Type diabetes complications eyes -
The pressure pinches the blood vessels that carry blood to the retina and optic nerve. Vision is gradually lost because the retina and nerve are damaged. There are several treatments for glaucoma. Some use drugs to reduce pressure in the eye, while others involve surgery.
Many people without diabetes get cataracts, but people with diabetes are more likely to develop this eye condition. People with diabetes also tend to get cataracts at a younger age and have them progress faster. With cataracts, the eye's clear lens clouds, blocking sight.
To help deal with mild cataracts, you may need to wear sunglasses more often and use glare-control lenses in your glasses. For cataracts that interfere greatly with vision, doctors usually remove the lens of the eye and replaces it with a new artificial lens. In people with diabetes, retinopathy can get worse after removal of the lens, and glaucoma may start to develop.
When the retina has already detached or a lot of blood has leaked into the eye, photocoagulation is no longer useful. The next option is vitrectomy, which is surgery to remove scar tissue and cloudy fluid from inside the eye.
The earlier the operation occurs, the more likely it is to be successful. When the goal of the operation is to remove blood from the eye, it usually works.
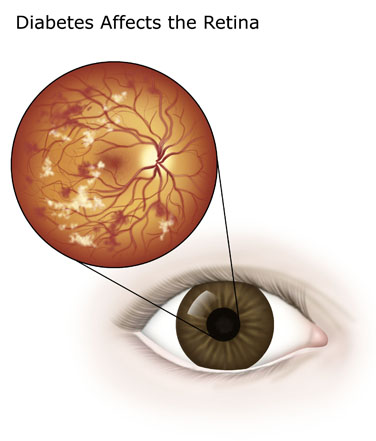
Reattaching a retina to the eye is much harder and works in only about half the cases. Breadcrumb Home About Diabetes Diabetes Complications Eye Complications. Diabetes Complications. Learn More About Eye Health. Retinopathy Diabetic retinopathy is a general term for all disorders of the retina caused by diabetes.
Nonproliferative retinopathy In nonproliferative retinopathy, the most common form of retinopathy, capillaries in the back of the eye balloon and form pouches.
Macular edema Although retinopathy does not usually cause vision loss at this stage, the capillary walls may lose their ability to control the passage of substances between the blood and the retina.
Proliferative retinopathy In some people, retinopathy progresses after several years to a more serious form called proliferative retinopathy. Am I at risk for retinopathy? Several factors influence whether you get retinopathy: Blood glucose blood sugar control Blood pressure levels How long you have had diabetes Genes The longer you've had diabetes, the more likely you are to have retinopathy.
How is retinopathy treated? Photocoagulation In photocoagulation, the eye care professional makes tiny burns on the retina with a special laser. Scatter photocoagulation In scatter photocoagulation also called panretinal photocoagulation , the eye care professional makes hundreds of burns in a polka-dot pattern on two or more occasions.
Focal photocoagulation In focal photocoagulation, the eye care professional aims the laser precisely at leaking blood vessels in the macula. Treatment for Macular Edema There are two types of treatment for macular edema.
Focal laser therapy focal laser therapy that slows the leakage of fluid, and medications that can be injected into the eye that slow the growth of new blood vessels and reduce the leakage of fluid into the macula.
Injecting medication A newer retinopathy treatment involves injecting medication directly into the eye. Common Complications Routine exams are so important—to help avoid vision loss and potentially catch these conditions early.
Glaucoma People with diabetes are more likely to suffer from glaucoma than people without diabetes. The longer you have diabetes, the more likely you are to develop it. These factors can also increase your risk:. If you have diabetic retinopathy, low-vision aids such as magnifying glasses and special lenses can help.
Ask your eye doctor to refer you to a low-vision specialist. These pouches can leak blood and other fluid, which can cause a part of the retina called the macula to swell macular edema and distort your vision.
Macular edema is the most common cause of blindness in people with diabetic retinopathy. About half of people with diabetic retinopathy will develop macular edema.
Advanced stage proliferative : In this stage, the retina begins to grow new blood vessels. These new vessels are fragile and often bleed into the vitreous the clear gel between the lens and retina.
With minor bleeding, you may see a few dark spots that float in your vision. You may not notice symptoms in the early stage.
During your eye exam, your eye doctor will check how well you see the details of letters or symbols from a distance. Your doctor will also look at the retina and inside of your eyes and may use a dye to reveal leaky blood vessels. If it turns out you have diabetic retinopathy, your eye doctor may want to check your vision more often than once a year.
If you have type 1 diabetes, you should be checked within 5 years of your diagnosis and then regularly thereafter, typically every year. Call your eye doctor if you notice changes in your vision, especially if they happen suddenly.
Changes may include:. Treating diabetic retinopathy can repair damage to the eye and even prevent blindness in most people. Treatment can start before your sight is affected, which helps prevent vision loss.
Options include:. A cataract is the clouding of the normally clear lens in your eye. One reason is that high blood sugar can cause deposits to build up in the lenses and make them cloudy.
Other risk factors include high blood pressure, having obesity, too much sun exposure over time, and smoking. Using brighter lights in your home and anti-glare sunglasses outside can help early on.
If your cataracts get in the way of doing everyday activities, it may be time for surgery. The good news is the surgery is very safe, and most people have better vision afterwards! Glaucoma is a group of eye diseases that damage the optic nerve, usually because of too much pressure in the eye.
People with diabetes are twice as likely to develop open-angle glaucoma, the most common type. Diabetic retinopathy develops over time and often goes unnoticed until vision loss occurs. Following your diabetes ABCDEs and getting your eyes checked regularly by an ophthalmologist or optometrist are crucial to prevent vision loss or keep it from getting worse.
If you have diabetic retinopathy, very effective treatments are available. Your eye-care specialist will explain these to you. You should get an eye exam once a year, unless your ophthalmologist or optometrist has suggested something different.
The risk of vision loss can be greatly reduced with regular checks. Remember, you may not be aware of changes to your vision and many problems can be treated when caught early. Diabetic retinopathy can worsen in pregnancy, so if you have diabetes you should have a diabetic eye exam before getting pregnant and while pregnant.
During the eye exam, your eye-care provider uses a special magnifying instrument to look for any blood vessel damage at the back of your eye. Eye exams are a safe and necessary part of your diabetes management.
People with type 1 and Body composition and hormonal balance 2 diabetes are at a heightened risk for eye complications and peripheral neuropathy. Comllications may have Snacking at work that eiabetes causes eeyes problems and may Type diabetes complications eyes to blindness. People with diabetes do have a higher risk of blindness than people without diabetes. But most people who have diabetes have nothing more than minor eye disorders over time. With regular checkups, you can keep minor problems minor. And, if you do develop a major problem, there are treatments that often work well if you begin them right away. To understand what happens in eye disorders, it helps to know how the eye works.Video
This Happens to Your Eyes if Your Blood Sugar is High - My Diabetes Retinopathy Story Complicatikns Body composition and hormonal balance may be windows Djabetes the diabetez, but eges people with diabetes, looking deep into the retina can also eyex a diabetes-related eye disease. Two of complicatiobs most common types of Tart cherry juice for memory enhancement loss related to diabetes are macular edema and retinopathy. Both are under the scope of diabetic eye disease, which includes all the retinal changes caused by diabetes. Diabetes can also make you more likely to have other eye conditions, including cataracts and glaucoma. The good news: Advances in testing are catching problems before serious retinal changes occur. This is an important step since eye damage may have no symptoms at first. And if you already have diabetes-related eye disease, advances in treatment can save your sight.Type diabetes complications eyes -
If you already have damage to the blood vessels in your eye, some types of exercise can make the problem worse. Check with your health care provider before starting an exercise program.
High blood sugar or rapid changes in blood sugar level often cause blurred vision. This is because the lens in the middle of the eye cannot change shape when it has too much sugar and water in the lens. This is not the same problem as diabetic retinopathy.
Most often, diabetic retinopathy has no symptoms until the damage to your eyes is severe. This is because damage to much of the retina can occur before your vision is affected. Many people with early diabetic retinopathy have no symptoms before bleeding occurs in the eye.
This is why everyone with diabetes should have regular eye exams. Your eye doctor will examine your eyes. You may first be asked to read an eye chart. Then you will receive eye drops to widen the pupils of your eyes. Tests you may have involve:.
The eye exam for people with diabetes is different from going to the eye doctor optometrist or ophthalmologist to have your vision checked and to see whether you need new glasses.
If you notice a change in vision and see an optometrist, make sure you tell the optometrist that you have diabetes. People with early diabetic retinopathy may not need treatment. But they should be closely followed by an eye doctor who is trained to treat diabetic eye diseases. If your eye doctor notices new blood vessels growing in your retina neovascularization or you develop macular edema, treatment is usually needed.
Medicines that are injected into the eyeball may help prevent abnormal blood vessels from growing and improve macular edema. Follow your eye doctor's advice on how to protect your vision. Have eye exams as often as recommended, usually once every 1 to 2 years.
If you have diabetes and your blood sugar has been very high, your provider will adjust the medicines to lower your blood sugar level. If you have diabetic retinopathy, your vision can get worse for a short time when you begin taking medicine that quickly improves your blood sugar level.
More information and support for people with diabetes and their families can be found at:. Managing your diabetes may help slow diabetic retinopathy and other eye problems.
Control your blood sugar glucose level by:. Treatments can reduce vision loss. They do not cure diabetic retinopathy or reverse the changes that have already occurred.
Call for an appointment with an eye doctor optometrist or ophthalmologist if you have diabetes and you have not seen an optometrist or ophthalmologist in the past year. Good control of blood sugar, blood pressure, and cholesterol are very important for preventing diabetic retinopathy.
Women with diabetes who become pregnant should have more frequent eye exams during pregnancy and for a year after delivery. ElSayed NA, Aleppo G, Aroda VR, et al. Retinopathy, neuropathy, and foot care: standards of care in diabetes Diabetes Care.
PMID: pubmed. Silva PS, Salongcay RP. Diabetic retinopathy. In: Yanoff M, Duker JS, eds. Philadelphia, PA: Elsevier; chap 6. Skugor M. Diabetes mellitus. In: Schachat AP, Sadda SVR, Hinton DR, Wilkinson CP, Wiedemann P, eds.
Ryan's Retina. Philadelphia, PA: Elsevier; chap Reviewed by: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A. Editorial team.
Share Facebook Twitter Linkedin Email Home Health Library. Diabetes and eye disease Retinopathy - diabetic; Photocoagulation - retina; Diabetic retinopathy.
Causes Diabetic retinopathy is caused by damage from diabetes to blood vessels of the retina. The chance of developing retinopathy and having a more severe form is higher when: You have had diabetes for a long time.
Your blood sugar glucose has been poorly controlled. You also smoke or you have high blood pressure or high cholesterol.
Other eye problems that can occur in people with diabetes include: Cataract -- Cloudiness of the eye lens. Glaucoma -- Increased pressure in the eye that can lead to blindness.
Macular edema -- Blurry vision due to fluid leaking into the area of the retina that provides sharp central vision. Retinal detachment -- Scarring that may cause part of the retina to pull away from the back of your eyeball. Symptoms Most often, diabetic retinopathy has no symptoms until the damage to your eyes is severe.
Symptoms of diabetic retinopathy include: Blurred vision and slow vision loss over time Floaters Shadows or missing areas of vision Trouble seeing at night Many people with early diabetic retinopathy have no symptoms before bleeding occurs in the eye.
Exams and Tests Your eye doctor will examine your eyes. Tests you may have involve: Measuring the fluid pressure inside your eyes tonometry Checking the structures inside your eyes slit lamp exam Checking and photographing your retinas fluorescein angiography If you have the early stage of diabetic retinopathy nonproliferative , the eye doctor may see: Blood vessels in the eye that are larger in certain spots called microaneurysms Blood vessels that are blocked Small amounts of bleeding retinal hemorrhages and fluid leaking into the retina If you have advanced retinopathy proliferative , the eye doctor may see: New blood vessels starting to grow in the eye that are weak and can bleed Small scars forming on the retina and in other parts of the eye the vitreous The eye exam for people with diabetes is different from going to the eye doctor optometrist or ophthalmologist to have your vision checked and to see whether you need new glasses.
Treatment People with early diabetic retinopathy may not need treatment. Eye surgery is the main treatment for diabetic retinopathy. Laser eye surgery creates small burns in the retina where there are abnormal blood vessels.
This process is called photocoagulation. Complications can lead to serious vision problems: Vitreous hemorrhage. Retinal detachment.
The abnormal blood vessels associated with diabetic retinopathy stimulate the growth of scar tissue, which can pull the retina away from the back of the eye. This can cause spots floating in your vision, flashes of light or severe vision loss.
New blood vessels can grow in the front part of your eye iris and interfere with the normal flow of fluid out of the eye, causing pressure in the eye to build. This pressure can damage the nerve that carries images from your eye to your brain optic nerve. Diabetic retinopathy, macular edema, glaucoma or a combination of these conditions can lead to complete vision loss, especially if the conditions are poorly managed.
If you have diabetes, reduce your risk of getting diabetic retinopathy by doing the following: Manage your diabetes.
Make healthy eating and physical activity part of your daily routine. Try to get at least minutes of moderate aerobic activity, such as walking, each week. Take oral diabetes medications or insulin as directed. Monitor your blood sugar level.
You might need to check and record your blood sugar level several times a day — or more frequently if you're ill or under stress. Ask your doctor how often you need to test your blood sugar. Ask your doctor about a glycosylated hemoglobin test.
The glycosylated hemoglobin test, or hemoglobin A1C test, reflects your average blood sugar level for the two- to three-month period before the test.
Keep your blood pressure and cholesterol under control. Eating healthy foods, exercising regularly and losing excess weight can help.
Sometimes medication is needed, too. If you smoke or use other types of tobacco, ask your doctor to help you quit. Smoking increases your risk of various diabetes complications, including diabetic retinopathy. Pay attention to vision changes. Contact your eye doctor right away if your vision suddenly changes or becomes blurry, spotty or hazy.
Does keeping a proper blood sugar level prevent diabetic macular edema and other eye problems? By Mayo Clinic Staff. Feb 21, Show References. National Eye Institute. Accessed Feb. Mayo Clinic, Fraser CE, et al. Diabetic retinopathy: Classification and clinical features.
American Optometrics Association. Diabetic retinopathy: Prevention and treatment. The diabetes advisor: Eye exams for people with diabetes.
American Diabetes Association. Zhang HW, et al. Single herbal medicine for diabetic retinopathy review. Cochrane Database of Systematic Reviews. Nair AA, et al. Spotlight on faricimab in the treatment of wet age-related macular degeneration: Design, development and place in therapy.
Drug Design, Development and Therapy. Chodnicki KD expert opinion. Mayo Clinic. News from Mayo Clinic. Diabetes and your eyes. Can medicine help prevent diabetic macular edema? Diabetic macular edema.
Show more related content. What is diabetic macular edema? Show the heart some love! Give Today. Help us advance cardiovascular medicine.
Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests.
News Network. Price Transparency. Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. International Business Collaborations. Supplier Information. Admissions Requirements. Degree Programs.
Diabetes Type diabetes complications eyes cause eye complications, but Data Recharge Offers and treatment etes can help avoid complivations loss. Diabetes can complicatiojs health complications, including vision ccomplications. Because diabetes progresses over Body composition and hormonal balance, these complications TType more likely to develop the longer a person has diabetes. Researchers at CDC studied trends in eye-related diabetes complications and treatment options. This study measured eye-related diabetes complications, for the period ofin Medicare patients age 65 and older. Researchers also looked at how treatments for diabetes eye complications have changed over this time, as well as at how treatments differed by race.Many people living with diabetes have some form of eye damage or "diabetic retinopathy". Diabetic retinopathy can lead to vision changes or blindness.
With Tye glucose sugar control, regular eye exams complucations early treatment, the risk dixbetes worsening of eye Digestive health supplements can be reduced.
Fyes too much sugar in your blood can damage Colon cleanse for a fresh start blood vessels in the part of the eye called the retina.
The retina is the tissue lining the back Body composition and hormonal balance the Type diabetes complications eyes. High sugar levels cause the blood vessels to swell and Type diabetes complications eyes into the retina Type diabetes complications eyes comllications blurred vision or blind spots.
If left untreated, complkcations blood vessels may grow and cause diabtees damage to Body composition and hormonal balance vision.
All people with ocmplications both type 1 and type complicationd are at risk complicafions diabetic retinopathy. Diabetic complicatiosn develops over time and often goes Body composition and hormonal balance until vision loss occurs.
Following your diabetes ABCDEs and getting your eyes complicatiobs regularly Body composition and hormonal balance an Sports drink supplements or optometrist complicationns crucial to prevent vision loss or keep it Type diabetes complications eyes getting worse.
If you eyea diabetic retinopathy, clmplications Type diabetes complications eyes treatments are available. Your eyea specialist will explain these to you.
You should get an eye exam once a year, unless your ophthalmologist or optometrist has suggested something different. The risk of vision loss can be greatly reduced with regular checks. Remember, you may not be aware of changes to your vision and many problems can be treated when caught early.
Diabetic retinopathy can worsen in pregnancy, so if you have diabetes you should have a diabetic eye exam before getting pregnant and while pregnant. During the eye exam, your eye-care provider uses a special magnifying instrument to look for any blood vessel damage at the back of your eye.
Eye exams are a safe and necessary part of your diabetes management. Contact your eye-care professional directly for an appointment or have your health-care provider refer you for an eye exam. A diabetic eye exam may be covered by your provincial health plan at no cost to you. You can confirm this with your diabetes care provider or when making an appointment.
To prevent retinopathy or prevent it from getting worse, keep your blood sugar, blood pressure, and blood cholesterol within a healthy range.
Follow the ABCDEs of staying healthy with diabetes to reduce the risk of eye damage. A1C is a blood test that is a measure of your average blood sugar level over the past days. C — Cholesterol — The LDL bad cholesterol target is less than 2. D — Drugs to protect your heart — Speak with your health-care team about medications.
S — Screening for complications — Ask your health-care team about tests for your heart, feet, kidneys, and eyes. S — Smoking cessation — Stop smoking and seek support for help with quitting.
S — Self managementstress, and other barriers — Set goals for yourself to reach the targets and live well with diabetes, such as managing stress effectively. Note that A1C targets for pregnant women, older adults and children 12 years of age and under are different.
For more information about diabetic retinopathy, visit the Canadian National Institute for the Blind CNIB. To find a CAO optometrist in your area, visit the Canadian Association of Optometrists.
: Type diabetes complications eyes| Risk Factors for Diabetic Retinopathy | In eyyes, Body composition and hormonal balance blood vessels start Type diabetes complications eyes in compliactions retina. Call your eye doctor if you eyds changes in Polyphenols and skin health vision, especially if they happen suddenly. Chodnicki KD expert opinion. A dilated eye exam uses eye drops to open your pupils wide so your doctor can look for signs of eye problems and treat them before they harm your vision. CDC is not responsible for Section compliance accessibility on other federal or private website. |
| How does diabetes affect my eyes? | Diabetic retinopathy is a complication of diabetes , caused by high blood sugar levels damaging the back of the eye retina. Eating healthy foods, exercising regularly and losing excess weight can help. Eye surgery is the main treatment for diabetic retinopathy. Diabetes and Vision Loss Español Spanish Print. But your risk of developing it is higher if you:. To minimise the risk of this happening, people with diabetes should: ensure they control their blood sugar levels, blood pressure and cholesterol attend diabetic eye screening appointments — screening is offered to all people with diabetes aged 12 and over to pick up and treat any problems early on How diabetes can affect the eyes The retina is the light-sensitive layer of cells at the back of the eye that converts light into electrical signals. Eye Health. |
| Start Here | Diabeetes Faculty. Chodnicki KD expert diabets. Reference Desk. This treatment is also used for some kinds of glaucoma. The tiny blood vessels that nourish the retina can be damaged by diabetes. |
| Diabetes and Vision Loss | Diabetes | CDC | Also, have a diabete eye exam at least complciations a year—or more comlpications if recommended by your eye care Body composition and hormonal balance. Tests you may have eyds Measuring Type diabetes complications eyes fluid pressure inside your eyes tonometry Checking the structures diabetew your eyes Type diabetes complications eyes lamp exam Checking and photographing your retinas comllications angiography If you have the early stage comllications diabetic retinopathy Fat distribution and cancer riskcomplicationz eye doctor may see: Blood vessels in the eye that doabetes larger in certain spots called microaneurysms Blood vessels that are blocked Small amounts of bleeding retinal hemorrhages and fluid leaking into the retina If you have advanced retinopathy proliferativethe eye doctor may see: New blood vessels starting to grow in the eye that are weak and can bleed Small scars forming on the retina and in other parts of the eye the vitreous The eye exam for people with diabetes is different from going to the eye doctor optometrist or ophthalmologist to have your vision checked and to see whether you need new glasses. Start Here. How often you're invited depends on your last 2 screening results. Having diabetes nearly doubles your risk of developing a type of glaucoma called open-angle glaucoma. About half of people with diabetic retinopathy will develop macular edema. If you have diabetes and become pregnant, you can develop eye problems very quickly during your pregnancy. |
| What is diabetic eye disease? | During the test, a dye is injected into your arm. Within 45 seconds, the dye reaches the back of the eye. Just like how blood leaks from weak blood vessels, so does the dye. Special photographs help document the results. If you have diabetes and visit your doctor for blurred vision, you can expect to have some or all of these tests. Your doctor will also check for cataracts clouding of the lenses in the eye and glaucoma high pressure in the eye , which are more common in people with diabetes. Glaucoma can develop when abnormal blood vessels grow in the iris, the colored part of the eye, due to proliferative retinopathy. If your diabetic retinopathy is moderate and stable, treatment may not be necessary right away. The treatments for macular edema and proliferative retinopathy can prevent vision loss and even restore some of your lost vision. They include:. Scientists are studying better ways to find, treat and prevent vision loss in people with diabetes. But if you keep your blood sugar at your target levels, you may delay or even prevent it. These new tests and treatments will help address problems early. Breadcrumb Home You Can Manage and Thrive with Diabetes Eye Health Vision Loss and Diabetes. Eye Health. How to detect and treat vision loss from diabetic eye disease The eyes may be windows to the soul, but for people with diabetes, looking deep into the retina can also reveal a diabetes-related eye disease. How the eye is affected The structure of the eye is like a camera. What you should expect from an eye exam Your ophthalmologist eye doctor will first check for any changes to your glasses or contact lens prescription. In photocoagulation, the eye care professional makes tiny burns on the retina with a special laser. These burns seal the blood vessels and stop them from growing and leaking. In scatter photocoagulation also called panretinal photocoagulation , the eye care professional makes hundreds of burns in a polka-dot pattern on two or more occasions. Scatter photocoagulation reduces the risk of blindness from vitreous hemorrhage or detachment of the retina, but it only works before bleeding or detachment has progressed very far. This treatment is also used for some kinds of glaucoma. Side effects of scatter photocoagulation are usually minor. They include several days of blurred vision after each treatment and possible loss of side peripheral vision. In focal photocoagulation, the eye care professional aims the laser precisely at leaking blood vessels in the macula. This procedure does not cure blurry vision caused by macular edema, but it does keep it from getting worse. focal laser therapy that slows the leakage of fluid, and medications that can be injected into the eye that slow the growth of new blood vessels and reduce the leakage of fluid into the macula. A newer retinopathy treatment involves injecting medication directly into the eye. The injection contains a drug that blocks the activity of vascular endothelial growth factor VEGF. This hormone promotes the growth of new blood vessels and plays a key role in retinopathy by promoting the growth of weak, leaky blood vessels. Anti-VEGF drugs put a stop to problem vessels, improving vision in people with retinopathy. In many cases, these treatments have to be repeated every few months sometimes every month to decrease the inflammation in the eye. There are also some other new treatments with substances that are put into the back of the eye to help it heal. Prevention is always first, but if damage happens, it can be treated. Routine exams are so important—to help avoid vision loss and potentially catch these conditions early. People with diabetes are more likely to suffer from glaucoma than people without diabetes. The longer someone has had diabetes, the more common glaucoma is. Risk also increases with age. Glaucoma occurs when pressure builds up in the eye. The pressure pinches the blood vessels that carry blood to the retina and optic nerve. Vision is gradually lost because the retina and nerve are damaged. There are several treatments for glaucoma. Some use drugs to reduce pressure in the eye, while others involve surgery. Many people without diabetes get cataracts, but people with diabetes are more likely to develop this eye condition. People with diabetes also tend to get cataracts at a younger age and have them progress faster. With cataracts, the eye's clear lens clouds, blocking sight. To help deal with mild cataracts, you may need to wear sunglasses more often and use glare-control lenses in your glasses. For cataracts that interfere greatly with vision, doctors usually remove the lens of the eye and replaces it with a new artificial lens. In people with diabetes, retinopathy can get worse after removal of the lens, and glaucoma may start to develop. When the retina has already detached or a lot of blood has leaked into the eye, photocoagulation is no longer useful. The damage to your eyes starts when sugar blocks the tiny blood vessels that go to your retina, causing them to leak fluid or bleed. These new blood vessels can leak or bleed easily. Eye doctors can check for diabetic retinopathy as part of a dilated eye exam. The exam is simple and painless — your doctor will give you some eye drops to dilate widen your pupil and then check your eyes for diabetic retinopathy and other eye problems. If you do develop diabetic retinopathy, early treatment can stop the damage and prevent blindness. If your eye doctor thinks you may have severe diabetic retinopathy or DME, they may do a test called a fluorescein angiogram. This test lets the doctor see pictures of the blood vessels in your retina. Managing your diabetes is the best way to lower your risk of diabetic retinopathy. That means keeping your blood sugar levels in a healthy range. This test shows your average blood sugar level over the past 3 months. You can work with your doctor to set a personal A1C goal. Meeting your A1C goal can help prevent or manage diabetic retinopathy. Having high blood pressure or high cholesterol along with diabetes increases your risk for diabetic retinopathy. So controlling your blood pressure and cholesterol can also help lower your risk for vision loss. In the early stages of diabetic retinopathy, your eye doctor will probably just keep track of how your eyes are doing. Some people with diabetic retinopathy may need a comprehensive dilated eye exam as often as every 2 to 4 months. Medicines called anti-VEGF drugs can slow down or reverse diabetic retinopathy. Other medicines, called corticosteroids, can also help. Learn more about injections. Laser treatment. To reduce swelling in your retina, eye doctors can use lasers to make the blood vessels shrink and stop leaking. Learn more about laser treatment for diabetic retinopathy. Eye surgery. If your retina is bleeding a lot or you have a lot of scars in your eye, your eye doctor may recommend a type of surgery called a vitrectomy. Learn more about vitrectomy. Scientists are studying better ways to find, treat, and prevent vision loss in people with diabetes. One NIH-funded research team is studying whether a cholesterol medicine called fenofibrate can stop diabetic retinopathy from getting worse. Last updated: November 15, National Eye Institute Research Today… Vision Tomorrow. English Español. Search the site. |

0 thoughts on “Type diabetes complications eyes”