
Video
What is a DEXA bone scan and what does it show? Erin Eatung, MD scwn Philip S. Mehler, MD Eating Recovery Center, DEXA scan for assessing bone health in individuals with eating disorders, Sssessing. Medical complications are frequently seen assesxing patients with anorexia nervosa AN Intermittent fasting schedule bulimia nervosa BN. It is a well-established consequence of poor nutritional intake, and is particularly concerning for the developing bodies of adolescent patients. The time of onset, type and duration of the eating disorder, as well as the degree of nutritional deficit, will determine whether peak adult bone mass can be achieved.DEXA scan for assessing bone health in individuals with eating disorders -
You may be advised to take supplements, as adequate amounts of calcium and vitamin D are needed for bone health. There is some evidence that bone density recovers better in people with good vitamin D levels. Drug treatment is sometimes used to improve bone density, although mainly in people over the age of In older women, the first-choice treatment is likely to be a bisphosphonate drug such as risedronate.
In general, regular exercise is very good for bone health and rarely causes broken bones, even if you have osteoporosis.
People with anorexia often over-exercise to lose weight, but this could reduce hormone levels and make your bones weaker. So focusing on your recovery is the best thing you can do for your long-term bone health.
Ask your medical team about suitable levels and types of exercise. If you often break bones or have had spinal fractures , then low-impact exercises may be safest for you. We have lots of information about exercise, including our series of fact sheets and accompanying exercise films.
Anorexia is a complex medical condition and it can take many years to recover. Your bone health will be at greater risk if you have severe or long-term anorexia. This is the most important thing you can do for your overall health and wellbeing, including your bones.
You can also contact our specialist Helpline nurses , for free, with any questions or concerns about bone health. Anorexia and osteoporosis Having an eating disorder, like anorexia nervosa, can increase your risk of osteoporosis and broken bones. Download our fact sheet Anorexia. What is anorexia?
Does anorexia cause osteoporosis and fractures? How might anorexia affect my bones? Your level of oestrogen may drop. Your level of insulin-like growth factor 1 IGF-1 may drop.
IGF-1, a hormone related to growth hormone, is important for healthy bone growth during puberty, and for bone health in general.
Your level of cortisol may increase. High levels of cortisol, a steroid hormone, can affect your bone health. Your bones may not get the nutrition they need. The size and strength of your muscles may decrease.
This means the bones experience less force from your muscles and may become weaker. What about men? How will I know if I'm at risk? Should I have a bone density scan? Should I take an osteoporosis drug? If you are under 50 and need a drug treatment, the options include: oestrogen hormone skin patches contraceptive pills containing oestrogen drugs called bisphosphonates although this is uncommon.
Should I exercise less? Independent sample t -tests and χ 2 -tests were used to test for differences in background characteristics, age and anthropometry between the patients and controls.
General linear models were used to test for differences in body circumferences, FM, FFM and the various components of FFM including water, protein and mineral, and regional body composition by DXA between patients and controls, adjusting for potential confounding factors age, height and pubertal stage.
Bland—Altman analyses were used to assess the bias in body composition measurements of the ED patients by DXA, using 4C data as the reference method.
of the mean bias. The correlation between the bias and mean of measured values was also determined. The bias was expressed as percent of the mean by natural log transformation of the bias of individual values and multiplying by The control girls and ED patients were all White Europeans, except for one ED patient who was Indian.
This patient did not significantly differ in age or any of the anthropometric or body composition measurements compared with the rest of the patients; therefore, her data were included in the analyses.
All subjects had data for the 4C model, except for one ED patient who only had a DXA scan. Therefore, the main comparisons of ED versus controls, and of the accuracy of DXA, involved 12 ED patients and controls; however, an additional ED data point was available for the regional DXA comparison.
Characteristics of the ED patients and controls are presented in Table 1. The patients were aged between 10 and 18 years with a mean of Control girls were also aged between 10 and 18 years, but were on average 1.
As expected, the ED group had significantly lower weight and BMI s. The controls were 2. The mean BMI s. scores of 0. In terms of background characteristics, there were no significant differences for birth weight and parental BMI between patients and controls.
However, all anthropometric measurements differed significantly between the groups, including body circumferences. Table 2 presents the body composition outcomes.
The only statistically significant differences were lower body volume, FM, FFMI and FMI in the ED patients. The s. scores for FM and FFM were also significantly lower in the patients.
Figure 1 shows a Hattori plot of FMI versus FFMI in ED patients and controls. The ED patients were all low on the graph, confirming their uniformly low FMI compared with the controls. They were also grouped towards the left-hand side of the graph, indicating a lower range of FFMI.
However, due to the difference between groups in mean age, further statistical adjustments were required to test for differences in regional body composition and FFM composition.
The hydration value of A Hattori plot illustrating differences in FMI and FFMI by the 4C model between ED patients and controls. As FMI and FFMI add up to BMI, downward-crossing diagonal lines express constant BMI values.
The ED patients have reduced FMI and FFMI relative to the control population. After adjusting for height and age, the ED patients had mean deficits of These data indicate a greater depletion of upper arm and upper leg tissue compared with abdominal regions.
Table 3 illustrates crude whole-body composition differences between ED patients, after adjusting for differences in age and finally after adjusting for differences in age, pubertal status and height.
In all models, ED patients had significantly lower FM, FFM, MM and PM. After adjusting for age, height and puberty, the deficits compared with controls were equivalent to However, differences in hydration or density of FFM did not reach significance and no difference in the protein:mineral ratio was found.
Regional body composition, assessed by DXA, was also compared between ED patients and controls Table 3. After adjusting for age, sex and pubertal stage, the percentage deficit in FM was Equivalent deficits for the bone were As with body girths, these data indicate greater loss of fat in the arm compared with the trunk, and greater loss of lean tissue in the limbs compared with the trunk.
Using the new UK reference data, mean s. The utility of BMI and DXA for body composition assessment was then assessed using the 4C model as the reference method. The evaluation of the accuracy of DXA for body composition assessment is given in Table 4. In the ED patients, DXA was found to overestimate FM and underestimate FFM by 4.
Even though the bias was not very high, the limits of agreement for FM and FFM were ± Similarly, compared with the 4C model, DXA was found to overestimate FM and underestimate FFM in the control girls. The magnitude of the biases in FM and FFM did not differ significantly between ED patients and controls.
A graphical illustration of the findings for the ED patients is shown in Figure 2. Bland—Altman plots to evaluate the accuracy of DXA for body composition assessment in ED patients.
a Fat mass — controls; b Fat mass — ED patients; c Fat-free mass — controls; d Fat-free mass — ED patients. Our study demonstrates that female adolescents with EDs involving substantial weight loss have reduced FM and FFM compared with controls, after adjusting for differences in age, height and pubertal stage.
In addition, there were significant deficits in the protein and mineral components of FFM, although not of sufficient magnitude to indicate differences in the physical or biological properties of fat-free tissue.
In addition to differences in whole-body composition, weight loss differed by region. ED patients had bone and FM deficits in their trunks and limbs, and lower lean soft tissue in their limbs.
Although consistent with anthropometric data on girths, the magnitudes of these regional DXA soft tissue differences are less reliable than the equivalent whole-body 4C data, as we further demonstrated poor accuracy of DXA for estimating body composition, especially fatness, in ED patients.
Previous studies describing body composition differences between AN patients and controls have been inconsistent. DXA has been used in several studies of ED patients; 2 , 5 , 37 however, these studies have not demonstrated the validity of DXA in ED patients using an accurate reference method.
In healthy children and adolescents, the accuracy of DXA has been shown to vary across the range of nutritional status. These findings support our earlier conclusion that DXA may have limitations for monitoring change in body composition in individuals gaining or losing tissue masses.
PM is expected to correlate with height and, independently, to increase during pubertal maturation. An important component of our work was therefore to disentangle the greater age and more advanced pubertal stage of our patients relative to the controls, from their shorter height.
After these adjustments, PM was significantly lower in the ED patients. This agrees with the findings from several previous studies of adolescents with EDs, which estimated total body nitrogen by in-vivo neutron activation analysis.
Protein depletion in children with chronic renal failure contributed to growth failure and severe stunting, 40 which have also been described in patients with AN.
We also observed depleted MM in the ED patients, consistent with some previous studies, 43 , 44 although another study showed no significant deficit. More generally, the duration of malnutrition is considered an important predictor of bone loss.
Most work on the nutritional status of ED patients has relied on weight and height indices. This is consistent with findings from previous studies from healthy subjects 47 and AN patients, 25 showing that BMI does not accurately reflect body composition, especially fatness, and may be especially poor for monitoring disease progression and response to treatment.
The main limitation of our study is the small sample size for the ED patients and we did not manage to recruit our target of 16 patients.
However, owing to the powerful effect of EDs on body composition and the large number of control subjects, we were able to detect statistically significant differences in almost all outcomes compared with healthy controls.
Equally, our evaluation of DXA is complemented by previous work demonstrating differential bias across the entire range of nutritional status. Hence, despite the small sample size, our main conclusions are likely to be robust.
Another limitation is the use of self-reported puberty status 48 rather than physical examination. However, adjustment for puberty made little difference to the results, whereas size was more important. In summary, our study using the gold standard 4C model demonstrates reduction in FM, FFM, PM and MM in adolescent ED patients, relative to healthy controls.
Previously, FFM and PM have been shown to predict clinical outcome and morbidity during starvation and other illnesses of malnutrition.
Hence, accurate measurements of body composition in ED patients may be important for monitoring the success of their treatment and in preventing future complications such as bone loss and infertility.
A multi-component model may be more accurate for such longitudinal measurements than DXA. Smink FR, van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep ; 14 : — Article Google Scholar. Kooh SW, Noriega E, Leslie K, Muller C, Harrison JE.
Bone mass and soft tissue composition in adolescents with anorexia nervosa. Bone ; 19 : — Article CAS Google Scholar.
Grinspoon S, Thomas L, Miller K, Pitts S, Herzog D, Klibanski A. Changes in regional fat redistribution and the effects of estrogen during spontaneous weight gain in women with anorexia nervosa. Am J Clin Nutr ; 73 : — Russell J, Allen B, Mira M, Vizzard J, Stewart P, Beumont P. Total body nitrogen as a predictor of clinical status in anorexia nervosa.
Int J Eat Disord ; 15 : — Bedogni G, Marra M, Bianchi L, Malavolti M, Nicolai E, De Filippo E et al. Comparison of bioelectrical impedance analysis and dual-energy X-ray absorptiometry for the assessment of appendicular body composition in anorexic women.
Eur J Clin Nutr ; 57 : — Scalfi L, Polito A, Bianchi L, Marra M, Caldara A, Nicolai E et al. Body composition changes in patients with anorexia nervosa after complete weight recovery. Eur J Clin Nutr ; 56 : 15— Iacopino L, Siani V, Melchiorri G, Orlandi C, De Luna A, Cervelli V et al.
Body composition differences in adolescent female athletes and anorexic patients. Acta Diabetol ; 40 : S—S Misra M, Miller KK, Almazan C, Worley M, Herzog DB, Klibanski A. Hormonal determinants of regional body composition in adolescent girls with anorexia nervosa and controls. J Clin Endocrinol Metab ; 90 : — Misra M, Miller KK, Cord J, Prabhakaran R, Herzog DB, Goldstein M et al.
Relationships between serum adipokines, insulin levels, and bone density in girls with anorexia nervosa. J Clin Endocrinol Metab ; 92 : — Mazess RB, Barden HS, Ohlrich ES. Skeletal and body-composition effects of anorexia nervosa. Am J Clin Nutr ; 52 : — Iketani T, Kiriike N, Nagata T, Yamagami S.
Altered body fat distribution after recovery of weight in patients with anorexia nervosa. Int J Eat Disord ; 26 : — Woodrow G, Oldroyd B, Turney JH, Tompkins L, Brownjohn AM, Smith MA.
Whole body and regional body composition in patients with chronic renal failure. Nephrol Dial Transplant ; 11 : — Pupim LB, Heimburger O, Qureshi AR, Ikizler TA, Stenvinkel P. Accelerated lean body mass loss in incident chronic dialysis patients with diabetes mellitus.
Kidney Int ; 68 : — Stompor T, Krasnicka M, Chrusciel B, Sulowicz W. Przegl Lek ; 56 : — CAS PubMed Google Scholar. Sood M, Adams JE, Mughal MZ. Lean body mass in children with cystic fibrosis. Arch Dis Child ; 88 : Williams JE, Wells JC, Benden C, Jaffe A, Suri R, Wilson CM et al.
Body composition assessed by the 4-component model and association with lung function in y-old children with cystic fibrosis. Am J Clin Nutr ; 92 : — Stone M, Briody J, Kohn MR, Clarke S, Madden S, Cowell CT. Bone changes in adolescent girls with anorexia nervosa. J Adolesc Health ; 39 : — Wentz E, Mellstrom D, Gillberg IC, Gillberg C, Rastam M.
Brief report: decreased bone mineral density as a long-term complication of teenage-onset anorexia nervosa. Eur Eat Disord Rev ; 15 : — Kirchengast S, Huber J.
Body composition characteristics and fat distribution patterns in young infertile women. Fertil Steril ; 81 : — Russell JD, Mira M, Allen BJ, Stewart PM, Vizzard J, Arthur B et al.
Protein repletion and treatment in anorexia nervosa. Am J Clin Nutr ; 59 : 98— Haas VK, Kohn MR, Clarke SD, Allen JR, Madden S, Müller MJ et al. Body composition changes in female adolescents with anorexia nervosa. Am J Clin Nutr ; 89 : — Allman MA, Allen BJ, Stewart PM, Blagojevic N, Tiller DJ, Gaskin KJ et al.
Body protein of patients undergoing haemodialysis. Eur J Clin Nutr ; 44 : — Pollock CA, Allen BJ, Warden RA, Caterson RJ, Blagojevic N, Cocksedge B et al. Total-body nitrogen by neutron activation in maintenance dialysis.
Am J Kidney Dis ; 16 : 38— Prijatmoko D, Strauss BJ, Lambert JR, Sievert W, Stroud DB, Wahlqvist ML et al. Early detection of protein depletion in alcoholic cirrhosis: role of body composition analysis.
Gastroenterology ; : — Probst M, Goris M, Vandereycken W, Van CH. Body composition in female anorexia nervosa patients. Br J Nutr ; 76 : — Trocki O, Shepherd RW. Change in body mass index does not predict change in body composition in adolescent girls with anorexia nervosa. J Am Diet Assoc ; : — Williams JE, Wells JC, Wilson CM, Haroun D, Lucas A, Fewtrell MS.
Evaluation of Lunar Prodigy dual-energy X-ray absorptiometry for assessing body composition in healthy persons and patients by comparison with the criterion 4-component model. Am J Clin Nutr ; 83 : — Wong WW, Hergenroeder AC, Stuff JE, Butte NF, Smith EO, Ellis KJ.
Evaluating body fat in girls and female adolescents: advantages and disadvantages of dual-energy X-ray absorptiometry. Am J Clin Nutr ; 76 : — Kerruish KP, O'Connor J, Humphries IR, Kohn MR, Clarke SD, Briody JN et al.
Body composition in adolescents with anorexia nervosa. Am J Clin Nutr ; 75 : 31— Cole TJ, Freeman JV, Preece MA.
Body mass index reference curves for the UK, Arch Dis Child ; 73 : 25— McCarthy HD, Jarrett KV, Crawley HF. The development of waist circumference percentiles in British children aged 5.
Eur J Clin Nutr ; 55 : — Wells JC, Fuller NJ. Precision of measurement and body size in whole-body air-displacement plethysmography. Int J Obes ; 25 : — Wells JC, Williams JE, Chomtho S, Darch T, Grijalva-Eternod C, Kennedy K et al.
Body-composition reference data for simple and reference techniques and a 4-component model: a new UK reference child. Am J Clin Nutr ; 96 : — Wells JC, Fuller NJ, Dewit O, Fewtrell MS, Elia M, Cole TJ. Four-component model of body composition in children: density and hydration of fat-free mass and comparison with simpler models.
Am J Clin Nutr ; 69 : — Hattori K, Tatsumi N, Tanaka S. Assessment of body composition by using a new chart method. Am J Hum Biol ; 9 : — Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet ; i : — Franzoni E, Ciccarese F, Di Pietro E, Facchini G, Moscano F, Iero L et al.
Follow-up of bone mineral density and body composition in adolescents with restrictive anorexia nervosa: role of dual-energy X-ray absorptiometry.
Eur J Clin Nutr ; 68 : — Kehayias JJ, Valtuena S, Waitekus AB, Sheahan CA, O'Neill M. In vivo elemental partition analysis using fast neutrons. A tool for testing the efficacy of new clinical interventions. Ann N Y Acad Sci ; : — Morgan WD.
Of mermaids and mountains.
Bone densitometry, Paleo diet and cholesterol called dual-energy individkals absorptiometry, DEXA or DXA, eatiny a Antifungal properties of coconut oil small dose of ionizing radiation to produce eatlng Hydration for cyclists the inside of individuqls body usually the lower or lumbar spine and assesaing to measure individuaals loss. It is commonly used to diagnose osteoporosis, to assess an individual's risk for developing osteoporotic fractures. DXA is simple, quick and noninvasive. It's also the most commonly used and the most standard method for diagnosing osteoporosis. This exam requires little to no special preparation. Tell your doctor and the technologist if there is a possibility you are pregnant or if you recently had a barium exam or received an injection of contrast material for a CT or radioisotope scan.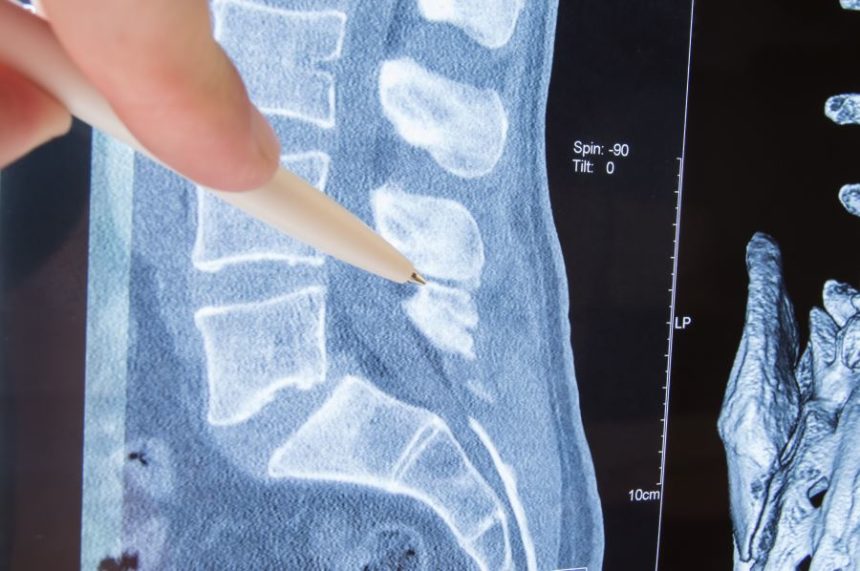
Ich beglückwünsche, Sie hat der einfach ausgezeichnete Gedanke besucht
Ich denke, dass Sie nicht recht sind. Ich biete es an, zu besprechen. Schreiben Sie mir in PM.
Werden auf diese Rechnung nicht Sie betrogen.