of these microvascular benefits over two decades despite the fact that the glycemic separation between the treatment groups diminished and disappeared during follow-up.
The Kumamoto Study 19 and UK Prospective Diabetes Study UKPDS 2021 confirmed that intensive glycemic control significantly decreased rates of microvascular complications in patients with short-duration type 2 diabetes. Long-term follow-up of the UKPDS cohorts showed enduring effects of early glycemic control on most microvascular complications Epidemiologic analyses of the DCCT 16 and UKPDS 23 demonstrate a curvilinear relationship between A1C and microvascular complications.
Given the substantially increased risk of hypoglycemia in type 1 diabetes trials and with polypharmacy in type 2 diabetes, the risks of lower glycemic targets may outweigh the potential benefits on microvascular complications. Three landmark trials Action to Control Cardiovascular Risk in Diabetes [ACCORD], Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation [ADVANCE], and Veterans Affairs Diabetes Trial [VADT] were conducted to test the effects of near normalization of blood glucose on cardiovascular outcomes in individuals with long-standing type 2 diabetes and either known cardiovascular disease CVD or high cardiovascular risk.
These trials showed that lower A1C levels were associated with reduced onset or progression of some microvascular complications 24 — The concerning mortality findings in the ACCORD trial 27discussed below, and the relatively intense efforts required to achieve near euglycemia should also be considered when setting glycemic targets for individuals with longstanding diabetes such as those studied in ACCORD, ADVANCE, and VADT.
Findings from these studies suggest caution is needed in treating diabetes aggressively to near-normal A1C goals in people with long-standing type 2 diabetes with or at significant risk of CVD. However, on the basis of physician judgment and patient preferences, select patients, especially those with little comorbidity and long life expectancy, may benefit from adopting more intensive glycemic targets e.
CVD is a more common cause of death than microvascular complications in populations with diabetes. There is evidence for a cardiovascular benefit of intensive glycemic control after long-term follow-up of cohorts treated early in the course of type 1 diabetes.
In the DCCT, there was a trend toward lower risk of CVD events with intensive control. The benefit of intensive glycemic control in this cohort with type 1 diabetes has been shown to persist for several decades 29 and to be associated with a modest reduction in all-cause mortality In type 2 diabetes, there is evidence that more intensive treatment of glycemia in newly diagnosed patients may reduce long-term CVD rates.
ACCORD, ADVANCE, and VADT suggested no significant reduction in CVD outcomes with intensive glycemic control in participants followed for shorter durations 3. All three trials were conducted in relatively older participants with longer known duration of diabetes mean duration 8—11 years and either CVD or multiple cardiovascular risk factors.
The glycemic control comparison in ACCORD was halted early due to an increased mortality rate in the intensive compared with the standard treatment arm 1.
Analysis of the ACCORD data did not identify a clear explanation for the excess mortality in the intensive treatment arm Longer-term follow-up has shown no evidence of cardiovascular benefit or harm in the ADVANCE trial The end-stage renal disease rate was lower in the intensive treatment group over follow-up.
However, year follow-up of the VADT cohort 33 showed a reduction in the risk of cardiovascular events Heterogeneity of mortality effects across studies was noted, which may reflect differences in glycemic targets, therapeutic approaches, and population characteristics Mortality findings in ACCORD 27 and subgroup analyses of VADT 35 suggest that the potential risks of intensive glycemic control may outweigh its benefits in higher-risk patients.
In all three trials, severe hypoglycemia was significantly more likely in participants who were randomly assigned to the intensive glycemic control arm.
As discussed further below, severe hypoglycemia is a potent marker of high absolute risk of cardiovascular events and mortality Providers should be vigilant in preventing hypoglycemia and should not aggressively attempt to achieve near-normal A1C levels in patients in whom such targets cannot be safely and reasonably achieved.
If the patient is not at A1C target, continue metformin unless contraindicated and add SGLT2i or GLP-1 RA with proven cardiovascular benefit. If the patient is meeting A1C target, consider one of three strategies 39 :. If already on dual therapy or multiple glucose-lowering therapies and not on an SGLT2i or GLP-1 RA, consider switching to one of these agents with proven cardiovascular benefit.
Numerous factors must be considered when setting glycemic targets. The ADA proposes general targets appropriate for many patients but emphasizes the importance of individualization based on key patient characteristics.
Glycemic targets must be individualized in the context of shared decision making to address the needs and preferences of each patient and the individual characteristics that influence risks and benefits of therapy for each patient.
The factors to consider in individualizing goals are depicted in Fig. Figure 6. More stringent control such as an A1C of 6. Severe or frequent hypoglycemia is an absolute indication for the modification of treatment regimens, including setting higher glycemic goals.
Diabetes is a chronic disease that progresses over decades. Thus, a goal that might be appropriate for an individual early in the course of the disease may change over time.
Thus, a finite period of intensive control to near-normal A1C may yield enduring benefits even if control is subsequently deintensified as patient characteristics change.
Over time, comorbidities may emerge, decreasing life expectancy and the potential to reap benefits from intensive control. Also, with longer duration of disease, diabetes may become more difficult to control, with increasing risks and burdens of therapy.
Thus, A1C targets should be reevaluated over time to balance the risks and benefits as patient factors change. Recommended glycemic targets for many nonpregnant adults are shown in Table 6. The issue of preprandial versus postprandial SMBG targets is complex Elevated postchallenge 2-h oral glucose tolerance test glucose values have been associated with increased cardiovascular risk independent of fasting plasma glucose in some epidemiologic studies, but intervention trials have not shown postprandial glucose to be a cardiovascular risk factor independent of A1C.
In subjects with diabetes, surrogate measures of vascular pathology, such as endothelial dysfunction, are negatively affected by postprandial hyperglycemia. However, outcome studies have clearly shown A1C to be the primary predictor of complications, and landmark trials of glycemic control such as the DCCT and UKPDS relied overwhelmingly on preprandial SMBG.
Additionally, a randomized controlled trial in patients with known CVD found no CVD benefit of insulin regimens targeting postprandial glucose compared with those targeting preprandial glucose Therefore, it is reasonable for postprandial testing to be recommended for individuals who have premeal glucose values within target but have A1C values above target.
More or less stringent glycemic goals may be appropriate for individual patients. Postprandial glucose may be targeted if A1C goals are not met despite reaching preprandial glucose goals. Postprandial glucose measurements should be made 1—2 h after the beginning of the meal, generally peak levels in patients with diabetes.
An analysis of data from participants in the ADAG study with type 1 diabetes and with type 2 diabetes found that actual average glucose levels associated with conventional A1C targets were higher than older DCCT and ADA targets Table 6.
These findings support that premeal glucose targets may be relaxed without undermining overall glycemic control as measured by A1C.
: HbAc targets for diabetes management| Recommendations | Type 2 diabetes in adults: management | Guidance | NICE | In selecting initial therapy, we consider patient presentation eg, presence or absence of symptoms of hyperglycemia, comorbidities, baseline A1C level , individualized treatment goals and preferences, the glucose-lowering efficacy of individual drugs, and their adverse effect profile, tolerability, and cost [ 47 ]. We prefer initiating a single agent typically metformin and then sequentially adding additional glucose-lowering agents as needed, rather than starting with combination therapy [ 48 ]. Related Pathway s : Diabetes: Initial therapy for non-pregnant adults with type 2 DM. Asymptomatic, not catabolic — The majority of patients with newly diagnosed type 2 diabetes are asymptomatic, without symptoms of catabolism eg, without polyuria, polydipsia, or unintentional weight loss. Hyperglycemia may be noted on routine laboratory examination or detected by screening. Metformin — In the absence of specific contraindications, we suggest metformin as initial therapy for patients with newly diagnosed type 2 diabetes who are asymptomatic. We begin with mg once daily with the evening meal and, if tolerated, add a second mg dose with breakfast. The dose can be increased slowly one tablet every one to two weeks as tolerated to reach a total dose of mg per day. See 'When to start' above and "Metformin in the treatment of adults with type 2 diabetes mellitus", section on 'Dosing'. Metformin is the preferred initial therapy because of glycemic efficacy see 'Glycemic efficacy' below , promotion of modest weight loss, very low incidence of hypoglycemia, general tolerability, and favorable cost [ 47 ]. Metformin does not have adverse cardiovascular effects, and it appears to decrease cardiovascular events [ ]. See "Metformin in the treatment of adults with type 2 diabetes mellitus", section on 'Cardiovascular effects'. Metformin is far less expensive and has more clinical practice experience than glucagon-like peptide 1 GLP-1 receptor agonists and sodium-glucose cotransporter 2 SGLT2 inhibitors. Although some guidelines and experts endorse the initial use of these alternative agents as monotherapy or in combination with metformin [ 48,52 ], we prefer initiating a single agent typically metformin and then sequentially adding additional glucose-lowering agents as needed, rather than starting with combination therapy. In the clinical trials that demonstrated the protective effects of GLP-1 receptor agonists and SGLT2 inhibitors, these agents were added to background metformin therapy in most participants. Further, the cardiorenal benefits of GLP-1 receptor agonists and SGLT2 inhibitors have not been demonstrated in drug-naïve patients without established CVD or at low cardiovascular risk or without severely increased albuminuria. Although each diabetes medication is associated with adverse events, metformin is associated with less weight gain and fewer episodes of hypoglycemia compared with sulfonylureas, and with less edema, heart failure HF , and weight gain compared with thiazolidinediones. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects'. Although virtually all recommendations for initial pharmacologic therapy outside of China, where alpha-glucosidase inhibitors are recommended as an alternate first-line monotherapy [ 53 ] endorse use of metformin , there are, in fact, relatively few relevant direct comparative effectiveness data available. Contraindications to or intolerance of metformin — For patients who have gastrointestinal intolerance of metformin , slower titration, ensuring that the patient is taking the medication with food, or switching to an extended-release formulation may improve tolerability. For patients who still cannot tolerate metformin or have contraindications to it, we choose an alternative glucose-lowering medication guided initially by patient comorbidities, and in particular, the presence of atherosclerotic CVD ASCVD or albuminuric chronic kidney disease. See "Metformin in the treatment of adults with type 2 diabetes mellitus", section on 'Contraindications'. When compared with placebo, the GLP-1 receptor agonists liraglutide , semaglutide , and dulaglutide demonstrated favorable atherosclerotic cardiovascular and kidney outcomes [ ]. The SGLT2 inhibitors empagliflozin , canagliflozin , and dapagliflozin have also demonstrated benefit, especially for HF hospitalization, risk of kidney disease progression, and mortality [ ]. Patients at high CVD risk but without a prior event might benefit, but the data are less supportive. Similarly, patients without severely increased albuminuria have some benefit, but the absolute benefits are greater among those with severely increased albuminuria. To select a medication, we use shared decision-making with a focus on beneficial and adverse effects within the context of the degree of hyperglycemia as well as a patient's comorbidities and preferences. As examples:. SGLT2 inhibitors with cardiovascular benefit empagliflozin or canagliflozin are good alternatives, especially in the presence of HF. Given the high cost of these classes of medications, formulary coverage often determines the choice of the first medication within the class. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Microvascular outcomes'. Choice of agent is primarily dictated by provider preference, insurance formulary restrictions, eGFR, and cost. In the setting of declining eGFR, the main reason to prescribe SGLT2 inhibitors is to reduce progression of DKD. However, kidney and cardiac benefits have been shown in patients with eGFR below this threshold. Dosing in the setting of DKD is reviewed in detail elsewhere. See "Treatment of diabetic kidney disease", section on 'Type 2 diabetes: Treat with additional kidney-protective therapy'. An alternative or an additional agent may be necessary to achieve glycemic goals. GLP-1 receptor agonists are an alternative in patients with DKD as their glycemic effect is not related to eGFR. In addition, GLP-1 receptor agonists have been shown to slow the rate of decline in eGFR and prevent worsening of albuminuria. See 'Microvascular outcomes' below and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus" and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus". Of note, we avoid use of SGLT2 inhibitors in patients with frequent bacterial urinary tract infections or genitourinary yeast infections, low bone density and high risk for falls and fractures, foot ulceration, and factors predisposing to diabetic ketoacidosis eg, pancreatic insufficiency, drug or alcohol abuse disorder because of increased risk while using these agents. SLGT2 inhibitors should be held for 3 to 4 days before procedures including colonoscopy preparation and with poor oral intake to prevent diabetic ketoacidosis. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Contraindications and precautions'. Repaglinide acts at the sulfonylurea receptor to increase insulin secretion but is much shorter acting than sulfonylureas and is principally metabolized by the liver, with less than 10 percent renally excreted. Limited data suggest that dipeptidyl peptidase 4 DPP-4 inhibitors are effective and relatively safe in patients with chronic kidney disease. However, linagliptin is the only DPP-4 inhibitor that does not require a dose adjustment in the setting of kidney failure. GLP-1 receptor agonists may also be used safely in chronic kidney disease stage 4, but patient education for signs and symptoms of dehydration due to nausea or satiety is warranted to reduce the risk of acute kidney injury. Insulin may also be used, with a greater portion of the total daily dose administered during the day due to the risk of hypoglycemia, especially overnight, in chronic kidney disease and end-stage kidney disease ESKD. See "Management of hyperglycemia in patients with type 2 diabetes and advanced chronic kidney disease or end-stage kidney disease", section on 'Patients not on dialysis'. Without established cardiovascular or kidney disease — For patients without established CVD or kidney disease who cannot take metformin , many other options for initial therapy are available table 1. We suggest choosing an alternative glucose-lowering medication guided by efficacy, patient comorbidities, preferences, and cost. Although historically insulin has been used for type 2 diabetes only when inadequate glycemic management persists despite oral agents and lifestyle intervention, there are increasing data to support using insulin earlier and more aggressively in type 2 diabetes. By inducing near normoglycemia with intensive insulin therapy, both endogenous insulin secretion and insulin sensitivity improve; this results in better glycemic management, which can then be maintained with diet, exercise, and oral hypoglycemics for many months thereafter. Insulin may cause weight gain and hypoglycemia. See "Insulin therapy in type 2 diabetes mellitus", section on 'Indications for insulin'. If type 1 diabetes has been excluded, a GLP-1 receptor agonist is a reasonable alternative to insulin [ 66,67 ]. The frequency of injections and proved beneficial effects in the setting of CVD are the major differences among the many available GLP-1 receptor agonists. In practice, given the high cost of this class of medications, formulary coverage often determines the choice of the first medication within the class. Cost and insurance coverage may limit accessibility and adherence. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Patient selection'. Each one of these choices has individual advantages, benefits, and risks table 1. See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus" and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Patient selection' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Patient selection' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Potential indications'. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Weight loss' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Patient selection' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Weight loss'. The choice of sulfonylurea balances glucose-lowering efficacy, universal availability, and low cost with risk of hypoglycemia and weight gain. Pioglitazone , which is generic and another relatively low-cost oral agent, may also be considered in patients with specific contraindications to metformin and sulfonylureas. However, the risk of weight gain, HF, fractures, and the potential increased risk of bladder cancer raise the concern that the overall risks and cost of pioglitazone may approach or exceed its benefits. See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus" and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Potential indications'. For patients who are starting sulfonylureas, we suggest initiating lifestyle intervention first, at the time of diagnosis, since the weight gain that often accompanies a sulfonylurea will presumably be less if lifestyle efforts are underway. However, if lifestyle intervention has not produced a significant reduction in symptoms of hyperglycemia or in glucose values after one or two weeks, then the sulfonylurea should be added. Side effects may be minimized with diabetes self-management education focusing on medication reduction or omission with changes in diet, food accessibility, or activity that may increase the risk of hypoglycemia. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Suggested approach to the use of GLP-1 receptor agonist-based therapies' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Mechanism of action' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Mechanism of action' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Hypoglycemia'. Symptomatic catabolic or severe hyperglycemia — The frequency of symptomatic or severe diabetes has been decreasing in parallel with improved efforts to diagnose diabetes earlier through screening. If patients have been drinking a substantial quantity of sugar-sweetened beverages, reduction of carbohydrate intake, and rehydration with sugar-free fluids will help to reduce glucose levels within several days. See "Insulin therapy in type 2 diabetes mellitus", section on 'Initial treatment'. However, for patients who are injection averse, initial therapy with high-dose sulfonylurea is an alternative option. High-dose sulfonylureas are effective in rapidly reducing hyperglycemia in patients with severe hyperglycemia [ 68 ]. Metformin monotherapy is not helpful in improving symptoms in this setting, because the initial dose is low and increased over several weeks. However, metformin can be started at the same time as the sulfonylurea, slowly titrating the dose upward. Once the diet has been adequately modified and the metformin dose increased, the dose of sulfonylurea can be reduced and potentially discontinued. Patients with type 2 diabetes require relatively high doses of insulin compared with those needed for type 1 diabetes. Insulin preparations, insulin regimens, and timing of dosing are discussed in detail elsewhere. See "Insulin therapy in type 2 diabetes mellitus". See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Administration'. We typically use glimepiride 4 or 8 mg once daily. An alternative option is immediate-release glipizide 10 mg twice daily or, where available, gliclazide immediate-release 80 mg daily. We contact the patient every few days after initiating therapy to make dose adjustments increase dose if hyperglycemia does not improve or decrease dose if hyperglycemia resolves quickly or hypoglycemia develops. See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Sulfonylureas'. Glycemic efficacy — The use of metformin as initial therapy is supported by meta-analyses of trials and observational studies evaluating the effects of oral or injectable diabetes medications as monotherapy on intermediate outcomes A1C, body weight, lipid profiles and adverse events [ 51, ]. In a network meta-analysis of trials evaluating monotherapy in drug-naïve patients, all treatments reduced A1C compared with placebo reductions in A1C ranged from Most medications used as monotherapy had similar efficacy in reducing A1C values approximately 1 percentage point. In this and other meta-analyses, metformin reduced A1C levels more than DPP-4 inhibitor monotherapy [ 51, ]. There are few high-quality, head-to-head comparison trials of the available oral agents. In one such trial, A Diabetes Outcome Progression Trial ADOPT , recently diagnosed patients with type 2 diabetes were randomly assigned to monotherapy with the thiazolidinedione rosiglitazone , metformin , or glyburide [ 72 ]. At the four-year evaluation, 40 percent of the subjects in the rosiglitazone group had an A1C value less than 7 percent, as compared with 36 percent in the metformin group and 26 percent in the glyburide group. Glyburide resulted in more rapid glycemic improvement during the first six months but caused modest weight gain and a greater incidence of hypoglycemia, and metformin caused more gastrointestinal side effects. Rosiglitazone caused greater increases in weight, peripheral edema, and concentrations of low-density lipoprotein LDL cholesterol. There was also an unexpected increase in fractures in women taking rosiglitazone. The study was limited by a high rate of withdrawal of study participants. Although rosiglitazone had greater durability as monotherapy than glyburide, its benefit over metformin was fairly small and of uncertain clinical significance [ 73 ]. See "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Safety'. Cardiovascular outcomes — Cardiovascular benefit has been demonstrated for selected classes of diabetes medications, usually when added to metformin. See "Management of persistent hyperglycemia in type 2 diabetes mellitus", section on 'Monotherapy failure'. The cardiovascular effects of diabetes drugs are reviewed in the individual topics. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Insulin therapy in type 2 diabetes mellitus". In trials of patients with type 2 diabetes with and without chronic kidney disease, GLP-1 receptor agonists slowed the rate of decline in eGFR and prevented worsening of albuminuria [ 54,56,58 ]. These trials and other trials evaluating microvascular outcomes are reviewed in the individual topics. Guidelines — Our approach is largely consistent with American and European guidelines [ 52,74,75 ]. A consensus statement regarding the management of hyperglycemia in type 2 diabetes by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD was developed in and has been updated regularly, with the most recent revision published in [ 75 ]. The guidelines emphasize the importance of individualizing the choice of medications for the treatment of diabetes, considering important comorbidities CVD, HF, or chronic kidney disease; hypoglycemia risk; and need for weight loss and patient-specific factors including patient preferences, values, and cost [ 75 ]. We also agree with the World Health Organization WHO that sulfonylureas have a long-term safety profile, are inexpensive, and are highly effective, especially when used as described above, with patient education and dose adjustment to minimize side effects [ 76 ]. Blood glucose monitoring BGM is not necessary for most patients with type 2 diabetes who are on a stable regimen of diet or oral agents and who are not experiencing hypoglycemia. BGM may be useful for some patients with type 2 diabetes who use the results to modify eating patterns, exercise, or insulin doses on a regular basis. See "Glucose monitoring in the ambulatory management of nonpregnant adults with diabetes mellitus", section on 'Type 2 diabetes'. The balance among efficacy in lowering A1C, side effects, and costs must be carefully weighed in considering which drugs or combinations to choose. Avoiding insulin, the most potent of all hypoglycemic medications, at the expense of poorer glucose management and greater side effects and cost, is not likely to benefit the patient in the long term. See "Management of persistent hyperglycemia in type 2 diabetes mellitus", section on 'Our approach'. SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. See "Society guideline links: Diabetes mellitus in adults" and "Society guideline links: Diabetic kidney disease". These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon. Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest. Weight reduction through diet, exercise, and behavioral modification can all be used to improve glycemic management, although the majority of patients with type 2 diabetes will require medication. See 'Diabetes education' above. Glycemic targets are generally set somewhat higher for older adults and for those with comorbidities or a limited life expectancy and little likelihood of benefit from intensive therapy. See 'Glycemic management' above and "Glycemic control and vascular complications in type 2 diabetes mellitus", section on 'Choosing a glycemic target'. In the absence of specific contraindications, we suggest metformin as initial therapy for most patients Grade 2B. Although some guidelines and experts endorse the initial use of alternative agents as monotherapy or in combination with metformin, we prefer initiating a single agent typically metformin and then sequentially adding additional glucose-lowering agents as needed. See 'Metformin' above and 'Glycemic efficacy' above. We suggest initiating metformin at the time of diabetes diagnosis Grade 2C , along with consultation for lifestyle intervention. See 'When to start' above. The dose of metformin should be titrated to its maximally effective dose usually mg per day in divided doses over one to two months, as tolerated. See 'Contraindications to or intolerance of metformin' above. See 'Established cardiovascular or kidney disease' above. The majority of patients in the cardiovascular and renal outcomes trials had established cardiovascular disease CVD or diabetic kidney disease DKD with severely increased albuminuria, and therefore, these are the primary indications for one of these drugs. See 'Without established cardiovascular or kidney disease' above. Each one of these choices has individual advantages and risks table 1. Choice of medication is guided by efficacy, patient comorbidities, preferences, and cost. Sulfonylureas remain a highly effective treatment for hyperglycemia, particularly when cost is a barrier. Side effects of hypoglycemia and weight gain can be mitigated with careful dosing and diabetes self-management education. For patients who are injection averse, initial therapy with high-dose sulfonylurea is an alternative, particularly for patients who have been consuming large amounts of sugar-sweetened beverages, in whom elimination of carbohydrates can be anticipated to cause a reduction in glucose within several days. See 'Symptomatic catabolic or severe hyperglycemia' above and "Insulin therapy in type 2 diabetes mellitus". Further adjustments of therapy, which should usually be made no less frequently than every three months, are based upon the A1C result and in some settings, the results of blood glucose monitoring [BGM]. See 'Monitoring' above. See "Management of persistent hyperglycemia in type 2 diabetes mellitus" and "Insulin therapy in type 2 diabetes mellitus". Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Initial management of hyperglycemia in adults with type 2 diabetes mellitus. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Author: Deborah J Wexler, MD, MSc Section Editor: David M Nathan, MD Deputy Editor: Katya Rubinow, MD Contributor Disclosures. All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Dec 23, TREATMENT GOALS Glycemic management — Target glycated hemoglobin A1C levels in patients with type 2 diabetes should be tailored to the individual, balancing the anticipated reduction in microvascular complications over time with the immediate risks of hypoglycemia and other adverse effects of therapy. Summary of glucose-lowering interventions. UK Prospective Diabetes Study UKPDS Group. Lancet ; Holman RR, Paul SK, Bethel MA, et al. N Engl J Med ; Hayward RA, Reaven PD, Wiitala WL, et al. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. ADVANCE Collaborative Group, Patel A, MacMahon S, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, et al. Effects of intensive glucose lowering in type 2 diabetes. Rawshani A, Rawshani A, Franzén S, et al. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes. Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. Kazemian P, Shebl FM, McCann N, et al. Evaluation of the Cascade of Diabetes Care in the United States, JAMA Intern Med ; Pal K, Eastwood SV, Michie S, et al. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochrane Database Syst Rev ; :CD Saffari M, Ghanizadeh G, Koenig HG. Health education via mobile text messaging for glycemic control in adults with type 2 diabetes: a systematic review and meta-analysis. Prim Care Diabetes ; Liang X, Wang Q, Yang X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a meta-analysis. Diabet Med ; Henry RR, Scheaffer L, Olefsky JM. Glycemic effects of intensive caloric restriction and isocaloric refeeding in noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab ; Utzschneider KM, Carr DB, Barsness SM, et al. Diet-induced weight loss is associated with an improvement in beta-cell function in older men. Wing RR, Blair EH, Bononi P, et al. Caloric restriction per se is a significant factor in improvements in glycemic control and insulin sensitivity during weight loss in obese NIDDM patients. Diabetes Care ; Lean ME, Leslie WS, Barnes AC, et al. Primary care-led weight management for remission of type 2 diabetes DiRECT : an open-label, cluster-randomised trial. Delahanty LM. The look AHEAD study: implications for clinical practice go beyond the headlines. J Acad Nutr Diet ; Evert AB, Dennison M, Gardner CD, et al. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. Lean MEJ, Leslie WS, Barnes AC, et al. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol ; Niskanen LK, Uusitupa MI, Sarlund H, et al. Five-year follow-up study on plasma insulin levels in newly diagnosed NIDDM patients and nondiabetic subjects. Norris SL, Zhang X, Avenell A, et al. Long-term effectiveness of lifestyle and behavioral weight loss interventions in adults with type 2 diabetes: a meta-analysis. Am J Med ; United Kingdom Prospective Diabetes Study UKPDS. BMJ ; Umpierre D, Ribeiro PA, Kramer CK, et al. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: a systematic review and meta-analysis. JAMA ; Jeon CY, Lokken RP, Hu FB, van Dam RM. Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. For a short explanation of why the committee made these recommendations see the rationale and impact section on continuous glucose monitoring. Full details of the evidence and the committee's discussion are in evidence review C: continuous glucose monitoring in adults with type 2 diabetes. NICE technology appraisals for SGLT2 inhibitors recommend the use of these medicines only in specific populations and in certain circumstances. The update of this guideline looked at the clinical- and cost-effectiveness evidence for SGLT2 inhibitors in people with cardiovascular disease or at high risk of developing cardiovascular disease. The guideline recommends SGLT2 inhibitors in a wider population than the technology appraisals that were published before February We have produced a visual summary to provide an overview of the recommendations and additional information to support medicines choice. Base the choice of drug treatments on:. the person's individual clinical circumstances, for example comorbidities, contraindications, weight, and risks from polypharmacy. the effectiveness of the drug treatments in terms of metabolic response and cardiovascular and renal protection. cost if 2 drugs in the same class are appropriate, choose the option with the lowest acquisition cost. Also see the visual summary on first-line drug treatment for an overview of the recommendations and additional information to support medicines choice. For adults with type 2 diabetes and chronic kidney disease, follow recommendations on SGLT2 inhibitors in the section on chronic kidney disease in this guideline. See the recommendations on using risk scores and QRISK2 to assess cardiovascular disease risk in adults with type 2 diabetes in NICE's guideline on cardiovascular disease: risk assessment and reduction, including lipid modification. If they have chronic heart failure or established atherosclerotic cardiovascular disease , offer an SGLT2 inhibitor with proven cardiovascular benefit in addition to metformin. If they are at high risk of developing cardiovascular disease , consider an SGLT2 inhibitor with proven cardiovascular benefit in addition to metformin. See the rationale and impact section on first-line drug treatment for an explanation of 'proven cardiovascular benefit'. Start the SGLT2 inhibitor as soon as metformin tolerability is confirmed. If they have chronic heart failure or established atherosclerotic cardiovascular disease , offer an SGLT2 inhibitor with proven cardiovascular benefit. If they are at high risk of developing cardiovascular disease , consider an SGLT2 inhibitor with proven cardiovascular benefit. an SGLT2 inhibitor for people who meet the criteria in NICE's technology appraisal guidance on canagliflozin, dapagliflozin and empagliflozin as monotherapies or ertugliflozin as monotherapy or with metformin for treating type 2 diabetes. they are following a very low carbohydrate or ketogenic diet. For example, for people who are following a very low carbohydrate or ketogenic diet , they may need to delay treatment until they have changed their diet. For a short explanation of why the committee made these recommendations and how they might affect practice, see the rationale and impact section on first-line drug treatment. Full details of the evidence and the committee's decision are in evidence review B: pharmacological therapies with cardiovascular and other benefits in people with type 2 diabetes. how to optimise their current treatment regimen before thinking about changing treatments, taking into account factors such as:. adverse effects. stopping medicines that have had no impact on glycaemic control or weight, unless there is an additional clinical benefit, such as cardiovascular or renal protection, from continued treatment see the note below on off-label use. the considerations about treatment choice in recommendation 1. See NICE's information on prescribing medicines. Also see the recommendations on medication review in the NICE guideline on medicines optimisation and on reviewing medicines and supporting adherence in the NICE guideline on medicines adherence. Only stop the SGLT2 inhibitor if the person's circumstances have changed and the SGLT2 inhibitor is no longer appropriate. If they have or develop chronic heart failure or established atherosclerotic cardiovascular disease , offer an SGLT2 inhibitor with proven cardiovascular benefit in addition to current treatment or replace an existing drug with the SGLT2 inhibitor. If they are or become at high risk of developing cardiovascular disease , consider adding an SGLT2 inhibitor with proven cardiovascular benefit to current treatment or replacing an existing drug with the SGLT2 inhibitor. Take into account the person's current treatment regimen and preferences and make a shared decision about switching treatments or adding an SGLT2 inhibitor, as appropriate also see recommendations 1. For a short explanation of why the committee made these recommendations and how they might affect practice, see the rationale and impact section on reviewing drug treatments. Full details of the evidence and the committee's discussion are in evidence review B: pharmacological therapies with cardiovascular and other benefits in people with type 2 diabetes. Also see our visual summary on treatment options if further interventions are needed for an overview of the recommendations and additional information to support medicines choice. an SGLT2 inhibitor for people who meet the criteria in NICE's technology appraisal guidance on canagliflozin in combination therapy , ertugliflozin as monotherapy or with metformin , or dapagliflozin or empagliflozin in combination therapy. starting insulin-based treatment see the section on insulin-based treatments. for whom insulin therapy would have significant occupational implications or. weight loss would benefit other significant obesity-related comorbidities. For a short explanation of why the committee did not make any new recommendations, see the rationale and impact section on treatment options if further interventions are needed. injection technique, including rotating injection sites and avoiding repeated injections at the same point within sites. the DVLA's Assessing fitness to drive: a guide for medical professionals. support from an appropriately trained and experienced healthcare professional. Review the continued need for other blood glucose lowering therapies. separately or. Consider, as an alternative to NPH insulin, using insulin detemir or insulin glargine if:. the person needs help from a carer or healthcare professional to inject insulin, and use of insulin detemir or insulin glargine would reduce the frequency of injections from twice to once daily or. the person's lifestyle is restricted by recurrent symptomatic hypoglycaemic episodes or. the person prefers injecting insulin immediately before a meal or. who experience significant hypoglycaemia on NPH insulin irrespective of the level of HbA1c reached or. Make a shared decision with the person after discussing their preferences. For a short explanation of why the committee made the recommendations on biosimilars and how they might affect practice, see the rationale and impact section on long-acting insulin. the section on drug treatment. NICE's technology appraisal guidance on canagliflozin , dapagliflozin , and empagliflozin in combination therapy. they are at higher risk of periodontitis. if they get periodontitis, managing it can improve their blood glucose control and can reduce their risk of hyperglycaemia. For a short explanation of why the committee made these recommendations, see the rationale and impact section on periodontitis. Full details of the evidence and the committee's discussion are in evidence review D: periodontitis. the strongest evidence for effectiveness is for domperidone, but prescribers must take into account its safety profile, in particular its cardiac risk and potential interactions with other medicines. consider domperidone only in exceptional circumstances if domperidone is the only effective treatment and in accordance with MHRA guidance on domperidone. For guidance on safe prescribing of antidepressants such as tricyclic drugs and managing withdrawal, see NICE's guideline on medicines associated with dependence or withdrawal symptoms. they meet the criteria in the marketing authorisation including relevant estimated glomerular filtration rate [eGFR] thresholds. In November , not all SGLT2 inhibitors were licensed for this indication. they meet the criteria in the marketing authorisation including relevant eGFR thresholds. For a short explanation of why the committee made these recommendations and how they might affect practice, see the rationale and impact section on SGLT2 inhibitors for adults with type 2 diabetes and chronic kidney disease. Full details of the evidence and the committee's discussion are in evidence review A: SGLT2 inhibitors for people with chronic kidney disease and type 2 diabetes. Initially choose the drug with the lowest acquisition cost and take into account any contraindications. Explain that the screening service is effective at identifying problems so that they can be treated early. This section defines terms that have been used in a particular way for this guideline. For other definitions, see the NICE glossary and the Think Local, Act Personal Care and Support Jargon Buster. This includes coronary heart disease, acute coronary syndrome, previous myocardial infarction, stable angina, previous coronary or other revascularisation, cerebrovascular disease ischaemic stroke and transient ischaemic attack and peripheral arterial disease. A consultant-led multidisciplinary team may include a wide range of staff based in primary, secondary and community care. This covers both real-time continuous glucose monitoring rtCGM and intermittently scanned continuous glucose monitoring isCGM, commonly referred to as 'flash'. A continuous glucose monitor is a device that measures blood glucose levels and sends the readings to a display device or smartphone. an elevated lifetime risk of cardiovascular disease defined as the presence of 1 or more cardiovascular risk factors in someone under Cardiovascular disease risk factors: hypertension, dyslipidaemia, smoking, obesity, and family history in a first-degree relative of premature cardiovascular disease. The recommendations in this guideline also apply to any current or future biosimilar product of insulin glargine that has an appropriate marketing authorisation that allows the use of the biosimilar in the same indication. Two or more daily insulin injections, which could either be a basal-bolus regimen or more than one daily insulin injection. A chronic inflammatory gum disease that destroys the supporting tissues of the teeth the periodontium. Gingivitis is a milder form of periodontal disease than periodontitis. |
| Key Messages | Added fat may retard and then prolong the acute glycemic response. Strength training is more effective than aerobic exercise for improving glycaemic control and body composition in people with normal-weight type 2 diabetes: a randomised controlled trial. See 'Bariatric metabolic surgery' above and "Bariatric surgery for management of obesity: Indications and preoperative preparation", section on 'Preoperative counseling'. Lin CC, Li CI, Yang SY, et al. The use of point-of-care A1C testing may provide an opportunity for more timely treatment changes during encounters between patients and providers. |
| Type 2 diabetes in adults: management | Cardiovascular benefit has been demonstrated for some of these medications when taken in combination with metformin , but benefit has not been definitively established in drug-naïve patients at low to moderate cardiovascular risk. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. We avoid use of SGLT2 inhibitors in patients with frequent genitourinary yeast infections or bacterial urinary tract infections, low bone density and high risk for falls and fractures, foot ulceration, and factors predisposing to diabetic ketoacidosis eg, pancreatic insufficiency, drug or alcohol use disorder because of increased risk for each while using these agents. John Boltri, M. Effects of medical therapies on retinopathy progression in type 2 diabetes. |
| Diabetes Care | Discuss, based on the literature, the reason that ACP has chosen higher HbA1c targets. Postgraduate Institute for Medicine PIM requires faculty, planners, and others in control of educational content to disclose all their financial relationships with ineligible companies. All identified conflicts of interest COI are thoroughly vetted and mitigated according to PIM policy. PIM is committed to providing its learners with high quality accredited continuing education activities and related materials that promote improvements or quality in healthcare and not a specific proprietary business interest of an ineligible company. The PIM planners and others have nothing to disclose. The OBG Project planners and others have nothing to disclose. Faculty: Susan J. Gross, MD, receives consulting fees from Cradle Genomics, and has financial interest in The ObG Project, Inc. Planners and Managers : The PIM planners and managers, Trace Hutchison, PharmD, Samantha Mattiucci, PharmD, CHCP, Judi Smelker-Mitchek, MBA, MSN, RN, and Jan Schultz, MSN, RN, CHCP have nothing to disclose. Fees for participating and receiving CME credit for this activity are as posted on The ObG Project website. If you wish to receive acknowledgment for completing this activity, please complete the test and evaluation. In support of improving patient care, this activity has been planned and implemented by the Postgraduate Institute for Medicine and The ObG Project. Postgraduate Institute for Medicine is jointly accredited by the Accreditation Council for Continuing Medical Education ACCME , the Accreditation Council for Pharmacy Education ACPE , and the American Nurses Credentialing Center ANCC , to provide continuing education for the healthcare team. Postgraduate Institute for Medicine designates this enduring material for a maximum of 0. Physicians should claim only the credit commensurate with the extent of their participation in the activity. The maximum number of hours awarded for this Continuing Nursing Education activity is 0. The ACP has updated guidance to help providers better target hemoglobin A1c HbA1c targets for the pharmacologic treatment of type 2 diabetes. The ACP recommends. Clinicians should consider deintensifying pharmacologic therapy in patients with type 2 diabetes who achieve HbA1c levels less than 6. Clinicians should treat patients with type 2 diabetes to minimize symptoms related to hyperglycemia and avoid targeting an HbA1c level in patients with a life expectancy less than 10 years due to advanced age 80 years or older , residence in a nursing home, or chronic conditions such as dementia, cancer, end-stage kidney disease, or severe chronic obstructive pulmonary disease or congestive heart failure because the harms outweigh the benefits in this population. Overall, the ACP did not find that the benefits of lower HbA1c targets justified potential risks. NOTE: All guidelines allow for higher HbA1c targets depending on comorbid conditions and limited life expectancy. Hemoglobin A1c Targets for Glycemic Control With Pharmacologic Therapy for Nonpregnant Adults With Type 2 Diabetes Mellitus: A Guidance Statement Update From the American College of Physicians. American Diabetes Association® Deeply Concerned About New Guidance from American College of Physicians Regarding Blood Glucose Targets for People with Type 2 Diabetes. ADA: Glycemic Targets: Standards of Medical Care in Diabetes— American Association of Clinical Endocrinology Clinical Practice Guideline: Developing a Diabetes Mellitus Comprehensive Care Plan — Update. NICE: Type 2 diabetes in adults: management. TAKE THE POST TEST. ObGFirst® — Try It Free! Get specially curated clinical summaries delivered to your inbox every week for free. Certain educational activities may require additional software to view multimedia, presentation, or printable versions of their content. These activities will be marked as such and will provide links to the required software. That software may be: Adobe Flash, Apple QuickTime, Adobe Acrobat, Microsoft PowerPoint, Windows Media Player, or Real Networks Real One Player. The planners of this activity do not recommend the use of any agent outside of the labeled indications. The opinions expressed in the educational activity are those of the faculty and do not necessarily represent the views of the planners. Please refer to the official prescribing information for each product for discussion of approved indications, contraindications, and warnings. Participants have an implied responsibility to use the newly acquired information to enhance patient outcomes and their own professional development. The information presented in this activity is not meant to serve as a guideline for patient management. It appears you don't have enough CME Hours to take this Post-Test. Feel free to buy additional CME hours or upgrade your current CME subscription plan. For many people with diabetes, glucose monitoring is key for the achievement of glycemic targets. Major clinical trials of insulin-treated patients have included SMBG as part of multifactorial interventions to demonstrate the benefit of intensive glycemic control on diabetes complications SMBG is thus an integral component of effective therapy of patients taking insulin. In recent years, CGM has emerged as a complementary method for the assessment of glucose levels. Glucose monitoring allows patients to evaluate their individual response to therapy and assess whether glycemic targets are being safely achieved. Integrating results into diabetes management can be a useful tool for guiding medical nutrition therapy and physical activity, preventing hypoglycemia, and adjusting medications particularly prandial insulin doses. Appropriate patients might include those with short duration of diabetes, type 2 diabetes treated with lifestyle or metformin only, long life expectancy, or no significant cardiovascular disease. Depicted are patient and disease factors used to determine optimal A1C targets. Characteristics and predicaments toward the left justify more stringent efforts to lower A1C; those toward the right suggest less stringent efforts. Adapted with permission from Inzucchi et al. Hyperglycemia defines diabetes, and glycemic control is fundamental to diabetes management. Follow-up of the DCCT cohorts in the Epidemiology of Diabetes Interventions and Complications EDIC study 17 , 18 demonstrated persistence of these microvascular benefits over two decades despite the fact that the glycemic separation between the treatment groups diminished and disappeared during follow-up. The Kumamoto Study 19 and UK Prospective Diabetes Study UKPDS 20 , 21 confirmed that intensive glycemic control significantly decreased rates of microvascular complications in patients with short-duration type 2 diabetes. Long-term follow-up of the UKPDS cohorts showed enduring effects of early glycemic control on most microvascular complications Epidemiologic analyses of the DCCT 16 and UKPDS 23 demonstrate a curvilinear relationship between A1C and microvascular complications. Given the substantially increased risk of hypoglycemia in type 1 diabetes trials and with polypharmacy in type 2 diabetes, the risks of lower glycemic targets may outweigh the potential benefits on microvascular complications. Three landmark trials Action to Control Cardiovascular Risk in Diabetes [ACCORD], Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation [ADVANCE], and Veterans Affairs Diabetes Trial [VADT] were conducted to test the effects of near normalization of blood glucose on cardiovascular outcomes in individuals with long-standing type 2 diabetes and either known cardiovascular disease CVD or high cardiovascular risk. These trials showed that lower A1C levels were associated with reduced onset or progression of some microvascular complications 24 — The concerning mortality findings in the ACCORD trial 27 , discussed below, and the relatively intense efforts required to achieve near euglycemia should also be considered when setting glycemic targets for individuals with longstanding diabetes such as those studied in ACCORD, ADVANCE, and VADT. Findings from these studies suggest caution is needed in treating diabetes aggressively to near-normal A1C goals in people with long-standing type 2 diabetes with or at significant risk of CVD. However, on the basis of physician judgment and patient preferences, select patients, especially those with little comorbidity and long life expectancy, may benefit from adopting more intensive glycemic targets e. CVD is a more common cause of death than microvascular complications in populations with diabetes. There is evidence for a cardiovascular benefit of intensive glycemic control after long-term follow-up of cohorts treated early in the course of type 1 diabetes. In the DCCT, there was a trend toward lower risk of CVD events with intensive control. The benefit of intensive glycemic control in this cohort with type 1 diabetes has been shown to persist for several decades 29 and to be associated with a modest reduction in all-cause mortality In type 2 diabetes, there is evidence that more intensive treatment of glycemia in newly diagnosed patients may reduce long-term CVD rates. ACCORD, ADVANCE, and VADT suggested no significant reduction in CVD outcomes with intensive glycemic control in participants followed for shorter durations 3. All three trials were conducted in relatively older participants with longer known duration of diabetes mean duration 8—11 years and either CVD or multiple cardiovascular risk factors. The glycemic control comparison in ACCORD was halted early due to an increased mortality rate in the intensive compared with the standard treatment arm 1. Analysis of the ACCORD data did not identify a clear explanation for the excess mortality in the intensive treatment arm Longer-term follow-up has shown no evidence of cardiovascular benefit or harm in the ADVANCE trial The end-stage renal disease rate was lower in the intensive treatment group over follow-up. However, year follow-up of the VADT cohort 33 showed a reduction in the risk of cardiovascular events Heterogeneity of mortality effects across studies was noted, which may reflect differences in glycemic targets, therapeutic approaches, and population characteristics Mortality findings in ACCORD 27 and subgroup analyses of VADT 35 suggest that the potential risks of intensive glycemic control may outweigh its benefits in higher-risk patients. In all three trials, severe hypoglycemia was significantly more likely in participants who were randomly assigned to the intensive glycemic control arm. As discussed further below, severe hypoglycemia is a potent marker of high absolute risk of cardiovascular events and mortality Providers should be vigilant in preventing hypoglycemia and should not aggressively attempt to achieve near-normal A1C levels in patients in whom such targets cannot be safely and reasonably achieved. If the patient is not at A1C target, continue metformin unless contraindicated and add SGLT2i or GLP-1 RA with proven cardiovascular benefit. If the patient is meeting A1C target, consider one of three strategies 39 :. If already on dual therapy or multiple glucose-lowering therapies and not on an SGLT2i or GLP-1 RA, consider switching to one of these agents with proven cardiovascular benefit. Numerous factors must be considered when setting glycemic targets. The ADA proposes general targets appropriate for many patients but emphasizes the importance of individualization based on key patient characteristics. Glycemic targets must be individualized in the context of shared decision making to address the needs and preferences of each patient and the individual characteristics that influence risks and benefits of therapy for each patient. The factors to consider in individualizing goals are depicted in Fig. Figure 6. More stringent control such as an A1C of 6. Severe or frequent hypoglycemia is an absolute indication for the modification of treatment regimens, including setting higher glycemic goals. Diabetes is a chronic disease that progresses over decades. Thus, a goal that might be appropriate for an individual early in the course of the disease may change over time. Thus, a finite period of intensive control to near-normal A1C may yield enduring benefits even if control is subsequently deintensified as patient characteristics change. Over time, comorbidities may emerge, decreasing life expectancy and the potential to reap benefits from intensive control. Also, with longer duration of disease, diabetes may become more difficult to control, with increasing risks and burdens of therapy. Thus, A1C targets should be reevaluated over time to balance the risks and benefits as patient factors change. Recommended glycemic targets for many nonpregnant adults are shown in Table 6. The issue of preprandial versus postprandial SMBG targets is complex Elevated postchallenge 2-h oral glucose tolerance test glucose values have been associated with increased cardiovascular risk independent of fasting plasma glucose in some epidemiologic studies, but intervention trials have not shown postprandial glucose to be a cardiovascular risk factor independent of A1C. In subjects with diabetes, surrogate measures of vascular pathology, such as endothelial dysfunction, are negatively affected by postprandial hyperglycemia. However, outcome studies have clearly shown A1C to be the primary predictor of complications, and landmark trials of glycemic control such as the DCCT and UKPDS relied overwhelmingly on preprandial SMBG. Additionally, a randomized controlled trial in patients with known CVD found no CVD benefit of insulin regimens targeting postprandial glucose compared with those targeting preprandial glucose Therefore, it is reasonable for postprandial testing to be recommended for individuals who have premeal glucose values within target but have A1C values above target. More or less stringent glycemic goals may be appropriate for individual patients. Postprandial glucose may be targeted if A1C goals are not met despite reaching preprandial glucose goals. Postprandial glucose measurements should be made 1—2 h after the beginning of the meal, generally peak levels in patients with diabetes. An analysis of data from participants in the ADAG study with type 1 diabetes and with type 2 diabetes found that actual average glucose levels associated with conventional A1C targets were higher than older DCCT and ADA targets Table 6. These findings support that premeal glucose targets may be relaxed without undermining overall glycemic control as measured by A1C. Fifteen minutes after treatment, if SMBG shows continued hypoglycemia, the treatment should be repeated. Once SMBG returns to normal, the individual should consume a meal or snack to prevent recurrence of hypoglycemia. Caregivers, school personnel, or family members of these individuals should know where it is and when and how to administer it. Glucagon administration is not limited to health care professionals. Hypoglycemia is the major limiting factor in the glycemic management of type 1 and type 2 diabetes. Recommendations regarding the classification of hypoglycemia are outlined in Table 6. Classification of hypoglycemia Studies of rates of level 3 hypoglycemia that rely on claims data for hospitalization, emergency department visits, and ambulance use substantially underestimate rates of level 3 hypoglycemia 45 , yet find high burden of hypoglycemia in adults over 60 years of age in the community African Americans are at substantially increased risk of level 3 hypoglycemia 46 , In addition to age and race, other important risk factors found in a community-based epidemiologic cohort of older black and white adults with type 2 diabetes include insulin use, poor or moderate versus good glycemic control, albuminuria, and poor cognitive function Symptoms of hypoglycemia include, but are not limited to, shakiness, irritability, confusion, tachycardia, and hunger. Hypoglycemia may be inconvenient or frightening to patients with diabetes. Level 3 hypoglycemia may be recognized or unrecognized and can progress to loss of consciousness, seizure, coma, or death. It is reversed by administration of rapid-acting glucose or glucagon. Hypoglycemia can cause acute harm to the person with diabetes or others, especially if it causes falls, motor vehicle accidents, or other injury. A large cohort study suggested that among older adults with type 2 diabetes, a history of level 3 hypoglycemia was associated with greater risk of dementia Conversely, in a substudy of the ACCORD trial, cognitive impairment at baseline or decline in cognitive function during the trial was significantly associated with subsequent episodes of level 3 hypoglycemia Level 3 hypoglycemia was associated with mortality in participants in both the standard and the intensive glycemia arms of the ACCORD trial, but the relationships between hypoglycemia, achieved A1C, and treatment intensity were not straightforward. An association of level 3 hypoglycemia with mortality was also found in the ADVANCE trial An association between self-reported level 3 hypoglycemia and 5-year mortality has also been reported in clinical practice Young children with type 1 diabetes and the elderly, including those with type 1 and type 2 diabetes 48 , 53 , are noted as particularly vulnerable to hypoglycemia because of their reduced ability to recognize hypoglycemic symptoms and effectively communicate their needs. Individualized glucose targets, patient education, dietary intervention e. CGM with automated low glucose suspend has been shown to be effective in reducing hypoglycemia in type 1 diabetes For patients with type 1 diabetes with level 3 hypoglycemia and hypoglycemia unawareness that persists despite medical treatment, human islet transplantation may be an option, but the approach remains experimental 56 , This change reflects the results of the ADAG study, which demonstrated that higher glycemic targets corresponded to A1C goals 7. An additional goal of raising the lower range of the glycemic target was to limit overtreatment and provide a safety margin in patients titrating glucose-lowering drugs such as insulin to glycemic targets. Hypoglycemia treatment requires ingestion of glucose- or carbohydrate-containing foods. The acute glycemic response correlates better with the glucose content of food than with the carbohydrate content of food. Pure glucose is the preferred treatment, but any form of carbohydrate that contains glucose will raise blood glucose. Added fat may retard and then prolong the acute glycemic response. In type 2 diabetes, ingested protein may increase insulin response without increasing plasma glucose concentrations Therefore, carbohydrate sources high in protein should not be used to treat or prevent hypoglycemia. Ongoing insulin activity or insulin secretagogues may lead to recurrent hypoglycemia unless more food is ingested after recovery. Once the glucose returns to normal, the individual should be counseled to eat a meal or snack to prevent recurrent hypoglycemia. The use of glucagon is indicated for the treatment of hypoglycemia in people unable or unwilling to consume carbohydrates by mouth. Those in close contact with, or having custodial care of, people with hypoglycemia-prone diabetes family members, roommates, school personnel, child care providers, correctional institution staff, or coworkers should be instructed on the use of glucagon kits, including where the kit is and when and how to administer glucagon. An individual does not need to be a health care professional to safely administer glucagon. Care should be taken to ensure that glucagon kits are not expired. Hypoglycemia prevention is a critical component of diabetes management. SMBG and, for some patients, CGM are essential tools to assess therapy and detect incipient hypoglycemia. Patients should understand situations that increase their risk of hypoglycemia, such as when fasting for tests or procedures, when meals are delayed, during and after the consumption of alcohol, during and after intense exercise, and during sleep. Hypoglycemia may increase the risk of harm to self or others, such as with driving. Teaching people with diabetes to balance insulin use and carbohydrate intake and exercise are necessary, but these strategies are not always sufficient for prevention. In type 1 diabetes and severely insulin-deficient type 2 diabetes, hypoglycemia unawareness or hypoglycemia-associated autonomic failure can severely compromise stringent diabetes control and quality of life. This syndrome is characterized by deficient counterregulatory hormone release, especially in older adults, and a diminished autonomic response, which both are risk factors for, and caused by, hypoglycemia. Hence, patients with one or more episodes of clinically significant hypoglycemia may benefit from at least short-term relaxation of glycemic targets. Stressful events e. may worsen glycemic control and precipitate diabetic ketoacidosis or nonketotic hyperglycemic hyperosmolar state, life-threatening conditions that require immediate medical care to prevent complications and death. Any condition leading to deterioration in glycemic control necessitates more frequent monitoring of blood glucose; ketosis-prone patients also require urine or blood ketone monitoring. If accompanied by ketosis, vomiting, or alteration in the level of consciousness, marked hyperglycemia requires temporary adjustment of the treatment regimen and immediate interaction with the diabetes care team. The patient treated with noninsulin therapies or medical nutrition therapy alone may require insulin. Adequate fluid and caloric intake must be ensured. Infection or dehydration is more likely to necessitate hospitalization of the person with diabetes than the person without diabetes. A physician with expertise in diabetes management should treat the hospitalized patient. Suggested citation: American Diabetes Association. Glycemic targets: Standards of Medical Care in Diabetes— Diabetes Care ;42 Suppl. |
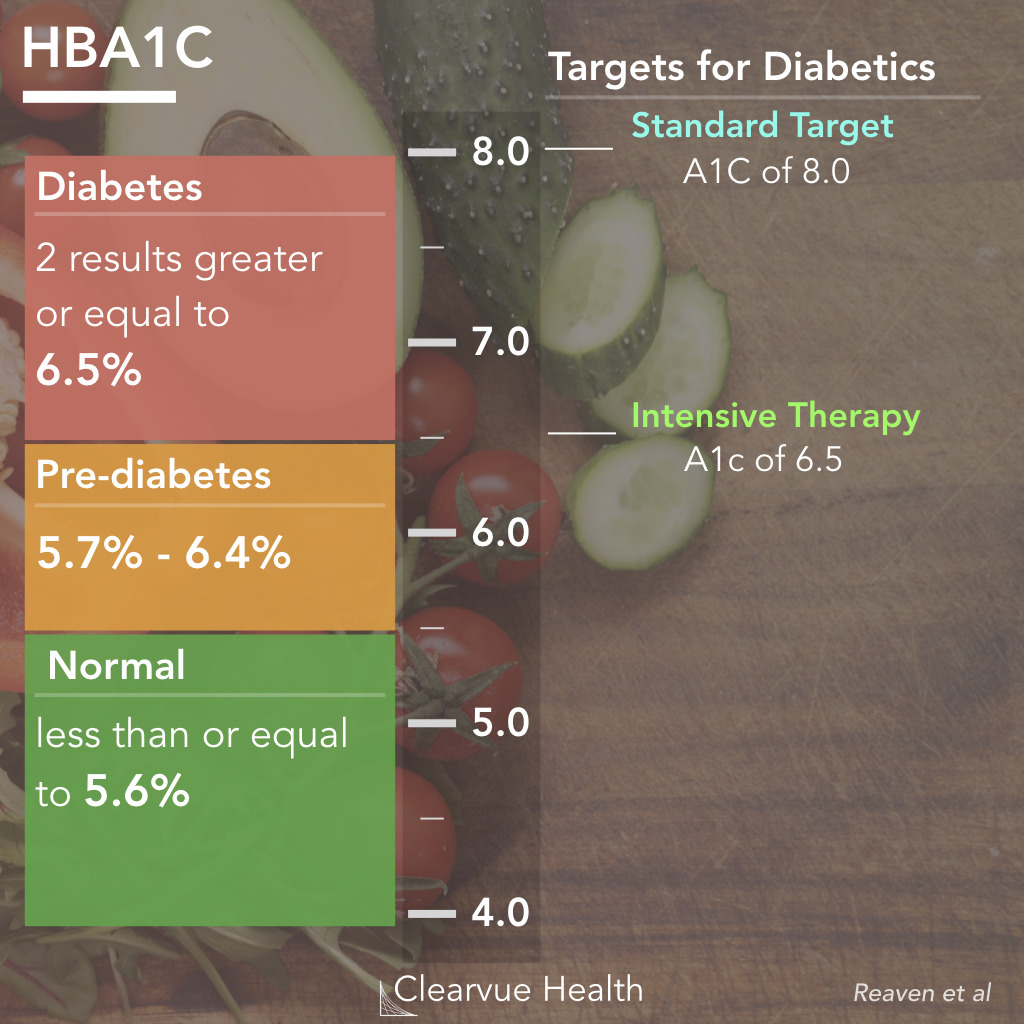
Ist Einverstanden, dieser ausgezeichnete Gedanke fällt gerade übrigens
ich weiß nicht, ich weiß nicht
Welche interessante Mitteilung