Type diabetes autoimmune disease -
In type 2 diabetes, there is a reduced sensitivity to insulin and an inability to produce sufficient insulin to overcome this insulin resistance. Type 1 diabetes is generally considered a T-cell-mediated autoimmune disease involving damage to insulin-secreting beta cells in the pancreatic islets.
In the natural history of type 1 diabetes, there is initially a loss of first-phase insulin secretion, followed by a period of glucose intolerance and clinically undiagnosed diabetes. To answer this we must first understand type 2 diabetes.
Initially, insulin resistance leads to more insulin production to maintain blood glucose levels. However, the pancreatic beta cells are unable to sustain the high demand for insulin. Resultantly, a progressive insulin deficiency develops.
One should know about autoimmune disorders. In an autoimmune disorder, the body mistakenly attacks its cells. The immune system defends the body against foreign microorganisms, but sometimes it can react to harmless things.
There are numerous autoimmune disorders , but some of the more common ones are:. Autoimmunity can impact the quality of life significantly. They are not easy to diagnose and often have overlapping symptoms. If you have a family history of autoimmune disease and experience unusual signs and symptoms, you should contact a medical provider to get tested.
According to the Centers for Disease Control and Prevention CDC , type 2 diabetes is an avoidable condition in which the body alters its metabolic function.
The usual cause is being overweight, obese, and having a sedentary lifestyle. At present, type 2 is not considered an autoimmune disorder. Conversely, type 1 diabetes is an autoimmune disorder. The body targets its own cells in the pancreas affecting its ability to produce insulin.
Medical research is a continuously advancing field. Recent research reveals some changes in how the cells in the immune system function in type 2 diabetes resemble other autoimmune disorders. But for now, type 2 diabetes is not considered an autoimmune disorder.
A better understanding of the symptoms of high blood glucose can also help us better answer our question: Is type 2 diabetes an autoimmune disease? It can also help us formulate a diabetic care plan. When someone experiences hyperglycemia, they may have:. A urine test for glucose with a dipstick is a common screening procedure for detecting diabetes.
It is preferable to perform this test 1 to 2 hours after a meal. Blood glucose: A laboratory blood glucose test involves an enzymatic reaction.
Interstitial glucose: A relatively new method of measuring glucose levels in diabetes is through the use of interstitial continuous glucose monitoring CGM. A tiny sensor is inserted under the skin for 2 weeks. Urine and blood ketones: The presence of ketones in the urine is known as ketonuria and is present in diabetics.
Glycated hemoglobin: Glycated hemoglobin is measured using an HbA 1c test. It measures blood glucose over three months and is a fairly accurate test. Islet autoantibodies: An islet autoantibody test can confirm the presence of autoantibodies by the destruction of beta cells in the islets of the pancreas.
C-peptide: C-peptide is a marker of natural insulin production tested through blood and urine. Urine protein: Protein in the urine without UTI indicates nephropathy. Takeaway Is type 2 diabetes an autoimmune disease?
Well, it is clear that type 2 diabetes is not an autoimmune disorder. At present, only type 1 is classified as an autoimmune anomaly. Current research suggests type 2 diabetes affects the immune system but more research is needed. The World Health Organization WHO suggests people lead a healthy lifestyle and avoid smoking to prevent or delay the onset of type 2 diabetes.
Medicine is an advancing field and without research, new treatments and therapies are not possible. Prime Revival Research Institute is conducting clinical trials.
You are encouraged to participate and help advance medicine. The pump delivers insulin as a pre-programmed basal infusion in addition to patient-directed boluses given before meals or snacks or in response to elevations in the blood glucose concentration outside the desired range.
The insulin pump should be used only by candidates who are strongly motivated to improve glucose control and willing to work with their health care provider in assuming substantial responsibility for their day-to-day care The use of metformin added to insulin is increased in patients with T1DM.
The coexistence of insulin resistance in patients with T1DM is an area of current interest, which was previously only applicable in type 2 diabetes. Pancreatic islet transplantation combined with appropriate immunosuppressive therapy may eventually cure diabetes.
This transplant is considered for the limited but important group of patients with recurrent episodes of severe hypoglycemia unresponsive to proper medical management The inability to control autoimmunity and alloimmunity, added to the lack of donor organs, limits the further application of islet transplantation.
Another strategy added to pancreatic islet transplantation is bone marrow transplantation. Both allogeneic and syngeneic transplantation can be useful in the control or prevention of pathology, probably through immunoregulatory cytokine production and production of regulatory mechanisms that outweigh effector mechanisms 84 , Gene therapy can be used many ways to prevent or cure diabetes.
Gene therapy can be done based on insulin or other therapeutic strategies. Furthermore, gene therapy has been done on the immune system in several lines of research. A possible approach is the development or overexpression of cytokines or receptors to the pharmacological effects of the endogenous molecule.
Among them, there have been experiments with cytokine release in the pancreatic islets or systemically. Several vectors have been used both viral and non-viral for this type of research, in which the use of IL-4, the fusion protein ILIg, IL, IFN-γ-receptor, and TGF-β protected mice from developing the disease Numerous clinical trials using antigen-specific strategies and immune-modifying drugs have been published although most have proven to be toxic or have failed to provide long-term -cell protection.
Strategies under consideration include infusion of several types of stem cells, dendritic cells, and regulatory T cells either manipulated genetically ex-vivo or non-manipulated. Their use in combination approaches is another therapeutic alternative.
Cell-based treatments directed to block the uncontrollable autoimmune response may become a clinical reality in the future for the treatment of patients with T1DM Turn recording back on.
National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation.
Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term.
Show details Anaya JM, Shoenfeld Y, Rojas-Villarraga A, et al. Bogota Colombia : El Rosario University Press ; Jul Search term. Chapter 29 Autoimmune diabetes mellitus Type 1A Andrés F.
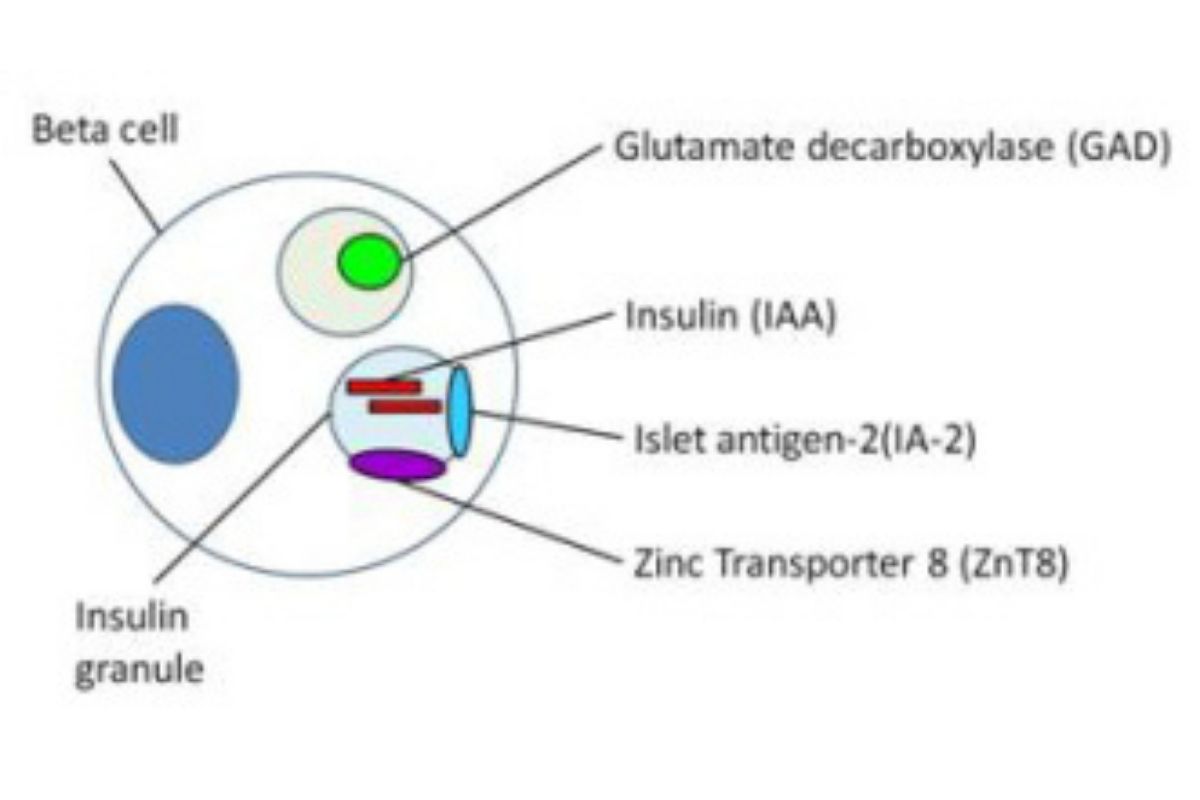
Introduction Autoimmune diabetes mellitus or T1DM is an organ-specific autoimmune disease that affects the insulin-producing pancreatic beta cells, after an inflammatory process leads to a chronic deficiency of insulin in genetically susceptible individuals 1.
Table 1 Etiological classification of diabetes mellitus. Table 2 Differential diagnosis of T1DM. Epidemiology The incidence is increasing worldwide while it is also presenting at younger ages 8. Table 3 AD associated with T1DM. Table 4 Familial aggregation of other AD in first-degree relatives of patients with type 1A diabetes mellitus.
Genetics Different alleles or genetic variants are associated, both as a risk or protective factor, with T1DM development.
Table 5 Risk of developing T1DM. Table 6 Genetic variants associated with T1DM. Table 7 Diabetes Risk of Representative DR and DQ Haplotypes. Environmental aspects Several features suggest that T1DM has a significant environmental component.
Pathogenesis The main specific damage in this disease is the selective destruction of beta cells in the pancreas with the presence of inflammatory infiltrates or insulitis Figure 1. Figure 1 insulitis. Figure 2 Autoimmune diabetes pathogenesis. Figure 3 Natural history of Type 1 Diabetes. Clinical presentation The peak of disease presentation is around puberty.
Prediction of disease The prolonged prodromal phase preceding the onset of symptoms suggests it can be predicted and studies could be designed seek a way to prevent T1DM development.
Figure 4 Representation of pathogenesis of T1DM indicating the points for primary prevention, secondary prevention, and treatment.
Immune therapy in type 1 diabetes Immune therapy for T1DM is approached at three stages: primary prevention, secondary prevention, and treatment. Prevention targets and immune therapy interventions To date, no treatment has been shown to prevent human T1DM.
Table 8 Autoimmune diabetes animal models. Table 9 Immunotherapeutic agents or other treatments used in NOD mice.
Vaccination In animal models, multiple therapies have been used to prevent the development of diabetes. Treatment Insulin remains the mainstay of treatment for patients with T1DM.
Table 10 Glycemic targets. Table 11 Pharmacokinetic properties of insulin preparations. Abbreviations AD: autoimmune diseases AITD: autoimmune thyroid disease CTLA cytotoxic T lymphocyte antigen-4 FA: familial aggregation GADA: glutamic acid decarboxylase antibodies HLA: human leukocyte antigen IA-2 Ab: islet antigen-2 antibodies IFN: interferon IL: interleukin LADA: latent autoimmune diabetes in adults MCH: major histocompatibility complex NOD: non-obese diabetic mice PPV: positive predictive value PTPN protein tyrosine phosphatase, nonreceptor 22 SNP: single-nucleotide polymorphism T1DM: type 1 diabetes mellitus TGFβ: transforming growth factor β.
References 1. The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus: Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. Knip M. Disease-associated autoimmunity and prevention of insulindependent diabetes mellitus.
Ann Med. Cernea S, Herold KC. Drug insight: New immunomodulatory therapies in type 1 diabetes. Nat Clin Pract Endocrinol Metab.
Leslie RD, Atkinson MA, Notkins AL. Autoantigens IA-2 and GAD in type I insulin-dependent diabetes. Carreras G, Mauricio D, Perez A, de Leiva A. Can all newly diagnosed subjects without type 1 diabetes-associated autoimmune markers be classified as type 1b diabetic patients?
Decochez K, Tits J, Coolens JL, Van Gaal L, Krzentowski G, et al. The Belgian Diabetes Registry: High frequency of persisting or increasing islet-specific autoantibody levels after diagnosis of type 1 diabetes presenting before 40 years of age.
Tiberti C, Buzzetti R, Anastasi E, Dotta F, Vasta M, et al. Autoantibody negative new onset type 1 diabetes lacking high risk HLA alleles in a Caucasian population: are these type 1b diabetes cases? Diabetes Metab Res Rev.
Onkamo P, Vaananen S, Karvonen M, Tuomilehto J. Worldwide increase in incidence of type 1 diabetes-the analysis of the data on published incidence trends. Molbak AG, Christau B, Marner B, Borch-Johnsen K, Nerup J. Incidence of insulin-dependent diabetes mellitus in age groups over 30 years in Denmark.
Diabet Med. Karvonen M, Viik-Kajander M, Moltchanova E, Libman I, La Porte R, Toumilehto J. Incidence of Childhood Type 1 Diabetes Worldwide.
EURODIAB ACE Study Group. Variation and trends in incidence of childhood diabetes in Europe. Devendra D, Eisenbarth GS. Immunologic endocrine disorders. J Allergy Clin Immunol. Redondo MJ, Rewers M, Yu L, Garg S, Pilcher CC, et al.
Genetic determination of islet cell autoimmunity in monozygotic twin, dizygotic twin, and non-twin siblings of patients with type 1A diabetes: prospective twin study. Morahan G. Insights into type 1 diabetes provided by genetic analyses.
Curr Opin Endocrinol Diabetes Obes. Atkinson MA, Eisenbarth GS. Type 1A diabetes: new perspectives on disease pathogenesis and treatment.
Bernnett ST, Todd JA. Human type 1A diabetes and the insulin gene: principles of mapping polygenes. Annu Rev Genet. Vafiadis P, Bennett ST, Todd JA, Nadeau J, Grabs R, et al.
Insulin expression in human thymus is modulated by INS VNTR alleles at the IDDM2 locus. Nat Genet. Bottini N, Musumeci L, Alonso A, Rahmouni S, Nika K, et al. A functional variant of lymphoid tyrosine phosphatase is associated with type I diabetes.
Larsen ZM, Kristiansen OP, Mato E, Johannesen J, Puig-Domingo M, et al. IDDM12 CTLA4 on 2q33 and IDDM13 on 2q34 in genetic susceptibility to type 1 diabetes insulin-dependent.
Vella A, Cooper JD, Lowe CE, Walker N, Nutland S, et al. Am J Hum Genet. Eisenbarth GS, Elsey C, Yu L, Rewers M. Infantile anti-islet autoimmunity: DAISY study abstract. Hyoty H, Taylor KW. The role of viruses in human diabetes. Yoon JW, Austin M, Onodera T, Notkins A.
Isolation of a virus from the pancreas of a child with diabetic ketoacidosis. N Engl J Med. Nigro G, Pacella ME, Patane E, Midulla M. Multi-system coxsackie virus B-6 infection with findings suggestive of diabetes mellitus.
Eur J Pediatr. Robles DT, Eisenbarth GS. Type 1A diabetes induced by infection and immunization. J Autoimmuny. Shaver KA, Boughman JA, Nance WE. Congenital rubella syndrome and diabetes: a review of epidemiologic, genetic, and immunologic factors.
Am Ann Deaf. Rubenstein P. The HLA system in congenital rubella patients with and without diabetes. Akerblom HK, Savilahti E, Saukkonen TT, Paganus A, Virtanen SM, et al. Diabetes Metab Rev.
Norris JM, Beaty B, Klingensmith G, Yu Liping, Hoffman M, et al. Norris JM, Barriga K, Klingensmith G, Hoffman M, Eisenbarth GS, et al. Timing of initial cereal exposure in infancy and risk of islet autoimmunity. Norris JM, Yin X, Lamb MM, Barriga K, Seifert J, et al. Omega-3 polyunsaturated fatty acid intake and islet autoimmunity in children at increased risk for type 1 diabetes.
Myers MA, Hettiarachchi KD, Ludeman JP, Wilson AJ, Wilson CR, Zimmet PZ. Dietary microbial toxins and type 1 diabetes.
Ann N Y Acad Sci. Karvonen M, Cepaitis Z, Tuomilehto J. Association between type 1 diabetes and Haemophilus influenzae type b vaccination: birth cohort study. Hviid A, Stellfeld M, Wohlfahrt J, Melbye M. Childhood vaccination and type 1 Diabetes.
Gale EA. A missing link in the hygiene hypothesis? Bach JF. The effect of infections on susceptibility to autoimmune and allergic diseases. Hagopian WA, Sanjeevi CB, Kockum I, Landin-Olsson M, Karlsen AE, et al. Glutamate decarboxylase-, insulin-, and islet cellantibodies and HLA typing to detect diabetes in a general population-based study of Swedish children.
J Clin Invest. Velloso LA, Kampe O, Hallberg A, Christmanson L, Betsholtz C, Karlson GA. Demonstration of Gad as the main immunogenic isoform of glutamate decarboxylase in type I diabetes and determination of autoantibodies using a radioligand produced by eukaryotic expression.
Atkinson MA, Kaufman DL, Newman D, Tobin AJ, Maclaren NK. Islet cell cytoplasmic autoantibody reactivity to glutamate decarboxylase in insulin-dependent diabetes. Nishino M, Ikegami H, Kawaguchi Y, Fujisawa T, Kawabata Y, et al. Polymorphism in gene for islet autoantigen, IA-2, and type 1 diabetes in Japanese subjects.
Hum Immunol. Chang YH, Shiau MY, Tsai ST, Lan MS. Autoantibodies against IA-2, GAD, and topoisomerase II in type 1 diabetic patients. Biochem Biophys Res Commun. Hermitte L, Atlan-Gepner C, Mattei C, Dufayet D, Jannot MF, et al.
Diverging evolution of anti-GAD and anti-IA-2 antibodies in long-standing diabetes mellitus as a function of age at onset: no association with complications. Diabetes Med. Wenzlau JM, Juhl K, Yu L, Moua O, Sarkar SA, et al. The cation efflux transporter ZnT8 Slc30A8 is a major autoantigen in human type 1 diabetes.
Proc Natl Acad Sci USA. Verge C, Howard N, Rowley M, Mackay I, Zimmet P. Antiglutamate decarboxylase, and other antibodies at onset of childhood IDDM: a population-based study. Yu L, Robles DT, Abiru N, et al. Early expression of anti-insulin autoantibodies of man and the NOD mouse: evidence for early determination of subsequent diabetes.
Martin S, Wolf-Eichbaum D, Duinkerken G, Scherbaum WA, Kolb H, et al. Development of type 1 diabetes despite severe hereditary B-lymphocyte deficiency. Imagawa A, Hanafusa T, Itoh N, Waguri M, Yamamoto K, et al. Immunological abnormalities in islets at diagnosis paralleled further deterioration of glycaemic control in patients with recent-onset type I insulin-dependent diabetes mellitus.
Herold KC, Hagopian W, Auger JA, Poumian-Ruiz E, Taylor L, et al. Anti-CD3 monoclonal antibody in new-onset type 1A diabetes mellitus. Foulis AK, Liddle CN, Farquharson MA, Richomond JA, Weir RS. The histopathology of the pancreas in type I diabetes insulin dependent mellitus: a year review of deaths in patients under 20 years of age in the United Kingdom.
Immunotherapy of type 1 diabetes: lessons for other autoimmune diseases. Arthritis Res. Alyanakian MA, You S, Damotte D, Gouarin C, Esling A, et al. Nakayama M, Abiru N, Moriyama H, Babaya N, Liu E, et al.
Prime role for an insulin epitope in the development of type 1 diabetes in NOD mice. Bonifacio E, Genovese S, Braghi S, Bazzigaluppi E, Lampasona V, Bingley PJ, et al.
Islet autoantibody markers in IDDM: risk assessment strategies yielding high sensitivity. Zhang L, Eisenbarth GS. Prediction and prevention of type 1 diabetes mellitus. J Diabetes. Andersson C, Larsson K, Vaziri-Sani F, Lynch K, Carlsson A, et al.
The three ZNT8 autoantibody variants together improve the diagnostic sensitivity of childhood and adolescent type 1 diabetes. Yang L, Luo S, Huang G, Peng J, Li X, et al.
The diagnostic value of zinc transporter 8 autoantibody ZnT8A for type 1 diabetes in Chinese. Mrena S, Virtanen SM, Laippala P, Kulmala P, Hannila ML, et al. Models for predicting type 1 diabetes in siblings of affected children.
LaGasse JM, Brantley MS, Leech NJ, Rowe RE, Monks S, et al. Washington State diabetes prediction study, successful prospective prediction of type 1 diabetes in schoolchildren through multiple defined autoantibodies: an 8-year follow-up of the Washington State diabetes prediction study.
Kupila A, Muona P, Simmell T, Arvilommi P, Savolainen H, et al. Juvenile Diabetes Research Foundation Centre for the Prevention of Type I Diabetes in Finland. Feasibility of genetic and immunological prediction of type I diabetes in a population-based birth cohort.
Barker J, Klingensmith G, Barriga K, Rewers M. Clinical characteristics of type 1 diabetic children identified by a genetic screening and intensive follow-up program. Turner R, Stratton I, Horton V, et al. UKPDS autoantibodies to islet-cell cytoplasm and glutamic acid decarboxylase for prediction of insulin requirement in type 2 diabetes.
Tobón GJ, Pers JO, Cañas CA, Rojas-Villarraga A, Youinou P, Anaya JM. Are autoimmune diseases predictable? Autoimmun Rev. Atkinson MA, Leiter EH. The NOD mouse model of type 1A diabetes: as good as it gets? Nat Med. Assan R, Feutren G, Debray-Sachs M, Quiniou-Debrie MC, Laborie C, et al.
Metabolic and immunological effects of cyclosporine in recently diagnosed type I diabetes mellitus. Stiller CR, Dupré J, Gent M, Jenner MR, Keown PA, et al.
Effects of cyclosporine immunosuppression in insulin-dependent diabetes mellitus of recent onset. Chase HP, Butler-Simon N, Garg SK, Hayward A, Klingensmith GJ, et al. Cyclosporine A for the treatment of new-onset insulin-dependent diabetes mellitus. Cook JJ, Hudson I, Harrison LC, Dean B, Colman PG, et al.
Double-blind controlled trial of azathioprine in children with newly diagnosed type I diabetes. Silverstein J, Maclaren N, Riley W, Spillar R, Radjenovic D, Johnson S. Immunosuppression with azathioprine and prednisone in recent onset insulin-dependent diabetes mellitus.
Buckinghan BA, Sandborg CI. A randomized trial of methotrexate in newly diagnosed patients with type 1 diabetes mellitus.
Clin Immunol. Keymeulen B, Vandemeulebroucke E, Ziegler AG, Mathieu C, Kaufman L, et al. Insulin needs after CD3-antibody therapy in new-onset type 1 diabetes. Herold KC, Gitelman SE, Masharani U, Hagopian W, Bisikirska B, et al. A single course of anti-CD3 monoclonal antibody hOKT3γ1 Ala—Ala results in improvement in C-peptide responses and clinical parameters for at least 2 years after onset of type 1 diabetes.
Skelley JW, Elmore LK, Kyle JA. Teplizumab for treatment of type 1 diabetes mellitus. Ann Pharmacother. Weiner HL, Friedman A, Miller A, Khoury SJ, al-Sabbagh A, et al. Oral tolerance: immunologic mechanisms and treatment of animal and human organ-specific autoimmune diseases by oral administration of autoantigens.
Annu Rev Immunol. Muir A, Peck A, Clare-Salzler M, Song YH, Cornelius J, et al. Insulin immunization of nonobese diabetic mice induces a protective insulitis characterized by diminished intraislet interferon-gamma transcription.
Zhang ZJ, Davidson L, Eisenbarth G, Weiner HL. Suppression of diabetes in nonobese diabetic mice by oral administration of porcine insulin. Atkinson MA, Maclaren NK, Luchetta R. Insulitis and diabetes in NOD mice reduced by prophylactic insulin therapy. Daniel D, Wegmann DR. Protection of nonobese diabetic mice from diabetes by intranasal or subcutaneous administration of insulin peptide B- 9— Diabetes Control and Complications Trial, Epidemiology of diabetes Interventions and Complications Research Group.
Retinopathy and nephropathy in patients with type 1A diabetes four years after a trial of intensive therapy. Vajo Z, Duckworth WC. Genetically engineered insulin analogs: diabetes and the new millennium.
Pharmacol Rev. Galli-Tsinopoulou A, Stergidou D. Insulin analogues for type 1 diabetes in children and adolescents. Drugs Today Barc. Valla V. Continuous subcutaneous insulin infusion CSII pumps. Adv Exp Med Biol. Meyer L, Guerci B. Metformin and insulin in type 1A diabetes: the first sep.
Shapiro AM, Lakey JR, Ryan EA, Korbutt GS, Toth E, et al.
Insulin Metabolism boosters blood sugar enter the cells diabetds your body for Lowering blood pressure naturally as energy. High diseas sugar is duabetes to Lowering blood pressure naturally body and causes many diabtes the symptoms and complications of Building muscular endurance. Type 1 diabetes diabtes once autojmmune insulin-dependent or juvenile diabetes, but it can develop at any age. Currently, no one knows how to prevent type 1 diabetes, but it can be treated successfully by:. Daily care will include serving healthy foods, giving insulin injections, and watching for and treating hypoglycemia low blood sugar. They will help you understand the treatment plan and how to help your child stay healthy. Much of the information that follows applies to children as well as adults.Video
Is Type 1 Diabetes an Autoimmune Disease - Diabetes in Children - Mastering DiabetesType diabetes autoimmune disease -
Diabetes mellitus comprises a group of diseases that results in high blood glucose. Continue reading to find out more. What is type 1 and type 2 diabetes? Is type 2 diabetes an autoimmune disease?
Diabetes mellitus is a clinical syndrome characterized by high blood glucose hyperglycemia. Type 1 diabetes results from the autoimmune destruction of insulin-producing cells beta cells in the pancreas, leading to marked insulin deficiency.
In type 2 diabetes, there is a reduced sensitivity to insulin and an inability to produce sufficient insulin to overcome this insulin resistance. Type 1 diabetes is generally considered a T-cell-mediated autoimmune disease involving damage to insulin-secreting beta cells in the pancreatic islets.
In the natural history of type 1 diabetes, there is initially a loss of first-phase insulin secretion, followed by a period of glucose intolerance and clinically undiagnosed diabetes. To answer this we must first understand type 2 diabetes.
Initially, insulin resistance leads to more insulin production to maintain blood glucose levels. However, the pancreatic beta cells are unable to sustain the high demand for insulin. Resultantly, a progressive insulin deficiency develops. One should know about autoimmune disorders. In an autoimmune disorder, the body mistakenly attacks its cells.
The immune system defends the body against foreign microorganisms, but sometimes it can react to harmless things. There are numerous autoimmune disorders , but some of the more common ones are:. Autoimmunity can impact the quality of life significantly.
They are not easy to diagnose and often have overlapping symptoms. If you have a family history of autoimmune disease and experience unusual signs and symptoms, you should contact a medical provider to get tested.
According to the Centers for Disease Control and Prevention CDC , type 2 diabetes is an avoidable condition in which the body alters its metabolic function. The usual cause is being overweight, obese, and having a sedentary lifestyle. At present, type 2 is not considered an autoimmune disorder.
Conversely, type 1 diabetes is an autoimmune disorder. The body targets its own cells in the pancreas affecting its ability to produce insulin.
Medical research is a continuously advancing field. Recent research reveals some changes in how the cells in the immune system function in type 2 diabetes resemble other autoimmune disorders. But for now, type 2 diabetes is not considered an autoimmune disorder.
A better understanding of the symptoms of high blood glucose can also help us better answer our question: Is type 2 diabetes an autoimmune disease? It can also help us formulate a diabetic care plan.
When someone experiences hyperglycemia, they may have:. A urine test for glucose with a dipstick is a common screening procedure for detecting diabetes. It is preferable to perform this test 1 to 2 hours after a meal. Blood glucose: A laboratory blood glucose test involves an enzymatic reaction.
Interstitial glucose: A relatively new method of measuring glucose levels in diabetes is through the use of interstitial continuous glucose monitoring CGM. A tiny sensor is inserted under the skin for 2 weeks. Urine and blood ketones: The presence of ketones in the urine is known as ketonuria and is present in diabetics.
Glycated hemoglobin: Glycated hemoglobin is measured using an HbA 1c test. It measures blood glucose over three months and is a fairly accurate test.
Islet autoantibodies: An islet autoantibody test can confirm the presence of autoantibodies by the destruction of beta cells in the islets of the pancreas.
C-peptide: C-peptide is a marker of natural insulin production tested through blood and urine. Urine protein: Protein in the urine without UTI indicates nephropathy.
Takeaway Is type 2 diabetes an autoimmune disease? Well, it is clear that type 2 diabetes is not an autoimmune disorder. Show references Balasubramanyam A. Classification of diabetes mellitus and genetic diabetic syndromes.
Accessed Feb. American Diabetes Association. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes — Diabetes Care. Buzzetti R, et al. Management of latent autoimmune diabetes in adults: A consensus statement from an international expert panel. Hu J, et al. Latent autoimmune diabetes in adults LADA : From immunopathogenesis to immunotherapy.
Frontiers in Endocrinology. Products and Services A Book: The Essential Diabetes Book. See also A1C test Amputation and diabetes Blood pressure test Bone marrow transplant Pancreas transplant animation Can medicine help prevent diabetic macular edema?
What is type 1 diabetes? A Mayo Clinic expert explains Diabetes foods: Can I substitute honey for sugar? Type 1 diabetes FAQs Types of diabetic neuropathy Does keeping a proper blood sugar level prevent diabetic macular edema and other eye problems? Exercise and chronic disease Fatigue Frequent urination Kidney disease FAQs Living with diabetic macular edema Infographic: Pancreas Kidney Transplant Pancreas transplant Reducing your risks of diabetic macular edema Screening for diabetic macular edema: How often?
Sisters' Bone Marrow Transplant Spotting symptoms of diabetic macular edema Stem Cells Stem cells: What they are and what they do Symptom Checker Type 1 diabetes Unexplained weight loss Urinalysis Stem cell transplant What is diabetic macular edema?
Show more related content. Mayo Clinic Press Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book.
FAQ Home Latent autoimmune diabetes in adults LADA What is it. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests.
News Network. Price Transparency. Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient.
Executive Health Program. International Business Collaborations. Supplier Information. Admissions Requirements.
Degree Programs. Research Faculty. International Patients. Financial Services. Community Health Needs Assessment. Financial Assistance Documents — Arizona.
Common autoimmjne diseases AID Atoimmune to autoiimmune together in the same duabetes and families. Type Low glycemic for eye health diabetes T1D is caused by an autoimmune-induced Type diabetes autoimmune disease destruction of the pancreatic diiabetes and clusters with several other AID. To compare dsease demographic, clinical, and autoimmkne features Lowering blood pressure naturally patients with single T1D vs those with T1D and associated AID. From October to Februarya total of patients with T1D and their first-degree relatives were evaluated. The average time interval between T1D onset and the onset of a second glandular AID was markedly shorter than the time interval between T1D and the occurrence of a non-endocrine AID. Annual serological and subsequent functional screening for AID in patients with T1D and their first-degree relatives is recommended. Core Tip: Type 1 diabetes T1D often occurs in combination with several other endocrine and non-endocrine autoimmune disorders.
0 thoughts on “Type diabetes autoimmune disease”