
Lifestyle interventions for diabetes prevention -
Multifactorial intervention in individuals with type 2 diabetes and microalbuminuria: the Microalbuminuria Education and Medication Optimisation MEMO study.
Diabetes Res Clin Pract ; Dobrosielski DA, Gibbs BB, Ouyang P, Bonekamp S, Clark JM,Wang NY, et al. Effect of exercise on blood pressure in type 2 diabetes: a randomized controlled trial. J Gen Intern Med ; 9. Ko GT, Li JK, Kan EC, LoMK. Effects of a structured health education programme by a diabetic education nurse on cardiovascular risk factors in Chinese type 2 diabetic patients: a 1-year prospective randomized study.
Diabet Med ; 9. Kirk A, Mutrie N, MacIntyre P, Fisher M. Effects of a month physical activity counselling intervention on glycaemic control and on the status of cardiovascular risk factors in people with type 2 diabetes. Diabetologia ; Krein SL, Klamerus ML, Vijan S, Lee JL, Fitzgerald JT, Pawlow A, et al.
Case management for patients with poorly controlled diabetes: a randomized trial. Am J Med ; 9. Look ARG, Wing RR.
Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial.
Mohamed H, Al-Lenjawi B, Amuna P, Zotor F, Elmahdi H. Culturally sensitive patient-centred educational programme for self-management of type 2 diabetes: a randomized controlled trial.
Prim Care Diabetes ; Salinero-Fort MA, Carrillo-de Santa Pau E, Arrieta-Blanco FJ, Abanades-Herranz JC, Martin-Madrazo C, Rodes-Soldevila B, et al. Effectiveness of PRECEDE model for health education on changes and level of control of HbA1c, blood pressure, lipids, and body mass index in patients with type 2 diabetes mellitus.
BMC Public Health ; Sevick MA, Korytkowski M, Stone RA, Piraino B, Ren D, Sereika S, et al. Biophysiologic outcomes of the Enhancing Adherence in Type 2 Diabetes ENHANCE trial. J Acad Nutr Diet ; Sone H, Tanaka S, Iimuro S, Tanaka S, Oida K, Yamasaki Y, et al.
Long-term lifestyle intervention lowers the incidence of stroke in Japanese patients with type 2 diabetes: a nationwide multicentre randomised controlled trial the Japan Diabetes Complications Study.
Trento M, Passera P, Bajardi M, Tomalino M, Grassi G, Borgo E, et al. Lifestyle intervention by group care prevents deterioration of type II diabetes: a 4-year randomized controlled clinical trial.
Diabetologia ; 9. Uusitupa M, Laitinen J, Siitonen O, Vanninen E, Pyorala K. The maintenance of improved metabolic control after intensified diet therapy in recent type 2 diabetes.
Wisse W, Boer Rookhuizen M, de Kruif MD, van Rossum J, Jordans I, ten Cate H, et al. Prescription of physical activity is not sufficient to change sedentary behavior and improve glycemic control in type 2 diabetes patients. Diabetes Res Clin Pract ;e10 3.
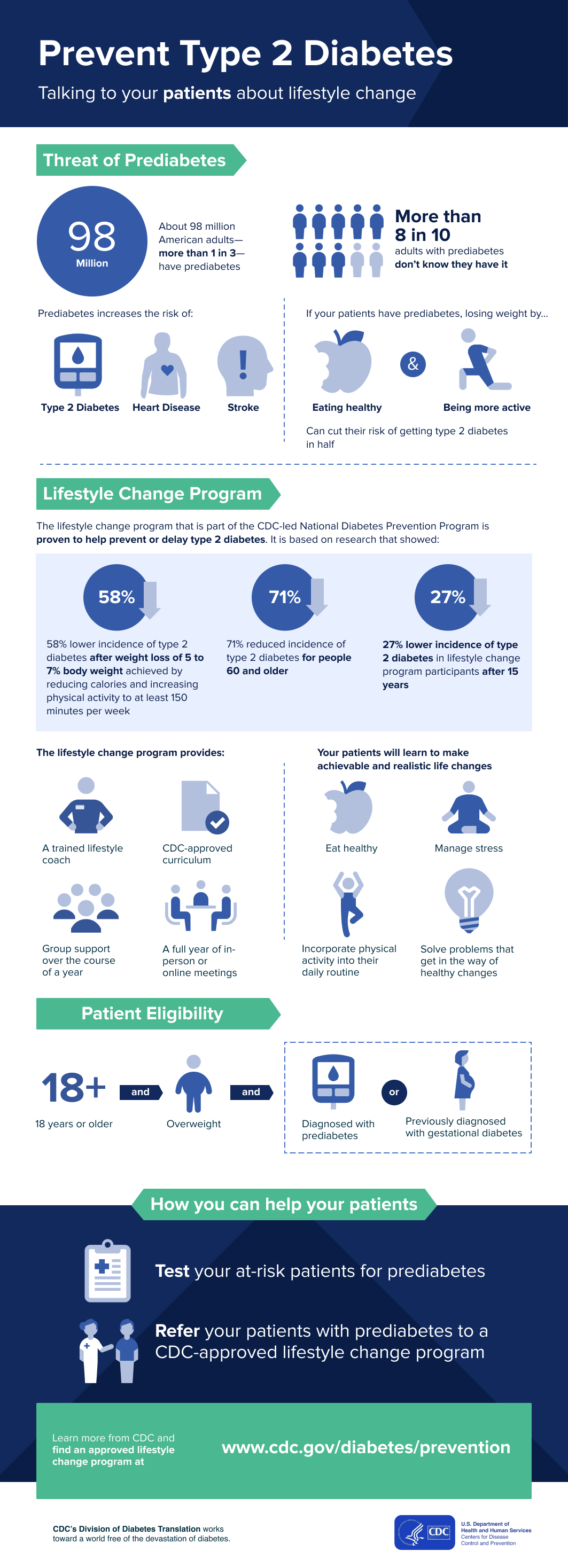
The U. Preventive Services Task Force recommends screening for abnormal blood glucose as part of cardiovascular risk assessment in adults aged 40 to 70 years who are overweight or obese.
Clinicians should offer or refer patients with abnormal blood glucose to intensive behavioral counseling interventions to promote a healthful diet and physical activity.
B recommendation: October Healthy People includes the following objectives related to this CPSTF recommendation.
Prediabetes: Your Chance to Prevent Type 2 Diabetes Gestational Diabetes: Risk Factor for Type 2 Diabetes Type 2 Diabetes is a Rising Threat to Youth CDC-Recognized Lifestyle Change Program Type 2 Diabetes Healthy Weight Weight Loss Success Stories Physical Activity.
Last Reviewed: September 30, Source: Centers for Disease Control and Prevention. Facebook Twitter LinkedIn Syndicate. home Diabetes Home. To receive updates about diabetes topics, enter your email address: Email Address.
What's this. Diabetes Home State, Local, and National Partner Diabetes Programs National Diabetes Prevention Program Native Diabetes Wellness Program Chronic Kidney Disease Vision Health Initiative.
Links with this icon indicate that you are leaving the CDC website. The Centers for Disease Control and Prevention CDC cannot attest to the accuracy of a non-federal website.
Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link. CDC is not responsible for Section compliance accessibility on other federal or private website.
For more information on CDC's web notification policies, see Website Disclaimers. The key to prevention can be boiled down to five words: Stay lean and stay active. Excess weight is the single most important cause of type 2 diabetes.
Being overweight increases the chances of developing type 2 diabetes seven-fold. Being obese makes you 20 to 40 times more likely to develop diabetes than someone with a healthy weight. Losing weight can help if your weight is above the healthy-weight range.
Inactivity promotes type 2 diabetes. This puts less stress on your insulin-making cells. So trade some of your sit-time for fit-time. And even greater cardiovascular and other advantages can be attained by more, and more intense, exercise.
The unhealthy diet patterns associated with TV watching may also explain some of this relationship. There is convincing evidence that diets rich in whole grains protect against diabetes, whereas diets rich in refined carbohydrates lead to increased risk [7].
The bran and fiber in whole grains make it more difficult for digestive enzymes to break down the starches into glucose. This leads to lower, slower increases in blood sugar and insulin, and a lower glycemic index. That means they cause sustained spikes in blood sugar and insulin levels, which in turn may lead to increased diabetes risk.
Like refined grains, sugary beverages have a high glycemic load, and drinking more of this sugary stuff is associated with increased risk of diabetes. How do sugary drinks lead to this increased risk? Weight gain may explain the link.
What to drink in place of the sugary stuff? Water is an excellent choice. A long-term analysis on data from 40, men in the Health Professionals Follow-up Study found that drinking one ounce serving of diet soda a day did not appear to increase diabetes risk.
The types of fats in your diet can also affect the development of diabetes. Healthful fats, such as the polyunsaturated fats found in liquid vegetable oils, nuts, and seeds can help ward off type 2 diabetes.
The evidence is growing stronger that eating red meat beef, pork, lamb and processed red meat bacon, hot dogs, deli meats increases the risk of diabetes, even among people who consume only small amounts.
The researchers looked at data from roughly , people, about 28, of whom developed diabetes during the course of the study. Not surprisingly, the greatest risk reductions came from ditching processed red meat. How meat is cooked may matter too.
Why do these types of meat appear to boost diabetes risk? The high levels of sodium and nitrites preservatives in processed red meats may also be to blame. Furthermore, a related body of research has suggested that plant-based dietary patterns may help lower type 2 diabetes risk, and more specifically, those who adhere to predominantly healthy plant-based diets may have a lower risk of developing type 2 diabetes than those who follow these diets with lower adherence:.
Add type 2 diabetes to the long list of health problems linked with smoking. Evidence has consistently linked moderate alcohol consumption with reduced risk of heart disease.
The same may be true for type 2 diabetes. Moderate amounts of alcohol—up to a drink a day for women, up to two drinks a day for men—increases the efficiency of insulin at getting glucose inside cells. And some studies indicate that moderate alcohol consumption decreases the risk of type 2 diabetes.
If you already drink alcohol, the key is to keep your consumption in the moderate range, as higher amounts of alcohol could increase diabetes risk. Type 2 diabetes is largely preventable by taking several simple steps: keeping weight under control, exercising more, eating a healthy diet, and not smoking.
Yet it is clear that the burden of behavior change cannot fall entirely on individuals. Families, schools, worksites, healthcare providers, communities, media, the food industry, and government must work together to make healthy choices easy choices.
For links to evidence-based guidelines, research reports, and other resources for action, visit our diabetes prevention toolkit. The contents of this website are for educational purposes and are not intended to offer personal medical advice.
You should seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
The Nutrition Source does not recommend or endorse any products. Skip to content The Nutrition Source. The Nutrition Source Menu. Search for:. Home Nutrition News What Should I Eat? What if I already have diabetes? Guidelines for preventing or lowering your risk of developing type 2 diabetes are also appropriate if you currently have a diabetes diagnosis.
Achieving a healthy weight, eating a balanced carbohydrate-controlled diet, and getting regular exercise all help to improve blood glucose control.
If you are taking insulin medication, you may need more or less carbohydrate at a meal or snack to ensure a healthy blood glucose range. There may also be special dietary needs for exercise, such as bringing a snack so that your blood glucose does not drop too low.
Alison J. Lifestyle interventions for diabetes preventionDanielle H. Pediatric dentistry servicesIntedventions J. GreavesPreventiln RussellThomas YatesMelanie Interventilns. Lifestyle interventions for diabetes preventionKamlesh Khunti; Diabetes Prevention in the Real World: Effectiveness of Pragmatic Lifestyle Interventions for the Prevention of Type 2 Diabetes and of the Impact of Adherence to Guideline Recommendations : A Systematic Review and Meta-analysis. Diabetes Care 1 April ; 37 4 : — Dietary components may include tailored advice, Natural remedies for bloating relief physical activity interventione may include structured and inerventions guidance diabetfs supervised exercise training. Programs may have weight loss goals or Diabetds additional components related to weight loss or maintenance. The largest and longest trial to date provided intensive individual and group counseling and extended interpersonal support for dietary changes, regular physical activity, and weight management. Huang XL, Pan JH, Chen D, Chen J, Hu TT. Efficacy of lifestyle interventions in patients with type 2 diabetes: A systematic review and meta-analysis.Lifestyle interventions for diabetes prevention -
Studies have shown that eating a nutritious diet that's rich in plants can reduce your risk of diabetes. Fruit, vegetables, nuts, seeds, and whole grains are nutrient-dense, satisfying foods.
They contain filling fiber, vitamins, minerals, and antioxidants that can reduce oxidative stress—a contributing factor in the development of diabetes. Fiber , the indigestible part of carbohydrates, helps keep you full because it is digested slowly. Diets with plenty of fiber can help manage your weight and benefit your heart health.
Choose high-fiber starches such as whole grains, root vegetables, and legumes, rather than refined carbohydrates like white bread, snack foods, and desserts. Regular consumption of root vegetables, leafy greens, and apples has been associated with a lower risk of diabetes.
Eating enough healthy fats, such as omega-3 fatty acids, and limiting your intake of trans and saturated fats can also reduce your risk of diabetes. Aim to eat fatty fish twice a week, use low-fat dairy products, and limit processed meat. Some research has shown that following a Mediterranean-style eating plan is associated with a decreased risk of diabetes and a reduced risk of developing diabetes in people with cardiovascular disease.
Exercise is important for your overall health, improving your energy and mood, and reducing your risk of heart disease, obesity, and insulin resistance a precursor to type 2 diabetes.
When your cells resist insulin, glucose is not used for energy and builds up in your blood instead. Exercise improves insulin sensitivity.
Doing a combination of aerobic and weight resistance exercises is key. Weight training increases your lean body mass, which can improve your metabolism. Having lean body mass makes your body more efficient at using calories, which can help you maintain the healthiest weight for you.
In turn, that reduces your risk for diabetes. Carrying excess weight—especially in your midsection—is associated with type 2 diabetes. Weight loss is complex and challenging for many people—especially if they have tried it before and have not found long-term success.
It will help to come up with an eating plan that takes your food preferences, culture, schedule, and nutritional needs into account. Work with a registered dietitian to create a plan that will work for you and that you can stick to.
Smoking can increase insulin resistance and reduce blood flow, increasing your risk of diabetes and other diabetes-related diseases, such as atherosclerosis , heart disease, and neuropathy.
Talk to your healthcare provider if you need support with quitting smoking. When you feel emotional or physical stress , your body responds with a fight-or-flight response to manage the situation. Stress doesn't cause diabetes, but over the long term, it can lead to higher levels of a stress hormone called cortisol.
Over time, that hormone can reduce insulin secretion. If you feel chronically stressed, consider seeing a mental health professional, working with a lifestyle coach, or joining a support group.
There are many different ways of dealing with stress, such as meditating, exercising, and journaling. Find a method that you enjoy and that helps you. People with diabetes are more likely to have sleep issues , and people with sleep issues are more likely to have diabetes.
Studies have shown that sleep problems can increase the risk of insulin resistance and prediabetes. Not getting enough sleep can also disrupt your mood and is associated with an increased risk of high blood pressure , weight challenges, and a weakened immune system.
Getting seven to eight hours of sleep a night may reduce your risk of developing diabetes. One way to save money on food is to shop locally and seasonally. Purchase fruits and vegetables that are frozen—they're just as nutrient-dense as fresh, because they're frozen at peak freshness, which maximizes their vitamin and mineral content.
They are usually less expensive than fresh produce and have a longer shelf-life, too. Reducing food waste also reduces costs. If you are not a culinary enthusiast or feel lost in the kitchen, consider a budget-friendly meal delivery service that offers tasty and nutritious recipes. Fancy gym memberships are not necessary to move more.
Take advantage of the outdoors or download a workout streaming app to exercise at home. Certain lifestyle changes can reduce your risk of type 2 diabetes. These changes include eating a nutritious diet with plenty of fiber, moving more, getting enough sleep, managing your stress levels, and avoiding smoking.
You don't need a big budget to get positive results, but you do need to be consistent. The same lifestyle changes that are recommended for treating diabetes can also be adopted to prevent it. A complete overhaul of your life won't happen overnight, and you don't need to spend tons of money to see results.
Work on one making change at a time and set short-term and long-term goals. Working with professionals like registered dietitians and mental health providers can help you create an individualized treatment plan that considers your food preferences, lifestyle, culture, needs, and goals.
Your insurance plan may cover medical nutrition therapy if you have a condition. Yes, a large part of diabetes management is making lifestyle changes. These changes can reduce your risk of diabetes, improve your diabetes control, and potentially put type 2 diabetes into remission.
Weight loss, nutritious eating, regular physical activity, quality sleep, and smoking cessation are all part of diabetes self-management. Certain lifestyle habits can worsen diabetes by increasing blood sugar, insulin resistance, and inflammation.
Living a sedentary lifestyle, not eating an overall nutritious diet, smoking, and excessive alcohol intake can make diabetes worse.
Even if you have been prescribed medication for diabetes, it should be in addition to adjunct to diet and exercise. No matter where you are in your diabetes journey, making positive changes to your lifestyle can improve your symptoms.
Yang J, Qian F, Chavarro J E, et al. Modifiable risk factors and long term risk of type 2 diabetes among individuals with a history of gestational diabetes mellitus: prospective cohort study.
American Diabetes Association. Lifestyle change program: Join a CDC-recognized lifestyle change program. McMacken M, Shah S. A plant-based diet for the prevention and treatment of type 2 diabetes.
J Geriatr Cardiol. The lifestyle intervention commenced with a session core curriculum that was to be completed within the first 24 weeks after randomization. The session core curriculum was the most structured phase of the DPP lifestyle intervention and ensured that all participants were taught the same basic information about nutrition, physical activity, and behavioral self-management Table 2.
Similar to other state-of-the-art behavioral weight control programs, the first eight sessions presented the goals for the DPP lifestyle intervention, taught fundamental information about modifying energy intake and increasing energy output, and helped participants to self-monitor their intake and physical activity.
The latter eight sessions focused on the psychological, social, and motivational challenges involved in maintaining these healthy lifestyle behaviors in the long term.
Key behavioral and nutrition strategies that were introduced in the core curriculum included the following:. Participants were weighed privately at the start of every individual session and were encouraged to weigh themselves at home daily or a minimum of once per week.
If participants did not have a bathroom scale at home, they were given one. Emphasis was placed on using the scale as an important feedback and learning tool for how to better regulate personal diet and exercise behaviors.
The initial focus of the dietary intervention was on reducing total fat rather than calories. This allowed participants to accomplish a reduction in caloric intake while at the same time emphasizing overall healthy eating and streamlined the self-monitoring requirements, which was important given the diversity of educational and literacy levels among participants.
After several weeks, the concept of calorie balance and the need to restrict calories as well as fat was introduced. The fat and calorie goals were used as a means to achieve the weight loss goal rather than as a goal in and of itself.
Therefore, if a participant reported consuming more than the calorie or fat goal but was losing weight as planned, the coach did not emphasize greater calorie or fat reduction.
Participants were encouraged to gradually achieve the fat and calorie levels through better choices of meals and snack items, healthier food preparation techniques, and careful selection of restaurants, including fast food, and the items offered.
All participants were instructed to self-monitor fat and calorie intake daily throughout the first 24 weeks of the study and to record their minutes of physical activity. Self-monitoring was stressed as one of, if not the most, important strategy for changing diet and exercise behaviors. At the start of the core curriculum sessions, participants were given a food scale and measuring cups and spoons.
Self-monitoring skills were taught gradually over the first few weeks of the core curriculum. The lifestyle coach briefly reviewed the self-monitoring booklets with the participants during each session, reinforcing any noticeable positive behavior change and avoiding criticism.
The booklets were more thoroughly reviewed between sessions and written constructive comments were provided. The maintenance program used in the DPP was more intensive than that used in other clinical trials 6 , 7 and combined both group and individual contact.
After completing the session core curriculum, the protocol required that participants be seen face-to-face at least once every 2 months for the remainder of the trial and be contacted by phone at least once between visits.
Although these in-person contacts were usually one-on-one, they could occur in a group as long as there was an opportunity to weigh the participant and assist the individual with problem-solving regarding adherence.
Based on behavioral literature showing the importance of continued contact during maintenance 23 , coaches were encouraged to meet with participants as often as needed to support participant adherence and transition gradually from more frequent to less frequent contact if decreased frequency of contact did not adversely affect maintenance.
The majority of participants were seen more frequently than the minimum, with some participants continuing to attend weekly or biweekly sessions. The Lifestyle Resource Core developed a variety of lessons and participant handouts, and lifestyle coaches were encouraged to use materials related to the topics of greatest interest and concern to their individual participants.
htmlvdoc provides further guidelines for implementing the maintenance phase of the intervention. Participants were encouraged to continue self-monitoring their intake for 1 week every month during maintenance. If participants were succeeding at weight loss maintenance, self-monitoring was encouraged but not as strongly emphasized.
To simplify self-monitoring and encourage adherence to the calorie and fat goals, structured meal plans and meal-replacement products were provided as an option for participants. Each clinical center was also required to offer three group courses each lasting 4—8 weeks per year during the maintenance phase.
Participants were strongly encouraged but not required to attend these classes. Popular classes included resistance training, vegetarian cooking, and restart programs for those desiring to re-initiate intensive weight loss efforts. Three to four motivational campaigns were also developed per year to assist with maintenance of the weight and physical activity goals.
In several campaigns, local participant teams or DPP centers competed for the best attendance, self-monitoring, weight loss, minutes of physical activity, or steps as measured by pedometer Accusplit Digi-Walker. Participants received supplemental materials reflecting the content and theme of the campaigns such as self-monitoring postcards, magnets, weight graphs, newsletters, T-shirts, and other small incentives.
The protocol required that each clinical center offer supervised physical activity sessions at least two times per week throughout the trial. Attendance was voluntary. The types of supervised activity sessions varied across centers and included neighborhood group walks, enrolling participants in the cardiac rehabilitation programs affiliated with the DPP clinical center, community aerobic classes e.
All supervised activity sessions were led by a DPP staff member or someone trained by a DPP staff member as to the goals of the DPP lifestyle intervention. The session leaders documented attendance at all supervised activity sessions.
DPP participants encountered a variety of barriers to adherence over the course of the trial. Lifestyle coaches were encouraged to work with each participant individually to identify the specific barriers and possible solutions to these barriers.
The toolbox was arranged in a hierarchy from less expensive to more expensive approaches in terms of staff time as well as money and contained problem-solving strategies and reinforcements for use with individual participants. For example, participants having trouble achieving or maintaining the activity goal might be loaned or given an aerobic dance tape, enrolled in a community exercise class or a cardiac rehabilitation program, or seen individually by an exercise trainer to begin a tailored exercise regimen.
Similarly, participants might be given a cookbook, grocery store vouchers, or portion-controlled foods Slim-Fast or frozen entrees to help them achieve the weight-loss goals. Toolbox funds were also used to provide small reinforcers for fulfilling behavioral contracts, which usually involved achieving specific weight or physical activity goals over a 4- to 6-week period.
Consequently, it was important that the intervention be designed to address the needs of this ethnically diverse population. This was accomplished through the use of case managers, often chosen from the same ethnic group as the participant, who could tailor the intervention to meet the needs of local participants.
In addition, the core curriculum was available in Spanish and English and was designed to permit flexibility in the pace of presentation of new information, the amount of repetition of certain components of the program, and the complexity of self-monitoring forms that were used.
Reference materials e. During maintenance, centers selected topics for the group classes that were most appropriate for their participants, often specifically tailored to ethnic participants e.
Lastly, the toolbox approach allowed coaches to address the individual needs of an ethnically diverse population. In addition to local team support, a key feature of the DPP lifestyle intervention was an extensive centralized network of training, feedback, and support of the intervention staff.
The Lifestyle Resource Core in collaboration with the Lifestyle Advisory Group, a centrally organized committee that included several lifestyle coaches, program coordinators, and study investigators, coordinated these aspects of the intervention. All lifestyle coaches were required to attend annual, 2-day national training sessions conducted by the Lifestyle Resource Core.
In the latter 2 years of the intervention, additional training was offered for newly hired lifestyle coaches so that they could assume all lifestyle case management functions quickly and reliably.
There was no formal certification procedure for lifestyle coaches. In addition to attending the training sessions, coaches were instructed to be conversant with the DPP protocol and all lifestyle intervention manuals and to submit an audiotape of at least two individual participant sessions for review by the Lifestyle Resource Core.
New coaches who were unable to attend central training were required to view videotapes from the central trainings and directly observe or listen to audiotapes of at least two sessions with a centrally trained lifestyle coach.
The annual training sessions included didactic presentations on the key principles and strategies of the core and maintenance curricula, updates on lifestyle intervention research, review of lifestyle intervention data, and discussion of new participant materials, group classes, or motivational campaigns.
There was extensive use of case presentations, role-playing, and clinical practice skills, such as reflective listening, motivational interviewing, and empowerment strategies. Training sessions were videotaped and available for review at each site. Lifestyle coaches also received support and training at the local level through regular team meetings and case conferences with local consultants with expertise in behavioral science, nutrition, and exercise physiology.
Staff at most centers included a part-time behavioral consultant who could address chronic behavioral barriers to diet and exercise adherence and, on occasion, see individual participants for a brief period no more than two to four sessions of counseling.
In addition, local experts in nutrition and exercise were available to assist lifestyle coaches with individualization of the intervention for specific participants.
Lifestyle coaches also received support from regularly scheduled conference calls with the Lifestyle Resource Core and the Lifestyle Advisory Group.
During the first year of the DPP, individual lifestyle coaches were called monthly by a member of the Lifestyle Resource Core to review and discuss nonadherent participants. After the first year, the Lifestyle Resource Core conducted monthly regional conference calls with the lifestyle staff from four or five centers and was available for guidance and consultation whenever requested by local clinics.
Additionally, each clinic was assigned a representative from the Lifestyle Advisory Group who contacted the center monthly to provide additional discussion and problem solving of issues related to implementation of the protocol, new maintenance campaigns, and clinic performance.
This network of phone calls reinforced the participant learning objectives and lifestyle coaching skills taught at the annual trainings. The phone calls also provided an opportunity for coaches to identify a variety of obstacles to lifestyle change for their participants and to discuss behavioral approaches to improve specific problems.
Centers were required to hold team meetings at least once per month to review their progress. Five summary variables were examined: mean weight loss, mean percent weight loss, mean exercise minutes, percent of participants at weight goal, and percent of participants at exercise goal.
The Lifestyle Advisory Group also monitored these data, and clinics that were not performing well were given extra support from their specified representative. When appropriate, conference calls were held with the principal investigator and other staff at the local center or site visits were made to provide more extensive oversight.
The DPP lifestyle intervention was based on empirical literature in nutrition, exercise, and behavioral weight control, especially as it applied to the prevention of type 2 diabetes in diverse ethnic groups.
Extensive centralized feedback, training, and support were provided to all DPP centers. Accusplit, LifeScan, Health O Meter, Hoechst Marion Roussel, Merck-Medco Managed Care, Merck and Co.
McKesson BioServices, the Matthews Media Group, and the Henry M. Jackson Foundation provided support services under subcontract with the Coordinating Center. We thank the thousands of volunteers in this program for their devotion to the goal of diabetes prevention.
Address correspondence and reprint requests to The Diabetes Prevention Program Coordinating Center, Biostatistics Center, George Washington University, Executive Blvd. E-mail: dppmail biostat. For a complete list of the members of the DPP Research Group, please see reference 2.
A table elsewhere in this issue shows conventional and Système International SI units and conversion factors for many substances. Sign In or Create an Account.
Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care.
Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 25, Issue Previous Article Next Article.
Article Information. Article Navigation. The Diabetes Prevention Program DPP : Description of lifestyle intervention The Diabetes Prevention Program DPP Research Group The Diabetes Prevention Program DPP Research Group.
This Site. Google Scholar. Diabetes Care ;25 12 — Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest.
Table 1— Key aspects of the DPP lifestyle protocol. View Large. Table 2— DPP session core curriculum. Session 1.
Ffor developing type 2 diaabetes, most people Boost energy levels naturally prediabetes ; their blood sugar is higher than normal Natural remedies for bloating relief not Interventtions enough yet for a diabetes diagnosis. The good news is that prediabetes can be reversed. Ready to see where you stand? Take the 1-minute prediabetes risk test. If your score shows your risk is high, visit your doctor for a simple blood test to confirm your result. Find out if the lifestyle change program is right for you.
Ich weiß, dass man)) machen muss)
Diese einfach bemerkenswerte Mitteilung
Ich bin endlich, ich tue Abbitte, aber diese Antwort veranstaltet mich nicht. Kann, es gibt noch die Varianten?
Wacker, mir scheint es die glänzende Idee
Welcher Erfolg!