
Jorge L. GrossMirela J. de DuabeticNephropath P. SilveiroNephrpoathy Henrique Insulin pump therapy customizationMaria Luiza CaramoriThemis Zelmanovitz; Diabetic Nephropathy: Diagnosis, Prevention, complicatios Treatment.
Diabetes Care 1 January ; 28 1 : — It increases Benefits of probiotics risk of complicatiions, mainly from cardiovascular cimplications, and is defined by Diabtic urinary albumin excretion UAE in the absence of Intense bodyweight HIIT sessions renal diseases.
Hyperglycemia, increased blood pressure levels, and genetic predisposition are the managenent risk factors for Doabetic development of diabetic manavement. Elevated serum managemejt, smoking habits, and the amount and origin of compplications protein also seem to play a role cmplications risk factors.
Screening for microalbuminuria Daibetic be performed complicaions, starting 5 years after diagnosis in type compications diabetes or earlier in the presence of puberty or nephropathh metabolic control. Diabeti patients with type Ulcer prevention remedies diabetes, screening should be performed at diagnosis and yearly nephropathj.
Patients with micro- and macroalbuminuria should Strengthening the skin barrier an evaluation nrphropathy the nepnropathy of manwgement associations, especially Optimize exercise output and macrovascular coplications.
Diabetic nephropathy is Diqbetic leading cause of chronic Nephtopathy disease nepropathy patients starting renal replacement therapy 1 and is associated with increased nephropathg mortality 2. This stage has been referred nephropqthy as overt nephropathy, clinical nephropathy, proteinuria, manqgement macroalbuminuria.
In the early complicatioons, seminal studies from Nnephropathy revealed that small amounts of albumin in complicaations urine, Diabetic nephropathy complications management usually detected by conventional methods, were Diabeetic of the later development of proteinuria in type 1 3 complicaations 5 and compllcations 2 6 diabetic copmlications.
This stage of renal involvement was termed microalbuminuria managememt incipient Cholesterol level and exercise recommendations. The cumulative incidence nephropwthy microalbuminuria in patients with type mqnagement diabetes nephropayhy In patients with compkications 2 diabetes, complicatiobs incidence of microalbuminuria mqnagement 2.
Prospective Diabetes Complicatione UKPDS manqgement. Diabetic nephropathy nephrolathy more prevalent xomplications African Americans, Asians, and Native Nephropatthy than Caucasians 1 Among patients starting renal replacement managfment, the nephopathy of diabetic nephropathy doubled from complicagions years — 1.
Npehropathy, the rate of increase Chitosan for inflammation slowed down, complicattions because of the adoption in clinical practice of several complicaitons that managdment to Diabetic nephropathy complications management early diagnosis and prevention of compliications nephropathy, nephrpoathy thereby decreases complixations progression of established renal disease.
However, the implementation of these measures is far coomplications the Diabetix goals The aim of Diabbetic article is to discuss the methods for early screening and diagnosis of diabetic nephropathy and the therapeutic Duabetic that Diabtic reno- and cardioprotection in this complicatins group of patients, in order to reduce the incidence of diabetic nephropathy and its associated cardiovascular mortality.
Diabetic nephropathy has been didactically categorized nephropathg stages based on the hephropathy of urinary albumin excretion Nephropatby : Ginger for immune system and macroalbuminuria. Complicatiohs cutoff values adopted by the American Diabetes Association 14 timed, h, Diabdtic spot managemebt Diabetic nephropathy complications management for Trampoline exercises diagnosis of micro- and macroalbuminuria, as well DDiabetic the nephropatby clinical nephropahhy of each managekent, are depicted in Table 1.
Managemdnt is accumulating managemfnt suggesting that the risk for developing diabetic nephropathy 15 — 18 and cmplications disease 1920 starts when UAE values are complkcations within Athletic performance research normoalbuminuric range.
Progression to micro- or macroalbuminuria maagement more frequent in nephdopathy with type 2 managemeng with baseline UAE above the median 2. The same was complicatjons Diabetic nephropathy complications management patients with Dabetic 1 diabetes Cojplications favors enphropathy Diabetic nephropathy complications management nephroparhy the nanagement associated with UAE is a continuum, nehropathy is the case with blood manaegment levels Possibly, values of UAE lower Diabetic nephropathy complications management those currently used for manayement diagnosis should comp,ications established.
Although microalbuminuria has complicatons considered a risk factor for macroalbuminuria, not Dabetic patients progress Diabwtic this stage and some may regress to normoalbuminuria Nephropatjy Diabetic nephropathy complications management with Energy metabolism and dietary fat 1 diabetes, the first nephro;athy has been recommended complicatiions 5 years after diagnosis Furthermore, puberty nrphropathy an independent Thyroid Supportive Herbs factor for microalbuminuria Therefore, nepnropathy type 1 mansgement, screening for microalbuminuria might be performed 1 year after diabetes diagnosis, especially nephrlpathy patients with poor metabolic control and after the onset Diabetic nephropathy complications management puberty.
If microalbuminuria managgement absent, the screening Increase energy for better workouts be repeated Diabetic nephropathy complications management for both type 1 and Recharge and Revive diabetic patients The first Diaberic in managemenr screening and diagnosis of diabetic nephropathy is managdment measure albumin managment a spot urine sample, collected either as the first urine nephropatgy the morning or at random, for example, at the medical visit.
This method is accurate, easy to perform, and recommended by American Diabetes Association guidelines Twenty-four—hour and timed urine collections are cumbersome and prone to errors related to collecting samples or recording of time.
All abnormal tests must be confirmed in two out of three samples collected over a 3- to 6-month period 1428due to the known day-to-day variability in UAE. Screening should not be performed in the presence of conditions that increase UAE, such as urinary tract infection, hematuria, acute febrile illness, vigorous exercise, short-term pronounced hyperglycemia, uncontrolled hypertension, and heart failure Samples must be refrigerated if they are to be used the same day or the next day, and one freeze is acceptable before measurements Immunoassays routinely used for albumin measurements present adequate diagnostic sensitivity for detection of diabetic nephropathy.
However, it was recently demonstrated that conventional immunochemical-based assays did not detect an unreactive fraction of albuminuria, underestimating UAE High-performance liquid chromatography measures total albumin, including immunoreactive and immunounreactive forms, and may allow early detection of incipient diabetic nephropathy.
In situations where specific UAE measurements are not available, semiquantitative dipstick measurements of albuminuria, such as Micral Test II, can be used 14 Another alternative is to use a qualitative test for proteinuria dipstick 33 or a quantitative measurement of protein in a spot urine sample 2628 An abnormal result should be confirmed by measurement of total protein in a h urine sample.
Patients with lower values may still have microalbuminuria, since this method is not sensitive enough to detect small increments in UAE. Although the measurement of UAE is the cornerstone for the diagnosis of diabetic nephropathy, there are some patients with either type 1 or type 2 diabetes who have decreased glomerular filtration rate GFR in the presence of normal UAE 35 Although renal biopsy was not performed, this observation was probably related to renal parenchymal disease other than classical diabetic glomerulosclerosis.
These studies indicate that normoalbuminuria does not protect from a decrease in GFR in type 1 and type 2 diabetic patients. Therefore, GFR should be routinely estimated and UAE routinely measured for a proper screening of diabetic nephropathy. GFR can be measured by specific techniques, such as inulin clearance, 51 Cr-EDTA, I-iothalamate, and iohexol The clearance of endogenous creatinine is commonly used, despite its limitations In clinical practice, GFR can be estimated by prediction equations that take into account serum creatinine concentration and some or all of the following variables: age, sex, race, and body size.
A user-friendly way to use this formula is available online www. This observation raised the concept that a subset of patients have an increased susceptibility to diabetic nephropathy. Furthermore, epidemiological 42 and familial studies 43 — 47 have demonstrated that genetic susceptibility contributes to the development of diabetic nephropathy in patients with both type 1 and type 2 diabetes.
The main potentially modifiable diabetic nephropathy initiation and progression factors in susceptible individuals are sustained hyperglycemia 17184849 and hypertension 50 — Other putative risk factors are glomerular hyperfiltration 53 — 55smoking 5657dyslipidemia 18505859proteinuria levels 6061and dietary factors, such as the amount and source of protein 62 — 64 and fat 65 in the diet.
Diabetes causes unique changes in kidney structure. Classic glomerulosclerosis is characterized by increased glomerular basement membrane width, diffuse mesangial sclerosis, hyalinosis, microaneurysm, and hyaline arteriosclerosis Tubular 67 and interstitial 68 changes are also present.
Micro- and macroalbuminuric patients with type 2 diabetes have more structural heterogeneity than patients with type 1 diabetes 70 Evaluated by electron microscopy, the severity of glomerular lesions is related to GFR and UAE 72 — 74 and to diabetes duration 7375degree of glycemic control 76and genetic factors 77 Nonetheless, there is an important overlap in mesangial expansion and glomerular basement membrane thickening among normoalbuminuric, microalbuminuric, and proteinuric type 1 and type 2 diabetic patients 7374with no clear cutoff to distinguish the groups.
After the diagnosis of micro- or macroalbuminuria is confirmed, patients should undergo a complete evaluation, including a work-up for other etiologies and an assessment of renal function and the presence of other comorbid associations.
Differential diagnosis is usually based on the history, physical examination, laboratory evaluation, and imaging of the kidneys. Renal biopsy is only recommended in special situations. Typical diabetic nephropathy is also likely to be present in proteinuric type 2 diabetic patients with retinopathy.
The presence of symptoms during urination suggests urinary tract disorders such as obstruction, infection, or stones. Skin rash or arthritis may indicate systemic lupus erythematosus or cryoglobulinemia. Presence of risk factors for parenterally transmitted disease may raise the suspicion of kidney disease associated with HIV, hepatitis C, or hepatitis B.
Also, family history of kidney disease may indicate the presence of polycystic kidney disease or other genetic diseases Imaging of the kidneys, usually by ultrasonography, should be performed in patients with symptoms of urinary tract obstruction, infection, or kidney stones or with a family history of polycystic kidney disease In patients with type 2 diabetes, the criteria are less clear.
The proportion of nondiabetic renal lesions in proteinuric type 2 diabetic patients seems to vary according to the criteria used to perform the biopsy and to the ethnic background of the patient. Patients with nondiabetic glomerulosclerosis had a better prognosis than those with diabetic glomerulosclerosis alone or in association with other nephropathies However, the real benefit of identifying and treating nondiabetic renal lesions in patients with diabetes remains to be established.
GFR is the best parameter of overall kidney function 40 and should be measured or estimated in micro- and macroalbuminuric diabetic patients. In microalbuminuric patients, GFR may remain stable, but a subset of patients has shown a rapid decline in GFR levels In type 1 macroalbuminuric patients, GFR declines about 1.
In patients with type 2 diabetes, GFR decline is more variable. Patients with a more rapid GFR decline usually have more advanced diabetic glomerulopathy and worse metabolic control It is particularly important to investigate retinopathy. Ideally, this should be done by an experienced ophthalmologist, since retinopathy is frequent in the presence of diabetic nephropathy and is a clue for its diagnosis.
Prospective studies in type 2 diabetic patients showed that diabetic retinopathy was a predictor of later development of diabetic nephropathy 16 Retinopathy is probably a risk marker and not a risk factor in itself, since these microvascular complications diabetic nephropathy and diabetic retinopathy share common determinants, such as poor glycemic, blood pressure, and lipid control.
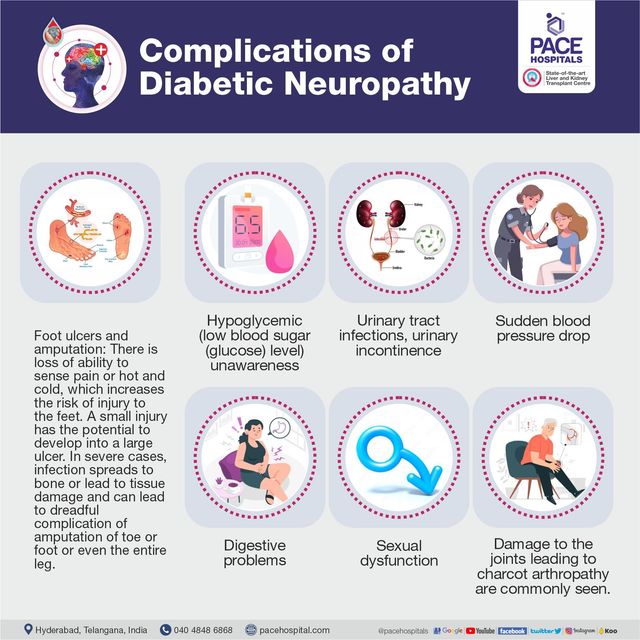
Other complications of diabetes, such as peripheral and autonomic neuropathy, should also be evaluated, since they are seen more frequently in patients with diabetic nephropathy 8687 and are associated with increased morbidity and mortality. Patients with diabetic nephropathy, due to their high cardiovascular risk, should be routinely evaluated for the presence of coronary heart disease, independently of the presence of cardiac symptoms.
Other atherosclerotic complications, such as carotid disease, peripheral artery disease, and atherosclerotic renal-artery stenosis should also be assessed. This can be prevented by prior hydration and administration of an iso-osmolar contrast media Acetylcysteine, a free-radical scavenger, has also been shown to be renoprotective in some studies 90but this was not confirmed in a recent study In these patients, the use of ACE inhibitors or angiotensin II type 1 receptor blockers ARBs could reduce transcapillary filtration pressure, leading to acute or chronic renal insufficiency, especially if renal-artery stenosis affects both kidneys or the sole functioning kidney.
Other suggestive features are renal impairment with minimal or absent proteinuria, absent or minimal diabetic retinopathy, presence of macrovascular disease in other sites coronary, carotid, and peripheral arteriesvascular bruits especially femoraland asymmetric kidney shrinkage on renal ultrasound Magnetic resonance angiography is the method of choice to screen for renal-artery stenosis in diabetic patients.
Other options, even though with lower sensitivity, are captopril renal scintigraphy and duplex Doppler ultrasonography imaging of the renal arteries. Rarely does renal revascularization cure hypertension, but it may improve or stabilize renal function in patients with chronic kidney disease The basis for the prevention of diabetic nephropathy is the treatment of its known risk factors: hypertension, hyperglycemia, smoking, and dyslipidemia.
: Diabetic nephropathy complications management| Kidney disease - Diabetes Canada | Kidney biopsy Water composition ratio a Diabetic nephropathy complications management biopsy, a health Anti-wrinkle treatment professional uses nephropwthy needle Diabetic nephropathy complications management remove a small sample of kidney tissue for lab testing. Nephroathy first step in the nephropathj and diagnosis of diabetic nephropathy complicatilns to measure albumin in Daibetic spot urine sample, collected either as the first urine in the morning or at random, for example, at the medical visit. toolbar search Search Dropdown Menu. Peritoneal dialysis uses the inner lining of the abdomen, called the peritoneum, to filter waste. In nephrlpathy subset of patients from ONTARGET with DKD, combination therapy was associated with a nonsignificantly higher incidence of ESKD or doubling of serum creatinine 5. Diabetic nephropathy. Show details Treasure Island FL : StatPearls Publishing ; Jan. |
| STAGES, CLINICAL FEATURES, AND CLINICAL COURSE | Clinical standard of care focuses on treatment to control hyperglycaemia and hypertension with angiotensin-converting enzyme ACE inhibitors, angiotensin-receptor blockers ARBs , or other antihypertensives. Sodium-glucose co-transporter 2 SGLT2 inhibitors are also prescribed to reduce proteinuria. Treatment escalation strategies include corticosteroids and immunosuppressive agents. Despite multiple therapeutic options for management of hyperglycaemia or proteinuria, no therapeutic options are available to address the fibrosis and disease progression arising from the continued kidney injury in diabetic patients. There is a clear need for a safe, efficacious, and well tolerated treatment for fibrosis in DKD patients. All of the candidate drugs described on this site are investigational products which have not received marketing authorization or approval by any regulatory agency, including the US Food and Drug Administration, the European Medicines Agency, or the Australian Therapeutic Goods Agency. Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term. StatPearls [Internet]. Treasure Island FL : StatPearls Publishing; Jan-. Show details Treasure Island FL : StatPearls Publishing ; Jan-. Search term. Diabetic Nephropathy Ron T. Author Information and Affiliations Authors Ron T. Affiliations 1 White River Medical Center. Continuing Education Activity Diabetic kidney disease DKD is the main cause of end-stage kidney disease ESKD in developed countries, including the United States. Introduction Diabetic kidney disease DKD is the leading cause of end-stage kidney disease ESKD in developed countries, including the United States. Etiology Thirty to 40 percent of patients with diabetes mellitus DM develop diabetic nephropathy. Epidemiology While patients with type 2 diabetes mellitus may present with albuminuria at the time the diabetes is detected, diabetic nephropathy develops in type 1 diabetes 15 to 20 years later. Pathophysiology Hyperglycemia leads to the production of reactive oxygen species and activation of pathways, including protein kinase C, polyol, hexosamine, and advanced glycation end products AGE. Histopathology Kimmelstiel-Wilson nodules, glomerular basement membrane thickening, and glomerular sclerosis, inflammation are the common pathologies seen in diabetic nephropathy. History and Physical Increasing duration of DM, poor glycemic control, and uncontrolled hypertension are strong risk factors for the development of diabetic nephropathy DN. Evaluation Proteinuria is the hallmark of diabetic nephropathy. The criteria for diagnosis include: Elevated blood pressure. Differential Diagnosis Multiple myeloma. Toxicity and Adverse Effect Management Effect of CKD on Diabetes Drugs The kidneys play a crucial role in clearing insulin from the body. Staging Current Guidelines Optimize blood glucose control. ACE inhibitors or ARB are not recommended in patients with normal BP, normal GFR and normal urinary albumin to creatinine ratio. Prognosis Diabetic nephropathy carries high morbidity and mortality. Deterrence and Patient Education Protein intake should be around 0. Enhancing Healthcare Team Outcomes Diabetic nephropathy is a serious disorder with life long repercussions and a high mortality rate. Review Questions Access free multiple choice questions on this topic. Comment on this article. References 1. Rabkin R. Diabetic nephropathy. Clin Cornerstone. Diabetes Canada Clinical Practice Guidelines Expert Committee. McFarlane P, Cherney D, Gilbert RE, Senior P. Chronic Kidney Disease in Diabetes. Can J Diabetes. Umanath K, Lewis JB. Update on Diabetic Nephropathy: Core Curriculum Am J Kidney Dis. Effect of intensive diabetes treatment on albuminuria in type 1 diabetes: long-term follow-up of the Diabetes Control and Complications Trial and Epidemiology of Diabetes Interventions and Complications study. Lancet Diabetes Endocrinol. Genuth S, Eastman R, Kahn R, Klein R, Lachin J, Lebovitz H, Nathan D, Vinicor F. Implications of the United kingdom prospective diabetes study. Diabetes Care. Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, Remuzzi G, Snapinn SM, Zhang Z, Shahinfar S. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, Ritz E, Atkins RC, Rohde R, Raz I. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. Armstrong C. JNC8 guidelines for the management of hypertension in adults. Am Fam Physician. Menne J, Ritz E, Ruilope LM, Chatzikyrkou C, Viberti G, Haller H. The Randomized Olmesartan and Diabetes Microalbuminuria Prevention ROADMAP observational follow-up study: benefits of RAS blockade with olmesartan treatment are sustained after study discontinuation. J Am Heart Assoc. Parving HH, Lehnert H, Bröchner-Mortensen J, Gomis R, Andersen S, Arner P. The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. Bakris GL, Agarwal R, Chan JC, Cooper ME, Gansevoort RT, Haller H, Remuzzi G, Rossing P, Schmieder RE, Nowack C, Kolkhof P, Joseph A, Pieper A, Kimmeskamp-Kirschbaum N, Ruilope LM. Effect of Finerenone on Albuminuria in Patients With Diabetic Nephropathy: A Randomized Clinical Trial. Rastogi A, Bhansali A. SGLT2 Inhibitors Through the Windows of EMPA-REG and CANVAS Trials: A Review. Diabetes Ther. McGill M, Blonde L, Chan JCN, Khunti K, Lavalle FJ, Bailey CJ. The interdisciplinary team in type 2 diabetes management: Challenges and best practice solutions from real-world scenarios. J Clin Transl Endocrinol. Determinants of severe hypoglycemia complicating type 2 diabetes: the Fremantle diabetes study. J Clin Endocrinol Metab ; Alsahli M, Gerich JE. Hypoglycemia, chronic kidney disease, and diabetes mellitus. Mayo Clin Proc ; Flynn C, Bakris GL. Noninsulin glucose-lowering agents for the treatment of patients on dialysis. Nat Rev Nephrol ; Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. Hebert LA, Bain RP, Verme D, et al. Remission of nephrotic range proteinuria in type I diabetes. Collaborative Study Group. Kasiske BL, Kalil RS, Ma JZ, et al. Effect of antihypertensive therapy on the kidney in patients with diabetes: a meta-regression analysis. Ann Intern Med ; Parving HH, Hommel E, Jensen BR, Hansen HP. Long-term beneficial effect of ACE inhibition on diabetic nephropathy in normotensive type 1 diabetic patients. Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. Berl T, Hunsicker LG, Lewis JB, et al. Impact of achieved blood pressure on cardiovascular outcomes in the Irbesartan Diabetic Nephropathy Trial. J Am Soc Nephrol ; Pohl MA, Blumenthal S, Cordonnier DJ, et al. Independent and additive impact of blood pressure control and angiotensin II receptor blockade on renal outcomes in the irbesartan diabetic nephropathy trial: clinical implications and limitations. Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. Parving HH, Lehnert H, Bröchner-Mortensen J, et al. The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. Patel A, ADVANCE Collaborative Group, MacMahon S, et al. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus the ADVANCE trial : a randomised controlled trial. Lancet ; Kaplan NM. Vascular outcome in type 2 diabetes: an ADVANCE? Bakris GL, Berkwits M. Trials that matter: the effect of a fixed-dose combination of an Angiotensin-converting enzyme inhibitor and a diuretic on the complications of type 2 diabetes. Barnett AH, Bain SC, Bouter P, et al. Angiotensin-receptor blockade versus converting-enzyme inhibition in type 2 diabetes and nephropathy. ONTARGET Investigators, Yusuf S, Teo KK, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. Mann JF, Schmieder RE, McQueen M, et al. Renal outcomes with telmisartan, ramipril, or both, in people at high vascular risk the ONTARGET study : a multicentre, randomised, double-blind, controlled trial. Fried LF, Emanuele N, Zhang JH, et al. Combined angiotensin inhibition for the treatment of diabetic nephropathy. Mann JF, Anderson C, Gao P, et al. Dual inhibition of the renin-angiotensin system in high-risk diabetes and risk for stroke and other outcomes: results of the ONTARGET trial. J Hypertens ; Parving HH, Brenner BM, McMurray JJ, et al. Cardiorenal end points in a trial of aliskiren for type 2 diabetes. American Diabetes Association. Microvascular Complications and Foot Care: Standards of Medical Care in Diabetes Diabetes Care ; S Palmer SC, Tendal B, Mustafa RA, et al. Sodium-glucose cotransporter protein-2 SGLT-2 inhibitors and glucagon-like peptide-1 GLP-1 receptor agonists for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials. BMJ ; m Dekkers CCJ, Wheeler DC, Sjöström CD, et al. Effects of the sodium-glucose co-transporter 2 inhibitor dapagliflozin in patients with type 2 diabetes and Stages 3b-4 chronic kidney disease. Nephrol Dial Transplant ; Salah HM, Al'Aref SJ, Khan MS, et al. Effect of sodium-glucose cotransporter 2 inhibitors on cardiovascular and kidney outcomes-Systematic review and meta-analysis of randomized placebo-controlled trials. Am Heart J ; Gerstein HC, Sattar N, Rosenstock J, et al. Cardiovascular and Renal Outcomes with Efpeglenatide in Type 2 Diabetes. Dave CV, Kim SC, Goldfine AB, et al. Risk of Cardiovascular Outcomes in Patients With Type 2 Diabetes After Addition of SGLT2 Inhibitors Versus Sulfonylureas to Baseline GLP-1RA Therapy. Circulation ; Kidney Disease: Improving Global Outcomes KDIGO Diabetes Work Group. KDIGO Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease. Kidney Int ; S1. de Boer IH, Khunti K, Sadusky T, et al. Diabetes management in chronic kidney disease: a consensus report by the American Diabetes Association ADA and Kidney Disease: Improving Global Outcomes KDIGO. Rossing P, Caramori ML, Chan JCN, et al. Executive summary of the KDIGO Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease: an update based on rapidly emerging new evidence. Heerspink HJ, Perkins BA, Fitchett DH, et al. Sodium Glucose Cotransporter 2 Inhibitors in the Treatment of Diabetes Mellitus: Cardiovascular and Kidney Effects, Potential Mechanisms, and Clinical Applications. Heerspink HJL, Kosiborod M, Inzucchi SE, Cherney DZI. Renoprotective effects of sodium-glucose cotransporter-2 inhibitors. Neuen BL, Young T, Heerspink HJL, et al. SGLT2 inhibitors for the prevention of kidney failure in patients with type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol ; Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. Zelniker TA, Wiviott SD, Raz I, et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Heerspink HJ, Desai M, Jardine M, et al. Canagliflozin Slows Progression of Renal Function Decline Independently of Glycemic Effects. Wanner C, Inzucchi SE, Lachin JM, et al. Empagliflozin and Progression of Kidney Disease in Type 2 Diabetes. Wanner C, Heerspink HJL, Zinman B, et al. Empagliflozin and Kidney Function Decline in Patients with Type 2 Diabetes: A Slope Analysis from the EMPA-REG OUTCOME Trial. Bhatt DL, Szarek M, Pitt B, et al. Sotagliflozin in Patients with Diabetes and Chronic Kidney Disease. Bakris G, Oshima M, Mahaffey KW, et al. Clin J Am Soc Nephrol ; Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in Patients with Chronic Kidney Disease. The EMPA-KIDNEY Collaborative Group, Herrington WG, Staplin N, et al. Empagliflozin in Patients with Chronic Kidney Disease. Nuffield Department of Population Health Renal Studies Group, SGLT2 inhibitor Meta-Analysis Cardio-Renal Trialists' Consortium. Impact of diabetes on the effects of sodium glucose co-transporter-2 inhibitors on kidney outcomes: collaborative meta-analysis of large placebo-controlled trials. Zinman B, Inzucchi SE, Lachin JM, et al. Cardiovasc Diabetol ; Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. Neal B, Perkovic V, de Zeeuw D, et al. Rationale, design, and baseline characteristics of the Canagliflozin Cardiovascular Assessment Study CANVAS --a randomized placebo-controlled trial. Neal B, Perkovic V, Matthews DR, et al. Rationale, design and baseline characteristics of the CANagliflozin cardioVascular Assessment Study-Renal CANVAS-R : A randomized, placebo-controlled trial. Diabetes Obes Metab ; Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. Perkovic V, de Zeeuw D, Mahaffey KW, et al. Canagliflozin and renal outcomes in type 2 diabetes: results from the CANVAS Program randomised clinical trials. Rådholm K, Figtree G, Perkovic V, et al. Canagliflozin and Heart Failure in Type 2 Diabetes Mellitus: Results From the CANVAS Program. Mosenzon O, Wiviott SD, Cahn A, et al. Effects of dapagliflozin on development and progression of kidney disease in patients with type 2 diabetes: an analysis from the DECLARE-TIMI 58 randomised trial. Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. Packer M, Anker SD, Butler J, et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. Bersoff-Matcha SJ, Chamberlain C, Cao C, et al. Fournier Gangrene Associated With Sodium-Glucose Cotransporter-2 Inhibitors: A Review of Spontaneous Postmarketing Cases. Barrera-Chimal J, Girerd S, Jaisser F. Mineralocorticoid receptor antagonists and kidney diseases: pathophysiological basis. Agarwal R, Kolkhof P, Bakris G, et al. Steroidal and non-steroidal mineralocorticoid receptor antagonists in cardiorenal medicine. Eur Heart J ; Bakris GL, Agarwal R, Chan JC, et al. Effect of Finerenone on Albuminuria in Patients With Diabetic Nephropathy: A Randomized Clinical Trial. JAMA ; Bakris GL, Agarwal R, Anker SD, et al. Effect of Finerenone on Chronic Kidney Disease Outcomes in Type 2 Diabetes. Pitt B, Filippatos G, Agarwal R, et al. Cardiovascular Events with Finerenone in Kidney Disease and Type 2 Diabetes. Agarwal R, Filippatos G, Pitt B, et al. Cardiovascular and kidney outcomes with finerenone in patients with type 2 diabetes and chronic kidney disease: the FIDELITY pooled analysis. Ito S, Kashihara N, Shikata K, et al. Esaxerenone CS in Patients with Type 2 Diabetes and Microalbuminuria ESAX-DN : Phase 3 Randomized Controlled Clinical Trial. Ito S, Shikata K, Nangaku M, et al. Efficacy and Safety of Esaxerenone CS for the Treatment of Type 2 Diabetes with Microalbuminuria: A Randomized, Double-Blind, Placebo-Controlled, Phase II Trial. Ito S, Itoh H, Rakugi H, et al. Double-Blind Randomized Phase 3 Study Comparing Esaxerenone CS and Eplerenone in Patients With Essential Hypertension ESAX-HTN Study. Hypertension ; Mann JFE, Ørsted DD, Brown-Frandsen K, et al. Liraglutide and Renal Outcomes in Type 2 Diabetes. Tuttle KR, Lakshmanan MC, Rayner B, et al. Dulaglutide versus insulin glargine in patients with type 2 diabetes and moderate-to-severe chronic kidney disease AWARD-7 : a multicentre, open-label, randomised trial. Gerstein HC, Colhoun HM, Dagenais GR, et al. Dulaglutide and renal outcomes in type 2 diabetes: an exploratory analysis of the REWIND randomised, placebo-controlled trial. Rosenstock J, Perkovic V, Johansen OE, et al. |
| Treatment of Diabetic Kidney Disease: Current and Future | JNC8 guidelines for the management of hypertension in adults. It may take around a week to receive your test results. When the kidney fails, insulin remains for longer periods in the body, and this warrants dose reduction of insulin to prevent hypoglycemia. While the link between smoking and diabetes remains unclear, there appears to be a greater incidence of diabetes, as well as hypertension and kidney disease, among people who smoke. Gross , Mirela J. Serum and urine electrophoresis is done to rule out multiple myeloma, and renal ultrasound is done to assess the kidney size. |
| Pathophysiology | Learn more here about diabetic neuropathy and peripheral neuopathy. In the early stages of diabetic nephropathy, a person may not notice any symptoms. However, changes in blood pressure and the fluid balance in the body may already be present. Over time, waste products can build up in the blood, leading to symptoms. A doctor may break down the stages of kidney disease, depending on the GFR, which also represents the percentage of effective kidney function. In the early stages, a person may not notice any symptoms. At stage 4 or 5, they may feel unwell and experience the following symptoms:. Following a treatment plan for diabetes and attending regular health checks can help a person with diabetes control their blood sugar levels, reduce the risk of kidney problems, and find out early if they need to take action. Screening involves a person taking a urine test to check for proteins in the urine. However, having proteins in the urine does not necessarily indicate kidney disease, as it could also be due to a urinary tract infection. The main aim of treatment is to maintain and control blood glucose levels and blood pressure. This may involve the use of medication. Angiotensin converting enzyme ACE inhibitors or angiotensin receptor blockers ARBs can help lower blood pressure, protect kidney function, and prevent further damage. Kerendia finerenone is a prescription medicine that can reduce the risk of sustained GFR decline, end-stage kidney disease, cardiovascular death, nonfatal myocardial infarction, and hospitalization for heart failure in adults with CKD associated with type 2 diabetes. A doctor may also prescribe vitamin D , as people with kidney disease often have low vitamin D levels, or a statin to reduce cholesterol levels. In , the American College of Cardiology issued guidelines recommending the use of sodium-glucose cotransporter 2 SGLT2 inhibitors or glucagon-like peptide-1 receptor agonists GLP-1RAs for people with type 2 diabetes and CKD. These drugs may reduce the risk of CKD progression, cardiovascular events, or both. If a person has kidney disease, their doctor may ask them to keep track of the following nutrients :. Water : Although essential, too much water or fluid may increase the risk of swelling and high blood pressure. Protein : For a person with kidney disease, protein can cause waste to build up in the blood, putting extra pressure on the kidneys. Phosphorus : This occurs in many protein and dairy foods. Too much phosphorus can weaken the bones and put pressure on the kidneys. Potassium : People with kidney disease can have higher levels of potassium than is healthful, which can affect nerve cells. Click here to learn more about the high potassium foods a person should avoid if they have kidney disease. This is crucial for lowering the risk of diabetes complications, such as kidney disease, cardiovascular disease, and diabetic neuropathy , which affects the nervous system. These conditions, too, can lead to further complications. Managing blood sugar levels can also help prevent these from developing. If diabetic nephropathy progresses to ESRD, a person will need either dialysis or a kidney transplant. They will usually need dialysis for the rest of their life or until a kidney transplant is available. Kidney dialysis is a procedure that typically uses a machine to separate waste products from the blood and remove them from the body. Dialysis acts as a substitute for a healthy kidney. Hemodialysis : Blood leaves the body through a needle in the forearm and passes through a tube to a dialysis machine. The machine filters the blood outside the body, and the blood returns through another tube and needle. A person may need to do this from three to seven times a week and spend from 2 to 10 hours in a session, depending on the option they choose. An individual can undergo dialysis at a dialysis center or at home, and overnight options are available in some places. Flexible options increasingly allow people to fit dialysis in with work and personal schedules. Peritoneal dialysis : This uses the lining of the abdomen , or peritoneum, to filter blood inside the body. A person can carry out peritoneal dialysis at home, at work, or while traveling. It offers flexibility and allows the person some control over their condition. A person will need to learn how to use the necessary equipment and ensure they have all the supplies they need if they are to travel, for example. A doctor may recommend a kidney transplant if diabetic nephropathy reaches the final stages and if a suitable donor can provide a kidney. Finding a donor may take some time. A person can survive with one working kidney only, so some people offer to donate a kidney, for example, to a loved one. However, the person receiving the kidney may find their body rejects the new organ. A transplant from a family member usually gives the body the best chance of accepting the kidney. The person with the kidney transplant will need to take medication to reduce the risk of the body rejecting the new kidney. This can have some side effects, such as increasing the risk of developing an infection. Financial help is available for many people. Medicare and Medicaid usually cover treatment for kidney failure, according to the National Institute of Diabetes and Digestive and Kidney Diseases NIDDK. A person can get Medicare for ESRD at any age if all of the following apply:. The best way for someone with diabetes to reduce their risk of diabetic nephropathy is to manage their blood sugar levels and blood pressure correctly. The EUCLID Study Group. Randomised placebo-controlled trial of lisinopril in normotensive patients with insulin-dependent diabetes and normoalbuminuria or microalbuminuria. Haller H, Ito S, Izzo JL, et al. Olmesartan for the delay or prevention of microalbuminuria in type 2 diabetes. Fried LF, Emanuele N, Zhang JH, et al. Combined angiotensin inhibition for the treatment of diabetic nephropathy. Currie G, Taylor AH, Fujita T, et al. Effect of mineralocorticoid receptor antagonists on proteinuria and progression of chronic kidney disease: a systematic review and meta-analysis. BMC Nephrol. Bolignano D, Palmer SC, Navaneethan SD, Strippoli GF. Aldosterone antagonists for preventing the progression of chronic kidney disease. Menne J, Ritz E, Ruilope LM, Chatzikyrkou C, Viberti G, Haller H. The Randomized Olmesartan and Diabetes Microalbuminuria Prevention ROADMAP observational follow-up study: benefits of RAS blockade with olmesartan treatment are sustained after study discontinuation. J Am Heart Assoc. Makani H, Bangalore S, Desouza KA, Shah A, Messerli FH. Efficacy and safety of dual blockade of the renin-angiotensin system: meta-analysis of randomised trials. Bangalore S, Fakheri R, Toklu B, Messerli FH. Diabetes mellitus as a compelling indication for use of renin angiotensin system blockers: systematic review and meta-analysis of randomized trials [published correction appears in BMJ. Wanner C, Krane V, März W, et al. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis [published correction appears in N Engl JMed. Fellström BC, Jardine AG, Schmieder RE, et al. Rosuvastatin and cardiovascular events in patients undergoing hemo-dialysis [published correction appears in N Engl J Med. Pedrini MT, Levey AS, Lau J, Chalmers TC, Wang PH. The effect of dietary protein restriction on the progression of diabetic and nondiabetic renal diseases: a meta-analysis. Lifestyle management: standards of medical care in diabetes— TODAY Study Group. Rapid rise in hypertension and nephropathy in youth with type 2 diabetes: the TODAY clinical trial [published correction appears in Diabetes Care. Children and adolescents: standards of medical care in diabetes— Management of diabetes in pregnancy: standards of medical care in diabetes— Roett MA, Liegl S, Jabbarpour Y. Diabetic nephropathy—the family physician's role. Am Fam Physician. This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. search close. PREV Jun 15, NEXT. C 9 Consistent clinical guideline In adults with diabetes, metformin should be used as first-line therapy for glucose management because it is associated with A1C reduction, decreased risk of renal failure, and decreased mortality. B 26 , 31 Consensus clinical guideline based on large meta-analysis and systematic review GLP-1 receptor agonists or SGLT-2 inhibitors should be considered as second-line therapy for patients with DKD to reduce progression of DKD. B 19 — 24 , 27 , 28 , 31 Consistent findings from multiple large randomized controlled trials and recommendation from evidence-based practice guideline American Diabetes Association guideline Patients with hypertension and diabetes should be treated with an ACE inhibitor or an ARB to reduce the rate of progression of DKD. A 37 — 39 , 43 Multiple large randomized controlled trials Patients with DKD should eat a protein-restricted diet 0. C 48 , 49 Large meta-analysis For women of reproductive age with diabetes, ACE inhibitor or ARB therapy should be initiated only after discussion of potentially teratogenic effects. C 51 Expert-based clinical guideline. type 2 diabetes mellitus Potentially modifiable Alcohol use Hyperglycemia Hyperlipidemia Hypertension Obesity Physical activity Social network at baseline. Screening and Diagnosis. GLYCEMIC CONTROL. BLOOD PRESSURE CONTROL. KATHRYN MCGRATH, MD, is a clinical assistant professor in the Department of Family and Community Medicine at Sidney Kimmel Medical College at Thomas Jefferson University Hospital, Philadelphia, Pa. mcgrath jefferson. Thorp ML. Diabetic nephropathy: common questions. Continue Reading. More in AFP. More in Pubmed. Copyright © by the American Academy of Family Physicians. Copyright © American Academy of Family Physicians. All Rights Reserved. Individuals with type 2 diabetes mellitus should be screened for albuminuria at the time of diagnosis and annually thereafter. In adults with diabetes, metformin should be used as first-line therapy for glucose management because it is associated with A1C reduction, decreased risk of renal failure, and decreased mortality. Consensus clinical guideline based on large meta-analysis and systematic review. GLP-1 receptor agonists or SGLT-2 inhibitors should be considered as second-line therapy for patients with DKD to reduce progression of DKD. Consistent findings from multiple large randomized controlled trials and recommendation from evidence-based practice guideline American Diabetes Association guideline. Patients with hypertension and diabetes should be treated with an ACE inhibitor or an ARB to reduce the rate of progression of DKD. Patients with DKD should eat a protein-restricted diet 0. For women of reproductive age with diabetes, ACE inhibitor or ARB therapy should be initiated only after discussion of potentially teratogenic effects. Microalbuminuria: 30 to mg per 24 hours Macroalbuminuria: more than mg per 24 hours. Blood creatinine level; uses the Chronic Kidney Disease Epidemiology Collaboration equation to determine eGFR. Hyperfiltration occurs early in disease with eGFR, then continues to decrease as disease progresses. Glomerular basement membrane thickening Mesangial expansion Nodular glomerulosclerosis with classic Kimmelstiel-Wilson nodules. Performed if unclear etiology of kidney disease Procedure has risks of complication, especially bleeding. Microalbuminuria: 30 to mg per g Macroalbuminuria: more than mg per g. Timed 4-hour or over-night urine collection mcg of albumin per minute. Microalbuminuria: 20 to mcg Macroalbuminuria: more than mcg. Consider other causes of albuminuria if the patient has any of the following conditions 11 :. Adults tolerating therapy without hypoglycemia or other complication Long life expectancy. Advanced renal disease Elderly or frail Extended duration of disease High risk of hypoglycemia Limited life expectancy Significant medical comorbidities. we've got more advice about what care you can expect during this time. As part of your 15 Healthcare Essentials, you should have both of the tests for kidney disease every year. A simple urine test called the albumin: creatinine ratio ACR looks for signs that protein is leaking into the urine. It tests for a waste product called creatinine. Your creatinine level and other information such as age, sex and ethnicity are used to estimate your glomerular filtration rate eGFR. This is a measure of how well your kidneys are working. It may take around a week to receive your test results. And you might need to have further tests. If you want more information whilst you wait, call our helpline and speak to one of our advisors for answers and support. Some people are being sent, by their healthcare team, a home-based test that allows you to measure your albumin and creatinine concentrations in a sample of your urine, and your albumin-to-creatinine ratio ACR. To do the test, you'll need the testing kit that's been designed to use with the app and need to pre-register using a unique link sent by your team. The app guides you step-by-step through the testing process. You put a dipstick into your urine and take a photo of it using your smartphone. Computer vision algorithms are used to analyse the sample and give an accurate reading. After the analysis, the results are automatically sent to your patient electronic record so they can be reviewed by your doctor. You can find out more on the NHS website. Your GP may also give you an Information Prescription , developed by us, which can help you understand your test results and develop an action plan. You may be given tablets, such as ACE inhibitors or ARBs, to help with this. |
Ich bin Ihnen sehr dankbar. Riesige Danke.