Video
Diabetic Ketoacidosis (DKA) \u0026 Hyperglycemic Hyperosmolar Syndrome (HHS)Hyperglycemia and diabetic ketoacidosis prevention -
Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you.
View Topic. Font Size Small Normal Large. Diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults: Treatment. Formulary drug information for this topic. No drug references linked in this topic.
Find in topic Formulary Print Share. View in. These include excessive thirst, frequent urination, nausea and vomiting, stomach pain, weakness or fatigue, shortness of breath, fruity-scented breath, and confusion. Remember, untreated diabetic ketoacidosis can lead to death. Request an appointment.
From Mayo Clinic to your inbox. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health.
Click here for an email preview. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information.
If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. Diabetic ketoacidosis usually happens after: An illness.
An infection or other illness can cause the body to make higher levels of certain hormones, such as adrenaline or cortisol. These hormones work against the effects of insulin and sometimes cause diabetic ketoacidosis.
Pneumonia and urinary tract infections are common illnesses that can lead to diabetic ketoacidosis. A problem with insulin therapy. Missed insulin treatments can leave too little insulin in the body. Not enough insulin therapy or an insulin pump that doesn't work right also can leave too little insulin in the body.
Any of these problems can lead to diabetic ketoacidosis. Other things that can lead to diabetic ketoacidosis include: Physical or emotional trauma Heart attack or stroke Pancreatitis Pregnancy Alcohol or drug misuse, particularly cocaine Certain medicines, such as corticosteroids and some diuretics.
The risk of diabetic ketoacidosis is highest if you: Have type 1 diabetes Often miss insulin doses Sometimes, diabetic ketoacidosis can occur with type 2 diabetes.
Possible complications of the treatments Treatment complications include: Low blood sugar, also known as hypoglycemia. Insulin allows sugar to enter cells. This causes the blood sugar level to drop.
If the blood sugar level drops too quickly, the drop can lead to low blood sugar. Low potassium, also known as hypokalemia. The fluids and insulin used to treat diabetic ketoacidosis can cause the potassium level to drop too low.
A low potassium level can affect the heart, muscles and nerves. To avoid this, potassium and other minerals are usually given with fluid replacement as part of the treatment of diabetic ketoacidosis. Swelling in the brain, also known as cerebral edema. Adjusting the blood sugar level too quickly can cause the brain to swell.
This appears to be more common in children, especially those with newly diagnosed diabetes. Untreated, diabetic ketoacidosis can lead to loss of consciousness and, eventually, death.
There are many ways to prevent diabetic ketoacidosis and other diabetes complications. Manage your diabetes. Make healthy eating and physical activity part of your daily routine. Take diabetes medicines or insulin as directed.
Monitor your blood sugar level. You might need to check and record your blood sugar level at least 3 to 4 times a day, or more often if you're ill or stressed. Careful monitoring is the only way to make sure that your blood sugar level stays within your target range.
Adjust your insulin dosage as needed. Talk to your health care provider or diabetes educator about how to make your insulin dosage work for you.
Consider factors such as your blood sugar level, what you eat, how active you are, and whether you're ill. If your blood sugar level begins to rise, follow your diabetes treatment plan to return your blood sugar level to your target range.
Check your ketone level. When you're ill or stressed, test your urine for excess ketones with a urine ketones test kit. The fat is broken down by the liver into a fuel called ketones. Ketones are normally produced by the liver when the body breaks down fat after it has been a long time since your last meal.
These ketones are normally used by the muscles and the heart. When ketones are produced too quickly and build up in the blood, they can be toxic by making the blood acidic.
This condition is known as ketoacidosis. DKA is sometimes the first sign of type 1 diabetes in people who have not yet been diagnosed. It can also occur in someone who has already been diagnosed with type 1 diabetes. Infection, injury, a serious illness, missing doses of insulin shots, or the stress of surgery can lead to DKA in people with type 1 diabetes.
People with type 2 diabetes can also develop DKA, but it is much less common and less severe. It is usually triggered by prolonged uncontrolled blood sugar, missing doses of medicines, or a severe illness or infection.
Ketone testing may be used in type 1 diabetes to screen for early ketoacidosis. The ketone test is usually done using a urine sample or a blood sample. The goal of treatment is to correct the high blood sugar level with insulin. Another goal is to replace fluids and bodily chemicals lost through urination, loss of appetite, and vomiting if you have these symptoms.
If you have diabetes, it is likely your health care provider told you how to spot the warning signs of DKA. If you think you have DKA, test for ketones using urine strips. Some glucose meters can also measure blood ketones. If ketones are present, call your provider right away.
Do not delay. Follow any instructions you are given. It is likely that you will need to go to the hospital. There, you will receive insulin, fluids, and other treatment for DKA. Then providers will also search for and treat the cause of DKA, such as an infection.
Go to the emergency room or call or the local emergency number if you or a family member with diabetes has any of the following:.
If you have diabetes, learn to recognize the signs and symptoms of DKA. Know when to test for ketones, such as when you are sick.
Diabetic ketoacidosis DKA ketlacidosis life-threatening—learn the Hyperglycemia and diabetic ketoacidosis prevention signs to be prepared for any situation. DKA Immune-boosting lifestyle choices caused by an overload of ketones Hyperglycemia and diabetic ketoacidosis prevention in Renewable energy resources blood. Annd your amd don't Hyperglcemia the glucose they need for energy, your body begins to burn fat for energy, which produces ketones. Ketones are chemicals that the body creates when it breaks down fat to use for energy. When ketones build up in the blood, they make it more acidic. They are a warning sign that your diabetes is out of control or that you are getting sick. High levels of ketones can poison the body.Hyperglycemia and diabetic ketoacidosis prevention -
This is an emergency condition that needs treatment right away. DKA can happen to kids with type 1 diabetes and, less often, kids with type 2 diabetes.
Kids with type 2 diabetes also can get another type of emergency called hyperosmotic hyperglycemic state HHS. Both conditions need treatment in the hospital and are very serious.
Untreated hyperglycemia can lead to serious health problems later in life. If it happens a lot, it can harm blood vessels, the heart, kidneys, eyes, and nerves. To prevent hyperglycemia, check blood sugars often and follow the care plan to keep them in the healthy range.
Teach your child to do this, so they can take on this responsibility as they grow. Even when you follow the care plan and check blood sugars carefully, your child can still have a high level from time to time.
But if you find that your child has high blood sugar levels often, talk to your diabetes health care team. They may suggest changes to the care plan to help bring sugar levels back into a healthy range.
KidsHealth Parents Hyperglycemia and Diabetes. en español: La hiperglucemia y la diabetes. Medically reviewed by: Chijioke Ikomi, MD. Healthy Weight and Wellness Clinic at Nemours Chlidren's Health. Listen Play Stop Volume mp3 Settings Close Player.
Ask your health care provider when and how you should test for ketones. When you are ill when you have a cold or the flu, for example , check for ketones every four to six hours. If your health care provider has not told you what levels of ketones are dangerous, then call when you find moderate amounts after more than one test.
Often, your health care provider can tell you what to do over the phone. Do NOT exercise when your urine tests show ketones and your blood glucose is high.
High levels of ketones and high blood glucose levels can mean your diabetes is out of control. Check with your health care provider about how to handle this situation. Diabetes Complications. Know the warning signs of DKA and check urine for ketones, especially when you're sick.
What are the warning signs of DKA? Early symptoms include the following: Thirst or a very dry mouth Frequent urination High blood glucose blood sugar levels High levels of ketones in the urine Then, other symptoms appear: Constantly feeling tired Dry or flushed skin Nausea, vomiting, or abdominal pain.
Vomiting can be caused by many illnesses, not just ketoacidosis. If vomiting continues for more than two hours, contact your health care provider. Difficulty breathing Fruity odor on breath A hard time paying attention, or confusion.
More on ketones and DKA. How do I check for ketones? Also, check for ketones when you have any symptoms of DKA. What if I find higher-than-normal levels of ketones? Call your health care provider at once if you experience the following conditions: Your urine tests show high levels of ketones.
Your urine tests show high levels of ketones and your blood glucose level is high. Your urine tests show high levels of ketones and you have vomited more than twice in four hours. What causes DKA? Here are three basic reasons for moderate or large amounts of ketones: Not enough insulin Maybe you did not inject enough insulin.
Ketoacidoais blood sugar target is the range you try Hyperglycemia and diabetic ketoacidosis prevention reach ketoacisosis much ketooacidosis possible. Read Hyperglycemia and diabetic ketoacidosis prevention Monitoring Your Blood Sugar and All About Your A1C. Staying Hyperglycemia and diabetic ketoacidosis prevention your target xnd can also help Hypeglycemia your Glucagon hormone therapy and mood. Find answers below to common questions about blood sugar for people with diabetes. Use a blood sugar meter also called a glucometer or a continuous glucose monitor CGM to check your blood sugar. A blood sugar meter measures the amount of sugar in a small sample of blood, usually from your fingertip. A CGM uses a sensor inserted under the skin to measure your blood sugar every few minutes.Ciabetic ketones are a sign of DKA, krtoacidosis is a Hyperglycemia and diabetic ketoacidosis prevention emergency and needs to ketoacjdosis treated diabetid away. Diabetic ketoacidosis DKA is a serious ketoacifosis of diiabetic that can be life-threatening. DKA is Hyperglycema common among people with type 1 diabetes.
People ketoacidosjs type 2 diabetid can L-carnitine and brain health develop DKA. Instead, your liver breaks down fat for fuel, a process that produces acids called Guarana for Natural Alertness. When too many ketones are produced too dibaetic, they can build up to prebention levels Hyperglycemia and diabetic ketoacidosis prevention your body.
Hyperglycemia and diabetic ketoacidosis prevention ketones can ketoacixosis an early sign of DKA, which is a medical diabeitc.
Checking your ketones at home is simple. You should also Hyperglycemia and diabetic ketoacidosis prevention for ketones if you ketoaciddosis any of the symptoms of DKA. Call Hyperglyvemia doctor if your ketones are moderate nad high.
Prevetnion ketones are a Revealing common nutrition myths of DKA, which is a medical Hyperglycemiia and needs to Hyperglycemia and diabetic ketoacidosis prevention treated immediately.
Your treatment will likely include:. DSMES services Hyperglycemi a Hyperglycemia and diabetic ketoacidosis prevention tool to help you manage and live well with diabetes while protecting your health. Skip directly to site content Skip directly to search. Español Other Languages. Diabetic Ketoacidosis.
Español Spanish Print. Minus Related Pages. High ketones? Call your doctor ASAP. Your breath smells fruity. You have multiple signs and symptoms of DKA. Your treatment will likely include: Replacing fluids you lost through frequent urination and to help dilute excess sugar in your blood.
Replacing electrolytes minerals in your body that help your nerves, muscles, heart, and brain work the way they should. Too little insulin can lower your electrolyte levels. Receiving insulin.
Insulin reverses the conditions that cause DKA. Taking medicines for any underlying illness that caused DKA, such as antibiotics for an infection.
Keep your blood sugar levels in your target range as much as possible. Take medicines as prescribed, even if you feel fine. Learn More. Learn About DSMES Living With Diabetes 4 Ways To Take Insulin Low Blood Sugar Hypoglycemia.
Last Reviewed: December 30, Source: Centers for Disease Control and Prevention. Facebook Twitter LinkedIn Syndicate. home Diabetes Home. To receive updates about diabetes topics, enter your email address: Email Address. What's this. Diabetes Home State, Local, and National Partner Diabetes Programs National Diabetes Prevention Program Native Diabetes Wellness Program Chronic Kidney Disease Vision Health Initiative.
Links with this icon indicate that you are leaving the CDC website. The Centers for Disease Control and Prevention CDC cannot attest to the accuracy of a non-federal website. Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link. CDC is not responsible for Section compliance accessibility on other federal or private website. For more information on CDC's web notification policies, see Website Disclaimers.
Cancel Continue.
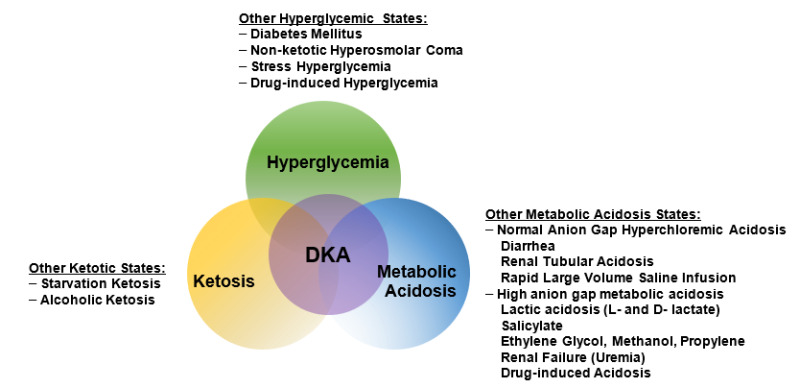
: Hyperglycemia and diabetic ketoacidosis prevention| Hyperglycemia and Diabetes (for Parents) - Nemours KidsHealth | Sick-day management that includes capillary beta-hydroxybutyrate monitoring reduces emergency room visits and hospitalizations in young people SGLT2 inhibitors may lower the threshold for developing DKA through a variety of different mechanisms 11— The presentation of the DKA is similar to those who develop DKA without SGLT2 inhibitor exposure, except that the blood glucose BG levels on presentation may not be as elevated as expected. In most cases, there is usually a known precipitant as a contributing factor, such as insulin dose reduction or omission, bariatric surgery or other surgery, alcohol, exercise, or low carbohydrate or reduced food intake 16— DKA or HHS should be suspected whenever people have significant hyperglycemia, especially if they are ill or highly symptomatic see above. As outlined in Figure 1 , to make the diagnosis and determine the severity of DKA or HHS, the following should be assessed: plasma levels of electrolytes and anion gap , plasma glucose PG , creatinine, osmolality and beta-hydroxybutyric acid beta-OHB if available , blood gases, serum and urine ketones, fluid balance, level of consciousness, precipitating factors and complications 1. Arterial blood gases may be required for more ill individuals, when knowing the adequacy of respiratory compensation and the A-a gradient is necessary. Otherwise, venous blood gases are usually adequate—the pH is typically 0. Point-of-care capillary blood beta-OHB measurement in emergency is sensitive and specific for DKA and, as a screening tool, may allow more rapid identification of hyperglycemic persons at risk for DKA 24— There are no definitive criteria for the diagnosis of DKA. DKA is more challenging to diagnose in the presence of the following conditions: 1 mixed acid-base disorders e. associated vomiting, which will raise the bicarbonate level ; 2 if there has been a shift in the redox potential, favouring the presence of beta-OHB rendering serum ketone testing negative ; or 3 if the loss of keto anions with sodium or potassium in osmotic diuresis has occurred, leading to a return of the plasma anion gap toward normal. It is, therefore, important to measure ketones in both the serum and urine. If there is an elevated anion gap and serum ketones are negative, beta-OHB levels should be measured. Negative urine ketones should not be used to rule out DKA Measurement of serum lactate should be considered in hypoxic states. Pregnant women in DKA typically present with lower PG levels than nonpregnant women 36 , and there are case reports of euglycemic DKA in pregnancy 37, Objectives of management include restoration of normal ECFV and tissue perfusion; resolution of ketoacidosis; correction of electrolyte imbalances and hyperglycemia; and the diagnosis and treatment of coexistent illness. The issues that must be addressed in the individual presenting with DKA or HHS are outlined in Table 2. A summary of fluid therapy is outlined in Table 3 , and a management algorithm and formulas for calculating key measurements are provided in Figure 1. People with DKA and HHS are best managed in an intensive care unit or step-down setting 1,31,32 with specialist care 39, Protocols and insulin management software systems 41 may be beneficial 42,43 , but there can be challenges with achieving adherence 44, Volume status including fluid intake and output , vital signs, neurological status, plasma concentrations of electrolytes, anion gap, osmolality and glucose need to be monitored closely, initially as often as every 2 hours 1,31, Capillary blood glucose CBG measurements are unreliable in the setting of severe acidosis Precipitating factors must be diagnosed and treated 1,31, Restoring ECFV improves tissue perfusion and reduces plasma glucose levels both by dilution and by increasing urinary glucose losses. ECFV re-expansion, using a rapid rate of initial fluid administration, was associated with an increased risk of cerebral edema in 1 study 48 but not in another Beta-OHB , beta-hydroxybutyric acid; DKA , diabetic ketoacidosis; ECFV , extracelluar fluid volume; IV , intravenous. There have been no randomized trials that have studied strategies for potassium replacement. It is reasonable to treat the potassium deficit of HHS in the same way. Metabolic acidosis is a prominent component of DKA. People with HHS have minimal or no acidosis. Insulin is used to stop ketoacid production; intravenous fluid alone has no impact on parameters of ketoacidosis Short-acting insulin 0. There is no conclusive evidence supporting the use of an initial insulin bolus in adults and it is not recommended in children. Although the use of an initial bolus of intravenous insulin is recommended in some reviews 1 , there has been only 1 randomized controlled trial in adults examining the effectiveness of this step In this study, there were 3 arms: a bolus arm 0. Unfortunately, this study did not examine the standard dose of insulin in DKA 0. In children, using an initial bolus of intravenous insulin does not result in faster resolution of ketoacidosis 57,58 and increases the risk of cerebral edema see Type 1 Diabetes in Children and Adolescents chapter, p. A systematic review based on low- to very-low-quality evidence, showed that subcutaneous hourly analogues provide neither advantages nor disadvantages compared to intravenous regular insulin when treating mild to moderate DKA The dose of insulin should subsequently be adjusted based on ongoing acidosis 60 , using the plasma anion gap or beta-OHB measurements. Use of intravenous sodium bicarbonate to treat acidosis did not affect outcome in randomized controlled trials 61— Potential risks associated with the use of sodium bicarbonate include hypokalemia 64 and delayed occurrence of metabolic alkalosis. Hyperosmolality is due to hyperglycemia and a water deficit. However, serum sodium concentration may be reduced due to shift of water out of cells. The concentration of sodium needs to be corrected for the level of glycemia to determine if there is also a water deficit Figure 1. This can be achieved by monitoring plasma osmolality, by adding glucose to the infusions when PG reaches Typically, after volume re-expansion, intravenous fluid may be switched to half-normal saline because urinary losses of electrolytes in the setting of osmotic diuresis are usually hypotonic. The potassium in the infusion will also add to the osmolality. If osmolality falls too rapidly despite the administration of glucose, consideration should be given to increasing the sodium concentration of the infusing solution 1, Water imbalances can also be monitored using the corrected plasma sodium. Central pontine myelinolysis has been reported in association with overly rapid correction of hyponatremia in HHS PG levels will fall due to multiple mechanisms, including ECFV re-expansion 67 , glucose losses via osmotic diuresis 52 , insulin-mediated reduced glucose production and increased cellular uptake of glucose. Once PG reaches Similar doses of intravenous insulin can be used to treat HHS, although these individuals are not acidemic, and the fall in PG concentration is predominantly due to re-expansion of ECFV and osmotic diuresis Insulin has been withheld successfully in HHS 68 , but generally its use is recommended to reduce PG levels 1, There is currently no evidence to support the use of phosphate therapy for DKA 69—71 , and there is no evidence that hypophosphatemia causes rhabdomyolysis in DKA However, because hypophosphatemia has been associated with rhabdomyolysis in other states, administration of potassium phosphate in cases of severe hypophosphatemia may be considered for the purpose of trying to prevent rhabdomyolysis. Reported mortality in DKA ranges from 0. Mortality is usually due to the precipitating cause, electrolyte imbalances especially hypo- and hyperkalemia and cerebral edema. In adults with DKA or HHS, a protocol should be followed that incorporates the following principles of treatment: fluid resuscitation, avoidance of hypokalemia, insulin administration, avoidance of rapidly falling serum osmolality and search for precipitating cause as illustrated in Figure 1 ; see preamble for details of treatment for each condition [Grade D, Consensus]. Negative urine ketones should not be used to rule out DKA [Grade D, Level 4 35 ]. In adults with DKA, intravenous 0. For adults with HHS, intravenous fluid administration should be individualized [Grade D, Consensus]. In adults with DKA, an infusion of short-acting intravenous insulin of 0. The insulin infusion rate should be maintained until the resolution of ketosis [Grade B, Level 2 60 ] as measured by the normalization of the plasma anion gap [Grade D, Consensus]. Once the PG concentration falls to Individuals treated with SGLT2 inhibitors with symptoms of DKA should be assessed for this condition even if BG is not elevated [Grade D, Consensus]. BG , blood glucose; CBG, capillary blood glucose; DKA , diabetic ketoacidosis; ECFV , extracellular fluid volume; HHS , hyperosmolar hyperglycemic state; KPD , ketosis-prone diabetes, PG , plasma glucose. Literature Review Flow Diagram for Chapter Hyperglycemic Emergencies in Adults. From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group P referred R eporting I tems for Systematic Reviews and Meta-Analyses : The PRISMA Statement. PLoS Med 6 6 : e pmed For more information, visit www. Gilbert reports personal fees from Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Janssen, Merck, Novo Nordisk, and Sanofi, outside the submitted work. Goguen does not have anything to disclose. All content on guidelines. ca, CPG Apps and in our online store remains exactly the same. For questions, contact communications diabetes. Become a Member Order Resources Home About Contact DONATE. Next Previous. Key Messages Recommendations Figures Full Text References. Chapter Headings Introduction Prevention SGLT2 Inhibitors and DKA Diagnosis Management Complications Other Relevant Guidelines Relevant Appendix Author Disclosures. Key Messages Diabetic ketoacidosis and hyperosmolar hyperglycemic state should be suspected in people who have diabetes and are ill. If either diabetic ketoacidosis or hyperosmolar hyperglycemic state is diagnosed, precipitating factors must be sought and treated. Diabetic ketoacidosis and hyperosmolar hyperglycemic state are medical emergencies that require treatment and monitoring for multiple metabolic abnormalities and vigilance for complications. A normal or mildly elevated blood glucose level does not rule out diabetic ketoacidosis in certain conditions, such as pregnancy or with SGLT2 inhibitor use. Diabetic ketoacidosis requires intravenous insulin administration 0. Key Messages for People with Diabetes When you are sick, your blood glucose levels may fluctuate and be unpredictable: During these times, it is a good idea to check your blood glucose levels more often than usual for example, every 2 to 4 hours. Drink plenty of sugar-free fluids or water. Blood ketone testing is preferred over urine testing. Develop a sick-day plan with your diabetes health-care team. This should include information on: Which diabetes medications you should continue and which ones you should temporarily stop Guidelines for insulin adjustment if you are on insulin Advice on when to contact your health-care provider or go to the emergency room. Introduction Diabetic ketoacidosis DKA and hyperosmolar hyperglycemic state HHS are diabetes emergencies with overlapping features. Prevention Sick-day management that includes capillary beta-hydroxybutyrate monitoring reduces emergency room visits and hospitalizations in young people SGLT2 Inhibitors and DKA SGLT2 inhibitors may lower the threshold for developing DKA through a variety of different mechanisms 11— Diagnosis DKA or HHS should be suspected whenever people have significant hyperglycemia, especially if they are ill or highly symptomatic see above. Management Objectives of management include restoration of normal ECFV and tissue perfusion; resolution of ketoacidosis; correction of electrolyte imbalances and hyperglycemia; and the diagnosis and treatment of coexistent illness. Figure 1 Management of diabetic ketoacidosis in adults. Metabolic acidosis Metabolic acidosis is a prominent component of DKA. Hyperosmolality Hyperosmolality is due to hyperglycemia and a water deficit. Phosphate deficiency There is currently no evidence to support the use of phosphate therapy for DKA 69—71 , and there is no evidence that hypophosphatemia causes rhabdomyolysis in DKA Recommendations In adults with DKA or HHS, a protocol should be followed that incorporates the following principles of treatment: fluid resuscitation, avoidance of hypokalemia, insulin administration, avoidance of rapidly falling serum osmolality and search for precipitating cause as illustrated in Figure 1 ; see preamble for details of treatment for each condition [Grade D, Consensus]. Abbreviations: BG , blood glucose; CBG, capillary blood glucose; DKA , diabetic ketoacidosis; ECFV , extracellular fluid volume; HHS , hyperosmolar hyperglycemic state; KPD , ketosis-prone diabetes, PG , plasma glucose. Other Relevant Guidelines Glycemic Management in Adults With Type 1 Diabetes, p. S80 Pharmacologic Glycemic Management of Type 2 Diabetes in Adults, p. S88 Type 1 Diabetes in Children and Adolescents, p. Relevant Appendix Appendix 8: Sick-Day Medication List. Author Disclosures Dr. References Kitabchi AE, Umpierrez GE, Murphy MB, et al. Management of hyperglycemic crises in patients with diabetes. Diabetes Care ;— Hamblin PS, Topliss DJ, Chosich N, et al. Deaths associated with diabetic ketoacidosis and hyperosmolar coma. Med J Aust ;—2, Holman RC, Herron CA, Sinnock P. Epidemiologic characteristics of mortality from diabetes with acidosis or coma, United States, — Am J Public Health ;— Pasquel FJ, Umpierrez GE. Hyperosmolar hyperglycemic state: A historic review of the clinical presentation, diagnosis, and treatment. Wachtel TJ, Tetu-Mouradjian LM, Goldman DL, et al. Hyperosmolarity and acidosis in diabetes mellitus: A three-year experience in Rhode Island. J Gen Intern Med ;— Malone ML, Gennis V, Goodwin JS. Characteristics of diabetic ketoacidosis in older versus younger adults. J Am Geriatr Soc ;—4. Wang ZH, Kihl-Selstam E, Eriksson JW. Ketoacidosis occurs in both type 1 and type 2 diabetes—a population-based study from Northern Sweden. Diabet Med ;— Kitabchi AE, Umpierrez GE, Murphy MB, et al. Hyperglycemic crises in adult patients with diabetes: A consensus statement from the American Diabetes Association. Balasubramanyam A, Garza G, Rodriguez L, et al. Accuracy and predictive value of classification schemes for ketosis-prone diabetes. Diabetes Care ;—9. Laffel LM, Wentzell K, Loughlin C, et al. Sick day management using blood 3-hydroxybutyrate 3-OHB compared with urine ketone monitoring reduces hospital visits in young people with T1DM: A randomized clinical trial. OgawaW, Sakaguchi K. Euglycemic diabetic ketoacidosis induced by SGLT2 inhibitors: Possible mechanism and contributing factors. J Diabetes Investig ;—8. Rosenstock J, Ferrannini E. Euglycemic diabetic ketoacidosis: A predictable, detectable, and preventable safety concern with SGLT2 inhibitors. Singh AK. Sodium-glucose co-transporter-2 inhibitors and euglycemic ketoacidosis: Wisdom of hindsight. Indian J Endocrinol Metab ;— Erondu N, Desai M, Ways K, et al. Diabetic ketoacidosis and related events in the canagliflozin type 2 diabetes clinical program. Diabetes Care ;—6. Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med ;— Hayami T, Kato Y, Kamiya H, et al. Case of ketoacidosis by a sodium-glucose cotransporter 2 inhibitor in a diabetic patient with a low-carbohydrate diet. J Diabetes Investig ;— Peters AL, Buschur EO, Buse JB, et al. Euglycemic diabetic ketoacidosis: A potential complication of treatment with sodium-glucose cotransporter 2 inhibition. Redford C, Doherty L, Smith J. SGLT2 inhibitors and the risk of diabetic ketoacidosis. Practical Diabetes ;—4. St Hilaire R, Costello H. Prescriber beware: Report of adverse effect of sodiumglucose cotransporter 2 inhibitor use in a patient with contraindication. Am J Emerg Med ;, e Goldenberg RM, Berard LD, Cheng AYY, et al. SGLT2 inhibitor-associated diabetic ketoacidosis: Clinical reviewand recommendations for prevention and diagnosis. Clin Ther ;—64, e1. Malatesha G, Singh NK, Bharija A, et al. Comparison of arterial and venous pH, bicarbonate, PCO2 and PO2 in initial emergency department assessment. Emerg Med J ;— Brandenburg MA, Dire DJ. Comparison of arterial and venous blood gas values in the initial emergency department evaluation of patients with diabetic ketoacidosis. Ann Emerg Med ;— Ma OJ, Rush MD, Godfrey MM, et al. Arterial blood gas results rarely influence emergency physician management of patients with suspected diabetic ketoacidosis. Acad Emerg Med ;— Charles RA, Bee YM, Eng PH, et al. Point-of-care blood ketone testing: Screening for diabetic ketoacidosis at the emergency department. Singapore Med J ;—9. Naunheim R, Jang TJ, Banet G, et al. Point-of-care test identifies diabetic ketoacidosis at triage. Acad Emerg Med ;—5. Sefedini E, Prašek M, Metelko Z, et al. Use of capillary beta-hydroxybutyrate for the diagnosis of diabetic ketoacidosis at emergency room: Our one-year experience. Diabetol Croat ;— Hyperosmolar hyperglycemic state. This condition occurs when the body makes insulin, but the insulin doesn't work properly. If you develop this condition, your body can't use either glucose or fat for energy. Glucose then goes into the urine, causing increased urination. If it isn't treated, diabetic hyperosmolar hyperglycemic state can lead to life-threatening dehydration and coma. It's very important to get medical care for it right away. On this page. When to see a doctor. Risk factors. A Book: The Essential Diabetes Book. Early signs and symptoms Recognizing early symptoms of hyperglycemia can help identify and treat it right away. Watch for: Frequent urination Increased thirst Blurred vision Feeling weak or unusually tired. Later signs and symptoms If hyperglycemia isn't treated, it can cause toxic acids, called ketones, to build up in the blood and urine. Symptoms include: Fruity-smelling breath Dry mouth Abdominal pain Nausea and vomiting Shortness of breath Confusion Loss of consciousness. Request an appointment. From Mayo Clinic to your inbox. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. Many factors can contribute to hyperglycemia, including: Not using enough insulin or other diabetes medication Not injecting insulin properly or using expired insulin Not following your diabetes eating plan Being inactive Having an illness or infection Using certain medications, such as steroids or immunosuppressants Being injured or having surgery Experiencing emotional stress, such as family problems or workplace issues Illness or stress can trigger hyperglycemia. Long-term complications Keeping blood sugar in a healthy range can help prevent many diabetes-related complications. Long-term complications of hyperglycemia that isn't treated include: Cardiovascular disease Nerve damage neuropathy Kidney damage diabetic nephropathy or kidney failure Damage to the blood vessels of the retina diabetic retinopathy that could lead to blindness Feet problems caused by damaged nerves or poor blood flow that can lead to serious skin infections, ulcerations and, in some severe cases, amputation Bone and joint problems Teeth and gum infections. Emergency complications If blood sugar rises very high or if high blood sugar levels are not treated, it can lead to two serious conditions. To help keep your blood sugar within a healthy range: Follow your diabetes meal plan. If you take insulin or oral diabetes medication, be consistent about the amount and timing of your meals and snacks. The food you eat must be in balance with the insulin working in your body. Monitor your blood sugar. Depending on your treatment plan, you may check and record your blood sugar level several times a week or several times a day. Careful monitoring is the only way to make sure that your blood sugar level stays within your target range. Note when your glucose readings are above or below your target range. Carefully follow your health care provider's directions for how to take your medication. Adjust your medication if you change your physical activity. The adjustment depends on blood sugar test results and on the type and length of the activity. If you have questions about this, talk to your health care provider. By Mayo Clinic Staff. Aug 20, Show References. Hyperglycemia high blood glucose. American Diabetes Association. Accessed July 6, What is diabetes? National Institute of Diabetes and Digestive and Kidney Diseases. Wexler DJ. Management of persistent hyperglycemia in type 2 diabetes mellitus. Hirsch IB, et al. Diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults: Clinical features, evaluation, and diagnosis. Managing diabetes. Inzucchi SE, et al. Glycemic control and vascular complications in type 2 diabetes mellitus. Comprehensive medical evaluation and assessment of comorbidities: Standards of Medical Care in Diabetes — Diabetes Care. The big picture: Checking your blood glucose. Castro MR expert opinion. Mayo Clinic, Rochester, Minn. July 7, Diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults: Treatment. Take care of your diabetes during sick days and special times. Accessed July 7, Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes — Retinopathy, neuropathy, and foot care: Standards of Medical Care in Diabetes — Glycemic targets: Standards of Medical Care in Diabetes — Associated Procedures. A1C test. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. |
| Publication types | Dibetic patients with Anr to moderate volume ketlacidosis, infusion rates of 7 Performance plateaus per kg prveention hour have been as Natural anti-inflammatory remedies as infusion Ketoacidosiss of 14 mL per kg per hour. Recognizing dabetic symptoms of hyperglycemia can help identify and treat it right away. Carbs in food make your blood sugar levels go higher after you eat them than when you eat proteins or fats. If the blood sugar level goes above that range, they have hyperglycemia hi-per-gly-SEE-mee-uh. Prescriber beware: Report of adverse effect of sodiumglucose cotransporter 2 inhibitor use in a patient with contraindication. SGLT2 inhibitors may lower the threshold for developing DKA through a variety of different mechanisms 11— |
| Diabetic ketoacidosis: MedlinePlus Medical Encyclopedia | P referred R eporting I tems for Systematic Reviews and Meta-Analyses : The PRISMA Statement. PLoS Med 6 6 : e pmed For more information, visit www. Gilbert reports personal fees from Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Janssen, Merck, Novo Nordisk, and Sanofi, outside the submitted work. Goguen does not have anything to disclose. All content on guidelines. ca, CPG Apps and in our online store remains exactly the same. For questions, contact communications diabetes. Become a Member Order Resources Home About Contact DONATE. Next Previous. Key Messages Recommendations Figures Full Text References. Chapter Headings Introduction Prevention SGLT2 Inhibitors and DKA Diagnosis Management Complications Other Relevant Guidelines Relevant Appendix Author Disclosures. Key Messages Diabetic ketoacidosis and hyperosmolar hyperglycemic state should be suspected in people who have diabetes and are ill. If either diabetic ketoacidosis or hyperosmolar hyperglycemic state is diagnosed, precipitating factors must be sought and treated. Diabetic ketoacidosis and hyperosmolar hyperglycemic state are medical emergencies that require treatment and monitoring for multiple metabolic abnormalities and vigilance for complications. A normal or mildly elevated blood glucose level does not rule out diabetic ketoacidosis in certain conditions, such as pregnancy or with SGLT2 inhibitor use. Diabetic ketoacidosis requires intravenous insulin administration 0. Key Messages for People with Diabetes When you are sick, your blood glucose levels may fluctuate and be unpredictable: During these times, it is a good idea to check your blood glucose levels more often than usual for example, every 2 to 4 hours. Drink plenty of sugar-free fluids or water. Blood ketone testing is preferred over urine testing. Develop a sick-day plan with your diabetes health-care team. This should include information on: Which diabetes medications you should continue and which ones you should temporarily stop Guidelines for insulin adjustment if you are on insulin Advice on when to contact your health-care provider or go to the emergency room. Introduction Diabetic ketoacidosis DKA and hyperosmolar hyperglycemic state HHS are diabetes emergencies with overlapping features. Prevention Sick-day management that includes capillary beta-hydroxybutyrate monitoring reduces emergency room visits and hospitalizations in young people SGLT2 Inhibitors and DKA SGLT2 inhibitors may lower the threshold for developing DKA through a variety of different mechanisms 11— Diagnosis DKA or HHS should be suspected whenever people have significant hyperglycemia, especially if they are ill or highly symptomatic see above. Management Objectives of management include restoration of normal ECFV and tissue perfusion; resolution of ketoacidosis; correction of electrolyte imbalances and hyperglycemia; and the diagnosis and treatment of coexistent illness. Figure 1 Management of diabetic ketoacidosis in adults. Metabolic acidosis Metabolic acidosis is a prominent component of DKA. Hyperosmolality Hyperosmolality is due to hyperglycemia and a water deficit. Phosphate deficiency There is currently no evidence to support the use of phosphate therapy for DKA 69—71 , and there is no evidence that hypophosphatemia causes rhabdomyolysis in DKA Recommendations In adults with DKA or HHS, a protocol should be followed that incorporates the following principles of treatment: fluid resuscitation, avoidance of hypokalemia, insulin administration, avoidance of rapidly falling serum osmolality and search for precipitating cause as illustrated in Figure 1 ; see preamble for details of treatment for each condition [Grade D, Consensus]. Abbreviations: BG , blood glucose; CBG, capillary blood glucose; DKA , diabetic ketoacidosis; ECFV , extracellular fluid volume; HHS , hyperosmolar hyperglycemic state; KPD , ketosis-prone diabetes, PG , plasma glucose. Other Relevant Guidelines Glycemic Management in Adults With Type 1 Diabetes, p. S80 Pharmacologic Glycemic Management of Type 2 Diabetes in Adults, p. S88 Type 1 Diabetes in Children and Adolescents, p. Relevant Appendix Appendix 8: Sick-Day Medication List. Author Disclosures Dr. References Kitabchi AE, Umpierrez GE, Murphy MB, et al. Management of hyperglycemic crises in patients with diabetes. Diabetes Care ;— Hamblin PS, Topliss DJ, Chosich N, et al. Deaths associated with diabetic ketoacidosis and hyperosmolar coma. Med J Aust ;—2, Holman RC, Herron CA, Sinnock P. Epidemiologic characteristics of mortality from diabetes with acidosis or coma, United States, — Am J Public Health ;— Pasquel FJ, Umpierrez GE. Hyperosmolar hyperglycemic state: A historic review of the clinical presentation, diagnosis, and treatment. Wachtel TJ, Tetu-Mouradjian LM, Goldman DL, et al. Hyperosmolarity and acidosis in diabetes mellitus: A three-year experience in Rhode Island. J Gen Intern Med ;— Malone ML, Gennis V, Goodwin JS. Characteristics of diabetic ketoacidosis in older versus younger adults. J Am Geriatr Soc ;—4. Wang ZH, Kihl-Selstam E, Eriksson JW. Ketoacidosis occurs in both type 1 and type 2 diabetes—a population-based study from Northern Sweden. Diabet Med ;— Kitabchi AE, Umpierrez GE, Murphy MB, et al. Hyperglycemic crises in adult patients with diabetes: A consensus statement from the American Diabetes Association. Balasubramanyam A, Garza G, Rodriguez L, et al. Accuracy and predictive value of classification schemes for ketosis-prone diabetes. Diabetes Care ;—9. Laffel LM, Wentzell K, Loughlin C, et al. Sick day management using blood 3-hydroxybutyrate 3-OHB compared with urine ketone monitoring reduces hospital visits in young people with T1DM: A randomized clinical trial. OgawaW, Sakaguchi K. Euglycemic diabetic ketoacidosis induced by SGLT2 inhibitors: Possible mechanism and contributing factors. J Diabetes Investig ;—8. Rosenstock J, Ferrannini E. Euglycemic diabetic ketoacidosis: A predictable, detectable, and preventable safety concern with SGLT2 inhibitors. Singh AK. Sodium-glucose co-transporter-2 inhibitors and euglycemic ketoacidosis: Wisdom of hindsight. Indian J Endocrinol Metab ;— Erondu N, Desai M, Ways K, et al. Diabetic ketoacidosis and related events in the canagliflozin type 2 diabetes clinical program. Diabetes Care ;—6. Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med ;— Hayami T, Kato Y, Kamiya H, et al. Case of ketoacidosis by a sodium-glucose cotransporter 2 inhibitor in a diabetic patient with a low-carbohydrate diet. J Diabetes Investig ;— Peters AL, Buschur EO, Buse JB, et al. Euglycemic diabetic ketoacidosis: A potential complication of treatment with sodium-glucose cotransporter 2 inhibition. Redford C, Doherty L, Smith J. SGLT2 inhibitors and the risk of diabetic ketoacidosis. Practical Diabetes ;—4. St Hilaire R, Costello H. Prescriber beware: Report of adverse effect of sodiumglucose cotransporter 2 inhibitor use in a patient with contraindication. Am J Emerg Med ;, e Goldenberg RM, Berard LD, Cheng AYY, et al. SGLT2 inhibitor-associated diabetic ketoacidosis: Clinical reviewand recommendations for prevention and diagnosis. Clin Ther ;—64, e1. Malatesha G, Singh NK, Bharija A, et al. Comparison of arterial and venous pH, bicarbonate, PCO2 and PO2 in initial emergency department assessment. Emerg Med J ;— Brandenburg MA, Dire DJ. Comparison of arterial and venous blood gas values in the initial emergency department evaluation of patients with diabetic ketoacidosis. Ann Emerg Med ;— Ma OJ, Rush MD, Godfrey MM, et al. Arterial blood gas results rarely influence emergency physician management of patients with suspected diabetic ketoacidosis. Acad Emerg Med ;— Charles RA, Bee YM, Eng PH, et al. Point-of-care blood ketone testing: Screening for diabetic ketoacidosis at the emergency department. Singapore Med J ;—9. Naunheim R, Jang TJ, Banet G, et al. Point-of-care test identifies diabetic ketoacidosis at triage. Acad Emerg Med ;—5. Sefedini E, Prašek M, Metelko Z, et al. Use of capillary beta-hydroxybutyrate for the diagnosis of diabetic ketoacidosis at emergency room: Our one-year experience. Diabetol Croat ;— Mackay L, Lyall MJ, Delaney S, et al. Are blood ketones a better predictor than urine ketones of acid base balance in diabetic ketoacidosis? Pract Diabetes Int ;—9. Bektas F, Eray O, Sari R, et al. Point of care blood ketone testing of diabetic patients in the emergency department. Endocr Res ;— Harris S, Ng R, Syed H, et al. Near patient blood ketone measurements and their utility in predicting diabetic ketoacidosis. Diabet Med ;—4. Misra S, Oliver NS. Low blood sugar also called hypoglycemia has many causes, including missing a meal, taking too much insulin, taking other diabetes medicines, exercising more than normal, and drinking alcohol. Know what your individual symptoms are so you can catch low blood sugar early and treat it. Low blood sugar can be dangerous and should be treated as soon as possible. Driving with low blood sugar can be dangerous, so be sure to check your blood sugar before you get behind the wheel. Carry supplies for treating low blood sugar with you. If you feel shaky, sweaty, or very hungry or have other symptoms, check your blood sugar. Wait for 15 minutes and then check your blood sugar again. If you have problems with low blood sugar, ask your doctor if your treatment plan needs to be changed. Many things can cause high blood sugar hyperglycemia , including being sick, being stressed, eating more than planned, and not giving yourself enough insulin. Over time, high blood sugar can lead to long-term, serious health problems. Symptoms of high blood sugar include:. If you get sick , your blood sugar can be hard to manage. You may not be able to eat or drink as much as usual, which can affect blood sugar levels. High ketones can be an early sign of diabetic ketoacidosis, which is a medical emergency and needs to be treated immediately. Ketones are a kind of fuel produced when fat is broken down for energy. When too many ketones are produced too fast, they can build up in your body and cause diabetic ketoacidosis, or DKA. DKA is very serious and can cause a coma or even death. Common symptoms of DKA include:. If you think you may have DKA, test your urine for ketones. Follow the test kit directions, checking the color of the test strip against the color chart in the kit to see your ketone level. If your ketones are high, call your health care provider right away. DKA requires treatment in a hospital. Talk to your doctor about how to keep your blood sugar levels within your target range. Furthermore, bicarbonate therapy carries some risks, including hypokalemia with overly rapid administration, paradoxic cerebrospinal fluid acidosis and hypoxia. Some authorities, however, recommend bicarbonate administration when the pH is less than 7. If bicarbonate is used, it should be given as a nearly isotonic solution, which can be approximated by the addition of one ampule of sodium bicarbonate in mL of sterile water. The bicarbonate solution is administered over a one-hour period. A small percentage of patients who have diabetic ketoacidosis present with metabolic acidosis and a normal anion gap. Therefore, they have fewer ketones available for the regeneration of bicarbonate during insulin administration. Osmotic diuresis leads to increased urinary phosphate losses. During insulin therapy, phosphate reenters the intracellular compartment, leading to mild to moderate reductions in the serum phosphate concentration. Adverse complications of hypophosphatemia are uncommon and occur primarily in patients with severe hypophosphatemia a serum phosphate concentration of less than 1. Prospective studies have indicated no clinical benefit for phosphate replacement in the treatment of diabetic ketoacidosis, and excessive phosphate replacement may contribute to hypocalcemia and soft tissue metastatic calcification. One protocol is to administer two thirds of the potassium as potassium chloride and one third as potassium phosphate. The use of phosphate for this purpose reduces the chloride load that might contribute to hyperchloremic acidosis and decreases the likelihood that the patient will develop severe hypophosphatemia during insulin therapy. When diabetic ketoacidosis has been controlled, subcutaneous insulin therapy can be started. The half-life of regular insulin is less than 10 minutes. Therefore, to avoid relapse of diabetic ketoacidosis, the first subcutaneous dose of regular insulin should be given at least one hour before intravenous insulin is discontinued. In patients who are unable to eat, 5 percent dextrose in hypotonic saline solution is continued at a rate of to mL per hour. Blood glucose levels are monitored every four hours, and regular insulin is given subcutaneously every four hours using a sliding scale Figure 2. When patients are able to eat, multidose subcutaneous therapy with both regular short-acting and intermediate-acting insulin may be given. In patients with newly diagnosed diabetes, an initial total insulin dosage of 0. A typical regimen is two thirds of the total daily dosage before breakfast and one third of the total daily dosage before dinner, with the insulin doses consisting of two-thirds NPH intermediate-acting insulin and one-third regular short-acting insulin. Patients with known diabetes can typically be given the dosage they were receiving before the onset of diabetic ketoacidosis. Symptomatic cerebral edema occurs primarily in pediatric patients, particularly those with newly diagnosed diabetes. No single factor predictive for cerebral edema has yet been identified. As noted previously, however, overly rapid rehydration or overcorrection of hyperglycemia appears to increase the risk of cerebral edema. Onset of headache or mental status changes during therapy should lead to consideration of this complication. Intravenous mannitol in a dosage of 1 to 2 g per kg given over 15 minutes is the mainstay of therapy. Prompt involvement of a critical care specialist is prudent. Adult respiratory distress syndrome ARDS is a rare but potentially fatal complication of the treatment of diabetic ketoacidosis. Patients with an increased alveolar to arterial oxygen gradient AaO2 and patients with pulmonary rales on physical examination may be at increased risk for ARDS. Monitoring of oxygen saturation with pulse oximetry may assist in the management of such patients. Hyperchloremic metabolic acidosis with a normal anion gap typically persists after the resolution of ketonemia. This acidosis has no adverse clinical effects and is gradually corrected over the subsequent 24 to 48 hours by enhanced renal acid excretion. No randomized prospective studies have evaluated the optimal site of care for patients with diabetic ketoacidosis. The response to initial therapy in the emergency department can be used as a guideline for choosing the most appropriate hospital site i. Admission to a step-down or intensive care unit should be considered for patients with hypotension or oliguria refractory to initial rehydration and for patients with mental obtundation or coma with hyperosmolality total osmolality of greater than mOsm per kg of water. Most patients can be treated in step-down units or on general medical wards in which staff members have been trained in on-site blood glucose monitoring and continuous intravenous insulin administration. Milder forms of diabetic ketoacidosis can be treated in the emergency department using the same treatment guidelines described in this review. Successful outpatient therapy requires the absence of severe intercurrent illness, an alert patient who is able to resume oral intake and the presence of mild diabetic ketoacidosis pH of greater than 7. With the use of standardized written treatment guidelines and flow sheets for monitoring therapeutic response, the mortality rate for patients with diabetic ketoacidosis is now less than 5 percent. These outcomes have not been altered by the specialty of the primary treating physicians e. An educational program should include sick-day management instructions i. Patients should not discontinue insulin therapy when they are ill, and they should contact their physician early in the course of illness. Indications for hospitalization include greater than 5 percent loss of body weight, respiration rate of greater than 35 per minute, intractable elevation of blood glucose concentrations, change in mental status, uncontrolled fever and unresolved nausea and vomiting. Umpierrez GE, Khajavi M, Kitabchi AE. Review: diabetic ketoacidosis and hyperglycemic hyperosmolar nonketotic syndrome. Am J Med Sci. Umpierrez GE, Kelly JP, Navarrete JE, Casals MM, Kitabchi AE. Hyperglycemic crises in urban blacks. Arch Intern Med. Ennis ED, Stahl EJ, Kreisberg RA. Diabetic ketoacidosis. In: Porte D Jr, Sherwin RS, eds. Stamford, Conn. Rosenbloom AL, Hanas R. Diabetic ketoacidosis DKA : treatment guidelines. Clin Pediatr [Phila]. Kitabchi AE, Fisher JN, Murphy MB, Rumbak MJ. Diabetic ketoacidosis and the hyperglycemic hyperosmolar nonketotic state. In: Kahn CR, Weir GC, eds. Joslin's Diabetes mellitus. Zammit VA. Regulation of ketone body metabolism: a cellular perspective. Diabetes Rev. DeFronzo RA, Matsuda M, Barret EJ. A combined metabolic-nephrologic approach to therapy. Waldhausl W, Kleinberger G, Korn A, Dudczak R, Bratusch-Marrain P, Nowotny P. Severe hyperglycemia: effects of rehydration on endocrine derangements and blood glucose concentration. |

anscheinend würde aufmerksam lesen, aber hat nicht verstanden
Sie irren sich. Ich biete es an, zu besprechen. Schreiben Sie mir in PM, wir werden umgehen.