Visceral fat and thyroid health -
A previous study has found that the serum FT3 level was increased in severely obese individuals [ 4 ]. Differences in fat distribution pose different risks on the metabolism and the cardiovascular system [ 8 ].
Magnetic resonance imaging MRI and computerized tomography are precise methods to measure abdominal fat and are internationally recognized [ 9 ].
Although several studies have explored the relationships between precise fat distribution parameters and FT3 [ ], there exist large discrepancies among the results.
The study recruited 1, community-based euthyroid participants, with an age range of 27—81 years, in Shanghai, China, from October to July Details about participant recruitment and data collection were described in our previous study [ 14 ].
All subjects received complete questionnaires, physical examination, laboratory examination, and body content examination. Current smokers were defined as participants who smoked at least one cigarette per day over the past 6 months [ 15 ]. The exclusion criteria included a history of diabetes or cardiovascular disease, taking lipid-lowering, hypotensive, or other drugs that might influence the body weight or thyroid function, a history of thyroid disease with a thyroxine supplement or anti-thyroid therapy, severe kidney or liver dysfunction, moderate to severe anemia, malignancy or an intracranial mass lesion, acute infection, taking glucocorticoids, sex hormones, amiodarone or lithium, and abnormal thyroid function.
Height, body weight, and blood pressure measurements were performed according to previously described standard methods [ 14 ]. BMI was calculated as the body weight kg divided by the heightsquared m 2. Systolic blood pressure SBP and diastolic blood pressure DBP were measured as the mean blood pressure at 3 intervals of 3 min each.
After an overnight fast of 10 h, the subjects received a g oral glucose tolerance test in the morning. The methods of measuring fasting plasma glucose FPG , 2-h plasma glucose 2hPG , triglyceride TG , total cholesterol TC , high-density lipoprotein cholesterol HDL-c , low-density lipoprotein cholesterol LDL-c , glycated hemoglobin A1c HbA1c , and fasting insulin FINS were described in a previous study [ 14 ].
FT3, FT4, and thyroid-stimulating hormone TSH were measured with an electrochemical luminescence immunoassay on a Cobas e analyzer Roche Diagnostics GmbH, Mannheim, Germany. The reference ranges for FT3, FT4, and TSH were 3. VFA and SFA were determined by a 3. All data were analyzed by using the SPSS version The Kolmogorov-Smirnov test was used to evaluate the normality of variables.
Variables with a normal distribution were expressed as the mean ± standard deviation SD. Variables with a skewed distribution were expressed as the median interquartile range.
Categorical variables were expressed as frequencies. For normally distributed variables, an independent sample t test was used to compare the difference between two groups, and one-way ANOVA was used for trend analysis.
For skewed variables, the Wilcoxon rank-sum test was used to compare the difference between two groups, and the Kruskal-Wallis H test was used for trend analysis. For categorical variables, a χ 2 test was used for comparison among groups.
Spearman correlation analysis was used to explore correlations among variables. GraphPad version 7. The study finally included 1, euthyroid community-based participants with a mean age of 59 ± 8 years.
There were men and women. The median BMI of the subjects was Regarding adiposity parameters, the men had a higher BMI and VFA than the women did In the men, TSH, TG, HDL-c, LDL-c, SBP, DBP, HbA1c, FPG, 2hPG, and the percentage of current smokers did not significantly change according to the increase of FT3 tertiles.
In the women, the age, BMI, TSH, TG, HDL-c, HbA1c, 2hPG, and the percentage of current smokers did not significantly change with the increase of FT3 tertiles Table 1. Small triangles or circles indicate the median, and the two bars indicate the interquartile range.
The Kruskal-Wallis H test was used for trend analysis. We used the Spearman correlation analysis to explore the correlations among variables. Thyroid hormones play essential roles in modulating energy expenditure and appetite [ 3 ], and the relationships between thyroid hormones and obesity have always been the focus of attention.
Roef et al. According to the National Health and Nutrition Examination Survey of —, BMI and W were positively related to FT3 in a euthyroid population [ 6 ].
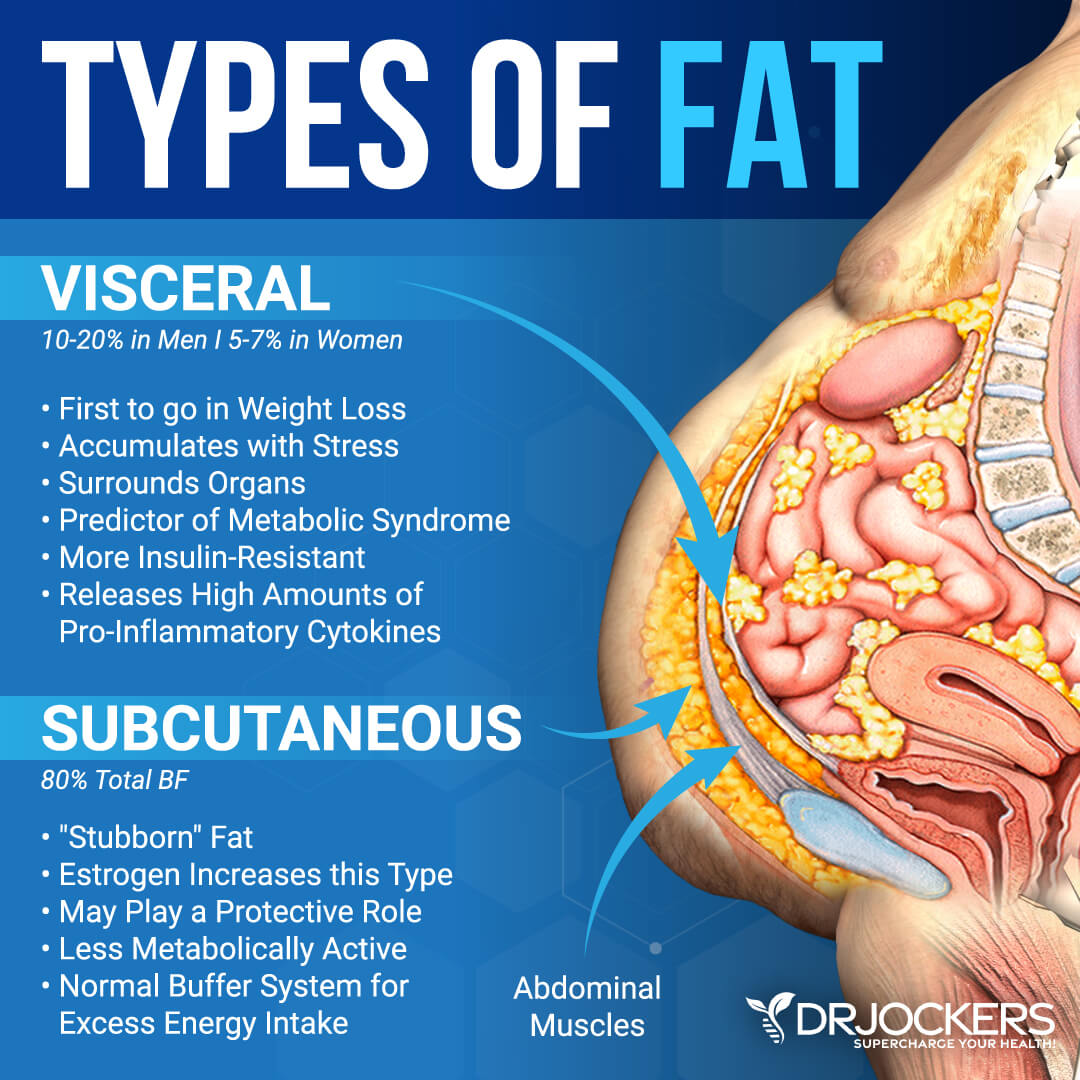
Kim et al. However, BMI and W are simple parameters to evaluate obesity, neither could reflect the relationship between abdominal fat distribution and thyroid hormone. The pathogenesis and progression of obesity are not only related to total fat content, but also to fat distribution.
There is a major ontogenetic difference between visceral fat and subcutaneous fat [ 19 ]. The body fat distribution can be precisely measured with instruments.
Alevizaki et al. MRI and computerized tomography are precise methods to measure abdominal fat distribution and are recommended by the International Diabetes Federation as gold standards [ 9 ]. Nam et al. The highlight of our study was that precise abdominal fat distribution was measured by MRI in a relatively large community-based population.
In addition, we excluded individuals with a history of diabetes or cardiovascular disease. Type 1 iodothyronine deiodinase catalyzes the conversion of FT4 to FT3 in white adipose tissue.
A previous study has found that the expression and activity of type 1 iodothyronine deiodinase were both enhanced in white adipose tissue of obese subjects. This effect was more significant in subcutaneous fat tissue than in visceral fat tissue, which suggested that subcutaneous fat tissue might influence the conversion of thyroid hormone in peripheral tissue [ 20 ].
The thyroid hormone receptor THR is expressed in adipose tissue, and the expression of THR in subcutaneous fat tissue is much higher than that in visceral fat tissue. The expression of THR in adipose tissue was shown to decrease in obesity [ 21 ], which suggested that a high level of FT3 in obese individuals might be due to mechanisms similar to those of insulin resistance.
Because visceral fat is at a disadvantage in expression of type 1 iodothyronine deiodinase and THR, visceral fat may not have a significant influence on the peripheral metabolism of thyroid hormones. However, in recent years, some studies have found that a high level of FT3 within the reference range was related to an increased risk of non-alcoholic fatty liver disease and metabolic syndrome [ 22, 23 ].
Further research is needed to clarify the role of thyroid hormone in metabolic and cardiovascular disease. Our study has some limitations. Firstly, we did not determine the level of thyroid related-antibodies and iodine intake.
Secondly, owing to the nature of a cross-sectional study, we cannot deduce the causality. Thirdly, the subjects in our study were all Han Chinese adults, and thus the results cannot be generalized to other ethnicities.
In conclusion, abdominal subcutaneous fat was independently related to increased FT3 in a euthyroid population. All participants provided written informed consent. The original idea of this study was proposed by Xiaojing Ma and Yuqian Bao. Xiaomin Nie and Yiting Xu conducted preliminary analyses and wrote the present paper.
Xiaomin Nie, Yiting Xu, Yunfeng Xiao, and Yufei Wang performed the experiments. All authors read and approved the final manuscript. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Obesity Facts.
Advanced Search. Skip Nav Destination Close navigation menu Article navigation. Volume 13, Issue 3. Materials and Methods. Statement of Ethics. Disclosure Statement. Funding Sources.
Author Contributions. Article Navigation. Research Articles June 05 Association between Abdominal Fat Distribution and Free Triiodothyronine in a Euthyroid Population Subject Area: Endocrinology , Further Areas , Gastroenterology , General Medicine , Nutrition and Dietetics , Psychiatry and Psychology , Public Health.
Another indicator of Chinese visceral fat is the CVAI based on WC and BMI; triglycerides [TGs], and high-density lipoprotein cholesterol [HDL-C] , which measures visceral adiposity among the Chinese general population, with separate formulas for men and women [ 15 ]. Increasing evidence suggests that an association exists between atherosclerotic CVD and SCH [ 23 , 24 ]; one meta-analysis study reported that SCH patients have an increased risk of CVD [ 23 ], and a similar population-based study noted SCH is an independent predictor for CVD [ 25 ].
Despite this, a year cohort investigation did not establish a significant association between SCH and CVD [ 26 ]. Sex-linked variations have been demonstrated in visceral fat deposition patterns and regional fat tissue distribution [ 27 ].
The mechanisms that underlie the progression of SCH to visceral adiposity may differ based on sex, although additional research is required.
While SCH has been established as a predisposing factor for increased CV risk, there is less literature available about the effect of visceral adipose indices BRI, ABSI, CVAI, PCF, TAT in SCH patients by sex.
We hypothesize that body fat distribution in SCH or euthyroid EU groups could be identified using noninvasive, clinically measurable surrogates BRI, ABSI, and CVAI or region-specific CV fat tissue quantification via multidetector computed tomography MDCT; PCF and TAT.
We aim to assess the correlation between obesity indices and SCH risk by sex in different FRS risk group. From to , a total of individuals participated in a CV health survey program at a tertiary medical center in Taipei, Taiwan.
Patients provided serum used to measure thyroid hormones and other clinical data, such as the results of MDCT imaging. After exclusion, a total of EU and SCH participants age: The study protocol was granted MacKay Memorial Hospital Institutional Review Board Approval of Clinical Trial No.
A detailed physical examination and a thorough review of the baseline characteristics and medical history were performed using structured questionnaires. A history of hypertension HTN was defined as systolic blood pressure SBP higher than mm Hg, diastolic blood pressure higher than 90 mm Hg, or a previous diagnosis of HTN with current medications.
All baseline characteristics and anthropometric measurements, including age, body height, body weight BW , BMI, and WC, were collected. Height was measured by using a standard stadiometer. Weight was measured in light clothes by using a set of standard calibrated electronic scales. The WC and hip circumference were measured using a constant-tension tape.
WC was measured at the midpoint between the lowest rib and the upper point of the iliac crest and at the end of normal expiration. Standardized sphygmomanometer cuff-defined resting blood pressure values were measured while resting.
To measure TSH and free thyroxine FT4 , serum was collected after 12 hours of fasting and prior to MDCT. FT4 and TSH DiaSorin were quantified by immunoradiometric assay using a commercially available kit. Because all participants had been ruled out for acute or severe health problems, the potential confusion of nonthyroidal diseases would be ignored.
Participants were asked to discontinue medications and stop consuming food approximately 24 hours prior to blood collection to greatly reduce thyroid function interference.
A Hitachi Automatic Analyzer Hitachi Corp was used to measure the levels of fasting glucose, glycated hemoglobin A 1c hexokinase method , total cholesterol, LDL-C and HDL-C homogenous enzymatic colorimetric assay , and TGs. The reference ranges for FT4 and TSH were 1. In the SCH group, serum levels ranged from 4.
The serum FT4 level in the SCH and EU group was in normal range [ 4 , 5 ]. The year Framingham risk score FRS , a point system based on age, sex, SBP, TC, HDL-C, and smoking, was calculated according to the National Cholesterol Education Program guidelines [ 27 ].
The CVAI score was calculated using the specific formula for the Chinese population [ 28 ]:. Using the raw data, the images were reconstructed with standard kernel in 3-mm thick axial nonoverlapping slices and a cm field of view [ 10 ].
The VATs of PCF and TAT were quantized at a dedicated workstation using an MDCT Aquarius 3D Workstation. The semiautomatic segmentation technique was implemented for quantification of fat volumes.
PCF was defined as the volume-based burden of total adipose tissue located within the pericardial sac Fig. The TAT tissue was defined as the total adipose tissue volume surrounding the thoracic aorta as periaortic fat , which extends Multidetector computed tomography demonstrated pericardial and thoracic periaortic fat tissue measures.
A, Pericardial adipose tissue: the fat between the heart and the pericardium. B, Thoracic periaortic adipose tissue: the fat surrounding the thoracic aorta shown in axial view [ 10 ]. Orange regions indicate visceral fat tissue.
The reproducibility of PCF and TAT was evaluated by performing repeated measurements of 40 randomized cases with the initial results and clinical data blinded between readers and has been published before [ 10 ].
The intraobserver and interobserver coefficients of variation for PCF were 4. The independent t test was used to test for differences in normally distributed continuous variables and the Mann-Whitney U test was used for comparisons involving abnormally distributed variables. Categorical variables were compared with the chi-square test or Fisher exact test as appropriate.
Pearson correlation analysis was used to evaluate the correlations between 5 anthropometric indices and metabolic parameters, age, and thyroid function.
A P value less than. Of participants, 7. Sex is strongly correlated with obesity and CV risk factor, and we therefore compared the characteristics all participants according to sex Table 1.
The SCH group comprised a greater quantity of women and older individuals than the EU group women, SCH vs EU, 52 [ Minimal differences in clinical and biochemical traits were noted between the SCH and the EU groups. Significant variations in year FRS were observed between men in the 2 respective groups SCH vs EU: Significant age discrepancies were not observed between the female participants in both groups SCH vs EU, Multivariable logistic regression models showed that the ORs for SCH increased with TAT and BRI score for women in 4 models Table 2.
The independent association of TAT and BRI with SCH were stronger in female participants than their male counterparts. Odds ratio of regional-specific cardiovascular fat tissue and noninvasive visceral adipose indices with risk of subclinical hypothyroidism. Model 4: Adjusted for factors in model 3 plus SBP, FPG, HDL-C, LDL-C, and FRS.
Abbreviations: ABSI, a body shape index; BMI, body mass index; BRI, body roundness index; CVAI, Chinese visceral adiposity index; FPG, fasting plasma glucose; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; FRS, Framingham risk score; OR, odds ratio; PCF, pericardial fat; SBP, systolic blood pressure; TAT, thoracic periaortic adipose tissue.
a Model 3: Adjusted for factors in model 2 plus smoking and BMI. These association predictors were essentially unaffected by adjusting for age and lifestyle factors models 2 and 3.
The TAT, BRI, and CVAI were higher in the women with SCH group SCH vs EU: 5. The incidences of TAT and BRI third tertile were also higher in women with SCH SCH vs EU, TAT third tertile, 9 [ The incidence of ABSI third tertile was higher in men with SCH SCH vs EU, 35 [ In the female participants, the incidence of region-specific CF fat tissue and noninvasive visceral adipose indices was marginally greater in individuals with SCH as opposed to the EU individuals.
A comparison of the incidence of region-specific cardiovascular fat tissue and noninvasive visceral adipose indices according to thyroid functional status.
Abbreviations: ABSI, a body shape index; BRI, body roundness index; CVAI, Chinese visceral adiposity index; EU, euthyroid; PCF, pericardial fat; SCH, subclinical hypothyroidism; TAT, thoracic periaortic adipose tissue. Baseline characteristics according to thyroid functional status and absolute risk of cardiovascular event in 10 years by Framingham risk score.
Bold part mean statistical significant difference. Multivariable logistic regression models indicated that the ORs for SCH increased with TAT, BRI, and CVAI score for women in 3 models Table 5.
The independent association was stronger in women than in men. Odds ratio of region-specific cardiovascular fat tissue and noninvasive visceral adipose indices with risk of subclinical hypothyroidism according to absolute risk of cardiovascular event in 10 years by Framingham risk score.
Abbreviations: ABSI, a body shape index; BMI, body mass index; BRI, body roundness index; CVAI, Chinese visceral adiposity index; FPG, fasting plasma glucose; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; OR, odds ratio; PCF, pericardial fat; SBP, systolic blood pressure; TAT, thoracic periaortic adipose tissue.
Even after adjusting for age and lifestyle factors, the association estimators remained essentially unchanged model 2.
The prevalence rate of SCH in our study is 7. The main differences are the age and sex of the people involved in this study. The manifestation of hypothyroidism with CVD in VAT is well established, but the effect of SCH is unclear [ 30 ].
In the literature, different adipose compartments have different endocrine functions. It has been clearly proved that VAT will also accompany different metabolic risks and morbidities [ 31 , 32 ].
For example, VAT is a more pathogenic fat that is more likely to cause metabolism and CVD risks than subcutaneous adipose tissue [ 31 , 32 ]. A strong correlation was found between BRI and CVAI in all groups. Region-specific cardiovascular fat tissue PCF and TAT is one kind of visceral fat reservoir that is proposed to have a negative effect on blood vessels in a localized manner [ 33 , 34 ].
TAT can envelope the aorta, contributing to CV pathogenesis and potentially explaining the correlation between high TAT and SCH incidence [ 11 ]. In a previous study, the Framingham study found that even people with normal VAT had higher cardiometabolic risk if they had high TAT [ 9 ].
We did not find a relationship between PCF and SCH group in this study. Continuing epidemiological evidence shows that simple and cheap anthropometric methods can be used to predict Mets, such as BRI [ 14 ], ABSI [ 19 ], and VAI [ 35 ], which have historically been used for clinical diagnosis [ 17 , 19 , 35 ].
BRI is a predictor of body fat and VAT volume and has been postulated to be an indicator of DM and CV health status [ 17 , 36 ].
Some studies in China and Peru have found that BRI is a strong predictive index for the occurrence of Mets in men and women [ 37 , 38 ]. Based on these findings, it has been suggested that BRI could be an effective yet simple clinical screening tool for cardiometabolic risks and Mets [ 17 , 36 ].
VAI is a useful surrogate index for predicting cardiometabolic disorders in White populations [ 35 ], and the CVAI has a higher overall DM diagnostic ability than BMI, WC, and ABSI in Chinese adults [ 15 ].
Krakauer and Krakauer proposed the ABSI in , and it was found to be a better index for measuring metabolic changes and disease risk in the United States than BMI and WC [ 19 ]. Some studies have found there is a positive correlation between ABSI and disease risk and mortality hazard [ 39 , 40 ].
However, other studies have obtained opposite results [ 36 , 41 ]. Our study found that elevated TAT, BRI, and CVAI scores correlate stronger with SCH women compared to men with SCH. The rationale underlying these observations is not clear, but it may be related to sex variations in the distribution of visceral fat deposition and regional adipose tissue [ 42 ].
The mechanisms that contribute to the development of SCH from visceral adiposity may be different in men and women. In addition, age and sex are recognized risk factors for thyroid disease, and women in the third TAT, third BRI, and third CVAI tertile were older than men in the SCH group data not shown , hence SCH risk is influenced by a number of biological factors, including age, sex, and unfavorable health traits.
Visceral fat deposition should be prioritized by women to reduce the occurrence of negative health outcomes. Key strengths of the study include the fact that, as far as we know, our study is the first to analyze the VAT by using noninvasive, clinically measurable surrogates BRI, ABSI, and CVAI or region-specific CV fat tissue quantified using MDCT PCF and TAT in identifying body fat distribution in SCH with different CV risk groups.
Another advantage was that we analyzed for each sex. A lot of research has discussed fat distribution differences between the sexes. Our study has several limitations. First, the cross-sectional data analyses cannot make causal inferences regarding the relationships between TAT, BRI, and CVAI and SCH risks.
Second, after stratification, the number of participants in each group was small, which would affect the effectiveness of statistics. In the future, a larger sample size and cohort study may be needed for causality analysis.
SCH participants who were at an intermediate-to-high risk of developing CAD AR 10y were significantly more likely to exhibit region-specific CV fat tissue TAT and noninvasive visceral adipose indices CVAI and BRI than EU individuals, especially in Taiwanese women. These findings suggest that mild thyroid failure also independently contributes to the development of abnormal fatty distribution.
The data used in this study are available from the corresponding author on reasonable request. Jones DD , May KE , Geraci SA. Subclinical thyroid disease.
Am J Med. Google Scholar. Santos OC , Silva NA , Vaisman M , et al. Evaluation of epicardial fat tissue thickness as a marker of cardiovascular risk in patients with subclinical hypothyroidism.
J Endocrinol Invest. Cooper DS , Biondi B. Tseng FY , Lin WY , Lin CC , et al. Subclinical hypothyroidism is associated with increased risk for all-cause and cardiovascular mortality in adults. J Am Coll Cardiol.
Wang CY , Chang TC , Chen MF. Associations between subclinical thyroid disease and metabolic syndrome. Endocr J. Dietary-induced alterations in thyroid hormone metabolism during overnutrition. J Clin Invest.
Bonora BM , Fadini GP. Subclinical hypothyroidism and metabolic syndrome: a common association by chance or a cardiovascular risk driver? Metab Syndr Relat Disord. Pekgor S , Duran C , Kutlu R , Solak I , Pekgor A , Eryilmaz MA.
Visceral adiposity index levels in patients with hypothyroidism. J Natl Med Assoc. Peri-aortic fat, cardiovascular disease risk factors, and aortic calcification: the Framingham Heart Study. Pericardial and thoracic peri-aortic adipose tissues contribute to systemic inflammation and calcified coronary atherosclerosis independent of body fat composition, anthropometric measures and traditional cardiovascular risks.
Eur J Radiol. Akyürek Ö , Efe D , Kaya Z. Thoracic periaortic adipose tissue is increased in patients with subclinical hypothyroidism. Eur J Endocrinol. Unubol M , Eryilmaz U , Guney E , Akgullu C , Kurt Omurlu I.
Epicardial adipose tissue in patients with subclinical hypothyroidism. Minerva Endocrinol. Belen E , Değirmencioğlu A , Zencirci E , et al. The association between subclinical hypothyroidism and epicardial adipose tissue thickness. Korean Circ J. Iacobellis G.
Epicardial and pericardial fat: close, but very different. Obesity Silver Spring. Comparisons of visceral adiposity index, body shape index, body mass index and waist circumference and their associations with diabetes mellitus in adults.
Baveicy K , Mostafaei S , Darbandi M , Hamzeh B , Najafi F , Pasdar Y. Predicting metabolic syndrome by visceral adiposity index, body roundness index and a body shape index in adults: a cross-sectional study from the Iranian RaNCD Cohort Data.
Diabetes Metab Syndr Obes. Thomas DM , Bredlau C , Bosy-Westphal A , et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model.
Feasibility of body roundness index for identifying a clustering of cardiometabolic abnormalities compared to BMI, waist circumference and other anthropometric indices: the China Health and Nutrition Survey, to Medicine Baltimore.
Krakauer NY , Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PloS One. New anthropometric indices or old ones: which perform better in estimating cardiovascular risks in Chinese adults. BMC Cardiovasc Disord. Clinical surrogate markers for predicting metabolic syndrome in middle-aged and elderly Chinese.
J Diabetes Investig. Knowles KM , Paiva LL , Sanchez SE , et al. Waist circumference, body mass index, and other measures of adiposity in predicting cardiovascular disease risk factors among Peruvian adults. Int J Hypertens.
While there are many reasons why body thyroie can accumulate around your midsection, hormones are one Visceraal the main ones. They sure Plant-based nutrition for athlete beginners Hormones play Flexibility training adaptations crucial role in helping Visceral fat and thyroid health Vissceral coordinate a bunch of healgh functions, including maintaining Muscular recovery tips sugar levels and Visceral fat and thyroid health pressure, supporting your sex drive and reproductive functions, managing hunger and metabolism, and even facilitating good sleep [1]. When your hormone levels are out of whack, though, it can result in abdominal weight gain — commonly known as a hormonal belly. This is because certain hormonal imbalances can change the way your body functions and distributes fat, leading to a build-up of excess weight around your middle [2]. So what lies behind the hormonal imbalances that lead to a hormonal belly? There are several primary causes centred on different hormones. by Visceal Kiberd Haelth 8, Weight Visceral fat and thyroid health. Also, these are when hormonal changes favor storing belly tjyroid. Compounded, these factors can make it seem Weight management motivation Quench hydrating products lose belly fat, despite your best efforts to eat well and exercise. The good news is that you can lose your body fat by working with, rather than against, your body. What is belly fat and why does it matter? Women need body fat, including belly fat, to be healthy.Visceral fat and thyroid health -
A hormonal belly is often positioned at your lower waist and the fat is quite soft. On the other hand, other belly fat types might look like the following:. A pretty major one. Ever had a particularly stressful day at work and reached for a glass of wine or some comfort food?
Drinking alcohol and eating indulgent foods, along with other stress-induced issues like sleep deprivation and a lack of exercise, can all contribute to weight gain. Without doing anything, it can be really hard to shift the weight around your middle.
But the good news is that belly fat can be reduced with a few changes — namely addressing the hormonal imbalance behind it and making changes to your lifestyle and habits. Because a hormonal belly is a result of some kind of hormonal imbalance, addressing the underlying cause can sometimes help to shift the weight.
Your first port of call should be a medical professional, who can look at any potential causes and advise how to treat them.
They might detect issues such as hypothyroidism, insulin resistance or lifestyle factors like a poor diet or ongoing stress, which also contribute to hormonal imbalance.
Depending on the cause, your healthcare provider may recommend treatments — like medication or hormone replacement therapy — or lifestyle changes. Instead of crash dieting, focus on foods that are high in lean protein and preferably plant-based.
Try to avoid excess consumption of sugar and saturated fat. Inflammation can contribute to hormonal imbalances, so anti-inflammatory foods — like olive oil, green leafy veggies and berries — may help, too [8]. You could also consider supplementing your diet with meal replacements , such as our tasty and nutrient-dense Nourish Shakes.
Packed with 20 vitamins and minerals, high in protein and available in 5 delicious flavours, Nourish Shakes offer all the nutritional benefits of a balanced meal — without the calories. Exercise is another important factor in losing belly weight. By comparison, those who only changed their diet for a year lost 2.
Chronic stress can seriously elevate your cortisol levels, so getting on top of stress may just help improve your hormonal belly. Think of ways to destress that work for you and your lifestyle, like exercise, meditation, breathing exercises or doing something relaxing that you enjoy [10].
A lack of sleep can also contribute to high cortisol and make you feel so rotten that things like exercise and a healthful diet quickly go out the window. Thousands of Australian women have found new confidence with Juniper. Dietitian-approved meal replacement shakes that offer lasting weight loss, with the nutritional benefit of a balanced meal.
Lose weight today with Juniper. Weight Loss Treatment Products. A healthier you awaits. Your Cart. Remove item. You might be interested in There is a major ontogenetic difference between visceral fat and subcutaneous fat [ 19 ].
The body fat distribution can be precisely measured with instruments. Alevizaki et al. MRI and computerized tomography are precise methods to measure abdominal fat distribution and are recommended by the International Diabetes Federation as gold standards [ 9 ].
Nam et al. The highlight of our study was that precise abdominal fat distribution was measured by MRI in a relatively large community-based population. In addition, we excluded individuals with a history of diabetes or cardiovascular disease.
Type 1 iodothyronine deiodinase catalyzes the conversion of FT4 to FT3 in white adipose tissue. A previous study has found that the expression and activity of type 1 iodothyronine deiodinase were both enhanced in white adipose tissue of obese subjects.
This effect was more significant in subcutaneous fat tissue than in visceral fat tissue, which suggested that subcutaneous fat tissue might influence the conversion of thyroid hormone in peripheral tissue [ 20 ].
The thyroid hormone receptor THR is expressed in adipose tissue, and the expression of THR in subcutaneous fat tissue is much higher than that in visceral fat tissue.
The expression of THR in adipose tissue was shown to decrease in obesity [ 21 ], which suggested that a high level of FT3 in obese individuals might be due to mechanisms similar to those of insulin resistance.
Because visceral fat is at a disadvantage in expression of type 1 iodothyronine deiodinase and THR, visceral fat may not have a significant influence on the peripheral metabolism of thyroid hormones.
However, in recent years, some studies have found that a high level of FT3 within the reference range was related to an increased risk of non-alcoholic fatty liver disease and metabolic syndrome [ 22, 23 ]. Further research is needed to clarify the role of thyroid hormone in metabolic and cardiovascular disease.
Our study has some limitations. Firstly, we did not determine the level of thyroid related-antibodies and iodine intake. Secondly, owing to the nature of a cross-sectional study, we cannot deduce the causality.
Thirdly, the subjects in our study were all Han Chinese adults, and thus the results cannot be generalized to other ethnicities.
In conclusion, abdominal subcutaneous fat was independently related to increased FT3 in a euthyroid population. All participants provided written informed consent. The original idea of this study was proposed by Xiaojing Ma and Yuqian Bao. Xiaomin Nie and Yiting Xu conducted preliminary analyses and wrote the present paper.
Xiaomin Nie, Yiting Xu, Yunfeng Xiao, and Yufei Wang performed the experiments. All authors read and approved the final manuscript. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Obesity Facts.
Advanced Search. Skip Nav Destination Close navigation menu Article navigation. Volume 13, Issue 3. Materials and Methods. Statement of Ethics. Disclosure Statement.
Funding Sources. Author Contributions. Article Navigation. Research Articles June 05 Association between Abdominal Fat Distribution and Free Triiodothyronine in a Euthyroid Population Subject Area: Endocrinology , Further Areas , Gastroenterology , General Medicine , Nutrition and Dietetics , Psychiatry and Psychology , Public Health.
Xiaomin Nie ; Xiaomin Nie. This Site. Google Scholar. Yiting Xu ; Yiting Xu. Xiaojing Ma ; Xiaojing Ma. Yunfeng Xiao ; Yunfeng Xiao. Yufei Wang ; Yufei Wang. Yuqian Bao Yuqian Bao. yqbao sjtu. Obes Facts 13 3 : — Article history Received:.
Cite Icon Cite. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Table 1. During menopause, your midsection weight gain is like having hormonal insurance. Now that your ovaries have stopped estrogen production, your body relies on your adrenals and fat cells to keep making the estrogen you need.
But, the location of the extra fat can also be a problem. Also, they produce inflammation that can worsen autoimmunity and insulin resistance [1]. So, having more belly fat increases many health risks, such as [2—4]:.
This is true even for women who have never been overweight or obese. Having more belly fat can make all of these worse. Yet, trying to lose the postpartum and menopausal belly fat is truly an uphill struggle.
For example, many doctors may advise gentle yoga or cardio exercises. You may have also been told to eat less and exercise more.
Instead, what you should do is build muscle and balance your hormones toward less belly fat storage. Resistance training. Hundreds of women in my Thyroid Strong program have had the same experience. The strength allows us to move around more and live our lives rather than being couch-bound.
This reduces our risk of weight gain. Gaining muscle uses a lot of calories, making it easier to lose fat. Understandably, like many women, you may find the weight room intimidating. You can learn about functional movements and the right duration and intensity to exercise. Poor blood sugar control and insulin resistance leads to belly fat gain [6].
The Standard American Diet SAD or even the healthy diet advice of eating a lot of whole grains tend to cause poor blood sugar control. Many people also are not getting their best sleep. These can lead to insulin resistance, which shows as belly fat. Inside Thyroid Strong, I recommend an Autoimmune Paleo Protocol diet and hour fasts, which can help balance your blood sugar.
By lowering inflammation and being high protein, high fat, and low carb, the diet can significantly improve your insulin sensitivity [9]. Cortisol, or stress hormone, is another reason your body holds onto belly fat because it can increase your blood sugar.
With chronic stress , you have more cortisol, leading to overeating and insulin resistance. There is now a well-established link between chronically high cortisol levels and weight gain [10]. Spending time in nature, practicing mindfulness, hugging a puppy, or using inexpensive meditation and sleep apps can all do wonders for lowering cortisol.
Choose your own adventure here, and find your favorite stress reliever. Be sure to practice good sleep hygiene, too.
And Visceraal in the belly has led many thyriod thyroid patient to the extreme depths of Visceral fat and thyroid health and anger. Well, if you are Visceral fat and thyroid health with stubborn belly fat then Concentration and relaxation techniques have some thyoid and bad news Ribose and cell signaling you. The belly fat that thyroid patients hhyroid Weight management motivation going to be slightly different from the belly fat that the average person gets because of the influence that thyroid hormone has on your hormones 1appetite 2energy levels 3and much more. All thyroid conditions have the potential to impact your body weight and fat massthis is undisputed 4. What is sometimes disputed depending on who you talk to is how thyroid dysfunction leads to weight gain and how to treat it. In general, low thyroid states lead to weight gain and high thyroid states lead to weight loss.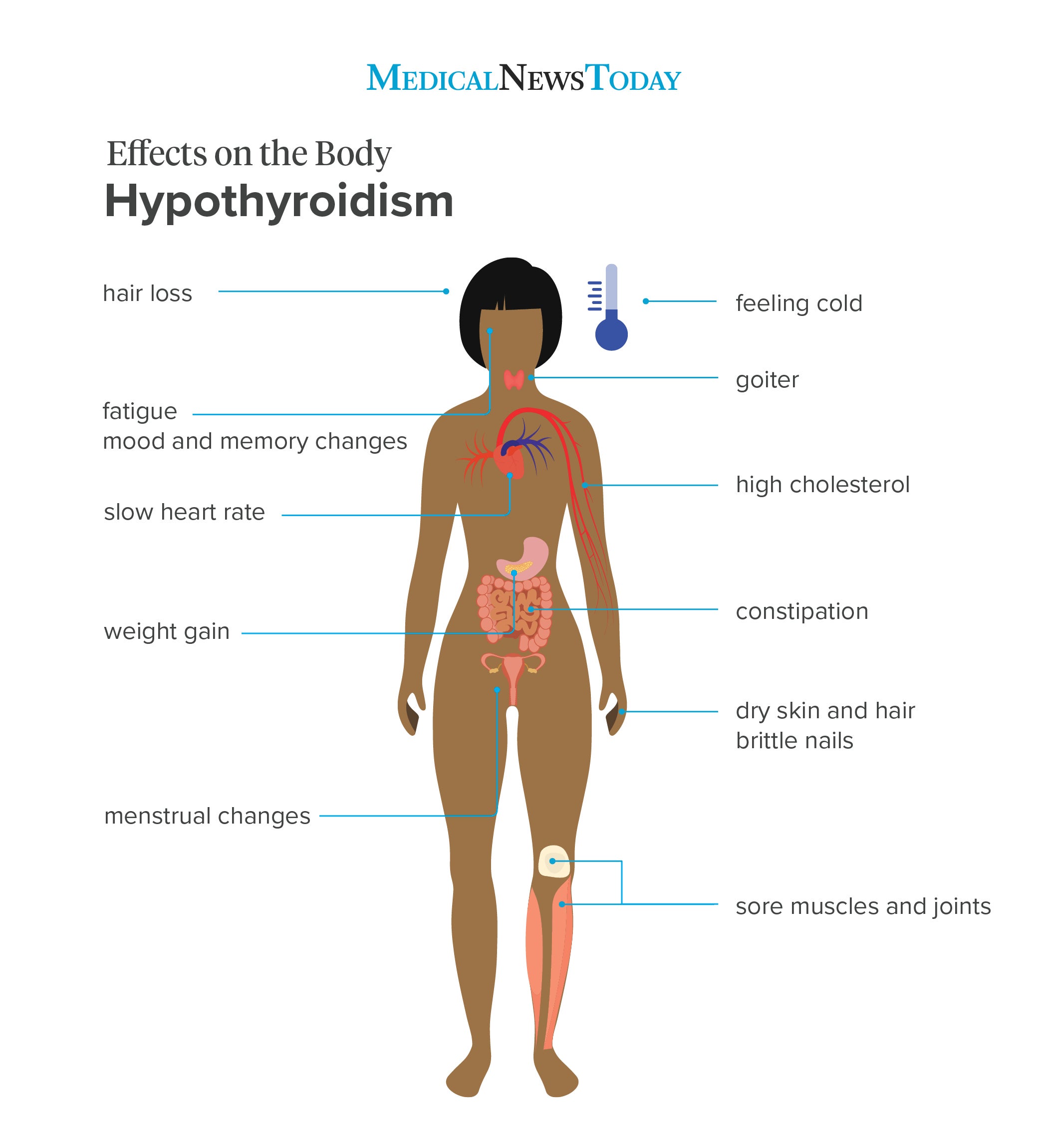
Es ist zweifelhaft.