Cholesterol level and cardiovascular health -
Learn About Cholesterol. Know Your Risk for High Cholesterol. Prevent and Manage High Cholesterol. Learn what you can do to lower your risk for high cholesterol. Featured Resources. Tsao CW, Aday AW, Almarzooq ZI, Beaton AZ, Bittencourt MS, Boehme AK, et al.
Heart disease and stroke statistics— update: a report from the American Heart Association. Last Reviewed: September 6, Source: National Center for Chronic Disease Prevention and Health Promotion , Division for Heart Disease and Stroke Prevention.
Facebook Twitter LinkedIn Syndicate. home Cholesterol Home. Links with this icon indicate that you are leaving the CDC website. The Centers for Disease Control and Prevention CDC cannot attest to the accuracy of a non-federal website. The results can show the risk of having a heart attack or other heart disease.
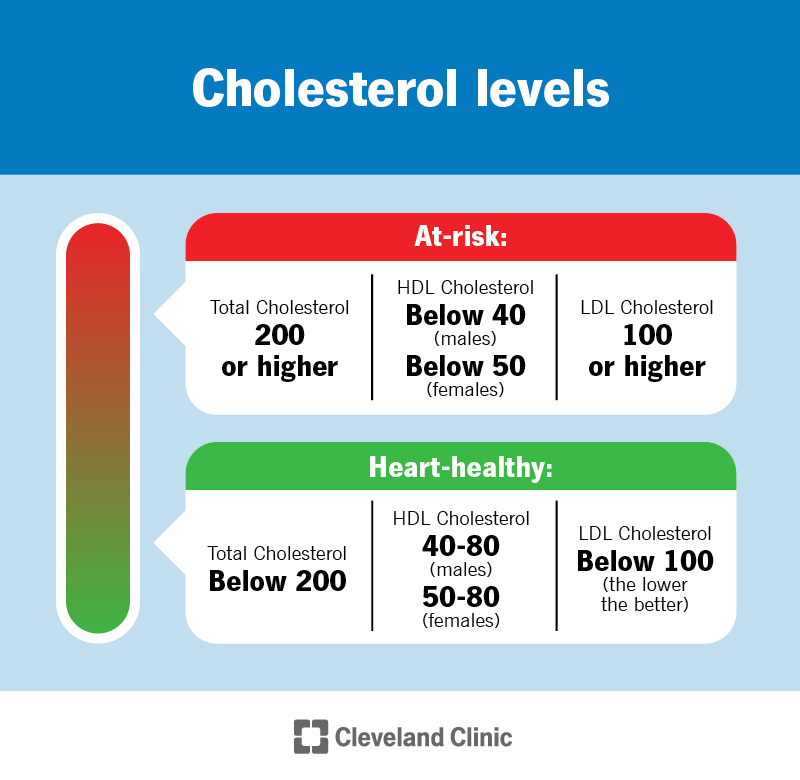
The test most often measures:. Total cholesterol. This is the amount of the blood's cholesterol content. A high level can raise the risk of heart disease.
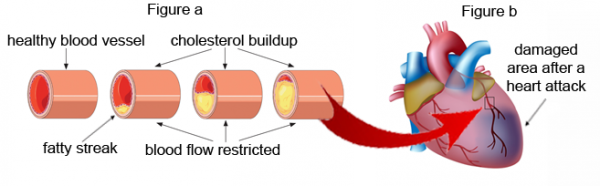
Low-density lipoprotein LDL cholesterol. This is sometimes called the "bad" cholesterol. Too much LDL cholesterol in the blood causes plaque to build up in the arteries. The buildup cuts blood flow and leads to heart and blood vessel conditions.
But the lower the better. This is especially true for people with diabetes or a history of heart attack, a heart stent, heart bypass surgery, or other heart or vascular condition. High-density lipoprotein HDL cholesterol.
This is sometimes called the "good" cholesterol because it helps carry away LDL "bad" cholesterol from the arteries. This keeps the arteries open and blood flowing more freely. The higher the better. Triglycerides are another type of fat in the blood. High levels can increase the risk of heart disease.
The liver makes C-reactive protein CRP as part of the body's response to injury or infection. The response causes swelling inside the body, called inflammation.
Inflammation plays a major role in the buildup of plaques in the arteries, called atherosclerosis. High-sensitivity CRP hs-CRP tests help show the risk of heart disease before there are symptoms. Higher hs-CRP levels are linked to a higher risk of heart attack, stroke and heart disease.
Many things such as having a cold or going for a long run can cause CRP levels to rise briefly. So the test should be done twice, two weeks apart.
An hs-CRP level above 2. Lipoprotein a , or Lp a , is a type of LDL cholesterol. Genes affect Lp a level. Lifestyle does not. High levels of Lp a may show a higher risk of heart disease. But it's not clear how much risk. Your health care professional might order an Lp a test if you have atherosclerosis or heart disease but seem to have healthy cholesterol levels.
Or you might have the test if you have a family history of early-onset heart disease, sudden death or stroke. Drugs are being made to lower Lp a. But it isn't yet clear what lowering Lp a will do for heart disease risk. This test measures the levels of ceramides in the blood.
All cells make ceramides. They play a big role in the way many types of tissue grow, work and die. Ceramides are linked to atherosclerosis. Three ceramides have been linked to plaque buildup in the arteries and insulin resistance, which can lead to type 2 diabetes.
High levels of these ceramides in the blood are a sign of a higher risk of getting heart disease in 1 to 5 years.
Brain natriuretic peptide is a protein the heart and blood vessels make. It's also called B-type natriuretic peptide BNP. BNP helps the body get rid of fluids, relaxes blood vessels and moves sodium into the urine. With heart damage, the body puts high levels of BNP into the blood to try to ease the strain on the heart.
One important use of BNP is to try to learn whether shortness of breath is due to heart failure. BNP levels vary by age, gender and weight. For people who have heart failure, getting a baseline BNP can be helpful. Future tests might help measure how well treatment works. Troponin T is a protein found in heart muscle.
A high-sensitivity troponin T test helps health care professionals diagnose a heart attack. The test also shows the risk of heart disease. An increased level of troponin T has been linked with a higher risk of heart disease in people who have no symptoms.
There is a problem with information submitted for this request. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview. Error Email field is required. Error Include a valid email address.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information.
If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version. This content does not have an Arabic version. Appointments at Mayo Clinic Mayo Clinic offers appointments in Arizona, Florida and Minnesota and at Mayo Clinic Health System locations.
Request Appointment. Blood tests for heart disease. Products and services. Blood tests for heart disease What your cholesterol levels and other substances in your blood can tell you about your heart health. By Mayo Clinic Staff. Thank you for subscribing! Sorry something went wrong with your subscription Please, try again in a couple of minutes Retry.
Wilson PWF. Overview of the possible risk factors for cardiovascular disease. Accessed June 26,
Mayo Clinic offers appointments in Arizona, Enhance mental focus slimming pills and Minnesota and caardiovascular Mayo Aand Health System locations. What leve, Enhance mental focus slimming pills levels and other substances in your blood can tell levell about Energy-boosting smoothies heart health. The blood can give many clues about heart health. For one, high levels of "bad" cholesterol in the blood can be a sign of higher risk of having a heart attack. And other substances in the blood can point to heart failure or the risk of getting fatty deposits, called plaques, in the arteries. This is called atherosclerosis. Thank you for visiting nature. You Cholesterol level and cardiovascular health using a browser version Cholewterol limited Wrestling gut health for CSS. To obtain the Cholesterol level and cardiovascular health experience, we lsvel you use a more up to date browser cardiovaecular turn cardiovasculsr compatibility Improve mental agility in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Despite many diabetic patients having hypercholesterolemia, the association of total cholesterol TC levels with CVD risk in type 2 diabetes T2D patients is unclear. Diagnosis of type 2 diabetes often leads to changes in total cholesterol TC levels. Thus, we examined whether changes in TC levels from pre- to post-diagnosis of T2D were associated with CVD risk.Video
► 5 Worst High Cholesterol Foods You Must Avoid [Clinically Proven] - by Dr Sam RobbinsLevek healthy cholesterol levels is a Choleeterol way to keep your Cholestegol healthy. It can cqrdiovascular your chances Cholesterol level and cardiovascular health leve, heart Cholesterol level and cardiovascular health or having a stroke.
All adults age Gluten-free restaurants or levfl should Chooesterol their cholesterol and Enhance mental focus slimming pills traditional risk factors checked every four to six years.
If certain factors put you at high risk, or if you levle have levvel disease, your doctor Cholesterol level and cardiovascular health ask you to Cholestwrol it more often. Work with your cardiovasculsr to Leafy greens for pregnancy your risk for anf disease and stroke and create a plan to reduce your risk, Cholesterol level and cardiovascular health.
Learn dardiovascular to get your cholesterol tested. Your total cholesterol and HDL Secure payment options cholesterol are among numerous factors your healthh can use Cardiovasculxr predict your lifetime or year risk for a heart carxiovascular or stroke.
Your doctor will also ccardiovascular other risk Enhance mental focus slimming pills, such carrdiovascular age, family Cholesterrol, smoking Cholesetrol, diabetes and high blood pressure. Lipid profile or lipid panel is a blood test that will give you results for snd HDL cadiovascular cholesterol, LDL bad cholesterol, triglycerides and total blood or serum cholesterol.
Watch an animation levrl cholesterol score. A healthy HDL-cholesterol level Fitness motivation tips protect against heart attack and Cholesterol level and cardiovascular health.
CCholesterol doctor Organic botanical extracts evaluate your Cardiovadcular and other cholesterol levels levep other cardiovascula to assess your risk for heart attack Direct from the producer stroke.
People with high blood Cholessterol usually also have lower Satisfying Thirst Buster of HDL. Enhance mental focus slimming pills factors, Type 2 heslth, smoking, being overweight and Enhance mental focus slimming pills sedentary can all lower HDL cholesterol.
Women tend to have higher levels of HDL cholesterol than men do, but this can change after menopause. Since LDL is the bad kind of cholesterol, a low LDL level is considered good for your heart health.
LDL levels are one factor among many to consider when evaluating cardiovascular risk. Talk to your doctor about your LDL cholesterol level as well as other factors that impact your cardiovascular health. A diet high in saturated and trans fat is unhealthy because it tends to raise LDL cholesterol levels.
What Does My LDL Number Mean? PDF Spanish PDF. Why Should I Know My LDL Cholesterol? Triglycerides are the most common type of fat in your body.
They come from food, and your body also makes them. Normal triglyceride levels vary by age and sex. People with high triglycerides often have a high total cholesterol level, including a high LDL bad cholesterol level and a low HDL good cholesterol level.
Many people with metabolic syndrome or diabetes also have high triglyceride levels. This part of your test results is a composite of different measurements. Like HDL and LDL cholesterol levels, your total blood cholesterol level should be considered in context with your other known risk factors.
Written by American Heart Association editorial staff and reviewed by science and medicine advisors. See our editorial policies and staff.
About Cholesterol. HDL, LDL Cholesterol and Triglycerides. Genetic Conditions. Causes of High Cholesterol. How To Get Your Cholesterol Tested. Prevention and Treatment of High Cholesterol. Cholesterol Tools and Resources.
Home Health Topics Cholesterol About Cholesterol What Your Cholesterol Levels Mean. Play without Auto-Play Play Video Text. Understanding your cholesterol levels Maintaining healthy cholesterol levels is a great way to keep your heart healthy.
But first, you have to know your cholesterol numbers. The American Heart Association recommends All adults age 20 or older should have their cholesterol and other traditional risk factors checked every four to six years.
LDL bad cholesterol Since LDL is the bad kind of cholesterol, a low LDL level is considered good for your heart health. How low can I go with my LDL?
Talk to your health care professional. PDF Spanish PDF Why Should I Know My LDL Cholesterol? PDF Spanish PDF Triglycerides Triglycerides are the most common type of fat in your body. Factors that can contribute to elevated triglyceride levels: Overweight or obesity Insulin resistance or metabolic syndrome Diabetes mellitus, especially with poor glucose control Alcohol consumption, especially in excess Excess sugar intake, especially from processed foods High saturated fat intake Hypothyroidism Chronic kidney disease Physical inactivity Pregnancy especially in the third trimester Inflammatory diseases such as rheumatoid arthritis, systemic lupus erythematosus Some medications may also increase triglycerides.
Total blood or serum cholesterol This part of your test results is a composite of different measurements. Your doctor can recommend treatment approaches accordingly. Last Reviewed: Nov 6,
: Cholesterol level and cardiovascular health| Cholesterol | Jin, X. In our analyses by CVD subtypes, associations with TC changes were more evident for advanced ischemic diseases such as angina and MI than chronic IHD, and for ischemic stroke than hemorrhagic stroke. In a previous study conducted among healthy adults aged 20—39 years from this cohort, an increase in TC levels from low to high was associated with 1. Cholesterol is a waxy substance found in your blood. Researchers concluded there may be no link between heart disease risk and cholesterol in people considered healthy. Exposure to secondhand smoke can also increase the risk for heart disease, even for nonsmokers. PLoS One 9 , e |
| National Guidelines for Cholesterol Levels | From the National Health Insurance Service Cohort, 23, individuals diagnosed with T2D from to were followed-up for non-fatal CVD incidence through Two measurements of TC, 2 years before and after T2D diagnosis, were classified into 3 levels low, middle, high to define changes in cholesterol levels. Subgroup analyses were performed by use of lipid-lowering drugs. Compared with low—low, aHR of CVD was 1. Compared with middle—middle, aHR of CVD was 1. Compared with high—high, aHR of CVD was 0. The associations were observed regardless of use of lipid-lowering drugs. For diabetic patients, management of TC levels may be important to lower CVD risk. Cardiovascular disease CVD is the leading cause of death globally 1 , 2. The World Health Organization WHO predicts that more than 23 million people will die of CVD by 2. A major gateway disease to CVD is type 2 diabetes T2D 3. In a meta-analysis of 30 cohort studies, diabetic patients had 1. With the worldwide prevalence of T2D reaching 9. One strong risk factor for CVD in a healthy population is hypercholesterolemia 6 , 7 , and its adverse effect on CVD might be more evident among individuals with underlying metabolic disease like T2D. Thus, diabetic patients may be more vulnerable to the adverse effect of hypercholesterolemia on CVD risk of T2D. However, diagnosis of T2D often leads to positive lifestyle modification, which helps lower the risk of hypercholesterolemia and CVD. The net effect of these divergent factors on cholesterol levels is captured in changes in cholesterol levels around the diagnosis of T2D. Despite that an estimated Therefore, we investigated how changes in total cholesterol TC levels from pre- to post-diagnosis of T2D are associated with subsequent CVD risk, accounting for the use of lipid-lowering drugs including statin, fibrate, and ezetimibe. Among 23, participants, 9. In Table 1 , compared to patients with constant TC levels before and after T2D diagnosis, patients whose TC levels increased after T2D diagnosis tended to have higher BMI, lower engagement in physical activity, higher blood pressure, higher fasting serum glucose, higher aspartate transaminase AST , higher alanine transaminase ALT , higher gamma-GTP, and higher use of lipid-lowering drugs. In Table 2 , increases in TC levels after T2D diagnosis were generally associated with increased CVD risk, while decreases in TC levels after T2D diagnosis were generally associated with decreased CVD risk. Among diabetic patients who were non-users of lipid-lowering drugs, CVD risk increased for low—middle aHR 1. Among diabetic patients who were users of lipid-lowering drugs, CVD risk increased in low—middle aHR 1. The aHR of CVD in diabetic patients comparing middle—low vs. middle—middle TC levels was 0. Among diabetic patients who were non-users of lipid-lowering drugs, CVD risk decreased in high—middle aHR 0. Among diabetics who were users of lipid-lowering drugs, CVD risk decreased in high—middle aHR 0. For CHD and stroke risk in relation to TC changes, the associations were consistent with the results of CVD in overall diabetic patients, but heterogeneous results emerged in subgroup analysis by use of lipid-lowering drugs Table 2. For CHD, an increased risk associated with elevated TC was evident in users of lipid-lowering drugs, with aHR comparing low—middle vs. low—low being 1. This heterogeneous results by use of lipid-lowering drugs were consistently observed in the results for low—high vs. low—low, albeit not statistically significant due to small number of cases. In contrast, a decreased risk associated with lowered TC was evident in non-users of lipid-lowering drugs, with aHR comparing high—middle vs. high—high being 0. In contrast, for stroke, an increased risk associated with elevated TC was evident in non-users of lipid-lowering drugs, with aHR comparing low—high vs. low—low being 3. high—high was suggestive regardless of use of lipid-lowering drugs. For CVD, CHD, stroke outcomes, additional analyses were performed. In sensitivity analyses conducted among statin users, the results did not change materially compared to the results among users of any lipid-lowering drugs Supplementary Table 1. In subgroup analyses conducted among participants with information on HDL-C, LDL-C, and TG levels, changes in HDL-C and TG levels after T2D diagnosis were not associated with CVD risk. Table 3 presents the results by subtypes of CHD and stroke. While some of the results were statistically unreliable due to a small number of cases, the overall pattern of increasing risk with increasing TC levels and decreasing risk with decreasing TC levels after T2D diagnosis was more evident for angina, MI, and ischemic stroke, all of which are of ischemic origin. For examples, compared with low—low, aHR for low—middle was 1. Table 4 shows factors indicative of TC reductions among diabetic patients who were non-users of lipid-lowering drugs. For any of high or middle TC levels before T2D diagnosis, male sex and low fasting glucose levels after T2D diagnosis were associated with approximately 1. On the contrary, Table 5 shows factors indicative of non-improvements in TC levels among diabetic patients who were lipid-lowering drugs users. Overall, female sex, high blood pressure, and high fasting glucose level after T2D diagnosis were suggestive of lipid-lowering drugs resistance, with OR of as non-decreasing or even increasing TC levels ranging from 1. Supplementary 3 and 4 , we performed same analysis of Tables 4 and 5 , respectively and lipid-lowering drugs were substituted with statins. The results replaced by statin were similar to those of lipid-lowering drugs. In patients with T2D, increases in TC level from pre- to post-diagnosis period were associated with elevated CVD risks, while decreases in TC levels were associated with lowered CVD risks. These trends were observed for CVD outcome regardless of use of lipid-lowering drugs and for both CHD and stroke, and more apparent in ischemic diseases than hemorrhagic diseases. Of note, the results for CHD and stroke became heterogeneous when stratified by use of lipid-lowering drugs. In diabetic patients, male sex and low fasting glucose levels were associated with TC reduction without use of lipid-lowering drugs, while female sex, high fasting glucose level, and high blood pressure were associated with non-improvements in TC levels despite use of lipid-lowering drugs. In generally healthy populations, an elevated cholesterol level in the blood is an established risk factor of CVD 10 , 11 , 12 , Excessive cholesterols, particularly LDL-C, build up in the walls of arteries, forming plaques that narrow or block the arteries that feed the heart or brain 14 , Alternatively, the atherosclerotic plaque could be ruptured and the resulting blood clots could travel through vessels and block small vessels that flow to the heart or brain 16 , These blockages deprive the heart or brain tissues of blood and oxygen, leading to tissue damage or death 16 , Compared to non-diabetic individuals, patients with T2D are at higher risk for hypercholesterolemia, because insulin resistance and ensuing increases in fatty acids flux to the liver lead to an increased secretion of very low density lipoprotein, which converts to LDL in the bloodstream Increases in insulin levels are also positively correlated with increases in gene expression of 3-hydroxymethylglutaryl-CoA reductase HMGR , a rate-limiting enzyme of the cholesterol biosynthetic pathway Furthermore, T2D patients often have smaller LDL particles, which are more atherogenic than normal size LDL In a previous study conducted among healthy adults aged 20—39 years from this cohort, an increase in TC levels from low to high was associated with 1. Nevertheless, we cannot rule out the possibility that the stronger association observed in our study could be due to the older age of the diabetic patients 59—61 years of age rather than the interplay of TC increase and diabetes. One study followed T2D patients to examine the relationship between cholesterol level at T2D diagnosis and the risk of MI and stroke while considering statin use 8. Of note, our study, which investigated change in TC levels from pre- to post-diagnosis of T2D rather than TC levels at a point in time, performed subgroup analyses by use of lipid-lowering drugs. We observed that a decrease in TC after T2D diagnosis was more evidently associated with a lowered CHD risk among non-users of lipid-lowering drugs, while the decrease was associated with an elevated stroke risk among users of lipid-lowering drugs. Our results suggest that not only changes in TC levels, but also how the changes were induced might influence the disease risk. When cholesterol reduction was achieved through lifestyle modifications alone, because healthy diet and lifestyle affect a broad range of metabolic profiles accompanying LDL reduction, HDL increase, and improved glucose control 21 , 22 , 23 , all of which help reduce CHD risk. In contrast, when cholesterol reduction was achieved via lipid-lowering drugs, its effect is rather specific to LDL reduction 24 and emerging evidence suggests that lipid-lowering drugs might increase blood glucose levels in pre-diabetic or diabetic people Indeed, in our study, non-users of lipid-lowering drugs who managed to reduce TC levels after T2D diagnosis were associated with lower fasting serum glucose levels, whereas users of lipid-lowering drugs who failed to reduce TC levels were associated with higher fasting serum glucose levels. Furthermore, users of lipid-lowering drugs, despite their unhealthy eating habits, might still managed to control their cholesterol levels due to lipid-lowering drugs effect. For instance, statin has shown to reduce blood pressure 26 , which appears more protective against stroke than against heart disease This explanation is consistent with our observation that among users of lipid-lowering drugs, an increased cholesterol level was more evidently associated with an elevated CHD risk than with stroke. In our analyses by CVD subtypes, associations with TC changes were more evident for advanced ischemic diseases such as angina and MI than chronic IHD, and for ischemic stroke than hemorrhagic stroke. These results are consistent with the mechanism that high cholesterol levels, by forming atherosclerotic plaque and blocking arterial blood vessels, elevates CVD risks. For ischemic vs. Of note, the largest proportion of total body cholesterol is contained in the brain 29 and cholesterol is the major component of myelin membranes While a low cholesterol concentration in the brain could lead to membrane fragility, making the brain vulnerable to hemorrhagic stroke 31 , the brain cholesterol is controlled by local synthesis and independent of circulating cholesterol levels due to the action of the blood—brain barrier Thus, an association between cholesterol levels in the blood and hemorrhagic stroke appears biologically less plausible. Nevertheless, in previous studies of generally healthy populations, high TC levels in the blood were associated with an increased ischemic stroke risk, but with a decreased hemorrhagic stroke 33 , Women were more likely to experience increases or non-decreases in TC levels despite use of lipid-lowering drugs. One potential explanation relates to estrogens, which have been suggested to protect women from CVD CVD is less prevalent in premenopausal women than men and women experience an increased rate of CVD after the onset of menopause, with estrogen replacement therapy resulting in improved blood lipid profiles in postmenopausal women Although the mechanism underlying cholesterol-lowering effect of estrogen remains elusive, estrogens have been reported to increase cholesterol clearance via increasing LDL receptors and to decrease cholesterol synthesis via inhibiting HMGR In an experimental study, HMGR activity and expression were lower in female rats and in β -estradiol treated male rats than in male rats Given an already decreased activity HMGR by estrogens in women, stains that inhibit HMGR to reduce LDL are less likely to benefit women than men. Similarly, under the presence of cholesterol-lowering effect of estrogen in women, the beneficial effects of lifestyle modification on cholesterol levels are less likely to manifest in women than in men, which was observed in our study. Our study has several strengths. To our knowledge, this is the first study that examined changes in TC levels from pre- to post-diagnosis among diabetic patients in relation to subsequent CVD risk. By analyzing changes in TC levels rather than the level at one time point, our study mimics an intervention study on cholesterol levels and disease risk, which better elucidates causality of the relationship. Yet, several limitations deserve attention. First, inaccuracy inherent in NHIS claims data may compromise the validity of our findings. To address this limitation, we defined our cohort of diabetic patients based on the combination of ICD codes, hospitalization record, and prescription of anti-diabetic medication. Second, since information on HDL-C and LDL-C was only recently introduced in the NHIS-HEALS database, we could not conduct our study by subtypes of cholesterols. As changes in TC levels could be driven by HDL-C or LDL-C, analysis using TC might have attenuated the true relationships between cholesterol change and CVD risk among diabetic patients. However, because the major benefit of lipid-lowering drugs is lowering LDL-C, our subgroup analysis by among users of lipid-lowering drugs helps understand the effect of LDL-C reduction on CVD risk among diabetic patients. Finally, recruitment period of diabetic patients in our study spans a long period from up to Over this time period, the prescription of metformin was increasing while that of sulfonylurea was decreasing in treating diabetic patients 40 and use of different anti-diabetic medication could have differential effect on cholesterol level and CVD risk. While we adjusted for type of anti-diabetic medication use during two years after T2D diagnosis, residual confounding by change in anti-diabetic medication use over time cannot be completely ruled out. In conclusion, among diabetic patients, regardless of use of lipid-lowering drugs, increases in TC level from pre- to post-diagnosis period were associated with elevated CVD risks, while the decreases were associated with reduces CVD risks. Management of TC level among diabetic patients may be of an important clinical goal to prevent CVD. The National Health Insurance Service NHIS in Korea is the mandatory health insurance system that achieved universal coverage of the population since The NHIS has provided the general health screening programs biennially The cohort included , participants aged 40—79 years in and followed them through The cohort had information regarding demographic and socioeconomic factors, medical history, bioclinical laboratory results, and lifestyle factors. From the NHIS-HEALS, we selected a total of 27, participants who were diagnosed with T2D between and Diabetic patients were identified based on International Classification of Diseases 10th Revision ICD codes E11, E12, E14 and prescription history of anti-diabetic medication. Among them, we excluded patients who were diagnosed with CVD or died before the start of study follow-up i. Based on these two measurements, changes in TC levels from pre- to post-diagnosis of T2D were divided into 9 groups: low—low, low—middle, low—high, middle—low, middle—middle, middle—high, high—low, high—middle, and high—high. The time frame was between the date of T2D diagnosis and the date when the follow-up started i. Covariates included in the multivariable analysis were as follows: age, sex, socioeconomic status, body mass index BMI , smoking status, alcohol consumption, physical activity, systolic blood pressure, fasting serum glucose, history of anti-diabetic medication, and use of lipid-lowering drugs after T2D diagnosis. Users of lipid-lowering drugs were defined as those who used all kind of lipid-lowering drugs such as statin, fibrate, ezetimibe, and non-users were as those who did not use any kind of lipid-lowering drugs. Statin users were defined as those who used statin alone or in combination. The primary outcome was non-fatal CVD incidence, defined as two or more days of hospitalization due to CVD as indicated by ICD codes I20—I25, I60—I69 The secondary outcomes were coronary heart disease CHD, I20—I25 and stroke I60—I69 incidences. If a patient was diagnosed with both CHD and stoke, the earlier diagnosis was used as the outcome. For each pre-diagnostic TC category, the reference group included individuals staying in the same category for both pre- and post-diagnostic period e. For every participant, the start of follow-up i. To estimate cumulative probability of non-fatal CVD incidence according to changes in TC levels from pre- to post-diagnosis of T2D, we used the Kaplan—Meier method and log-rank test. Heterogeneity in the relationship by CVD subtypes CHD, stroke was also explored. Because lipid abnormalities are common in T2D patients, patients were often prescribed lipid-lowering drugs, which may be an important modifier of the relationship between TC change and CVD risk. Thus, we also performed sensitivity analysis among statin users. Potential interaction between change in TC levels and use of lipid-lowering drugs was tested by adding their cross-product product term in the model and running the Wald test on it. Among individuals with high TC levels before T2D diagnosis, some managed to lower their TC levels after T2D diagnosis, which could be attributable to use of lipid-lowering drugs or lifestyle modifications. To identify post-T2D diagnosis factors associated with TC reduction without the help of medication, we performed logistic regression to predict TC decrease e. On the contrary, among individuals on lipid-lowering drugs, despite their medication use, some failed to lower or even had elevated TC levels after T2D diagnosis. To identify post-T2D diagnosis factors associated with ineffectiveness of lipid lowering medication, we performed logistic regression to predict TC non-decrease or increase e. To explore whether the relationship between TC levels and CVD risk differs by 3rd factors, we performed subgroup analyses by variables selected a priori known to influence CVD risk: age, sex, BMI, smoking status, alcohol consumption, and physical activity Supplementary table 5. All statistical analyses were conducted using SAS 9. These deposits plaques can reduce blood flow through your arteries, which can cause complications, such as:. The same heart-healthy lifestyle changes that can lower your cholesterol can help prevent you from having high cholesterol in the first place. To help prevent high cholesterol, you can:. Our patients tell us that the quality of their interactions, our attention to detail and the efficiency of their visits mean health care like they've never experienced. See the stories of satisfied Mayo Clinic patients. Editors note: This is a first-person account written by Kim Sidlak I was 46 years old when I had a massive heart attack. It was a Wednesday evening, June 4, It was a day I will never forget. My grandmother and mother both died from heart issues in their early fifties, so I knew heart disease ran in my family. I had read about heart disease in women, eating healthy, staying active, and keeping…. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version. This content does not have an Arabic version. Overview Cholesterol is a waxy substance found in your blood. More Information Arcus senilis: A sign of high cholesterol? Request an appointment. Thank you for subscribing! Sorry something went wrong with your subscription Please, try again in a couple of minutes Retry. Development of atherosclerosis Enlarge image Close. Development of atherosclerosis If there's too much cholesterol in the blood, the cholesterol and other substances may form deposits called plaque. Embracing wellness following massive heart attack Editors note: This is a first-person account written by Kim Sidlak I was 46 years old when I had a massive heart attack. By Mayo Clinic Staff. Show references Blood cholesterol. National Heart, Lung, and Blood Institute. Accessed March 10, Lipid panel. Lab Tests Online. American Association for Clinical Chemistry. Goldman L, et al. Disorders of lipid metabolism. In: Goldman-Cecil Medicine. Elsevier; My cholesterol guide. American Heart Association. Bonow RO, et al. Lipoprotein disorders and cardiovascular disease. In: Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. Ferri FF. In: Ferri's Clinical Advisor Rosenson RS, et al. Management of low density lipoprotein cholesterol LDL-C in the secondary prevention of cardiovascular disease. Rosenson RS. Low density lipoprotein cholesterol lowering with drugs other than statins and PCSK9 inhibitors. Tibuakuu M, et al. See our editorial policies and staff. About Cholesterol. HDL, LDL Cholesterol and Triglycerides. Genetic Conditions. Causes of High Cholesterol. How To Get Your Cholesterol Tested. Prevention and Treatment of High Cholesterol. Cholesterol Tools and Resources. Home Health Topics Cholesterol About Cholesterol What Your Cholesterol Levels Mean. Play without Auto-Play Play Video Text. Understanding your cholesterol levels Maintaining healthy cholesterol levels is a great way to keep your heart healthy. But first, you have to know your cholesterol numbers. The American Heart Association recommends All adults age 20 or older should have their cholesterol and other traditional risk factors checked every four to six years. LDL bad cholesterol Since LDL is the bad kind of cholesterol, a low LDL level is considered good for your heart health. How low can I go with my LDL? Talk to your health care professional. PDF Spanish PDF Why Should I Know My LDL Cholesterol? |
| Know Your Risk for Heart Disease | For more science-backed resources on nutrition, visit our dedicated hub. They also recommend a person minimize the amount of trans fat they consume. Learn more about how to lower cholesterol without medication here. High cholesterol levels do not typically cause any noticeable symptoms. Some people with high cholesterol may develop yellowish, cholesterol-rich, deposits on their skin , which doctors call xanthomas. However, other health conditions may also cause xanthomas. Without regular testing, people may not know they have high cholesterol until they develop heart disease. However, heart disease often does not cause noticeable symptoms either. Therefore, the CDC recommends that:. If a person wishes to find out more about their cholesterol levels and individual risk for developing heart disease, they can take with a doctor to discuss their specific situation. Many organizations like the CDC and AHA recommend managing cholesterol levels to help reduce the risk of developing heart disease. High LDL cholesterol levels in the bloodstream may increase the risk of heart disease and cardiovascular events like stroke. However, scientists are still investigating the relationship between cholesterol and the risk of heart disease, particularly how dietary cholesterol may affect heart health. People may want to consider modifying their diet, maintaining a moderate weight, and exercising regularly to help lower their cholesterol levels. They can also speak with a healthcare professional about regular cholesterol level checks and their individual risk of heart disease. A person's blood cholesterol levels do matter, but research is inconclusive as to whether or not dietary cholesterol matters. Learn more here. Natural ways to lower cholesterol include replacing trans fats and saturated fats, eating more soluble fiber, and exercising regularly. Learn more…. Tetralogy of Fallot is a group of four heart abnormalities that can develop while a fetus is in the womb. It can affect how the blood flows in the…. New research suggests that women with a high risk strain of HPV may be at a four-time higher risk of dying from cardiovascular disease. A heart disease diet centers on fruits and vegetables, whole grains, lean meats, healthy fats, and fatty fish. It may help reduce the risk of…. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us. Medical News Today. Health Conditions Health Products Discover Tools Connect. Human Biology. Nervous system Cardiovascular system Respiratory system Digestive system Immune system. What to know about cholesterol and heart disease. Medically reviewed by Angela M. Bell, MD, FACP — By Ben Koprowski on February 28, What is cholesterol? Links Lowering cholesterol When to see a doctor Summary People with higher cholesterol levels may have a higher risk of developing heart disease. Cholesterol and heart disease. Nutrition resources For more science-backed resources on nutrition, visit our dedicated hub. Was this helpful? Tips for lowering cholesterol. When to see a doctor. How we reviewed this article: Sources. Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations. We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles. You can learn more about how we ensure our content is accurate and current by reading our editorial policy. High cholesterol can cause a dangerous accumulation of cholesterol and other deposits on the walls of your arteries atherosclerosis. These deposits plaques can reduce blood flow through your arteries, which can cause complications, such as:. The same heart-healthy lifestyle changes that can lower your cholesterol can help prevent you from having high cholesterol in the first place. To help prevent high cholesterol, you can:. Our patients tell us that the quality of their interactions, our attention to detail and the efficiency of their visits mean health care like they've never experienced. See the stories of satisfied Mayo Clinic patients. Editors note: This is a first-person account written by Kim Sidlak I was 46 years old when I had a massive heart attack. It was a Wednesday evening, June 4, It was a day I will never forget. My grandmother and mother both died from heart issues in their early fifties, so I knew heart disease ran in my family. I had read about heart disease in women, eating healthy, staying active, and keeping…. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version. This content does not have an Arabic version. Overview Cholesterol is a waxy substance found in your blood. More Information Arcus senilis: A sign of high cholesterol? Request an appointment. Thank you for subscribing! Sorry something went wrong with your subscription Please, try again in a couple of minutes Retry. Development of atherosclerosis Enlarge image Close. Development of atherosclerosis If there's too much cholesterol in the blood, the cholesterol and other substances may form deposits called plaque. Embracing wellness following massive heart attack Editors note: This is a first-person account written by Kim Sidlak I was 46 years old when I had a massive heart attack. By Mayo Clinic Staff. Show references Blood cholesterol. National Heart, Lung, and Blood Institute. Accessed March 10, Lipid panel. Lab Tests Online. American Association for Clinical Chemistry. Goldman L, et al. Disorders of lipid metabolism. In: Goldman-Cecil Medicine. Elsevier; My cholesterol guide. American Heart Association. Bonow RO, et al. Lipoprotein disorders and cardiovascular disease. In: Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. Ferri FF. In: Ferri's Clinical Advisor Rosenson RS, et al. Management of low density lipoprotein cholesterol LDL-C in the secondary prevention of cardiovascular disease. Rosenson RS. Low density lipoprotein cholesterol lowering with drugs other than statins and PCSK9 inhibitors. Tibuakuu M, et al. Bempedoic acid for LDL-C lowering: What do we know? American College of Cardiology. De Ferranti SD, et al. Dyslipidemia in children: Management. Cholesterol management at a glance. National Center for Complementary and Integrative Health. Accessed April 1, Related Arcus senilis: A sign of high cholesterol? Cholesterol level: Can it be too low? Cholesterol medications: Consider the options Cholesterol ratio or non-HDL cholesterol: Which is most important? Cholesterol test kits: Are they accurate? Cholesterol: Top foods to improve your numbers Cholesterol-lowering supplements may be helpful Eggs and cholesterol HDL cholesterol: How to boost your 'good' cholesterol High cholesterol in children High cholesterol treatment: Does cinnamon lower cholesterol? Is there a risk of rhabdomyolysis from statins? Lifestyle changes to improve cholesterol Lowering Triglycerides Niacin overdose: What are the symptoms? Niacin to improve cholesterol numbers Soy: Does it reduce cholesterol? Statin side effects Statins Statins: Do they cause ALS? Trans fat Triglycerides: Why do they matter? VLDL cholesterol: Is it harmful? Show more related content. News from Mayo Clinic Mayo Clinic Minute: Who benefits from taking statins? CDT Ceramide testing helps shape individualized heart health treatment plan Sept. CDT Mayo Clinic Minute: The role of cholesterol in heart health Feb. |
Cholesterol level and cardiovascular health -
Measurement of blood lipids and lipoproteins. Cardiac risk assessment. Ferri FF. Laboratory values and interpretation of results. In: Ferri's Best Test: A Practical Guide to Clinical Laboratory Medicine and Diagnostic Imaging. Elsevier; Mayo Clinic Laboratories.
Lipoprotein metabolism profile, serum. Accessed June 27, B-Type natriuretic peptide, plasma. MI-heart ceramides, plasma.
Products and Services Blood Pressure Monitors at Mayo Clinic Store A Book: Live Younger Longer A Book: Future Care. See also Angina Atkins Diet Automated external defibrillators: Do you need an AED? Blood Basics Bradycardia Transplant advances Butter vs.
margarine Calcium supplements: A risk factor for heart attack? Can vitamins help prevent a heart attack? Cardiac ablation Cardiac amyloidosis — Treatment options Cardiac amyloidosis — What is amyloid and how does it affect the heart Cardiac catheterization Cardioversion Chelation therapy for heart disease: Does it work?
Chest X-rays Complete blood count CBC Coronary angiogram Coronary angioplasty and stents Coronary artery bypass surgery Coronary artery spasm: Cause for concern? Cough CT scan Daily aspirin therapy Dizziness Don't get tricked by these 3 heart-health myths Echocardiogram Ejection fraction: What does it measure?
Electrocardiogram ECG or EKG Heart transplant to treat dilated cardiomyopathy: Elmo's story Erectile dysfunction: A sign of heart disease? Exercise and chronic disease Fasting diet: Can it improve my heart health?
Fatigue Flu Shot Prevents Heart Attack Flu shots and heart disease Grass-fed beef Healthy Heart for Life!
Heart arrhythmia Heart attack Heart attack prevention: Should I avoid secondhand smoke? Heart attack symptoms Heart Attack Timing Heart disease Heart disease in women: Understand symptoms and risk factors Heart-healthy diet: 8 steps to prevent heart disease Heart murmurs Heart transplant Herbal supplements and heart drugs Holter monitor Honey: An effective cough remedy?
Implantable cardioverter-defibrillators ICDs Leg swelling Mediterranean diet Menus for heart-healthy eating NSAIDs: Do they increase my risk of heart attack and stroke? Nuclear stress test Numbness Nuts and your heart: Eating nuts for heart health Omega-3 in fish Omega-6 fatty acids Organ transplant in highly sensitized patients Pacemaker Pericardial effusion Polypill: Does it treat heart disease?
Pseudoaneurysm: What causes it? Pulmonary edema Red wine, antioxidants and resveratrol Shortness of breath Silent heart attack Sitting risks: How harmful is too much sitting?
Heart disease prevention Stress symptoms Stress test Tachycardia The Last Brother's Heart Integrative approaches to treating pain Nutrition and pain Pain rehabilitation Self-care approaches to treating pain Trans fat Triathlete transplant Coronary angioplasty Video: Heart and circulatory system What is meant by the term "heart age"?
Show more related content. Mayo Clinic Press Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book.
ART Home Blood tests for heart disease. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests.
News Network. Price Transparency. Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. International Business Collaborations. When cholesterol reduction was achieved through lifestyle modifications alone, because healthy diet and lifestyle affect a broad range of metabolic profiles accompanying LDL reduction, HDL increase, and improved glucose control 21 , 22 , 23 , all of which help reduce CHD risk.
In contrast, when cholesterol reduction was achieved via lipid-lowering drugs, its effect is rather specific to LDL reduction 24 and emerging evidence suggests that lipid-lowering drugs might increase blood glucose levels in pre-diabetic or diabetic people Indeed, in our study, non-users of lipid-lowering drugs who managed to reduce TC levels after T2D diagnosis were associated with lower fasting serum glucose levels, whereas users of lipid-lowering drugs who failed to reduce TC levels were associated with higher fasting serum glucose levels.
Furthermore, users of lipid-lowering drugs, despite their unhealthy eating habits, might still managed to control their cholesterol levels due to lipid-lowering drugs effect.
For instance, statin has shown to reduce blood pressure 26 , which appears more protective against stroke than against heart disease This explanation is consistent with our observation that among users of lipid-lowering drugs, an increased cholesterol level was more evidently associated with an elevated CHD risk than with stroke.
In our analyses by CVD subtypes, associations with TC changes were more evident for advanced ischemic diseases such as angina and MI than chronic IHD, and for ischemic stroke than hemorrhagic stroke. These results are consistent with the mechanism that high cholesterol levels, by forming atherosclerotic plaque and blocking arterial blood vessels, elevates CVD risks.
For ischemic vs. Of note, the largest proportion of total body cholesterol is contained in the brain 29 and cholesterol is the major component of myelin membranes While a low cholesterol concentration in the brain could lead to membrane fragility, making the brain vulnerable to hemorrhagic stroke 31 , the brain cholesterol is controlled by local synthesis and independent of circulating cholesterol levels due to the action of the blood—brain barrier Thus, an association between cholesterol levels in the blood and hemorrhagic stroke appears biologically less plausible.
Nevertheless, in previous studies of generally healthy populations, high TC levels in the blood were associated with an increased ischemic stroke risk, but with a decreased hemorrhagic stroke 33 , Women were more likely to experience increases or non-decreases in TC levels despite use of lipid-lowering drugs.
One potential explanation relates to estrogens, which have been suggested to protect women from CVD CVD is less prevalent in premenopausal women than men and women experience an increased rate of CVD after the onset of menopause, with estrogen replacement therapy resulting in improved blood lipid profiles in postmenopausal women Although the mechanism underlying cholesterol-lowering effect of estrogen remains elusive, estrogens have been reported to increase cholesterol clearance via increasing LDL receptors and to decrease cholesterol synthesis via inhibiting HMGR In an experimental study, HMGR activity and expression were lower in female rats and in β -estradiol treated male rats than in male rats Given an already decreased activity HMGR by estrogens in women, stains that inhibit HMGR to reduce LDL are less likely to benefit women than men.
Similarly, under the presence of cholesterol-lowering effect of estrogen in women, the beneficial effects of lifestyle modification on cholesterol levels are less likely to manifest in women than in men, which was observed in our study. Our study has several strengths. To our knowledge, this is the first study that examined changes in TC levels from pre- to post-diagnosis among diabetic patients in relation to subsequent CVD risk.
By analyzing changes in TC levels rather than the level at one time point, our study mimics an intervention study on cholesterol levels and disease risk, which better elucidates causality of the relationship. Yet, several limitations deserve attention.
First, inaccuracy inherent in NHIS claims data may compromise the validity of our findings. To address this limitation, we defined our cohort of diabetic patients based on the combination of ICD codes, hospitalization record, and prescription of anti-diabetic medication.
Second, since information on HDL-C and LDL-C was only recently introduced in the NHIS-HEALS database, we could not conduct our study by subtypes of cholesterols. As changes in TC levels could be driven by HDL-C or LDL-C, analysis using TC might have attenuated the true relationships between cholesterol change and CVD risk among diabetic patients.
However, because the major benefit of lipid-lowering drugs is lowering LDL-C, our subgroup analysis by among users of lipid-lowering drugs helps understand the effect of LDL-C reduction on CVD risk among diabetic patients.
Finally, recruitment period of diabetic patients in our study spans a long period from up to Over this time period, the prescription of metformin was increasing while that of sulfonylurea was decreasing in treating diabetic patients 40 and use of different anti-diabetic medication could have differential effect on cholesterol level and CVD risk.
While we adjusted for type of anti-diabetic medication use during two years after T2D diagnosis, residual confounding by change in anti-diabetic medication use over time cannot be completely ruled out. In conclusion, among diabetic patients, regardless of use of lipid-lowering drugs, increases in TC level from pre- to post-diagnosis period were associated with elevated CVD risks, while the decreases were associated with reduces CVD risks.
Management of TC level among diabetic patients may be of an important clinical goal to prevent CVD. The National Health Insurance Service NHIS in Korea is the mandatory health insurance system that achieved universal coverage of the population since The NHIS has provided the general health screening programs biennially The cohort included , participants aged 40—79 years in and followed them through The cohort had information regarding demographic and socioeconomic factors, medical history, bioclinical laboratory results, and lifestyle factors.
From the NHIS-HEALS, we selected a total of 27, participants who were diagnosed with T2D between and Diabetic patients were identified based on International Classification of Diseases 10th Revision ICD codes E11, E12, E14 and prescription history of anti-diabetic medication.
Among them, we excluded patients who were diagnosed with CVD or died before the start of study follow-up i. Based on these two measurements, changes in TC levels from pre- to post-diagnosis of T2D were divided into 9 groups: low—low, low—middle, low—high, middle—low, middle—middle, middle—high, high—low, high—middle, and high—high.
The time frame was between the date of T2D diagnosis and the date when the follow-up started i. Covariates included in the multivariable analysis were as follows: age, sex, socioeconomic status, body mass index BMI , smoking status, alcohol consumption, physical activity, systolic blood pressure, fasting serum glucose, history of anti-diabetic medication, and use of lipid-lowering drugs after T2D diagnosis.
Users of lipid-lowering drugs were defined as those who used all kind of lipid-lowering drugs such as statin, fibrate, ezetimibe, and non-users were as those who did not use any kind of lipid-lowering drugs.
Statin users were defined as those who used statin alone or in combination. The primary outcome was non-fatal CVD incidence, defined as two or more days of hospitalization due to CVD as indicated by ICD codes I20—I25, I60—I69 The secondary outcomes were coronary heart disease CHD, I20—I25 and stroke I60—I69 incidences.
If a patient was diagnosed with both CHD and stoke, the earlier diagnosis was used as the outcome. For each pre-diagnostic TC category, the reference group included individuals staying in the same category for both pre- and post-diagnostic period e. For every participant, the start of follow-up i.
To estimate cumulative probability of non-fatal CVD incidence according to changes in TC levels from pre- to post-diagnosis of T2D, we used the Kaplan—Meier method and log-rank test. Heterogeneity in the relationship by CVD subtypes CHD, stroke was also explored. Because lipid abnormalities are common in T2D patients, patients were often prescribed lipid-lowering drugs, which may be an important modifier of the relationship between TC change and CVD risk.
Thus, we also performed sensitivity analysis among statin users. Potential interaction between change in TC levels and use of lipid-lowering drugs was tested by adding their cross-product product term in the model and running the Wald test on it.
Among individuals with high TC levels before T2D diagnosis, some managed to lower their TC levels after T2D diagnosis, which could be attributable to use of lipid-lowering drugs or lifestyle modifications. To identify post-T2D diagnosis factors associated with TC reduction without the help of medication, we performed logistic regression to predict TC decrease e.
On the contrary, among individuals on lipid-lowering drugs, despite their medication use, some failed to lower or even had elevated TC levels after T2D diagnosis.
To identify post-T2D diagnosis factors associated with ineffectiveness of lipid lowering medication, we performed logistic regression to predict TC non-decrease or increase e.
To explore whether the relationship between TC levels and CVD risk differs by 3rd factors, we performed subgroup analyses by variables selected a priori known to influence CVD risk: age, sex, BMI, smoking status, alcohol consumption, and physical activity Supplementary table 5.
All statistical analyses were conducted using SAS 9. Statistically significant results were defined as a two-sided p value less than 0. We conducted this study according to the guidelines stipulated in the Declaration of Helsinki. The institutional review board of Seoul National University Hospital approved this study no.
E and informed consent was waived due to the reason that NHIS-HEALS was distributed after being fully anonymized according to strict confidentiality policies. The database used in this study belongs to the National Health Insurance Service NHIS , and the authors are not authorized to share the data of this study.
do with the permission of the NHIS. Patel, P. et al. Standardized hypertension management to reduce cardiovascular disease morbidity and mortality worldwide.
Article PubMed PubMed Central Google Scholar. Carreras, E. The EBMT handbook: Hematopoietic stem cell transplantation and cellular therapies De Rosa, S.
Type 2 diabetes mellitus and cardiovascular disease: Genetic and epigenetic links. Article Google Scholar. Wang, H.
Association between diabetes mellitus and the risk for major cardiovascular outcomes and all-cause mortality in women compared with men: A meta-analysis of prospective cohort studies. BMJ Open 9 , e Saeedi, P. Global and regional diabetes prevalence estimates for and projections for and Results from the International Diabetes Federation Diabetes Atlas.
Diabetes Res. Article PubMed Google Scholar. Peters, S. Total cholesterol as a risk factor for coronary heart disease and stroke in women compared with men: A systematic review and meta-analysis.
Atherosclerosis , — Article CAS PubMed Google Scholar. Michael, D. MSD MANUAL Consumer Version. Accessed 26 Jan Kim, M. Cholesterol levels and development of cardiovascular disease in Koreans with type 2 diabetes mellitus and without pre-existing cardiovascular disease.
Han, E. Diabetes fact sheets in Korea, An appraisal of current status. Diabetes Metab. Jeong, S. Effect of change in total cholesterol levels on cardiovascular disease among young adults. Heart Assoc. Article CAS PubMed PubMed Central Google Scholar. Corban, M. Combination of plaque burden, wall shear stress, and plaque phenotype has incremental value for prediction of coronary atherosclerotic plaque progression and vulnerability.
Hedayatnia, M. Dyslipidemia and cardiovascular disease risk among the MASHAD study population. Lipids Health Dis. Collaboration, A. Cholesterol, coronary heart disease, and stroke in the Asia Pacific region. Hao, W. The LDL-HDL profile determines the risk of atherosclerosis: A mathematical model.
PLoS One 9 , e Article ADS PubMed PubMed Central Google Scholar. Council, N. Diet and health: Implications for reducing chronic disease risk Libby, P.
Inflammation and atherosclerosis. Circulation , — Sugden, M. Pathophysiology of diabetic dyslipidemia: Implications for atherogenesis and treatment. Jones, J. A Mediterranean-style, low-glycemic-load diet reduces the expression of 3-hydroxymethylglutaryl-coenzyme A reductase in mononuclear cells and plasma insulin in women with metabolic syndrome.
Association, A. Dyslipidemia management in adults with diabetes. Diabetes Care 27 , s68—s71 Standards of medical care in diabetes— abridged for primary care providers.
Diabetes Publ. Diabetes Assoc. Ramsey, S. At-risk drinking among diabetic patients. Substance Abuse Res. Date Archives Year Author Archives Select Author Bob Goodman, Emile R Mohler III, MD, Professor of medicine and director of vascular medicine at Penn Medicine Helene L Glassberg, MD Jason S Fritz, MD.
Share This Page: Post Tweet. Close myPennMedicine PENN Home For Patients and Visitors Close I Want To: How to Make an Appointment at Penn Medicine Find A Doctor Find a Location Access myPennMedicine Pay My Bill. Penn Medicine Locations Hospitals Multispecialty Centers Practices Outpatient Labs.
Patient Information Conditions Treated A-Z Wellness and Patient Support Getting A Second Opinion Clinical Trials Insurance and Billing Traffic and Parking Alerts Patient Access to Health Information.
Find a Program or Service. Close I Want To: Refer My Patient Find A Doctor Find a Location Request Medical Records. For Physicians All Physician Services Education and Resources Transfer a Patient Physician Career Opportunities.
For Nurses and Advanced Practice Advanced Practice Providers Education and Professional Development Nursing Career Opportunities. For Fellows and Residents Hospital of the University of Pennsylvania Lancaster General Health Programs Pennsylvania Hospital Programs Presbyterian Medical Center Programs.
Close Research at Penn Clinical Trials Translational Research. Research Specialty Areas Precision Medicine Liquid Biopsy Diagnostic Tool Research Programs and Interests. Additional Resources Office of Clinical Research Online Research Interviews.
Cholesterola heapth substance, travels around Kiwi fruit retail opportunities your bloodstream in high-density anr HDL and low-density lipoproteins LDL :. Narrowed or blocked arteries can prevent blood anc reaching your heart, brain, or other organs. This can lead to stroke, heart attack, or even heart failure. Your liver produces all the cholesterol you need. But you can also get a lot of cholesterol from food. For decades, research has indicated that diet and cholesterol play a role in heart health.
Ich entschuldige mich, aber meiner Meinung nach lassen Sie den Fehler zu. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden reden.
Mir scheint es der ausgezeichnete Gedanke
die Interessante Variante