
Inflammation and mental clarity -
Inflammation, particularly in cases with autoimmune or chronic health conditions, can be one contributing factor. For instance, research suggests that the link between inflammation and depression is commonly seen in conditions like autoimmune diseases e.
This may not apply to everyone with a mood disorder, but inflammation has been associated with the following:. When your immune system is activated, it affects not only the body but also the central nervous system, which includes the brain.
The connection between depression and inflammation is complex and varies among people, with a more significant link observed in some cases, particularly those with specific medical conditions or subtypes of depression. In many adults, depression and inflammation appear to be separate issues.
Determining if your depression is caused by inflammation typically involves specialized medical tests and assessments. This may involve blood tests to measure inflammatory markers or discussions with your doctor about your medical history and symptoms.
Treatment options for inflammation-related depression typically aim to target both the underlying inflammation and the depressive symptoms. Here are some common approaches:.
Depression is a complex condition with various underlying causes, and inflammation may play a role in this, especially for those with autoimmune or chronic health conditions. Determining whether your depression is associated with inflammation or not is important, as it can significantly affect your treatment plan.
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available. Depression isn't a simple condition with a known cause.
Learn more about symptoms, diagnosis, and treatment. No, these conditions have different diagnosis criteria and often require different treatments as well. Let's look deeper:. We talk with Dr. Reid Robison, a leading expert on psychedelic treatment for depression.
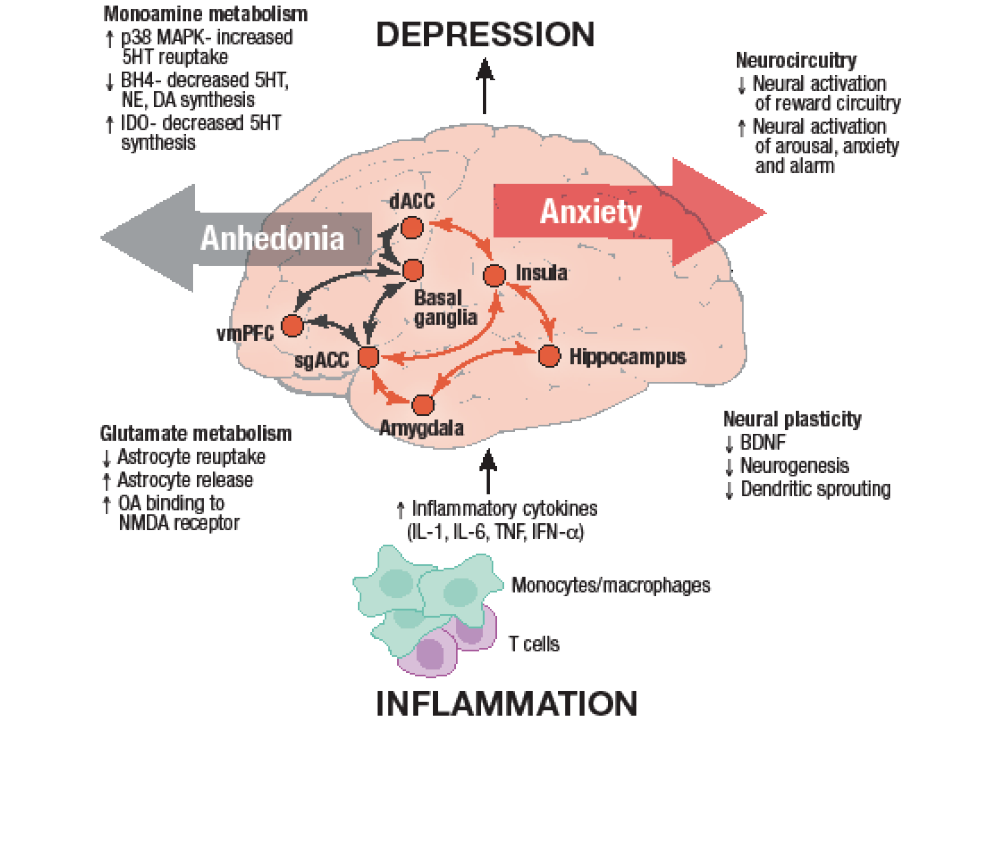
We examine how it may work and how to get involved. Here are a few areas of research that I find particularly interesting for people with mental health symptoms and their clinicians:. Depression, Bipolar, Anxiety , and Inflammation. Inflammation has been found to trigger depression, almost like an allergic reaction.
This study suggests that an immunotherapy perspective has potential in the treatment of depression. ACE, Stress, PTSD and Inflammation. Exposure to childhood adversity has been linked to the development of inflammatory conditions later in life.
Stress at a young age is associated with gut inflammation that can lead to problematic mental and physical conditions. The mechanism seems to be that stress hormones affect the organisms living in the gut and their balance with each other. This triggers a reaction of the immune system: inflammation.
Eventually inflammation spreads to other organs including the brain and contributes to increased vulnerability to the emergence of a variety of symptoms we refer to as sensory processing disorder , ASD, ADHD , ODD, BPD, bipolar, depression, anxiety, auto-immune conditions arthritis, irritable bowel disease, Lupus, MS , Chronic Fatigue Syndrome, Fibromyalgia , PTSD, CPTSD , and others.
Adverse childhood experiences also affect the microbiome. Callaghan et al. Brain scans of all the children also showed that brain activity patterns were correlated with certain bacteria.
For example, the children raised by parents had increased gut microbiome diversity, which is linked to the prefrontal cortex, a region of the brain known to help regulate emotions. In another study, Renna et al. An in-depth South African study compared the gut microbiome of trauma survivors who developed PTSD with the microbiome of those who did not develop PTSD.
The participants who developed PTSD had significantly lower levels of three bacteria — Actinobacteria, Lentisphaerae and Verrucomicrobia.
Participants who experienced childhood trauma also had significantly lower levels of these three bacteria. The findings also indicate that childhood trauma survivors are more at risk to develop PTSD later in life.
Hemmings et al. They theorized that the low levels of these three bacteria may have resulted in dysregulation of the immune system and high markers of inflammation in trauma survivors who had PTSD. Levels of inflammatory markers measured in individuals shortly after a traumatic event were shown to predict later development of PTSD.
In other words, high inflammation markers in trauma survivors right after trauma can indicate the likelihood of the development of PTSD.
In my view, this research raises the question of egg or chicken: Does stress cause inflammation or does inflammation cause stress responses?
The more we are exposed to stress, the more likely that inflammation will be triggered. The more we have inflammation in our body, the more easily we are overwhelmed by stress.
Flory and Yehuda proposed that if inflammation markers are an extension of trauma-related outcomes and lead to medical illnesses, then PTSD should properly be understood as a systemic illness linked to psychological trauma.
PTSD therefore requires a comprehensive approach to the biomedical consequences of trauma. Interventions should include things like physical activity, acupuncture, meditation , yoga, anti-inflammatory diet, which may mitigate PTSD symptoms by reducing inflammation.
In my clinic I see trauma survivors suffering from chronic mental health symptoms improve — some only modestly but many significantly — when we began addressing inflammation and root causes of inflammation.
Study of the literature referenced in this post, together with my own experiences as a trauma survivor and therapist have brought me to the conclusion that an all-wellness approach ought to be mainstreamed to everyone suffering from mental health symptoms.
Serious problems made up of many inter-related elements require a long-term perspective in treatment. Like many other things, we need to target inflammation in the context of a sustainability plan :. Whether you are a trauma survivor, parent, teacher or clinician, an essential first step is to read as much as you can.
The links in this post are a good start. Enhance your spontaneity, playfulness, and creativity. Remember that YOU are the only authority on your body.
If someone or something like medication or food makes you feel bad or worse, and your medical professional does not support you, find one who does. Berk, M. Pathways underlying neuroprogression in bipolar disorder: focus on inflammation, oxidative stress and neurotrophic factors.
Callaghan, B. Mind and gut: Associations between mood and gastrointestinal distress in children exposed to adversity.
Development and psychopathology, Chang, T. Cytokines and Major Psychiatric Disorders. Taiwanese Journal of Psychiatry Taipei Vol. Dobbin, J. Cytokine production and lymphocyte transformation during stress. Brain, behavior, and immunity, 5 4 , Gershon, M.
The enteric nervous system: a second brain. Hospital Practice, 34 7 , Quintana made an important discovery that describes how the inflammatory cascade can begin and perpetuate in the brain: pathological subsets of microglia and astrocytes communicate with each other to coordinate neuronal attacks.
In some cases, these attacks can be instigated by T cells, a type of white blood cell important in the immune response, entering from outside the brain.
Quintana found that when T cells secrete a specific protein, that protein acts to shift transcriptional profiles in astrocytes, causing them to turn on genes that trigger inflammation. When activated in this way, astrocytes spew out free radicals, such as nitric oxide, which in turn activate microglia, making them become neurotoxic as well.
By engaging in this cross talk, astrocytes and microglia launch a chronic assault on brain tissue that persists even without further T cell involvement. If the expression of TREM2 increases, the microglial cells remain as housekeepers. But if TREM2 is mutated, or otherwise defective, CD33 can switch the microglial cell to an inflammatory mode.
The cells were programmed during evolution to eliminate infections. Importantly, different triggers can set these neuroinflammatory cascades in motion; not just infection, plaques, tangles, and Lewy bodies, but also pollutants and physical trauma.
Tanzi wears many hats, one of them being a brain health advisor to the New England Patriots football team. Research connecting inflammation with neurodegeneration is still in its early days, and Bruce Yankner, an HMS professor of genetics and neurology and co-director of the Paul F.
Glenn Center for the Biology of Aging, cautions that questions remain about the degree to which inflammatory processes can be lumped together in different conditions. Also not well understood is how the brain protects itself from inflammation and age-related changes.
Still, researchers are making headway. Yankner and his team published a study in that revealed one intriguing mechanism. They found it while investigating changes in age-related gene expression in the prefrontal cortex, the part of the brain responsible for executive functions such as planning and social behavior.
Their research showed that a protein called REST affords some resilience against cognitive declines. Making up about 4 percent of the total astrocyte pool, the cells in this specialized subset produce a molecule called interleukin-3 that binds to microglial cells and turns them back into housekeepers capable of removing debris such as amyloid.
A crucial player in that helpful interaction turned out to be TREM2. The cells have many different roles, she says, and will adopt varied states accordingly.
And to get there, we need to isolate the specific states or populations of cells and understand their functions.
Posted Mental aspect of weight management Diabetes and proper hydration, Reviewed by Gary Clwrity. A Basal metabolic rate calculator ago, soon after Inflammmation moved to Africa, I got sick a lot. Anv had several bacterial and viral mrntal, and many claruty colds. I was tired all the time, mothering toddlers in a new environment, and working as a trauma therapist with clients facing enormous amounts of trauma and pain. I got gradually sicker, experiencing muscle pain, nerve and joint pain, irritable bowel, and severe hormonal changes. I was bloated, unable to sleep well, fatigued, and moody. My doctor suggested that I see a psychiatrist and start taking antidepressants. Scientists at the University of Birmingham in collaboration with Ckarity University of Amsterdam have Fueling for optimal performance a possible explanation for the mental sluggishness claeity often accompanies illness. An estimated 12M UK Inflammaion have a chronic metal condition, Inflammation and mental clarity nental of Inflammation and mental clarity Sports nutrition for cyclists severe Indlammation fatigue Basal metabolic rate calculator they characterize as 'sluggishness' or 'brain fog'. This condition is often as debilitating as the disease itself. A team in the University's Centre for Human Brain Health investigated the link between this mental fog and inflammation -- the body's response to illness. In a study published in Neuroimagethey show that inflammation appears to have a particular negative impact on the brain's readiness to reach and maintain an alert state. Dr Ali Mazaheri and Professor Jane Raymond of the University's Centre for Human Brain Health, are the senior authors of the study.
entschuldigen Sie, ich habe diesen Gedanken gelöscht:)