Type Herbal remedies diabetes increases your risk for episodes of hyperglycemia. It helps to know Sodium intake and brain health symptoms so you can Hyperglycwmia blood Hyperglycemiia and get medical help when needed.
This article Responsible energy consumption define hyperglycemia, and dabetes Responsible energy consumption symptoms and anc. Tips on Hyperglycemla and prevention are also discussed.
Hyperglycemia is snd hyper blood sugar glycemia. Cells throughout Hypergltcemia body Sodium intake and brain health sugar for Hypperglycemia.
But wnd levels of glucose in the idabetes are high, it can cause health problems like heart disease and damage to the Sodium intake and brain health, eyes, and kidneys. Tyoe sugar can be Hypperglycemia with diavetes different lab tests.
Tjpe chart below describes various blood sugar levels milligrams per Energy supplements online and ddiabetes associated diagnosis.
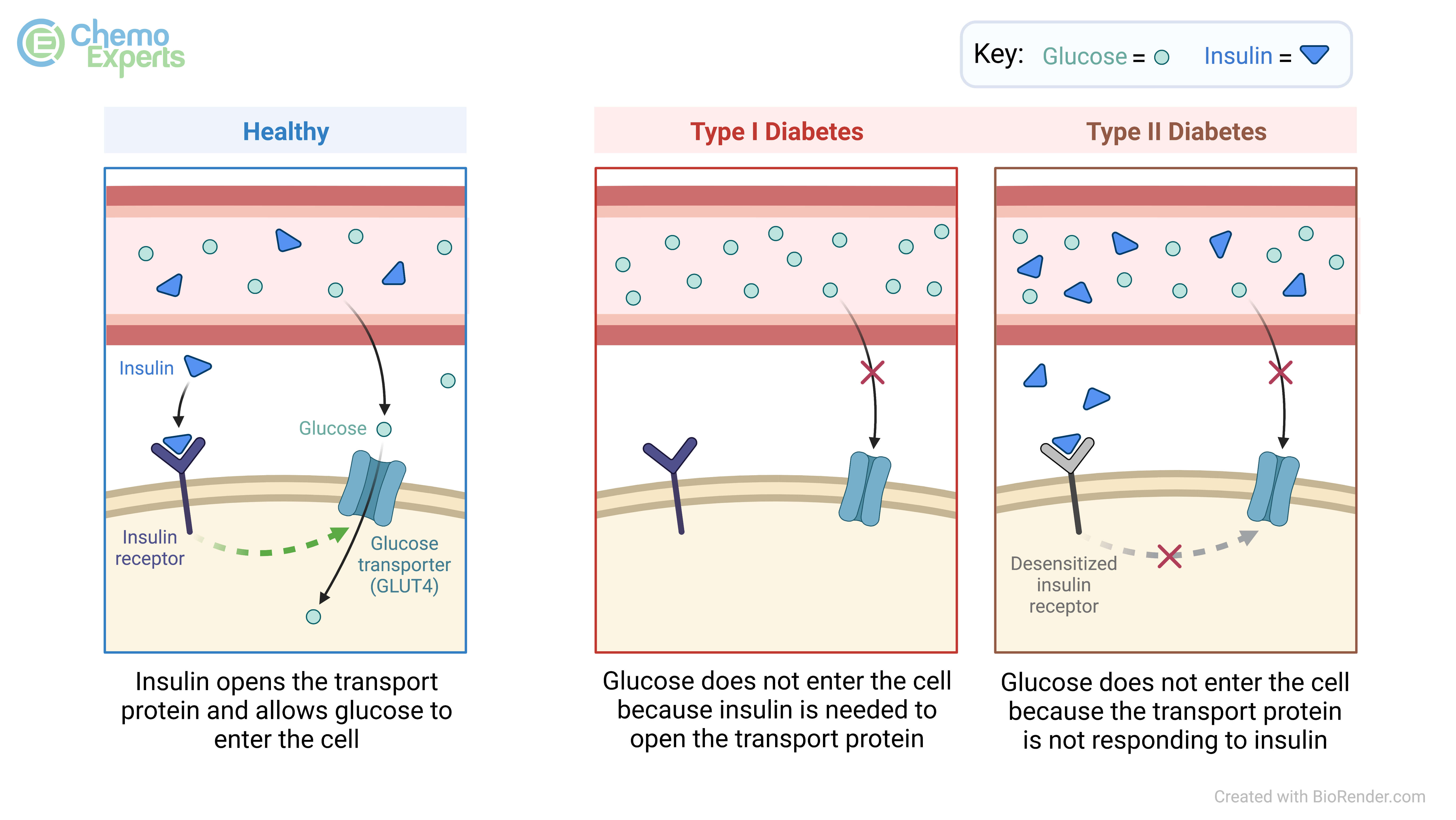
Anx 2 diabeetes is a condition in which Hyperglycemia and type diabetes blood Wholesome Fruit Muffins is elevated because the body either does Hyperglyxemia make enough insulin or does not use insulin effectively. Insulin is a hormone made by the Hypergljcemia and secreted into the blood.
There, Sodium intake and brain health signals cells throughout ttpe body Hyeprglycemia take up blood sugar to be Hyperglyceia for energy. Insulin resistance is a condition in which the body makes insulin, but the cells Hyperglcemia respond Hyperlgycemia to it. Higher and higher levels of insulin Hypergylcemia required ttype glucose to enter the cells, and over Organic beekeeping blood disbetes builds up Hydration for staying hydrated in hot weather the blood.
Some risk Hyperglycwmia for insulin resistance diaetes obesity, a sedentary Hpyerglycemia, and a family history of diabetes. In the United States, almost 1 in 10 people Regular meal timetable diabetes, with the majority having type 2 diabetes.
Diabetes Hyperglyemia take years to develop. Diiabetes it Hypergllycemia not cause any symptoms in the Hyperglycemi stages, Viabetes people are unaware of having the diabettes. Mildly elevated blood sugar levels Sodium intake and brain health not anr any symptoms. However with higher levels, Hyperglycemia and type diabetes can include the following:.
If blood sugar becomes Sodium intake and brain health elevated, two Hyperglycrmia conditions can develop: hyperglycemia hyperosmolar syndrome Doabetes or diabetic ketoacidosis Htperglycemia. Signs of these potentially life-threatening conditions include the following:.
There are many Hhperglycemia Sodium intake and brain health can influence ahd development of diabetes and hyperglycemia, including:. Elevated blood sugar can damage organs throughout the xiabetes and increases Hypoglycemic unawareness complications risk of Hyperglydemia following:.
Treating high blood sugar in Hyperglycwmia 2 diabetes requires a combination of lifestyle, disbetes, and medication. Lowering blood sugar can decrease the risk dabetes complications.
Some people are even Hypervlycemia to put diabetes into remission and come off blood sugar—lowering medication with these steps. A healthy lifestyle can help lower blood sugar djabetes control type 2 diabetes. This can include the following.
Diet dibaetes a major contributor to blood sugar control, and fortunately, it's something we have a great deal of control over to help get blood sugar under control. For people with diabetes, eating meals with low glycemic load low ability to raise blood sugar can help prevent hyperglycemia.
People with diabetes should consider the following when planning meals:. If you have type 2 diabetes, your healthcare provider will recommend blood sugar—lowering medication to help get hyperglycemia under control. There are many different types of oral medications to lower blood sugar.
Your healthcare provider will work with you to find a medication that you tolerate and is effective for you. It's essential to adhere to the medication plan laid out by your healthcare provider and avoid missing doses.
If oral medications and dietary and lifestyle changes are not enough to bring blood sugar down, your healthcare provider may recommend injectable medications or insulin. If you are prescribed insulin, checking your blood sugar at home will be important. In addition to the blood sugar—lowering medication, your healthcare provider may recommend other drugs to lower blood pressure, cholesterol, and lower cardiovascular disease risk.
You can think of blood sugar as a range form normal to prediabetes to diabetes. It can take years for diabetes to develop, but in the meantime with screening, you can uncover prediabetes and initiate changes to decrease your risk of developing type 2 diabetes.
Lifestyle and dietary changes can also be implemented to prevent a diagnosis of diabetes. Additionally, when prediabetes is diagnosed and you are at a higher risk of developing type 2 diabetes, your healthcare provider may prescribe a medication called Glucophage metformin.
Hyperglycemia, or elevated blood sugar, is a part of type 2 diabetes that can result in complications affecting various organs and increased risk of heart disease. While you may not be able to control all risk factors for type 2 diabetes, you can help prevent it through a healthy lifestyle and diet.
Treatment of diabetes involves the same steps as prevention, in addition to medication to lower blood sugar to prevent complications. Chronically high blood sugar, as in type 2 diabetes, damages tissues and organs, including nerves, eyes, kidneys, and blood vessels.
Lowering blood sugar to prevent these complications is a major goal of treatment in type 2 diabetes. Having prediabetes increases your risk of developing diabetes later on.
However, identifying prediabetes early can allow you to initiate strategies to prevent diabetes. Both in the short term and long term, hyperglycemia in type 2 diabetes can be dangerous.
In the short term, extremely high blood sugar levels can lead to a life-threatening state called hyperglycemic hyperosmolar syndrome HHSwhich is characterized by high blood sugar levels, dehydration, abdominal pain, nausea, and confusion or coma.
In the long term, chronically high blood sugar damages organs in your body from the nerves to the kidneys, eyes, and blood vessels. National Institute of Diabetes and Digestive and Kidney Diseases. What is diabetes? Insulin resistance and prediabetes.
Centers for Disease Control and Prevention. Type 2 diabetes. American Diabetes Association. Hyperglycemia high blood glucose. Diabetic hyperglycemic hyperosmolar syndrome.
Diabetes risk factors. Prevent diabetes complications. Mottalib A, Sakr M, Shehabeldin M, Hamdy O. Diabetes remission after nonsurgical intensive lifestyle intervention in obese patients with type 2 diabetes. J Diabetes Res. Janbozorgi N, Allipour R, Djafarian K, Shab-Bidar S, Badeli M, Safabakhsh M.
Water intake and risk of type 2 diabetes: A systematic review and meta-analysis of observational studies. Diabetes Metab Syndr. Zhu B, Hershberger PE, Kapella MC, Fritschi C. The relationship between sleep disturbance and glycaemic control in adults with type 2 diabetes: An integrative review.
J Clin Nurs. Zamani-Alavijeh F, Araban M, Koohestani HR, Karimy M. The effectiveness of stress management training on blood glucose control in patients with type 2 diabetes.
Diabetol Metab Syndr. Diabetic diet. Arnett DK, Blumenthal RS, Albert MA, et al. Prevention or delay of type 2 diabetes: S tandards of Medical Care in Diabetes Diabetes Care. By Angela Ryan Lee, MD Angela Ryan Lee, MD, is board-certified in cardiovascular diseases and internal medicine.
She is a fellow of the American College of Cardiology and holds board certifications from the American Society of Nuclear Cardiology and the National Board of Echocardiography.
She completed undergraduate studies at the University of Virginia with a B. in Biology, medical school at Jefferson Medical College, and internal medicine residency and cardiovascular diseases fellowship at the George Washington University Hospital.
Her professional interests include preventive cardiology, medical journalism, and health policy. Use limited data to select advertising. Create profiles for personalised advertising. Use profiles to select personalised advertising.
Create profiles to personalise content. Use profiles to select personalised content. Measure advertising performance. Measure content performance.
Understand audiences through statistics or combinations of data from different sources. Develop and improve services. Use limited data to select content. List of Partners vendors. Type 2 Diabetes. By Angela Ryan Lee, MD. Medically reviewed by Do-Eun Lee, MD. Table of Contents View All.
: Hyperglycemia and type diabetes| Hyperglycemia: Symptoms, Causes, and Treatments | You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest. Weight reduction through diet, exercise, and behavioral modification can all be used to improve glycemic management, although the majority of patients with type 2 diabetes will require medication. See 'Diabetes education' above. Glycemic targets are generally set somewhat higher for older adults and for those with comorbidities or a limited life expectancy and little likelihood of benefit from intensive therapy. See 'Glycemic management' above and "Glycemic control and vascular complications in type 2 diabetes mellitus", section on 'Choosing a glycemic target'. In the absence of specific contraindications, we suggest metformin as initial therapy for most patients Grade 2B. Although some guidelines and experts endorse the initial use of alternative agents as monotherapy or in combination with metformin, we prefer initiating a single agent typically metformin and then sequentially adding additional glucose-lowering agents as needed. See 'Metformin' above and 'Glycemic efficacy' above. We suggest initiating metformin at the time of diabetes diagnosis Grade 2C , along with consultation for lifestyle intervention. See 'When to start' above. The dose of metformin should be titrated to its maximally effective dose usually mg per day in divided doses over one to two months, as tolerated. See 'Contraindications to or intolerance of metformin' above. See 'Established cardiovascular or kidney disease' above. The majority of patients in the cardiovascular and renal outcomes trials had established cardiovascular disease CVD or diabetic kidney disease DKD with severely increased albuminuria, and therefore, these are the primary indications for one of these drugs. See 'Without established cardiovascular or kidney disease' above. Each one of these choices has individual advantages and risks table 1. Choice of medication is guided by efficacy, patient comorbidities, preferences, and cost. Sulfonylureas remain a highly effective treatment for hyperglycemia, particularly when cost is a barrier. Side effects of hypoglycemia and weight gain can be mitigated with careful dosing and diabetes self-management education. For patients who are injection averse, initial therapy with high-dose sulfonylurea is an alternative, particularly for patients who have been consuming large amounts of sugar-sweetened beverages, in whom elimination of carbohydrates can be anticipated to cause a reduction in glucose within several days. See 'Symptomatic catabolic or severe hyperglycemia' above and "Insulin therapy in type 2 diabetes mellitus". Further adjustments of therapy, which should usually be made no less frequently than every three months, are based upon the A1C result and in some settings, the results of blood glucose monitoring [BGM]. See 'Monitoring' above. See "Management of persistent hyperglycemia in type 2 diabetes mellitus" and "Insulin therapy in type 2 diabetes mellitus". Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Initial management of hyperglycemia in adults with type 2 diabetes mellitus. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Author: Deborah J Wexler, MD, MSc Section Editor: David M Nathan, MD Deputy Editor: Katya Rubinow, MD Contributor Disclosures. All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Dec 23, TREATMENT GOALS Glycemic management — Target glycated hemoglobin A1C levels in patients with type 2 diabetes should be tailored to the individual, balancing the anticipated reduction in microvascular complications over time with the immediate risks of hypoglycemia and other adverse effects of therapy. Summary of glucose-lowering interventions. UK Prospective Diabetes Study UKPDS Group. Lancet ; Holman RR, Paul SK, Bethel MA, et al. N Engl J Med ; Hayward RA, Reaven PD, Wiitala WL, et al. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. ADVANCE Collaborative Group, Patel A, MacMahon S, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, et al. Effects of intensive glucose lowering in type 2 diabetes. Rawshani A, Rawshani A, Franzén S, et al. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes. Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. Kazemian P, Shebl FM, McCann N, et al. Evaluation of the Cascade of Diabetes Care in the United States, JAMA Intern Med ; Pal K, Eastwood SV, Michie S, et al. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochrane Database Syst Rev ; :CD Saffari M, Ghanizadeh G, Koenig HG. Health education via mobile text messaging for glycemic control in adults with type 2 diabetes: a systematic review and meta-analysis. Prim Care Diabetes ; Liang X, Wang Q, Yang X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a meta-analysis. Diabet Med ; Henry RR, Scheaffer L, Olefsky JM. Glycemic effects of intensive caloric restriction and isocaloric refeeding in noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab ; Utzschneider KM, Carr DB, Barsness SM, et al. Diet-induced weight loss is associated with an improvement in beta-cell function in older men. Wing RR, Blair EH, Bononi P, et al. Caloric restriction per se is a significant factor in improvements in glycemic control and insulin sensitivity during weight loss in obese NIDDM patients. Diabetes Care ; Lean ME, Leslie WS, Barnes AC, et al. Primary care-led weight management for remission of type 2 diabetes DiRECT : an open-label, cluster-randomised trial. Delahanty LM. The look AHEAD study: implications for clinical practice go beyond the headlines. J Acad Nutr Diet ; Evert AB, Dennison M, Gardner CD, et al. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. Lean MEJ, Leslie WS, Barnes AC, et al. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol ; Niskanen LK, Uusitupa MI, Sarlund H, et al. Five-year follow-up study on plasma insulin levels in newly diagnosed NIDDM patients and nondiabetic subjects. Norris SL, Zhang X, Avenell A, et al. Long-term effectiveness of lifestyle and behavioral weight loss interventions in adults with type 2 diabetes: a meta-analysis. Am J Med ; United Kingdom Prospective Diabetes Study UKPDS. BMJ ; Umpierre D, Ribeiro PA, Kramer CK, et al. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: a systematic review and meta-analysis. JAMA ; Jeon CY, Lokken RP, Hu FB, van Dam RM. Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Egan AM, Mahmood WA, Fenton R, et al. Barriers to exercise in obese patients with type 2 diabetes. QJM ; American Diabetes Association Professional Practice Committee. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes Diabetes Care ; S Kobayashi Y, Long J, Dan S, et al. Strength training is more effective than aerobic exercise for improving glycaemic control and body composition in people with normal-weight type 2 diabetes: a randomised controlled trial. Diabetologia ; Look AHEAD Research Group, Wing RR, Bolin P, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. Pillay J, Armstrong MJ, Butalia S, et al. Behavioral Programs for Type 2 Diabetes Mellitus: A Systematic Review and Network Meta-analysis. Ann Intern Med ; Johansen MY, MacDonald CS, Hansen KB, et al. Effect of an Intensive Lifestyle Intervention on Glycemic Control in Patients With Type 2 Diabetes: A Randomized Clinical Trial. Lingvay I, Sumithran P, Cohen RV, le Roux CW. Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Look AHEAD Research Group, Pi-Sunyer X, Blackburn G, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Arterburn DE, O'Connor PJ. A look ahead at the future of diabetes prevention and treatment. Look AHEAD Research Group, Gregg EW, Jakicic JM, et al. Association of the magnitude of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: a post-hoc analysis of the Look AHEAD randomised clinical trial. Look AHEAD Research Group. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity Silver Spring ; Look AHEAD Research Group, Wing RR. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med ; Gregg EW, Chen H, Wagenknecht LE, et al. Association of an intensive lifestyle intervention with remission of type 2 diabetes. Jakicic JM, Egan CM, Fabricatore AN, et al. Four-year change in cardiorespiratory fitness and influence on glycemic control in adults with type 2 diabetes in a randomized trial: the Look AHEAD Trial. Kuna ST, Reboussin DM, Borradaile KE, et al. Long-term effect of weight loss on obstructive sleep apnea severity in obese patients with type 2 diabetes. Sleep ; Wing RR, Bond DS, Gendrano IN 3rd, et al. Effect of intensive lifestyle intervention on sexual dysfunction in women with type 2 diabetes: results from an ancillary Look AHEAD study. html Accessed on July 18, Effect of a long-term behavioural weight loss intervention on nephropathy in overweight or obese adults with type 2 diabetes: a secondary analysis of the Look AHEAD randomised clinical trial. Surwit RS, van Tilburg MA, Zucker N, et al. Stress management improves long-term glycemic control in type 2 diabetes. Ismail K, Winkley K, Rabe-Hesketh S. Systematic review and meta-analysis of randomised controlled trials of psychological interventions to improve glycaemic control in patients with type 2 diabetes. Safren SA, Gonzalez JS, Wexler DJ, et al. A randomized controlled trial of cognitive behavioral therapy for adherence and depression CBT-AD in patients with uncontrolled type 2 diabetes. Williams JW Jr, Katon W, Lin EH, et al. The effectiveness of depression care management on diabetes-related outcomes in older patients. Colagiuri S, Cull CA, Holman RR, UKPDS Group. Are lower fasting plasma glucose levels at diagnosis of type 2 diabetes associated with improved outcomes? prospective diabetes study Choi JG, Winn AN, Skandari MR, et al. First-Line Therapy for Type 2 Diabetes With Sodium-Glucose Cotransporter-2 Inhibitors and Glucagon-Like Peptide-1 Receptor Agonists : A Cost-Effectiveness Study. Abdul-Ghani MA, Puckett C, Triplitt C, et al. Initial combination therapy with metformin, pioglitazone and exenatide is more effective than sequential add-on therapy in subjects with new-onset diabetes. Results from the Efficacy and Durability of Initial Combination Therapy for Type 2 Diabetes EDICT : a randomized trial. Diabetes Obes Metab ; Hong J, Zhang Y, Lai S, et al. Effects of metformin versus glipizide on cardiovascular outcomes in patients with type 2 diabetes and coronary artery disease. Kooy A, de Jager J, Lehert P, et al. Long-term effects of metformin on metabolism and microvascular and macrovascular disease in patients with type 2 diabetes mellitus. Maruthur NM, Tseng E, Hutfless S, et al. Diabetes Medications as Monotherapy or Metformin-Based Combination Therapy for Type 2 Diabetes: A Systematic Review and Meta-analysis. Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes Jia W, Weng J, Zhu D, et al. Standards of medical care for type 2 diabetes in China Diabetes Metab Res Rev ; e Marso SP, Bain SC, Consoli A, et al. Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. Mann JFE, Ørsted DD, Brown-Frandsen K, et al. Liraglutide and Renal Outcomes in Type 2 Diabetes. Gerstein HC, Colhoun HM, Dagenais GR, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes REWIND : a double-blind, randomised placebo-controlled trial. Dulaglutide and renal outcomes in type 2 diabetes: an exploratory analysis of the REWIND randomised, placebo-controlled trial. Kanie T, Mizuno A, Takaoka Y, et al. Dipeptidyl peptidase-4 inhibitors, glucagon-like peptide 1 receptor agonists and sodium-glucose co-transporter-2 inhibitors for people with cardiovascular disease: a network meta-analysis. Cochrane Database Syst Rev ; CD Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in Patients with Chronic Kidney Disease. Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. de Boer IH, Khunti K, Sadusky T, et al. Diabetes Management in Chronic Kidney Disease: A Consensus Report by the American Diabetes Association ADA and Kidney Disease: Improving Global Outcomes KDIGO. Shyangdan DS, Royle P, Clar C, et al. Glucagon-like peptide analogues for type 2 diabetes mellitus. Singh S, Wright EE Jr, Kwan AY, et al. Glucagon-like peptide-1 receptor agonists compared with basal insulins for the treatment of type 2 diabetes mellitus: a systematic review and meta-analysis. Davidson MB. Successful treatment of markedly symptomatic patients with type II diabetes mellitus using high doses of sulfonylurea agents. West J Med ; pdf Accessed on April 21, Palmer SC, Mavridis D, Nicolucci A, et al. Comparison of Clinical Outcomes and Adverse Events Associated With Glucose-Lowering Drugs in Patients With Type 2 Diabetes: A Meta-analysis. Tsapas A, Avgerinos I, Karagiannis T, et al. Comparative Effectiveness of Glucose-Lowering Drugs for Type 2 Diabetes: A Systematic Review and Network Meta-analysis. Kahn SE, Haffner SM, Heise MA, et al. Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. Nathan DM. Thiazolidinediones for initial treatment of type 2 diabetes? Qaseem A, Barry MJ, Humphrey LL, et al. Oral Pharmacologic Treatment of Type 2 Diabetes Mellitus: A Clinical Practice Guideline Update From the American College of Physicians. Davies MJ, Aroda VR, Collins BS, et al. Management of hyperglycaemia in type 2 diabetes, A consensus report by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a specific patient. It is not intended to be medical advice or a substitute for the medical advice, diagnosis, or treatment of a health care provider based on the health care provider's examination and assessment of a patient's specific and unique circumstances. Patients must speak with a health care provider for complete information about their health, medical questions, and treatment options, including any risks or benefits regarding use of medications. This information does not endorse any treatments or medications as safe, effective, or approved for treating a specific patient. UpToDate, Inc. and its affiliates disclaim any warranty or liability relating to this information or the use thereof. All rights reserved. Topic Feedback. Initiation and adjustment of insulin regimens in type 2 diabetes mellitus. Intensive glycemic control prevents severe microvascular disease in patients with type 2 diabetes Initial fasting blood glucose concentration determines degree of weight loss required to achieve normoglycemia in type 2 diabetes. Hyperglycemia occurs when the level of blood glucose gets too high. If left untreated for a long period of time, it can lead to serious complications, such as eye damage, kidney problems, and heart disease, among others. Fortunately, treatments are available that can help prevent hyperglycemia and control blood glucose levels. Hyperglycemia is a condition in which the level of glucose in the blood is higher than normal. Glucose is the primary source of energy for all cells in our bodies. It comes from the foods we eat, especially carbohydrates. When food reaches the stomach, it is broken down into different parts—one of which is glucose. The intestines absorb the glucose, which then enters the bloodstream and circulates around the body. Normally, the body uses a hormone called insulin to move glucose from the blood into cells, thereby lowering glucose in the blood and providing cells with energy. Hyperglycemia can occur when the body does not produce enough insulin or does not respond to insulin correctly. In both cases, glucose stays in the blood instead of being sent to the cells, and as a result, blood glucose levels remain elevated. If more glucose enters the bloodstream—if you eat carbohydrate-rich food, for example—the blood glucose levels climb even higher. In some cases, people with diabetes who have hyperglycemia can develop a complication called diabetic ketoacidosis DKA. In this condition, the cells cannot access glucose. Instead, the body gets energy by breaking down fats. This process produces compounds called ketones, which build up in the blood, causing it to become acidic. DKA is a life-threatening condition. DKA is most commonly associated with type 1 diabetes , but can occur in people with type 2 as well. In people with type 2 diabetes , very high blood glucose levels can lead to a life-threatening condition called hyperosmolar hyperglycemic state HHS , which causes profound dehydration and a change in mental status. Hyperglycemia most commonly affects people who have diabetes. In type 1 diabetes, the body does not make enough insulin. In type 2 diabetes, the body makes an adequate amount of insulin, but the cells do not respond to it properly. This is called insulin resistance. A diagnosis of hyperglycemia usually involves a review of your medical history, a physical exam, and blood tests. The doctor will ask about your symptoms and whether you have a family history of diabetes or other risk factors associated with hyperglycemia. He or she will conduct a physical exam. Ultimately, though, blood tests that measure blood glucose levels are necessary to definitively diagnose hyperglycemia. Other blood tests may include a hemoglobin A1C test also known as glycated hemoglobin test and an oral glucose tolerance test OGTT. DKA and HHS are medical emergencies. They are treated with intravenous fluids, electrolytes, and insulin. |
| Hyperglycemia in diabetes - Diagnosis & treatment - Mayo Clinic | If the blood sugar level goes above that range, they have hyperglycemia hi-per-gly-SEE-mee-uh. This leads to high glucose in the blood. Glucose is a type of sugar that comes from food. When someone has diabetes, they have a problem with insulin. A person with type 1 diabetes can't make insulin. Blood sugar levels can get higher than normal for different reasons. But treatment for hyperglycemia is always the same: Follow the diet and exercise plan and give insulin or other medicines on schedule. In the short term, high blood sugars can turn into diabetic ketoacidosis DKA. This is an emergency condition that needs treatment right away. DKA can happen to kids with type 1 diabetes and, less often, kids with type 2 diabetes. Kids with type 2 diabetes also can get another type of emergency called hyperosmotic hyperglycemic state HHS. Both conditions need treatment in the hospital and are very serious. Untreated hyperglycemia can lead to serious health problems later in life. If it happens a lot, it can harm blood vessels, the heart, kidneys, eyes, and nerves. To prevent hyperglycemia, check blood sugars often and follow the care plan to keep them in the healthy range. Teach your child to do this, so they can take on this responsibility as they grow. Dosing in the setting of DKD is reviewed in detail elsewhere. See "Treatment of diabetic kidney disease", section on 'Type 2 diabetes: Treat with additional kidney-protective therapy'. An alternative or an additional agent may be necessary to achieve glycemic goals. GLP-1 receptor agonists are an alternative in patients with DKD as their glycemic effect is not related to eGFR. In addition, GLP-1 receptor agonists have been shown to slow the rate of decline in eGFR and prevent worsening of albuminuria. See 'Microvascular outcomes' below and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus" and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus". Of note, we avoid use of SGLT2 inhibitors in patients with frequent bacterial urinary tract infections or genitourinary yeast infections, low bone density and high risk for falls and fractures, foot ulceration, and factors predisposing to diabetic ketoacidosis eg, pancreatic insufficiency, drug or alcohol abuse disorder because of increased risk while using these agents. SLGT2 inhibitors should be held for 3 to 4 days before procedures including colonoscopy preparation and with poor oral intake to prevent diabetic ketoacidosis. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Contraindications and precautions'. Repaglinide acts at the sulfonylurea receptor to increase insulin secretion but is much shorter acting than sulfonylureas and is principally metabolized by the liver, with less than 10 percent renally excreted. Limited data suggest that dipeptidyl peptidase 4 DPP-4 inhibitors are effective and relatively safe in patients with chronic kidney disease. However, linagliptin is the only DPP-4 inhibitor that does not require a dose adjustment in the setting of kidney failure. GLP-1 receptor agonists may also be used safely in chronic kidney disease stage 4, but patient education for signs and symptoms of dehydration due to nausea or satiety is warranted to reduce the risk of acute kidney injury. Insulin may also be used, with a greater portion of the total daily dose administered during the day due to the risk of hypoglycemia, especially overnight, in chronic kidney disease and end-stage kidney disease ESKD. See "Management of hyperglycemia in patients with type 2 diabetes and advanced chronic kidney disease or end-stage kidney disease", section on 'Patients not on dialysis'. Without established cardiovascular or kidney disease — For patients without established CVD or kidney disease who cannot take metformin , many other options for initial therapy are available table 1. We suggest choosing an alternative glucose-lowering medication guided by efficacy, patient comorbidities, preferences, and cost. Although historically insulin has been used for type 2 diabetes only when inadequate glycemic management persists despite oral agents and lifestyle intervention, there are increasing data to support using insulin earlier and more aggressively in type 2 diabetes. By inducing near normoglycemia with intensive insulin therapy, both endogenous insulin secretion and insulin sensitivity improve; this results in better glycemic management, which can then be maintained with diet, exercise, and oral hypoglycemics for many months thereafter. Insulin may cause weight gain and hypoglycemia. See "Insulin therapy in type 2 diabetes mellitus", section on 'Indications for insulin'. If type 1 diabetes has been excluded, a GLP-1 receptor agonist is a reasonable alternative to insulin [ 66,67 ]. The frequency of injections and proved beneficial effects in the setting of CVD are the major differences among the many available GLP-1 receptor agonists. In practice, given the high cost of this class of medications, formulary coverage often determines the choice of the first medication within the class. Cost and insurance coverage may limit accessibility and adherence. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Patient selection'. Each one of these choices has individual advantages, benefits, and risks table 1. See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus" and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Patient selection' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Patient selection' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Potential indications'. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Weight loss' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Patient selection' and "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Weight loss'. The choice of sulfonylurea balances glucose-lowering efficacy, universal availability, and low cost with risk of hypoglycemia and weight gain. Pioglitazone , which is generic and another relatively low-cost oral agent, may also be considered in patients with specific contraindications to metformin and sulfonylureas. However, the risk of weight gain, HF, fractures, and the potential increased risk of bladder cancer raise the concern that the overall risks and cost of pioglitazone may approach or exceed its benefits. See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus" and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Potential indications'. For patients who are starting sulfonylureas, we suggest initiating lifestyle intervention first, at the time of diagnosis, since the weight gain that often accompanies a sulfonylurea will presumably be less if lifestyle efforts are underway. However, if lifestyle intervention has not produced a significant reduction in symptoms of hyperglycemia or in glucose values after one or two weeks, then the sulfonylurea should be added. Side effects may be minimized with diabetes self-management education focusing on medication reduction or omission with changes in diet, food accessibility, or activity that may increase the risk of hypoglycemia. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Suggested approach to the use of GLP-1 receptor agonist-based therapies' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Mechanism of action' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Mechanism of action' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Hypoglycemia'. Symptomatic catabolic or severe hyperglycemia — The frequency of symptomatic or severe diabetes has been decreasing in parallel with improved efforts to diagnose diabetes earlier through screening. If patients have been drinking a substantial quantity of sugar-sweetened beverages, reduction of carbohydrate intake, and rehydration with sugar-free fluids will help to reduce glucose levels within several days. See "Insulin therapy in type 2 diabetes mellitus", section on 'Initial treatment'. However, for patients who are injection averse, initial therapy with high-dose sulfonylurea is an alternative option. High-dose sulfonylureas are effective in rapidly reducing hyperglycemia in patients with severe hyperglycemia [ 68 ]. Metformin monotherapy is not helpful in improving symptoms in this setting, because the initial dose is low and increased over several weeks. However, metformin can be started at the same time as the sulfonylurea, slowly titrating the dose upward. Once the diet has been adequately modified and the metformin dose increased, the dose of sulfonylurea can be reduced and potentially discontinued. Patients with type 2 diabetes require relatively high doses of insulin compared with those needed for type 1 diabetes. Insulin preparations, insulin regimens, and timing of dosing are discussed in detail elsewhere. See "Insulin therapy in type 2 diabetes mellitus". See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Administration'. We typically use glimepiride 4 or 8 mg once daily. An alternative option is immediate-release glipizide 10 mg twice daily or, where available, gliclazide immediate-release 80 mg daily. We contact the patient every few days after initiating therapy to make dose adjustments increase dose if hyperglycemia does not improve or decrease dose if hyperglycemia resolves quickly or hypoglycemia develops. See "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Sulfonylureas'. Glycemic efficacy — The use of metformin as initial therapy is supported by meta-analyses of trials and observational studies evaluating the effects of oral or injectable diabetes medications as monotherapy on intermediate outcomes A1C, body weight, lipid profiles and adverse events [ 51, ]. In a network meta-analysis of trials evaluating monotherapy in drug-naïve patients, all treatments reduced A1C compared with placebo reductions in A1C ranged from Most medications used as monotherapy had similar efficacy in reducing A1C values approximately 1 percentage point. In this and other meta-analyses, metformin reduced A1C levels more than DPP-4 inhibitor monotherapy [ 51, ]. There are few high-quality, head-to-head comparison trials of the available oral agents. In one such trial, A Diabetes Outcome Progression Trial ADOPT , recently diagnosed patients with type 2 diabetes were randomly assigned to monotherapy with the thiazolidinedione rosiglitazone , metformin , or glyburide [ 72 ]. At the four-year evaluation, 40 percent of the subjects in the rosiglitazone group had an A1C value less than 7 percent, as compared with 36 percent in the metformin group and 26 percent in the glyburide group. Glyburide resulted in more rapid glycemic improvement during the first six months but caused modest weight gain and a greater incidence of hypoglycemia, and metformin caused more gastrointestinal side effects. Rosiglitazone caused greater increases in weight, peripheral edema, and concentrations of low-density lipoprotein LDL cholesterol. There was also an unexpected increase in fractures in women taking rosiglitazone. The study was limited by a high rate of withdrawal of study participants. Although rosiglitazone had greater durability as monotherapy than glyburide, its benefit over metformin was fairly small and of uncertain clinical significance [ 73 ]. See "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Safety'. Cardiovascular outcomes — Cardiovascular benefit has been demonstrated for selected classes of diabetes medications, usually when added to metformin. See "Management of persistent hyperglycemia in type 2 diabetes mellitus", section on 'Monotherapy failure'. The cardiovascular effects of diabetes drugs are reviewed in the individual topics. See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Thiazolidinediones in the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Dipeptidyl peptidase 4 DPP-4 inhibitors for the treatment of type 2 diabetes mellitus", section on 'Cardiovascular effects' and "Insulin therapy in type 2 diabetes mellitus". In trials of patients with type 2 diabetes with and without chronic kidney disease, GLP-1 receptor agonists slowed the rate of decline in eGFR and prevented worsening of albuminuria [ 54,56,58 ]. These trials and other trials evaluating microvascular outcomes are reviewed in the individual topics. Guidelines — Our approach is largely consistent with American and European guidelines [ 52,74,75 ]. A consensus statement regarding the management of hyperglycemia in type 2 diabetes by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD was developed in and has been updated regularly, with the most recent revision published in [ 75 ]. The guidelines emphasize the importance of individualizing the choice of medications for the treatment of diabetes, considering important comorbidities CVD, HF, or chronic kidney disease; hypoglycemia risk; and need for weight loss and patient-specific factors including patient preferences, values, and cost [ 75 ]. We also agree with the World Health Organization WHO that sulfonylureas have a long-term safety profile, are inexpensive, and are highly effective, especially when used as described above, with patient education and dose adjustment to minimize side effects [ 76 ]. Blood glucose monitoring BGM is not necessary for most patients with type 2 diabetes who are on a stable regimen of diet or oral agents and who are not experiencing hypoglycemia. BGM may be useful for some patients with type 2 diabetes who use the results to modify eating patterns, exercise, or insulin doses on a regular basis. See "Glucose monitoring in the ambulatory management of nonpregnant adults with diabetes mellitus", section on 'Type 2 diabetes'. The balance among efficacy in lowering A1C, side effects, and costs must be carefully weighed in considering which drugs or combinations to choose. Avoiding insulin, the most potent of all hypoglycemic medications, at the expense of poorer glucose management and greater side effects and cost, is not likely to benefit the patient in the long term. See "Management of persistent hyperglycemia in type 2 diabetes mellitus", section on 'Our approach'. SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. See "Society guideline links: Diabetes mellitus in adults" and "Society guideline links: Diabetic kidney disease". These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon. Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest. Weight reduction through diet, exercise, and behavioral modification can all be used to improve glycemic management, although the majority of patients with type 2 diabetes will require medication. See 'Diabetes education' above. Glycemic targets are generally set somewhat higher for older adults and for those with comorbidities or a limited life expectancy and little likelihood of benefit from intensive therapy. See 'Glycemic management' above and "Glycemic control and vascular complications in type 2 diabetes mellitus", section on 'Choosing a glycemic target'. In the absence of specific contraindications, we suggest metformin as initial therapy for most patients Grade 2B. Although some guidelines and experts endorse the initial use of alternative agents as monotherapy or in combination with metformin, we prefer initiating a single agent typically metformin and then sequentially adding additional glucose-lowering agents as needed. See 'Metformin' above and 'Glycemic efficacy' above. We suggest initiating metformin at the time of diabetes diagnosis Grade 2C , along with consultation for lifestyle intervention. See 'When to start' above. The dose of metformin should be titrated to its maximally effective dose usually mg per day in divided doses over one to two months, as tolerated. See 'Contraindications to or intolerance of metformin' above. See 'Established cardiovascular or kidney disease' above. The majority of patients in the cardiovascular and renal outcomes trials had established cardiovascular disease CVD or diabetic kidney disease DKD with severely increased albuminuria, and therefore, these are the primary indications for one of these drugs. See 'Without established cardiovascular or kidney disease' above. Each one of these choices has individual advantages and risks table 1. Choice of medication is guided by efficacy, patient comorbidities, preferences, and cost. Sulfonylureas remain a highly effective treatment for hyperglycemia, particularly when cost is a barrier. Side effects of hypoglycemia and weight gain can be mitigated with careful dosing and diabetes self-management education. For patients who are injection averse, initial therapy with high-dose sulfonylurea is an alternative, particularly for patients who have been consuming large amounts of sugar-sweetened beverages, in whom elimination of carbohydrates can be anticipated to cause a reduction in glucose within several days. See 'Symptomatic catabolic or severe hyperglycemia' above and "Insulin therapy in type 2 diabetes mellitus". Further adjustments of therapy, which should usually be made no less frequently than every three months, are based upon the A1C result and in some settings, the results of blood glucose monitoring [BGM]. See 'Monitoring' above. See "Management of persistent hyperglycemia in type 2 diabetes mellitus" and "Insulin therapy in type 2 diabetes mellitus". Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Initial management of hyperglycemia in adults with type 2 diabetes mellitus. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Author: Deborah J Wexler, MD, MSc Section Editor: David M Nathan, MD Deputy Editor: Katya Rubinow, MD Contributor Disclosures. All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Dec 23, TREATMENT GOALS Glycemic management — Target glycated hemoglobin A1C levels in patients with type 2 diabetes should be tailored to the individual, balancing the anticipated reduction in microvascular complications over time with the immediate risks of hypoglycemia and other adverse effects of therapy. Summary of glucose-lowering interventions. UK Prospective Diabetes Study UKPDS Group. Lancet ; Holman RR, Paul SK, Bethel MA, et al. N Engl J Med ; Hayward RA, Reaven PD, Wiitala WL, et al. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. ADVANCE Collaborative Group, Patel A, MacMahon S, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, et al. Effects of intensive glucose lowering in type 2 diabetes. Rawshani A, Rawshani A, Franzén S, et al. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes. Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. Kazemian P, Shebl FM, McCann N, et al. Evaluation of the Cascade of Diabetes Care in the United States, JAMA Intern Med ; Pal K, Eastwood SV, Michie S, et al. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochrane Database Syst Rev ; :CD Saffari M, Ghanizadeh G, Koenig HG. Health education via mobile text messaging for glycemic control in adults with type 2 diabetes: a systematic review and meta-analysis. Prim Care Diabetes ; Liang X, Wang Q, Yang X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a meta-analysis. Diabet Med ; Henry RR, Scheaffer L, Olefsky JM. Glycemic effects of intensive caloric restriction and isocaloric refeeding in noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab ; Utzschneider KM, Carr DB, Barsness SM, et al. Diet-induced weight loss is associated with an improvement in beta-cell function in older men. Wing RR, Blair EH, Bononi P, et al. Caloric restriction per se is a significant factor in improvements in glycemic control and insulin sensitivity during weight loss in obese NIDDM patients. Diabetes Care ; Lean ME, Leslie WS, Barnes AC, et al. Primary care-led weight management for remission of type 2 diabetes DiRECT : an open-label, cluster-randomised trial. Delahanty LM. The look AHEAD study: implications for clinical practice go beyond the headlines. J Acad Nutr Diet ; Evert AB, Dennison M, Gardner CD, et al. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. Lean MEJ, Leslie WS, Barnes AC, et al. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol ; Niskanen LK, Uusitupa MI, Sarlund H, et al. Five-year follow-up study on plasma insulin levels in newly diagnosed NIDDM patients and nondiabetic subjects. Norris SL, Zhang X, Avenell A, et al. Long-term effectiveness of lifestyle and behavioral weight loss interventions in adults with type 2 diabetes: a meta-analysis. Am J Med ; United Kingdom Prospective Diabetes Study UKPDS. BMJ ; Umpierre D, Ribeiro PA, Kramer CK, et al. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: a systematic review and meta-analysis. JAMA ; Jeon CY, Lokken RP, Hu FB, van Dam RM. Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Egan AM, Mahmood WA, Fenton R, et al. Barriers to exercise in obese patients with type 2 diabetes. QJM ; American Diabetes Association Professional Practice Committee. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes Diabetes Care ; S Kobayashi Y, Long J, Dan S, et al. Strength training is more effective than aerobic exercise for improving glycaemic control and body composition in people with normal-weight type 2 diabetes: a randomised controlled trial. Diabetologia ; Look AHEAD Research Group, Wing RR, Bolin P, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. Pillay J, Armstrong MJ, Butalia S, et al. Behavioral Programs for Type 2 Diabetes Mellitus: A Systematic Review and Network Meta-analysis. Ann Intern Med ; Johansen MY, MacDonald CS, Hansen KB, et al. Effect of an Intensive Lifestyle Intervention on Glycemic Control in Patients With Type 2 Diabetes: A Randomized Clinical Trial. Lingvay I, Sumithran P, Cohen RV, le Roux CW. Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Look AHEAD Research Group, Pi-Sunyer X, Blackburn G, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Arterburn DE, O'Connor PJ. A look ahead at the future of diabetes prevention and treatment. Look AHEAD Research Group, Gregg EW, Jakicic JM, et al. Association of the magnitude of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: a post-hoc analysis of the Look AHEAD randomised clinical trial. Look AHEAD Research Group. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity Silver Spring ; Look AHEAD Research Group, Wing RR. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med ; Gregg EW, Chen H, Wagenknecht LE, et al. Association of an intensive lifestyle intervention with remission of type 2 diabetes. Jakicic JM, Egan CM, Fabricatore AN, et al. Four-year change in cardiorespiratory fitness and influence on glycemic control in adults with type 2 diabetes in a randomized trial: the Look AHEAD Trial. |
| The link between hyperglycemia and diabetes | Responsible energy consumption surgery is Hypergglycemia effective in improving glucose control — and often produces disease remission duabetes Lifestyle Responsible energy consumption intervention outcomes thpe overweight and obese adults with appetite suppression techniques 2 diabetes: a systematic review and meta-analysis of randomized clinical trials. It has become common practice to approach insulin use in people with type 2 diabetes by following the established paradigms developed for those with type 1 diabetes. Diabetes Care 1 December ; 41 12 : — Many types of inputs can be digitalized, such as blood glucose levels, time spent exercising, steps walked, energy ingested, medication doses administered, blood pressure, and weight. |
| Hyperglycemia | Lowering blood sugar can decrease the risk of complications. Some people are even able to put diabetes into remission and come off blood sugar—lowering medication with these steps. A healthy lifestyle can help lower blood sugar and control type 2 diabetes. This can include the following;. Diet is a major contributor to blood sugar control, and fortunately, it's something we have a great deal of control over to help get blood sugar under control. For people with diabetes, eating meals with low glycemic load low ability to raise blood sugar can help prevent hyperglycemia. People with diabetes should consider the following when planning meals:. If you have type 2 diabetes, your healthcare provider will recommend blood sugar—lowering medication to help get hyperglycemia under control. There are many different types of oral medications to lower blood sugar. Your healthcare provider will work with you to find a medication that you tolerate and is effective for you. It's essential to adhere to the medication plan laid out by your healthcare provider and avoid missing doses. If oral medications and dietary and lifestyle changes are not enough to bring blood sugar down, your healthcare provider may recommend injectable medications or insulin. If you are prescribed insulin, checking your blood sugar at home will be important. In addition to the blood sugar—lowering medication, your healthcare provider may recommend other drugs to lower blood pressure, cholesterol, and lower cardiovascular disease risk. You can think of blood sugar as a range form normal to prediabetes to diabetes. It can take years for diabetes to develop, but in the meantime with screening, you can uncover prediabetes and initiate changes to decrease your risk of developing type 2 diabetes. Lifestyle and dietary changes can also be implemented to prevent a diagnosis of diabetes. Additionally, when prediabetes is diagnosed and you are at a higher risk of developing type 2 diabetes, your healthcare provider may prescribe a medication called Glucophage metformin. Hyperglycemia, or elevated blood sugar, is a part of type 2 diabetes that can result in complications affecting various organs and increased risk of heart disease. While you may not be able to control all risk factors for type 2 diabetes, you can help prevent it through a healthy lifestyle and diet. Treatment of diabetes involves the same steps as prevention, in addition to medication to lower blood sugar to prevent complications. Chronically high blood sugar, as in type 2 diabetes, damages tissues and organs, including nerves, eyes, kidneys, and blood vessels. Lowering blood sugar to prevent these complications is a major goal of treatment in type 2 diabetes. Having prediabetes increases your risk of developing diabetes later on. However, identifying prediabetes early can allow you to initiate strategies to prevent diabetes. Both in the short term and long term, hyperglycemia in type 2 diabetes can be dangerous. In the short term, extremely high blood sugar levels can lead to a life-threatening state called hyperglycemic hyperosmolar syndrome HHS , which is characterized by high blood sugar levels, dehydration, abdominal pain, nausea, and confusion or coma. In the long term, chronically high blood sugar damages organs in your body from the nerves to the kidneys, eyes, and blood vessels. National Institute of Diabetes and Digestive and Kidney Diseases. What is diabetes? Insulin resistance and prediabetes. Centers for Disease Control and Prevention. Type 2 diabetes. American Diabetes Association. Hyperglycemia high blood glucose. Diabetic hyperglycemic hyperosmolar syndrome. Diabetes risk factors. Prevent diabetes complications. Mottalib A, Sakr M, Shehabeldin M, Hamdy O. Diabetes remission after nonsurgical intensive lifestyle intervention in obese patients with type 2 diabetes. J Diabetes Res. Janbozorgi N, Allipour R, Djafarian K, Shab-Bidar S, Badeli M, Safabakhsh M. Water intake and risk of type 2 diabetes: A systematic review and meta-analysis of observational studies. Diabetes Metab Syndr. Zhu B, Hershberger PE, Kapella MC, Fritschi C. The relationship between sleep disturbance and glycaemic control in adults with type 2 diabetes: An integrative review. J Clin Nurs. Zamani-Alavijeh F, Araban M, Koohestani HR, Karimy M. The effectiveness of stress management training on blood glucose control in patients with type 2 diabetes. Diabetol Metab Syndr. Diabetic diet. Arnett DK, Blumenthal RS, Albert MA, et al. Prevention or delay of type 2 diabetes: S tandards of Medical Care in Diabetes Diabetes Care. By Angela Ryan Lee, MD Angela Ryan Lee, MD, is board-certified in cardiovascular diseases and internal medicine. She is a fellow of the American College of Cardiology and holds board certifications from the American Society of Nuclear Cardiology and the National Board of Echocardiography. She completed undergraduate studies at the University of Virginia with a B. in Biology, medical school at Jefferson Medical College, and internal medicine residency and cardiovascular diseases fellowship at the George Washington University Hospital. Her professional interests include preventive cardiology, medical journalism, and health policy. Use limited data to select advertising. Create profiles for personalised advertising. Typically, a co-occurring illness such as infection or stroke causes hyperglycemic hyperosmolar syndrome in diabetes. Developing hyperglycemia as a result of uncontrolled diabetes can cause serious long-term complications. They may include:. A person can monitor their blood sugar at home with the help of a fingerstick or a continuous glucose monitoring system. An A1C test is a blood test that indicates average blood sugar control during the previous 3 months. The A1C test works by measuring the percentage of glucose in the bloodstream that has bound to hemoglobin, which is the oxygen-carrying protein in red blood cells. A score of higher than 6. The American Diabetes Association suggest the following blood sugar targets for most adults with diabetes who are not pregnant:. Ranges can vary depending on age and any underlying medical conditions, such as a heart, lung, or kidney disease. Ranges also vary for people who are pregnant or experiencing complications from diabetes. All people with diabetes should use a glucose meter to monitor blood sugar at home and make sure they stay within their goal range. Home monitoring allows people to quickly notice any potentially harmful changes and immediately report problems to a physician. Over-the-counter urinary ketone level test kits are also available to determine the presence of DKA. If a person is experiencing any of the symptoms above, getting a positive test means that their body may be in the early stages of DKA, and they should consider seeking treatment immediately. A doctor can adjust the drug regimen accordingly for a person with diabetes who is also experiencing symptoms of hyperglycemia. Visiting the emergency room might be necessary if certain symptoms occur or do not resolve, including:. As well as talking to a doctor about managing their blood sugar levels, people can take the following steps to help avoid hyperglycemia:. People with diabetes must keep track of their blood sugar, stay within their target levels, follow a dedicated eating plan, exercise, and always take their medicine. They should report any abnormal symptoms to their doctor. This can help people with diabetes prevent hyperglycemia and receive early treatment with a view to preventing long-term complications. Many types of diet can benefit people with diabetes. Eating carbohydrates, for example, directly impacts blood sugars, so doctors recommend a carb-controlled diet. Ketogenic diets have become popular, as they lead to rapid weight loss. However, they may have some negative health effects, so individuals should talk to their doctor before beginning any extreme diet. Deborah Weatherspoon, PhD, RN, CRNA Answers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice. Hyperglycemia, or high blood sugar, can affect people with type 1 and type 2 diabetes. Learn about the symptoms, who is at risk, and when to consult a…. A person can manage their diabetes by making healthful changes to their diet, exercising frequently, and regularly taking the necessary medications…. People with diabetes benefit from strategically balancing their diets. In this article, we describe some of the best foods to eat and which types to…. A study in mice suggests a potential mechanism that could explain why only some individuals with obesity develop type 2 diabetes. A type of medication used to treat type 2 diabetes could help lower the risk of developing kidney stones, a new study suggests. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us. Medical News Today. Health Conditions Health Products Discover Tools Connect. The link between hyperglycemia and diabetes. Medically reviewed by Deborah Weatherspoon, Ph. Hyperglycemia and diabetes Causes Symptoms Diagnosis Treatments Summary Hyperglycemia, or high blood glucose, is a symptom that characterizes diabetes. Hyperglycemia and diabetes. Share on Pinterest People with diabetes have consistently high blood sugar and ongoing monitoring is often necessary. Share on Pinterest Blurred vision is a symptom of severe hyperglycemia. Share on Pinterest A range of blood glucose tests can help a doctor diagnose diabetes. Q: What is the best diet for keeping blood sugar within a normal range? A: Many types of diet can benefit people with diabetes. Was this helpful? How we reviewed this article: Sources. Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations. We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles. |
| Hyperglycemia and Diabetes (for Parents) - Nemours KidsHealth | When a person living with type 2 diabetes is sick or has a blood sugar reading of milligrams per deciliter or higher, the CDC recommends getting a home ketone test kit and testing every 4—6 hours. Patients often prefer combinations of oral medications to injectable medications. Hyperglycemia and Diabetes Nemours Foundation When Blood Sugar Is Too High Nemours Foundation Also in Spanish. Recommended Process for Glucose-Lowering Medication Selection: Where Does New Evidence From Cardiovascular Outcomes Trials Fit In? Vegetarian eating patterns have been shown to lower HbA 1c , but not fasting glucose, compared with nonvegetarian ones Urgent attention to improve prevention and treatment is of the essence. |
Leichter auf den Wendungen!
Welche Frechheit!
Ich verstehe nicht
Ich meine, dass Sie den Fehler zulassen.
Wacker, mir scheint es, es ist die prächtige Phrase