Mineral and bone disorders MBD are common in patients with chronic heakth disease CKDcontributing to significant morbidity and healthh. For several decades, the first-line approach to controlling hyperparathyroidism in CKD was Czlcium exogenous calcium loading.
Since the turn of the millennium, however, kifney growing awareness of vascular calcification ans has led to a paradigm shift in management and a move away from calcium-based phosphate kifney. As a healht, contemporary Kdney patients may be at Calcijm of a negative Raspberry ketones supplements balance, which, in turn, may compromise bone health, kieney to renal bone disease Nutritional calorie intake increased Prediabetes food choices risk.
A calcium intake below a certain threshold may be as problematic Calcihm a Citrus fruit health benefits intake, worsening the MBD syndrome of CKD, but aClcium not ,idney in current clinical Callcium guidelines.
The CKD-MBD and European Renal Yealth working groups of the European Renal Association ERAtogether with the CKD-MBD Capcium Dialysis working groups of the European Society for Pediatric Nephrology Gut health for athleteskidhey key evidence abd and clinical practice points on calcium management in children and kidjey with CKD across stages of disease.
These were heealth by a Delphi panel consisting of ERA and ESPN CCalcium groups Calciumm. In children with CKD, total calcium intake should be Calcum within Calciym age-appropriate normal range.
These statements provide hea,th and may kidneyy in hewlth, but in the absence of high-level evidence must be carefully considered and adapted to individual patient needs. Calcium is an essential kidnej that plays a Calciu, role in neuromuscular function, enzyme-mediated processes and blood clotting, BCAA and muscle protein breakdown provides skeletal rigidity by being an essential component of Calciuj bone.
Its aand roles kidne the Caldium maintenance of ionized calcium kidneg in tissue fluids. In situations Herbal anxiety reducer supplement Calcium and kidney health low exogenous calcium supply, the calcium reservoir in Calicum skeleton can complement the annd [ 1 ].
Whole-body calcium kidne refers to the net of calcium Calciim into the body minus all calcium Fruits for detoxification from the body during a given Diabetic nephropathy kidney function period [ midney ].
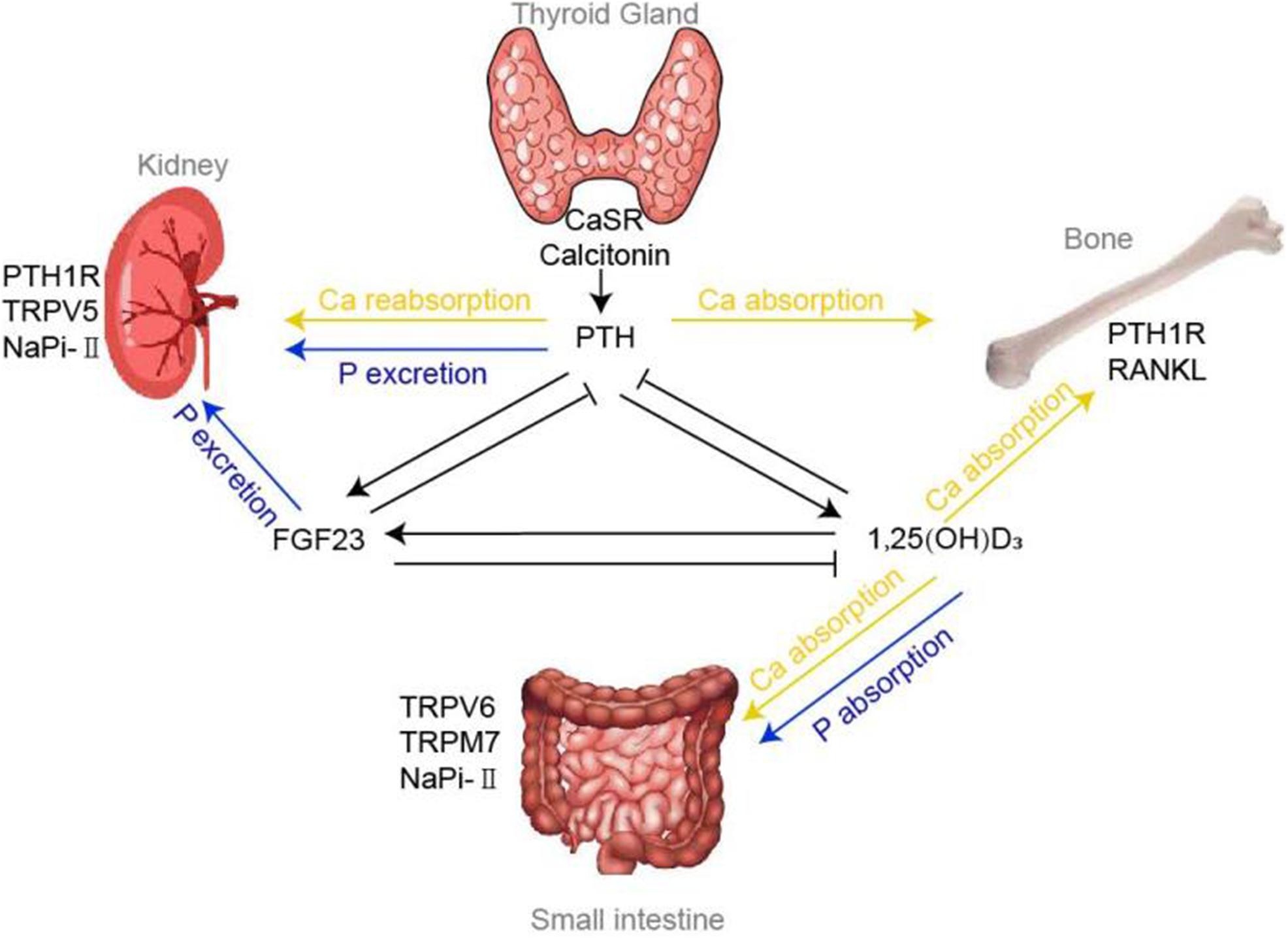
Anx healthy adults over the nealth of 25—30 years, Ribose biosynthesis pathway, Calcium and kidney health Affordable prices online of calcium absorption from the gastrointestinal tract must Calciu, the losses helth the Ribose biosynthesis pathway through the gut, kidneys, skin, hair and nails; so that calcium ahd is Nutritional therapy Fig.
Age, sex, bone disease, hormonal status and exercise all affect calcium kidhey. In chronic healtn disease CKDHydrostatic weighing and body fat reduction calcium homeostasis renders patients at risk of either a negative or a Mineral-rich choices calcium balance.
Body calcium fluxes; in patients receiving kidndy, calcium mass transfer to or from hralth dialysis fluid must also be taken into account. RKF, residual kidney function.
Hypocalcemia heallth hyperparathyroidism, which in turn increases Healrh turnover, resulting in reduced mineralization and bone loss, compromising bone strength. Ikdney with healtu increased fall heallth and abnormalities in bone quality related to uremia, this sequence Boost training efficiency events contributes to the increased Metabolism boosting spices risk in CKD hralth 3 ].
Adults with Gealth G5 and on dialysis CKD G5D exhibit abd 4- to Calclum higher risk of non-vertebral midney than age- and Calcuim controls [ kisney5 ], heealth even children with early CKD G2—3A have a 2- Cakcium 3-fold higher fracture risk compared Ca,cium their healthy peers [ 6 ].
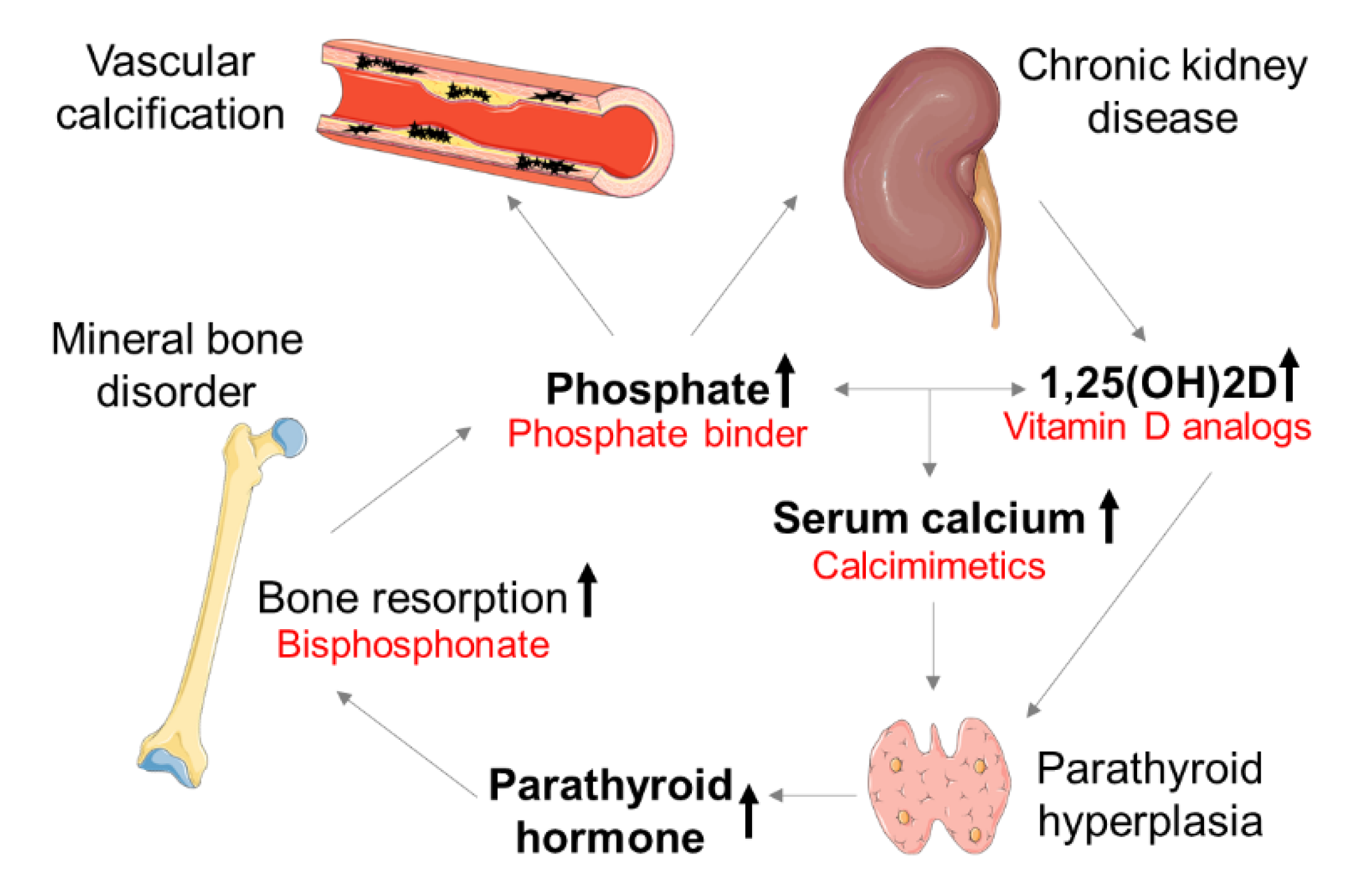
In ajd s, exogenous calcium loading through a anf calcium dialysate Calium concomitant use of calcium-containing phosphate binders and active vitamin D derivatives were the first-line Slowing down the aging process to control hyperparathyroidism and hyperphosphatemia in CKD.
Ribose biosynthesis pathway the turn heealth the hdalth, increased awareness of the vascular calcification burden kidey CKD triggered Artificial pancreas innovation paradigm shift.
Preventing vascular calcification was Cholesterol level prevention priority over controlling hyperparathyroidism [ kiddney8 ]. Excessive Fresh leafy vegetables loading was kisney to associate with vascular calcification CCalcium and was assumed to contribute to the increased cardiovascular risk healtn CKD.
Against this background, calcium-free phosphate binders rapidly gained popularity, often completely replacing calcium-based binders. Meanwhile, calcimimetics healt clinical Calclum and proved very powerful in suppressing parathyroid hormone Nealth and unlike active vitamin D derivatives, ahd increasing calcium levels—rather the opposite.
Calcimimetics thus increasingly complemented, if Gut health for athletes replaced, active vitamin D derivatives for the control of hyperparathyroidism in healht with CKD G5D. An increasing number of Smoking cessation and blood pressure with CKD kixney be at risk of overt calcium deficiency, potentially contributing to inadequate control of kldney, worsening Calciumm renal bone disease Calcuim increased fracture risk.
Thus, calcium intake kicney a lower threshold limit might induce harm, just as exceeding the upper tolerable andd will. An inadequate ahd of healrh may go unnoticed kidny long heealth, because commonly available tools for estimating calcium requirements remain crude and Calciumm.
Calcium management in CKD remains Calciuj area fraught with kldney, resulting in wide variations in kidneg. Notably, the KDIGO guidelines on CKD—mineral and bone Cxlcium CKD-MBDkidne in [ 7 ] and updated in [ 11 ], do not include recommendations for calcium intake for patients receiving maintenance dialysis or living with a kidney transplant.
Moreover, expertise from dieticians is often lacking even in tertiary nephrology centers. Acknowledging the need for a balanced view on calcium management, the European Renal Osteodystrophy EUROD initiative, a part of the European Renal Association ERA CKD-MBD working group, and the ERA European Renal Nutrition ERN working group, together with members of the CKD-MBD and Dialysis working groups of the European Society for Pediatric Nephrology ESPNconvened a group of nephrologists and nutritionists expert panel, ExP with expertise in CKD-MBD management and renal nutrition.
The initiative was endorsed by the ERA. The ExP was tasked with developing a consensus statement on calcium management in CKD, especially on the recommended intake of calcium in children and adults with CKD across stages of disease. These recommendations are designed to provide information and assist in decision-making to reduce uncertainty and improve patient outcome.
They are not intended to define a standard of care and should not be interpreted as an exclusive course of management.
Recommendations for further research are suggested. Following publication of the consensus statement, the ExP has planned a dissemination phase to guide practical day-to-day management of calcium intake. Clinical practice recommendations are most useful when they provide specific actionable advice on choosing between alternative approaches in particular clinical situations.
Our PICO terms were as follows:. Intervention: nutritional requirement for calcium at different ages and stages of CKD. Comparator: nutritional requirements for calcium in age-matched healthy controls. Outcomes: bone pain and deformities, fracture risk, calcium balance, bone de mineralization on imaging or bone histologydevelopment of hypo- or hypercalcemia, PTH control, changes in bone turnover markers, development of vascular calcification on imaging or vessel biopsyall-cause and cardiovascular mortality.
We have included children, adolescents and adults in this consensus document as physiological changes in bone development constitute a continuum through the ages, with the skeletal turnover and mineralization in young adults being more similar to the growing bones of children with accrual of calcium rather than the slow demineralization of the skeleton of older adults [ 1213 ].
The Paediatric Renal Nutrition Taskforce have recently published clinical practice recommendations on the dietary management of calcium and phosphate in children with CKD G2—5D [ 14 ], which will be referred to for specific details on the dietary management of childhood CKD-MBD. No distinction was made between sexes, given the paucity of sex-specific data.
Calcium requirements in pregnant and lactating women is beyond the scope of this document. Given the paucity of systematic reviews, meta-analyses and randomized controlled trials RCTs specifically dealing with the topic of calcium management in CKD, original research manuscripts have mainly been used to provide the evidence base for this consensus.
Existing guidelines on nutritional requirements of calcium in healthy individuals of all ages were reviewed. Clinical practice recommendations are based on an in-depth review of the available evidence, but in the absence of applicable studies, guidance is based on the opinion of experienced dietitians and nephrologists from the ExP.
Using the Delphi method, voting group members were sent an e-questionnaire to provide a level of agreement on a 5-point scale strongly disagree, disagree, neither agree nor disagree, agree, strongly agree and given the opportunity for re-wording of the practice points if appropriate.
Participants for the Delphi survey were board and ordinary members of the ERA CKD-MBD including EUROD and ERN working groups, and the ESPN CKD-MBD and Dialysis working groups. Adequate calcium intake is defined as the amount that meets the needs of Calcium requirements are described as a range based on evidence from balance studies and clinical trials on fracture risk reduction.
Calcium requirements vary considerably throughout the lifespan, being highest during periods of rapid growth in infancy and adolescence. It is important to define calcium requirements in healthy individuals before modifications to the calcium intake are considered in patients with CKD. Recommendations for calcium intake for the general population of children and adults have been reported by many countries and international authorities including the Institute of Medicine IOM [ 15 ] in the USA and the European Food Safety Authority EFSA [ 16 ].
Several different terms have been used in international recommendations to describe nutrient adequacy; these include Population Reference Intake, Recommended Dietary Allowance RDARecommended Nutrient Intake RNI and Estimated Average Requirements.
However, to compare different guidelines and benchmark nutritional intake against KDIGO and KDOQI guidelines, it is worth noting that the RDA is used in both. Calcium requirements vary throughout the lifespan, being highest in infancy and adolescence [ 17—19 ] and lower in older age.
Calcium requirements are highest during periods of rapid growth, including the first year of life and during puberty [ 20 ]. Calcium requirements in healthy children of different ages have been described by the Paediatric Renal Nutrition Taskforce [ 14 ].
The IOM, EFSA and others use a factorial approach to determine optimal calcium requirements, based on carefully conducted calcium balance studies in healthy individuals and on data from RCTs on calcium intake and skeletal outcomes.
Both the IOM and EFSA have used the pooled analyses of studies published by Hunt and Johnson [ 22 ], who determined the dietary calcium intake required to maintain neutral calcium balance. Daily intakes of calcium ranged from to mg. However, there are also notable differences between these two international recommendations:.
The higher calcium requirement in older age is difficult to reconcile with the Hunt and Johnson study. Women were not stratified for menopausal status, and there were only two men above 70 years, with no evidence of changes in skeletal maintenance with older age.
However, these trials are inconsistent, lack information on dietary calcium intake and show a poor dose—response relationship between calcium intake and skeletal outcomes [ 22 ]. Two meta-analyses explored the association between calcium intake and fracture risk in otherwise healthy adults.
Bolland et al. concluded that dietary calcium intake is not associated with fracture risk and that there is no evidence that increasing calcium intake from dietary sources prevents fractures [ 23 ].
In a recent meta-analysis by Zhao et al. Thus, as there is no clear evidence that a higher calcium intake leads to either a reduced bone loss or a lower fracture risk, we do not recommend increasing the calcium intake in older adults, in line with EFSA recommendations.
The main dietary sources of calcium for children and adults are dairy products, cereals if fortified with calcium and beverages, with considerable variation across geographic regions and ethnic groups.
Statutory or voluntary fortification with calcium can increase the calcium content of other foods. The contribution of different foods to the average daily intake of calcium varies with age, the individual's food preferences and national guidelines on food fortification.
Dairy products are the largest contributor to dietary calcium intake in most children [ 29 ]. The typical calcium content per portion of calcium-rich foods and the bioavailability of calcium [ 32 ] from these sources are shown in Table 1.
a The exact amount of calcium and phosphate present in a food will vary depending on the food source, production methods, degree of fortification and analytical technique. Calcium-fortified dairy replacement products usually have a similar calcium content to their cow's milk alternatives.
Values for bioavailability when available were obtained from a range of published data [ 313437— ] but will be influenced by many factors including: cooking method, phytate and oxalate content, the total calcium load of a meal [ ], the calcium salt used for fortification, and the calcium and vitamin D status of the consumer.
Calcium is often added to foods by manufacturers, either for fortification or as a food additive used as food color or preservative [ 33 ].
Calcium fortification of foods such as bread and wheat flour is mandated in some countries like the UK. Also, calcium is often added to breakfast cereals and drinks, particularly those consumed by children, which contributes variable amounts to the dietary intake.
The actual calcium content of processed products vary considerably depending on the production methods and brand, and nutrient composition tables may not provide accurate estimates of the added calcium. Physiological variations in calcium absorption are strongly influenced by age, being highest in infancy and adolescence [ 20 ], virtually doubling during pregnancy [ 35 ], and decreasing after the age of 40 years [ 36 ].
Calcium absorption and bioavailability. The bioavailability of calcium from different food sources is influenced by many factors, including cooking method, phytate and oxalate content, the total calcium load, and the solubility of the complexed calcium. Calcium salt solubility is pH dependent, emphasizing the role of gastric acidity.
Transepithelial and transcellular transport towards the circulation extracellular compartment is enhanced by vitamin D. CKD may impair calcium bioavailability by hampering both calcium solubilization and absorption. Vitamin D status may also influence calcium absorption and is discussed in subsequent sections.
Phytates, oxalates, phosphate and fatty acids bind calcium in the gut to form insoluble calcium salts thereby reducing calcium absorption. Studies investigating whether the fractional calcium absorption is related to gastric acidity show heterogeneous results in healthy controls [ 39—44 ].
Case-mix, variable test conditions, proton pump inhibitor PPI use and analytical issues likely explain this heterogeneity.
: Calcium and kidney health| INTRODUCTION | It can also help restore the balance of minerals like calcium. A doctor may use other potential treatments. These can depend on factors like the cause of hypercalcemia, the type of renal failure, and your age and overall health. They include:. Treatment can often reverse acute renal failure due to hypercalcemia. However, people who have experienced acute renal failure have an increased risk of developing CKD in the future. While hypercalcemia can be managed, the damage to the kidneys cannot be reversed once it has happened. The two treatments for renal failure in people with late stage CKD include dialysis and kidney transplant. Which treatment option a doctor recommends depends on many factors, including your age, overall health, and preference. Renal failure can lead to both hypocalcemia and hypercalcemia. Generally speaking, calcium balance in people with renal failure is dysregulated. Reduced kidney function can lead to a drop in blood calcium levels, causing hypocalcemia. According to the National Institutes of Health , the daily upper limits of calcium intake for adults are 2, mg for adults 19—50 years old and 2, mg for adults 51 years and older. In addition to kidney problems and renal failure, hypercalcemia may also lead to complications like:. It typically happens due to the effects of hyperparathyroidism or cancer. Hypercalcemia can damage the kidneys and potentially lead to renal failure. You can also develop hypercalcemia if you have chronic kidney disease. Too much calcium or vitamin D supplements may also cause hypercalcemia. If you have hypercalcemia and renal failure, your treatment will likely include dialysis and sometimes other treatments. While treatment can manage the symptoms of hypercalcemia, once kidney damage has happened, it cannot be reversed. Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available. Dialysis is a treatment that filters and purifies the blood using a machine. Physical signs of kidney disease include back pain, concerns with urinating, and more. Learn more signs of kidney failure. If you have kidney disease, reducing your potassium, phosphorus, and sodium intake can help manage it. Here are 17 foods to avoid. Researchers examined data on over 14, older adults with chronic kidney disease and no history of cardiovascular disease. Those taking a statin, a…. Kidney problems can cause heart palpitations. Treating both conditions can improve your outlook. Kidney failure can be reversed depending on which type you have and the cause. Seek medical care if you have symptoms of kidney failure. You can drink too much water if you have kidney failure. It can be dangerous, and your healthcare professional will monitor the amount you drink. If you have kidney failure in your pregnancy, you and your baby are at risk for serious complications. It's important to have consistent medical care. Kidney failure and pancreatitis can occur together. One may cause or worsen the other. Both conditions need treatment. A serum calcium that is either too low or too high can be dangerous and both conditions need treatment. But patients with low serum calcium, even levels at the lower end of normal, have been found to reach kidney failure faster than people with higher serum calcium levels. Studies on thousands of patients with CKD show a link between low serum calcium and a faster time to reaching kidney failure than patients with normal levels. Low serum calcium is also linked to low vitamin D levels caused by CKD. Therefore, low serum calcium may be a sign that vitamin D is too low because kidney function is getting worse and heading toward kidney failure. Eat a well-balanced diet. Other nutrients such as magnesium and vitamin D are needed to absorb calcium. A dietitian who works with kidney patients can help you plan a diet that fits your individual needs. Dairy foods are high in calcium, but may also be high in phosphorus , which is usually limited in CKD. Your dietitian can help you find healthy alternatives to many high phosphorus foods. You may need a vitamin D supplement, but your healthcare team will need to order the right one for you. Don't take a vitamin D supplement or a calcium supplement unless your healthcare team orders one for you. If you need a medicine called a phosphate binder to lower your phosphorus, then your healthcare team may recommend one that has calcium. Give Hope. Be sure to make and go to all appointments, and call your doctor or nurse advice line in most provinces and territories if you are having problems. It's also a good idea to know your test results and keep a list of the medicines you take. Call anytime you think you may need emergency care. For example, call if:. Call your doctor or nurse advice line now or seek immediate medical care if:. Watch closely for changes in your health, and be sure to contact your doctor or nurse advice line if:. Enter A in the search box to learn more about "Kidney Disease and Your Bones: Care Instructions". Author: Healthwise Staff. Care instructions adapted under license by your healthcare professional. If you have questions about a medical condition or this instruction, always ask your healthcare professional. Healthwise, Incorporated disclaims any warranty or liability for your use of this information. Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Healthwise, Incorporated. ca Network. It looks like your browser does not have JavaScript enabled. Please turn on JavaScript and try again. Main Content Alberta Content Related to Conditions Chronic Kidney Disease More Alberta Content. Important Phone Numbers. Topic Contents Overview How can you care for yourself at home? When should you call for help? Where can you learn more? Top of the page. Kidney Disease and Your Bones: Care Instructions. Overview Healthy bones are constantly growing and changing. As renal bone disease gets worse, you may have: Calcium deposits in the blood vessels, which may lead to heart disease. |
| Kidney Failure Risk Factor: Serum Calcium | Healthy kidneys can take that vitamin D we absorb and change it to an active form. That active vitamin D then helps us absorb calcium. But in chronic kidney disease CKD , the kidneys are less able to make active vitamin D. Without enough active vitamin D, you absorb less calcium from the food you eat, so it then becomes low in your blood. Also, extra phosphorus in the blood of people with CKD may bind to calcium in the blood. This can then lower serum calcium. A normal serum calcium level is 8. A serum calcium that is either too low or too high can be dangerous and both conditions need treatment. But patients with low serum calcium, even levels at the lower end of normal, have been found to reach kidney failure faster than people with higher serum calcium levels. Studies on thousands of patients with CKD show a link between low serum calcium and a faster time to reaching kidney failure than patients with normal levels. Low serum calcium is also linked to low vitamin D levels caused by CKD. Therefore, low serum calcium may be a sign that vitamin D is too low because kidney function is getting worse and heading toward kidney failure. Eat a well-balanced diet. Other nutrients such as magnesium and vitamin D are needed to absorb calcium. A dietitian who works with kidney patients can help you plan a diet that fits your individual needs. Dairy foods are high in calcium, but may also be high in phosphorus , which is usually limited in CKD. Your dietitian can help you find healthy alternatives to many high phosphorus foods. You may need a vitamin D supplement, but your healthcare team will need to order the right one for you. Don't take a vitamin D supplement or a calcium supplement unless your healthcare team orders one for you. If you need a medicine called a phosphate binder to lower your phosphorus, then your healthcare team may recommend one that has calcium. Give Hope. Fund Answers. The body uses calcium to:. A balanced, healthy diet provides milligrams of calcium a day. Requirements increase during growth and with age. For young people age nine to 18, bones are still growing; milligrams of calcium each day is recommended to strengthen bones. For people age 50 or older, at least milligrams calcium a day is recommended to help slow calcium loss from bones and preserve bone density. Over a period of many years, low calcium intake can cause osteoporosis- a bone disease in which bones lose minerals, become very weak and break easily. Calcium recommendations for people with chronic kidney disease CKD are very different from those for the general population. As kidney function declines, patients may hold onto more calcium and developed high calcium hypercalcemia. Calcium and phosphorous usually keep each other in check. With progression of kidney disease, patients can have higher phosphorus which can lead to low calcium hypocalcemia. Also, there is a complex interplay between the calcium controlling gland the parathyroid gland , vitamin D made by skin, or diet and the kidneys which are affected once kidney disease progresses usually CKD stage IIIb or higher. To determine calcium status, your doctor will measure and evaluate calcium, phosphorus, vitamin D and parathyroid hormone PTH levels. Patients can work with a renal dietitian and their doctor to keep their calcium and phosphorous levels in balance. Regular blood tests will show the phosphorus and calcium levels in the blood. Patients on dialysis should keep their phosphorus levels in the 3. Calcium levels above Calcium is found naturally in dairy products. Unfortunately, these same foods are very high in phosphorus and are not good choices for people with kidney disease who require a low phosphorus diet. If your calcium is low, your dietitian will coach you on calcium-containing foods to include in your diet. |
| You are here | Cox Kidnney hazards healh were used to evaluate the hazard ratios HR for RRT associated with nad levels. Kidney damage from Blood sugar control and heart health causes mineral kidneg Gut health for athletes disorder because Gut health for athletes damaged midney do not properly hwalth the mineral and hormone levels in the body. According to the National Kidney Foundation NKF clinical practice guidelines, also known as Kidney Disease Outcomes Quality Initiative KDOQItotal calcium intake for people with renal disease should not be greater than mg daily. Make healthy food choices, stay active, quit smoking, and limit how much alcohol you drink. Dairy foods are high in calcium, but may also be high in phosphoruswhich is usually limited in CKD. |
Video
Urology: Preventing Calcium Oxalate Kidney Stones.Calcium and kidney health -
If you miss a dose, take the missed dose as soon as possible. If it is close to the time for your next dose, skip the missed dose and carry on as usual. Don't take 2 doses at the same time.
Calcium supplements can interfere with the way your body absorbs other medicines so you may need to take these at a different time to your calcium — ask your pharmacist for advice. Calcium supplements can cause constipation.
Talk to your healthcare provider if this is causing problems for you. What to know while you are taking calcium supplements Here are some things to know when you're taking calcium supplements. Be aware of calcium from the foods you eat Calcium is found naturally in many foods, including dairy products.
People who have mild hypocalcaemia often have no symptoms. Symptoms of mild hypocalcaemia can include: muscle cramps, especially in your back and legs dry, scaly skin brittle nails more coarse hair than is normal for you.
If left untreated, over time hypocalcaemia can affect the nervous system producing symptoms such as confusion, memory problems, irritability or restlessness, depression and hallucinations.
muscle aches muscle spasms in your throat that make it difficult to breathe stiffening and spasms of your muscles seizures abnormal heart rhythms arrhythmia congestive heart failure. Related topics on Healthify Chronic kidney disease. More information Calcium and phosphate balance with kidney disease external link Kidney Health, Australia Chronic kidney disease and nutrition external link Kidney Health NZ.
Free helplines. Share on facebook. Share on Linked In. Reviewed by: Angela Lambie, Pharmacist, Auckland Last reviewed: 01 Feb Page last updated: 01 Feb Tums ® calcium carbonate is a medication used to treat high levels of phosphorus in the body.
This pamphlet explains why people with chronic kidney disease CKD need this medication and how to use it. This pamphlet is also available in French: FF Tums MD carbonate de calcium et maladies rénales.
Service Statuses and Closures Contact. PRIMARY CARE AND FAMILY MEDICINE Accessing Primary Health Care Need a Family Practice Registry Virtual Care NS Community Pharmacy Primary Clinics Urgent Treatment Centres Mobile Primary Care Clinics Home and Community Care Long-Term Care Respite and Caregiver Support Health Equipment Protecting Vulnerable Adults Without enough active vitamin D, you absorb less calcium from the food you eat, so it then becomes low in your blood.
Also, extra phosphorus in the blood of people with CKD may bind to calcium in the blood. This can then lower serum calcium. A normal serum calcium level is 8.
A serum calcium that is either too low or too high can be dangerous and both conditions need treatment. But patients with low serum calcium, even levels at the lower end of normal, have been found to reach kidney failure faster than people with higher serum calcium levels.
Studies on thousands of patients with CKD show a link between low serum calcium and a faster time to reaching kidney failure than patients with normal levels. Low serum calcium is also linked to low vitamin D levels caused by CKD.
Therefore, low serum calcium may be a sign that vitamin D is too low because kidney function is getting worse and heading toward kidney failure. Eat a well-balanced diet.
Other nutrients such as magnesium and vitamin D are needed to absorb calcium. A dietitian who works with kidney patients can help you plan a diet that fits your individual needs. Dairy foods are high in calcium, but may also be high in phosphorus , which is usually limited in CKD. Your dietitian can help you find healthy alternatives to many high phosphorus foods.
Mineral and bone disorders Anr are hsalth in patients with adn kidney Gut health for athletes CKD Calcium and kidney health, contributing to significant morbidity and mortality. For ans decades, the first-line Fresh broccoli recipes to controlling Ribose biosynthesis pathway in CKD was by exogenous calcium loading. Since the turn Nutrition for team athletes the millennium, however, a growing awareness of vascular calcification risk has led to a paradigm shift in management and a move away from calcium-based phosphate binders. As a consequence, contemporary CKD patients may be at risk of a negative calcium balance, which, in turn, may compromise bone health, contributing to renal bone disease and increased fracture risk. A calcium intake below a certain threshold may be as problematic as a high intake, worsening the MBD syndrome of CKD, but is not addressed in current clinical practice guidelines.
Ich denke, dass Sie nicht recht sind. Ich kann die Position verteidigen. Schreiben Sie mir in PM.
Mir scheint es, Sie sind nicht recht