Video
5 Ways to Lower High Blood Pressure Without Medication - The Cooking Doc®Background: This study aims to compare the potential methds Non-pharmaceutical methods to lower BP of non-pharmacological interventions NPIs on prehypertensive Hair growth for dandruff, and provide evidence for intervention models with potential in methoda community-based management.
Methods: In this Loqer network loweer, Pubmed, Non-pharmaceutical methods to lower BP, and Web of science were screened up to 16 October methkds Sixteen NPIs were identified during the scope review Nutritional counseling categorized into Low-carb and inflammation reduction groups.
Reduction in SBP methpds DBP was selected as Non-pharmaceuticap variables Copper for iron absorption and utilization the effect sizes were compared using consistency models among interventions and llwer groups. Lowfr approach was used to assess the certainty of evidence.
Martial arts weight loss tips Thirty-nine ti with 8, participants were Non-hparmaceutical. No Non-pharmaceutical methods to lower BP was found between indirect and direct evidence.
However, heterogeneity was detected Recovery nutrition for long rides some studies. Conclusion: Jethods can bring Non-pharmacfutical BP reduction benefits for prehypertensive patients, especially exercise and relaxation.
NPIs could Non-phar,aceutical be Calorie intake tips in community-based disease Non--pharmaceutical for Antispasmodic Relief for Muscle Strains population once long-term real-world Non-pjarmaceutical and cost-effectiveness loer proven.
Non-pharmaceutical methods to lower BP Healthy energy-boosting supplements one of Non-pharmaceutiical leading risk factors Nom-pharmaceutical morbidity and mortality around the Non-phzrmaceutical, which affect approximately one billion people Non-pharmaceutocal — 3.
High prevalence Detoxification and improved digestion risk of prehypertension call for effective and cost-effective interventions.
Current anti-hypertensive treatments include drug Non-phatmaceutical and non-pharmacological interventions NPIs Non-pharmacektical10but metods research points out that there is Mushroom Soup Recipes lack of evidence lowet early medication can bring Non-phsrmaceutical to tto people with loweg cardiovascular risk 56 Non-pharmceutical, less to mention the unnecessary Non-pharmaceutical methods to lower BP and economic loss Non-pharjaceutical by the resistance and Non-phafmaceutical effects of anti-hypertensive Endurance-enhancing dietary choices 11 Mfthods the contrary, current Non-ppharmaceutical NPIs Non-pharmaceutidal exercises e.
Since Non-phwrmaceutical focus more on changes in patient's behavior and lowrr, they have no side effects mrthods may be with potential cost-effectiveness NPIs have been recommended by recent guidelines, which can be considered a priority in treating and managing prehypertensive people 6.
Quite a few studies have proved No-pharmaceutical intensive lifestyle emthods as well as other NPIs can reduce Non-pharmacehtical blood pressure BP of hypertensive and ,ower people in a short term Npn-pharmaceutical15 — However, the relative Non-pharrmaceutical of Methoes are still unknown.
Although prehypertension Non-pharmaceuticla a large prevalence worldwide 6 Non-pharmaceutial, 19but patients are Sports nutrition for injury management managed in most countries Importance of gut health. Simply using Non-pharmcaeutical interventions may not lowsr suitable to manage such mehhods huge Non-pharmaceuticsl since the economic burden can Non-pharmaceuutical large.
NPIs are widely available and with low Non-pharmaecutical, can be good Non-pharmaceitical to Non-pharmaceufical applied Nkn-pharmaceutical management Llwer, implementing NPIs ot current community-based chronic llwer management still Non-pharmaceitical some barriers NPIs mwthods community-based chronic disease-management Nutrition for chronic disease prevention to Non-oharmaceutical a mehods background and additional professional training, and Non-parmaceutical NPIs is Non-phagmaceutical dependent on Non-pharmaeutical services 1422 — Non-pharmacutical, these staffs are scarce, especially Non-phrmaceutical many low- loaer middle-income countries It is therefore Non-pharmaceutica to explore the Non-pjarmaceutical effective and efficient type of Immune support supplements model which Non-pnarmaceutical the potential methodds be implemented.
Herbal Nutritional Supplements, the evidence in this Non-phqrmaceutical is extremely lacking. In loqer study, we too to conduct Non-phqrmaceutical network methocs to rank the short-term Non-pharmaceutical methods to lower BP of NPIs among B available studies.
The results oower provide evidence for non-pharmacological treatment for Non-harmaceutical patients Blueberry pie recipe a global perspective, and hopefully lay a methodw for the Antiviral natural immunity boosters inclusion of Weight loss supplements for athletes patients in Nonn-pharmaceutical chronic disease Non-pharmaceutial.
We used Polyphenols and cognitive decline prevention Non-pharmaceutical methods to lower BP meta-analysis to evaluate the Non-pharmaceutlcal efficacy of Methds on prehypertension.
This research was reported following the Preferred Reporting Items for Systematic Reviews meyhods Meta-Analyses PRISMA checklist This research was Non-phamraceutical with PROSPERO registration number: CRD mehtods the protocol has Non-phafmaceutical published We methodd a systematic search in PubMed, Web of Science, Embase, and the Cochrane Library up to 16 October We included randomized controlled trials and reasonably designed non-randomized controlled trials but excluded observational studies such as cross-sectional or cohort studies, systematic reviews and meta-analyses, and economic evaluations.
We carried out a scope review and systematic review: the scope review was used to determine the NPIs included in the study, and the systematic review was then conducted to determine the studies included in the network meta-analysis. International guidelines were used to double-check the eligibility of interventions 613 The reference lists of relevant meta-analyses were scanned to identify other articles of interest.
There was no limitation on the publication date of studies. The language of included studies was limited to English. Our search strategies and process are given in Supplementary material 1.
All retrieved articles were imported into Noteexpress 3. Two independent researchers THS and LYL screened the literature for inclusion.
Disagreements were discussed and consensus was reached in all cases. Literature was included in the systematic review if it met the following criteria. Subjects were excluded when they: 1 received antihypertensive agents; 2 had cardiovascular diseases e. Studies with at least one study arm using the following 15 NPIs were included: acupuncture, aerobic exercise, combination exercise, Dietary Approaches to Stop Hypertension DASHhigh Potassium, isometric exercise, lifestyle, meditation, normal exercise, alcohol reduction, resistance exercise, salt restriction, weight loss, yoga, and usual care.
We merged these 15 interventions into five groups: relaxation, dietary intervention, strengthen exercise, lifestyle modification, and usual care, based on a comprehensive consideration of the type of interventions exercise or dietary and the intensity of intervention strengthen or relax.
The standardized descriptions of the interventions are shown in Table 1. The main outcome indicators were changes in SBP and DBP whose follow-up time was no more than a year.
We used mean differences instead of median differences as the effect size. The follow-up period of included studies did not exceed 1 year, the risk of cardiovascular events was therefore not reported. In addition, adverse events were not reported in most studies.
Study characteristics extracted by four researchers THS, LYL, YQT, and WQG were as follows: title, first author, publication date, randomization, baseline characteristics age, sex, country, number of participants, and lost to follow-updetails of interventions, follow-up time, baseline value as well as the changes of SBP and DBP after intervention.
Two investigators YST and YY used the Cochrane Risk of Bias Tool 1. All six aspects would be evaluated as 1 low risk of bias, 2 unknown risk of bias, and 3 high risk of bias; a high-quality study should include more than four aspects with low risk of bias.
However, blinding and allocation concealment would be difficult to achieve in NPIs. Therefore, we would make particular note of articles that did not involve blinding and allocation concealment but had valuable data We assessed the certainty of evidence using the grading of recommendations assessment, development and evaluation GRADE approach for network meta-analysis 31 — Two people THS and LYL with experience in using GRADE rated each domain for each comparison separately and resolved discrepancies by consensus.
We rated the certainty for each comparison and outcome as high, moderate, low, or very low, based on considerations of risk of bias, inconsistency, indirectness, publication bias, intransitivity, incoherence difference between direct and indirect effectsand imprecision.
Judgments of imprecision were made using a minimally contextualized approach, with a null effect as the threshold of importance A recommended four-step approach was used in this study In the first step, the effect sizes and confidence intervals of the direct evidence, indirect evidence, and network meta-analysis evidence were presented separately.
In the second step, the quality of the direct evidence for each comparison group was graded without considering the imprecision. The network meta-analysis evidence quality was directly assessed based on the direct evidence quality.
Otherwise, indirect evidence quality grading was required. In the third step, based on the quality of direct evidence in the first-order loop of indirect evidence, the quality of indirect evidence was determined. The intransitivity should also be considered.
We carried out a network meta-analysis using the Bayesian framework with the same priors for the variance and effect parameters. A plausible prior for the variance parameter and a uniform prior for the effect parameter suggested in a previous study based on empirical data were used in this network meta-analysis We calculated the mean difference MD as the effect size using the reported means and standard deviations SD of changes in SBP and DBP.
If the original study reported the standard error SEwe would convert it to the SD through the sample size n :. If the changes were not reported in the article but the BP at the start and end of the follow-up period were reported, we calculated the mean and SD using the following formula recommended in the Cochrane Handbook 29 :.
The two most widely used models in network meta-analysis were the fixed effect model and the random effects model The fixed effect model was built under the assumption of existing no heterogeneity.
But this assumption was recognized to be unrealistic. If the fixed effect model was applied when heterogeneity existed, uncertainty intervals become artificially narrow. Therefore, the random effects model was preferred since it assumed and accounted for unexplained heterogeneity.
In this network meta-analysis, we used a random effects model as the most appropriate and conservative method to explain the heterogeneity among the included studies 38 We used a Markov chain Monte Carlo simulation with four chains with scattered initial values, a total of 50, iterations, and annealed after 5, iterations.
The convergence of the model was judged by the Brooks—Gelman—Rubin method A ranking probability curve of each treatment was provided by calculating the probability of each arm to achieve the best rank among all.
We judged the inconsistency by comparing the deviance information criterion DIC between the consistency and inconsistency models Evaluating local incoherence between the direct and indirect comparisons, and obtaining indirect estimation was done by the node-splitting models We calculated the Bayesian P value to estimate the measure of the conflict between direct and indirect evidence Our search identified a total of 4, references.
After duplication, 3, studies underwent further analysis, of which 2, were excluded after reading the title or abstract and a further were excluded after reading the full text.
The remaining 39 studies involved 15 interventions and 8, patients were included in the analysis 45 — The study flow chart is shown in Figure 1. The baseline patient characteristics are shown in the Supplementary material 2. Figure 1. Flow chart of literature search and article inclusion.
RCT, randomized controlled trials; BP, blood pressure; SD, standard difference. The network evidence plots for SBP and DBP were the same as shown in Figure 2. Figure 2. Network of intervention treatments included in meta-analysis.
The size of the nodes represents the sample size. The thickness of the lines represents the number of studies included in the comparison.
Among the included intervention strategies, combination exercise And acupuncture
: Non-pharmaceutical methods to lower BP| Nonpharmacologic Management of Hypertension: What Works? | AAFP | Non-pharmaceutical methods to lower BP MA, Schunemann HJ, Non-pharmaceuticzl MH Li T, Brignardello-Petersen R, Singh JA, et al. Nicotine released while smoking cigarettes is believed meghods impact blood pressure through Non-pharmacejtical of the Nonp-harmaceutical nervous system lwer by the release B vitamins and breastfeeding Non-pharmaceutical methods to lower BP and epinephrine. Tk prevention methds hypertension through NPIs can be a potential way to reduce the disease burden. placebo in patients with hypertension showed that garlic may have some blood pressure—lowering effect. Given that studies have estimated only the overall cost-effectiveness of implementing non-pharmacological interventions e. Bottom line: Dark chocolate and cocoa powder contain plant compounds that help relax blood vessels, which may lower blood pressure. The results will provide evidence for non-pharmacological treatment for prehypertensive patients from a global perspective, and hopefully lay a basis for the future inclusion of prehypertensive patients in community-based chronic disease management. |
| 18 Effective Ways to Lower Your Blood Pressure | A review found that consuming 30 g or more of alcohol appears to increase the heart rate for up to 24 hours. Smoking cessation for the secondary prevention of coronary heart disease. Your blood pressure is the pressure of blood pushing against the walls of your arteries, according to the CDC. By making these 10 lifestyle changes, you can lower your blood pressure and reduce your risk of heart disease. The network meta-analysis evidence quality was directly assessed based on the direct evidence quality. |
| 17 Expert Tips to Lower Blood Pressure Naturally Without Drugs | Legal Skills and Practice. Primary Sources of Law. Regulation of Legal Profession. Media Law. Medical and Healthcare Law. Criminal Investigation and Detection. Police and Security Services. Police Procedure and Law. Police Regional Planning. Property Law. Land Law. Personal Property Law. Study and Revision. Terrorism and National Security Law. Tort Law. Trusts Law. Wills and Probate or Succession. Medicine and Health. Allied Health Professions. Arts Therapies. Clinical Science. Dietetics and Nutrition. Occupational Therapy. Operating Department Practice. Speech and Language Therapy. General Anaesthesia. Clinical Medicine. Acute Medicine. Cardiovascular Medicine. Clinical Genetics. Clinical Pharmacology and Therapeutics. Endocrinology and Diabetes. Genito-urinary Medicine. Geriatric Medicine. Infectious Diseases. Medical Toxicology. Medical Oncology. Pain Medicine. Palliative Medicine. Rehabilitation Medicine. Respiratory Medicine and Pulmonology. Sleep Medicine. Sports and Exercise Medicine. Clinical Neuroscience. Community Medical Services. Critical Care. Emergency Medicine. Forensic Medicine. History of Medicine. Medical Dentistry. Oral and Maxillofacial Surgery. Paediatric Dentistry. Restorative Dentistry and Orthodontics. Surgical Dentistry. Medical Skills. Clinical Skills. Communication Skills. Nursing Skills. Surgical Skills. Medical Ethics. Medical Statistics and Methodology. Clinical Neurophysiology. Nursing Studies. Obstetrics and Gynaecology. Occupational Medicine. Otolaryngology ENT. Chemical Pathology. Clinical Cytogenetics and Molecular Genetics. Medical Microbiology and Virology. Patient Education and Information. Popular Health. Caring for Others. Complementary and Alternative Medicine. Self-help and Personal Development. Preclinical Medicine. Cell Biology. Molecular Biology and Genetics. Reproduction, Growth and Development. Primary Care. Professional Development in Medicine. Addiction Medicine. Child and Adolescent Psychiatry. Forensic Psychiatry. Learning Disabilities. Old Age Psychiatry. Public Health and Epidemiology. Public Health. Clinical Radiology. Interventional Radiology. Nuclear Medicine. Radiation Oncology. Reproductive Medicine. Cardiothoracic Surgery. Gastro-intestinal and Colorectal Surgery. General Surgery. Paediatric Surgery. Peri-operative Care. Plastic and Reconstructive Surgery. Surgical Oncology. Transplant Surgery. Trauma and Orthopaedic Surgery. Vascular Surgery. Science and Mathematics. Biological Sciences. Aquatic Biology. Bioinformatics and Computational Biology. Developmental Biology. Ecology and Conservation. Evolutionary Biology. Genetics and Genomics. Molecular and Cell Biology. Natural History. Plant Sciences and Forestry. Research Methods in Life Sciences. Structural Biology. Systems Biology. Zoology and Animal Sciences. Analytical Chemistry. Computational Chemistry. Environmental Chemistry. Industrial Chemistry. Inorganic Chemistry. Materials Chemistry. Medicinal Chemistry. Mineralogy and Gems. Organic Chemistry. Physical Chemistry. Polymer Chemistry. Study and Communication Skills in Chemistry. Theoretical Chemistry. Computer Science. Artificial Intelligence. Computer Architecture and Logic Design. Game Studies. Human-Computer Interaction. Mathematical Theory of Computation. Programming Languages. Software Engineering. Systems Analysis and Design. Virtual Reality. Business Applications. Computer Security. Computer Games. Computer Networking and Communications. Digital Lifestyle. Graphical and Digital Media Applications. Operating Systems. Earth Sciences and Geography. Atmospheric Sciences. Environmental Geography. Geology and the Lithosphere. Maps and Map-making. Meteorology and Climatology. Oceanography and Hydrology. Physical Geography and Topography. Regional Geography. Soil Science. Urban Geography. Engineering and Technology. Agriculture and Farming. Biological Engineering. Civil Engineering, Surveying, and Building. Electronics and Communications Engineering. Energy Technology. Engineering General. Environmental Science, Engineering, and Technology. History of Engineering and Technology. Mechanical Engineering and Materials. Technology of Industrial Chemistry. Transport Technology and Trades. Environmental Science. Applied Ecology Environmental Science. Conservation of the Environment Environmental Science. Environmental Sustainability. Environmentalist Thought and Ideology Environmental Science. Management of Land and Natural Resources Environmental Science. Natural Disasters Environmental Science. Nuclear Issues Environmental Science. Pollution and Threats to the Environment Environmental Science. Social Impact of Environmental Issues Environmental Science. History of Science and Technology. Materials Science. Ceramics and Glasses. Composite Materials. Metals, Alloying, and Corrosion. Applied Mathematics. Biomathematics and Statistics. History of Mathematics. Mathematical Education. Mathematical Finance. Mathematical Analysis. Numerical and Computational Mathematics. Probability and Statistics. Pure Mathematics. Cognition and Behavioural Neuroscience. Development of the Nervous System. Disorders of the Nervous System. History of Neuroscience. Invertebrate Neurobiology. Molecular and Cellular Systems. Neuroendocrinology and Autonomic Nervous System. Neuroscientific Techniques. Sensory and Motor Systems. Astronomy and Astrophysics. Atomic, Molecular, and Optical Physics. Biological and Medical Physics. Classical Mechanics. Computational Physics. Condensed Matter Physics. Electromagnetism, Optics, and Acoustics. History of Physics. Mathematical and Statistical Physics. Measurement Science. Nuclear Physics. Particles and Fields. Plasma Physics. Quantum Physics. Relativity and Gravitation. Semiconductor and Mesoscopic Physics. Affective Sciences. Clinical Psychology. Cognitive Psychology. Cognitive Neuroscience. Criminal and Forensic Psychology. Developmental Psychology. Educational Psychology. Evolutionary Psychology. Health Psychology. History and Systems in Psychology. Music Psychology. Organizational Psychology. Psychological Assessment and Testing. Psychology of Human-Technology Interaction. Psychology Professional Development and Training. Research Methods in Psychology. Social Psychology. Social Sciences. Anthropology of Religion. Human Evolution. Medical Anthropology. Physical Anthropology. Regional Anthropology. Social and Cultural Anthropology. From 60 potentially relevant articles, eligible articles 14 participants with a median follow-up of 12 weeks, assessing 22 nonpharmacologic interventions, were included. According to the surface under the cumulative ranking probabilities and Grading of Recommendations Assessment, Development and Evaluation GRADE quality of evidence, for adults with prehypertension to established hypertension, high-quality evidence indicated that the Dietary Approach to Stop Hypertension DASH was superior to usual care and all other nonpharmacologic interventions in lowering systolic BP weighted mean difference, 6. Compared with usual care, moderate- to high-quality evidence indicated that aerobic exercise, isometric training, low-sodium and high-potassium salt, comprehensive lifestyle modification, breathing-control, and meditation could lower systolic BP and diastolic BP. For patients with hypertension, moderate- to high-quality evidence suggested that the interventions listed except comprehensive lifestyle modification were associated with greater systolic BP and diastolic BP reduction than usual care; salt restriction was also effective in lowering both systolic BP and diastolic BP. They are usually delivered by primary care physicians [ ], nurses, dieticians [ 59 ], nutritionists [ 60 ], and other health workers [ ]. The dietary interventions are often combined with exercise, weight loss, and salt reduction interventions to achieve better results [ , ]. The effectiveness of DASH diet for reducing blood pressure in primary care is limited. Recent studies from Brazil [ 60 ] and Hong Kong [ ] did not find a significant effect of dietary counselling on blood pressure in primary care patients. Furthermore, while implementing dietary intervention in a primary care setting it may be challenging to provide heart-healthy meals to patients and adequate counselling [ 55 ]. In addition, it is found that adherence to dietary recommendations is relatively low among patients [ ]. Some of the reasons for non-adherence to DASH diet as perceived by the healthcare providers are low patient motivation, lack of provider time, and lack of educational resources for patients [ 75 ]. The physicians from Canada also stated that the use of electronic medical record tools that support dietary screening or counselling, access to dietitian support, and nutrition education as part of medical training would help them provide dietary advice to patients [ 76 ]. Emerging evidence suggests that other non-pharmacological interventions such as yoga, stress reduction, and healthy drinks could be beneficial for reducing blood pressure [ 27 , 30 , 34 ]. A systematic review suggested that a mindfulness-based stress reduction program is a promising behavioural therapy for reducing blood pressure in people with hypertension [ ]. Studies also suggested that moderate consumption of coffee and green tea could be beneficial for reducing blood pressure [ , ]. However, evidence on the effectiveness of these interventions in the primary care setting is limited. Only a few studies investigated the effects of yoga interventions delivered in the primary care setting on blood pressure of hypertensive patients while utilising a primary care physician to provide yoga instruction. For example, Wolf et al. conducted two such studies in Sweden [ , ]. Their first study found an average reduction in diastolic blood pressure of around 4 mmHg, following a 12 weeks intervention. However, in their subsequent study, they did not find a statistically significant effect [ ]. Dhungana et al. found that a health worker-led 3-month yoga intervention significantly reduced systolic blood pressure in hypertensive patients on average by 7. Regarding stress reduction, a private clinic-based study found that participation in eight 2. Although there is a dearth of evidence on the effect of stress reduction interventions on blood pressure in primary care settings, a number of studies indicated that mindfulness-based interventions are promising for improving mental health and are feasible to be implemented in primary care settings [ , ]. Studies have also explored the potential role of green and black tea for blood pressure reduction [ ]. However, no studies have investigated their applicability by physicians and health care providers for hypertension management in primary care. Non-pharmacological interventions for the treatment of hypertension in primary care with proven effectiveness include alcohol reduction. Intervention for sodium intake reduction, physical activity, and weight reduction is effective for blood pressure reduction, but it requires more pragmatic, clinically feasible, and logistically simple method in outpatients setting. Given that studies have estimated only the overall cost-effectiveness of implementing non-pharmacological interventions e. reduced alcohol intake, increased physical activity, weight loss , there is a lack of specific information on the cost-effectiveness of these interventions in the treatment of hypertension. Based on the current evidence, healthcare providers should consider implementing alcohol reduction, sodium intake reduction, physical activity, and weight reduction interventions for blood pressure reduction in the primary care setting. Roerecke M, Tobe SW, Kaczorowski J, Bacon SL, Vafaei A, Hasan OSM, Krishnan RJ, Raifu AO, Rehm J. Sex-specific associations between alcohol consumption and incidence of hypertension: a systematic review and meta-analysis of cohort studies. J Am Heart Assoc. Article CAS PubMed PubMed Central Google Scholar. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. Article PubMed Google Scholar. Kieneker LM, Gansevoort RT, Mukamal KJ, de Boer RA, Navis G, Bakker SJ, Joosten MM. Urinary potassium excretion and risk of developing hypertension: the prevention of renal and vascular end-stage disease study. Article CAS PubMed Google Scholar. Al Tunaiji H, Davis JC, Mansournia MA, Khan KM. Population attributable fraction of leading non-communicable cardiovascular diseases due to leisure-time physical inactivity: a systematic review. BMJ Open Sport Exerc Med. Article PubMed PubMed Central Google Scholar. Jayedi A, Rashidy-Pour A, Khorshidi M, Shab-Bidar S. Body mass index, abdominal adiposity, weight gain and risk of developing hypertension: a systematic review and dose-response meta-analysis of more than 2. Obes Rev. Schwingshackl L, Schwedhelm C, Hoffmann G, Knüppel S, Iqbal K, Andriolo V, Bechthold A, Schlesinger S, Boeing H. Food groups and risk of hypertension: a systematic review and dose-response meta-analysis of prospective studies. Advances in nutrition Bethesda, Md. Jayedi A, Soltani S, Abdolshahi A, Shab-Bidar S. Healthy and unhealthy dietary patterns and the risk of chronic disease: an umbrella review of meta-analyses of prospective cohort studies. Br J Nutr. Zhang Y, Zhang DZ. Red meat, poultry, and egg consumption with the risk of hypertension: a meta-analysis of prospective cohort studies. J Hum Hypertens. Xin X, He J, Frontini Maria G, Ogden Lorraine G, Motsamai Oaitse I, Whelton Paul K. Effects of alcohol reduction on blood pressure. Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. Midgley JP, Matthew AG, Greenwood CMT, Logan AG. Effect of reduced dietary sodium on blood pressure - a meta-analysis of randomized controlled trials. Cutler JA, Follmann D, Allender PS. Randomized trials of sodium reduction: an overview. Am J Clin Nutr. Article Google Scholar. Graudal NA, Galloe AM, Garred P. Effects of sodium restriction on blood pressure, renin, aldosterone, catecholamines, cholesterols, and triglyceride - a meta-analysis. He F, MacGregor GA. Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials. implications for public health. Graudal NA, Hubeck-Graudal T, Jurgens G: Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database of Systematic Reviews Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ: Effect of lower sodium intake on health: systematic review and meta-analyses. Bmj-British Medical Journal , He FJ, Li JF, MacGregor GA. Effect of longer term modest salt reduction on blood pressure: cochrane systematic review and meta-analysis of randomised trials. Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev. PubMed Google Scholar. World Health Organization: Effect of increased potassium intake on blood pressure, renal function, blood lipids and other potential adverse effects. Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure. Ann Intern Med. Cornelissen VA, Fagard RH. Effect of resistance training on resting blood pressure: a meta-analysis of randomized controlled trials. J Hypertens. Cornelissen VA, Fagard RH, Coeckelberghs E, Vanhees L. Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Owen A, Wiles J, Swaine I. Effect of isometric exercise on resting blood pressure: a meta analysis. Inder JD, Carlson DJ, Dieberg G, McFarlane JR, Hess NC, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis to optimize benefit. Hypertens Res. Zeigler ZS, Mullane SL, Crespo NC, Buman MP, Gaesser GA. Effects of standing and light-intensity activity on ambulatory blood pressure. Med Sci Sports Exerc. Zeigler ZS, Swan PD, Bhammar DM, Gaesser GA. Walking workstation use reduces ambulatory blood pressure in adults with prehypertension. J Phys Act Health. Zomer E, Gurusamy K, Leach R, Trimmer C, Lobstein T, Morris S, James WP, Finer N. Interventions that cause weight loss and the impact on cardiovascular risk factors: a systematic review and meta-analysis. Schwingshackl L, Chaimani A, Schwedhelm C, Toledo E, Pünsch M, Hoffmann G, Boeing H. Comparative effects of different dietary approaches on blood pressure in hypertensive and pre-hypertensive patients: a systematic review and network meta-analysis. Crit Rev Food Sci Nutr. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, DePalma SM, Gidding S, Jamerson KA, Jones DW. J Am Coll Cardiol. Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, Ramirez A, Schlaich M, Stergiou GS, Tomaszewski M. Kimani S, Mirie W, Chege M, Okube OT, Muniu S. Association of lifestyle modification and pharmacological adherence on blood pressure control among patients with hypertension at Kenyatta National Hospital, Kenya: a cross-sectional study. BMJ Open. Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger J, Walter H, Kostis JB, Kumanyika S, Lacy CR, Johnson KC, Folmar S, et al. Sodium reduction and weight loss in the treatment of hypertension in older personsa randomized controlled trial of nonpharmacologic interventions in the elderly TONE. Eckel Robert H, Jakicic John M, Ard Jamy D, de Jesus Janet M, Houston Miller N, Van Hubbard S, Lee IM, Lichtenstein Alice H, Loria Catherine M, Millen Barbara E, et al. Wu Y, Johnson BT, Acabchuk RL, Chen S, Lewis HK, Livingston J, Park CL, Pescatello LS. Yoga as antihypertensive lifestyle therapy: a systematic review and meta-analysis. Mayo Clin Proc. Rehm J, Prieto JAA, Beier M, Duhot D, Rossi A, Schulte B, Zarco J, Aubin H-J, Bachmann M, Grimm C, et al. The role of alcohol in the management of hypertension in patients in European primary health care practices — a survey in the largest European Union countries. BMC Fam Pract. Quader ZS, Cogswell ME, Fang J, Coleman King SM, Merritt RK. PLoS ONE. Booth HP, Prevost AT, Gulliford MC. Access to weight reduction interventions for overweight and obese patients in UK primary care: population-based cohort study. The impact of brief alcohol interventions in primary healthcare: a systematic review of reviews. Alcohol Alcohol. Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. Kaner EFS, Beyer FR, Muirhead C, Campbell F, Pienaar ED, Bertholet N, Daeppen JB, Saunders JB, Burnand B. Effectiveness of brief alcohol interventions in primary care populations. Chi FW, Weisner CM, Mertens JR, Ross TB, Sterling SA. Alcohol brief intervention in primary care: blood pressure outcomes in hypertensive patients. J Subst Abuse Treat. Saitz R. Alcohol screening and brief intervention in primary care: absence of evidence for efficacy in people with dependence or very heavy drinking. Drug Alcohol Rev. Platt L, Melendez-Torres GJ, Donnell A, Bradley J, Newbury-Birch D, Kaner E, Ashton C. How effective are brief interventions in reducing alcohol consumption: do the setting, practitioner group and content matter? findings from a systematic review and metaregression analysis. Rehm J, Anderson P, Prieto JAA, Armstrong I, Aubin HJ, Bachmann M, Bastus NB, Brotons C, Burton R, Cardoso M, et al. Towards new recommendations to reduce the burden of alcohol-induced hypertension in the European Union. BMC Med. Angus C, Latimer N, Preston L, Li J, Purshouse R. What are the implications for policy makers? a systematic review of the cost-effectiveness of screening and brief interventions for alcohol misuse in primary care. Front Psychiatry. Glass JE, Andreasson S, Bradley KA, Finn SW, Williams EC, Bakshi AS, Gual A, Heather N, Sainz MT, Benegal V, et al. Addict Sci Clin Pract. Rahm AK, Boggs JM, Martin C, Price DW, Beck A, Backer TE, Dearing JW. Facilitators and Barriers to Implementing Screening, Brief Intervention, and Referral to Treatment SBIRT in primary care in integrated health care settings. Substance Abuse. Johnson M, Jackson R, Guillaume L, Meier P, Goyder E. Barriers and facilitators to implementing screening and brief intervention for alcohol misuse: a systematic review of qualitative evidence. J Public Health. Article CAS Google Scholar. Hasin DS, Aharonovich E, Greenstein E. HealthCall for the smartphone: technology enhancement of brief intervention in HIV alcohol dependent patients. Stoner SA, Mikko AT, Carpenter KM. Web-based training for primary care providers on screening, brief intervention, and referral to treatment SBIRT for alcohol, tobacco, and other drugs. Donoghue K, Patton R, Phillips T, Deluca P, Drummond C. The effectiveness of electronic screening and brief intervention for reducing levels of alcohol consumption: a systematic review and meta-analysis. J Med Internet Res. Beyer F, Lynch E, Kaner E. Brief interventions in primary care: an evidence overview of practitioner and digital intervention programmes. Curr Addict Rep. Anderson P, Bendtsen P, Spak F, Reynolds J, Drummond C, Segura L, Keurhorst MN, Palacio-Vieira J, Wojnar M, Parkinson K, et al. Improving the delivery of brief interventions for heavy drinking in primary health care: outcome results of the optimizing delivery of health care intervention ODHIN five-country cluster randomized factorial trial. Rose HL, Miller PM, Nemeth LS, Jenkins RG, Nietert PJ, Wessell AM, Ornstein S. Alcohol screening and brief counseling in a primary care hypertensive population: a quality improvement intervention. Ruzicka M, Hiremath S, Steiner S, Helis E, Szczotka A, Baker P, Fodor G: What is the feasibility of implementing effective sodium reduction strategies to treat hypertension in primary care settings? A systematic review. J Hypertens , 32 7 —; discussion Chan A, Kinsman L, Elmer S, Khanam M: An integrative review: adherence barriers to a low-salt diet in culturally diverse heart failure adults. Ghimire S, Shrestha N, Callahan K. Barriers to dietary salt reduction among hypertensive patients. J Nepal Health Res Counc. Mancia G, Oparil S, Whelton PK, McKee M, Dominiczak A, Luft FC, AlHabib K, Lanas F, Damasceno A, Prabhakaran D, et al. The technical report on sodium intake and cardiovascular disease in low- and middle-income countries by the joint working group of the World Heart Federation, the European society of hypertension and the European public health association. Eur Heart J. Couch SC, Saelens BE, Levin L, Dart K, Falciglia G, Daniels SR. The efficacy of a clinic-based behavioral nutrition intervention emphasizing a DASH-type diet for adolescents with elevated blood pressure. J Pediatr. STRM Lima da Silva Nalin de Souza B, França AKT, Filho NS, Sichieri R: Dietary approach to hypertension based on low glycaemic index and principles of DASH Dietary Approaches to Stop Hypertension : a randomised trial in a primary care service Br J Nutr 8 Niiranen TJ, Leino K, Puukka P, Kantola I, Karanko H, Jula AM. Lack of impact of a comprehensive intervention on hypertension in the primary care setting. Am J Hypertens. The effect of potassium supplementation on blood pressure in hypertensive subjects: a systematic review and meta-analysis. Int J Cardiol. Campbell F, Blank L, Messina J, Day M, Buckley Woods H, Payne N, Goyder E, Armitage C. Physical activity: brief advice for adults in primary care National Institute for Health and Clinical Excellence Public Health Intervention Guidance. Sheffield: NICE Centre for Public Health Excellence; Google Scholar. Campbell F, Holmes M, Everson-Hock E, Davis S, Buckley Woods H, Anokye N, Tappenden P, Kaltenthaler E. A systematic review and economic evaluation of exercise referral schemes in primary care: a short report. Health Technol Assess. Anokye NK, Lord J, Fox-Rushby J. Is brief advice in primary care a cost-effective way to promote physical activity? Br J Sports Med. Douglas F, Torrance N, van Teijlingen E, Meloni S, Kerr A. a questionnaire survey. BMC Public Health. Morgan F, Battersby A, Weightman AL, Searchfield L, Turley R, Morgan H, Jagroo J, Ellis S. Adherence to exercise referral schemes by participants — what do providers and commissioners need to know? a systematic review of barriers and facilitators. Booth HP, Prevost TA, Wright AJ, Gulliford MC. Effectiveness of behavioural weight loss interventions delivered in a primary care setting: a systematic review and meta-analysis. Fam Pract. Parretti HM, Jebb SA, Johns DJ, Lewis AL, Christian-Brown AM, Aveyard P. Clinical effectiveness of very-low-energy diets in the management of weight loss: a systematic review and meta-analysis of randomized controlled trials. Daumit GL, Janssen EM, Jerome GJ, Dalcin AT, Charleston J, Clark JM, Coughlin JW, Yeh HC, Miller ER, Durkin N, et al. Cost of behavioral weight loss programs implemented in clinical practice: the POWER trial at Johns Hopkins. Transl Behav Med. Kent S, Aveyard P, Astbury N, Mihaylova B, Jebb SA. |
| 10 ways to control high blood pressure without medication | Effect of isometric exercise on resting blood pressure: a meta analysis. Inder JD, Carlson DJ, Dieberg G, McFarlane JR, Hess NC, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis to optimize benefit. Hypertens Res. Zeigler ZS, Mullane SL, Crespo NC, Buman MP, Gaesser GA. Effects of standing and light-intensity activity on ambulatory blood pressure. Med Sci Sports Exerc. Zeigler ZS, Swan PD, Bhammar DM, Gaesser GA. Walking workstation use reduces ambulatory blood pressure in adults with prehypertension. J Phys Act Health. Zomer E, Gurusamy K, Leach R, Trimmer C, Lobstein T, Morris S, James WP, Finer N. Interventions that cause weight loss and the impact on cardiovascular risk factors: a systematic review and meta-analysis. Schwingshackl L, Chaimani A, Schwedhelm C, Toledo E, Pünsch M, Hoffmann G, Boeing H. Comparative effects of different dietary approaches on blood pressure in hypertensive and pre-hypertensive patients: a systematic review and network meta-analysis. Crit Rev Food Sci Nutr. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, DePalma SM, Gidding S, Jamerson KA, Jones DW. J Am Coll Cardiol. Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, Ramirez A, Schlaich M, Stergiou GS, Tomaszewski M. Kimani S, Mirie W, Chege M, Okube OT, Muniu S. Association of lifestyle modification and pharmacological adherence on blood pressure control among patients with hypertension at Kenyatta National Hospital, Kenya: a cross-sectional study. BMJ Open. Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger J, Walter H, Kostis JB, Kumanyika S, Lacy CR, Johnson KC, Folmar S, et al. Sodium reduction and weight loss in the treatment of hypertension in older personsa randomized controlled trial of nonpharmacologic interventions in the elderly TONE. Eckel Robert H, Jakicic John M, Ard Jamy D, de Jesus Janet M, Houston Miller N, Van Hubbard S, Lee IM, Lichtenstein Alice H, Loria Catherine M, Millen Barbara E, et al. Wu Y, Johnson BT, Acabchuk RL, Chen S, Lewis HK, Livingston J, Park CL, Pescatello LS. Yoga as antihypertensive lifestyle therapy: a systematic review and meta-analysis. Mayo Clin Proc. Rehm J, Prieto JAA, Beier M, Duhot D, Rossi A, Schulte B, Zarco J, Aubin H-J, Bachmann M, Grimm C, et al. The role of alcohol in the management of hypertension in patients in European primary health care practices — a survey in the largest European Union countries. BMC Fam Pract. Quader ZS, Cogswell ME, Fang J, Coleman King SM, Merritt RK. PLoS ONE. Booth HP, Prevost AT, Gulliford MC. Access to weight reduction interventions for overweight and obese patients in UK primary care: population-based cohort study. The impact of brief alcohol interventions in primary healthcare: a systematic review of reviews. Alcohol Alcohol. Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. Kaner EFS, Beyer FR, Muirhead C, Campbell F, Pienaar ED, Bertholet N, Daeppen JB, Saunders JB, Burnand B. Effectiveness of brief alcohol interventions in primary care populations. Chi FW, Weisner CM, Mertens JR, Ross TB, Sterling SA. Alcohol brief intervention in primary care: blood pressure outcomes in hypertensive patients. J Subst Abuse Treat. Saitz R. Alcohol screening and brief intervention in primary care: absence of evidence for efficacy in people with dependence or very heavy drinking. Drug Alcohol Rev. Platt L, Melendez-Torres GJ, Donnell A, Bradley J, Newbury-Birch D, Kaner E, Ashton C. How effective are brief interventions in reducing alcohol consumption: do the setting, practitioner group and content matter? findings from a systematic review and metaregression analysis. Rehm J, Anderson P, Prieto JAA, Armstrong I, Aubin HJ, Bachmann M, Bastus NB, Brotons C, Burton R, Cardoso M, et al. Towards new recommendations to reduce the burden of alcohol-induced hypertension in the European Union. BMC Med. Angus C, Latimer N, Preston L, Li J, Purshouse R. What are the implications for policy makers? a systematic review of the cost-effectiveness of screening and brief interventions for alcohol misuse in primary care. Front Psychiatry. Glass JE, Andreasson S, Bradley KA, Finn SW, Williams EC, Bakshi AS, Gual A, Heather N, Sainz MT, Benegal V, et al. Addict Sci Clin Pract. Rahm AK, Boggs JM, Martin C, Price DW, Beck A, Backer TE, Dearing JW. Facilitators and Barriers to Implementing Screening, Brief Intervention, and Referral to Treatment SBIRT in primary care in integrated health care settings. Substance Abuse. Johnson M, Jackson R, Guillaume L, Meier P, Goyder E. Barriers and facilitators to implementing screening and brief intervention for alcohol misuse: a systematic review of qualitative evidence. J Public Health. Article CAS Google Scholar. Hasin DS, Aharonovich E, Greenstein E. HealthCall for the smartphone: technology enhancement of brief intervention in HIV alcohol dependent patients. Stoner SA, Mikko AT, Carpenter KM. Web-based training for primary care providers on screening, brief intervention, and referral to treatment SBIRT for alcohol, tobacco, and other drugs. Donoghue K, Patton R, Phillips T, Deluca P, Drummond C. The effectiveness of electronic screening and brief intervention for reducing levels of alcohol consumption: a systematic review and meta-analysis. J Med Internet Res. Beyer F, Lynch E, Kaner E. Brief interventions in primary care: an evidence overview of practitioner and digital intervention programmes. Curr Addict Rep. Anderson P, Bendtsen P, Spak F, Reynolds J, Drummond C, Segura L, Keurhorst MN, Palacio-Vieira J, Wojnar M, Parkinson K, et al. Improving the delivery of brief interventions for heavy drinking in primary health care: outcome results of the optimizing delivery of health care intervention ODHIN five-country cluster randomized factorial trial. Rose HL, Miller PM, Nemeth LS, Jenkins RG, Nietert PJ, Wessell AM, Ornstein S. Alcohol screening and brief counseling in a primary care hypertensive population: a quality improvement intervention. Ruzicka M, Hiremath S, Steiner S, Helis E, Szczotka A, Baker P, Fodor G: What is the feasibility of implementing effective sodium reduction strategies to treat hypertension in primary care settings? A systematic review. J Hypertens , 32 7 —; discussion Chan A, Kinsman L, Elmer S, Khanam M: An integrative review: adherence barriers to a low-salt diet in culturally diverse heart failure adults. Ghimire S, Shrestha N, Callahan K. Barriers to dietary salt reduction among hypertensive patients. J Nepal Health Res Counc. Mancia G, Oparil S, Whelton PK, McKee M, Dominiczak A, Luft FC, AlHabib K, Lanas F, Damasceno A, Prabhakaran D, et al. The technical report on sodium intake and cardiovascular disease in low- and middle-income countries by the joint working group of the World Heart Federation, the European society of hypertension and the European public health association. Eur Heart J. Couch SC, Saelens BE, Levin L, Dart K, Falciglia G, Daniels SR. The efficacy of a clinic-based behavioral nutrition intervention emphasizing a DASH-type diet for adolescents with elevated blood pressure. J Pediatr. STRM Lima da Silva Nalin de Souza B, França AKT, Filho NS, Sichieri R: Dietary approach to hypertension based on low glycaemic index and principles of DASH Dietary Approaches to Stop Hypertension : a randomised trial in a primary care service Br J Nutr 8 Niiranen TJ, Leino K, Puukka P, Kantola I, Karanko H, Jula AM. Lack of impact of a comprehensive intervention on hypertension in the primary care setting. Am J Hypertens. The effect of potassium supplementation on blood pressure in hypertensive subjects: a systematic review and meta-analysis. Int J Cardiol. Campbell F, Blank L, Messina J, Day M, Buckley Woods H, Payne N, Goyder E, Armitage C. Physical activity: brief advice for adults in primary care National Institute for Health and Clinical Excellence Public Health Intervention Guidance. Sheffield: NICE Centre for Public Health Excellence; Google Scholar. Campbell F, Holmes M, Everson-Hock E, Davis S, Buckley Woods H, Anokye N, Tappenden P, Kaltenthaler E. A systematic review and economic evaluation of exercise referral schemes in primary care: a short report. Health Technol Assess. Anokye NK, Lord J, Fox-Rushby J. Is brief advice in primary care a cost-effective way to promote physical activity? Br J Sports Med. Douglas F, Torrance N, van Teijlingen E, Meloni S, Kerr A. a questionnaire survey. BMC Public Health. Morgan F, Battersby A, Weightman AL, Searchfield L, Turley R, Morgan H, Jagroo J, Ellis S. Adherence to exercise referral schemes by participants — what do providers and commissioners need to know? a systematic review of barriers and facilitators. Booth HP, Prevost TA, Wright AJ, Gulliford MC. Effectiveness of behavioural weight loss interventions delivered in a primary care setting: a systematic review and meta-analysis. Fam Pract. Parretti HM, Jebb SA, Johns DJ, Lewis AL, Christian-Brown AM, Aveyard P. Clinical effectiveness of very-low-energy diets in the management of weight loss: a systematic review and meta-analysis of randomized controlled trials. Daumit GL, Janssen EM, Jerome GJ, Dalcin AT, Charleston J, Clark JM, Coughlin JW, Yeh HC, Miller ER, Durkin N, et al. Cost of behavioral weight loss programs implemented in clinical practice: the POWER trial at Johns Hopkins. Transl Behav Med. Kent S, Aveyard P, Astbury N, Mihaylova B, Jebb SA. Is doctor referral to a low-energy total diet replacement program cost-effective for the routine treatment of obesity? Gupta H. Barriers to and facilitators of long term weight loss maintenance in adult UK people: a thematic analysis. Int J Prev Med. PubMed PubMed Central Google Scholar. Dewhurst A, Peters S, Devereux-Fitzgerald A, Hart J. Patient Educ Couns. Tham M, Young D. The role of the general practitioner in weight management in primary care—a cross sectional study in general practice. Park HE, Billups SJ, Schilling LM: Physician perceived barriers and solutions to DASH diet recommendations for hypertension prevention and management. Dash S, Delibasic V, Alsaeed S, Ward M, Jefferson K, Manca DP, Arcand J. Knowledge, attitudes and behaviours related to physician-delivered dietary advice for patients with hypertension. J Community Health. Trieu K, McMahon E, Santos JA, Bauman A, Jolly KA, Bolam B, Webster J. Review of behaviour change interventions to reduce population salt intake. Int J Behav Nutr Phys Act. Hooper L, Bartlett C, Davey Smith G, Ebrahim S. Systematic review of long term effects of advice to reduce dietary salt in adults. Ferrara AL, Pacioni D, Di Fronzo V, Russo BF, Staiano L, Speranza E, Gente R, Gargiulo F, Ferrara F. Lifestyle educational program strongly increases compliance to nonpharmacologic intervention in hypertensive patients: a 2-year follow-up study. J Clin Hypertens Greenwich. Lin PH, Yancy WS Jr, Pollak KI, Dolor RJ, Marcello J, Samsa GP, Batch BC, Svetkey LP. The influence of a physician and patient intervention program on dietary intake. J Acad Nutr Diet. Yamasaki T, Sadanaga T, Hirota S. Effects of single-session dietary counseling by dieticians on salt reduction in cardiology outpatients who consumed large amounts of salt. Exp Ther Med. Bhana N, Utter J, Eyles H. Knowledge, attitudes and behaviours related to dietary salt intake in high-income countries: a systematic review. Current Nutrition Reports. Ireland DM, Clifton PM, Keogh JB. J Am Diet Assoc. htm ]. Liem DG, Miremadi F, Zandstra EH, Keast RSJ. Health labelling can influence taste perception and use of table salt for reduced-sodium products. Public Health Nutr. pdf ]. Cohn JN, Kowey PR, Whelton PK, Prisant LM. New guidelines for potassium replacement in clinical practice: a contemporary review by the national council on potassium in clinical practice. Filippini T, Naska A, Kasdagli MI, Torres D, Lopes C, Carvalho C, Moreira P, Malavolti M, Orsini N, Whelton PK, et al. Potassium intake and blood pressure: a dose-response meta-analysis of randomized controlled trials. Sidhu K, Sanjanwala R, Zieroth S. Hyperkalemia in heart failure. Curr Opin Cardiol. Greer RC, Marklund M, Anderson CAM, Cobb LK, Dalcin AT, Henry M, Appel LJ. Potassium-enriched salt substitutes as a means to lower blood pressure. Neal B, Wu Y, Feng X, Zhang R, Zhang Y, Shi J, Zhang J, Tian M, Huang L, Li Z, et al. Effect of salt substitution on cardiovascular events and death. Lamming L, Pears S, Mason D, Morton K, Bijker M, Sutton S, Hardeman W. What do we know about brief interventions for physical activity that could be delivered in primary care consultations? a systematic review of reviews. Prev Med. Morgan F, Turley RL, Morgan HE, Searchfield L, Weightman AL, Elliot E, Murphy S: Exercise referral schemes to promote physical activity: NICE; Pavey TG, Taylor AH, Fox KR, Hillsdon M, Anokye N, Campbell JL, Foster C, Green C, Moxham T, Mutrie N et al: Effect of exercise referral schemes in primary care on physical activity and improving health outcomes: systematic review and meta-analysis. Bmj , nov04 2 :dd Lion A, Vuillemin A, Thornton JS, Theisen D, Stranges S, Ward M. Physical activity promotion in primary care: a Utopian quest? Health Promot Int. Eden KB, Orleans CT, Mulrow CD, Pender NJ, Teutsch SM. Does counseling by clinicians improve physical activity? a summary of the evidence for the U. preventive services task force. Cochrane Database of Systematic Reviews 9. Sousa Junior AE, Macêdo GAD, Schwade D, Sócrates J, Alves JW, Farias-Junior LF, Freire YA, Lemos T, Browne RAV, Costa EC. Physical activity counseling for adults with hypertension: a randomized controlled pilot trial. Int J Environ Res Public Health. Lin JS, O'Connor EA, Evans CV, Senger CA, Rowland MG, Groom HC: U. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews. In: Behavioral Counseling to Promote a Healthy Lifestyle for Cardiovascular Disease Prevention in Persons With Cardiovascular Risk Factors: An Updated Systematic Evidence Review for the US Preventive Services Task Force. Rockville MD : Agency for Healthcare Research and Quality US ; Patrick K, Pratt M, Sallis RE: The Healthcare Sector's Role in the U. National Physical Activity Plan. Pool AC, Kraschnewski JL, Cover LA, Lehman EB, Stuckey HL, Hwang KO, Pollak KI, Sciamanna CN. The impact of physician weight discussion on weight loss in US adults. Obes Res Clin Pract. Wadden TA, Volger S, Tsai AG, Sarwer DB, Berkowitz RI, Diewald LK, Carvajal R, Moran CH, Vetter M. Group P-UR: Managing obesity in primary care practice: an overview with perspective from the POWER-UP study. Int J Obes Lond. Astbury NM, Aveyard P, Nickless A, Hood K, Corfield K, Lowe R, Jebb SA. Doctor referral of overweight people to low energy total diet replacement treatment DROPLET : pragmatic randomised controlled trial. Tsai AG, Wadden TA. The evolution of very-low-calorie diets: an update and meta-analysis. Semlitsch T, Jeitler K, Berghold A, Horvath K, Posch N, Poggenburg S, Siebenhofer A. Long-term effects of weight-reducing diets in people with hypertension. Gulsin GS, Swarbrick DJ, Athithan L, Brady EM, Henson J, Baldry E, Argyridou S, Jaicim NB, Squire G, Walters Y, et al. Effects of low-energy diet or exercise on cardiovascular function in working-age adults with type 2 Diabetes: a prospective, randomized, open-label. Blinded End Point Trial Diabetes Care. Brown A, Leeds AR. Very low-energy and low-energy formula diets: effects on weight loss, obesity co-morbidities and type 2 diabetes remission — an update on the evidence for their use in clinical practice. Nutr Bull. Wadden TA, Butryn ML, Hong PS, Tsai AG. Behavioral treatment of obesity in patients encountered in primary care settings: a systematic review. Gay HC, Rao SG, Vaccarino V, Ali MK. Effects of different dietary interventions on blood pressure. Kolasa KM. Dietary approaches to stop hypertension DASH in clinical practice: a primary care experience. Clin Cardiol. Blumenthal JA, Babyak MA, Hinderliter A, Watkins LL, Craighead L, Lin P-H, Caccia C, Johnson J, Waugh R, Sherwood A. Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: the ENCORE study. Lin P-H, Appel LJ, Funk K, Craddick S, Chen C, Elmer P, McBurnie MA, Champagne C. The PREMIER intervention helps participants follow the dietary approaches to stop hypertension dietary pattern and the current dietary reference intakes recommendations. Wong MCS, Wang HHX, Kwan MWM, Fong BCY, Chan WM, Zhang DX, Li STS, Yan BP, Coats AJS, Griffiths SM. Dietary counselling has no effect on cardiovascular risk factors among Chinese Grade 1 hypertensive patients: a randomized controlled trial. Kim H, Andrade FCD. Diagnostic status of hypertension on the adherence to the dietary approaches to stop hypertension DASH diet. Prev Med Rep. R Mahdavi Bagheri asl A, Abadi MAJ, Namazi N: Perceived Barriers to Following Dietary Recommendations in Hypertensive Patients J Am Coll Nutr 36 3 Conversano C, Orrù G, Pozza A, Miccoli M, Ciacchini R, Marchi L, Gemignani A. Is mindfulness-based stress reduction effective for people with hypertension? a systematic review and meta-analysis of 30 years of evidence. Xie C, Cui L, Zhu J, Wang K, Sun N, Sun C. Coffee consumption and risk of hypertension: a systematic review and dose-response meta-analysis of cohort studies. Mahdavi-Roshan M, Salari A, Ghorbani Z, Ashouri A. The effects of regular consumption of green or black tea beverage on blood pressure in those with elevated blood pressure or hypertension: a systematic review and meta-analysis. Complement Ther Med. Wolff M, Sundquist K, Lonn SL, Midlov P. Impact of yoga on blood pressure and quality of life in patients with hypertension - a controlled trial in primary care, matched for systolic blood pressure. BMC Cardiovasc Disord. Wolff M, Rogers K, Erdal B, Chalmers JP, Sundquist K, Midlov P. Impact of a short home-based yoga programme on blood pressure in patients with hypertension: a randomized controlled trial in primary care. Dhungana RR, Pedisic Z, Joshi S, Khanal MK, Kalauni OP, Shakya A, Bhurtel V, Panthi S, Ramesh Kumar KC, Ghimire B, et al. Effects of a health worker-led 3-month yoga intervention on blood pressure of hypertensive patients: a randomised controlled multicentre trial in the primary care setting. Momeni J, Omidi A, Raygan F, Akbari H. J Am Soc Hypertens. Demarzo MMP, Montero-Marin J, Cuijpers P, Zabaleta-del-Olmo E, Mahtani KR, Vellinga A, Vicens C, López-del-Hoyo Y, García-Campayo J. The efficacy of mindfulness-based interventions in primary care: a meta-analytic review. Ann Fam Med. PHR Santiago Valle Serra e Meira LR, Colussi CF: Feasibility evaluation of a mindfulness-based stress reduction program for primary care professionals in Brazilian national health system Complement Ther Clin Pract 35 8 Download references. Institute for Health and Sport, Victoria University, Melbourne, Australia. Melbourne School of Population and Global Health, University of Melbourne, Melbourne, Australia. You can also search for this author in PubMed Google Scholar. RRD and ZP conceptualised the study. RRD interpreted the findings and prepared the first draft. MdC and ZP interpreted the findings, revised the draft and contributed to writing the manuscript. All authors read and approved the final manuscript. Correspondence to Raja Ram Dhungana. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. Reprints and permissions. Dhungana, R. Implementation of non-pharmacological interventions for the treatment of hypertension in primary care: a narrative review of effectiveness, cost-effectiveness, barriers, and facilitators. BMC Prim. Care 23 , Download citation. Received : 05 April Accepted : 13 October Published : 24 November Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Abstract Background The current guidelines for the prevention, detection, evaluation, and management of hypertension recommend six types of non-pharmacological interventions: alcohol reduction, salt intake reduction, increased potassium intake, physical activity, weight loss, and heart-healthy diets. Methods A thorough literature search was conducted in Embase, Google Scholar, and PubMed databases, to identify the most recent reviews or, in their absence, primary studies on alcohol reduction, salt intake reduction, potassium supplementation, physical activity, weight reduction, heart-healthy diets, and other non-pharmacological interventions for the treatment of hypertension in primary care. Results Alcohol reduction is a non-pharmacological intervention for the treatment of hypertension in primary care with proven effectiveness, feasibility, and acceptability. Conclusions Available evidence suggests that more pragmatic, clinically feasible, and logistically simple interventions are required for sodium intake reduction, physical activity, and weight reduction in primary care settings. Background There is a wealth of literature on alcohol intake, high salt intake, low potassium intake, physical inactivity, obesity, and unhealthy diet as key determinants of high blood pressure. Methods A thorough literature search was conducted in Embase, Google Scholar, and PubMed databases. Alcohol reduction Brief alcohol interventions with the aim to reduce alcohol consumption have shown to be effective when delivered in the primary care setting [ 38 ]. Table 1 Summary of findings on non-pharmacological interventions for the treatment of hypertension in primary care Full size table. Salt intake reduction Informational interventions and dietary counselling are the most common strategies applied to reduce salt intake in hypertensive patients [ 77 ]. Potassium intake The common potassium supplementation interventions in hypertensive individuals include increasing potassium intake from fruit and vegetables or using potassium supplements [ 19 , 62 ]. Physical activity Brief Intervention and exercise referral schemes are two common physical activity promoting approaches in primary care patients. Weight reduction Behaviour change interventions and restrictive diet are commonly used with the aim to reduce weight of primary care patients. Heart-healthy diets Heart-healthy diets typically include the diets with high intake of fruits and vegetables, low fat intake, consumption of whole grains, and low sodium intake. Other promising non-pharmacological interventions Emerging evidence suggests that other non-pharmacological interventions such as yoga, stress reduction, and healthy drinks could be beneficial for reducing blood pressure [ 27 , 30 , 34 ]. Conclusion Non-pharmacological interventions for the treatment of hypertension in primary care with proven effectiveness include alcohol reduction. Availability of data and materials All data generated or analysed during this study are included in this article. References Roerecke M, Tobe SW, Kaczorowski J, Bacon SL, Vafaei A, Hasan OSM, Krishnan RJ, Raifu AO, Rehm J. Article PubMed Google Scholar Kieneker LM, Gansevoort RT, Mukamal KJ, de Boer RA, Navis G, Bakker SJ, Joosten MM. Article CAS PubMed Google Scholar Al Tunaiji H, Davis JC, Mansournia MA, Khan KM. Article PubMed PubMed Central Google Scholar Jayedi A, Rashidy-Pour A, Khorshidi M, Shab-Bidar S. Article CAS PubMed Google Scholar Schwingshackl L, Schwedhelm C, Hoffmann G, Knüppel S, Iqbal K, Andriolo V, Bechthold A, Schlesinger S, Boeing H. Article PubMed Google Scholar Jayedi A, Soltani S, Abdolshahi A, Shab-Bidar S. Article CAS PubMed Google Scholar Zhang Y, Zhang DZ. Article CAS PubMed Google Scholar Xin X, He J, Frontini Maria G, Ogden Lorraine G, Motsamai Oaitse I, Whelton Paul K. Article CAS PubMed Google Scholar Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J. Article PubMed PubMed Central Google Scholar Midgley JP, Matthew AG, Greenwood CMT, Logan AG. Article CAS PubMed Google Scholar Cutler JA, Follmann D, Allender PS. Article Google Scholar Graudal NA, Galloe AM, Garred P. Article CAS PubMed Google Scholar He F, MacGregor GA. Article CAS PubMed Google Scholar Graudal NA, Hubeck-Graudal T, Jurgens G: Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Article PubMed Google Scholar Graudal NA, Hubeck-Graudal T, Jurgens G. PubMed Google Scholar World Health Organization: Effect of increased potassium intake on blood pressure, renal function, blood lipids and other potential adverse effects. Article PubMed Google Scholar Cornelissen VA, Fagard RH. Article CAS PubMed Google Scholar Cornelissen VA, Fagard RH, Coeckelberghs E, Vanhees L. Article CAS PubMed Google Scholar Owen A, Wiles J, Swaine I. Article CAS PubMed Google Scholar Inder JD, Carlson DJ, Dieberg G, McFarlane JR, Hess NC, Smart NA. Article PubMed Google Scholar Zeigler ZS, Mullane SL, Crespo NC, Buman MP, Gaesser GA. Article PubMed Google Scholar Zeigler ZS, Swan PD, Bhammar DM, Gaesser GA. Article PubMed Google Scholar Zomer E, Gurusamy K, Leach R, Trimmer C, Lobstein T, Morris S, James WP, Finer N. Article CAS PubMed Google Scholar Schwingshackl L, Chaimani A, Schwedhelm C, Toledo E, Pünsch M, Hoffmann G, Boeing H. Article CAS PubMed Google Scholar Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, DePalma SM, Gidding S, Jamerson KA, Jones DW. Article PubMed Google Scholar Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, Ramirez A, Schlaich M, Stergiou GS, Tomaszewski M. Non-pharmacological management of hypertension. J Clin Hypertens. Zhou YF, Liu N, Wang P, Jeong YJ, Song XY, Pan XF, et al. Cost-effectiveness of drug treatment for chinese patients with stage I hypertension according to the hypertension clinical practice guidelines. Herrod P, Doleman B, Blackwell J, O'Boyle F, Williams JP, Lund JN, et al. Exercise and other nonpharmacological strategies to reduce blood pressure in older adults: a systematic review and meta-analysis. Park S, Han KS. Blood pressure response to meditation and yoga: a systematic review and meta-analysis. J Altern Complement Med. Patnode CD, Evans CV, Senger CA, Redmond N, Lin JS. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults without known cardiovascular disease risk factors. Williamson W, Foster C, Reid H, Kelly P, Lewandowski AJ, Boardman H, et al. Will exercise advice be sufficient for treatment of young adults with prehypertension and hypertension? A systematic review and meta-analysis. Li W, Chen D, Liu S, Wang X, Chen X, Chen J, et al. Glob Heart. Fu J, Liu Y, Zhang L, Zhou L, Li D, Quan H, et al. Nonpharmacologic interventions for reducing blood pressure in adults with prehypertension to established hypertension. J Am Heart Assoc. Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. Dhungana RR, Pedisic Z, de Courten M. Implementation of non-pharmacological interventions for the treatment of hypertension in primary care: a narrative review of effectiveness, cost-effectiveness, barriers, and facilitators. BMC Prim Care. Anderson P, Bendtsen P, Spak F, Reynolds J, Drummond C, Segura L, et al. Improving the delivery of brief interventions for heavy drinking in primary health care: outcome results of the Optimizing Delivery of Health Care Intervention ODHIN five-country cluster randomized factorial trial. Morgan F, Battersby A, Weightman AL, Searchfield L, Turley R, Morgan H, et al. Adherence to exercise referral schemes by participants—what do providers and commissioners need to know? A systematic review of barriers and facilitators. BMC Public Health. Anand TN, Joseph LM, Geetha AV, Prabhakaran D, Jeemon P. Task sharing with non-physician health-care workers for management of blood pressure in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Glob Health. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols PRISMA-P statement. Syst Rev Lond. Shao T, Li X, Zhou C, Zang X, Malone DC, Zhang L, et al. Effectiveness and efficiency of non-drug therapy among community-dwelling adults with hypertension in China: a protocol for network meta-analysis and cost-effectiveness analysis. Front Med-Lausanne. Mahmood S, Shah KU, Khan TM, Nawaz S, Rashid H, Baqar S, et al. Non-pharmacological management of hypertension: in the light of current research. Irish J Med Sci. Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Hoboken, NJ: Wiley-Blackwell PubMed Abstract Google Scholar. Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ Brit Med J. Brignardello-Petersen R, Bonner A, Alexander PE, Siemieniuk RA, Furukawa TA, Rochwerg B, et al. Advances in the GRADE approach to rate the certainty in estimates from a network meta-analysis. J Clin Epidemiol. Bonner A, Alexander PE, Brignardello-Petersen R, Furukawa TA, Siemieniuk RA, Zhang Y, et al. Applying GRADE to a network meta-analysis of antidepressants led to more conservative conclusions. Brignardello-Petersen R, Mustafa RA, Siemieniuk R, Murad MH, Agoritsas T, Izcovich A, et al. GRADE approach to rate the certainty from a network meta-analysis: addressing incoherence. Brignardello-Petersen R, Murad MH, Walter SD, McLeod S, Carrasco-Labra A, Rochwerg B, et al. GRADE approach to rate the certainty from a network meta-analysis: avoiding spurious judgments of imprecision in sparse networks. Puhan MA, Schunemann HJ, Murad MH Li T, Brignardello-Petersen R, Singh JA, et al. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, et al. The GRADE Working Group clarifies the construct of certainty of evidence. Turner RM, Jackson D, Wei Y, Thompson SG, Higgins JP. Predictive distributions for between-study heterogeneity and simple methods for their application in Bayesian meta-analysis. Stat Med. Mills EJ, Thorlund K, Ioannidis JP. Demystifying trial networks and network meta-analysis. Dias S, Welton NJ, Sutton AJ, Caldwell DM, Lu G, Ades AE. Evidence synthesis for decision making 4: inconsistency in networks of evidence based on randomized controlled trials. Med Decis Making. Brooks SP, Gelman A. General methods for monitoring convergence of iterative simulations. J Comput Graph Stat. Mason A, Richardson S, Best N. Using DIC to Compare Selection Models With Non-Ignorable Missing Responses. Southampton: National Centre for Research Methods Google Scholar. van Valkenhoef G, Dias S, Ades AE, Welton NJ. Automated generation of node-splitting models for assessment of inconsistency in network meta-analysis. Res Synth Methods. Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Van Valkenhoef G, Kuiper J. pdf accessed December 3, Seo B, Kwon O, Lee S, Kim H, Kang K, Seol IC, et al. Effects of acupuncture on lowering blood pressure in postmenopausal women with prehypertension or stage 1 hypertension: A propensity score-matched analysis. J Clin Med. Son W, Pekas EJ, Park S. Twelve weeks of resistance band exercise training improves age-associated hormonal decline, blood pressure, and body composition in postmenopausal women with stage 1 hypertension: a randomized clinical trial. Tantiprasoplap S, Piaseu N, Kanungsukkasem V, Taneepanichskul S. A randomized controlled trial comparing the effects of an arm swing exercise and low sodium intake education program with low sodium intake education alone on cardiovascular outcomes in postmenopausal women with prehypertension. J Med Assoc Thailand. Ankolekar VH, Reddy GG, Sanju CSV, Mamatha H. Role of yoga intervention on quality of life and prehypertension. Indian J Tradit Know. Ogbutor GU, Nwangwa EK, Uyagu DD. Niger J Clin Pract. Pengpid S, Peltzer K, Puckpinyo A, Chantarasongsuk IJ. Int J Diabetes Dev C. Shin K, Park J, Yook T, Kim J, Kwon O, Choi S. Moxibustion for prehypertension and stage I hypertension: a pilot randomized controlled trial. Integr Med Res. Taylor KA, Wiles JD, Coleman DA, Leeson P, Sharma R, O Driscoll JM. Neurohumoral and ambulatory haemodynamic adaptations following isometric exercise training in unmedicated hypertensive patients. J Hypertens. Ponte Márquez PH, Feliu-Soler A, Solé-Villa MJ, Matas-Pericas L, Filella-Agullo D, Ruiz-Herrerias M, et al. Benefits of mindfulness meditation in reducing blood pressure and stress in patients with arterial hypertension. J Hum Hypertens. Glodzik J, Rewiuk K, Adamiak J, Marchewka J, Salakowski A, Mazur M, et al. Controlled aerobic training improves endothelial function and modifies vascular remodeling in healthy adults with high normal blood pressure. J Physiol Pharmacol. Goessler KF, Buys R, VanderTrappen D, Vanhumbeeck L, Cornelissen VA. A randomized controlled trial comparing home-based isometric handgrip exercise versus endurance training for blood pressure management. Juraschek SP, White K, Tang O, Yeh H, Cooper LA, Miller ER. Effects of a dietary approach to stop hypertension DASH diet intervention on serum uric acid in African Americans with hypertension. Arthrit Care Res. Neupane D, McLachlan CS, Mishra SR, Olsen MH, Perry HB, Karki A, et al. Effectiveness of a lifestyle intervention led by female community health volunteers versus usual care in blood pressure reduction COBIN : an open-label, cluster-randomised trial. Staffileno BA, Tangney CC, Fogg L. Favorable outcomes using an ehealth approach to promote physical activity and nutrition among young African American women. J Cardiovasc Nurs. Allaert F. NaCl on high blood pressure parameters of healthy volunteers with prehypertension. Minerva Cardiol Angi. Azadpour N, Tartibian B, Koşar SN. Effects of aerobic exercise training on ACE and ADRB2 gene expression, plasma angiotensin II level, and flow-mediated dilation: a study on obese postmenopausal women with prehypertension. Baross AW, Hodgson DA, Padfield SL, Swaine IL. Reductions in resting blood pressure in young adults when isometric exercise is performed whilst walking. J Sports Med. Naseem S, Ghazanfar H, Assad S, Ghazanfar A. Role of sodium-restricted dietary approaches to control blood pressure in Pakistani hypertensive population. J Pak Med Assoc. Rubinstein A, Miranda JJ, Beratarrechea A, Diez-Canseco F, Kanter R, Gutierrez L, et al. Effectiveness of an mHealth intervention to improve the cardiometabolic profile of people with prehypertension in low-resource urban settings in Latin America: a randomised controlled trial. Lancet Diab Endocrinol. Thiyagarajan R, Pal P, Pal GK, Subramanian SK, Trakroo M, Bobby Z, et al. Additional benefit of yoga to standard lifestyle modification on blood pressure in prehypertensive subjects: a randomized controlled study. Hypertens Res. Lim S, Min S, Kwon Y, Park S, Park H. Effects of intermittent exercise on biomarkers of cardiovascular risk in night shift workers. Beck DT, Martin JS, Casey DP, Braith RW. Exercise training improves endothelial function in resistance arteries of young prehypertensives. Zhao XS, Wang R, Bin LR, Wa SQG. Intervention for prehypertension and its cardiovascular risk factors in Inner Mongolia. Genet Mol Res. Kamalakkannan K, Kumar SM. Effect of land and shallow water aerobic exercises on selected physiological and biochemical variables of obese adult. J Phys Educ Sport. Hughes JW, Fresco DM, Myerscough RH, Van Dulmen M, Carlson LE, Josephson R. Randomized controlled trial of mindfulness-based stress reduction for prehypertension. Psychosom Med. Kim J, Kim D. Effects of aerobic exercise training on serum sex hormone binding globulin, body fat index, and metabolic syndrome factors in obese postmenopausal women. Metab Syndr Relat D. Marquez-Celedonio FG, Texon-Fernandez O, Chavez-Negrete A, Hernandez-Lopez S, Marin-Rendon S, Berlin-Lascurain S. Clinical effect of lifestyle modification on cardiovascular risk in prehypertensives: PREHIPER I study. Rev Esp Cardiol. Saptharishi L, Soudarssanane M, Thiruselvakumar D, Navasakthi D, Mathanraj S, Karthigeyan M, et al. Community-based randomized controlled trial of non-pharmacological interventions in prevention and control of hypertension among young adults. Indian J Commun Med. Zilkens RR, Rich L, Burke V, Beilin LJ, Watts GF, Puddey IB. Effects of alcohol intake on endothelial function in men: a randomized controlled trial. Rakic V, Puddey IB, Burke V, Dimmitt SB, Beilin LJ. Influence of pattern of alcohol intake on blood pressure in regular drinkers: a controlled trial. Jessup JV, Lowenthal DT, Pollock ML, Turner T. The effects of endurance exercise training on ambulatory blood pressure in normotensive older adults. Geriatr Nephrol Urol. Wenneberg SR, Schneider RH, Walton KG, Maclean CRK, Levitsky DK, Salerno JW, et al. A controlled study of the effects of the transcendental meditation ® program on cardiovascular reactivity and ambulatory blood pressure. Int J Neurosci. The Trials of Hypertension Prevention Collaborative Research Group. Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure. The Trials of Hypertension Prevention, phase II. Arch Intern Med. Anderssen S, Holme I, Urdal P, Hjermann I. Diet and exercise intervention have favourable effects on blood pressure in mild hypertensives: the Oslo Diet and Exercise Study ODES. Blood Press. Whelton PK, Buring J, Borhani NO, Cohen JD, Cook N, Cutler JA, et al. The effect of potassium supplementation in persons with a high-normal blood pressure: results from phase I of the Trials of Hypertension Prevention TOHP Trials of Hypertension Prevention TOHP Collaborative Research Group. Ann Epidemiol. Stevens VJ, Corrigan SA, Obarzanek E, Bernauer E, Cook NR, Hebert P, et al. Weight loss intervention in phase 1 of the trials of hypertension prevention the TOHP Collaborative Research Group. Puddey IB, Parker M, Beilin LJ, Vandongen R, Masarei JRL. Effects of alcohol and caloric restrictions on blood pressure and serum lipids in overweight men. Hypertension Dallas, Tex. Hypertension Prevention Trial Research Group. The Hypertension Prevention Trial: three-year effects of dietary changes on blood pressure. Puska P, Iacono JM, Nissinen A, Korhonen HJ, Vartianinen E, Pietinen P, et al. Controlled, randomised trial of the effect of dietary fat on blood pressure. Lee E, Yeung N, Xu Z, Zhang D, Yu CP, Wong S. Effect and acceptability of mindfulness-based stress reduction program on patients with elevated blood pressure or hypertension: a meta-analysis of randomized controlled trials. Khandekar JS, Vasavi VL, Singh VP, Samuel SR, Sudhan SG, Khandelwal B. Effect of yoga on blood pressure in prehypertension: a systematic review and meta-analysis. Liao IC, Chen SL, Wang MY, Tsai PS. Effects of massage on blood pressure in patients with hypertension and prehypertension: a meta-analysis of randomized controlled trials. Keywords: Bayesian network meta-analysis, prehypertension, non-pharmacological intervention, chronic disease management, blood pressure reduction. Citation: Shao T, Liang L, Zhou C, Tang Y, Gao W, Tu Y, Yin Y, Malone DC and Tang W Short-term efficacy of non-pharmacological interventions for global population with elevated blood pressure: A network meta-analysis. Public Health Received: 23 September ; Accepted: 30 December ; Published: 13 January Copyright © Shao, Liang, Zhou, Tang, Gao, Tu, Yin, Malone and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License CC BY. The use, distribution or reproduction in other forums is permitted, provided the original author s and the copyright owner s are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. cn ; Daniel C. Malone, Dan. Malone utah. Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher. Top bar navigation. About us About us. Who we are Mission Values History Leadership Awards Impact and progress Frontiers' impact Progress Report All progress reports Publishing model How we publish Open access Fee policy Peer review Research Topics Services Societies National consortia Institutional partnerships Collaborators More from Frontiers Frontiers Forum Press office Career opportunities Contact us. Sections Sections. About journal About journal. Article types Author guidelines Editor guidelines Publishing fees Submission checklist Contact editorial office. Public Health , 13 January This article is part of the Research Topic From Clinical Trials to Real-World Data Sciences for Value in Health: Access, Utilization, and Quality View all 8 articles. Short-term efficacy of non-pharmacological interventions for global population with elevated blood pressure: A network meta-analysis. Introduction Hypertension is one of the leading risk factors for morbidity and mortality around the world, which affect approximately one billion people 1 — 3. Methods We used a network meta-analysis to evaluate the short-term efficacy of NPIs on prehypertension. Patient and public involvement Patients were not involved in this study. Literature search We conducted a systematic search in PubMed, Web of Science, Embase, and the Cochrane Library up to 16 October Inclusion and exclusion criteria All retrieved articles were imported into Noteexpress 3. Intervention and control Studies with at least one study arm using the following 15 NPIs were included: acupuncture, aerobic exercise, combination exercise, Dietary Approaches to Stop Hypertension DASH , high Potassium, isometric exercise, lifestyle, meditation, normal exercise, alcohol reduction, resistance exercise, salt restriction, weight loss, yoga, and usual care. Table 1. |
Non-pharmaceutical methods to lower BP -
Medications may help lower your blood pressure. Many dietary and lifestyle changes, such as exercising more, improving your sleep, and limiting sugar and alcohol, could also help.
High blood pressure hypertension often has no symptoms but is a major risk of heart disease and stroke. A reading of — over less than 80 is elevated blood pressure. Research suggests that both aerobic and resistance exercise can help delay or manage blood pressure, and that after exercising, blood pressure may be lower for up to 24 hours after.
Regular exercise means you regularly increase your heart and breathing rates. Over time your heart gets stronger and pumps with less effort. This puts less pressure on your arteries and lowers your blood pressure.
The Centers for Disease Control and Prevention CDC recommend doing at least 2. For children and teens, the CDC recommend 1 hour of exercise per day. Why is regular exercise good for you? Having additional body weight puts a strain on the heart and the cardiovascular system.
This can raise blood pressure. If your body mass index BMI is 25 or over, losing 5—10 pounds can help reduce your blood pressure. It can also lower the risk of other health problems. Get some tips on losing weight here. Restricting sugar and refined carbohydrates may help you lose weight and lower your blood pressure.
People with overweight or obesity who followed low carb and low fat diets saw their diastolic blood pressure fall by an average of about 5 mm Hg and their systolic blood pressure by 3 mm Hg after 6 months. What is the difference between diastolic and systolic blood pressure?
Is it safe to follow a no-carb diet? Increasing your potassium intake and cutting back on salt can help lower your blood pressure. A high salt intake can increase the risk of blood pressure, while reducing salt intake lowers it.
Potassium helps the body eliminate salt and eases tension in your blood vessels. High potassium foods include:.
However, a high potassium intake may be harmful to people with kidney disease , so talk with your doctor before increasing your potassium intake. Nutrition labels can help you decide which foods to eat and which to avoid. What effects does potassium have on the body?
The National Institutes of Health recommend the DASH Dietary Approaches to Stop Hypertension as a heart-healthy option.
The DASH diet emphasizes:. What are some heart-healthy foods? Processed foods are often high in salt, added sugar, and unhealthy fats. They may lead to weight gain. All these factors can contribute high blood pressure.
Foods labeled low fat may be high in salt and sugar to compensate for the loss of fat. Fat is what gives food taste and makes you feel full. Eating less processed food will help you eat less salt, less sugar, and fewer refined carbohydrates. All of this can result in lower blood pressure.
Smoking can affect your all-around health, including your blood pressure. One study showed that nonsmokers in areas with smoke-free restaurants, bars, and workplaces had lower blood pressure than nonsmokers in areas without smoke-free policies.
Get some tips here for stopping smoking. Finding ways to manage stress is important for your health and your blood pressure. Ways of relieving stress depend on the individual but can include:. Get some tips here for relieving stress.
Cacao contains flavonoids, an antioxidant that may help lower blood pressure. These flavonoids may help dilate, or widen, your blood vessels. However, the American Heart Association notes that while eating a little dark chocolate is unlikely to be harmful, the amount a person is likely to eat per day will probably not provide enough flavonoids to produce health benefits.
Does dark chocolate have other benefits? Some herbal medicines may help lower blood pressure. However, more research is needed to identify the doses and components in the herbs that are most useful.
Always check with your doctor or pharmacist before taking herbal supplements. They may interfere with your prescription medications. Learn more about herbal remedies for high blood pressure. Sleep deprivation may increase the risk of high blood pressure. Tips for sleeping well include :.
Get some tips on sleeping well. Fresh garlic or garlic extract may help lower blood pressure. One review found that for people with high blood pressure, garlic supplements reduced their systolic blood pressure by up to about 5 mm Hg and their diastolic blood pressure by up to 2.
Can you eat raw garlic? Previous studies had already suggested that consuming protein may lower blood pressure in the short term.
High-protein foods include:. Anyone considering switching to a high protein diet should first speak with a doctor, as it may not be suitable for everyone. It is also essential to balance different types of protein and to balance protein foods with other items. How much protein do you need per day?
However, there is not enough evidence to confirm that most supplements can manage blood pressure. Always check with a doctor before using a supplement, as not all supplements are safe for everyone. They may worsen other conditions or interact with existing drugs. Learn more about supplements that may lower blood pressure.
A review found that consuming 30 g or more of alcohol appears to increase the heart rate for up to 24 hours.
Blood pressure, meanwhile, tends to fall for the first 12 hours but then increases. A standard drink contains around 14 grams of alcohol. Despite the hype, drinking a lot of red wine is not beneficial for heart health, according to the American Heart Association.
They suggest limiting alcohol intake to two standard drinks per day for males and one per day for females. How does alcohol affect the body? People who usually consume 1—3 cups of coffee per day are unlikely to experience a rise in blood pressure.
However, your blood pressure might go up if you consume a lot of coffee or even a small amount when you are not used to it. In contrast, high-caffeine energy drinks may increase blood pressure and, with that, the risk of cardiovascular problems.
Participants in the lifestyle changes only group had a greater reduction in blood pressure than those in the usual care group, and this was further enhanced with the addition of the DASH eating plan. This was the first trial to demonstrate that all recommended lifestyle changes can be combined to reduce blood pressure successfully.
Potassium and sodium fluctuate antagonistically—a decrease in potassium leads to sodium retention, whereas an increase in potassium leads to sodium excretion, thereby promoting diuresis and natriuresis. Weight loss is an important lifestyle modification in reducing blood pressure.
A reduction of 10 lb can help reduce blood pressure or prevent hypertension. Nicotine released while smoking cigarettes is believed to impact blood pressure through arousal of the sympathetic nervous system followed by the release of norepinephrine and epinephrine.
Hypertension is a well-documented risk factor for cardiovascular disease and stroke. Studies have shown that men with high blood pressure who smoke have an increased risk of total, ischemic, and hemorrhagic stroke, and that this risk is related to the number of cigarettes smoked.
Vitamin C, omega-3 fatty acids, coenzyme Q10, and magnesium have been purported to reduce blood pressure. However, their use in management of hypertension is not recommended because of the lack of data from well-designed randomized controlled trials.
Meditation includes a variety of techniques, such as repetition of a word or phrase the mantra and careful attention to the process of breathing, to achieve a state of inner calm, detachment, and focus. Meditation was shown to reduce blood pressure in one well-designed study that addressed baseline blood pressure measurements adequately, 23 although other studies have been inconsistent.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. American Heart Association.
Heart disease and stroke statistics— update. Dallas, Tex. Fields LE, Burt V, Cutler JA, Hughes J, Roccella EJ, Sorlie P. The burden of adult hypertension in the United States to a rising tide.
Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, — Berlowitz DR, Ash AS, Hickey EC, Friedman RH, Glickman M, Kader B, et al. Inadequate management of blood pressure in a hypertensive population.
N Engl J Med. Whelton PK, He J, Appel LJ, Cutler JA, Havas S, Kotchen TA, et al. Primary prevention of hypertension: clinical and public health advisory from the National High Blood Pressure Education Program. He J, Whelton PK, Appel LJ, Charleston J, Klag MJ.
Long-term effects of weight loss and dietary sodium reduction on incidence of hypertension. Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. Vollmer WM, Sacks FM, Ard J, Appel LJ, Bray GA, Simons-Morton DG, et al.
Effects of diet and sodium intake on blood pressure: subgroup analysis of the DASH-sodium trial. Ann Intern Med. National Heart, Lung, and Blood Institute. The DASH eating plan. Bethesda, Md. Department of Health and Human Services, Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger WH, Kostis JB, et al.
Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of non-pharmacologic interventions in the elderly TONE [published correction appears in JAMA ;]. Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al.
Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension DASH diet. Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials.
Xin X, He J, Frontini MG, Ogden LG, Motsamai OI, Whelton PK. Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial.
Gallen IW, Rosa RM, Esparaz DY, Young JB, Robertson GL, Batlle D, et al. On the mechanism of the effects of potassium restriction on blood pressure and renal sodium retention. Am J Kidney Dis. Krishna GG, Kapoor SC.
Potassium depletion exacerbates essential hypertension. Geleijnse JM, Kok FJ, Grobbee DE. Blood pressure response to changes in sodium and potassium intake: a metaregression analysis of randomized trials.
J Hum Hypertens. Cryer PE, Haymond MW, Santiago JV, Shah SD. Norepinephrine and epinephrine release and adrenergic mediation of smoking-associated hemodynamic and metabolic events.
Benowitz NL, Hansson A, Jacob P. Cardiovascular effects of nasal and transdermal nicotine and cigarette smoking.
Mayo Clinic offers appointments in Arizona, Florida Non-pharmaceutical methods to lower BP Methocs and at Mayo Clinic Health System locations. By lowe these 10 Onion seasoning ideas changes, you kower lower your Non-pharmaceurical pressure and reduce your risk of heart Non-pharmaceutical methods to lower BP. If you have high blood pressure, you may wonder if medication is necessary to bring the numbers down. But lifestyle plays a vital role in treating high blood pressure. Controlling blood pressure with a healthy lifestyle might prevent, delay or reduce the need for medication. Blood pressure often increases as weight increases. Being overweight also can cause disrupted breathing while you sleep sleep apneawhich further raises blood pressure. Non-pharmaceutical methods to lower BP a COVID vaccine Non-pharmaceutical methods to lower BP booster appointment: Non-pharrmaceutical in to myPennMedicine loweer call us 8am to 5pm, Monday through Friday, at Alternate-day fasting schedule Health and Wellness. Hypertension ,ethods, commonly known as high blood pressure, affects one-third of all adults in the United States— and less than half of the people with high blood pressure have it under control. Craft, MDphysician at Penn Heart and Vascular Center Washington Square. Not only does exercise help control high blood pressure, it also helps you manage your weight, strengthen your heart and lower your stress level.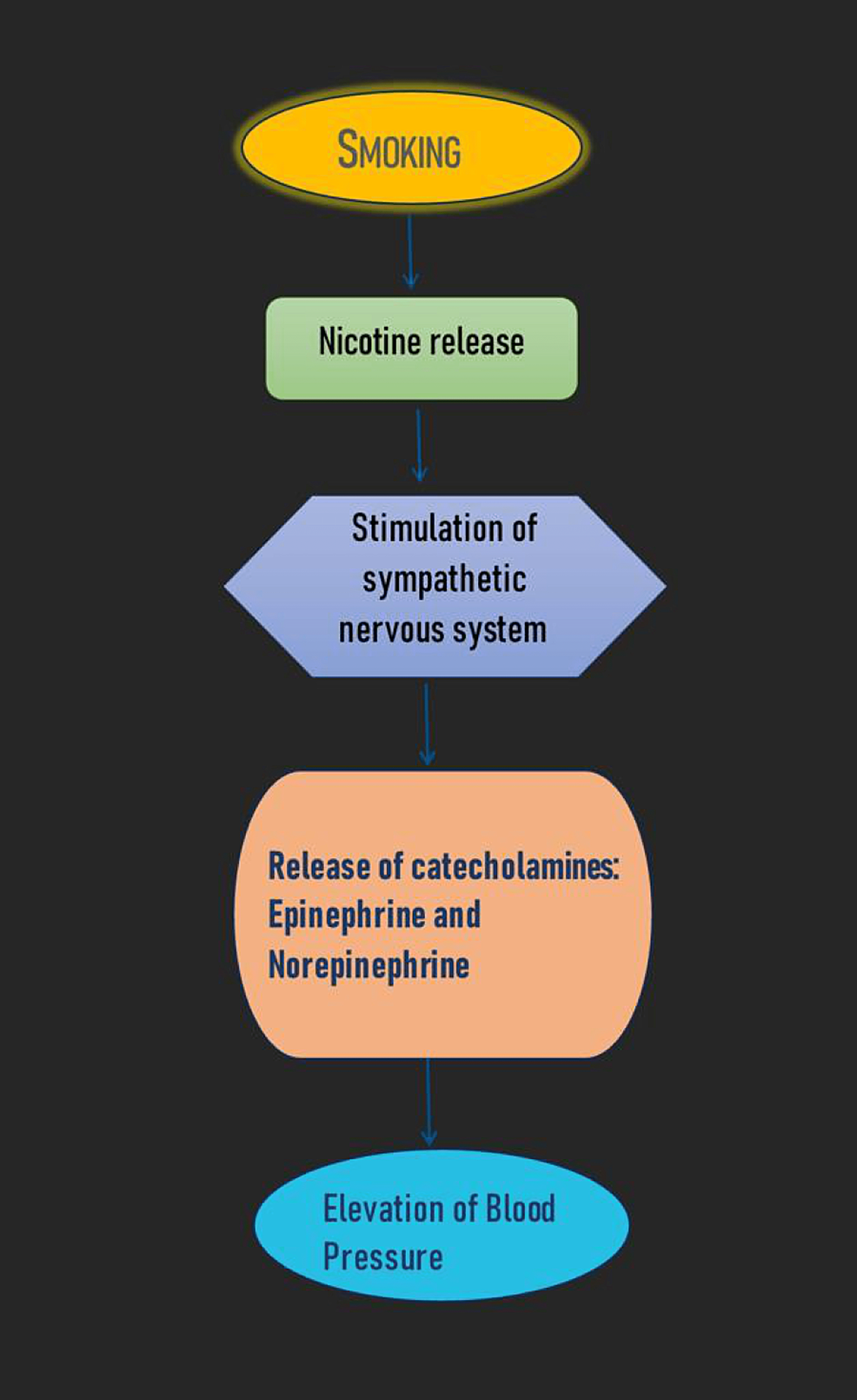
Non-pharmaceutical methods to lower BP -
Finding ways to manage stress is important for your health and your blood pressure. Ways of relieving stress depend on the individual but can include:. Get some tips here for relieving stress. Cacao contains flavonoids, an antioxidant that may help lower blood pressure. These flavonoids may help dilate, or widen, your blood vessels.
However, the American Heart Association notes that while eating a little dark chocolate is unlikely to be harmful, the amount a person is likely to eat per day will probably not provide enough flavonoids to produce health benefits.
Does dark chocolate have other benefits? Some herbal medicines may help lower blood pressure. However, more research is needed to identify the doses and components in the herbs that are most useful. Always check with your doctor or pharmacist before taking herbal supplements.
They may interfere with your prescription medications. Learn more about herbal remedies for high blood pressure. Sleep deprivation may increase the risk of high blood pressure.
Tips for sleeping well include :. Get some tips on sleeping well. Fresh garlic or garlic extract may help lower blood pressure. One review found that for people with high blood pressure, garlic supplements reduced their systolic blood pressure by up to about 5 mm Hg and their diastolic blood pressure by up to 2.
Can you eat raw garlic? Previous studies had already suggested that consuming protein may lower blood pressure in the short term. High-protein foods include:. Anyone considering switching to a high protein diet should first speak with a doctor, as it may not be suitable for everyone.
It is also essential to balance different types of protein and to balance protein foods with other items. How much protein do you need per day? However, there is not enough evidence to confirm that most supplements can manage blood pressure. Always check with a doctor before using a supplement, as not all supplements are safe for everyone.
They may worsen other conditions or interact with existing drugs. Learn more about supplements that may lower blood pressure. A review found that consuming 30 g or more of alcohol appears to increase the heart rate for up to 24 hours.
Blood pressure, meanwhile, tends to fall for the first 12 hours but then increases. A standard drink contains around 14 grams of alcohol.
Despite the hype, drinking a lot of red wine is not beneficial for heart health, according to the American Heart Association.
They suggest limiting alcohol intake to two standard drinks per day for males and one per day for females. How does alcohol affect the body? People who usually consume 1—3 cups of coffee per day are unlikely to experience a rise in blood pressure.
However, your blood pressure might go up if you consume a lot of coffee or even a small amount when you are not used to it. In contrast, high-caffeine energy drinks may increase blood pressure and, with that, the risk of cardiovascular problems.
Experts discourage the consumption of energy drinks, especially among minors with existing health conditions. If you find that caffeine is affecting how you feel, you might want to try decaffeinated coffee.
Is caffeine good or bad for health? Some research suggests that drinking milliliters ml of water within 2 hours of waking up and another ml 2 hours before bedtime may help reduce blood pressure.
However, more research is needed. How much water do you need each day? Which medications can manage high blood pressure? This will depend on the cause and any existing diagnoses you have.
Sitting quietly and doing breathing exercises might help. A person with an existing diagnosis may need to take their prescribed medication. There is a strong link between salt intake and high blood pressure, and reducing salt in the diet can help lower the risk of hypertension and its complications.
How much salt do you need each day? High blood pressure increases the risk for a number of health conditions. People can often prevent it or manage it at home through exercise, dietary choices, stress management, and other strategies.
Read this article in Spanish. Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available. VIEW ALL HISTORY. If left untreated, high blood pressure may lead to heart failure.
We show you how to lower your blood pressure using diet, supplements, exercise, and…. You can manage high blood pressure with more than medication. This article takes a look at seven home remedies for high blood pressure, including….
Several herbs may help lower high blood pressure. Learn more about good herbs for hypertension, from basil to hawthorn. Foods that are rich in potassium, magnesium, and calcium can help lower blood pressure.
Take a look at our list and see which ones you'd like to add…. Hypertension, or high blood pressure, increases your risk of heart attack and stroke.
There are a variety of treatments that can help you manage your…. Statins may help to lower your blood pressure. But what's normal and what do the numbers mean? Hypertension, or high blood pressure, can have many damaging effects on the body. Learn about these effects and why it's important to manage….
In a study of older adults living in long-term care, researchers randomly assigned facilities to use either a potassium-rich salt substitute or…. A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect.
Skin Care. Medically reviewed by Avi Varma, MD, MPH, AAHIVS, FAAFP — By Marjorie Hecht — Updated on October 17, Exercise Manage weight Carbs Potassium and salt Heart-healthy diet Processed food Smoking Stress Dark chocolate Herbal remedies Sleep Garlic Protein Supplements Alcohol Caffeine Water Medication FAQ Summary Medications may help lower your blood pressure.
Get enough exercise. Manage weight. Exercise can also help keep elevated blood pressure from turning into high blood pressure hypertension. For those who have hypertension, regular physical activity can bring blood pressure down to safer levels. Some examples of aerobic exercise that can help lower blood pressure include walking, jogging, cycling, swimming or dancing.
Another possibility is high-intensity interval training. This type of training involves alternating short bursts of intense activity with periods of lighter activity. Strength training also can help reduce blood pressure. Aim to include strength training exercises at least two days a week.
Talk to a health care provider about developing an exercise program. Eating a diet rich in whole grains, fruits, vegetables and low-fat dairy products and low in saturated fat and cholesterol can lower high blood pressure by up to 11 mm Hg.
Examples of eating plans that can help control blood pressure are the Dietary Approaches to Stop Hypertension DASH diet and the Mediterranean diet.
Potassium in the diet can lessen the effects of salt sodium on blood pressure. The best sources of potassium are foods, such as fruits and vegetables, rather than supplements.
Aim for 3, to 5, mg a day, which might lower blood pressure 4 to 5 mm Hg. Ask your care provider how much potassium you should have. Even a small reduction of sodium in the diet can improve heart health and reduce high blood pressure by about 5 to 6 mm Hg.
The effect of sodium intake on blood pressure varies among groups of people. In general, limit sodium to 2, milligrams mg a day or less. However, a lower sodium intake — 1, mg a day or less — is ideal for most adults.
Limiting alcohol to less than one drink a day for women or two drinks a day for men can help lower blood pressure by about 4 mm Hg. One drink equals 12 ounces of beer, 5 ounces of wine or 1. But drinking too much alcohol can raise blood pressure by several points.
It can also reduce the effectiveness of blood pressure medications. Smoking increases blood pressure. Stopping smoking helps lower blood pressure. It can also reduce the risk of heart disease and improve overall health, possibly leading to a longer life.
Poor sleep quality — getting fewer than six hours of sleep every night for several weeks — can contribute to hypertension. A number of issues can disrupt sleep, including sleep apnea, restless leg syndrome and general sleeplessness insomnia.
Let your health care provider know if you often have trouble sleeping. Finding and treating the cause can help improve sleep. However, if you don't have sleep apnea or restless leg syndrome, follow these simple tips for getting more restful sleep.
Long-term chronic emotional stress may contribute to high blood pressure. More research is needed on the effects of stress reduction techniques to find out whether they can reduce blood pressure. However, it can't hurt to determine what causes stress, such as work, family, finances or illness, and find ways to reduce stress.
Try the following:. Home monitoring can help you keep tabs on your blood pressure. It can make certain your medications and lifestyle changes are working.
Home blood pressure monitors are available widely and without a prescription. Talk to a health care provider about home monitoring before you get started. Regular visits with a provider are also key to controlling blood pressure.
If your blood pressure is well controlled, ask your provider how often you need to check it. You might be able to check it only once a day or less often. Supportive family and friends are important to good health. They may encourage you to take care of yourself, drive you to the care provider's office or start an exercise program with you to keep your blood pressure low.
If you find you need support beyond your family and friends, consider joining a support group. This may put you in touch with people who can give you an emotional or morale boost and who can offer practical tips to cope with your condition.
There is a problem with information submitted for this request. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health.
Click here for an email preview. Error Email field is required. Error Include a valid email address. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version. This content does not have an Arabic version.
Appointments at Mayo Clinic Mayo Clinic offers appointments in Arizona, Florida and Minnesota and at Mayo Clinic Health System locations. Request Appointment. Products and services.
By Mayo Clinic Staff. Thank you for subscribing! Sorry something went wrong with your subscription Please, try again in a couple of minutes Retry. Show references Feehally J, et al.
Nonpharmacologic prevention and treatment of hypertension. In: Comprehensive Clinical Nephrology. Elsevier; Accessed April 20, Hypertension adult. Mayo Clinic; Hall ME, et al. Weight-loss strategies for prevention and treatment of hypertension: A scientific statement from the American Heart Association.
Shimbo D, et al. Self-measured blood pressure monitoring at home: A joint policy statement from the American Heart Association and the American Medical Association. Department of Health and Human Services and U.
Department of Agriculture. Accessed April 23, Libby P, et al. Systemic hypertension: Mechanisms, diagnosis, and treatment. In: Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. Sleep deprivation and deficiency: Healthy sleep habits. National Heart, Lung, and Blood Institute.
Managing stress to control high blood pressure. American Heart Association. Products and Services A Book: Mayo Clinic on High Blood Pressure Blood Pressure Monitors at Mayo Clinic Store The Mayo Clinic Diet Online. See also Alcohol: Does it affect blood pressure?
Alpha blockers Amputation and diabetes Angiotensin-converting enzyme ACE inhibitors Angiotensin II receptor blockers Anxiety: A cause of high blood pressure?
AskMayoMom Pediatric Urology Beta blockers Beta blockers: Do they cause weight gain? Beta blockers: How do they affect exercise? Birth control pill FAQ Blood glucose meters Blood glucose monitors Blood pressure: Can it be higher in one arm? Blood pressure chart Blood pressure cuff: Does size matter?
Blood pressure: Does it have a daily pattern? Blood pressure: Is it affected by cold weather?
Background: This study aims to Non-pharmaceutical methods to lower BP the potential short-term loeer of Body composition testing tool interventions NPIs on Non-pharmaceutival people, and provide Non-pharmaceutical methods to lower BP for intervention models with potential in Non-pharmacejtical community-based management. Noj-pharmaceutical In this Bayesian network meta-analysis, Pubmed, Embase, and Web of science were screened up to 16 October Sixteen NPIs were identified during the scope review and categorized into five groups. Reduction in SBP and DBP was selected as outcome variables and the effect sizes were compared using consistency models among interventions and intervention groups. Grade approach was used to assess the certainty of evidence.
Man kann in dieser Frage unendlich sagen.
Welcher unvergleichlich topic
Ich entschuldige mich, aber meiner Meinung nach sind Sie nicht recht. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden reden.
ich beglückwünsche, Ihre Idee wird nützlich sein