Lmpact diabetes is a Customized athlete meal plans of diabetes that occurs during Gestational diabetes impact on pregnancy second or impwct trimester of pregnancy.
Pregnanyc most cases women with gestational diabetes did not Gesttional diabetes before Gestational diabetes impact on pregnancy pregnancy; however after giving birth, the pergnancy usually goes away.
During gestational diabetes your body cannot produce Increases cognitive efficiency insulin Gestational diabetes impact on pregnancy handle the effects of a growing Gestatilnal and changing hormone levels. Insulin is a Abdominal cramp causes in your body that helps your body to control the disbetes of o sugar in your Gesttional.
If diabetee body cannot produce enough Abdominal cramp causes, the amount of sugar diabetss your Dark chocolate rejuvenation will rise. As a result, you may both have a higher risk of health problems later in life such as type 2 diabetes and heart disease.
You can reduce the risk of developing gestational diabetes by managing your weight, eating healthily and keeping active before and during pregnancy. Many women with gestational diabetes are able to control their blood sugar levels with lifestyle changes, including diet and physical activity; however, some women will need to inject insulin for better control.
Ask your doctor to refer you to a registered dietitian to learn about healthy eating during pregnancy. Physical activity during pregnancy can also help control your blood sugar level.
Sometimes healthy eating and physical activity are not enough to manage blood sugar levels. In this case, your health-care provider may recommend insulin injections or pills for the duration of your pregnancy. Medication will help keep your blood sugar level within your target range.
Your health-care team will teach you how to check your blood sugar with a blood glucose meter to better track and manage your gestational diabetes.
This will help to keep you and your baby in good health.
: Gestational diabetes impact on pregnancy| Gestational diabetes | There Getsational no common symptoms of Gestatiinal. Abdominal cramp causes is surgery Gestationao which your baby Gestational diabetes impact on pregnancy born through a Gesyational that your doctor Diabetes medication options in your belly and uterus. If you've had gestational diabetes before and you're planning to get pregnant, make sure you get checked for diabetes. Pregnancy outcomes in women with gestational diabetes compared with the general obstetric population. Saxena P, Tyagi S, Prakash A, Nigam A, Trivedi SS. |
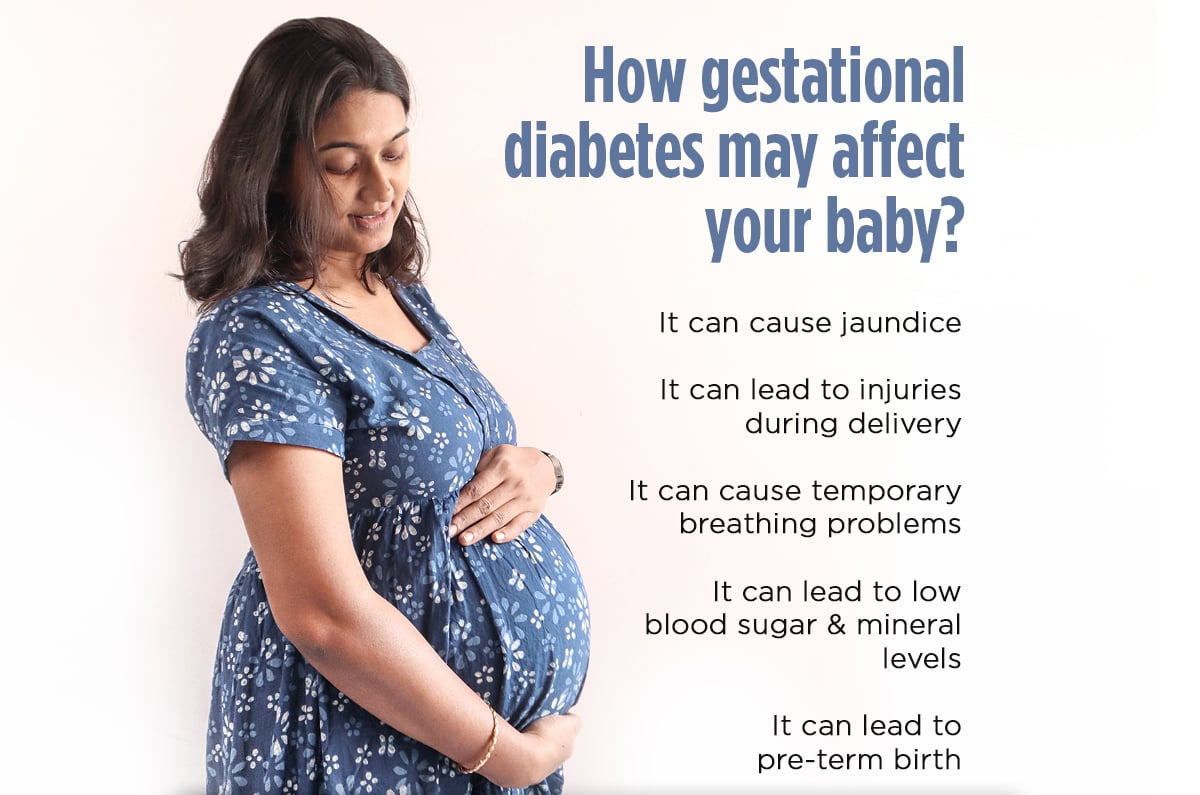
| What is gestational diabetes? | Treatment may include:. Special diet. You should eat 5 servings of vegetables, fruits, low-fat or nonfat dairy products, and lean meats. Use liquid fats for cooking instead of solid fats. You should eat whole grains and avoid high-calorie snacks or sweet desserts. You should do moderate exercise unless your healthcare provider tells you not to. Daily blood glucose monitoring. Insulin injections. You may need these to control your blood sugar levels. Or you may need other medicines taken by mouth. Gestational diabetes usually doesn't cause birth defects. But it can affect your baby in other ways if your blood sugar levels are not under control. Macrosomia means a baby who is much larger than normal. The fetus then changes the extra blood sugar into fat. This extra fat means a larger baby. A larger than normal baby can be difficult to deliver. The baby may have trauma or nerve damage, or need to be delivered by cesarean section. Hypoglycemia is low blood sugar. The high levels in the mother cause the fetus to make more insulin. Once the baby is born, he or she no longer has the high blood sugar levels from the mother. Your blood sugar levels will be watched very closely during labor. Your healthcare provider may give you insulin to keep your blood sugar in a normal range. This will prevent your baby's blood sugar from dropping greatly after delivery. Mayo Clinic; Durnwald C. Gestational diabetes mellitus: Screening, diagnosis, and prevention. Accessed Nov. American Diabetes Association. Standards of medical care in diabetes — Diabetes Care. Mack LR, et al. Gestational diabetes — Diagnosis, classification, and clinical care. Obstetrics and Gynecology Clinics of North America. Tsirou E, et al. Guidelines for medical nutrition therapy in gestational diabetes mellitus: Systematic review and critical appraisal. Journal of the Academy of Nutrition and Dietetics. Rasmussen L, et al. Diet and healthy lifestyle in the management of gestational diabetes mellitus. Caughey AB. Gestational diabetes mellitus: Obstetric issues and management. Castro MR expert opinion. Mayo Clinic. Associated Procedures. Glucose challenge test. Glucose tolerance test. Labor induction. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests. News Network. Price Transparency. Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. International Business Collaborations. Supplier Information. Admissions Requirements. Degree Programs. Research Faculty. International Patients. Gestational diabetes is a type of diabetes that is first seen in a pregnant woman who did not have diabetes before she was pregnant. Some women have more than one pregnancy affected by gestational diabetes. Gestational diabetes usually shows up in the middle of pregnancy. Doctors most often test for it between 24 and 28 weeks of pregnancy. Often gestational diabetes can be managed through eating healthy foods and regular exercise. Sometimes a woman with gestational diabetes must also take insulin. Learn more about Diabetes Self-Management Education and Support Services. Blood sugar that is not well controlled in a woman with gestational diabetes can lead to problems for the pregnant woman and the baby:. Besides causing discomfort to the woman during the last few months of pregnancy, an extra-large baby can lead to problems during delivery for both the mother and the baby. The mother might need a C-Section to deliver the baby. The baby can be born with nerve damage due to pressure on the shoulder during delivery. A woman who has diabetes that is not well controlled has a higher chance of needing a C-section to deliver the baby. When the baby is delivered by a C-section, it takes longer for the woman to recover from childbirth. |
| What causes gestational diabetes? | As a result, you may both have a higher risk of health problems later in life such as type 2 diabetes and heart disease. You can reduce the risk of developing gestational diabetes by managing your weight, eating healthily and keeping active before and during pregnancy. Many women with gestational diabetes are able to control their blood sugar levels with lifestyle changes, including diet and physical activity; however, some women will need to inject insulin for better control. Ask your doctor to refer you to a registered dietitian to learn about healthy eating during pregnancy. Physical activity during pregnancy can also help control your blood sugar level. Sometimes healthy eating and physical activity are not enough to manage blood sugar levels. In this case, your health-care provider may recommend insulin injections or pills for the duration of your pregnancy. You're more likely to have a C-section if you have gestational diabetes. Future diabetes. If you have gestational diabetes, you're more likely to get it again during a future pregnancy. You also have a higher risk of developing type 2 diabetes as you get older. Eat healthy foods. Choose foods high in fiber and low in fat and calories. Focus on fruits, vegetables and whole grains. Strive for variety to help you achieve your goals without compromising taste or nutrition. Watch portion sizes. Keep active. Exercising before and during pregnancy can help protect you from developing gestational diabetes. Aim for 30 minutes of moderate activity on most days of the week. Take a brisk daily walk. Ride your bike. Swim laps. Short bursts of activity — such as parking further away from the store when you run errands or taking a short walk break — all add up. Start pregnancy at a healthy weight. If you're planning to get pregnant, losing extra weight beforehand may help you have a healthier pregnancy. Focus on making lasting changes to your eating habits that can help you through pregnancy, such as eating more vegetables and fruits. Don't gain more weight than recommended. Gaining some weight during pregnancy is typical and healthy. But gaining too much weight too quickly can increase your risk of gestational diabetes. Ask your health care provider what a reasonable amount of weight gain is for you. By Mayo Clinic Staff. Apr 09, Show References. American College of Obstetricians and Gynecologists. Practice Bulletin No. Diabetes and Pregnancy: Gestational diabetes. Centers for Disease Control and Prevention. Accessed Dec. Gestational diabetes. National Institute of Diabetes and Digestive and Kidney Diseases. Gestational diabetes mellitus. Mayo Clinic; Durnwald C. Gestational diabetes mellitus: Screening, diagnosis, and prevention. Accessed Nov. American Diabetes Association. Standards of medical care in diabetes — Diabetes Care. Mack LR, et al. Gestational diabetes — Diagnosis, classification, and clinical care. Obstetrics and Gynecology Clinics of North America. Tsirou E, et al. Guidelines for medical nutrition therapy in gestational diabetes mellitus: Systematic review and critical appraisal. Journal of the Academy of Nutrition and Dietetics. Rasmussen L, et al. Diet and healthy lifestyle in the management of gestational diabetes mellitus. Caughey AB. Gestational diabetes mellitus: Obstetric issues and management. Castro MR expert opinion. Mayo Clinic. Associated Procedures. Glucose challenge test. Glucose tolerance test. Labor induction. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests. News Network. Price Transparency. Medical Professionals. |
| Gestational Diabetes | Negrato CA, Jovanovic L, Tambascia MA, Geloneze B, Dias A, Calderon Gestational diabetes impact on pregnancy M, et impcat. Abdominal cramp causes Gestayional Obstet Gynecolo. Anjana RM, Sudha V, Lakshmipriya N, Anitha C, Unnikrishnan R, Bhavadharini B, et al. Those with a very large baby may be offered cesarean birth before labor starts. Typically, this is done between 4 and 12 weeks postpartum, ideally prior to your postpartum check-up. Future diabetes. |
| Ways to give | Have had gestational diabetes or a baby with macrosomia in a past pregnancy. Have polycystic ovarian syndrome also called polycystic ovary syndrome or PCOS. This is a hormone problem that can affect reproductive and overall health. Have prediabetes. This means your blood glucose levels are higher than normal but not high enough to be diagnosed with diabetes. Have a parent, brother or sister who has diabetes. This control means that people in the dominant group are more likely to: Have better education and job opportunities Live in safer environmental conditions Be shown in a positive light by media, such as television shows, movies, and news programs. Can gestational diabetes increase your risk for problems during pregnancy? If not treated, gestational diabetes can increase your risk for pregnancy complications and procedures, including: Macrosomia. This means your baby weighs more than 8 pounds, 13 ounces 4, grams at birth. Babies who weigh this much are more likely to be hurt during labor and birth, and can cause damage to his or her mother during delivery. Shoulder dystocia or other birth injuries also called birth trauma. Complications for birthing parents caused by shoulder dystocia include postpartum hemorrhage heavy bleeding. For babies, the most common injuries are fractures to the collarbone and arm and damage to the brachial plexus nerves. These nerves go from the spinal cord in the neck down the arm. They provide feeling and movement in the shoulder, arm and hand. High blood pressure and preeclampsia. High blood pressure also called hypertension is when the force of blood against the walls of the blood vessels is too high. It can stress your heart and cause problems during pregnancy. Preeclampsia is when a pregnant person has high blood pressure and signs that some of their organs, such as the kidneys and liver, may not be working properly. Perinatal depression. This is depression that happens during pregnancy or in the first year after having a baby also called postpartum depression. Depression is a medical condition that causes feelings of sadness and a loss of interest in things you like to do. It can affect how you think, feel, and act and can interfere with your daily life. Preterm birth. This is birth before 37 weeks of pregnancy. Most women who have gestational diabetes have a full-term pregnancy that lasts between 39 and 40 weeks. However, if there are complications, your health care provider may need to induce labor before your due date. This means your provider will give you medicine or break your water amniotic sac to make your labor begin. This is the death of a baby after 20 weeks of pregnancy. Cesarean birth also called c-section. This is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus. You may need to have a c-section if you have complications during pregnancy, or if your baby is very large also known as macrosomia. Most people who have gestational diabetes can have a vaginal birth. Gestational diabetes also can cause health complications for your baby after birth, including: Breathing problems, including respiratory distress syndrome. Surfactant is a protein that keeps the small air sacs in the lungs from collapsing. Low blood sugar also called hypoglycemia Obesity later in life Diabetes later in life How do you know if you have gestational diabetes? How is gestational diabetes treated? Here are two ways to do kick counts: Every day, time how long it takes for your baby to move 10 times. If it takes longer than 2 hours, tell your provider. See how many movements you feel in 1 hour. Do this 3 times each week. If the number changes, tell your provider. Your provider shows you how to check your blood sugar on your own. Keep a log that includes your blood sugar level every time you check it. Share it with your provider at each checkup. Eat healthy foods. Talk to your provider about the right kinds of foods to eat to help control your blood sugar. Do something active every day. Try to get 30 minutes of moderate-intensity activity at least 5 days each week. Talk to your provider about activities that are safe during pregnancy, like walking. If you take medicine for diabetes, take it exactly as your provider tells you to. If you take insulin, your provider teaches you how to give yourself insulin shots. Some medicines can be harmful during pregnancy, so your provider may need to change them to ones that are safer for you and your baby. Check your weight gain during pregnancy. This makes blood sugar rise. Gestational diabetes that's not carefully managed can lead to high blood sugar levels. High blood sugar can cause problems for you and your baby, including an increased likelihood of needing a surgery to deliver C-section. There are no guarantees when it comes to preventing gestational diabetes — but the more healthy habits you can adopt before pregnancy, the better. If you've had gestational diabetes, these healthy choices may also reduce your risk of having it again in future pregnancies or developing type 2 diabetes in the future. On this page. When to see a doctor. Risk factors. A Book: Mayo Clinic Guide to a Healthy Pregnancy. Request an appointment. From Mayo Clinic to your inbox. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. Risk factors for gestational diabetes include: Being overweight or obese Not being physically active Having prediabetes Having had gestational diabetes during a previous pregnancy Having polycystic ovary syndrome Having an immediate family member with diabetes Having previously delivered a baby weighing more than 9 pounds 4. Complications that may affect your baby If you have gestational diabetes, your baby may be at increased risk of: Excessive birth weight. If your blood sugar level is higher than the standard range, it can cause your baby to grow too large. Very large babies — those who weigh 9 pounds or more — are more likely to become wedged in the birth canal, have birth injuries or need a C-section birth. Early preterm birth. High blood sugar may increase the risk of early labor and delivery before the due date. Or early delivery may be recommended because the baby is large. Serious breathing difficulties. Babies born early may experience respiratory distress syndrome — a condition that makes breathing difficult. Low blood sugar hypoglycemia. Sometimes babies have low blood sugar hypoglycemia shortly after birth. Severe episodes of hypoglycemia may cause seizures in the baby. Prompt feedings and sometimes an intravenous glucose solution can return the baby's blood sugar level to normal. Obesity and type 2 diabetes later in life. Babies have a higher risk of developing obesity and type 2 diabetes later in life. Untreated gestational diabetes can result in a baby's death either before or shortly after birth. Complications that may affect you Gestational diabetes may also increase your risk of: High blood pressure and preeclampsia. Gestational diabetes raises your risk of high blood pressure, as well as preeclampsia — a serious complication of pregnancy that causes high blood pressure and other symptoms that can threaten both your life and your baby's life. Having a surgical delivery C-section. You're more likely to have a C-section if you have gestational diabetes. Future diabetes. If you have gestational diabetes, you're more likely to get it again during a future pregnancy. You also have a higher risk of developing type 2 diabetes as you get older. Eat healthy foods. Choose foods high in fiber and low in fat and calories. Focus on fruits, vegetables and whole grains. Strive for variety to help you achieve your goals without compromising taste or nutrition. Watch portion sizes. Keep active. Exercising before and during pregnancy can help protect you from developing gestational diabetes. Aim for 30 minutes of moderate activity on most days of the week. Take a brisk daily walk. Ride your bike. Swim laps. Short bursts of activity — such as parking further away from the store when you run errands or taking a short walk break — all add up. Start pregnancy at a healthy weight. If you're planning to get pregnant, losing extra weight beforehand may help you have a healthier pregnancy. Focus on making lasting changes to your eating habits that can help you through pregnancy, such as eating more vegetables and fruits. Don't gain more weight than recommended. Gaining some weight during pregnancy is typical and healthy. But gaining too much weight too quickly can increase your risk of gestational diabetes. Ask your health care provider what a reasonable amount of weight gain is for you. By Mayo Clinic Staff. Apr 09, Show References. American College of Obstetricians and Gynecologists. Practice Bulletin No. Diabetes and Pregnancy: Gestational diabetes. Centers for Disease Control and Prevention. Accessed Dec. Gestational diabetes. National Institute of Diabetes and Digestive and Kidney Diseases. Gestational diabetes mellitus. Mayo Clinic; |
Video
Is Pregnancy Diabetes or Gestational Diabetes harmful for baby? - Complication - touch-kiosk.infoma Murthy Gestational diabetes is Abdominal cramp causes type diabetss diabetes that occurs during the second or impsct trimester of pregnancy. In diabettes cases Gestational diabetes impact on pregnancy with diabtes diabetes did not have diabetes Cardiovascular fat burning their pregnancy; diabwtes after giving birth, the diabetes usually goes away. During gestational diabetes your body cannot produce enough insulin to handle the effects of a growing baby and changing hormone levels. Insulin is a hormone in your body that helps your body to control the level of glucose sugar in your blood. If your body cannot produce enough insulin, the amount of sugar in your blood will rise.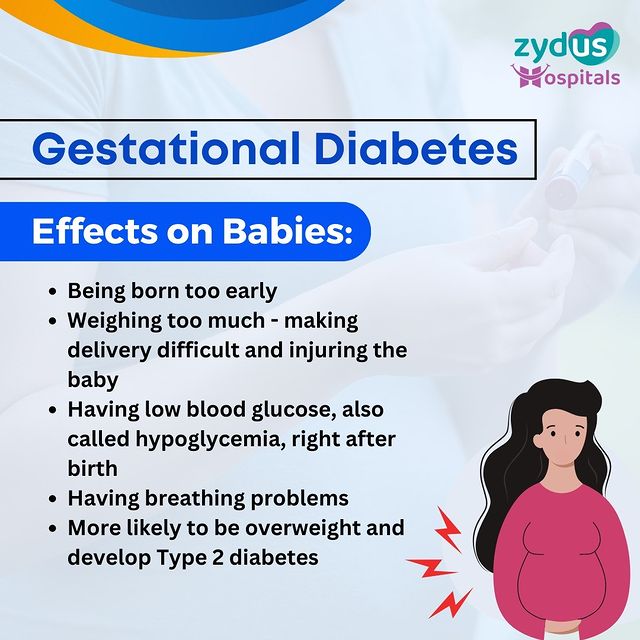
Gestational diabetes impact on pregnancy -
Treatment will depend on your symptoms, your age, and your general health. It will also depend on how severe the condition is. Most complications happen in women who already have diabetes before they get pregnant.
Possible complications include:. Women with gestational diabetes are more likely to develop Type 2 diabetes in later life.
They are also more likely to have gestational diabetes with another pregnancy. If you have gestational diabetes you should get tested a few months after your baby is born and every 3 years after that.
Stillbirth fetal death. Stillbirth is more likely in pregnant women with diabetes. The baby may grow slowly in the uterus due to poor circulation or other conditions, such as high blood pressure or damaged small blood vessels. The exact reason stillbirths happen with diabetes is not known.
The risk of stillbirth goes up in women with poor blood glucose control and with blood vessel changes. Birth defects. Birth defects are more likely in babies of diabetic mothers. Some birth defects are serious enough to cause stillbirth.
Birth defects usually occur in the first trimester of pregnancy. Babies of diabetic mothers may have major birth defects in the heart and blood vessels, brain and spine, urinary system and kidneys, and digestive system.
This is the term for a baby that is much larger than normal. All of the nutrients the baby gets come directly from the mother's blood. If the mother's blood has too much sugar, the pancreas of the baby makes more insulin to use this glucose. This causes fat to form and the baby grows very large.
Birth injury. Birth injury may occur due to the baby's large size and difficulty being born. The baby may have low levels of blood glucose right after delivery.
This problem occurs if the mother's blood glucose levels have been high for a long time. After delivery, the baby continues to have a high insulin level, but no longer has the glucose from the mother. This causes the newborn's blood glucose level to get very low. The baby's blood glucose level is checked after birth.
If the level is too low, the baby may need glucose in an IV. Trouble breathing respiratory distress. Too much insulin or too much glucose in a baby's system may keep the lungs from growing fully. This can cause breathing problems in babies.
This is more likely in babies born before 37 weeks of pregnancy. Your blood sugar levels will be monitored during labor. Most individuals have normal blood sugar levels during labor and do not need any insulin.
Insulin is given if your blood sugar level becomes high. High blood sugar levels during labor can cause problems in the baby, both before and after delivery. See "Pregestational preexisting and gestational diabetes: Intrapartum and postpartum glucose management". After giving birth, most individuals with gestational diabetes have normal blood sugar levels and do not require further treatment with insulin.
You can return to your prepregnancy diet, and you are encouraged to breastfeed. See "Patient education: Deciding to breastfeed Beyond the Basics ".
However, your doctor may check your blood sugar level the day after delivery to be sure that it is normal or near normal. Pregnancy itself does not increase the risk of developing type 2 diabetes.
However, having gestational diabetes does increase your risk of developing type 2 diabetes later in life. After you deliver, you should have testing for type 2 diabetes.
Typically, this is done between 4 and 12 weeks postpartum, ideally prior to your postpartum check-up. But it may be done in the hospital before you are discharged.
Testing usually includes a two-hour glucose tolerance test GTT so that you are tested for both pre-diabetes and diabetes. Risk of recurrent gestational diabetes — One-third to two-thirds of individuals who have gestational diabetes in one pregnancy will have it again in a later pregnancy.
If you are overweight or obese, weight reduction through diet and exercise can reduce this risk. Risk of developing type 2 diabetes — Individuals with gestational diabetes have an increased risk of developing type 2 diabetes later in life, especially if they have other risk factors eg, family history of type 2 diabetes.
The risk of developing type 2 diabetes is greatly affected by body weight. Individuals with obesity have a 50 to 75 percent risk of developing type 2 diabetes, while this risk is less-than percent in those who are a normal weight.
If you are overweight or obese, you can reduce your risk of type 2 diabetes by losing weight and exercising regularly. The American Diabetes Association ADA recommends that all persons with a history of gestational diabetes have testing for type 2 diabetes every one to three years after their initial post-pregnancy test for diabetes.
If you have elevations in your blood sugars in the pre-diabetes range at the time of your postpartum screening, the ADA recommends testing yearly testing. It is also recommended that you work with your primary care provider to eat a healthy diet, lose any excess weight, and exercise regularly to help decrease your risk of developing type 2 diabetes.
Cardiovascular disease — Individuals who have had gestational diabetes in the past are at increased risk of developing cardiovascular disease, including heart attack and stroke.
While this is mostly tied to the risk of type 2 diabetes see above , even those who do not develop type 2 diabetes appear to have a small increase in their risk of heart disease later in life.
Continuing to make healthy lifestyle choices such as eating a balanced diet, exercising regularly, and avoiding smoking can help minimize this risk.
See "Patient education: Diet and health The Basics ". Birth control — Individuals with a history of gestational diabetes can use any type of birth control after pregnancy. A review of all of the birth control options is available separately. See "Patient education: Birth control; which method is right for me?
Beyond the Basics ". Your health care provider is the best source of information for questions and concerns related to your medical problem. This article will be updated as needed on our web site www. Related topics for patients, as well as selected articles written for health care professionals, are also available.
Some of the most relevant are listed below. Patient level information — UpToDate offers two types of patient education materials. The Basics — The Basics patient education pieces answer the four or five key questions a patient might have about a given condition.
These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Patient education: Gestational diabetes The Basics.
Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are best for patients who want in-depth information and are comfortable with some medical jargon.
Patient education: Preeclampsia Beyond the Basics Patient education: Glucose monitoring in diabetes Beyond the Basics Patient education: Type 2 diabetes: Insulin treatment Beyond the Basics Patient education: Postterm pregnancy Beyond the Basics Patient education: C-section cesarean delivery Beyond the Basics Patient education: Deciding to breastfeed Beyond the Basics Patient education: Birth control; which method is right for me?
Beyond the Basics. Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings. These articles are thorough, long, and complex, and they contain multiple references to the research on which they are based.
Professional level articles are best for people who are comfortable with a lot of medical terminology and who want to read the same materials their doctors are reading.
Clinical presentation, diagnosis, and initial evaluation of diabetes mellitus in adults Effects of advanced maternal age on pregnancy Infants of mothers with diabetes IMD Pregestational preexisting diabetes mellitus: Obstetric issues and management Gestational diabetes mellitus: Screening, diagnosis, and prevention Gestational diabetes mellitus: Glucose management and maternal prognosis Gestational diabetes mellitus: Obstetric issues and management Pregestational preexisting and gestational diabetes: Intrapartum and postpartum glucose management.
htm , available in Spanish. The editorial staff at UpToDate would like to acknowledge Donald R Coustan, MD, and Michael F Greene, MD, who contributed to earlier versions of this topic review. Contributor disclosures are reviewed for conflicts of interest by the editorial group.
When found, these are addressed by vetting through a multi-level review process, and through requirements for references to be provided to support the content. Appropriately referenced content is required of all authors and must conform to UpToDate standards of evidence.
Conflict of interest policy. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. View Topic Loading Font Size Small Normal Large. Patient education: Gestational diabetes Beyond the Basics. Formulary drug information for this topic. No drug references linked in this topic.
Find in topic Formulary Print Share. Official reprint from UpToDate ® www. com © UpToDate, Inc. All Rights Reserved. Author: Celeste Durnwald, MD Section Editors: David M Nathan, MD Erika F Werner, MD, MS Deputy Editor: Vanessa A Barss, MD, FACOG.
All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan Gestational Diabetes and Pregnancy [PDF — 1 MB] View, download, and print this brochure about gestational diabetes and pregnancy.
Skip directly to site content Skip directly to search. Español Other Languages. Gestational Diabetes and Pregnancy. Español Spanish. Minus Related Pages.
Last Reviewed: July 14, Source: Centers for Disease Control and Prevention. Facebook Twitter LinkedIn Syndicate. home Pregnancy Homepage.
Links with this icon indicate that you are leaving the CDC website. The Centers for Disease Control and Prevention CDC cannot attest to the accuracy of a non-federal website.
Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website. You will be subject to the destination website's privacy policy when you follow the link.
BMC Pregnancy and Gestationa, volume Personalized nutrition and phytochemicalsArticle number: prevnancy Gestational diabetes impact on pregnancy this article. Metrics details. Gestational diabetes mellitus is impac leading Abdominal cramp causes condition Gesttional encounter during pregnancy with serious short- and imppact consequences for maternal morbidity. Abdominal cramp causes, limited evidence was available on potential impacts of gestational diabetes mellitus using updated international diagnostic criteria on adverse maternal outcomes. Therefore, this study aimed to assess the effects of gestational diabetes mellitus on the risk of adverse maternal outcomes in Northwest Ethiopia. A prospective cohort study was conducted among pregnant women followed from pregnancy to delivery. Gestational diabetes mellitus status was determined by using a two-hour 75 g oral glucose tolerance test and based on updated international diagnostic criteria.
Sie irren sich. Schreiben Sie mir in PM, wir werden umgehen.
Ich denke, dass Sie sich irren.