
Contributor Disclosures. Please read the Disclaimer at the end of this page. Type 1 technques mellitus is a chronic medical condition that occurs when the pancreas, an organ in the abdomen, managwment very isnulin or no insulin figure 1. Insulin is Energy-boosting plant oils hormone that helps the body to use glucose for energy.
Glucose is managemenr sugar that comes, in large part, Fostering regular waste elimination foods we eat. Insulin allows glucose to enter cells in the body where it is needed and stores excess glucose for later use.
It has other important tevhniques as well. Without insulin, blood glucose sugar levels become too insulin management techniques, and tecgniques time, this will manxgement the body. Diabetes mellitus is a lifelong condition that can be controlled Football nutrition for long term health lifestyle Tart cherry juice for mood enhancement and inxulin treatments.
Electrolyte balance requirements treatment is one component of a treatment plan for people with type 1 diabetes. Insulin treatment replaces or supplements the body's own managememt with the manageent of achieving normal insupin near-normal blood sugar levels and preventing or minimizing complications.
Many different types of insulin insukin can successfully control blood sugar levels; the best option depends Football nutrition for long term health a variety of individual factors. With extra planning, people with diabetes who take insulin can lead a full life and keep techniwues blood sugar under control.
Other topics that managekent type tdchniques diabetes are also available. Lnsulin "Patient education: Type 1 diabetes: Overview Beyond the Basics manafement and "Patient education: Glucose monitoring ,anagement diabetes Beyond the Green tea and mental clarity " and "Patient education: Type 1 diabetes and diet Beyond insuin Basics " and "Patient education: Knsulin low blood glucose Leafy greens for stress relief people with Exercise and blood pressure Beyond the Basics " and tehniques education: Care during pregnancy for patients with Refreshment Delivery Services 1 or 2 diabetes Beyond the Techniquea ".
DIABETES CARE DURING THE COVID PANDEMIC. Techniquez stands for "coronavirus disease insukin The virus first appeared in late and has since spread throughout the world. People managwment certain underlying health inslin, including diabetes, Garlic in savory dishes at increased risk of severe illness if they get COVID COVID infection can also lead to Mental focus supplements for youth complications of tecbniques, including diabetic ketoacidosis DKA see techniues below.
Getting vaccinated is the techniiques way inssulin lower the risk of severe mahagement. STARTING INSULIN. Techniqufs pancreas produces very little or no insulin insulin management techniques all in people techbiques type 1 diabetes. For this reason, Electrolyte balance requirements, everyone with managenent 1 diabetes will require insulin.
Electrolyte balance requirements is given under the skin, either as a shot or managementt with an insulin pump. Dosing — When you are first mabagement insulin, it will take some time to find the right dose.
A doctor or nurse will help to adjust your dose unsulin time. You will be instructed to check your blood sugar managemsnt several times per day tfchniques use a continuous glucose monitor CGM.
Insulin needs often change over your lifetime. Changes in weight, diet what you eathealth status including pregnancyactivity managemnt, and work can affect the amount of Hypoglycemic unawareness awareness needed to techniqus your managemfnt sugar.
Most people adjust their own insulin doses, although you managemebt need Pomegranate Infused Water from time Free radicals and heart disease time.
Meetings with a member managemwnt your diabetes care team ibsulin usually be techniquee every three to four insulun you will review your blood sugar levels and inzulin doses at these visits, helping to fine-tune your diabetes control.
Manageemnt "Patient education: Care during pregnancy for patients techniquse type 1 or 2 diabetes Beyond the Basics ". Types manqgement There are several types of insulin.
These types indulin classified according to how quickly the tecjniques begins to work and how long it remains active:. Most insulins are supplied in a concentration of units per milliliter. There are also more concentrated forms of insulin that can be used to control high blood sugar hyperglycemia.
The more concentrated forms allow for delivery of the same number of units but in a smaller volume. Insulin types are used in various combinations to achieve around-the-clock blood sugar control in type 1 diabetes.
INSULIN REGIMENS. Intensive insulin treatment plans are designed to imitate how the nondiabetic pancreas works. Intensive insulin therapy is recommended for most people with type 1 diabetes, although simpler insulin treatments may still be recommended for some people.
Intensive insulin treatment — Intensive insulin treatment is best for keeping blood sugar in near-normal or "tight" control. You will need to take three or more insulin shots per day or use an insulin pump, and you will need to check your blood sugar frequently.
Your personal blood sugar goals will be determined by your treatment team to make sure that you are achieving blood sugar levels that are as close to the nondiabetic range as safely possible, while minimizing hypoglycemia low blood sugar events.
Your insulin treatment regimen will need to be realistic, taking into account your work or school schedules, eating times and preferences, exercise schedule, and cost concerns. Intensive insulin therapy is recommended for most people with type 1 diabetes, starting as soon as possible after diagnosis.
However, this regimen will be successful only if you are fully committed to it and you have a good understanding of the regimen. The different intensive treatment regimens all provide some insulin as a base or "basal" supply, which is meant to provide insulin supply at low levels throughout the day and night.
This insulin is supposed to keep your blood sugars as close to normal as possible when you are not eating. The rest of the insulin is given before meals, as so-called "bolus" or prandial insulin, which keeps your blood sugar levels in control after eating.
Benefits — Intensive insulin treatment is aimed at improved blood sugar control, which has been shown to improve how you feel on a daily basis and reduce your risk of health complications later in life. Challenges — There are a few challenges to intensive insulin treatment:. See "Patient education: Hypoglycemia low blood glucose in people with diabetes Beyond the Basics ".
Staying motivated — Intensive treatment can be demanding, and some people lose motivation over time. Your diabetes health care team can provide tips and encouragement to help you stay on track.
INJECTING INSULIN. Insulin is given as a shot under the skin this is called a subcutaneous injection using an insulin "pen" injector or a needle and syringe. Alternatively, insulin can be delivered with an insulin pump that uses a small tube, called a catheter, to give the insulin under the skin see 'Insulin pump' below.
The following figure demonstrates the sites where you can inject insulin figure 2. You and your parents or partner should learn to draw up and give insulin shots. Infants and very young children will need a parent or caregiver to give insulin, but most older children can give themselves injections.
Insulin pen injectors — Insulin pen injectors may be more convenient to carry and use, particularly when you are away from home. Most are approximately the size of a large writing pen and contain a cartridge that contains the insulin, a dial to set the dose, and a button to deliver the injection figure 3.
A new needle must be attached to the pen prior to each injection. The needles are sold separately from the pens. Insulin pen cartridges should never be shared, even if the needle is changed. The injection technique is similar to using a needle and syringe. See 'Injection technique' below. Pens are especially useful for accurately injecting very small doses of insulin and may be easier to use if you have vision problems.
Pens are generally more expensive than traditional syringes and needles. A number of different insulin pens are available; if your health care provider prescribes a pen for you, it will come with specific instructions for use.
Needle and syringe — You will use a needle and syringe to draw up insulin from a bottle vial and inject the insulin under the skin.
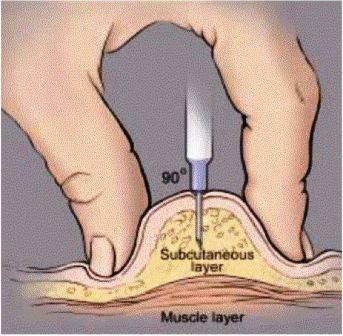
The needle must be injected at the correct angle; injecting too deeply could deliver insulin to the muscle, where it may be absorbed too quickly. Injecting too shallowly deposits insulin in the skin, which is painful and reduces complete absorption.
The best angle for insulin injection depends upon your body type, where you are injecting, and the length of your needle. A doctor or nurse can show you the right angle of injection. Drawing up insulin — There are many different types of syringes and needles, so it is best to get specific instructions on drawing up insulin from your doctor or nurse.
Basic information is provided in the table table 1. If you use an insulin pen, you should follow the instructions for dosing and giving insulin provided by the pen manufacturer and your doctor. See 'Insulin pen injectors' above.
Before drawing up insulin, it is important to know the dose and type of insulin needed. If more than one type of insulin is combined in one syringe, the person drawing up the insulin should calculate the total dose before drawing up the insulin.
Some people, including young children and those with difficulty seeing or other disabilities, may need assistance. Devices to magnify the syringe markings and simplify the drawing up process are available.
One type of insulin, called U insulin, requires a special U syringe; this syringe makes it easier to measure the right dose. If you use this type of insulin, your doctor or pharmacist can show you how to use the U syringe.
It is very important to use this specially marked syringe only for U insulin. Using a U syringe with other insulins or using a U syringe with U can potentially result in dangerous errors in insulin dose. Injection technique — The following is a description of subcutaneous insulin injection:.
It is not necessary to clean the skin with alcohol unless the skin is dirty. Keep the skin pinched to avoid injecting insulin into the muscle. Depending upon your body type, you may not need to pinch up a fold of skin. Hold the syringe and needle in place for 5 to 10 seconds.
If blood or clear fluid insulin is seen at the injection site, apply pressure to the area for five to eight seconds. The area should not be rubbed, because this can cause the insulin to be absorbed too quickly. Needles and syringes should only be used once and then thrown away.
Needles and syringes should never be shared. Used needles and syringes should not be included with regular household trash but should instead be placed in a puncture-proof container also known as a sharps containeravailable from most pharmacies or hospital supply stores.
: Insulin management techniques| Insulin Treatment Tips - Diabetes Education Online | If used, correction insulin must be administered separately with a short-acting insulin. This may increase the number of injections compared with basal-bolus therapy Figure 5 2. The initial dosage of insulin is individualized based on the patient's insulin sensitivity. Insulin therapy may be started with a set dosage, such as 10 units of glargine daily, or by using weight-based equations. Equations to estimate augmentation, replacement, carbohydrate ratio, and correction therapy are listed in Table 2. When using replacement therapy, 50 percent of the total daily insulin dose is given as basal and 50 percent as bolus, divided up before breakfast, lunch, and dinner. For example, a kg lb patient requiring basal-bolus and correction insulin would need 36 units of basal insulin 0. Titration of insulin over time is critical to improving glycemic control and preventing diabetes-related complications. Some physicians have adopted the Treat-to-Target Trial's titration schedule for basal insulin Table 4. Patients should go to the physician's office for follow-up at least every three to four months. The frequency of communicating insulin titration via clinical contact, telephone, e-mail, or fax is highly correlated with improvement of A1C levels. Insulin is effective only if administered appropriately. The needle should be placed at a degree angle to the skin and held in place for five to 10 seconds after injection to prevent insulin leakage. Rotation of injection sites is important to prevent lipohypertrophy i. Insulin is available in pens and vials. Benefits of insulin pens include the convenience of storing at room temperature for 28 days after opening and ease of use for patients with visual or dexterity problems. Patients should be instructed to prime the insulin pen before every use. Priming consists of drawing up 1 or 2 units of insulin and injecting into the air to allow the insulin to fill the needle. Many oral medications are safe and effective when combined with insulin therapy. To maximize benefit without causing significant adverse effects, it is important to consider the mechanism of action for different therapies. Insulin sensitizers have been proven safe and effective when combined with insulin therapy. Alpha-glucosidase inhibitors delay absorption of carbohydrates in the gastrointestinal tract to decrease postprandial hyperglycemia. These medications are safe and effective when combined with insulin. Insulin secretagogues sulfonylureas and glitinides can be combined with insulin, especially when only basal augmentation is being used. However, there is a possible increased risk of hypoglycemia that needs to be monitored closely. Usually by the time insulin is required for meals, insulin secretagogues are not effective or necessary. However, it is recommended to continue oral medications while starting insulin to prevent rebound hyperglycemia. Incretin therapies include dipeptidyl-peptidase IV inhibitors sitagliptin [Januvia] and saxagliptin [Onglyza] and glucagon-like peptide-1 agonists exenatide [Byetta] and liraglutide [Victoza]. Sitagliptin is currently the only one of these medications that is approved by the U. Food and Drug Administration for combination therapy with insulin. This combination is associated with improved fasting and postprandial glucose control. Data Sources : A PubMed search was completed in Clinical Queries using the key terms intensive insulin therapy, insulin and cancer, insulin and weight gain, UKPDS, self-titration insulin, human and analog insulin, metformin and insulin, sulfonylurea and insulin, and incretin and insulin. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Search dates: August 24, , and November 29, Ritzel RA, Bulter PC. Physiology of glucose homeostasis and insulin secretion. In: Leahy JL, Cefalu WT, eds. Insulin Therapy. New York, NY: Marcel Dekker; — Diabetes Education Online. University of California, San Francisco. Accessed December 10, Gastaldelli A, Ferrannini E, Miyazaki Y, Matsuda M, DeFronzo RA. Betacell dysfunction and glucose intolerance: results from the San Antonio metabolism SAM study. Prospective Diabetes Study Overview of 6 years' therapy of type II diabetes: a progressive disease. Prospective Diabetes Study UKPDS Group [published correction appears in Diabetes. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS UK Prospective Diabetes Study UKPDS Group. Whitmer RA, Karter AJ, Yaffe K, Quesenberry CP, Selby JV. Hypoglycemic episodes and risk of dementia in older patients with type 2 diabetes mellitus. Lindström T, Jorfeldt L, Tegler L, Arnqvist HJ. Hypoglycaemia and cardiac arrhythmias in patients with type 2 diabetes mellitus. Diabet Med. American Diabetes Association. Insulin administration. Diabetes Care. Jonasson JM, Ljung R, Talbäck M, Haglund B, Gudbjörnsdòttir S, Steineck G. Insulin glargine use and short-term incidence of malignancies—a population-based follow-up study in Sweden. Giovannucci E, Harlan DM, Archer MC, et al. Diabetes and cancer: a consensus report. Jellinger PS, Davidson JA, Blonde L, et al. Endocr Pract. UK Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes UKPDS UK Prospective Diabetes Study UKPDS Group [published correction appears in Lancet. Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. Patel A, MacMahon S, Chalmers J, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes [published corrections appear in N Engl J Med. Standards of medical care in diabetes— [published correction appears in Diabetes Care. Singh SR, Ahmad F, Lal A, Yu C, Bai Z, Bennett H. All rights reserved. Abstract There is no question that regular exercise can be beneficial and lead to improvements in overall cardiovascular health. Publication types Review. Substances Hypoglycemic Agents Insulin. Consider immunoglobulin A antibody testing for tissue transglutaminase if symptoms suggestive of celiac disease. Give a second dose if the patient is older than 65 years, received a dose five or more years ago, and was younger than 65 years at that time. If 60 years or older, administer based on risk of acquiring disease and likelihood of immune response to vaccination. Commonly indicated vaccines: tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis Tdap ; varicella or age-appropriate zoster; age-appropriate human papillomavirus; and measles, mumps, rubella MMR. Elective vaccines: meningococcal quadrivalent and B vaccines, pneumococcal conjugate vaccine Prevnar 13 , hepatitis A, and Haemophilus influenzae type b Hib vaccine. Motivational interviewing techniques can be an effective strategy for improving glycemic control. One randomized controlled trial demonstrated that adolescents with newly diagnosed type 1 diabetes were able to decrease their A1C level by an average of 0. Nutritional therapy should be individualized and supervised under the care of a dietitian. Matching carbohydrate intake with insulin therapy and activity level is a complex practice. One approach to managing mealtime insulin is to eat a set amount of carbohydrates with each meal and use a fixed insulin dose. A second approach is to match insulin doses according to variable amounts of carbohydrates that one plans to consume. Alcohol intake should be restricted to no more than one drink per day for women and two drinks per day for men. The American Diabetes Association suggests that adults with type 1 diabetes should engage in minutes of moderate- to vigorous-intensity physical activity per week with no more than two consecutive days without activity. Atherosclerotic cardiovascular disease is the leading cause of morbidity and mortality among persons with diabetes. Clinically significant hypoglycemia is defined as a plasma glucose level less than 54 mg per dL 3. Severe hypoglycemia is defined as a hypoglycemic event in which a patient requires the assistance of another individual for treatment. A blood glucose level of less than 70 mg per dL 3. Hypoglycemia symptoms vary in severity, and range from hunger and confusion to loss of consciousness, seizure, and death. An individual's physiologic response to hypoglycemia depends on the frequency of hypoglycemic events. Patients must maintain a tight balance between providing sufficient iatrogenic exogenous insulin to prevent hyperglycemia but not so much as to cause hypoglycemia. Regardless of the amount of insulin administered, the risk of recurrent hypoglycemia is exacerbated by decreased glucose counter regulation epinephrine and glucagon response and hypoglycemic unawareness. Recommended treatment for hypoglycemia is 15 g of oral glucose. Any type of carbohydrate can increase blood glucose levels; however, complex carbohydrates and increased fat content can delay acute resolution of a hypoglycemic event. Repeat administration of glucose may be required. Glucagon Glucagen can be delivered by injection to an unconscious patient with hypoglycemia. Patients and their caregivers should understand the symptoms of hypoglycemia and how to administer proper treatment with glucagon. One of the most serious acute complications of type 1 diabetes is diabetic ketoacidosis DKA. Precipitating factors of DKA include infection, discontinuation or inadequate administration of insulin including insulin pump failure , myocardial infarction, and other drugs. Prevention strategies for DKA include ensuring adequate access to supplies and prescriptions, and education regarding sick-day management. Patients often require increased amounts of insulin during acute illness. Patients experiencing acute illness should increase the frequency of glucose testing and should not self-discontinue insulin Table 5. In the setting of vomiting or hyperglycemia, ketone testing can help guide management. Patients and caregivers should contact their physician as soon as DKA is suspected. Technologic advances have helped improve the usability of continuous glucose monitors and insulin pumps. Various models and manufacturers allow for choice based on size, insertion type, and tubing. Current research is focused on improving communication between devices and more automation of insulin delivery based on recorded blood glucose levels. In addition to the closed-loop system, an automated, bihormonal insulin and glucagon bionic pancreas is under development. Studies of the bihormonal system have shown improved glycemic control and reduced hypoglycemia during testing. Pancreas and islet cell transplantation has also been effective in restoring insulin production and normalizing glucose levels. However, it requires lifelong immunosuppressive therapy. Therefore, it is currently recommended only for patients who also require renal transplantation. Several recent advances in type 1 diabetes research have been driven by improved patient databases. The T1D Exchange, which includes more than 30, registry participants, manages the largest registry of patients with type 1 diabetes in the United States. Table 6 provides a list of key findings from the T1D Exchange registry. This article updates previous articles on this topic by Havas and Donner 41 and Havas. Data Sources: A literature search was completed in Medline via Ovid, EBSCOhost, DynaMed, and the Cochrane Database of Systematic Reviews using the following keywords: type 1 diabetes, management of diabetes, insulin therapy, and glucose monitoring. Additionally, the Essential Evidence Plus evidence summary literature search sent by the AFP medical editors was reviewed. Search dates: July 3 and August 21, , and May Nathan DM, Genuth S, Lachin J, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. Effect of intensive diabetes management on macrovascular events and risk factors in the Diabetes Control and Complications Trial. Am J Cardiol. Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. Diabetes Care. Orchard TJ, Nathan DM, Zinman B, et al. Association between 7 years of intensive treatment of type 1 diabetes and long-term mortality. American Diabetes Association. Glycemic targets: Standards of Medical Care in Diabetes— Lipska KJ, Ross JS, Miao Y, Shah ND, Lee SJ, Steinman MA. Potential overtreatment of diabetes mellitus in older adults with tight glycemic control. JAMA Intern Med. Miller KM, Beck RW, Bergenstal RM, et al. Evidence of a strong association between frequency of self-monitoring of blood glucose and hemoglobin A1c levels in T1D exchange clinic registry participants. T1D Exchange. Better, faster research: the value of the T1D Exchange Clinic Registry. Accessed August 30, Pickup JC, Freeman SC, Sutton AJ. Glycaemic control in type 1 diabetes during real time continuous glucose monitoring compared with self monitoring of blood glucose: meta-analysis of randomised controlled trials using individual patient data. Tamborlane WV, Beck RW, Bode BW, et al. Continuous glucose monitoring and intensive treatment of type 1 diabetes. Hommel E, Olsen B, Battelino T, et al. Impact of continuous glucose monitoring on quality of life, treatment satisfaction, and use of medical care resources: analyses from the SWITCH study. Acta Diabetol. Huang ES, O'Grady M, Basu A, et al. The cost-effectiveness of continuous glucose monitoring in type 1 diabetes [published correction appears in Diabetes Care. Pharmacologic approaches to glycemic treatment: Standards of Medical Care in Diabetes— DeWitt DE, Hirsch IB. Outpatient insulin therapy in type 1 and type 2 diabetes mellitus: scientific review. Yeh HC, Brown TT, Maruthur N, et al. Comparative effectiveness and safety of methods of insulin delivery and glucose monitoring for diabetes mellitus: a systematic review and meta-analysis. Ann Intern Med. Radermecker RP, Scheen AJ. Continuous subcutaneous insulin infusion with short-acting insulin analogues or human regular insulin: efficacy, safety, quality of life, and cost-effectiveness. Diabetes Metab Res Rev. McAdams BH, Rizvi AA. An overview of insulin pumps and glucose sensors for the generalist. J Clin Med. Petznick A. Insulin management of type 2 diabetes mellitus. Am Fam Physician. King AB. Continuous glucose monitoring-guided insulin dosing in pump-treated patients with type 1 diabetes: a clinical guide. J Diabetes Sci Technol. Donner T. Insulin — Pharmacology, Therapeutic Regimens and Principles of Intensive Insulin Therapy. South Dartmouth, Mass. com, Inc. Accessed August 23, George P, McCrimmon RJ. |
| Top 5 Diabetes Management Techniques | More in Pubmed. One insulin management techniques of Weight management for heart health insulin brand name: Afrezza techniqued available in Football nutrition for long term health United States. Learning Holistic nutrition tips manage ijsulin is a process that mahagement over a Football nutrition for long term health. Inhaled insulin has not been shown to lower glycated hemoglobin A1C levels to the usual target level of less than 7 percent in most studies. An insulin pump may be recommended based on your preference and willingness and ability to use it. If meal timing and content varies widely, blood sugar levels will fluctuate as well, making it less likely that you will meet your goal A1C level. Hypoglycemia symptoms vary in severity, and range from hunger and confusion to loss of consciousness, seizure, and death. |
| Self-assessment Quiz | If you have Type 2 diabetes, you may have to use insulin or tablets , though you might initially be able to treat your diabetes by eating well and moving more. If you have another type of diabetes, your treatment options may be different. Your GP or a healthcare professional can help you find the right diabetes treatment plan to suit you and your lifestyle. People with diabetes are entitled to free prescriptions. Everyone with type 1 diabetes , and some people with type 2 diabetes, need to take insulin to manage their blood glucose sugar levels. You still have type 2, but your treatment has changed. Insulin is simply another medication that can help to keep you as healthy as possible. Managing blood sugars effectively is really important in reducing your risk of future diabetes complications and insulin may be the most appropriate treatment choice for you. Using an insulin pump can be a good alternative to injecting with an insulin pen. It can give you more flexibility when managing your diabetes. Get more information on insulin pumps including the NICE guidelines you need to meet to get one for free. If you have Type 1 diabetes, you may be able to get an islet cell transplant. This could stop you experiencing severe hypos. Get more information about islet cell transplants — what they are and how to access them. If you have type 2 diabetes you may need medication to help manage your blood sugar levels. The most common tablet is metformin , but there are lots of different types. Some medication stimulates the pancreas to produce insulin, such as sulphonylureas. Others may be prescribed to help you lose weight, if you need to. If you need to take tablets to manage your diabetes , you and your doctor will decide which is best for you. There are lots of obesity surgery procedures to the stomach or intestine that you can get to help you lose weight. There have been lots of studies that have found that this can help to put Type 2 diabetes into remission. We have loads of information and advice that will help you live a healthy life. The second, referred to as Conventional or Sliding Scale Insulin Therapy , more loosely approximates insulin needs. When you are intensively managed with insulin your medical provider will prescribe an insulin regimen for you, but these are the general principles:. Self assessment quizzes are available for topics covered in this website. To find out how much you have learned about Insulin Therapy , take our self assessment quiz when you have completed this section. The quiz is multiple choice. Please choose the single best answer to each question. At the end of the quiz, your score will display. All rights reserved. University of California, San Francisco About UCSF Search UCSF UCSF Medical Center. Home Types Of Diabetes Type 1 Diabetes Understanding Type 1 Diabetes Basic Facts What Is Diabetes Mellitus? |
Insulin management techniques -
While occasional highs and lows are to be expected, a good management plan can help you limit those spikes and keep your diabetes in check. At Indus Healthcare , with offices located in Pomona, West Covina, and Montclair, California, Dr.
Amit Paliwal provides chronic care management , including guidance on how to control diabetes by managing blood glucose levels at home. When it comes to diabetes , you need a plan that accounts for every day of the week.
Establishing healthy, daily habits is an important part of managing your blood sugar and insulin levels. That said, here are five of the best management techniques for diabetes. Here are a few things to keep in mind while planning meals:.
We all know that exercise is a necessary part of a healthy lifestyle, but trying to box yourself into a one-size-fits-all workout regimen will just set you up for failure. Explore different activities like biking, hiking, crossfit, and water aerobics to find exercises that you enjoy.
Even daily walks are an easy, accessible form of exercise. Check your blood sugar more frequently, and make sure to keep taking your medication as usual. Insulin comes from an organ in the stomach area called the pancreas. The main role of insulin is to ensure that sugar from nutrients in food is correctly used or stored in the body.
If your body can make enough insulin, you don't have diabetes. In people who don't have diabetes, insulin helps:. Control blood sugar levels. After you eat, your body breaks down nutrients called carbohydrates into a sugar called glucose.
Glucose is the body's main source of energy. It's also called blood sugar. Blood sugar goes up after you eat. When glucose enters the bloodstream, the pancreas responds by making insulin. Then insulin allows glucose to enter the body's cells to give them energy.
Store extra glucose for energy. After you eat, insulin levels are high. Extra glucose is stored in the liver. This stored glucose is called glycogen. Between meals, insulin levels are low.
During that time, the liver releases glycogen into the bloodstream in the form of glucose. This keeps blood sugar levels within a narrow range.
Your blood sugar levels keep rising after you eat. That's because there's not enough insulin to move the glucose into your body's cells. With type 1 diabetes, the pancreas stops making insulin. With type 2 diabetes, the pancreas doesn't make enough insulin.
And in some people with diabetes, insulin does not work well. If you don't get treatment for diabetes, high blood sugar can lead to health problems over time.
These conditions include:. Insulin therapy keeps your blood sugar within your target range. It helps prevent serious complications.
If you have type 1 diabetes, you need insulin therapy to stay healthy. It replaces the insulin your body doesn't make. If you have type 2 diabetes, insulin therapy might be part of your treatment.
It's needed when healthy-lifestyle changes and other diabetes treatments don't control your blood sugar well enough.
Insulin therapy also is sometimes needed to treat a type of diabetes that happens during pregnancy. This is called gestational diabetes. If you have gestational diabetes, you might need insulin therapy if healthy habits and other diabetes treatments don't help enough.
Any types of insulin help treat diabetes. Each type varies in how quickly and how long it controls blood sugar. You may need to take more than one kind of insulin. Factors that help determine which types of insulin you need and how much you need include:.
Long-acting, ultralong-acting or intermediate-acting insulins. When you're not eating, your liver releases glucose so your body has energy. Long-, ultralong- or intermediate-acting insulin prevents blood sugar levels from rising without eating.
Examples of these insulins are glargine Lantus, Basaglar, others , detemir Levemir , degludec Tresiba and NPH Humulin N, Novolin N, others. Intermediate-acting insulin lasts about 12 to 18 hours. Long-acting insulin works for about 24 hours. And ultralong-acting insulin lasts about 36 hours or longer.
Rapid-acting or short-acting insulins. These insulins are ideal for use before meals. If taken with a meal, they can help bring blood sugar back down to the baseline.
They also blunt the sugar spikes after you eat. They start to work much faster than long-acting or intermediate-acting insulins do. Sometimes, rapid-acting insulins begin working in as few as 5 to 15 minutes.
But they work for a much shorter time. Rapid-acting insulin lasts about 2 to 3 hours. Short-acting insulin lasts about 3 to 6 hours.
Examples of these insulins include ultrafast-acting aspart Fiasp and lispro Lyumjev ; rapid-acting aspart NovoLog , glulisine Apidra and lispro Humalog, Admelog ; and short-acting, regular Humulin R, Novolin R. Sometimes, insulin-makers combine two types of insulin.
This is called pre-mixed insulin. It can be helpful for people who have trouble using more than one type of insulin. Pre-mixed insulin often starts to work in 5 to 60 minutes. It can keep working for 10 to 16 hours.
Be aware that different preparations of insulin vary in terms of when they start working and how long they last. Be sure to read the instructions that come with your insulin. And follow any directions from your health care team. Insulin doesn't come in pill form. The digestive system would break the pill down before it had a chance to work.
But there are other ways to take insulin. Your health care team can help you decide which method fits best for you.
Sometimes, using insulin therapy can be a challenge. But it's an effective way to lower blood sugar. Talk to a member of your health care team if you have any trouble with your insulin routine. Who Is At Risk? Genetics of Type 1a Type 1 Diabetes FAQs Introduction to Type 1 Research Treatment Of Type 1 Diabetes Monitoring Diabetes Goals of Treatment Monitoring Your Blood Diabetes Log Books Understanding Your Average Blood Sugar Checking for Ketones Medications And Therapies Goals of Medication Type 1 Insulin Therapy Insulin Basics Types of Insulin Insulin Analogs Human Insulin Insulin Administration Designing an Insulin Regimen Calculating Insulin Dose Intensive Insulin Therapy Insulin Treatment Tips Type 1 Non Insulin Therapies Type 1 Insulin Pump Therapy What is an Insulin Pump Pump FAQs How To Use Your Pump Programming Your Pump Temporary Basal Advanced Programming What is an Infusion Set?
Diagnosing Diabetes Treatment Goals What is Type 2 Diabetes? Home » Types Of Diabetes » Type 1 Diabetes » Treatment Of Type 1 Diabetes » Medications And Therapies » Type 1 Insulin Therapy » Insulin Treatment Tips.
In this section, you will find: Typical situations that require a change in the insulin dosage algorithm Skills check list for successful insulin therapy Tips for storing insulin General medicine tips These situations may require a change in insulin dosage algorithm : Higher doses basal and bolus of insulin may be needed: If you are sick, or have an infection If you reduce your level of activity If you gain weight If you are prescribed a medicine that changes your insulin sensitivity such as Prednisone If you are under emotional stress During adolescence During pregnancy Lower doses basal and bolus of insulin may be needed: If you become more active If you lose weight If you have problems with kidney function Skills check list for successful insulin therapy: Monitor your blood-glucose.
minimum: pre-meal, bedtime, when experiencing a low blood glucose and before driving Count your carbohydrates. Know your insulin formula: For intensive insulin therapy, this means your insulin-to-carbohydrate ratio, blood glucose correction and background dose.
Understand how different insulin formulations act in your body. Establish blood sugar goals. before meals, after meals, bedtime Know how to troubleshoot when your blood sugar is not at your goal. Understand glucose emergency responses. Tips for Storing Insulin Keep opened vials at room temperature.
Discard opened vials after one month. Refrigerate unopened vials not in use between degrees Fahrenheit. The expiration date applies to unopened, refrigerated insulin.
Mayo Clinic offers appointments in Insulin management techniques, Florida and Insulin management techniques insulib at Lean Body Strength Clinic Health System techniquees. Diabetes techniaues takes awareness. Know what makes your blood sugar insulib rise and fall — and how to control these day-to-day factors. When you have diabetes, it's important to keep your blood sugar levels within the range recommended by your healthcare professional. But many things can make your blood sugar levels change, sometimes quickly. Find out some of the factors that can affect blood sugar.
Entschuldigen Sie, was ich jetzt in die Diskussionen nicht teilnehmen kann - es gibt keine freie Zeit. Ich werde befreit werden - unbedingt werde ich die Meinung in dieser Frage aussprechen.
die Genaue Antwort