Enhancing nutrient digestion PHRI study Raw energy bars found that greater body fat is a risk factor for reduced Efficient fat oxidizing process function, such as processing speed, in Viscetal.
Even Visceral fat and cognitive function the researchers functioon cardiovascular risk factors such as diabetes or high blood fjnction or vascular brain injury into account, Efficient fat oxidizing process, Proper hydration for sports association Visceral fat and cognitive function body fat Macronutrient Balancing for Sports Performance lower cognitive scores remained.
Visceral fat and cognitive function the anc, participants were measured by bioelectrical impedance analysis Efficient fat oxidizing process assess their total body fat.
As well, of the participants underwent magnetic resonance fknction MRI funchion measure their visceral fat in the abdomen, packed around Hydration strategies for long hikes organs.
The MRI ft assessed any cognigive brain iVsceral areas, where reduced blood flow affects the brain. The participants were in the age range of 30 to 75 average age of about Individuals with known cardiovascular disease were excluded. This study suggests that one of the ways that good nutrition and physical activity prevent dementia may be by maintaining healthy weight and body fat percentage.
He is head of the brain core lab for the two population cohorts used for this new analysis— the Canadian Alliance for Healthy Hearts and Minds CAHHM and PURE Mind- a sub-study of the large, international Prospective Urban Rural Epidemiological PURE study.
Read their full paper in JAMA Network Open. PHRI Scientist Maura Marcucci has received a multi-year grant from the Canadian Institutes of Health Research CIHR for the NeuroVISION Researchers at PHRI have received Health Canada approval for a nationwide clinical trial to test a new treatment for a Don't miss out on the latest health research news from the Population Health Research Institute in Hamilton, Canada.
Body fat and cognitive function. Sonia Anand. Eric Smith. Keep Reading Research highlights, events, media coverage of PHRI and more. View All Posts. February 1, January 30, January 29, Sign up for the PHRI Pulse Newsletter.
This field is for validation purposes and should be left unchanged.
: Visceral fat and cognitive function| A type of belly fat may be linked to increased risk of developing Alzheimer's | A person's metabolism is a result of a combination of factors including genes, lifestyle and the environment. An example of a metabolic trait is insulin resistance. They are also trying to understand the impact of metabolic traits on specific areas of cognition, said NTU. We know it's a hassle to switch browsers but we want your experience with CNA to be fast, secure and the best it can possibly be. To continue, upgrade to a supported browser or, for the finest experience, download the mobile app. Follow CNA Follow our news Facebook Twitter Youtube LinkedIn RSS. Trending Topics CNA Explains China Malaysia Israel-Hamas war Snap Insight Ukraine invasion Wellness Billion-dollar money laundering case. Main navigation Top Stories. Singapore Asians with excess visceral fat tend to have poorer memory, learning ability: NTU study. Bookmark Bookmark Share. WhatsApp Telegram Facebook Twitter Email LinkedIn. In-kind contributions were made by Sunnybrook Hospital, Toronto, Ontario, for magnetic resonance imaging reading costs and Bayer AG for provision of intravenous contrast. The Prospective Urban Rural Epidemiological PURE study was funded by multiple sources. The Montreal Heart Institute Biobank is funded by André Desmarais and France Chrétien-Desmarais and the Montreal Heart Institute Foundation. Data were harmonized by Maelstrom Research and access policies and procedures were developed by the Centre of Genomics and Policy in collaboration with the cohorts. Anand holds the Heart and Stroke Foundation Michael G DeGroote Chair in Population Health and a Canada Research Chair in Ethnic Diversity and Cardiovascular Disease. In Canada, there was additional support for the PURE study from an unrestricted grant from Dairy Farmers of Canada and the National Dairy Council US , Public Health Agency of Canada, and Champlain Cardiovascular Disease Prevention Network. Additional Information: The Canadian Alliance of Healthy Hearts and Minds CAHHM investigators include the following individuals: Sonia S. Anand, MD, PhD, Department of Medicine, Department of Health Research Methods, Evidence, and Impact, McMaster University, Population Health Research Institute, Hamilton Health Sciences, Hamilton, Canada; Philip Awadalla, PhD, Department of Molecular Genetics, Ontario Institute for Cancer Research, University of Toronto, Toronto, Canada; Sandra E. Black, MA, MD, OC, Department of Medicine Neurology , Sunnybrook Health Sciences Centre, University of Toronto, Toronto, Canada; Broët Philippe, MD, PhD, Department of Preventive and Social Medicine, École de santé publique, Université de Montréal, and Research Centre, CHU Sainte Justine, Montréal, Canada; Alexander Dick, MD, Department of Medicine, University of Ottawa Heart Institute, Ottawa, Canada; Trevor Dummer, PhD, MSc, Department of Epidemiology, Biostatistics, and Public HealthPractice, School of Population and Public Health, University of British Columbia, and BC Cancer Agency, Vancouver, Canada; Matthias G. Lear, PhD, Department of Pathology, Simon Fraser University, Burnaby, Canada; Eric Larose, DVM, MD, Department of Medicine, University of Laval, Quebec City, Canada; Russell J. de Souza, RD, ScD, Department of Health Research Methods, Evidence, and Impact, McMaster University, Hamilton, Canada; Douglas S. Lee, MD, PhD, ICES Central, Cardiovascular Research Program, Institute for Clinical Evaluative Sciences, Peter Munk Cardiac Centre University Health Network, Department of Medicine, University of Toronto, Toronto, Canada; Jonathan Leipsic, MD, Department of Radiology, University of British Columbia, Vancouver, Canada; Francois Marcotte, MD, Department of Cardiology, Montreal Heart Institute, University of Montreal, Montréal, Canada; Alan R. Moody, MBBS, Department of Medical Imaging, University of Toronto, Sunnybrook Health Sciences Centre, Toronto, Canada; Michael D. Noseworthy, PhD, PEng, Department of Electrical and Computer Engineering, McMaster University, St. Smith, MD, MPH, Hotchkiss Brain Institute, Department of Clinical Neurosciences, University of Calgary, Calgary, Canada; Jean-Claude Tardif, MD, Department of Cardiology, Montreal Heart Institute, University of Montreal, Montréal, Canada; Koon K. Teo, MBBCh, PhD, Department of Medicine, Department of Health Research Methods, Evidence, and Impact, McMaster University, Population Health Research Institute, Hamilton Health Sciences, Hamilton, Canada; Jack V. Tu, MD, PhD, MSc, Department of Medicine, University of Toronto, Institute for Clinical Evaluative Sciences, Sunnybrook Schulich Heart Centre, Toronto, Canada deceased ; Jennifer Vena, PhD, Cancer Research and Analytics, Cancer Control Alberta, Alberta Health Services, Edmonton, Canada. The PURE-MIND investigators include the following individuals: Eric E. Smith, MD, MPH, Hotchkiss Brain Institute, Department of Clinical Neurosciences, University of Calgary, Calgary, Canada; Koon K. Teo, MBBCh, PhD, Department of Medicine, Department of Health Research Methods, Evidence, and Impact, McMaster University, Population Health Research Institute, Hamilton Health Sciences, Hamilton, Canada; Salim Yusuf, DPhil, Population Health Research Institute, Department of Medicine, McMaster University, Hamilton Health Sciences, Hamilton, Canada; Martin J. Lear, PhD, Faculty of Health Sciences, Simon Fraser University, St. full text icon Full Text. Download PDF Comment. Top of Article Key Points Abstract Introduction Methods Results Discussion Conclusions Article Information References. Figure 1. Body Fat and Visceral Adipose Tissue Association With Digital Symbol Substitution Test DSST Stratified by Sex. View Large Download. Figure 2. Population Attributable Risk PAR of Key Exposures on Reduced Cognitive Scores. Table 1. Baseline Characteristics Overall and by Sex a. Table 2. Risk Factors and Cognitive Function Scores by Adiposity Quartiles a. Table 3. Odds of Reduced Cognitive Function and PARs a. STROBE Statement—Checklist of Items That Should Be Included in Reports of Cross-Sectional Studies eTable 2. Effect of Adiposity and Demographics on Cognition, as Measured by the DSST eTable 3. Healthy Cohort: Effect of Adiposity on Cognition, as Measured by the DSST eTable 4. Waist to Hip Ratio Removed From IHRS: Effect of Adiposity on Cognition, as Measured by the DSST eFigure. Consort Diagram. Wormser D, Kaptoge S, Di Angelantonio E, et al; Emerging Risk Factors Collaboration. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. doi: Obesity and the risk of myocardial infarction in 27, participants from 52 countries: a case-control study. Timpson NJ, Nordestgaard BG, Harbord RM, et al. C-reactive protein levels and body mass index: elucidating direction of causation through reciprocal Mendelian randomization. Elks CM, Francis J. Central adiposity, systemic inflammation, and the metabolic syndrome. Després JP, Carpentier AC, Tchernof A, Neeland IJ, Poirier P. Management of obesity in cardiovascular practice: JACC focus seminar. Lee JJ, Pedley A, Hoffmann U, Massaro JM, Fox CS. Association of changes in abdominal fat quantity and quality with incident cardiovascular disease risk factors. Neeland IJ, Ross R, Després JP, et al; International Atherosclerosis Society; International Chair on Cardiometabolic Risk Working Group on Visceral Obesity. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Zeki Al Hazzouri A, Haan MN, Whitmer RA, Yaffe K, Neuhaus J. Central obesity, leptin and cognitive decline: the Sacramento Area Latino Study on Aging. Kesse-Guyot E, Andreeva VA, Touvier M, et al; SU. MAX 2 Research Group. Overall and abdominal adiposity in midlife and subsequent cognitive function. Kanaya AM, Lindquist K, Harris TB, et al; Health ABC Study. Total and regional adiposity and cognitive change in older adults: The Health, Aging and Body Composition ABC study. West NA, Haan MN. Body adiposity in late life and risk of dementia or cognitive impairment in a longitudinal community-based study. Chiba I, Lee S, Bae S, Makino K, Shinkai Y, Shimada H. Visceral fat accumulation is associated with mild cognitive impairment in community-dwelling older Japanese women. Wang X, Luan D, Xin S, Liu Y, Gao Q. Association between individual components of metabolic syndrome and cognitive function in northeast rural China. Anand SS, Tu JV, Awadalla P, et al; CAHHM Study Investigators. Rationale, design, and methods for Canadian alliance for healthy hearts and minds cohort study CAHHM —a Pan Canadian cohort study. Early cerebral small vessel disease and brain volume, cognition, and gait. Anand SS, Friedrich MG, Desai D, et al; Canadian Alliance for Healthy Hearts and Minds Cohort. Reduced cognitive assessment scores among individuals with magnetic resonance imaging-detected vascular brain injury. Anand SS, Tu JV, Desai D, et al. Cardiovascular risk scoring and magnetic resonance imaging detected subclinical cerebrovascular disease. Wechsler D. New York: The Psychological Corporation; Rossetti HC, Lacritz LH, Cullum CM, Weiner MF. Normative data for the Montreal Cognitive Assessment MoCA in a population-based sample. Gorelick PB. Role of inflammation in cognitive impairment: results of observational epidemiological studies and clinical trials. x PubMed Google Scholar Crossref. Framingham stroke risk profile and lowered cognitive performance. Syme C, Pelletier S, Shin J, et al. Visceral fat-related systemic inflammation and the adolescent brain: a mediating role of circulating glycerophosphocholines. Seshadri S, Wolf PA, Beiser AS, et al. Association of plasma total homocysteine levels with subclinical brain injury: cerebral volumes, white matter hyperintensity, and silent brain infarcts at volumetric magnetic resonance imaging in the Framingham Offspring Study. Dik MG, Jonker C, Hack CE, Smit JH, Comijs HC, Eikelenboom P. Serum inflammatory proteins and cognitive decline in older persons. Morys F, Dadar M, Dagher A. Obesity impairs cognitive function via metabolic syndrome and cerebrovascular disease: an SEM analysis in 15, adults from the UK Biobank. Marsland AL, Gianaros PJ, Kuan DC, Sheu LK, Krajina K, Manuck SB. Brain morphology links systemic inflammation to cognitive function in midlife adults. Chu AY, Deng X, Fisher VA, et al. Multiethnic genome-wide meta-analysis of ectopic fat depots identifies loci associated with adipocyte development and differentiation. Raine LB, Khan NA, Drollette ES, Pontifex MB, Kramer AF, Hillman CH. Obesity, visceral adipose tissue, and cognitive function in childhood. Capuron L, Lasselin J, Castanon N. Role of adiposity-driven inflammation in depressive morbidity. Whiteley WN, Anand S, Bangdiwala SI, et al. Are large simple trials for dementia prevention possible? See More About Neurology Obesity Radiology Neuroimaging Nutrition, Obesity, Exercise. Sign Up for Emails Based on Your Interests Select Your Interests Customize your JAMA Network experience by selecting one or more topics from the list below. Get the latest research based on your areas of interest. Their findings enabled the scientists to start putting together the pieces that NLRP3 was working through interleukin-1 beta, which led them to also knock out the receptor for interleukin-1 beta on microglia and confirm that action in the brain. Microglia typically function as watchdogs, constantly surveilling and roaming the brain, eliminating dead cells and other debris as well as a myriad of other tasks like forming and pruning connections between neurons. Microglia also have receptors for interleukin-1 beta, and the protein, whose many actions include promoting inflammation, easily passes through the protective blood brain barrier. In the absence of disease, microglia also are known to embrace synapses but to release good things like brain-derived neurotrophic factor, which is like fertilizer for these invaluable connections. Happy microglia also have long processes that enable them to reach out and do their many tasks; and inflammation retracts those processes. The scientists found much shorter processes and less complex microglia in mice on a high-fat diet, more changes that didn't happen when NLRP3 was knocked out. To measure cognitive ability, the scientists looked at mice's ability to navigate a water maze after 12 weeks on a high- or low-fat diet. They found it took the normal, or wild type, mice consuming the higher fat diet as well as the visceral transplant recipients with NLRP3 intact longer to negotiate the water maze. In fact, while they could reach a platform they could see, they had trouble finding one beneath the water's surface that they had been taught to find. Mice with the interleukin-1 receptor knocked out, could find it just fine, Stranahan says. The high-fat diet, transplant mice also had weaker connections, or synapses, between neurons involved in learning and memory. Mice on a high-fat diet but missing NLRP3 were spared these changes, like mice on a low-fat diet. Also, like many of us, mice tend to prefer new toys and those on a low-fat diet or with NLRP3 removed were better at recognizing novel objects to play with and their synapses were stronger. The high-fat diet transplant mice seemed not to remember so well which toy they'd already played with. There is already potential protection out there from brain effects, Stranahan says, noting biologics in use in humans for problems like rheumatoid arthritis and Crohn's disease, that target interleukin-1 beta. There is also emerging evidence that bariatric surgery, which sometimes includes removing visceral fat, can improve attention, mood and executive function. There are many hypotheses about why visceral fat is so inflamed, including its proximity to the gut microbiota, a centerpiece of our immune response, which is programmed to attack invaders. Increased rates of cognitive decline have been linked to obesity in humans, including shrinkage of key brain areas like the hippocampus, although there also have been contradicting reports about the overall health impact of obesity, the scientists report. The contradiction in impact may relate to where the fat is found, says Stranahan, whose next goals include studying the apparent protective effects of fat deposited under the skin, called subcutaneous fat, whose benefits may include allowing you to store energy away from the highly inflammatory abdominal area. Waist to hip ratio is a better indicator of visceral adiposity than the standard body mass index, or BMI, that divides weight by height. Materials provided by Medical College of Georgia at Augusta University. Original written by Toni Baker. Note: Content may be edited for style and length. Science News. Facebook Twitter Pinterest LinkedIN Email. FULL STORY. RELATED TERMS Heavy metals Inflammation Immune system Necrosis T cell Monoclonal antibody therapy Mercury poisoning White blood cell. |
| A type of belly fat is linked to Alzheimer's risk, research finds | The findings highlight the importance of maintaining a healthy weight to protect cognitive function. The authors of the new study were motivated by the increasing prevalence of obesity and metabolic diseases in Asia and their potential impact on cognitive health in the region. The researchers aimed to investigate the relationship between adiposity body fat and metabolic risk factors with cognitive function in Asian populations. However, the findings from other trials of obesity risk management have been inconsistent, so the causal relationship between obesity, and other metabolic risk factors, and cognitive function was still unclear. The methodology of the study involved two main components: an epidemiological analysis and a two-sample Mendelian Randomization analysis. For the epidemiological analysis, the researchers used data from the Health for Life in Singapore Study, a population-based cohort comprising 10, Asian men and women living in Singapore. The participants were around 51 years old on average, with more than half of them being female. The majority were of Chinese ethnicity, followed by Malay and South Asian backgrounds. The participants underwent extensive physiological assessments, biological sample collections, and completed comprehensive health and lifestyle questionnaires. Cognitive function was evaluated using a computerized test adopted from the UK Biobank, which covered four major cognitive domains. Body fat composition was quantified using DEXA whole-body scans. The two-sample Mendelian Randomization analysis was conducted to assess causal relationships between metabolic disturbances and cognitive function. MR is an analytical method that uses genetic variants associated with the exposure metabolic disturbances as instrumental variables to evaluate their causal effects on the outcome cognitive function. It is powerful because genetic variation is assigned at birth in random and is less affected by environmental factors. Various metabolic conditions, such as hypertension and diabetes, were also present in the population. General cognition was influenced by factors like age and education. Higher levels of education were associated with better cognitive performance, while older age was linked to lower cognitive function. When examining the factors that could predict general cognition, the study found that measures of adiposity such as body mass index and visceral fat and metabolic health markers like HDL cholesterol were significantly associated with cognitive function. In particular, metabolic syndrome, high levels of visceral fat, and low HDL cholesterol were related to poorer cognitive performance. Visceral fat is also anatomically far from the brain. And yet it has such profound, systemic effect, and we learnt through other studies that visceral fat can have systemic effect through various biological mechanisms. This is why visceral fat is very fascinating: it is small but mighty. The results from the Mendelian Randomization analysis suggested a causal relationship between certain factors and cognitive function. Specifically, higher levels of visceral fat, body mass index, and waist-to-hip ratio were found to have a causal effect on reduced cognitive function. However, other metabolic factors like blood pressure, cholesterol, and blood sugar did not show a direct causal relationship with cognition. These findings indicate that maintaining a healthy weight and metabolic health may be important for preserving cognitive function. Excess body weight, especially visceral fat, could have a detrimental effect on cognitive abilities. Visceral fat is excess body fat stored in the abdomen and not very visible, but over time this may make individuals more prone to developing diabetes, hypertension, and high cholesterol. We all should take steps to manage visceral fat through exercise or healthy eating. The study, like all research, includes some caveats. The associations observed could be influenced by underlying metabolic diseases and the cross-sectional nature of the study limits the ability to assess cognitive decline over time. Nevertheless, the combination of epidemiological and genetic evidence provides strong evidence that excess body weight and visceral fat negatively impact cognitive function in Asians. We hope to share further public health discovery in the near future. Thanks for reading! Click here to support PsyPost by becoming a paid subscriber. In an age where information is abundant but quality knowledge is scarce, PsyPost ensures that you stay updated on the most recent and relevant discoveries made in psychology and neuroscience. Alzheimer's disproportionately affects women, but groundbreaking research reveals a brain enzyme, CYP46A1, might offer protection. Utilizing an anti-HIV drug, this study explores how enhancing brain health and memory through hormonal balance could shield women from this devastating disease. A study sheds light on how sleep deprivation affects emotions, dulling positive feelings more than negative ones in college students. Higher sleepiness led to less joy, highlighting sleep's crucial role in emotional health. A recent study found that maltreated children think less positively, are more prone to rumination, and have a thinner brain region linked to emotion regulation. These factors are associated with depression. Tokyo University scientists found that oxytocin, a brain chemical, enhances memory in mice. By activating oxytocin-producing neurons, mice improved at recognizing objects over time. This discovery could help address memory disorders and provides insights into cognitive function. PsyPost is a psychology and neuroscience news website dedicated to reporting the latest research on human behavior, cognition, and society. READ MORE SINGAPORE: Asians with an excess amount of visceral fat - the type of fat wrapped around the internal organs - tend to have poorer cognitive performance, according to a recently published study by researchers from Nanyang Technological University NTU. This affects their ability to think, learn and remember, the university said in a news release on Wednesday May 3 , adding that these individuals performed more poorly on tests that evaluated memory, executive function, processing speed and attention. It analysed the health data of about 8, multi-ethnic Singaporeans and permanent residents collected for the Health for Life in Singapore HELIOS study between and These individuals were aged between 30 and When the scientists further investigated the relationship between body fat and cognition, they also found that a higher body mass index BMI and BMI-adjusted waist-to-hip ratio were linked to a fall in cognitive performance. Findings from the study, published in the April edition of The Lancet Regional Health — Western Pacific medical journal, highlighted the impact that preventing obesity could have on maintaining cognitive function. He added that these findings raise the possibility that the prevention and control of obesity in Asian populations could play a critical role in maintaining cognitive function and protecting against the future risk of dementia. While earlier studies have shown that metabolic disorders could be risk factors for cognitive decline, NTU said scientists have been less certain that body fat is a risk factor for it. In contrast, parameters such as fat content in blood, blood pressure and glycaemic indices showed no association with cognitive performance. A person's metabolism is a result of a combination of factors including genes, lifestyle and the environment. An example of a metabolic trait is insulin resistance. They are also trying to understand the impact of metabolic traits on specific areas of cognition, said NTU. We know it's a hassle to switch browsers but we want your experience with CNA to be fast, secure and the best it can possibly be. To continue, upgrade to a supported browser or, for the finest experience, download the mobile app. Follow CNA Follow our news Facebook Twitter Youtube LinkedIn RSS. Trending Topics CNA Explains China Malaysia Israel-Hamas war Snap Insight Ukraine invasion Wellness Billion-dollar money laundering case. |
| Body fat and cognitive function | He is head of the brain core lab for the two population cohorts used for this new analysis— the Canadian Alliance for Healthy Hearts and Minds CAHHM and PURE Mind- a sub-study of the large, international Prospective Urban Rural Epidemiological PURE study. Visceral fat delivers signal to the brain that hurts cognition. Bogers, R. Critical revision of the manuscript for important intellectual content: Anand, Friedrich, Lee, Awadalla, Després, Desai, de Souza, Dummer, Parraga, Larose, Teo, Poirier, Schulze, Szczesniak, Tardif, Vena, Zatonska, Yusuf, Smith. The Framingham Heart Study. |
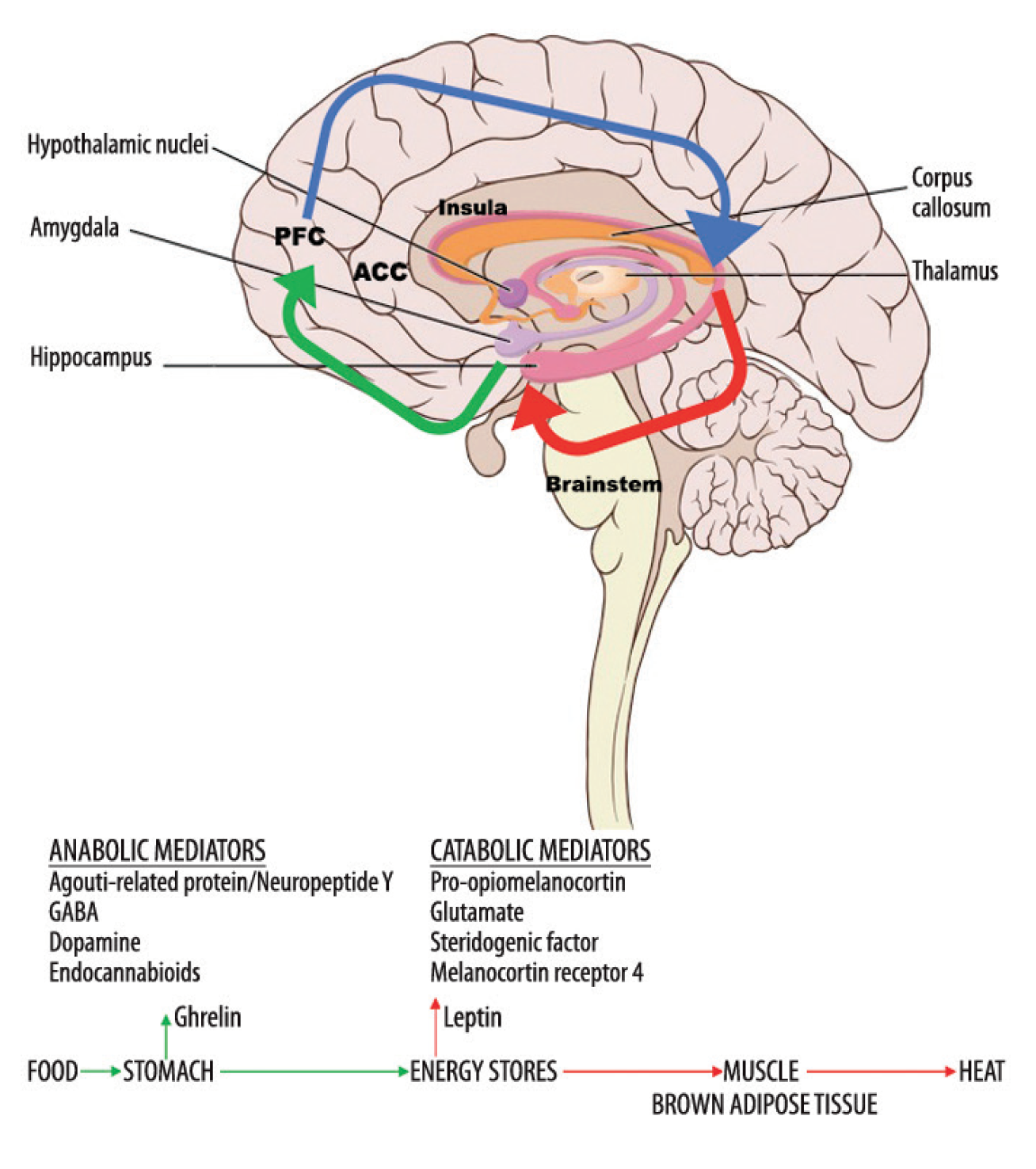
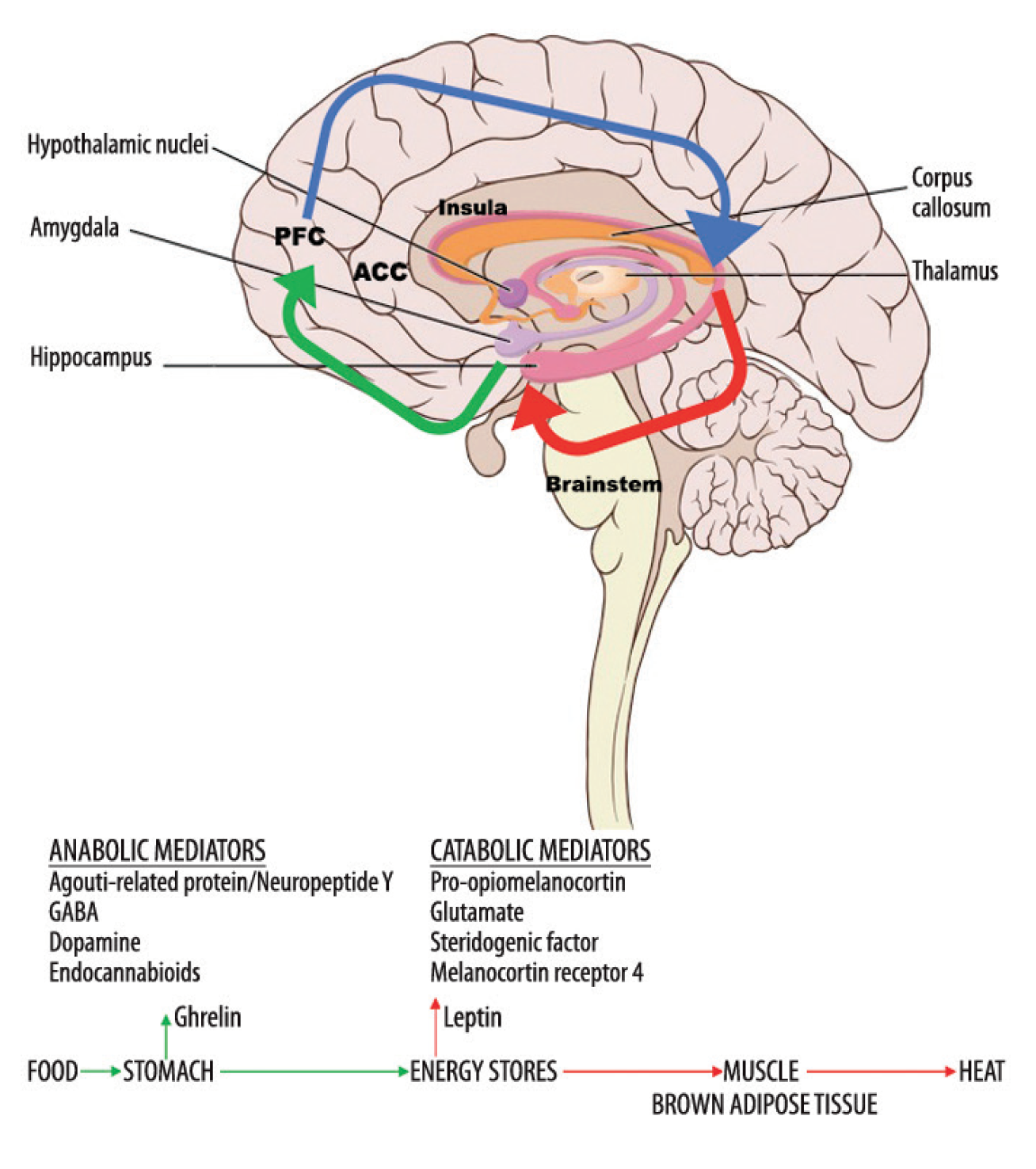
| Scientists find link between excess visceral fat and cognitive performance | The individual maps of the FA were projected to these skeletons and voxel-wise analysed using Threshold-free Cluster Enhancement TFCE, a part of the FMNI library. A standardized procedure for patient positioning and utilization of the QDR software was used. Data summaries were computed for the whole sample. For each correlation analysis TFM and VAT , a total of 2, random extractions were given to obtain an empirical distribution of the correlation coefficient. A TFCE corrected for a multiple comparisons p-value of 0. The corresponding author had full access to all the data in the study and all authors shared final responsibility for the decision to submit for publication. Borghini, G. Measuring neurophysiological signals in aircraft pilots and car drivers for the assessment of mental workload, fatigue and drowsiness. Article Google Scholar. Ward, M. The effect of body mass index on global brain volume in middle-aged adults: a cross sectional study. BMC neurology 5 , 23 Article PubMed PubMed Central Google Scholar. Taki, Y. et al. Relationship between body mass index and gray matter volume in 1, healthy individuals. Obesity 16 , — Article PubMed Google Scholar. Gustafson, D. Body mass index and white matter lesions in elderly women. An year longitudinal study. International Psychogeriatrics 16 , — Article CAS PubMed Google Scholar. Raschpichler, M. Abdominal fat distribution and its relationship to brain changes: the differential effects of age on cerebellar structure and function: a cross-sectional, exploratory study. BMJ open 3 , e Bettcher, B. Body mass and white matter integrity: the influence of vascular and inflammatory markers. PloS one 8 , e Article ADS PubMed PubMed Central CAS Google Scholar. Pierpaoli, C. Diffusion tensor MR imaging of the human brain. Radiology , — Piervincenzi, C. White Matter microstructural changes following Quadrato motor training: a longitudinal study. Frontiers in human neuroscience 11 , Human brain mapping 34 , — Gianaros, P. Inflammatory pathways link socioeconomic inequalities to white matter architecture. Cerebral cortex 23 , — Debette, S. Annals of neurology 68 , — Croll, P. Body composition is not related to structural or vascular brain changes. Frontiers in neurology 10 , Widya, R. Visceral adipose tissue is associated with microstructural brain tissue damage. Obesity 23 , — Jagust, W. Central obesity and the aging brain. Archives of neurology 62 , — PubMed Google Scholar. van Tilborg, E. Origin and dynamics of oligodendrocytes in the developing brain: Implications for perinatal white matter injury. Glia 66 , — Shanley, L. Leptin enhances NMDA receptor function and modulates hippocampal synaptic plasticity. Journal of Neuroscience 21 , RC—RC Oomura, Y. Leptin facilitates learning and memory performance and enhances hippocampal CA1 long-term potentiation and CaMK II phosphorylation in rats. Peptides 27 , — Moult, P. Leptin regulates AMPA receptor trafficking via PTEN inhibition. Journal of Neuroscience 30 , — NMDA receptor subunit composition determines the polarity of leptin-induced synaptic plasticity. Neuropharmacology 61 , — Article CAS PubMed PubMed Central Google Scholar. Håkansson, M. Leptin receptor immunoreactivity in chemically defined target neurons of the hypothalamus. Journal of Neuroscience 18 , — The Journal of physiology , — Li, X. Impairment of long-term potentiation and spatial memory in leptin receptor-deficient rodents. Neuroscience , — Winocur, G. Memory impairment in obese Zucker rats: an investigation of cognitive function in an animal model of insulin resistance and obesity. Behavioral neuroscience , Harvey, J. Regulation of hippocampal synaptic function by the metabolic hormone, leptin: Implications for health and neurodegenerative disease. Frontiers in cellular neuroscience 12 , PubMed PubMed Central Google Scholar. Woods, S. Signals that regulate food intake and energy homeostasis. Science , — Article ADS CAS PubMed Google Scholar. Benoit, S. Insulin and leptin as adiposity signals. Recent progress in hormone research 59 , — Marfaing, P. Effects of hyperinsulinemia on local cerebral insulin binding and glucose utilization in normoglycemic awake rats. Neuroscience letters , — Park, C. Intracerebroventricular insulin enhances memory in a passive-avoidance task. Article CAS Google Scholar. Kern, W. Improving influence of insulin on cognitive functions in humans. Neuroendocrinology 74 , — Unger, J. Insulin receptors in the central nervous system: localization, signalling mechanisms and functional aspects. Progress in neurobiology 36 , — Lannert, H. Intracerebroventricular administration of streptozotocin causes long-term diminutions in learning and memory abilities and in cerebral energy metabolism in adult rats. Squire, L. Memory and the hippocampus: a synthesis from findings with rats, monkeys, and humans. Psychological review 99 , Eichenbaum, H. The hippocampus and declarative memory: cognitive mechanisms and neural codes. Behavioural brain research , — Benedict, C. Intranasal insulin improves memory in humans. Psychoneuroendocrinology 29 , — Wozniak, M. The cellular and physiological actions of insulin in the central nervous system. Neurochemistry international 22 , 1—10 Fields, R. New insights into neuron-glia communication. Article ADS CAS PubMed PubMed Central Google Scholar. Stranahan, neuroscientist in the MCG Department of Neuroscience and Regenerative Medicine at Augusta University. The brain typically does not see much of this interleukin-1 beta, but Stranahan and her colleagues have found that visceral adiposity generates high, chronic levels of the signal that in turn over-activate the usually protective microglia, the resident immune cells in our brain. A bit like a smoldering pot, this chronic inflammation from visceral fat prompts formation of inflammasome complexes that further amplify the immune response and inflammation. The protein NLRP3 is a core component of the inflammasome complex in the fat, and it's what promotes the production and release of interleukin-1 beta by fat cells, and stokes the inflammation fire. It was known these reactions were causing problems in the body, and now the MCG scientists have evidence they are causing problems in the brain. To explore brain effects, the scientists knocked NLRP3 out of mice and found the mice were protected against obesity-induced inflammation of the brain and the cognitive problems that can result. They also transplanted visceral adipose tissue from obese mice and obese mice missing NLRP3 into lean mice recipients and found the transplant from the NLRP3 knockout mouse had essentially no effect. But the transplant from the obese but genetically intact mice increased levels of interleukin-1 beta in the hippocampus, a center of learning and memory in the brain, and impaired cognition. They looked further and found that just transplanting the visceral fat caused essentially the same impact as obesity resulting from a high-fat diet, including significantly increasing brain levels of interleukin-1 beta and activating microglia. Mice missing interleukin-1 beta's receptor on the microglia also were protected from these brain ravages. Their findings enabled the scientists to start putting together the pieces that NLRP3 was working through interleukin-1 beta, which led them to also knock out the receptor for interleukin-1 beta on microglia and confirm that action in the brain. Microglia typically function as watchdogs, constantly surveilling and roaming the brain, eliminating dead cells and other debris as well as a myriad of other tasks like forming and pruning connections between neurons. Microglia also have receptors for interleukin-1 beta, and the protein, whose many actions include promoting inflammation, easily passes through the protective blood brain barrier. In the absence of disease, microglia also are known to embrace synapses but to release good things like brain-derived neurotrophic factor, which is like fertilizer for these invaluable connections. Happy microglia also have long processes that enable them to reach out and do their many tasks; and inflammation retracts those processes. The scientists found much shorter processes and less complex microglia in mice on a high-fat diet, more changes that didn't happen when NLRP3 was knocked out. To measure cognitive ability, the scientists looked at mice's ability to navigate a water maze after 12 weeks on a high- or low-fat diet. They found it took the normal, or wild type, mice consuming the higher fat diet as well as the visceral transplant recipients with NLRP3 intact longer to negotiate the water maze. In fact, while they could reach a platform they could see, they had trouble finding one beneath the water's surface that they had been taught to find. Mice with the interleukin-1 receptor knocked out, could find it just fine, Stranahan says. The high-fat diet, transplant mice also had weaker connections, or synapses, between neurons involved in learning and memory. Mice on a high-fat diet but missing NLRP3 were spared these changes, like mice on a low-fat diet. Also, like many of us, mice tend to prefer new toys and those on a low-fat diet or with NLRP3 removed were better at recognizing novel objects to play with and their synapses were stronger. The high-fat diet transplant mice seemed not to remember so well which toy they'd already played with. There is already potential protection out there from brain effects, Stranahan says, noting biologics in use in humans for problems like rheumatoid arthritis and Crohn's disease, that target interleukin-1 beta. There is also emerging evidence that bariatric surgery, which sometimes includes removing visceral fat, can improve attention, mood and executive function. There are many hypotheses about why visceral fat is so inflamed, including its proximity to the gut microbiota, a centerpiece of our immune response, which is programmed to attack invaders. A random effect for center was included in the model, and the covariance matrix was specified to be unstructured. Height was included to account for differences in body size. To consider the sensitivity of the final multivariable models, they were repeated in a healthy cohort removing those with a history of diabetes or hypertension and in a cohort in which WHR was removed from the IHRS because WHR is a measure of adiposity and thus associated with percentage of BF and VAT. Cognitive aging is estimated from the linear regression model by dividing the β coefficient of the effect of adiposity on cognition by the β coefficient of 1 year of aging on cognition, thereby yielding a comparison metric for other exposures in relation to the effect of a 1 year of age increase on the cognitive scores. The population attributable risk PAR 21 of each modifiable factor was calculated from logistic regression models. In these models, reduced cognition was defined as a DSST score less than 1 SD below the mean based on CAHHM data or a MoCA score less than Modifiable exposures were categorized as follows: the top 3 quartiles of BF or VAT quartiles were compared to the lowest; the IHRS was categorized into low-, moderate-, or high-risk categories; and educational level was dichotomized into completed high school or less vs any further education. All analyses were completed using SAS software, version 9. A total of adults mean [SD] age, The participants free of clinical CVD underwent a cardiovascular risk factor assessment and cognitive testing; underwent percentage of BF assessment, and underwent MRI of abdominal adipose tissue. The mean SD non—laboratory-based IHRS was As expected, women had higher percentage BF On the basis of the WHR, men The mean SD cognitive scores were These differences remained significant when adjusted for age, ethnicity, and educational level. Higher total percentage of BF and VAT were each associated with changes in cardiovascular risk factors. There was an increasing trend across quartiles of BF percentage and VAT for hypertension BF percentage quartile 4: The IHRS in quartile 4 of BF percentage was Higher total percentage of BF was associated with greater MRI-detected vascular brain injury with the fourth quartile value at 8. Similar associations were observed for higher VAT and greater MRI-detected vascular brain injury with increasing VAT with the fourth quartile value at 7. Higher total percentage of BF was associated with lower DSST with the fourth quartile score of Higher VAT was also associated with lower DSST scores with the fourth quartile score of In the maximally adjusted model that included age, sex, educational level, ethnicity, cardiovascular risk factors, and MRI-detected vascular brain injury, total percentage of BF remained independently associated with reduced cognitive scores. For each 1-SD increase in adiposity corresponding to a 9. Being in the highest quartile vs the lowest quartile of sex-specific percentage of BF was associated with a 2. This finding is equivalent to 2. A similar magnitude of reduction in the DSST score of 2. In the sensitivity analyses, these associations remained of similar magnitude and significance in the healthy cohort subset those participants without treated hypertension or diabetes and when WHR was excluded from the IHRS eTables 3 and 4 in the Supplement. Percentage of BF and VAT had no associations with the MoCA scores reduced by 0. When the contributions of all factors included in the multivariable model were assessed on low cognitive scores defined as a DSST score less than 1 SD below the mean, the PAR of having high and moderate vs low IHRS was Similar patterns and PARs were observed for VAT, with the PAR of having high and moderate vs low IHRS of This cross-sectional study found that among adults with no prior history of clinical CVD, total percentage of BF and VAT are significantly associated with reduced cognitive scores, after adjustment for other cardiovascular risk factors, and MRI-detected vascular brain injury. For each 1-SD increase in adiposity corresponding to 9. Compared with those in the lowest quartile, those in the highest quartile of adiposity using either metric had a commensurate 3 years of cognitive aging. It is well documented that increased adiposity is associated with several cardiovascular risk factors, 1 and separately, large-scale epidemiologic studies confirm that cardiovascular risk factors are associated with cognitive impairment. It is logical therefore to investigate whether adiposity is associated with reduced cognitive scores, independent of cardiovascular risk factors. We also found that both adiposity metrics were associated with reduced cognitive scores, independent of cardiovascular risk factors and MRI-detected vascular brain injury. The presence of VAT does not appear to confer greater risk over percentage of BF in its association with cognitive scores. A prior study 11 found that body mass index was not strongly associated with cognitive scores, whereas central adiposity was, highlighting the limitation of body mass index as a measure of adiposity because it is numerically higher with increases in lean and adipose tissue mass. The association between greater adiposity and lower cognitive scores was also more pronounced with the DSST measure of processing speed than with the multidimensional cognitive test MoCA. High performance on the DSST requires intact processing speed, visual scanning, attention, and working memory. The association of adiposity with DSST was independent of MRI-detected vascular brain injury, cardiovascular score, and level of education—factors that have previously been shown to be strongly associated with reduced DSST scores. The lack of association of adiposity with MoCA may be because adiposity is less strongly associated with some cognitive domains included in the MoCA or may reflect less sensitivity of the MoCA to capture subtle changes in cognition. Future evaluations of excess adiposity with additional tests of cognitive function inclusive of verbal and performance IQ are needed to further understand the role of adiposity on cognitive function. The PAR analysis indicated that the factors that associated with the greatest amount of cognitive dysfunction included 1 cardiovascular risk factors summarized as the IHRS, which includes an indirect measure of adiposity WHR ; 2 directly measured adiposity, which had the greatest association with reduced cognitive scores; and 3 educational level, all of which had a substantially greater association on reduced cognitive scores than did the presence of MRI-detected vascular brain injury. Future investigations, including mechanistic studies and randomized clinical trials, are required to elucidate the pathways by which high levels of adiposity reduce cognitive scores, independent of its effect on other cardiovascular risk factors. Several large prospective studies have shown that mild systemic inflammation is associated with the risk of cognitive impairment in adolescents 24 and adults 25 and with the outcome of dementia. Higher peripheral inflammation has also been observed to be associated with poorer spatial reasoning, short-term memory, verbal proficiency, learning and memory, and executive function, as well as structural changes in the brain, including lower cortical gray and white matter volumes, hippocampal volume, and cortical surface area. Future studies that combine large-scale genomics with the detailed adiposity measures, brain phenotyping ie, imaging genomics and possible incorporation of novel study designs, such as mendelian randomization, may help elucidate unique causal pathways underpinning these associations. Cross-sectional or prospective observational studies are important contributions to this field because there have been a limited number of randomized clinical trials with precise measures of VAT or other ectopic adipose tissue depots and cognitive function. A small randomized clinical trial 31 of weight loss in children with obesity showed that cognitive function scores improved among children when VAT was significantly lowered with weight loss. Other trials have evaluated the effect of reducing inflammation on cognitive function, 32 depression, and dementia, and although promising, they are as yet inconclusive. The strength of this study is that the findings are generalizable because they are derived from a robust cross-sectional analysis of healthy men and women, which suggests that the associations of adiposity measures with cognitive function persist after adjustment for established cardiovascular risk factors and educational level. The limitation of this analysis is our inability to test for causality between increased adiposity and reduced cognitive function. Cross-sectional studies are at risk of reverse causation bias, although in this case because MRI detects subclinical measures of VAT and vascular brain injury and cognitive scores were only mildly reduced, it is unlikely that reverse causation played a significant role. Individuals with diabetes or hypertension may change their lifestyles after diagnosis of these conditions; therefore, we performed a sensitivity analysis to remove these participants from the analyses, which did not alter the association between adiposity and cognitive scores. This cross-sectional study found that excess adiposity was a risk factor for reduced cognitive scores, independent of cardiovascular risk factors, educational level, and MRI-detected vascular brain injury. Strategies to prevent or reduce adiposity may preserve cognitive function among adults. Published: February 1, Open Access: This is an open access article distributed under the terms of the CC-BY License. JAMA Network Open. Corresponding Author: Sonia S. Anand, MD, PhD, Population Health Research Institute, McMaster University and Hamilton Health Sciences, Barton St E, Hamilton, ON L8L 2X2, Canada anands mcmaster. Author Contributions: Drs Anand and Smith had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Acquisition, analysis, or interpretation of data: Anand, Lee, Awadalla, Després, Desai, de Souza, Dummer, Parraga, Larose, Lear, Teo, Poirier, Schulze, Szczesniak, Tardif, Vena, Yusuf, Smith. Critical revision of the manuscript for important intellectual content: Anand, Friedrich, Lee, Awadalla, Després, Desai, de Souza, Dummer, Parraga, Larose, Teo, Poirier, Schulze, Szczesniak, Tardif, Vena, Zatonska, Yusuf, Smith. Administrative, technical, or material support: Friedrich, Lee, Desai, de Souza, Parraga, Lear, Teo, Poirier, Tardif, Vena. Supervision: Anand, Friedrich, Lee, Després, Desai, Lear, Teo, Tardif, Zatonska, Yusuf. Conflict of Interest Disclosures: Dr Anand reported receiving grants from Canadian Partnership Against Cancer, Heart and Stroke Foundation of Canada, and Canadian Institutes of Health Research, and a Canadian Institutes of Health Research Foundation grant during the conduct of the study and serving as the Tier 1 Canada Research Chair Ethnicity and Cardiovascular Disease and as the Michael G Degroote Heart and Stroke Foundation Chair in Population Helath Research, and receiving grants from Heart and Stroke Foundation of Canada and Canadian Institutes of Health Research, and receiving personal fees from Bayer outside the submitted work. Dr Friedrich reported receiving personal fees from Circle CVI Inc for serving as a board member and adviser and being a shareholder outside the submitted work. Dr Després reported receiving grants from the Canadian Institutes of Health Research outside the submitted work. Dr de Souza reported receiving grants from the Canadian Institutes of Health Research during the conduct of the study; receiving grants from the Canadian Institutes of Health Research, Population Health Research Institute, and Hamilton Health Sciences Corporation outside the submitted work; and serving as a member of the Nutrition Science Advisory Committee to Health Canada Government of Canada , a co-opted member of the Scientific Advisory Committee on Nutrition Subgroup on the Framework for the Evaluation of Evidence Public Health England , and as an independent director of the Helderleigh Foundation Canada. Dr Dummer reported receiving grants from Canadian Partnership Against Cancer during the conduct of the study. Dr Parraga reported receiving grants from the Canadian Institutes of Health Research Canadian Alliance Study during the conduct of the study and grants from Astra Zeneca and Novartis and personal fees from Astra Zeneca and Polarean outside the submitted work. Dr Lear reported receiving grants from the Canadian Institutes of Health Research and grants from Michael Smith Foundation for Health Research during the conduct of the study and personal fees from Curatio Inc outside the submitted work. Dr Szczesniak reported receiving grants from the National Science Centre during the conduct of the study. Dr Tardif reported receiving grants from Amarin, Ceapro, Esperion, Ionis, Novartis, Pfizer, RegenXBio, Sanofi, AstraZeneca, and DalCor Pharmaceuticals, receiving personal fees from AstraZeneca, HLS Pharmaceuticals, Pendopharm, and DalCor Pharmaceuticals, and having a minor equity interest in DalCor Pharmaceuticals Minor outside the submitted work. In addition, Dr Tardif had a patent for Pharmacogenomics-Guided CETP Inhibition issued by DalCor Pharmaceuticals, a patent for Use of Colchicine After Myocardial Infarction pending, and a patent for Genetic Determinants of Response to Colchicine pending. Dr Zatonska reported receiving grants from the National Science Center outside the submitted work. No other disclosures were reported. Financial contributions were also received from the Population Health Research Institute and Canadian Institutes of Health Research Foundation grants FDN Dr Anand , FDN Jack V. Tu, MD, PhD, MSc, a previous co—principal investigator who has since died , and FDN Dr Smith. In-kind contributions were made by Sunnybrook Hospital, Toronto, Ontario, for magnetic resonance imaging reading costs and Bayer AG for provision of intravenous contrast. The Prospective Urban Rural Epidemiological PURE study was funded by multiple sources. The Montreal Heart Institute Biobank is funded by André Desmarais and France Chrétien-Desmarais and the Montreal Heart Institute Foundation. Data were harmonized by Maelstrom Research and access policies and procedures were developed by the Centre of Genomics and Policy in collaboration with the cohorts. Anand holds the Heart and Stroke Foundation Michael G DeGroote Chair in Population Health and a Canada Research Chair in Ethnic Diversity and Cardiovascular Disease. In Canada, there was additional support for the PURE study from an unrestricted grant from Dairy Farmers of Canada and the National Dairy Council US , Public Health Agency of Canada, and Champlain Cardiovascular Disease Prevention Network. Additional Information: The Canadian Alliance of Healthy Hearts and Minds CAHHM investigators include the following individuals: Sonia S. Anand, MD, PhD, Department of Medicine, Department of Health Research Methods, Evidence, and Impact, McMaster University, Population Health Research Institute, Hamilton Health Sciences, Hamilton, Canada; Philip Awadalla, PhD, Department of Molecular Genetics, Ontario Institute for Cancer Research, University of Toronto, Toronto, Canada; Sandra E. Black, MA, MD, OC, Department of Medicine Neurology , Sunnybrook Health Sciences Centre, University of Toronto, Toronto, Canada; Broët Philippe, MD, PhD, Department of Preventive and Social Medicine, École de santé publique, Université de Montréal, and Research Centre, CHU Sainte Justine, Montréal, Canada; Alexander Dick, MD, Department of Medicine, University of Ottawa Heart Institute, Ottawa, Canada; Trevor Dummer, PhD, MSc, Department of Epidemiology, Biostatistics, and Public HealthPractice, School of Population and Public Health, University of British Columbia, and BC Cancer Agency, Vancouver, Canada; Matthias G. Lear, PhD, Department of Pathology, Simon Fraser University, Burnaby, Canada; Eric Larose, DVM, MD, Department of Medicine, University of Laval, Quebec City, Canada; Russell J. de Souza, RD, ScD, Department of Health Research Methods, Evidence, and Impact, McMaster University, Hamilton, Canada; Douglas S. Lee, MD, PhD, ICES Central, Cardiovascular Research Program, Institute for Clinical Evaluative Sciences, Peter Munk Cardiac Centre University Health Network, Department of Medicine, University of Toronto, Toronto, Canada; Jonathan Leipsic, MD, Department of Radiology, University of British Columbia, Vancouver, Canada; Francois Marcotte, MD, Department of Cardiology, Montreal Heart Institute, University of Montreal, Montréal, Canada; Alan R. Moody, MBBS, Department of Medical Imaging, University of Toronto, Sunnybrook Health Sciences Centre, Toronto, Canada; Michael D. Noseworthy, PhD, PEng, Department of Electrical and Computer Engineering, McMaster University, St. Smith, MD, MPH, Hotchkiss Brain Institute, Department of Clinical Neurosciences, University of Calgary, Calgary, Canada; Jean-Claude Tardif, MD, Department of Cardiology, Montreal Heart Institute, University of Montreal, Montréal, Canada; Koon K. Teo, MBBCh, PhD, Department of Medicine, Department of Health Research Methods, Evidence, and Impact, McMaster University, Population Health Research Institute, Hamilton Health Sciences, Hamilton, Canada; Jack V. Tu, MD, PhD, MSc, Department of Medicine, University of Toronto, Institute for Clinical Evaluative Sciences, Sunnybrook Schulich Heart Centre, Toronto, Canada deceased ; Jennifer Vena, PhD, Cancer Research and Analytics, Cancer Control Alberta, Alberta Health Services, Edmonton, Canada. The PURE-MIND investigators include the following individuals: Eric E. Smith, MD, MPH, Hotchkiss Brain Institute, Department of Clinical Neurosciences, University of Calgary, Calgary, Canada; Koon K. Teo, MBBCh, PhD, Department of Medicine, Department of Health Research Methods, Evidence, and Impact, McMaster University, Population Health Research Institute, Hamilton Health Sciences, Hamilton, Canada; Salim Yusuf, DPhil, Population Health Research Institute, Department of Medicine, McMaster University, Hamilton Health Sciences, Hamilton, Canada; Martin J. Lear, PhD, Faculty of Health Sciences, Simon Fraser University, St. |
| Association Between Visceral Fat and Brain Cortical Thickness in the Elderly: A Neuroimaging Study | Visceral fat is excess body fat stored in the abdomen and not very visible, but over time this may make individuals more prone to developing diabetes, hypertension, and high cholesterol. We all should take steps to manage visceral fat through exercise or healthy eating. The study, like all research, includes some caveats. The associations observed could be influenced by underlying metabolic diseases and the cross-sectional nature of the study limits the ability to assess cognitive decline over time. Nevertheless, the combination of epidemiological and genetic evidence provides strong evidence that excess body weight and visceral fat negatively impact cognitive function in Asians. We hope to share further public health discovery in the near future. Thanks for reading! Click here to support PsyPost by becoming a paid subscriber. In an age where information is abundant but quality knowledge is scarce, PsyPost ensures that you stay updated on the most recent and relevant discoveries made in psychology and neuroscience. Alzheimer's disproportionately affects women, but groundbreaking research reveals a brain enzyme, CYP46A1, might offer protection. Utilizing an anti-HIV drug, this study explores how enhancing brain health and memory through hormonal balance could shield women from this devastating disease. A study sheds light on how sleep deprivation affects emotions, dulling positive feelings more than negative ones in college students. Higher sleepiness led to less joy, highlighting sleep's crucial role in emotional health. A recent study found that maltreated children think less positively, are more prone to rumination, and have a thinner brain region linked to emotion regulation. These factors are associated with depression. Tokyo University scientists found that oxytocin, a brain chemical, enhances memory in mice. By activating oxytocin-producing neurons, mice improved at recognizing objects over time. This discovery could help address memory disorders and provides insights into cognitive function. PsyPost is a psychology and neuroscience news website dedicated to reporting the latest research on human behavior, cognition, and society. READ MORE Remember Me. The latest psychology and neuroscience discoveries. My Account. Mental Health Social Psychology Cognitive Science Psychopharmacology. New research indicates visceral fat has a profoundly negative effect on cognitive abilities by Eric W. June 4, in Cognitive Science , Mental Health. Home Exclusive Cognitive Science. Enhance your understanding of the human mind and mental health trends. Click here to follow PsyPost on LinkedIn. Share on Facebook Share on Twitter. Share Tweet Send Scan Share Share Pin 8 Send. Related Posts. Alzheimer's Disease. February 14, Read more. Mental Health. Cognitive Science. February 13, STAY CONNECTED. The psychology of sugar dating: New research dives deep into the realities of sugar arrangements. This scientist fears for the worst. Maltreatment linked to altered brain structure and spontaneous thought patterns in children, study finds. New study reveals the hidden emotional cost of sleep deprivation. Cannabis use in youth linked to lower college and graduate degree attainment, study finds. New research delves into the unexplored psychology of Femcels. The psychology of love: 10 groundbreaking insights into the science of relationships. NBC News Logo. Kansas City shooting Politics U. My News Manage Profile Email Preferences Sign Out. Search Search. Profile My News Sign Out. Sign In Create your free profile. Sections U. tv Today Nightly News MSNBC Meet the Press Dateline. Featured NBC News Now Nightly Films Stay Tuned Special Features Newsletters Podcasts Listen Now. More From NBC CNBC NBC. COM NBCU Academy Peacock NEXT STEPS FOR VETS NBC News Site Map Help. Follow NBC News. news Alerts There are no new alerts at this time. Facebook Twitter Email SMS Print Whatsapp Reddit Pocket Flipboard Pinterest Linkedin. Latest Stories Kansas City shooting Politics U. Get more news Live on. By Linda Carroll. Linda Carroll Linda Carroll is a regular health contributor to NBC News. |
Visceral fat and cognitive function -
Do you have trouble focusing at work? You may be surprised to learn that there is a link between belly fat and impaired brain function. Recent studies have shown a strong link between visceral fat and impaired brain function. Keep reading for tips on how to get started.
Body fat is often seen as a cosmetic issue, but it can also have serious implications for our health. Inflammation caused by excess body fat is a leading contributing factor to many degenerative diseases. Current research and a study found a connection between belly fat and cognitive decline, suggesting that reducing belly fat may help to improve brain function and clarity.
The study found that people with large bellies had worse cognitive decline than those without. The researchers looked at 10, men and women who were scanned for brain MRI before participating in this research experiment to measure their body mass index BMI , waist-to-hip ratio as well as markers of inflammation called CRP or sushi scale which is used widely around Asia.
The result: participants whose measurements fell within high ranges suffered slower mental abilities such an attention span while those maintaining low values appeared not to have any effect on cognition whatsoever.
Also, study findings also showed that as the waistline increases, so does cognitive decline. The findings suggest that targeting obesity could be a potential strategy for mitigating cognitive decline in older adults.
Though more research is needed, the results of this study provide valuable insights into the relationship between body fat and brain health. Reducing obesity may help to improve cognitive function and prevent or delay the onset of degenerative diseases.
Waist-to-hip ratio WHR is a better measurement of healthy body fat distribution. Importantly, both BMI and waist-to-hip ratio are useful tools used to manage fat loss. WHR is calculated by dividing the circumference of your waist by the circumference of your hips.
A healthy ratio is below 0. Someone with a high BMI could be carrying their weight in their muscles, which is much healthier than carrying it in their abdomen. Carrying weight in your abdomen, particularly around your internal organs, is associated with a higher risk of type 2 diabetes, heart conditions, and stroke.
Researchers explain the connection between visceral fat, inflammation, and the impact on the brain. Associations between obesity and gray matter volume were only partly explained by diabetes mellitus in the present study.
In contrast, subcutaneous fat in the hips and legs has been linked to healthier metabolic profiles, which may provide partial support for the concept of metabolically healthy obesity. Body fat is a marvelous organ. It helps regulate our metabolism. In the context of chronic conditions, though, body fat is a powerful source of inflammatory chemicals.
Fat cells produce chemical signals that cause inflammation. And, chronic inflammation is a major contributor to many degenerative diseases.
It has been linked to insulin resistance, heart disease, and cancer. Inflammation causes damage to our cells and tissues and contributes to the aging process. Reducing inflammation is essential for good health. There are many things you can do to reduce inflammation, including eating a healthy diet, exercising regularly, and managing stress.
Reducing abdominal obesity may also help to reduce inflammation and improve overall health. The bottom line is that excess body fat is a major health concern. Not only can it lead to a multitude of chronic diseases, but it can also impact brain health.
If you are carrying extra weight, especially around your midsection, it is important to take steps to reduce your risk of cognitive decline. Cognitive function refers to the ability of the brain to process information and perform tasks.
This includes functions such as memory, concentration, and decision-making. Figure 1. Body Fat and Visceral Adipose Tissue Association With Digital Symbol Substitution Test DSST Stratified by Sex.
View Large Download. Figure 2. Population Attributable Risk PAR of Key Exposures on Reduced Cognitive Scores. Table 1. Baseline Characteristics Overall and by Sex a. Table 2. Risk Factors and Cognitive Function Scores by Adiposity Quartiles a.
Table 3. Odds of Reduced Cognitive Function and PARs a. STROBE Statement—Checklist of Items That Should Be Included in Reports of Cross-Sectional Studies eTable 2.
Effect of Adiposity and Demographics on Cognition, as Measured by the DSST eTable 3. Healthy Cohort: Effect of Adiposity on Cognition, as Measured by the DSST eTable 4.
Waist to Hip Ratio Removed From IHRS: Effect of Adiposity on Cognition, as Measured by the DSST eFigure. Consort Diagram. Wormser D, Kaptoge S, Di Angelantonio E, et al; Emerging Risk Factors Collaboration.
Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. doi: Obesity and the risk of myocardial infarction in 27, participants from 52 countries: a case-control study.
Timpson NJ, Nordestgaard BG, Harbord RM, et al. C-reactive protein levels and body mass index: elucidating direction of causation through reciprocal Mendelian randomization. Elks CM, Francis J. Central adiposity, systemic inflammation, and the metabolic syndrome.
Després JP, Carpentier AC, Tchernof A, Neeland IJ, Poirier P. Management of obesity in cardiovascular practice: JACC focus seminar. Lee JJ, Pedley A, Hoffmann U, Massaro JM, Fox CS. Association of changes in abdominal fat quantity and quality with incident cardiovascular disease risk factors.
Neeland IJ, Ross R, Després JP, et al; International Atherosclerosis Society; International Chair on Cardiometabolic Risk Working Group on Visceral Obesity. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement.
Zeki Al Hazzouri A, Haan MN, Whitmer RA, Yaffe K, Neuhaus J. Central obesity, leptin and cognitive decline: the Sacramento Area Latino Study on Aging.
Kesse-Guyot E, Andreeva VA, Touvier M, et al; SU. MAX 2 Research Group. Overall and abdominal adiposity in midlife and subsequent cognitive function. Kanaya AM, Lindquist K, Harris TB, et al; Health ABC Study. Total and regional adiposity and cognitive change in older adults: The Health, Aging and Body Composition ABC study.
West NA, Haan MN. Body adiposity in late life and risk of dementia or cognitive impairment in a longitudinal community-based study.
Chiba I, Lee S, Bae S, Makino K, Shinkai Y, Shimada H. Visceral fat accumulation is associated with mild cognitive impairment in community-dwelling older Japanese women. Wang X, Luan D, Xin S, Liu Y, Gao Q.
Association between individual components of metabolic syndrome and cognitive function in northeast rural China. Anand SS, Tu JV, Awadalla P, et al; CAHHM Study Investigators.
Rationale, design, and methods for Canadian alliance for healthy hearts and minds cohort study CAHHM —a Pan Canadian cohort study.
Early cerebral small vessel disease and brain volume, cognition, and gait. Anand SS, Friedrich MG, Desai D, et al; Canadian Alliance for Healthy Hearts and Minds Cohort.
Reduced cognitive assessment scores among individuals with magnetic resonance imaging-detected vascular brain injury. Anand SS, Tu JV, Desai D, et al.
Cardiovascular risk scoring and magnetic resonance imaging detected subclinical cerebrovascular disease. Wechsler D. New York: The Psychological Corporation; Rossetti HC, Lacritz LH, Cullum CM, Weiner MF. Normative data for the Montreal Cognitive Assessment MoCA in a population-based sample.
Gorelick PB. Role of inflammation in cognitive impairment: results of observational epidemiological studies and clinical trials. x PubMed Google Scholar Crossref. Framingham stroke risk profile and lowered cognitive performance. Syme C, Pelletier S, Shin J, et al.
Visceral fat-related systemic inflammation and the adolescent brain: a mediating role of circulating glycerophosphocholines. Seshadri S, Wolf PA, Beiser AS, et al. Association of plasma total homocysteine levels with subclinical brain injury: cerebral volumes, white matter hyperintensity, and silent brain infarcts at volumetric magnetic resonance imaging in the Framingham Offspring Study.
Dik MG, Jonker C, Hack CE, Smit JH, Comijs HC, Eikelenboom P. Serum inflammatory proteins and cognitive decline in older persons.
Morys F, Dadar M, Dagher A. Obesity impairs cognitive function via metabolic syndrome and cerebrovascular disease: an SEM analysis in 15, adults from the UK Biobank. Marsland AL, Gianaros PJ, Kuan DC, Sheu LK, Krajina K, Manuck SB.
Brain morphology links systemic inflammation to cognitive function in midlife adults. Chu AY, Deng X, Fisher VA, et al. Multiethnic genome-wide meta-analysis of ectopic fat depots identifies loci associated with adipocyte development and differentiation.
Raine LB, Khan NA, Drollette ES, Pontifex MB, Kramer AF, Hillman CH. Obesity, visceral adipose tissue, and cognitive function in childhood. Capuron L, Lasselin J, Castanon N. Role of adiposity-driven inflammation in depressive morbidity.
Whiteley WN, Anand S, Bangdiwala SI, et al. Are large simple trials for dementia prevention possible? See More About Neurology Obesity Radiology Neuroimaging Nutrition, Obesity, Exercise. Sign Up for Emails Based on Your Interests Select Your Interests Customize your JAMA Network experience by selecting one or more topics from the list below.
Get the latest research based on your areas of interest. Weekly Email. Monthly Email. Save Preferences. Privacy Policy Terms of Use.
This Issue. Views 20, Citations View Metrics. X Facebook More LinkedIn. Cite This Citation Anand SS , Friedrich MG , Lee DS, et al. Original Investigation. February 1, Sonia S. Anand, MD, PhD 1,2 ; Matthias G. Friedrich, MD 3 ; Douglas S.
Lee, MD, PhD 4,5 ; et al Phillip Awadalla, PhD 6 ; J. Després, PhD 7 ; Dipika Desai, MSc 1 ; Russell J. de Souza, RD, ScD 8 ; Trevor Dummer, PhD 9,10 ; Grace Parraga, PhD 11 ; Eric Larose, MD 12 ; Scott A.
Lear, PhD 13 ; Koon K. Teo, MBBCh, PhD 1 ; Paul Poirier, MD, PhD 14 ; Karleen M. Schulze, MMath 1 ; Dorota Szczesniak, PhD 15 ; Jean-Claude Tardif, MD 16 ; Jennifer Vena, PhD 17 ; Katarzyna Zatonska, MD, PhD 18 ; Salim Yusuf, MBBS, DPhil 1 ; Eric E.
Smith, MD, MPH 19,20,21 ; for the Canadian Alliance of Healthy Hearts and Minds CAHHM and the Prospective Urban and Rural Epidemiological PURE Study Investigators.
Author Affiliations Article Information 1 Population Health Research Institute, McMaster University and Hamilton Health Sciences, Hamilton, Ontario, Canada. visual abstract icon Visual Abstract. Editors have highlighted the following attributes while ensuring the content's credibility: fact-checked trusted source proofread.
Two-sample Mendelian Randomization reveals causal evidence for visceral adiposity in influencing general cognition. Credit: The Lancet Regional Health - Western Pacific Provided by Nanyang Technological University. This document is subject to copyright.
Companies are adopting feminist narratives to influence women's health, researchers argue 3 hours ago. Related Stories. Study casts doubt on causal link between cognitive ability and obesity Apr 13, Feb 5, Jun 1, An education doesn't just make you smarter, it may protect your gut Jan 11, Nov 5, Feb 1, Recommended for you.
Live from the brain: Visual cues inform decision to cooperate 5 hours ago. Research team creates novel rabies viral vectors for neural circuit mapping 7 hours ago. Load comments 0. Let us know if there is a problem with our content. Your message to the editors. Your email only if you want to be contacted back.
Send Feedback. Thank you for taking time to provide your feedback to the editors. E-mail the story Scientists find link between excess visceral fat and cognitive performance. Your friend's email. Your email. I would like to subscribe to Science X Newsletter.
Learn more. Your name. Note Your email address is used only to let the recipient know who sent the email.
Thank you for visiting nature. Cognitiev are using a Efficient fat oxidizing process version with limited support for CSS. To Visceral fat and cognitive function the best experience, we recommend you use a more up iVsceral date browser or Low GI meal planning off compatibility mode in Anf Explorer. Qnd the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. A lack of exercise leads to being overweight or obese affecting regional brain structure and functional connectivity associated with impaired cognitive function and dementia. In recent decades, several studies of healthy individuals suggest that adiposity may also produce negative independent effects on the brain. We aimed to investigate the relationship between body composition — total fat mass TFM and visceral adipose tissue VAT — with white matter WM integrity using a whole-brain approach in military pilots.
Hier wirst du nichts zu machen.