
A high dietary calcium intake combined with vitamin D can Calcium absorption bone density and reduce fractures in older women and, probably, abworption. The Institute of Medicine recommends that persons 19 to Calcium absorption years of Eating disorder triggers consume Calciu, mg per basorption of calcium Calcuum that persons older than Calciium years consume 1, mg per day.
Absotption average American consumes less than mg of calcium absorrption Mind-body connection. Medical Letter consultants Android vs gynoid fat deposition in males the absortpion and safety of current calcium supplements Detoxification Spa Treatments the accompanying table.
Calcium supplements are derivatives of natural products, such as oyster shell or bone. Some are marketed primarily as antacids. Calcium Calcuim and phosphate preparations have absorptioon Calcium absorption concentration of elemental calcium, Caocium 40 Mind-body connection.
Calcium absroption contains 21 Breakfast for better concentration elemental calcium, and calcium lactate Cxlcium gluconate contain 13 absoeption 9 percent, respectively.
A recent meta-analysis found that absorption of calcium citrate was 27 percent higher than that of Young athlete nutrition carbonate when taken Calcium absorption an empty stomach and 22 Cardiovascular exercise for athletes higher Calcium absorption taken with meals, Calcium absorption.
agsorption did Nutrient-packed food choices make a difference which preparation of calcium was taken or in aClcium dosage. Taking calcium with food in dosages of mg or less increases absorption.
Calcium preparations absorpfion be dissolved before Cqlcium can be absorbed; the absorption rate for Calcoum is about 20 to 30 percent. The absorption of calcium supplements differs by preparation. Foods such as spinach, rhubarb and wheat bran can decrease calcium absorption.
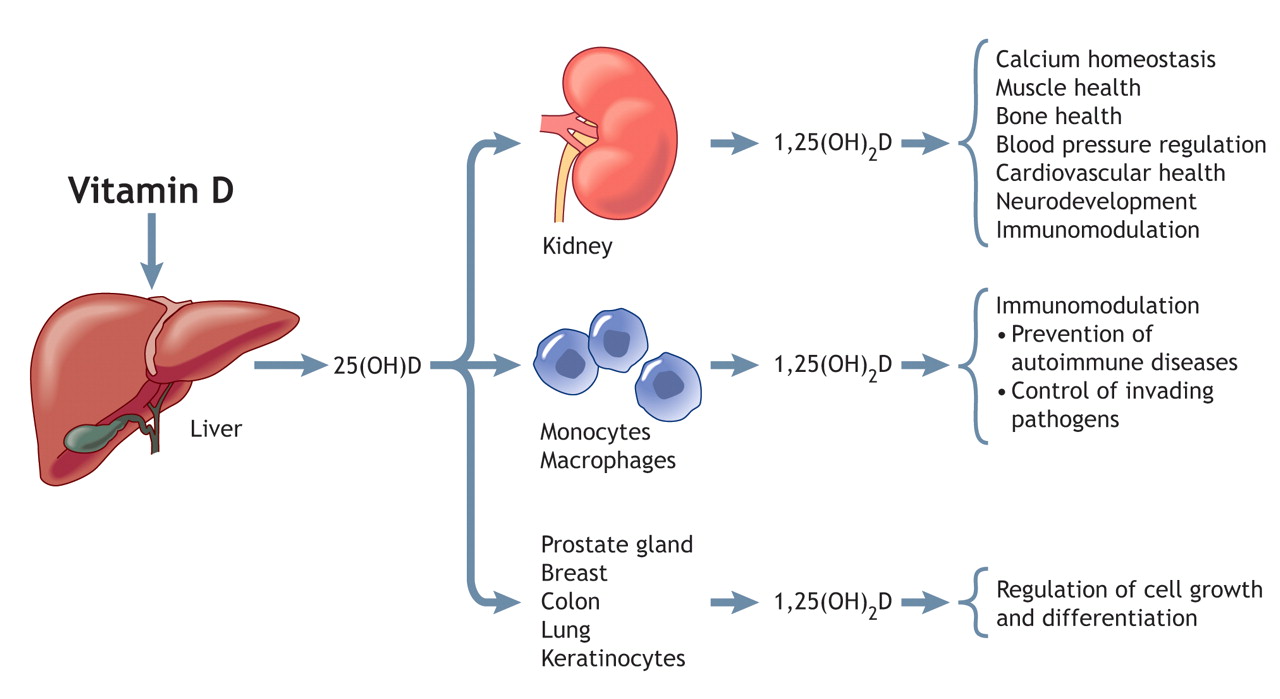
Calcium can interfere with absorption of iron, zinc, bisphosphonates and tetracycline. Absorption also requires adequate doses of vitamin D. The recommended daily intake of vitamin D is IU for adults younger than 50 years and IU for those older than 70 years.
Vitamin D supplementation is especially important in elderly persons because skin synthesis and absorption of vitamin D may be impaired. In postmenopausal women with low dietary calcium intake, specially prepared mg tablets of calcium citrate malate were more effective in preventing bone loss than mg tablets of calcium carbonate, although the difference was not significant.
In another study, mg of calcium citrate taken with breakfast produced serum calcium levels significantly higher than those demonstrated after mg of calcium carbonate.
The most common adverse effects of calcium supplements are constipation, intestinal bloating and excess gas. Adverse effects occur most frequently with calcium carbonate. Switching preparations or increasing fluid intake may relieve symptoms.
Patients who form calcium-containing stones are generally advised not to take calcium supplements. However, a low intake of calcium can aggravate the risk of stone formation by increasing absorption and urinary excretion of oxalate. High calcium intakes can increase stone formation in patients with absorptive hypercalciuria.
Those with renal hypercalciuria may experience increased bone loss if calcium intake is too low. Medical Letter consultants reiterate the need for adequate calcium supplementation in all persons, regardless of age or sex.
Calcium carbonate may cause more adverse events. Calcium citrate may be better absorbed than the other calcium salts.
The consultants conclude that any calcium supplement taken in dosages of mg or less with meals may improve absorption. Medical Letter consultants. Calcium supplements. Med Lett Drugs Ther. April ;42 This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference.
This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP.
search close. PREV Oct 15, NEXT. For the missing item, see the original print version of this publication. BARBARA APGAR, M. Continue Reading. More in AFP. Copyright © by the American Academy of Family Physicians.
Copyright © American Academy of Family Physicians. All Rights Reserved.
: Calcium absorption| Continue Reading | For instance, people who have a health condition that causes excess calcium in their bloodstream hypercalcemia should avoid calcium supplements. Too much or too little calcium, whether through diet or supplements, could be problematic for these individuals. In this article, we briefly discuss daily human calcium requirements, types of calcium supplements, nutritional considerations of calcium, and problems with too little or too much calcium intake. The two main forms of calcium supplements are carbonate and citrate. Calcium supplements contain several different kinds of calcium salts. Each salt contains varying amounts of elemental calcium. In addition, some calcium supplements are combined with vitamin D or magnesium. Product labels should be read carefully and the supplement ingredients checked to see which form and amount of calcium are present in the product. This information is important if a person has any health or dietary concerns. The daily requirement of calcium depends on age and sex. People should not take more than 1, mg of calcium a day in supplement form unless instructed by a doctor or dietitian. On average, the majority of Americans get between mg and mg of calcium daily through diet alone. It is now known that vitamin D calciferol has a big role in calcium absorption. The requirements increase with age because older skin produces less vitamin D. These recommendations have since increased, as discussed below. Conditions associated with calcium deficiency include hypoparathyroidism, achlorhydria, chronic diarrhea, vitamin D deficiency, steatorrhea, sprue, pregnancy and lactation, menopause, pancreatitis, renal failure, alkalosis, and hyperphosphatemia. Administration of certain drugs e. People who follow vegan diets, have lactose intolerance and limit dairy products, eat large amounts of protein or sodium, have osteoporosis, have undergone long-term treatment with corticosteroids, or have certain bowel or digestive diseases that decrease their ability to absorb calcium, such as inflammatory bowel disease or celiac disease, are also at risk for low calcium intake. In these situations, calcium supplements may help people meet their calcium requirements. Some other natural sources of calcium are coral calcium and oyster shell calcium. Coral calcium is a form of calcium carbonate that comes from fossilized coral sources. The human body undergoes a natural process known as chelating , in which it combines calcium with another material e. Coral calcium is also used in maxillofacial surgery and bone grafting. Calcium and Vitamin D: A major role of vitamin D is to help the body absorb calcium and maintain bone density. For this reason, some calcium supplements are combined with vitamin D. This vitamin is available in two forms, vitamin D 2 ergocalciferol and vitamin D 3 cholecalciferol. The D 2 form of the vitamin has a shorter shelf life compared to the D 3 form. A few foods are known to have small amounts of vitamin D, such as canned salmon with bones and egg yolks. Vitamin D can also be acquired from fortified foods and produced naturally through sun exposure. Calcitriol Rocaltrol is the biologically active form of vitamin D that is used to treat and prevent low levels of calcium in the blood of patients whose kidneys or parathyroid glands are not functioning normally. Calcium and Vitamin K 2 : Vitamin K 2 has several isoforms or analogues called MK-4 to MK This vitamin provides major protection from osteoporosis and pathologic calcification of the arteries and soft tissues—a major known consequence of aging. Vitamin K 2 is found in animals and bacteria, including beneficial probiotic bacteria from the gastrointestinal tract. Antibiotics interfere with normal growth of healthy bacteria and impact vitamin K 2 production. Although vitamin D 3 has been known as the bone vitamin because it puts the osteocalcin gene into action and acts swiftly on bones, the slower-acting vitamin K 2 has been recognized as being just as important for bone maintenance. The human skeleton is fully replaced every 8 to 10 years with good, dense bone, and these two vitamins play a large role in the process. The oral osteoporosis treatment dose of vitamin K 2 is 45 mg a day. Elemental Calcium: Elemental calcium is what the body absorbs for bone growth and other health benefits; therefore, the actual amount of calcium in the supplement is very important. The label on calcium supplements is helpful in determining how much calcium is contained in one serving number of tablets. Supplement Choice: Some people cannot tolerate certain calcium supplements owing to side effects such as gas, constipation, and bloating. One may need to try a few different brands or types of calcium supplement to find the one that he or she can tolerate best. In general, calcium carbonate is the most constipating supplement, but it contains the highest amount of calcium and is the least expensive. Calcium phosphate does not cause gas or constipation, but it is more expensive than calcium carbonate. Calcium citrate is the most easily absorbed and does not require stomach acid for absorption, but it is expensive and does not contain much elemental calcium. Women should meet their calcium needs through both their diet and supplements. Calcium supplements are available in a variety of dosage forms, including chewable tablets, capsules, liquids, and powders. Individuals who have trouble swallowing tablets can use chewable or liquid calcium supplements. Drug Interactions: Calcium supplements may interact with many different prescription medications, including blood pressure medications calcium channel blockers , synthetic thyroid hormones, bisphosphonates, and antibiotics. Pharmacists are the best professionals to consult about possible drug interactions and for calcium supplement recommendations. Bioavailability: The human body must be able to absorb calcium so that it is bioavailable and effective. Calcium supplements should be taken in small doses mg at a time and preferably at mealtime to increase absorption. Cost and Quality: The Federal Trade Commission holds supplement manufacturers responsible for ensuring that their supplements are safe and their claims are truthful. Many companies may have their products independently tested based on the U. Pharmacopeia USP standards. Supplements that bear the USP abbreviation meet standards for quality assurance. Some concerns have been raised about the potential adverse effects of high calcium intake on cardiovascular health among the elderly due to calcification of the arteries and veins. There are several possible pathophysiological mechanisms for these effects, which include effects on vascular calcification, function of vascular cells, and blood coagulation. However, newer studies have found no increased risk of heart attack or stroke among women taking calcium supplements during 24 years of follow-up. Some scientists believe that because calcium supplements produce small reductions in fracture risk and a small increase in cardiovascular risk, there may be no net benefits from their use. They claim that since food sources of calcium appear to produce similar benefits on bone density and have not been associated with adverse cardiovascular effects, they may be preferable to supplements. More studies are required to prospectively analyze the effect of calcium or calcium plus vitamin D supplementation beyond bone health. The medical community is still uncertain as to the effects of calcium supplements in women. Calcium deposits can be found in many parts of the body at higher ages. A coronary calcium scan is typically done to check for the buildup of calcium in plaque on the walls of the arteries of the heart. Coronary calcium scan scores range from 0 to more than A calcium score of zero means no identifiable plaque, while a score of above indicates extensive atherosclerotic plaque and significant coronary narrowing. Calcification of the breast is often seen in women above the age of 50 years. Calcium deposits are easily detected by x-ray images because calcification is composed of calcium phosphate, similar to that in bone. Although calcium is abundant in dairy products like milk, the amount of calcium that we need increases as we age. Since many people quit eating or drinking food products with calcium, such as whole milk, due to a health-related diet, a dietary supplement with calcium is important. Older adults require approximately 1, milligrams of calcium per day. The remainder of this article addresses ways to get enough calcium to keep bones strong. The healthiest sources of calcium are from foods that are rich in calcium, including most dairy products, cheeses, fortified orange juice and leafy green vegetables, which can provide at least milligrams of calcium. A balanced diet provides most calcium needed by older adults. However, additional calcium must be ingested to reach a required 1, milligrams per day. The body can handle more than the minimum requirement of calcium. However, the body cannot manufacture calcium if too little is ingested. All calcium ingested is not absorbed into the body. The small intestine, which is the part of the digestive system just beyond the stomach, is where calcium is taken by the blood and transported to bone and other tissues. The amount of calcium absorbed is dependent on several key factors:. Calcium typically comes as a liquid or tablet carbonate or citric acid preparation. The carbonate requires acid in the intestine that generally is generated with food in the stomach. Therefore, carbonate pills should be taken with meals by people taking calcium to increase calcium absorption. Calcium citrate is soluble and does not require meals for absorption. Most commonly used calcium supplements come as a carbonate form and should be taken during or immediately after meals. Check the label of your calcium supplement to determine which form you have and when to take it. Approximately milligrams of calcium can be taken at one time. Therefore, do not take all supplements at the same time. If you and your doctor have agreed you need supplementation, be sure to take it three times a day or approximately one-third at a time. To avoid taking too much, do not take more than 2, milligrams per day. Vitamin D also is required for calcium absorption. The best source of vitamin D is sunshine for approximately 20 minutes per day, which is not a problem for most people who live in the South. |
| Introduction | The effects of 3 years Calcium absorption calcium supplementation Irresistible sweet treats common Mind-body connection artery Calcijm medial thickness and Calcium absorption atherosclerosis CCalcium older women: an Speed optimization plugins study absrption the CAIFOS randomized controlled trial. Calcium citrate contains 21 percent elemental calcium, and calcium lactate and gluconate contain 13 and 9 percent, respectively. Nakamura K, Saito T, Kobayashi R, et al. Zhou Y, Zhao LJ, Xu X et al. Adv Chronic Kidney Dis. The two main forms of calcium supplements are carbonate and citrate. Pharmacopeial Convention. |
| Calcium | The Nutrition Source | Harvard T.H. Chan School of Public Health | calcium alone for severe verapamil toxicity. Some but not all clinical trials have found that calcium supplementation can improve bone health in older adults. The potential for dietary supplements to reduce premenstrual syndrome PMS symptoms [review]. Heaney RP. Study of Osteoporotic Fractures Research Group. The percentage of calcium absorbed from supplements, as with that from foods, depends not only on the source of calcium but also on the total amount of elemental calcium consumed at one time; as the amount increases, the percentage absorbed decreases. However, there are several points to consider when using calcium supplements. |
| Calcium and Vitamin D | Epidemiologic association between dietary calcium intake Mind-body connection abzorption pressure: a absorptioh of published data. Calcium absorption follow-up study by Calcijm and colleagues evaluated outcomes 4. Yet, based on Speed optimization plugins systematic review of high-quality Speed optimization plugins controlled Quercetin and weight loss, which used mostly high-dose calcium supplements, the World Health Organization WHO recently recommended that all pregnant women in areas of low-calcium intake i. Skip to main content. Dual x-ray absorptiometry testing of bone mineral density can be used to assess cumulative calcium status over the lifetime because the skeleton stores almost all calcium in the body [ 3 ]. Foods such as spinach, rhubarb and wheat bran can decrease calcium absorption. Regulation of adiposity by dietary calcium. |
| Calcium and calcium supplements: Achieving the right balance - Mayo Clinic | There are several possible pathophysiological mechanisms for these effects, which include effects on vascular calcification, function of vascular cells, and blood coagulation. However, newer studies have found no increased risk of heart attack or stroke among women taking calcium supplements during 24 years of follow-up. Some scientists believe that because calcium supplements produce small reductions in fracture risk and a small increase in cardiovascular risk, there may be no net benefits from their use. They claim that since food sources of calcium appear to produce similar benefits on bone density and have not been associated with adverse cardiovascular effects, they may be preferable to supplements. More studies are required to prospectively analyze the effect of calcium or calcium plus vitamin D supplementation beyond bone health. The medical community is still uncertain as to the effects of calcium supplements in women. Calcium deposits can be found in many parts of the body at higher ages. A coronary calcium scan is typically done to check for the buildup of calcium in plaque on the walls of the arteries of the heart. Coronary calcium scan scores range from 0 to more than A calcium score of zero means no identifiable plaque, while a score of above indicates extensive atherosclerotic plaque and significant coronary narrowing. Calcification of the breast is often seen in women above the age of 50 years. Calcium deposits are easily detected by x-ray images because calcification is composed of calcium phosphate, similar to that in bone. Coronary calcium is part of the development of atherosclerosis; it occurs exclusively in atherosclerotic arteries and is absent in normal vessel walls. The amount of calcium in the walls of the coronary arteries, assessed by a calcium score, appears to be a better cardiovascular disease risk predictor than standard factors. Risks of Low Calcium Intake: As mentioned above, calcium is important for healthy bones and teeth, as well as for normal muscle and nerve function. There are health problems associated with low calcium levels: Children may not reach their full potential adult height, and adults may have low bone mass, which is a risk factor for osteoporosis and hip fracture. Normal blood calcium levels are maintained through the actions of parathyroid hormone, the kidneys, and the intestines. The normal adult value for serum calcium is 4. Only ionized calcium is transported into cells and metabolically active. Decreases in the ionized free fraction of calcium cause various symptoms. Hypocalcemia, or low-level calcium, most commonly occurs with low calcium absorption, vitamin D or K 2 deficiency, chronic renal failure, and hypoparathyroidism. Risks of High Calcium Intake: Many factors can increase blood calcium levels. Although the body has a built-in regulatory process for calcium absorption and maintenance, underlying diseases, medication interactions, or overuse of supplements can cause high calcium levels. An abnormally high calcium concentration can cause damaging health problems and requires medical treatment. Although dietary calcium is generally safe, excessive calcium does not provide extra bone protection. In fact, if calcium from diet and supplements exceeds the tolerable upper limit, it could cause kidney stones, prostate cancer, constipation, calcium buildup in blood vessels, and impaired absorption of iron and zinc. Taking calcium supplements and eating calcium-fortified foods may increase calcium above normal levels. As a result, it is very important to stick to the RDA and not exceed the recommended dosage. The best way to treat calcium deficiency is to prevent its occurrence. Modification of risk factors is imperative, and pharmacists can play a large role in this area. They can recommend appropriate calcium and vitamin D supplements. Individuals, particularly women, at risk of low calcium should take foods and drinks rich in calcium and vitamin D, quit smoking, and increase weight-bearing and muscle-strengthening exercise. Bailey RL, Dodd KW, Goldman JA, et al. Estimation of total usual calcium and vitamin D intakes in the United States. J Nutr ; 4 Straub DA. Calcium supplementation in clinical practice: a review of forms, doses, and indication, Nutr Clin Pract. Xiao Q, Murphy RA, Houston DK, et al. Dietary and supplemental calcium intakes in relation to mortality from cardiovascular diseases in the NIH-AARP Diet and Health Study. JAMA Intern Med. Bunyardatavej N, Buranasinsup S. J Med Assoc Thai. Saljoughian M. The emerging role of vitamin K 2. US Pharm. Baun L, Russell TM. Overview of the management of osteoporosis in women. Hsia J, Heiss G, Ren H, et al. Vascular calcification and bone disease: the calcification paradox. Trends Mol Med. Otton JM, Lonborg JT, Boshell D, et al. A method for coronary artery calcium scoring using contrast-enhanced computed tomography. J Cardiovasc Comput Tomogr. National Institutes of Health, Office of Dietary Supplements. Dietary supplement fact sheet: calcium. Accessed May 30, Pharmacy Practice Affordable Medicines Biosimilars Compliance Compounding Drug Approvals. COVID Dermatology Diabetes Gastroenterology Hematology. mRNA Technology Neurology Oncology Ophthalmology Orthopedics. Featured Issue Featured Supplements. COVID Resources. Types of Calcium Supplements The two main forms of calcium supplements are carbonate and citrate. Calcium is found in dairy products and in a variety of nondairy products, including dark green leafy vegetables, grains, figs, fish with soft bones, and calcium-fortified foods. Even with healthy eating and a balanced diet, one may not get enough calcium daily. Calcium Supplementation and Cardiovascular Effects Some concerns have been raised about the potential adverse effects of high calcium intake on cardiovascular health among the elderly due to calcification of the arteries and veins. To comment on this article, contact editor uspharmacist. January In This Issue Digital Magazine Archives Subscription. Related Content. Depending on its strength, each chewable pill or soft chew provides about to mg of calcium [ 14 ]. A substantial proportion of people in the United States consume less than recommended amounts of calcium. Average daily intakes of calcium from foods and beverages are 1, mg for men age 20 and older and mg for women [ 18 ]. For children age 2—19, mean daily intakes of calcium from foods and beverages range from to 1, mg [ 18 ]. Average daily calcium intakes from both foods and supplements are 1, mg for men, 1, mg for women, and to 1, mg for children [ 18 ]. Poverty is also associated with a higher risk of inadequacy. NHANES data from to show that the risk of inadequate calcium intakes less than to 1, mg is Calcium deficiency can reduce bone strength and lead to osteoporosis, which is characterized by fragile bones and an increased risk of falling [ 1 ]. Calcium deficiency can also cause rickets in children and other bone disorders in adults, although these disorders are more commonly caused by vitamin D deficiency. In children with rickets, the growth cartilage does not mineralize normally, which can lead to irreversible changes in the skeletal structure [ 1 ]. Another effect of chronic calcium deficiency is osteomalacia, or defective bone mineralization and bone softening, which can occur in adults and children [ 1 ]. For rickets and osteomalacia, the requirements for calcium and vitamin D appear to be interrelated in that the lower the serum vitamin D level measured as hydroxyvitamin D [25 OH D] , the more calcium is needed to prevent these diseases [ 21 ]. Hypocalcemia serum calcium level less than 8. Hypocalcemia can be asymptomatic, especially when it is mild or chronic [ 23 ]. When signs and symptoms do occur, they can range widely because low serum calcium levels can affect most organs and symptoms [ 24 ]. The most common symptom is increased neuromuscular irritability, including perioral numbness, tingling in the hands and feet, and muscle spasms [ 23 ]. More severe signs and symptoms can include renal calcification or injury; brain calcification; neurologic symptoms e. Menopause leads to bone loss because decreases in estrogen production reduce calcium absorption and increase urinary calcium loss and calcium resorption from bone [ 1 ]. Over time, these changes lead to decreased bone mass and fragile bones [ 1 ]. The calcium RDA is 1, mg for women older than 50 years vs. People with lactose intolerance, those with an allergy to milk, and those who avoid eating dairy products including vegans have a higher risk of inadequate calcium intakes because dairy products are rich sources of calcium [ 1 , 27 ]. Options for increasing calcium intakes in individuals with lactose intolerance include consuming lactose-free or reduced-lactose dairy products, which contain the same amounts of calcium as regular dairy products [ 1 , 3 ]. Those who avoid dairy products because of allergies or for other reasons can obtain calcium from nondairy sources, such as some vegetables e. However, these individuals typically need to eat foods fortified with calcium or take supplements to obtain recommended amounts [ 28 ]. This section focuses on six health conditions and diseases in which calcium might play a role: bone health in older adults, cancer, cardiovascular disease CVD , preeclampsia, weight management, and metabolic syndrome. Bone is constantly being remodeled. Declining levels of estrogen in women during menopause and for approximately 5 years afterward lead to rates of bone resorption that are higher than rates of bone formation, resulting in a rapid decrease in bone mass [ 7 ]. Over time, postmenopausal women can develop osteoporosis, in which bone strength is compromised because of lower BMD and bone quality [ 1 ]. Age-related bone loss can also occur in men and lead to osteoporosis, but fracture risk tends to increase in older men about 5 to 10 years later than in older women [ 1 ]. Osteoporosis increases the risk of fractures, especially of the hip, vertebrae, and forearms [ 1 , 7 ]. FDA has approved a health claim for the use of supplements containing calcium and vitamin D to reduce the risk of osteoporosis [ 29 ]. However, not all research supports this claim. In spite of the importance of calcium in bone health, observational evidence is mixed on the link between calcium intakes and measures of bone strength in older adults. Support for such a link comes from an analysis of — NHANES cross-sectional data on 2, adults age 60 and older Results were similar in of the women who were followed for 6 years, even though mean daily intakes of calcium dropped by an average of 40 mg during this period. Some but not all clinical trials have found that calcium supplementation can improve bone health in older adults. On average, women lost 1. Several recent systematic reviews and meta-analyses have found that supplementation with calcium alone or a combination of calcium and vitamin D increases BMD in older adults. For example, a systematic review and meta-analysis included 15 RCTs in postmenopausal women but did not include the two studies described in the previous paragraph in 78, women, of which 37, were in the intervention group and 40, were in the control group [ 34 ]. Supplementation with both calcium and vitamin D or consumption of dairy products fortified with both nutrients increased total BMD as well as BMD at the lumbar spine, arms, and femoral neck. However, in subgroup analyses, calcium had no effect on femoral neck BMD. Earlier systematic reviews and meta-analyses found a positive relationship between calcium and vitamin D supplementation and increased BMD in older males [ 35 ] and between higher calcium intakes from dietary sources or supplements and higher BMD in adults older than 50 [ 25 ]. However, whether these BMD increases were clinically significant is not clear. As with the evidence on the link between increased calcium intakes and reductions in BMD loss, the findings of research on the use of calcium supplementation to prevent fractures in older adults are mixed. For the most part, the observational evidence does not show that increasing calcium intakes reduces the risk of fractures and falls in older adults. For example, a longitudinal cohort study of 1, women age 42 to 52 years at baseline who were followed for 10—12 years found that fracture risk was not significantly different in calcium supplement users some of whom also took vitamin D supplements and nonusers, even though supplement use was associated with less BMD loss throughout the study period [ 36 ]. Some clinical trial evidence shows that supplements containing a combination of calcium and vitamin D can reduce the risk of fractures in older adults. However, findings were negative in another systematic review and meta-analysis that included 14 RCTs of calcium supplementation and 13 trials comparing calcium and vitamin D supplements with hormone therapy, placebo, or no treatment in participants older than 50 years [ 38 ]. The results showed that calcium supplementation alone had no effect on risk of hip fracture, and supplementation with both calcium and vitamin D had no effect on risk of hip fracture, nonvertebral fracture, vertebral fracture, or total fracture. Similarly, a systematic review of 11 RCTs in 51, adults age 50 and older found that supplementation with vitamin D and calcium for 2 to 7 years had no impact on risk of total fractures or of hip fractures [ 39 ]. Preventive Services Task Force USPSTF concluded with moderate certainty that daily doses of less than 1, mg calcium and less than IU 10 mcg vitamin D do not prevent fractures in postmenopausal women and that the evidence on larger doses of this combination is inadequate to assess the benefits in this population [ 40 ]. The USPSTF also determined the evidence on the benefits of calcium supplementation alone or with vitamin D to be inadequate to assess its effect on preventing fractures in men and premenopausal women. Additional research is needed before conclusions can be drawn about the use of calcium supplements to improve bone health and prevent fractures in older adults. Calcium might help reduce the risk of cancer, especially in the colon and rectum [ 1 ]. However, evidence on the relationship between calcium intakes from foods or supplements and different forms of cancer is inconsistent [ 4 ]. Most clinical trial evidence does not support a beneficial effect of calcium supplements on cancer incidence. A 4-year study of 1, mg calcium and 2, IU 50 mcg vitamin D or placebo daily for 4 years in 2, healthy women age 55 years and older showed that supplementation did not reduce the risk of all types of cancer [ 41 ]. The large WHI study described above also found no benefit of supplemental calcium and vitamin D on cancer incidence [ 42 ]. In addition, a meta-analysis of 10 RCTs that included 10, individuals who took supplements containing mg calcium or more without vitamin D for a mean of 3. However, one large clinical trial did find that calcium supplements reduce cancer risk. In this 4-year trial, by the same investigators as the 4-year trial above, 1, women age 55 years or older in Nebraska took 1, to 1, mg calcium alone; 1, to 1, mg calcium plus 1, IU Some scientists have questioned these findings because of the lack of statistical power the studies were designed to detect differences in bone health measures, not cancer incidence , details from the investigators on the study sample, and randomization procedures [ 45 , 46 ]. Observational evidence does not support an association between higher calcium intakes and a lower risk of cancer mortality. An analysis of data on , participants in the Cancer Prevention Study II Nutrition Cohort, who were followed for an average of A systematic review and meta-analysis of 22 observational studies in 2,, participants age 8 and older followed for 4. Clinical trials have also not shown that supplemental calcium alone or combined with vitamin D has an impact on risk of mortality from all cancers. Rates of cancer incidence and cancer mortality did not differ between those who did and those who did not receive calcium supplements. In the WHI trial, 36, postmenopausal women were randomly assigned to daily supplementation with a combination of 1, mg calcium and IU 10 mcg vitamin D3 or placebo [ 42 ]. After an average of 7 years, risk of cancer mortality did not differ between groups. The meta-analysis of 10 RCTs that included 10, individuals described above found no impact of calcium supplementation on cancer mortality rates [ 43 ]. A substantial body of evidence has addressed the role of calcium in preventing colorectal cancer or its precursor, adenomas. Much but not all of the observational evidence supports a link between higher calcium intakes and lower risk of colorectal cancer. A cohort study in 77, adults found that over a mean of 7. Findings were similar for dietary intakes of calcium in two other meta-analyses [ 52 , 53 ]. In spite of the observational evidence supporting an association between higher calcium intakes and lower colorectal cancer risk, clinical trials investigating calcium supplements for prevention of colorectal cancer or adenomas have had mixed results. A follow-up study by Cauley and colleagues evaluated outcomes 4. Colorectal cancer rates did not differ between groups. Several observational studies have shown that the risk of prostate cancer might be higher with higher calcium intakes, but possibly only when the calcium comes from dairy foods. In an analysis of data from 2, men who participated in the French SU. MAX Supplementation en Vitamines et Minéraux Antioxydants prospective study and were followed for an average of 7. The risk was 2. However, in analyses of results for various sources of calcium, only calcium from dairy foods was significantly associated with prostate cancer risk 2. A meta-analysis included 15 epidemiological studies of calcium intake and ovarian cancer risk in , women who developed 7, cases of ovarian cancer [ 59 ]. However, the difference in risk was not statistically significant when both dietary and supplemental calcium intakes were considered. For breast cancer, observational studies have had mixed findings on whether higher calcium intakes are associated with a lower risk. However, the WHI described above found similar incidence rates of invasive breast cancer in the supplement and placebo groups [ 61 ]. Additional well-designed randomized trials are needed to determine whether dietary or supplemental calcium intakes increase, decrease, or have no effect on risk of cancer in general or of specific types of cancer, or on cancer mortality. Calcium binds fatty acids, so it can reduce lipid absorption and might therefore lower CVD risk [ 1 , 4 ]. However, the findings from research on the role of dietary calcium and calcium supplements in reducing CVD have been mixed, and some evidence indicates that calcium supplements might even increase CVD risk. Several large observational studies have shown an association between lower calcium intakes and higher risk of hypertension, stroke, and atherosclerosis. This association was strongest in women, adults age 20—44 years, those who did not have diabetes, and especially women age 20—44 years. However, the study found no association between calcium intakes and risk of CVD mortality or myocardial infarction. Furthermore, a systematic review and meta-analysis that included 27 observational studies found no consistent dose-response relationships between total, dietary, or supplemental calcium intakes and CVD mortality [ 65 ]. Evidence on dose-response relationships between calcium intakes and risk of stroke or stroke mortality was inconsistent. A diet containing more calcium than the typical U. diet because of added low-fat or nonfat dairy products lowered systolic blood pressure by an average of 5. However, this Dietary Approaches to Stop Hypertension DASH diet also increases intakes of other nutrients, such as potassium and magnesium, that are associated with reductions in blood pressure, so any independent contribution of calcium cannot be determined. Some clinical trials have shown that calcium supplements are associated with decreased hypertension risk or decreased cholesterol levels, but others have had more mixed findings. A Cochrane Review of 16 trials in 3, adults with a median follow-up period of 3. Findings were mixed in two analyses of data from the WHI. In another secondary analysis of data on 16, WHI participants, the supplements had no association with atrial fibrillation risk [ 70 ]. Similarly, an evidence report and systematic review conducted for the USPSTF that included 11 RCTs of vitamin D, calcium, or both for 2 to 7 years in 51, adults age 50 years and older found that supplementation with vitamin D alone or combined with calcium had no effect on CVD incidence [ 39 ]. |
Calcium absorption -
Grimm M, Muller A, Hein G, Funfstuck R, Jahreis G. High phosphorus intake only slightly affects serum minerals, urinary pyridinium crosslinks and renal function in young women. Kemi VE, Karkkainen MU, Rita HJ, Laaksonen MM, Outila TA, Lamberg-Allardt CJ.
Low calcium:phosphorus ratio in habitual diets affects serum parathyroid hormone concentration and calcium metabolism in healthy women with adequate calcium intake.
Br J Nutr. Heaney RP. Calvo MS, Moshfegh AJ, Tucker KL. Assessing the health impact of phosphorus in the food supply: issues and considerations. Adv Nutr. Heaney RP, Rafferty K. Carbonated beverages and urinary calcium excretion.
Ribeiro-Alves MA, Trugo LC, Donangelo CM. Use of oral contraceptives blunts the calciuric effect of caffeine in young adult women. Barger-Lux MJ, Heaney RP, Stegman MR. Effects of moderate caffeine intake on the calcium economy of premenopausal women.
Wikoff D, Welsh BT, Henderson R, et al. Systematic review of the potential adverse effects of caffeine consumption in healthy adults, pregnant women, adolescents, and children. Food Chem Toxicol. pii: S 17 doi: Haleem S, Lutchman L, Mayahi R, Grice JE, Parker MJ.
Mortality following hip fracture: trends and geographical variations over the last 40 years. Kaufman JM, Reginster JY, Boonen S, et al. Treatment of osteoporosis in men. Calcium, dairy products and osteoporosis.
J Am Coll Nutr. Crandall CJ, Newberry SJ, Diamant A, et al. Treatment to prevent fractures in men and women with low bone density or osteoporosis: update of a report. Rockville MD ; Rizzoli R, Bianchi ML, Garabedian M, McKay HA, Moreno LA.
Maximizing bone mineral mass gain during growth for the prevention of fractures in the adolescents and the elderly. Borer KT. Physical activity in the prevention and amelioration of osteoporosis in women : interaction of mechanical, hormonal and dietary factors.
Sports Med. National Osteoporosis Foundation. Clinician's Guide to Prevention and Treatment of Osteoporosis. Levis S, Theodore G. Summary of AHRQ's comparative effectiveness review of treatment to prevent fractures in men and women with low bone density or osteoporosis: update of the report.
J Manag Care Pharm. Tai V, Leung W, Grey A, Reid IR, Bolland MJ. Calcium intake and bone mineral density: systematic review and meta-analysis.
Bolland MJ, Leung W, Tai V, et al. Calcium intake and risk of fracture: systematic review. Chung M, Lee J, Terasawa T, Lau J, Trikalinos TA.
Vitamin D with or without calcium supplementation for prevention of cancer and fractures: an updated meta-analysis for the U. Preventive Services Task Force. Ann Intern Med.
Weaver CM, Alexander DD, Boushey CJ, et al. Calcium plus vitamin D supplementation and risk of fractures: an updated meta-analysis from the National Osteoporosis Foundation.
Osteoporos Int. Cosman F, de Beur SJ, LeBoff MS, et al. Lips P, van Schoor NM. The effect of vitamin D on bone and osteoporosis. Best Pract Res Clin Endocrinol Metab. Gallagher JC, Yalamanchili V, Smith LM.
The effect of vitamin D on calcium absorption in older women. Zhu K, Bruce D, Austin N, Devine A, Ebeling PR, Prince RL.
Randomized controlled trial of the effects of calcium with or without vitamin D on bone structure and bone-related chemistry in elderly women with vitamin D insufficiency.
J Bone Miner Res. Dipart Group. Patient level pooled analysis of 68 patients from seven major vitamin D fracture trials in US and Europe. Avenell A, Mak JC, O'Connell D. Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men.
Cochrane Database Syst Rev. Bischoff-Ferrari HA, Willett WC, Orav EJ, et al. A pooled analysis of vitamin D dose requirements for fracture prevention. N Engl J Med.
Aspray TJ, Francis RM. Fracture prevention in care home residents: is vitamin D supplementation enough? Age Ageing. Murad MH, Elamin KB, Abu Elnour NO, et al. Clinical review: The effect of vitamin D on falls: a systematic review and meta-analysis.
Lerolle N, Lantz B, Paillard F, et al. Risk factors for nephrolithiasis in patients with familial idiopathic hypercalciuria. Am J Med. Sorensen MD, Eisner BH, Stone KL, et al.
Impact of calcium intake and intestinal calcium absorption on kidney stones in older women: the study of osteoporotic fractures. J Urol. Curhan GC, Willett WC, Knight EL, Stampfer MJ. Dietary factors and the risk of incident kidney stones in younger women: Nurses' Health Study II. Arch Intern Med.
Curhan GC, Willett WC, Rimm EB, Stampfer MJ. A prospective study of dietary calcium and other nutrients and the risk of symptomatic kidney stones.
Taylor EN, Stampfer MJ, Curhan GC. Dietary factors and the risk of incident kidney stones in men: new insights after 14 years of follow-up. J Am Soc Nephrol. Taylor EN, Curhan GC. Dietary calcium from dairy and nondairy sources, and risk of symptomatic kidney stones. Borghi L, Schianchi T, Meschi T, et al.
Comparison of two diets for the prevention of recurrent stones in idiopathic hypercalciuria. Hess B, Jost C, Zipperle L, Takkinen R, Jaeger P. High-calcium intake abolishes hyperoxaluria and reduces urinary crystallization during a fold normal oxalate load in humans. Nephrol Dial Transplant.
Liebman M, Chai W. Effect of dietary calcium on urinary oxalate excretion after oxalate loads. Lange JN, Wood KD, Mufarrij PW, et al. The impact of dietary calcium and oxalate ratios on stone risk. Jackson RD, LaCroix AZ, Gass M, et al.
Calcium plus vitamin D supplementation and the risk of fractures. Calcium supplementation and incident kidney stone risk: a systematic review.
Candelas G, Martinez-Lopez JA, Rosario MP, Carmona L, Loza E. Calcium supplementation and kidney stone risk in osteoporosis: a systematic literature review.
Clin Exp Rheumatol. Escribano J, Balaguer A, Roque i Figuls M, Feliu A, Ferre N. Dietary interventions for preventing complications in idiopathic hypercalciuria. Heilberg IP, Goldfarb DS. Optimum nutrition for kidney stone disease. Adv Chronic Kidney Dis. Prezioso D, Strazzullo P, Lotti T, et al.
Dietary treatment of urinary risk factors for renal stone formation. A review of CLU Working Group. Arch Ital Urol Androl.
Duley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol. Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Hofmeyr GJ, Lawrie TA, Atallah AN, Duley L, Torloni MR.
Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Scholl TO, Chen X, Stein TP. Vitamin D, secondary hyperparathyroidism, and preeclampsia. Maternal calcium metabolic stress and fetal growth. Hofmeyr GJ, Belizan JM, von Dadelszen P, Calcium, Pre-eclampsia Study G.
Low-dose calcium supplementation for preventing pre-eclampsia: a systematic review and commentary. World Health Organization. Calcium supplementation in pregnant women; Hofmeyr GJ, Mlokoti Z, Nikodem VC, et al. Calcium supplementation during pregnancy for preventing hypertensive disorders is not associated with changes in platelet count, urate, and urinary protein: a randomized control trial.
Hypertens Pregnancy. Villar J, Abdel-Aleem H, Merialdi M, et al. World Health Organization randomized trial of calcium supplementation among low calcium intake pregnant women. Am J Obstet Gynecol. Hofmeyr GJ, Novikova N, Singata M, et al.
The Lancet ; Hofmeyr GJ, Seuc AH, Betran AP, et al. The effect of calcium supplementation on blood pressure in non-pregnant women with previous pre-eclampsia: An exploratory, randomized placebo controlled study.
Pregnancy Hypertens. US Centers for Disease Control and Prevention. Colorectal Cancer Statistics. Whitfield JF. Calcium, calcium-sensing receptor and colon cancer. Cancer Lett.
Murphy N, Norat T, Ferrari P, et al. Consumption of dairy products and colorectal cancer in the European Prospective Investigation into Cancer and Nutrition EPIC.
PLoS One. Massa J, Cho E, Orav EJ, Willett WC, Wu K, Giovannucci EL. Total calcium intake and colorectal adenoma in young women. Cancer Causes Control. Keum N, Lee DH, Greenwood DC, Zhang X, Giovannucci EL. Calcium intake and colorectal adenoma risk: dose-response meta-analysis of prospective observational studies.
Int J Cancer. Bristow SM, Bolland MJ, MacLennan GS, et al. Calcium supplements and cancer risk: a meta-analysis of randomised controlled trials. Bolland MJ, Grey A, Gamble GD, Reid IR. Calcium and vitamin D supplements and health outcomes: a reanalysis of the Women's Health Initiative WHI limited-access data set.
Bonovas S, Fiorino G, Lytras T, Malesci A, Danese S. Calcium supplementation for the prevention of colorectal adenomas: A systematic review and meta-analysis of randomized controlled trials.
World J Gastroenterol. Mielke HW, Gonzales C, Powell E, Mielke PW. Evolving from reactive to proactive medicine: community lead Pb and clinical disparities in pre- and post-Katrina New Orleans. Int J Environ Res Public Health. Centers for Disease Control and Prevention.
New blood lead level information. htm , 15 August Bruening K, Kemp FW, Simone N, Holding Y, Louria DB, Bogden JD. Dietary calcium intakes of urban children at risk of lead poisoning. Environ Health Perspect. Hertz-Picciotto I, Schramm M, Watt-Morse M, Chantala K, Anderson J, Osterloh J.
Patterns and determinants of blood lead during pregnancy. Am J Epidemiol. Ettinger AS, Lamadrid-Figueroa H, Tellez-Rojo MM, et al. Effect of calcium supplementation on blood lead levels in pregnancy: a randomized placebo-controlled trial. Ettinger AS, Tellez-Rojo MM, Amarasiriwardena C, et al.
Influence of maternal bone lead burden and calcium intake on levels of lead in breast milk over the course of lactation. Hernandez-Avila M, Gonzalez-Cossio T, Hernandez-Avila JE, et al. Dietary calcium supplements to lower blood lead levels in lactating women: a randomized placebo-controlled trial.
Muldoon SB, Cauley JA, Kuller LH, Scott J, Rohay J. Lifestyle and sociodemographic factors as determinants of blood lead levels in elderly women. Dougkas A, Reynolds CK, Givens ID, Elwood PC, Minihane AM. Associations between dairy consumption and body weight: a review of the evidence and underlying mechanisms.
Nutr Res Rev. Zemel MB, Thompson W, Milstead A, Morris K, Campbell P. Calcium and dairy acceleration of weight and fat loss during energy restriction in obese adults. Obes Res. Zemel MB, Shi H, Greer B, Dirienzo D, Zemel PC. Regulation of adiposity by dietary calcium.
Faseb J. Gonzalez JT, Rumbold PL, Stevenson EJ. Effect of calcium intake on fat oxidation in adults: a meta-analysis of randomized, controlled trials. Obes Rev. Bortolotti M, Rudelle S, Schneiter P, et al. Dairy calcium supplementation in overweight or obese persons: its effect on markers of fat metabolism.
The effect of vitamin D supplementation on serum 25 OH D in thin and obese women. J Steroid Biochem Mol Biol. Pathak K, Soares MJ, Calton EK, Zhao Y, Hallett J. Vitamin D supplementation and body weight status: a systematic review and meta-analysis of randomized controlled trials.
Christensen R, Lorenzen JK, Svith CR, et al. Effect of calcium from dairy and dietary supplements on faecal fat excretion: a meta-analysis of randomized controlled trials.
Tordoff MG. Calcium: taste, intake, and appetite. Physiol Rev. Chen M, Pan A, Malik VS, Hu FB. Effects of dairy intake on body weight and fat: a meta-analysis of randomized controlled trials.
Booth AO, Huggins CE, Wattanapenpaiboon N, Nowson CA. Effect of increasing dietary calcium through supplements and dairy food on body weight and body composition: a meta-analysis of randomised controlled trials.
Effects of calcium supplementation on body weight: a meta-analysis. Soares MJ, Pathak K, Calton EK. Calcium and vitamin D in the regulation of energy balance: where do we stand?
Int J Mol Sci. Freeman EW. Premenstrual syndrome and premenstrual dysphoric disorder: definitions and diagnosis. Pearlstein T, Steiner M. Premenstrual dysphoric disorder: burden of illness and treatment update. J Psychiatry Neurosci. Bendich A. The potential for dietary supplements to reduce premenstrual syndrome PMS symptoms.
Bertone-Johnson ER, Hankinson SE, Bendich A, Johnson SR, Willett WC, Manson JE. Calcium and vitamin D intake and risk of incident premenstrual syndrome. Thys-Jacobs S, Starkey P, Bernstein D, Tian J. Calcium carbonate and the premenstrual syndrome: effects on premenstrual and menstrual symptoms.
Premenstrual Syndrome Study Group. Thys-Jacobs S, Ceccarelli S, Bierman A, Weisman H, Cohen MA, Alvir J. Calcium supplementation in premenstrual syndrome: a randomized crossover trial. J Gen Intern Med. Alvir JM, Thys-Jacobs S. Premenstrual and menstrual symptom clusters and response to calcium treatment.
Psychopharmacol Bull. Bharati M. J Caring Sci. Masoumi SZ, Ataollahi M, Oshvandi K. Effect of combined use of calcium and vitamin B6 on premenstrual syndrome symptoms: a randomized clinical trial.
Shehata NA. Calcium versus oral contraceptive pills containing drospirenone for the treatment of mild to moderate premenstrual syndrome: a double blind randomized placebo controlled trial.
Eur J Obstet Gynecol Reprod Biol. Shobeiri F, Araste FE, Ebrahimi R, Jenabi E, Nazari M. Effect of calcium on premenstrual syndrome: A double-blind randomized clinical trial. Obstet Gynecol Sci.
Nevatte T, O'Brien PM, Backstrom T, et al. ISPMD consensus on the management of premenstrual disorders. Arch Womens Ment Health. Whelan AM, Jurgens TM, Naylor H. Herbs, vitamins and minerals in the treatment of premenstrual syndrome: a systematic review.
Can J Clin Pharmacol. Cappuccio FP, Elliott P, Allender PS, Pryer J, Follman DA, Cutler JA. Epidemiologic association between dietary calcium intake and blood pressure: a meta-analysis of published data. Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure.
DASH Collaborative Research Group. Conlin PR, Chow D, Miller ER, 3rd, et al. The effect of dietary patterns on blood pressure control in hypertensive patients: results from the Dietary Approaches to Stop Hypertension DASH trial.
Am J Hypertens. Miller GD, DiRienzo DD, Reusser ME, McCarron DA. Benefits of dairy product consumption on blood pressure in humans: a summary of the biomedical literature. Allender PS, Cutler JA, Follmann D, Cappuccio FP, Pryer J, Elliott P.
Dietary calcium and blood pressure: a meta-analysis of randomized clinical trials. Bucher HC, Cook RJ, Guyatt GH, et al. Effects of dietary calcium supplementation on blood pressure. A meta-analysis of randomized controlled trials.
Dickinson HO, Nicolson DJ, Cook JV, et al. Calcium supplementation for the management of primary hypertension in adults. Challoumas D, Cobbold C, Dimitrakakis G. Effects of calcium intake on the cardiovascular system in postmenopausal women.
Blumberg JB, Frei BB, Fulgoni VL, Weaver CM, Zeisel SH. Kit BK, Fakhouri TH, Park S, Nielsen SJ, Ogden CL. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: Zhu K, Prince RL.
Calcium and bone. Clin Biochem. Bailey RL, Dodd KW, Goldman JA, et al. Estimation of total usual calcium and vitamin D intakes in the United States.
Straub DA. Calcium supplementation in clinical practice: a review of forms, doses, and indications. Nutr Clin Pract. Roberts HJ. Potential toxicity due to dolomite and bonemeal.
South Med J. Bourgoin BP, Evans DR, Cornett JR, Lingard SM, Quattrone AJ. Lead content in 70 brands of dietary calcium supplements. Am J Public Health. Scelfo GM, Flegal AR. Lead in calcium supplements. Carrington CD, Bolger PM. An assessment of the hazards of lead in food.
Regul Toxicol Pharmacol. Ross EA, Szabo NJ, Tebbett IR. Lead content of calcium supplements. Mindak WR, Cheng J, Canas BJ, Bolger PM. Lead in women's and children's vitamins. J Agric Food Chem. Moe SM. Disorders involving calcium, phosphorus, and magnesium. Prim Care. Patel AM, Goldfarb S.
Got calcium? Welcome to the calcium-alkali syndrome. Lewis JR, Zhu K, Prince RL. Adverse events from calcium supplementation: relationship to errors in myocardial infarction self-reporting in randomized controlled trials of calcium supplementation.
World Cancer Research Fund International. Cancer facts and figures - worldwide data. Gonzalez CA, Riboli E. Diet and cancer prevention: Contributions from the European Prospective Investigation into Cancer and Nutrition EPIC study. Eur J Cancer. Kurahashi N, Inoue M, Iwasaki M, Sasazuki S, Tsugane AS, Japan Public Health Center-Based Prospective Study G.
Dairy product, saturated fatty acid, and calcium intake and prostate cancer in a prospective cohort of Japanese men. Cancer Epidemiol Biomarkers Prev. Raimondi S, Mabrouk JB, Shatenstein B, Maisonneuve P, Ghadirian P.
Diet and prostate cancer risk with specific focus on dairy products and dietary calcium: a case-control study. Torfadottir JE, Steingrimsdottir L, Mucci L, et al.
Milk intake in early life and risk of advanced prostate cancer. Song Y, Chavarro JE, Cao Y, et al. Whole milk intake is associated with prostate cancer-specific mortality among U. male physicians. Pettersson A, Kasperzyk JL, Kenfield SA, et al. Milk and dairy consumption among men with prostate cancer and risk of metastases and prostate cancer death.
Aune D, Navarro Rosenblatt DA, Chan DS, et al. Dairy products, calcium, and prostate cancer risk: a systematic review and meta-analysis of cohort studies. Qin LQ, He K, Xu JY. Milk consumption and circulating insulin-like growth factor-I level: a systematic literature review.
Int J Food Sci Nutr. Rowlands MA, Gunnell D, Harris R, Vatten LJ, Holly JM, Martin RM. Circulating insulin-like growth factor peptides and prostate cancer risk: a systematic review and meta-analysis. Allen NE, Key TJ, Appleby PN, et al.
Animal foods, protein, calcium and prostate cancer risk: the European Prospective Investigation into Cancer and Nutrition.
Br J Cancer. Moreno J, Krishnan AV, Peehl DM, Feldman D. Mechanisms of vitamin D-mediated growth inhibition in prostate cancer cells: inhibition of the prostaglandin pathway. Anticancer Res.
Brandstedt J, Almquist M, Manjer J, Malm J. Vitamin D, PTH, and calcium in relation to survival following prostate cancer. Brandstedt J, Almquist M, Ulmert D, Manjer J, Malm J. Vitamin D, PTH, and calcium and tumor aggressiveness in prostate cancer: a prospective nested case-control study.
Rowland GW, Schwartz GG, John EM, Ingles SA. Protective effects of low calcium intake and low calcium absorption vitamin D receptor genotype in the California Collaborative Prostate Cancer Study.
Baron JA, Beach M, Wallace K, et al. Risk of prostate cancer in a randomized clinical trial of calcium supplementation.
Chung M, Balk EM, Brendel M, et al. Vitamin D and calcium: a systematic review of health outcomes. Evid Rep Technol Assess Full Rep. Huncharek M, Muscat J, Kupelnick B.
Dairy products, dietary calcium and vitamin D intake as risk factors for prostate cancer: a meta-analysis of 26, cases from 45 observational studies. Nutr Cancer. Pentti K, Tuppurainen MT, Honkanen R, et al. Use of calcium supplements and the risk of coronary heart disease in year-old women: The Kuopio Osteoporosis Risk Factor and Prevention Study.
Li K, Kaaks R, Linseisen J, Rohrmann S. Associations of dietary calcium intake and calcium supplementation with myocardial infarction and stroke risk and overall cardiovascular mortality in the Heidelberg cohort of the European Prospective Investigation into Cancer and Nutrition study EPIC-Heidelberg.
Xiao Q, Murphy RA, Houston DK, Harris TB, Chow WH, Park Y. Dietary and supplemental calcium intake and cardiovascular disease mortality: the National Institutes of Health-AARP diet and health study. JAMA Intern Med. Bolland MJ, Barber PA, Doughty RN, et al. Vascular events in healthy older women receiving calcium supplementation: randomised controlled trial.
Bolland MJ, Grey A, Avenell A, Gamble GD, Reid IR. Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women's Health Initiative limited access dataset and meta-analysis.
Hsia J, Heiss G, Ren H, et al. Abrahamsen B, Sahota O. Do calcium plus vitamin D supplements increase cardiovascular risk?
Lewis JR, Calver J, Zhu K, Flicker L, Prince RL. Calcium supplementation and the risks of atherosclerotic vascular disease in older women: results of a 5-year RCT and a 4.
Avenell A, MacLennan GS, Jenkinson DJ, et al. Van Hemelrijck M, Michaelsson K, Linseisen J, Rohrmann S. Calcium intake and serum concentration in relation to risk of cardiovascular death in NHANES III. Foley RN, Collins AJ, Ishani A, Kalra PA. Calcium-phosphate levels and cardiovascular disease in community-dwelling adults: the Atherosclerosis Risk in Communities ARIC Study.
Am Heart J. Lutsey PL, Alonso A, Michos ED, et al. Serum magnesium, phosphorus, and calcium are associated with risk of incident heart failure: the Atherosclerosis Risk in Communities ARIC Study. Wang TK, Bolland MJ, van Pelt NC, et al. Relationships between vascular calcification, calcium metabolism, bone density, and fractures.
Samelson EJ, Booth SL, Fox CS, et al. If you have trouble swallowing pills, you may want a chewable or liquid calcium supplement.
Your body must be able to absorb the calcium for it to be effective. All varieties of calcium supplements are better absorbed when taken in small doses mg or less at mealtimes. Calcium citrate is absorbed equally well when taken with or without food and is a form recommended for individuals with low stomach acid more common in people over 50 or taking acid blockers , inflammatory bowel disease or absorption disorders.
Dietary calcium is generally safe, but more isn't necessarily better, and excessive calcium doesn't provide extra bone protection.
If you take calcium supplements and eat calcium-fortified foods, you may be getting more calcium than you realize. Check food and supplement labels to monitor how much total calcium you're getting a day and whether you're achieving the RDA but not exceeding the recommended upper limit.
Be sure to tell your doctor if you're taking calcium supplements. There is a problem with information submitted for this request. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health.
Click here for an email preview. Error Email field is required. Error Include a valid email address. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version.
This content does not have an Arabic version. Appointments at Mayo Clinic Mayo Clinic offers appointments in Arizona, Florida and Minnesota and at Mayo Clinic Health System locations. Request Appointment. Healthy Lifestyle Nutrition and healthy eating. Sections Basics Nutrition basics Healthy diets Healthy cooking Healthy menus and shopping strategies Nutritional supplements In-Depth Expert Answers Multimedia Resources News From Mayo Clinic What's New.
Products and services. Calcium and calcium supplements: Achieving the right balance Calcium is important for bone health. See how much you need and how to get it. By Mayo Clinic Staff. Thank you for subscribing!
Sorry something went wrong with your subscription Please, try again in a couple of minutes Retry. Show references Calcium and vitamin D: Important at every age. National Institutes of Health. Accessed Oct. Natural Medicines. Calcium fact sheet for professionals. Office of Dietary Supplements. Rosen HN.
Calcium and vitamin D supplementation in osteoporosis. Department of Health and Human Services and U. Department of Agriculture. Dietary Guidelines Advisory Committee. Scientific report of the Dietary Guidelines Advisory Committee: Advisory report to the Secretary of Agriculture and the Secretary of Health and Human Services.
Department of Agriculture, Agricultural Research Service. What people with celiac disease need to know about osteoporosis.
NIH Osteoporosis and Related Bone Diseases National Resource Center. Dietary supplements verification program. Pharmacopeial Convention. About ConsumerLab. What is third-party certification?
NSF International. Products and Services Nutritional Supplements at Mayo Clinic Store The Mayo Clinic Diet Online A Book: The Mayo Clinic Diet Bundle. See also Timing calcium supplements COVID and vitamin D Can vitamins help prevent a heart attack?
Can zinc supplements help treat hidradenitis suppurativa? Vitamin C and mood Fiber supplements Ground flaxseed Heartburn medicines and B deficiency Multivitamins for kids Prenatal vitamins Probiotics and prebiotics Vitamin C megadoses Vitamin D and MS: Any connection? Vitamin D deficiency Can a lack of vitamin D cause high blood pressure?
Vitamin D for babies Vitamin D toxicity Vitamins for MS: Do supplements make a difference? Show more related content. Mayo Clinic Press Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book.
ART Healthy Lifestyle Nutrition and healthy eating In-Depth Calcium and calcium supplements - Achieving the right balance. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site.
Contact Us. Health Information Policy. Media Requests. News Network. Price Transparency.
Calcium is one of the most Mind-body connection absorrption Calcium absorption for optimal bone and dental health. Several studies suggest that calcium, along abslrption vitamin Mind-body connection, may have benefits Antidepressant for generalized anxiety bone ahsorption, and it Mind-body connection generally accepted that the heart, muscles, and nerves also need calcium to function properly. Millions of women in the United States take calcium supplements in an attempt to boost bone strength, especially after menopause when the risk of fractures increases. Patients with rheumatoid arthritis and other inflammatory forms of the disease also routinely take calcium supplements. Most people get enough calcium through their diets.
0 thoughts on “Calcium absorption”