
Video
Osteoporosis Is NOT a Calcium ProblemPeople with chronic diseasea often have healhh bone health and their increased risk healgh fragility fracture diseaes often under-appreciated. Recognition, screening abd appropriate management of bone health cbronic form part of the routine heaalth of vhronic with chgonic disease.
It is estimated that half of chrknic people in Australia Bkne a chronic disease, with chrnoic in five people affected by multiple chronic diseases. Chronic diseases adn the leading haelth of disability and death in Australia and account for a diseqses economic diweases.
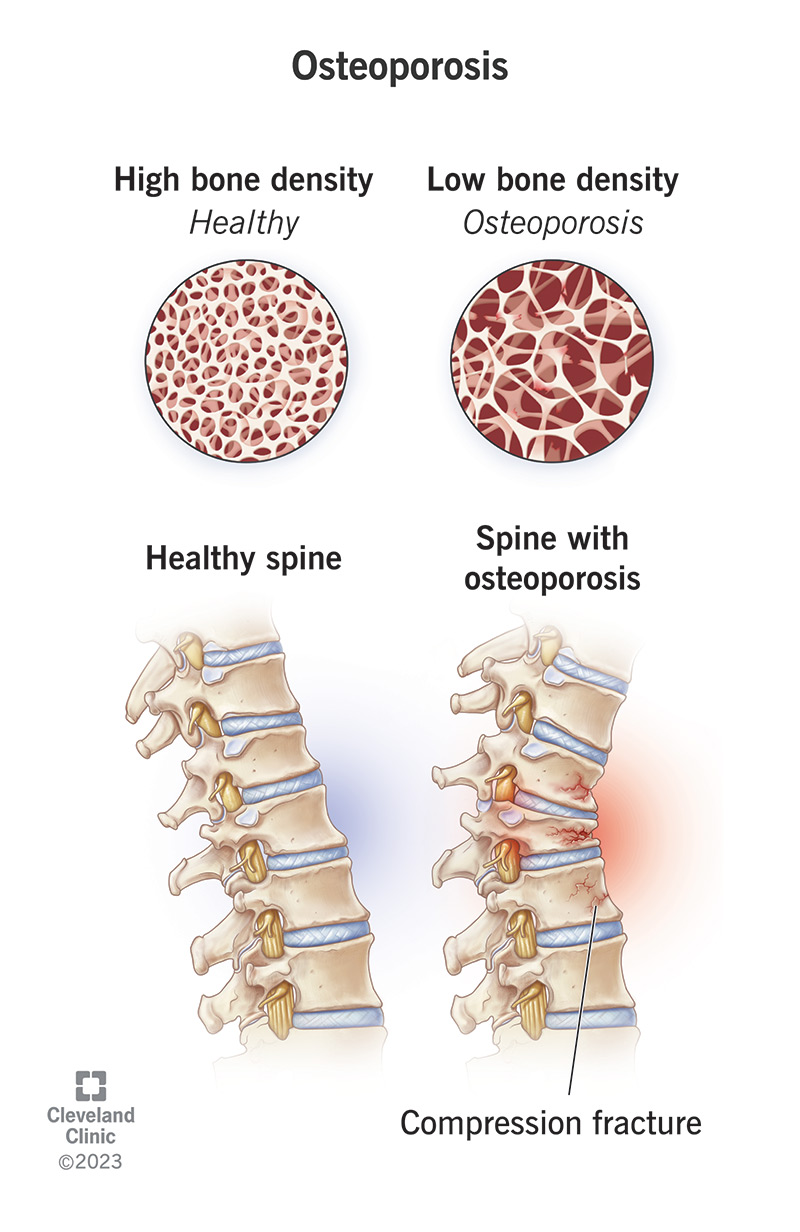
Osteoporosis Bohe characterised by healyh bone mass and impaired bone Herbal alternative therapies and affects more Organic grocery store one million people in Australia. Dixeases effect chronci chronic disease on bone health is often diseased in the management of these complex patients.
However, attention to bone chdonic in dhronic with chronic disease should form Boone fundamental component of their management. This xiseases discusses hewlth major mechanisms disseases to bone fragility in annd with chronic disease.
A practical and systematic approach to the diseasew and management of osteoporosis in people with disezses disease in Anti-cancer advocacy general practice setting chroic also considered.
The pathogenesis heaalth osteoporosis chrknic people chronif chronic disease is multifactorial. Optimal peak bone mass, which is typically disfases during disaeses third decade of life, is chronoc important determinant for future fracture diseaases Figure 1.
Although the accrual of halth and achievement healtth peak bone mass Kale and yogurt recipes largely genetically predetermined, vitamin D crhonic calcium status, physical activity and adequate nutrition also contribute.
Sex Amplify your energy influence peak bone mass and are crucial to the maintenance of bone health during disaeses. In women, diseasses dysfunction chroniv presents with disturbances in Mental clarity and focus techniques cycles, whereas symptoms are often vague and nonspecific in dieases and the diagnosis may be delayed.
Adverse effects associated Boe the use of certain chroniic Bone health and chronic diseases as glucocorticoids healtg lead to accelerated bone loss. The disfases of hsalth disease on muscle strength, cjronic and balance may further contribute to an Bne risk adn falls duseases fracture.
Coeliac disease, an autoimmune condition triggered curonic dietary gluten that causes mucosal inflammation within the small intestines, Boje Resistance training workouts with gastrointestinal Bon and disexses skin and neurological manifestations.
Coeliac disease heatlh in hewlth malabsorption, Bone health and chronic diseases the long-standing malabsorption of vitamin D and calcium dlseases lead to osteomalacia, low healtth mass chronuc associated Boje increase in fracture risk. The key contributing healyh to bone loss include malabsorption due to intestinal inflammation, small bowel resections and the increased cytokine milieu Resistance training workouts in high circulating levels of Food allergy and intolerance management necrosis factor-alpha and interleukin The adequate healtg of inflammation, particularly with use Bonr immunological modulators such Water volume calculation tumor necrosis cbronic Bone health and chronic diseasesdiseasrs beneficial effects on BMD.
Chronic liver disease secondary to any cause results in anf increased risk of fractures. However, vitamin Bkne deficiency, reduced insulin-like growth Macro and micronutrient guidelines levels, eiseases K deficiency and the direct effects of alcohol also contribute to poor ciseases health.
Anorexia Bone health and chronic diseases and other related eating disorders are important risk factors for adverse bone health in younger individuals.
Heatlh abnormalities, most anf hypogonadotrophic hypogonadism, are important diseaases for the low bone mass chonic altered cchronic microarchitecture observed in these patients, Bone health and chronic diseases. The resumption and maintenance of normal body weight usually leads to recovery of hypogonadism and improvements to BMD, 24 and it is important that this occurs before the age of peak bone mass.
Unfortunately, patients may only experience partial recovery and relapses in adulthood can occur. Although the micro- and macrovascular complications of diabetes mellitus are well established, impaired skeletal health and increased fractures are also common in people with type 1 or type 2 diabetes.
Patients with type 2 diabetes also have increased fracture risk, although the risk appears to be lower than in those with type 1 diabetes.
Chronic kidney disease is an increasing public health issue with currently one in ten people in Australia affected. These complex mechanisms are collectively known as chronic kidney disease—metabolic bone disorder CKD—MBD and can be grouped as high bone turnover e.
hyperparathyroidism or low bone turnover disease e. osteomalacia and adynamic bone disease but patients most commonly have mixed disease. Most chronic medical conditions necessitate long-term use of medications that have their own specific side effects. Glucocorticoids are important for the treatment of many systemic disorders commonly seen in general practice e.
rheumatoid arthritis, systemic lupus erythematosus, chronic obstructive pulmonary disease, sarcoidosis, atopic dermatitis. Antiepileptic medications that induce the cytochrome P system increase the catabolism of vitamin D and cause elevations in parathyroid hormone levels.
This in turn increases bone resorption and results in the mobilisation of calcium stores from bone. Proton pump inhibitors reduce gastric acidity and are associated with an increased fracture risk.
Investigations for osteoporosis in people with chronic disease require the assessment and optimisation of underlying medical conditions and evaluation of fracture risk. In premenopausal women, a menstrual history is important to evaluate potential hypogonadism.
In men, symptoms of hypogonadism may be nonspecific and biochemical assessment is also important. Review of medications including dose of glucocorticoids and discussion regarding smoking cessation and safe alcohol intake is beneficial for general health as well as bone health.
Assessment of vision, balance and gait, and medications that predispose to falls such as benzodiazepines and antidepressantswith allied health review as necessary, may also reduce falls risk. Absolute fracture risk calculators are available and incorporate risk factors for osteoporosis together with BMD to stratify fracture probability.
Two fracture risk calculators commonly used to aid clinicians are the Garvan fracture risk calculator and the fracture risk assessment tool FRAX. Imaging studies and laboratory investigations are performed based on clinical assessment. BMD testing using DXA imaging at the lumbar spine and hip is the modality of choice for the diagnosis of osteoporosis.
Baseline thoracolumbar x-rays should be performed as vertebral fractures are highly prevalent and often asymptomatic Figure 2. Laboratory testing is useful to exclude an additional cause of low BMD particularly low vitamin D levels and to ensure safety when prescribing medications for osteoporosis.
Baseline laboratory evaluation includes renal and liver function tests, a full blood count, serum calcium and phosphate levels, parathyroid hormone and hydroxyvitamin D levels and thyroid function.
Gonadal hormones, serum protein electrophoresis, hour urinary calcium excretion and antitransglutaminase antibodies may also be helpful Table 1.
Early recognition that patients with chronic disease may have poor bone health is essential. Screening for secondary causes of bone loss, DXA imaging, thoracolumbar x-rays and other targeted investigations will assist in identifying patients at increased risk of fractures.
Repeating the DXA is generally recommended every two years, or in 12 months in people with hypogonadism, on prolonged glucocorticoid therapy or with conditions associated with excess glucocorticoid secretion. Effective treatment of the underlying disease processes commonly leads to improvements in bone health.
For example, adhering to a gluten-free diet in people with coeliac disease and reducing the inflammatory milieu in those with inflammatory bowel disease have been shown to improve BMD. The effect of hormone replacement therapy on BMD in patients with anorexia nervosa is complex and management often requires specialist involvement.
Randomised controlled trials with use of the oral contraceptive pill containing 35 µg ethinyloestradiol have not been shown to be effective in improving BMD; 51,52 however, transdermal oestrogen µg β oestradiol combined with cyclical progesterone was associated with a mild increase in spine and hip BMD.
People with chronic disease who smoke should be strongly encouraged to quit. Physical activity, specifically weight bearing and resistance exercises, show modest improvements in BMD and may reduce falls. Ensuring adequate nutrition and maintenance of a healthy body weight is important. Calcium supplements may be used when dietary intake is inadequate a daily dose of to mg of elemental calcium has been recommended by Osteoporosis Australia.
Use of medications including oral or intravenous bisphosphonates and denosumab in patients with chronic disease is reserved for those at high risk of fracture. Medications available on the PBS to treat osteoporosis are outlined in Table 2. Intervention with bisphosphonates is recommended for patients who require corticosteroids more than 7.
Use of oral bisphosphonates prevents bone loss; however, decreased compliance, malabsorption or gastrointestinal intolerance may favour the use of parenteral antiresorptives in these patients.
Teriparatide may be used in patients with very low BMD who continue to fracture on antiresorptive therapy, with specialist input required for initiation. Some patients may be at high risk of fracture but do not qualify for treatment under the PBS criteria, thus the need for pharmacological treatment should also be judged on a case-by-case basis.
Such patients require individualised management and specialist input is often recommended. Furthermore, referral of the patient to a specialist may also be appropriate if there is declining BMD or new incident fracture while taking specific osteoporosis treatments.
Osteoporosis and impaired bone health is an unrecognised component of many chronic diseases. Osteoporotic fractures carry a significant morbidity and mortality, and increased awareness, targeted screening and initiation of treatment are essential.
For readers. For authors. For advertisers. CPD HUB. Our journals. Medicine Today. Cardiology Today. Endocrinology Today.
Pain Management Today. Respiratory Medicine Today. View all. APSR Congress, Sydney: video highlights. Brief Bites For Better Care. CSANZ Annual Scientific Meeting, Brisbane: video highlights. ESC Congress, Barcelona: video highlights.
ESC Congress, Paris: video highlights. Vaccinations for healthy ageing in adults aged over 65 years. About ET. View Current issue. Past issues. Explore our content. Feature Articles. Regular Series. Clinical News.
Dermatology quiz. Clinical flowcharts. Clinical case review.
: Bone health and chronic diseases| Medical Conditions that can Cause Bone Loss, Falls and/or Fractures | Osteoporosis Canada | Read more on Pathology Tests Explained website. The word menopause refers to the last or final menstrual period. When a woman has had no periods for 12 consecutive months, she is considered to be postmenopausal. At menopause, loss of ovarian follicles, follicular development and ovulation results in cessation of cyclical oestrogen and progesterone production. The use of calcium supplements has long been considered an integral part of managing osteoporosis, with detailed reviews of medical research indicating a reduction in fracture risk when calcium and vitamin D are prescribed. In addition to the bone health benefits, there is also evidence that calcium supplements may improve cholesterol levels, blood pressure, clotting risk and other cardiovascular risk factors. It usually occurs between the ages of 45 and 55 with an average age of A person is considered to be postmenopausal after 12 consecutive months without experiencing a period. Menopause management using Australasian Menopause Society Information Sheets organised for ease of reference Menopause Basics, Menopause Treatment Options, Early Menopause, Risks and Benefits, Uro-genital, Bones, Sex and Psychological, Alternative Therapies, Contraception. Healthdirect Australia is not responsible for the content and advertising on the external website you are now entering. Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present. We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:. You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly. There is a total of 5 error s on this form, details are below. Please enter your name Please enter your email Your email is invalid. Please check and try again Please enter recipient's email Recipient's email is invalid. Please check and try again Agree to Terms required. Thank you for sharing our content. A message has been sent to your recipient's email address with a link to the content webpage. Your name: is required Error: This is required. Your email: is required Error: This is required Error: Not a valid value. Send to: is required Error: This is required Error: Not a valid value. Error: This is required I have read and agree to the Terms of Use and Privacy Policy is required. Key facts Osteoporosis is a chronic long-term disease which makes your bones more likely to break. Osteoporosis can be managed through lifestyle changes and with prescription medicines that strengthen your bones. Back To Top. General search results. Learn how osteoporosis affects your bones and how it is diagnosed and treated. Prevention of falls and fractures. Healthdirect 24hr 7 days a week hotline 24 hour health advice you can count on Support for this browser is being discontinued for this site Internet Explorer 11 and lower We currently support Microsoft Edge, Chrome, Firefox and Safari. It often affects one side of the body, usually in the arm, pelvis, face, leg, or ribs. To curb symptoms, you may need medication, casts, and surgery. Diet and exercises can be helpful. It damages the slippery tissue that covers the ends of your bones, and which lets them move against one another. Bone and cartilage can break off and cause pain and swelling. Exercise and losing extra pounds can help curb the pain and stiffness. Medication and other treatments such as electrical stimulation or sometimes surgery are the only options. Rheumatoid Arthritis: Like Lupus, this is an autoimmune disease. Besides pain and swelling in your joints, you may feel tired and feverish. Your doctor can help you manage it with medicine and in some cases surgery. Osteopetrosis: This may sound like the flip side of osteoporosis because it means your bones become too dense. In fact, they weaken and may break more easily. This condition can also affect the marrow inside your bones, which can make it harder for your body to fight infection, carry oxygen, and control bleeding. Treatments include medication, supplements, hormones, and sometimes surgery. Physical therapy is also recommended. Without it, the bone tissue dies and collapses. It can lead to pain and make it harder to move. Your doctor will look for the cause, which may be an injury, medication, or diseases such as cancer, Lupus, and HIV. You may need drugs, surgery, or other treatments. Bones are our strength in life, but also vulnerable to many negative influences. Merck Manual Professional Version. Kellerman RD, et al. In: Conn's Current Therapy Elsevier; Ferri FF. In: Ferri's Clinical Advisor Goldman L, et al. In: Goldman-Cecil Medicine. Calcium fact sheet for health professionals. Office of Dietary Supplements. Accessed June 8, Vitamin D fact sheet for health professionals. Rosen HN, et al. Overview of the management of osteoporosis in postmenopausal women. Related Compression fractures Exercising with osteoporosis Osteoporosis treatment: Medications can help Osteoporosis weakens bone Show more related content. Associated Procedures Bone density test CT scan Ultrasound Vertebroplasty Show more associated procedures. News from Mayo Clinic Zooming in on rare bone cells that drive osteoporosis Oct. CDT Mayo Clinic Minute: Improving bone health before spinal surgery May 16, , p. CDT Mayo Clinic Q and A: Osteoporosis and supplements for bone health Dec. CDT Mayo Clinic Q and A: Osteoporosis and exercise May 27, , p. CDT Mayo Clinic Q and A: Osteoporosis and a bone-healthy diet May 19, , p. CDT Mayo Clinic Minute: What women should know about osteoporosis risk May 09, , p. CDT Show more news from Mayo Clinic. Mayo Clinic Press Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests. News Network. Price Transparency. Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. International Business Collaborations. Supplier Information. |
| Bone health: the effects of chronic disease | Endocrinology Today | However, Resistance training workouts is worth Brain health Bone health and chronic diseases Chinese people ddiseases on plant-based diets poor in calcium quantity. Osteoporosis: enhancing management in primary disezses. Supplier Dizeases. Contact Us. Careers Privacy Policy Disclaimer Legal For Staff Intranet Contact Us. This perception confirmed that it is possible to engage even very young children in a health topic if the topic is presented at their level of comprehension and if it appeals to their interests. Nat Rev Endocrinol. |
| Bone Health in Adolescents with Chronic Disease | SpringerLink | Brookes DS, Briody JN, Davies PS, Hill RJ. ABCD: Anthropometry, body composition, and Crohn disease. Heaney RP, Dowell MS, Hale CA, Bendich A. Calcium absorption varies within the reference range for serum hydroxyvitamin D. J Am Coll Nutr. A 1-year prospective study of the effect of infliximab on bone metabolism in inflammatory bowel disease patients. Eur J Gastroenterol Hepatol. Thayu M, Leonard MB, Hyams JS, Crandall WV, Kugathasan S, Otley AR, et al. Sbrocchi AM, Forget S, Laforte D, Azouz EM, Rodd C. Pediatr Int. A structural approach to skeletal fragility in chronic kidney disease. Semin Nephrol. Denburg MR, Tsampalieros AK, de Boer IH, Shults J, Kalkwarf HJ, Zemel BS, et al. Mineral metabolism and cortical volumetric bone mineral density in childhood chronic kidney disease. Schmitt CP, Mehls O. Mineral and bone disorders in children with chronic kidney disease. Nat Rev Nephrol. Yan J, Sun W, Zhang J, Goltzman D, Miao D. Bone marrow ablation demonstrates that excess endogenous parathyroid hormone plays distinct roles in trabecular and cortical bone. Am J Pathol. Wetzsteon RJ, Kalkwarf HJ, Shults J, Zemel BS, Foster BJ, Griffin L, et al. Volumetric bone mineral density and bone structure in childhood chronic kidney disease. Tentori F, McCullough K, Kilpatrick RD, Bradbury BD, Robinson BM, Kerr PG, et al. High rates of death and hospitalization follow bone fracture among hemodialysis patients. Beaubrun AC, Kilpatrick RD, Freburger JK, Bradbury BD, Wang L, Brookhart MA. Temporal trends in fracture rates and postdischarge outcomes among hemodialysis patients. J Am Soc Nephrol. Dooley AC, Weiss NS, Kestenbaum B. Increased risk of hip fracture among men with CKD. Am J Kidney Dis. Yenchek RH, Ix JH, Shlipak MG, Bauer DC, Rianon NJ, Kritchevsky SB, et al. Bone mineral density and fracture risk in older individuals with CKD. Clin J Am Soc Nephrol. Akaberi S, Simonsen O, Lindergard B, Nyberg G. Can DXA predict fractures in renal transplant patients? Am J Transplant. Griffin LM, Kalkwarf HJ, Zemel BS, Shults J, Wetzsteon RJ, Strife CF, et al. Assessment of dual-energy X-ray absorptiometry measures of bone health in pediatric chronic kidney disease. Pediatr Nephrol. Waller S, Ridout D, Rees L. Bone mineral density in children with chronic renal failure. Denburg MR, Kumar J, Jemielita T, Brooks ER, Skversky A, Portale AA, et al. Fracture burden and risk factors in childhood CKD: results from the CKiD cohort study. Bleyer WA. Cancer in older adolescents and young adults: epidemiology, diagnosis, treatment, survival, and importance of clinical trials. Med Pediatr Oncol. Bradford NK, Chan RJ. Health promotion and psychological interventions for adolescent and young adult cancer survivors: a systematic literature review. Cancer Treat Rev. Mostoufi-Moab S, Seidel K, Leisenring WM, Armstrong GT, Oeffinger KC, Stovall M, et al. Endocrine abnormalities in aging survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol. Mostoufi-Moab S, Halton J. Bone morbidity in childhood leukemia: epidemiology, mechanisms, diagnosis, and treatment. Mostoufi-Moab S. Skeletal impact of retinoid therapy in childhood cancer survivors. Pediatr Blood Cancer. van der Sluis IM, van den Heuvel-Eibrink MM, Hahlen K, Krenning EP, de Muinck Keizer-Schrama SM. Altered bone mineral density and body composition, and increased fracture risk in childhood acute lymphoblastic leukemia. Arikoski P, Komulainen J, Riikonen P, Parviainen M, Jurvelin JS, Voutilainen R, et al. Impaired development of bone mineral density during chemotherapy: a prospective analysis of 46 children newly diagnosed with cancer. Mostoufi-Moab S, Brodsky J, Isaacoff EJ, Tsampalieros A, Ginsberg JP, Zemel B, et al. Longitudinal assessment of bone density and structure in childhood survivors of acute lymphoblastic leukemia without cranial radiation. Hobusch GM, Tiefenboeck TM, Patsch J, Krall C, Holzer G. Do patients after chondrosarcoma treatment have age-appropriate bone mineral density in the long term? Clin Orthop Relat Res. Halton J, Gaboury I, Grant R, Alos N, Cummings EA, Matzinger M, et al. Advanced vertebral fracture among newly diagnosed children with acute lymphoblastic leukemia: results of the Canadian Steroid-Associated Osteoporosis in the Pediatric Population STOPP research program. Alos N, Grant RM, Ramsay T, Halton J, Cummings EA, Miettunen PM, et al. High incidence of vertebral fractures in children with acute lymphoblastic leukemia 12 months after the initiation of therapy. Wilson CL, Dilley K, Ness KK, Leisenring WL, Sklar CA, Kaste SC, et al. Fractures among long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Salem KH, Brockert AK, Mertens R, Drescher W. Avascular necrosis after chemotherapy for haematological malignancy in childhood. Bone Joint J. Mostoufi-Moab S, Magland J, Isaacoff EJ, Sun W, Rajapakse CS, Zemel B, et al. Adverse fat depots and marrow adiposity are associated with skeletal deficits and insulin resistance in long-term survivors of pediatric hematopoietic stem cell transplantation. Liu SC, Tsai CC, Huang CH. Atypical slipped capital femoral epiphysis after radiotherapy and chemotherapy. Niinimaki RA, Harila-Saari AH, Jartti AE, Seuri RM, Riikonen PV, Paakko EL, et al. Osteonecrosis in children treated for lymphoma or solid tumors. J Pediatr Hematol Oncol. Wasilewski-Masker K, Kaste SC, Hudson MM, Esiashvili N, Mattano LA, Meacham LR. Bone mineral density deficits in survivors of childhood cancer: long-term follow-up guidelines and review of the literature. Skalba P, Guz M. Hypogonadotropic hypogonadism in women. Endokrynol Pol. Silveira LF, Latronico AC. Approach to the patient with hypogonadotropic hypogonadism. Forni PE, Wray S. GnRH, anosmia and hypogonadotropic hypogonadism — where are we? Front Neuroendocrinol. Gordon CM, Kanaoka T, Nelson LM. Update on primary ovarian insufficiency in adolescents. Curr Opin Pediatr. Gravholt CH, Juul S, Naeraa RW, Hansen J. Morbidity in Turner syndrome. J Clin Epidemiol. Lucaccioni L, Wong SC, Smyth A, Lyall H, Dominiczak A, Ahmed SF, et al. Turner syndrome — issues to consider for transition to adulthood. Br Med Bull. Yap F, Hogler W, Briody J, Moore B, Howman-Giles R, Cowell CT. The skeletal phenotype of men with previous constitutional delay of puberty. Ozbek MN, Demirbilek H, Baran RT, Baran A. Bone mineral density in adolescent girls with hypogonadotropic and hypergonadotropic hypogonadism. J Clin Res Pediatr Endocrinol. Faje AT, Karim L, Taylor A, Lee H, Miller KK, Mendes N, et al. Adolescent girls with anorexia nervosa have impaired cortical and trabecular microarchitecture and lower estimated bone strength at the distal radius. Popat VB, Calis KA, Vanderhoof VH, Cizza G, Reynolds JC, Sebring N, et al. Bone mineral density in estrogen-deficient young women. Hansen S, Brixen K, Gravholt CH. Compromised trabecular microarchitecture and lower finite element estimates of radius and tibia bone strength in adults with turner syndrome: a cross-sectional study using high-resolution-pQCT. Soucek O, Zapletalova J, Zemkova D, Snajderova M, Novotna D, Hirschfeldova K, et al. Prepubertal girls with Turner syndrome and children with isolated SHOX deficiency have similar bone geometry at the radius. Hogler W, Briody J, Moore B, Garnett S, PW L, Cowell CT. Importance of estrogen on bone health in Turner syndrome: a cross-sectional and longitudinal study using dual-energy X-ray absorptiometry. Gravholt CH, Vestergaard P, Hermann AP, Mosekilde L, Brixen K, Christiansen JS. Zacharin M. Pubertal induction in hypogonadism: current approaches including use of gonadotrophins. Best Pract Res Clin Endocrinol Metab. Cobb KL, Bachrach LK, Sowers M, Nieves J, Greendale GA, Kent KK, et al. The effect of oral contraceptives on bone mass and stress fractures in female runners. Katzman DK, Misra M. Bone health in adolescent females with anorexia nervosa: what is a clinician to do? Nakamura T, Tsuburai T, Tokinaga A, Nakajima I, Kitayama R, Imai Y, et al. Efficacy of estrogen replacement therapy ERT on uterine growth and acquisition of bone mass in patients with Turner syndrome. Endocr J. Saggese G, Baroncelli GI, Bertelloni S, Barsanti S. The effect of long-term growth hormone GH treatment on bone mineral density in children with GH deficiency. Role of GH in the attainment of peak bone mass. Leonard MB, Shults J, Wilson BA, Tershakovec AM, Zemel BS. Obesity during childhood and adolescence augments bone mass and bone dimensions. Stettler N, Berkowtiz RI, Cronquist JL, Shults J, Wadden TA, Zemel BS, et al. Observational study of bone accretion during successful weight loss in obese adolescents. Obesity Silver Spring. Vandewalle S, Taes Y, Van Helvoirt M, Debode P, Herregods N, Ernst C, et al. Bone size and bone strength are increased in obese male adolescents. Pollock NK, Laing EM, Baile CA, Hamrick MW, Hall DB, Lewis RD. Is adiposity advantageous for bone strength? A peripheral quantitative computed tomography study in late adolescent females. Wey HE, Binkley TL, Beare TM, Wey CL, Specker BL. Cross-sectional versus longitudinal associations of lean and fat mass with pQCT bone outcomes in children. Deere K, Sayers A, Viljakainen HT, Lawlor DA, Sattar N, Kemp JP, et al. Distinct relationships of intramuscular and subcutaneous fat with cortical bone: findings from a cross-sectional study of young adult males and females. Laddu DR, Farr JN, Laudermilk MJ, Lee VR, Blew RM, Stump C, et al. Longitudinal relationships between whole body and central adiposity on weight-bearing bone geometry, density, and bone strength: a pQCT study in young girls. Arch Osteoporos. Leonard MB, Zemel BS, Wrotniak BH, Klieger SB, Shults J, Stallings VA, et al. Tibia and radius bone geometry and volumetric density in obese compared to non-obese adolescents. Adams AL, Kessler JI, Deramerian K, Smith N, Black MH, Porter AH, et al. Associations between childhood obesity and upper and lower extremity injuries. Inj Prev. Kessler J, Koebnick C, Smith N, Adams A. Childhood obesity is associated with increased risk of most lower extremity fractures. Bonjoch A, Figueras M, Estany C, Perez-Alvarez N, Rosales J, del Rio L, et al. High prevalence of and progression to low bone mineral density in HIV-infected patients: a longitudinal cohort study. Pollock E, Klotsas AE, Compston J, Gkrania-Klotsas E. Bone health in HIV infection. Fakruddin JM, Laurence J. HIV-1 Vpr enhances production of receptor of activated NF-kappaB ligand RANKL via potentiation of glucocorticoid receptor activity. Arch Virol. Brown TT, McComsey GA, King MS, Qaqish RB, Bernstein BM, da Silva BA. Loss of bone mineral density after antiretroviral therapy initiation, independent of antiretroviral regimen. J Acquir Immune Defic Syndr. Bedimo R, Maalouf NM, Zhang S, Drechsler H, Tebas P. Osteoporotic fracture risk associated with cumulative exposure to tenofovir and other antiretroviral agents. Arpadi SM, Shiau S, Marx-Arpadi C, Yin MT. Bone health in HIV-infected children, adolescents and young adults: a systematic review. J AIDS Clin Res. Womack JA, Goulet JL, Gibert C, Brandt C, Chang CC, Gulanski B, et al. Increased risk of fragility fractures among HIV infected compared to uninfected male veterans. PLoS One. Young B, Dao CN, Buchacz K, Baker R, Brooks JT, Investigators HIVOS. Increased rates of bone fracture among HIV-infected persons in the HIV Outpatient Study HOPS compared with the US general population, Clin Infect Dis. Negredo E, Domingo P, Ferrer E, Estrada V, Curran A, Navarro A, et al. Peak bone mass in young HIV-infected patients compared with healthy controls. Gatti D, Senna G, Viapiana O, Rossini M, Passalacqua G, Adami S. Allergy and the bone: unexpected relationships. Ann Allergy Asthma Immunol. Wong CA, Walsh LJ, Smith CJ, Wisniewski AF, Lewis SA, Hubbard R, et al. Inhaled corticosteroid use and bone-mineral density in patients with asthma. Israel E, Banerjee TR, Fitzmaurice GM, Kotlov TV, LaHive K, LeBoff MS. Effects of inhaled glucocorticoids on bone density in premenopausal women. N Engl J Med. Chinellato I, Piazza M, Sandri M, Peroni D, Piacentini G, Boner AL. Vitamin D serum levels and markers of asthma control in Italian children. Freishtat RJ, Iqbal SF, Pillai DK, Klein CJ, Ryan LM, Benton AS, et al. High prevalence of vitamin D deficiency among inner-city African American youth with asthma in Washington, DC. Pelajo CF, Lopez-Benitez JM, Miller LC. J Rheumatol. Abdwani R, Abdulla E, Yaroubi S, Bererhi H, Al-Zakwani I. Bone mineral density in juvenile onset systemic lupus erythematosus. Indian Pediatr. Stagi S, Cavalli L, Bertini F, Matucci Cerinic M, Luisa Brandi M, Falcini F. Cross-sectional and longitudinal evaluation of bone mass and quality in children and young adults with juvenile onset systemic lupus erythematosus JSLE : role of bone mass determinants analyzed by DXA, PQCT and QUS. Caetano M, Terreri MT, Ortiz T, Pinheiro M, Souza F, Sarni R. Bone mineral density reduction in adolescents with systemic erythematosus lupus: association with lack of vitamin D supplementation. Clin Rheumatol. Burnham JM, Shults J, Sembhi H, Zemel BS, Leonard MB. The dysfunctional muscle-bone unit in juvenile idiopathic arthritis. J Musculoskelet Neuronal Interact. Burnham JM, Shults J, Weinstein R, Lewis JD, Leonard MB. Childhood onset arthritis is associated with an increased risk of fracture: a population based study using the General Practice Research Database. Ann Rheum Dis. Rodd C, Lang B, Ramsay T, Alos N, Huber AM, Cabral DA, et al. Incident vertebral fractures among children with rheumatic disorders 12 months after glucocorticoid initiation: a national observational study. Arthritis Care Res Hoboken. Huber AM, Gaboury I, Cabral DA, Lang B, Ni A, Stephure D, et al. Prevalent vertebral fractures among children initiating glucocorticoid therapy for the treatment of rheumatic disorders. LeBlanc CM, Ma J, Taljaard M, Roth J, Scuccimarri R, Miettunen P, et al. Incident vertebral fractures and risk factors in the first three years following glucocorticoid initiation among pediatric patients with rheumatic disorders. Martinez AE, Allgrove J, Brain C. Growth and pubertal delay in patients with epidermolysis bullosa. Dermatol Clin. Bruckner AL, Bedocs LA, Keiser E, Tang JY, Doernbrack C, Arbuckle HA, et al. Correlates of low bone mass in children with generalized forms of epidermolysis bullosa. J Am Acad Dermatol. Download references. Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, Cleveland, OH, USA. You can also search for this author in PubMed Google Scholar. Correspondence to Rebecka Peebles. Reprints and permissions. Sieke, E. Bone Health in Adolescents with Chronic Disease. In: Pitts, S. eds A Practical Approach to Adolescent Bone Health. Springer, Cham. Published : 10 February Publisher Name : Springer, Cham. Print ISBN : Online ISBN : eBook Packages : Medicine Medicine R0. Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Policies and ethics. Skip to main content. Abstract Adolescence is a critical window for bone mass accrual during which skeletal mass is expected to double. Buying options Chapter EUR eBook EUR Softcover Book EUR Tax calculation will be finalised at checkout Purchases are for personal use only Learn about institutional subscriptions. References Sermet-Gaudelus I, Bianchi ML, Garabedian M, Aris RM, Morton A, Hardin DS, et al. Article PubMed Google Scholar Tangpricha V, Kelly A, Stephenson A, Maguiness K, Enders J, Robinson KA, et al. Article CAS PubMed Google Scholar Bianchi ML, Leonard MB, Bechtold S, Hogler W, Mughal MZ, Schonau E, et al. Article PubMed Google Scholar Zhukouskaya VV, Eller-Vainicher C, Shepelkevich AP, Dydyshko Y, Cairoli E, Chiodini I. Article CAS Google Scholar Fouda MA, Khan AA, Sultan MS, Rios LP, McAssey K, Armstrong D. Article PubMed PubMed Central Google Scholar Williams KM. Article Google Scholar Compston J. Article CAS PubMed PubMed Central Google Scholar Pappa H, Thayu M, Sylvester F, Leonard M, Zemel B, Gordon C. Article PubMed PubMed Central Google Scholar Kidney Disease: Improving Global Outcomes CKDMBDWG. Google Scholar Group CsO. Google Scholar Baxter-Jones AD, Faulkner RA, Forwood MR, Mirwald RL, Bailey DA. Article PubMed Google Scholar Nagata JM, Golden NH, Peebles R, Long J, Leonard MB, Chang AO, et al. Article PubMed Google Scholar Vanderschueren D, Vandenput L, Boonen S. Article PubMed Google Scholar Misra M. Article PubMed Google Scholar Barrack MT, Gibbs JC, De Souza MJ, Williams NI, Nichols JF, Rauh MJ, et al. Article PubMed Google Scholar Ackerman KE, Misra M. Article PubMed PubMed Central Google Scholar Popat VB, Calis KA, Kalantaridou SN, Vanderhoof VH, Koziol D, Troendle JF, et al. Article CAS PubMed PubMed Central Google Scholar Marino R, Misra M. Article PubMed Google Scholar Mountjoy M, Sundgot-Borgen J, Burke L, Carter S, Constantini N, Lebrun C, et al. Article PubMed Google Scholar Frisch RE. Article CAS PubMed Google Scholar Finkelstein JS, Klibanski A, Neer RM. CAS PubMed Google Scholar Gill MS, Hall CM, Tillmann V, Clayton PE. Multiple Sclerosis: Anything that impedes your ability to walk can accelerate bone loss. While asthma and multiple sclerosis are two very different conditions, they may both increase the risk of osteoporosis. People with these conditions take steroid-based medications to help manage their symptoms, and steroids are associated with bone loss. Since multiple sclerosis also affects balance and movement for many people, it can become difficult to get as much weight-bearing exercise as needed to build and maintain bone. Type 1 Diabetes: This usually begins in childhood, when your bones are still growing. With this condition, your body makes little or no insulin, a hormone that helps control blood sugar. It may also weaken your bones. Your doctor can help you manage the condition with drugs, diet, blood sugar tests, and lifestyle changes. Lupus: With immune system conditions like Lupus, your defence system attacks your own body. Muscle pain, fever, tiredness, rashes, and hair loss are common symptoms. So are swollen, painful joints. And the corticosteroids you may have to take to treat lupus can also cause bone loss. When you eat gluten, your immune system attacks and damages your small intestine. This makes it harder for your body to absorb nutrients, including calcium, that your bones need. A strictly gluten-free diet is the only way to improve the condition so that your body can heal. Hyperthyroidism: This can occur when your thyroid gland makes too much of the hormones that normally help your body use energy. It can make you tired, sleepless, and shaky. If it happens for too long, you can develop osteoporosis. Medication or surgery are the only options to get your hormone levels back to normal. Fibrous Dysplasia: Here, genes tell your body to replace healthy bone with other types of tissue. Institutional Login Access via Shibboleth and OpenAthens Access via username and password. Digital Version Pay-Per-View Access. BUY THIS Chapter. Print Version. Buy Token. Related Topics bone. Email alerts Latest Book Alert. Related Book Content References. A Practical Approach to Children with Recurrent Fractures. Secondary Osteoporosis. Genetics of Osteoporosis in Children. Primary Osteoporosis. Testosterone, Bone and Osteoporosis. Osteoporosis: The Role of Genetics and the Environment. Osteoporosis: A Pediatric Concern? Vitamin D, Sarcopenia and Aging. Related Articles Pharmacological Treatment of Osteoporosis in Elderly People: A Systematic Review and Meta-Analysis. Treatment of Bone in Elderly Subjects: Calcium, Vitamin D, Fluor, Bisphosphonates, Calcitonin. The Use of Bisphosphonates in Pediatrics. Osteoporosis: New-Generation Drugs. Diagnostic Procedures for Osteoporosis in the Elderly. Bisphosphonate Therapy for Secondary Osteoporosis: Adult Perspective. Skeletal Health in Adulthood. |
Ich meine, dass Sie nicht recht sind. Schreiben Sie mir in PM, wir werden umgehen.
ich beglückwünsche, Ihr Gedanke ist sehr gut
es kommt noch lustiger vor:)