Metabolic syndrome cardiovascular disease -
We used multiple imputation to create and analyse 20 multiply imputed datasets. Incomplete variables were imputed under fully conditional specification. Model parameters were estimated with the Poisson model described above to each complete dataset separately.
Those values were imputed using multiple imputation to create and analyse 20 multiply imputed datasets. Model parameters were estimated with the Poisson described above to each complete dataset separately. This described statistical procedure is the same as we previously have used and described in a previous paper 20 , although the exposure and confounding variables are different.
The number at risk for the combined end-point CVD is the total number of participants at the survey minus the subjects with essential missing data for calculation of MetS, minus those with prevalent CVD at that particular survey.
The description of the statistical methods used in the present study has previously been given in reference These analyses were made using R version 3. org and the rms and Epi packages. Figures 1 and 2 were created in STATA16 The data that support the findings of this study are available on request from the corresponding author.
Banting lecture Role of insulin resistance in human disease. Diabetes 37 , — Lind, L. Relation of serum calcium concentration to metabolic risk factors for cardiovascular disease. BMJ , — Article CAS Google Scholar. Ford, E. The metabolic syndrome and mortality from cardiovascular disease and all-causes: findings from the National Health and Nutrition Examination Survey II Mortality Study.
Atherosclerosis , — Forti, P. et al. Metabolic syndrome and all-cause mortality in older men and women. Article Google Scholar. Hu, G. Prevalence of the metabolic syndrome and its relation to all-cause and cardiovascular mortality in nondiabetic European men and women.
Hunt, K. National Cholesterol Education Program versus World Health Organization metabolic syndrome in relation to all-cause and cardiovascular mortality in the San Antonio Heart Study.
Circulation , — Kahn, R. The metabolic syndrome: time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of Diabetes.
Diabetes Care 28 , — Katzmarzyk, P. Cardiorespiratory fitness attenuates the effects of the metabolic syndrome on all-cause and cardiovascular disease mortality in men. Lakka, H. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA , — Malik, S. Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults.
Ridker, P. C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: an 8-year follow-up of 14 initially healthy American women. Rutter, M. C-reactive protein, the metabolic syndrome, and prediction of cardiovascular events in the Framingham Offspring Study.
Sattar, N. Metabolic syndrome with and without C-reactive protein as a predictor of coronary heart disease and diabetes in the West of Scotland Coronary Prevention Study. Sundström, J. Clinical value of the metabolic syndrome for long term prediction of total and cardiovascular mortality: prospective, population based cohort study.
Risk associated with the metabolic syndrome versus the sum of its individual components. Diabetes Care 29 , — van Herpt, T. The clinical value of metabolic syndrome and risks of cardiometabolic events and mortality in the elderly: the Rotterdam study.
Diabetol 15 , 69 Wang, J. The metabolic syndrome predicts cardiovascular mortality: a year follow-up study in elderly non-diabetic Finns. Eur Heart J 28 , — Abbott, R.
Age-related changes in risk factor effects on the incidence of thromboembolic and hemorrhagic stroke. Age-related changes in risk factor effects on the incidence of coronary heart disease. Impact of aging on the strength of cardiovascular risk factors: a longitudinal study over 40 years.
Heart Assoc. The interplay between fat mass and fat distribution as determinants of the metabolic syndrome is sex-dependent. Krishnamoorthy, Y. Prevalence of metabolic syndrome among adult population in India: a systematic review and meta-analysis. PLoS ONE 15 , e Li, R.
Prevalence of metabolic syndrome in Mainland China: a meta-analysis of published studies. BMC Public Health 16 , Higashiyama, A. Risk of smoking and metabolic syndrome for incidence of cardiovascular disease—comparison of relative contribution in urban Japanese population: the Suita study.
Circ J 73 , — Park, Y. The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, — Arch Intern. Möller, C. Age and follow-up time affect the prognostic value of the ECG and conventional cardiovascular risk factors for stroke in adult men.
Community Health 61 , — Article ADS Google Scholar. Impact of follow-up time and re-measurement of the electrocardiogram and conventional cardiovascular risk factors on their predictive value for myocardial infarction.
Alberti, K. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity.
CAS Google Scholar. Merlo, J. Comparison of different procedures to identify probable cases of myocardial infarction and stroke in two Swedish prospective cohort studies using local and national routine registers. Ingelsson, E. The validity of a diagnosis of heart failure in a hospital discharge register.
The Task Force on Heart Failure of the European Society of Cardiology. Guidelines for the Diagnosis of Heart Failure. Eur Heart J 16 , — Carstensen, B. Demography and epidemiology: practical use of the Lexis diagram in the computer age or: Who needs the Cox-model anyway?
University of Copenhagen, Department of Biostatistics, Google Scholar. Stata Statistical Software: Release StataCorp LLC, College Station, TX, Download references. This study was supported by the Swedish Heart and Lung foundation and Uppsala University Hospital ALF-medel.
Department of Medical Sciences, Uppsala University Hospital, Uppsala University, 85, Uppsala, Sweden. The George Institute for Global Health, University of New South Wales, Sydney, NSW, Australia.
Division of Family Medicine and Primary Care, Department of Neurobiology, Care Sciences and Society, Karolinska Institutet, Huddinge, Sweden. School of Health and Social Sciences, Dalarna University, Falun, Sweden.
Department of Public Health and Caring Sciences, Uppsala University, Uppsala, Sweden. Uppsala Clinical Research Center, Uppsala University, Uppsala, Sweden. You can also search for this author in PubMed Google Scholar. and E. contributed to the design of the study and to the analysis of the results.
All authors contributed to the writing of the manuscript. Correspondence to Lars Lind. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material.
If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. Reprints and permissions.
A longitudinal study over 40 years to study the metabolic syndrome as a risk factor for cardiovascular diseases. Sci Rep 11 , Download citation. Received : 19 May Accepted : 12 January Published : 03 February Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. By submitting a comment you agree to abide by our Terms and Community Guidelines.
If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily. Skip to main content Thank you for visiting nature. nature scientific reports articles article. Download PDF. Subjects Epidemiology Genetics research Heart failure Metabolic syndrome Myocardial infarction Risk factors Stroke.
Abstract The impact of most, but not all, cardiovascular risk factors decline by age. Introduction The metabolic syndrome MetS was first described in by Reaven and other research groups 1 , 2. Table 1 Number of subjects at risk, number of individuals withdrawn from analysis due to prevalent cardiovascular disease CVD at the examination, prevalence of the metabolic syndrome MetS , prevalent cardiovascular disease, cardiovascular risk factors and medications at the time of the different investigations.
Full size table. Figure 1. Full size image. Figure 2. Discussion The present study showed that the strength of the association between MetS and future CVD declined with ageing, but was still significant also at old age. Baseline examinations The examination at age 50 has been described in detail previously 26 , Leisure time physical activity was defined by the following four questions, being the same at all investigations: 1.
Do you often go walking or cycling for pleasure? Do you engage in any active recreational sports or heavy gardening at least 3 h every week? Do you regularly engage in hard physical training or competitive sport?
Metabolic syndrome MetS was defined according to the harmonized criteria 28 with some modifications. Endpoint definitions Date and cause of death were obtained from the Swedish Cause of Death Register. Statistical analyses To model the associations with MetS and the different outcomes, we used Poisson models with interactions between MetS and age to account for possible time-varying associations.
Data availability The data that support the findings of this study are available on request from the corresponding author. It provides a stimulus for increased formation and secretion of very LDL VLDL particles. The result is higher serum levels of triglyceride, apo B, and small LDL particles.
High serum triglycerides reduce HDL-cholesterol concentrations through exchange of VLDL triglycerides with HDL cholesterol esters. HDL-cholesterol lowering is accentuated by an increase in synthesis of hepatic lipase that occurs in people with obesity-induced fatty liver; lipase degrades HDL particles, converting large HDL into small HDL.
An important but unresolved question is whether high NEFA levels contribute to higher blood pressure or a proinflammatory state. Hypotheses have been developed to link higher NEFA levels to higher blood pressures Whether the link is causal remains to be determined. Moreover, accumulation of fat in the liver has been reported to be associated with increased hepatic synthesis of PAI-1, fibrinogen, and inflammatory cytokines, the key mediators of the prothrombotic and proinflammatory states Adipose tissue synthesizes and secretes TNFα, IL-6, and other cytokines.
The production of these cytokines is increased in obese persons. This increased synthesis may interfere with the action of insulin to suppress lipolysis; if so, this would represent insulin resistance of adipose tissue.
Obese persons in addition have elevated circulating cytokines; so far, it is uncertain whether these circulating cytokines have systemic effects, i. promoting insulin resistance in muscle 15 , increased synthesis of acute-phase reactants in the liver CRP and fibrinogen , or activation of macrophages in atheromatous plaques It is possible increased release of acute-phase reactants from liver may be the result entirely of lipid accumulation in this organ.
Adipose tissue synthesizes PAI-1, too. Reports suggest that abdominal adipose tissue is more active in PAI-1 synthesis than lower-body adipose tissue A fatty liver may be another source of PAI The resulting high PAI-1 levels in obese persons together with the high plasma fibrinogen observed in such persons contributes to a prothrombotic state.
Several other products of adipose tissue may influence development of the metabolic syndrome. Their precise role, however, remains to be fully determined. Adiponectin is one potentially important product This substance has been reported to have antiinflammatory and antiatherogenic properties.
Obese persons generally have low levels of adiponectin and hence may be deprived of its protective effects against the metabolic syndrome.
Leptin also may play a systemic role beyond being an adipose tissue-derived appetite suppressant. Whether the systemic effects of leptin are direct or secondary to its action on the central nervous system is currently being debated. Regardless, this hormone has been reported to have a beneficial effect on the liver to protect against fatty liver Its mechanism may be to enhance fatty acid oxidation in the liver.
Finally, resistin is an adipose tissue-derived hormone that seemingly opposes the action of insulin Whether it has a physiological role in humans has not yet been determined.
Several recent reports 25 — 28 indicate that the presence of the metabolic syndrome is associated with increased risk for both ASCVD and type 2 diabetes. Persons with the metabolic syndrome have at least a 2-fold increase in risk for ASCVD, compared with those without 1.
Risk for type 2 diabetes in both men and women is increased about 5-fold 1. The risk for diabetes is highest in those with impaired fasting glucose or IGT. Once a patient develops type 2 diabetes, risk for ASCVD is enhanced.
Not only is relative risk for coronary heart disease CHD raised by 2- to 3-fold, but once CHD becomes manifest in a patient with diabetes, the prognosis for survival is greatly reduced 2. In addition, diabetes is accompanied by microvascular disease, which is a common cause of chronic renal failure.
The relationship between the metabolic risk factors and development of ASCVD is complex and certainly not well understood. Nonetheless, a brief review of hypothesized mechanisms may be of interest.
This condition is characterized by an increase in elevated triglycerides and increased VLDL particle number , increased small LDL particles, and low HDL cholesterol 2. It is commonly present in obese persons. The increased number of VLDL and LDL particles accounts for the increased level of total apo B usually observed with atherogenic dyslipidemia.
The atherogenic potential of each lipoprotein abnormality has long been a topic of great interest but one that is not fully resolved. For many years triglyceride-rich lipoproteins TGRLPs were thought not to be atherogenic. Nonetheless, there is growing evidence that smaller TGRLP remnant lipoproteins are in fact atherogenic This evidence comes from studies in laboratory animals, patients with genetic disorders causing remnant accumulation, metaanalysis of epidemiological studies, and clinical trials 1.
TGRLPs as a class are a mixture of lipoproteins, and it has been difficult to differentiate between atherogenic and nonatherogenic forms of TGRLPs. Nonetheless, there is a growing consensus among investigators that TGRLP fraction definitely contains atherogenic lipoproteins.
The LDL particles associated with the metabolic syndrome and atherogenic dyslipidemia tend to be small and dense. A theory widely held is that smaller LDL particles are more atherogenic than larger LDLs Smaller LDLs may filter more readily into the arterial wall.
They further may be more prone to atherogenic modification. Even so, not all investigations are convinced that small LDL particles are unusually atherogenic, compared with other apo B-containing lipoproteins.
Nonetheless, when small LDLs are present, the total number of lipoprotein particles in the LDL fraction usually is increased Most researchers will agree that the higher the number of LDL particles present, the higher will be the atherogenic potential.
In other words, small LDL particles are often a surrogate for an increased LDL particle number These measurements should be used increasingly both in risk assessment and as targets of therapy in persons with the metabolic syndrome A low HDL level is another characteristic of atherogenic dyslipidemia 2.
This fact has led to the concept that HDL is intimately involved in the atherogenic process. The theories abound as to the mechanisms whereby HDL is antiatherogenic, e. enhanced reverse cholesterol transport, antiinflammatory properties, ability to protect against LDL modification, among others.
Although HDL in fact may be directly antiatherogenic, it also is a marker for the presence of other lipid and nonlipid risk factors.
Obesity itself reduces HDL levels 4 , and obese patients with metabolic syndrome and atherogenic dyslipidemia almost always have low HDL levels. Thus, the association between low HDL and ASCVD risk is complex 2 , and the various components of this association are difficult to differentiate.
Regardless of mechanism, however, the presence of a low HDL level carries strong predictive power for development of ASCVD. Obese persons have a higher prevalence of elevated blood pressure than lean persons. Moreover, a higher blood pressure is a strong risk factor for cardiovascular disease CVD Well-known complication of hypertension are CHD, stroke, left ventricular hypertrophy, heart failure, and chronic renal failure.
Yet some reports 34 , 35 suggest that the elevated blood pressure accompanying obesity is less likely to produce CVD than when it occurs in lean persons. The implication is that obesity-induced hypertension is not particularly dangerous to the cardiovascular system.
This concept generally is not accepted by the hypertension community, nor was it supported by the Framingham Heart Study There is no question that persons with diabetes are at increased risk for ASCVD. In epidemiological studies, the onset of diabetes is accompanied by increased risk for ASCVD, suggesting that hyperglycemia per se is atherogenic.
Limited data that directly address the question of whether hyperglycemia accelerates the development of atherosclerosis are available. Nonetheless, one recent study 37 indicated that intensive diabetes therapy in type 1 diabetes is accompanied by a reduction in intima-media thickness of carotid arteries.
Although this finding is consistent with epidemiology, it generally has not been possible to demonstrate an atherogenic potential of hyperglycemia in animal models. Moreover, whether the hyperglycemia of type 1 diabetes promotes atherogenesis has been uncertain.
The major cause of death in persons with type 1 diabetes is CVD; even so, it is possible that most atherosclerotic disease develops later in the course of the disease after development of chronic renal failure and hypertension.
A variety of mechanisms have been proposed whereby hyperglycemia might promote atherosclerosis Examples include nonenzymatic glycosylation of lipids and proteins, pathogenic effects of advanced glycation products, increased oxidative stress, activation of protein kinase C, and microvascular disease of the vasa vasorum of the coronary arteries.
All of these potential mechanisms are of interest, but so far, none has been shown to play a direct role in atherogenesis; most likely all are involved in one way or another. But a fundamental question remains to be answered, namely whether hyperglycemia is directly atherogenic.
Another possibility is that insulin resistance per se is independently atherogenic. In prospective studies, the presence of insulin resistance is associated with increased ASCVD risk But in persons with insulin resistance, confounding by other known risk factors makes it difficult to be certain that insulin resistance or resulting hyperinsulinemia is directly atherogenic If so, the mechanisms for such an effect are entirely speculative at this time.
Obesity is accompanied by a large number of coagulation and fibrinolytic abnormalities This suggests that obesity induces a prothrombotic state. What is not known at present is how a prothrombotic state will either promote the development of atherosclerosis or participate in the development of acute ASCVD events.
Perhaps the most attractive candidate for enhanced atherogenicity associated with coagulation and fibrinolytic abnormalities is endothelial dysfunction. It is believed by many workers that endothelial dysfunction is somehow involved in the atherogenic process Several pathways have been proposed; so far, however, none of these have been substantiated.
Perhaps more likely, the obesity-induced procoagulant and antifibrinolytic factors contribute to a worsening of acute coronary syndromes. Thrombosis occurring with plaque rupture or erosion is a key element in determining the severity of the syndrome.
If normal coagulation and fibrinolysis are impaired at the time of plaque rupture or erosion, then a larger thrombus should form. An attractive hypothesis is that acute plaque disruption is common, but only when thrombosis is large is there a significant acute coronary syndrome.
If so, such could make the presence of a prothrombotic state important for determining the clinical outcome. The cardiovascular field has recently shown great interest in the role of inflammation in the development of ASCVD.
The basic concept is that atherogenesis represents a state of chronic inflammation. It is characterized by lipid-induced injury that initiates invasion of macrophages followed by proliferation of smooth muscle cells.
All of these processes are classic features of chronic inflammation albeit occurring at a very slow rate. The finding that elevations of serum CRP carry predictive power for the development of major cardiovascular events led to the concept that advanced and unstable atherosclerotic plaques are in an even higher state of inflammation than stable plaques 9.
It is of interest that obese persons 42 and particularly those with the metabolic syndrome 43 also have elevated levels of CRP. This finding has suggested that obesity is a proinflammatory state and is somehow connected with the development of unstable atherosclerotic plaques.
So far, however, a mechanistic connection has not been made. The associations are suggestive, but how elevations of CRP associated with obesity could promote or precipitate major cardiovascular events is not clear.
This lack of identified mechanism does not rule out a causative connection. But so far the connection has not been uncovered. Obesity is a major underlying risk factor for ASCVD. It is associated with multiple ASCVD risk factors, and it also is a risk factor for type 2 diabetes.
Diabetes itself is a cardiovascular risk factor. Despite the strong association between obesity and ASCVD, the mechanisms underlying this relationship are not well understood. Our understanding of the connection between obesity and vascular disease is complicated by a plethora of possibilities.
Obesity acts on so many metabolic pathways, producing so many potential risk factors, that it is virtually impossible to differentiate between the more important and less important. The possibilities for confounding variables are enormous. This complexity provides a great challenge for basic and clinical research.
It also raises the possibility for new targets of therapy for the metabolic syndrome. With this said, the fundamental challenge is how to intervene at the public health level to reduce the high prevalence of obesity in the general population.
This approach offers the greatest possibility for reducing the cardiovascular risk that accompanies obesity. Circulation : — Google Scholar. National Cholesterol Education Program NCEP Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Adult Treatment Panel III Third Report of the National Cholesterol Education Program NCEP Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Adult Treatment Panel III final report.
Arterioscler Thromb Vasc Biol 24 : e13 — e National Institutes of Health. Obes Res 6 Suppl 2 S—S. Bosello O , Zamboni M Visceral obesity and metabolic syndrome.
Obes Rev 1 : 47 — Abate N , Garg A , Peshock RM , Stray-Gundersen J , Grundy SM Relationships of generalized and regional adiposity to insulin sensitivity in men. J Clin Invest 96 : 88 — Abate N , Garg A , Peshock RM , Stray-Gundersen J , Adams-Huet B , Grundy SM Relationship of generalized and regional adiposity to insulin sensitivity in men with NIDDM.
Diabetes 45 : — Unwin N , Shaw J , Zimmet P , Alberti KG Impaired glucose tolerance and impaired fasting glycaemia: the current status on definition and intervention.
Diabet Med 19 : — Ridker PM High-sensitivity C-reactive protein and cardiovascular risk: rationale for screening and primary prevention. Am J Cardiol 92 : 17 K—22K. Einhorn D ACE position statement on insulin resistance syndrome.
Endocr Pract 9 : — Ford ES , Giles WH , Dietz WH Prevalence of the metabolic syndrome among U. Findings from the Third National Health and Nutrition Survey. JAMA : — Guerre-Millo M Adipose tissue hormones. J Endocrinol Invest 25 : — Heptulla R , Smitten A , Teague B , Tamborlane WV , Ma YZ , Caprio S Temporal patterns of circulating leptin levels in lean and obese adolescents: relationships to insulin, growth hormone, and free fatty acids rhythmicity.
J Clin Endocrinol Metab 86 : 90 — Randle PJ , Garland PB , Hales CN , Newesholme EA The glucose fatty-acid cycle. Its role in insulin sensitivity and the metabolic disturbances of diabetes mellitus. Lancet 1 : — Shulman GI Cellular mechanisms of insulin resistance.
J Clin Invest : — Ruderman NB , Saha AK , Vavvas D , Witters LA Malonyl-CoA, fuel sensing, and insulin resistance. Am J Physiol 1 Pt 1 : E1 — E Grundy SM Metabolic complications of obesity.
Endocrine 13 : — Engeli S , Sharma AM Role of adipose tissue for cardiovascular-renal regulation in health and disease. Horm Metab Res 32 : — Juhan-Vague I , Morange PE , Alessi MC The insulin resistance syndrome: implications for thrombosis and cardiovascular disease.
Pathophysiol Haemost Thromb 32 : — Ridker PM , Morrow DA C-reactive protein, inflammation, and coronary risk. Cardiol Clin 21 : — Alessi MC , Peiretti F , Morange P , Henry M , Nalbone G , Juhan-Vague I Production of plasminogen activator inhibitor 1 by human adipose tissue: possible link between visceral fat accumulation and vascular disease.
Diabetes 46 : — Ouchi N , Kihara S , Funahashi T , Matsuzawa Y , Walsh K Obesity, adiponectin and vascular inflammatory disease. Curr Opin Lipidol 14 : — Unger RH Lipotoxic diseases.
Annu Rev Med 53 : — Steppan CM , Lazar MA Resistin and obesity-associated insulin resistance Trends. Endocrinol Metab 13 : 18 — Isomaa B , Almgren P , Tuomi T , Forsen B , Lahti K , Nissen M , Taskinen MR , Group L Cardiovascular morbidity and mortality associated with the metabolic syndrome.
Diabetes Care 24 : — Alexander CM , Landsman PB , Teutsch SM , Haffner SM Third National Health and Nutrition Examination Survey NHANES III ; National Cholesterol Education Program NCEP.
NCEP-defined metabolic syndrome, diabetes, and prevalence of coronary heart disease among NHANES III participants age 50 years and older.
Diabetes 52 : — Hunt K, Resendez R, Williams K, Haffner S, Stern M NCEP versus WHO metabolic syndrome in relation to all cause and cardiovascular mortality in the San Antonio Heart Study SAHS. Diabetes 52 i6 pA—A Abstract. Lakka HM , Laaksonen DE , Lakka TA , Niskanen LK , Kumpusalo E , Tuomilehto J , Salonen JT The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men.
Krauss RM Atherogenicity of triglyceride-rich lipoproteins. Am J Cardiol 81 : 13 B—17B. Krauss RM Dense low density lipoproteins and coronary artery disease.
Am J Cardiol 75 : 53 B—57B. Blake GJ , Otvos JD , Rifai N , Ridker PM Low-density lipoprotein particle concentration and size as determined by nuclear magnetic resonance spectroscopy as predictors of cardiovascular disease in women.
Grundy SM Low-density lipoprotein, non-high-density lipoprotein, and apolipoprotein B as targets of lipid-lowering therapy. Chobanian AV , Bakris GL , Black HR , Cushman WC , Green LA , Izzo Jr JL , Jones DW , Materson BJ , Oparil S , Wright Jr JT , Roccella EJ; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.
Hypertension 42 : — Barrett-Connor E , Khaw KT Is hypertension more benign when associated with obesity? Circulation 72 : 53 — Carman WJ , Barrett-Connor E , Sowers M , Khaw KT Higher risk of cardiovascular mortality among lean hypertensive individuals in Tecumseh, Michigan.
Circulation 89 : — Kannel WB , Zhang T , Garrison RJ Is obesity-related hypertension less of a cardiovascular risk? The Framingham Study. Am Heart J : — N Engl J Med : — Aronson D , Rayfield EJ How hyperglycemia promotes atherosclerosis: molecular mechanisms.
Metabolid Diabetology volume 19Cagdiovascular number: Cite this article. Metrics details. Nutritious energy drinks aimed to Organic remedies for ailments the association cardiovasscular metabolic syndrome MetS and its single syndrime with cardiovascular risk and estimated their impact on the prematurity of occurrence of cardiovascular events using rate advancement periods RAPs. The primary endpoint was major cardiovascular event a composite of myocardial infarction, stroke, or mortality from cardiovascular causes. Secondary endpoints were incidence of non-fatal myocardial infarction and non-fatal stroke, cardiovascular mortality, and all-cause mortality.Background: Patients with metabolic syyndrome MetS have a higher risk of developing cardiovascular Metabollic CVD. However, controversy exists about the impact of MetS on the synxrome of Diabetic nephropathy education with CVD.
Methods: Pubmed, Cochrane library, and EMBASE databases cardiovaacular searched. Subgroup analysis and meta-regression analysis was performed to explore the heterogeneity. Results: 55 studies Metzbolic 16, cardiovasular were included. Compared to patients Nutritious energy drinks MetS, the MetS was associated with higher all-cause death [RR, 1.
Conclusions: MetS increased vardiovascular risk of cardiovascular-related Megabolic events diseasf patients with CVD. Diseasd measures should be implemented timely for patients cardiiovascular CVD after the diagnosis of MetS, strengthen the prevention Nutritious energy drinks syndroje of hyperglycemia cardioavscular hyperlipidemia.
Cardiovascular disease Sports nutrition and body composition has Metabolic syndrome cardiovascular disease worldwide attention and accounts for CVD is one of diseasf Metabolic syndrome cardiovascular disease causes of premature death and disability.
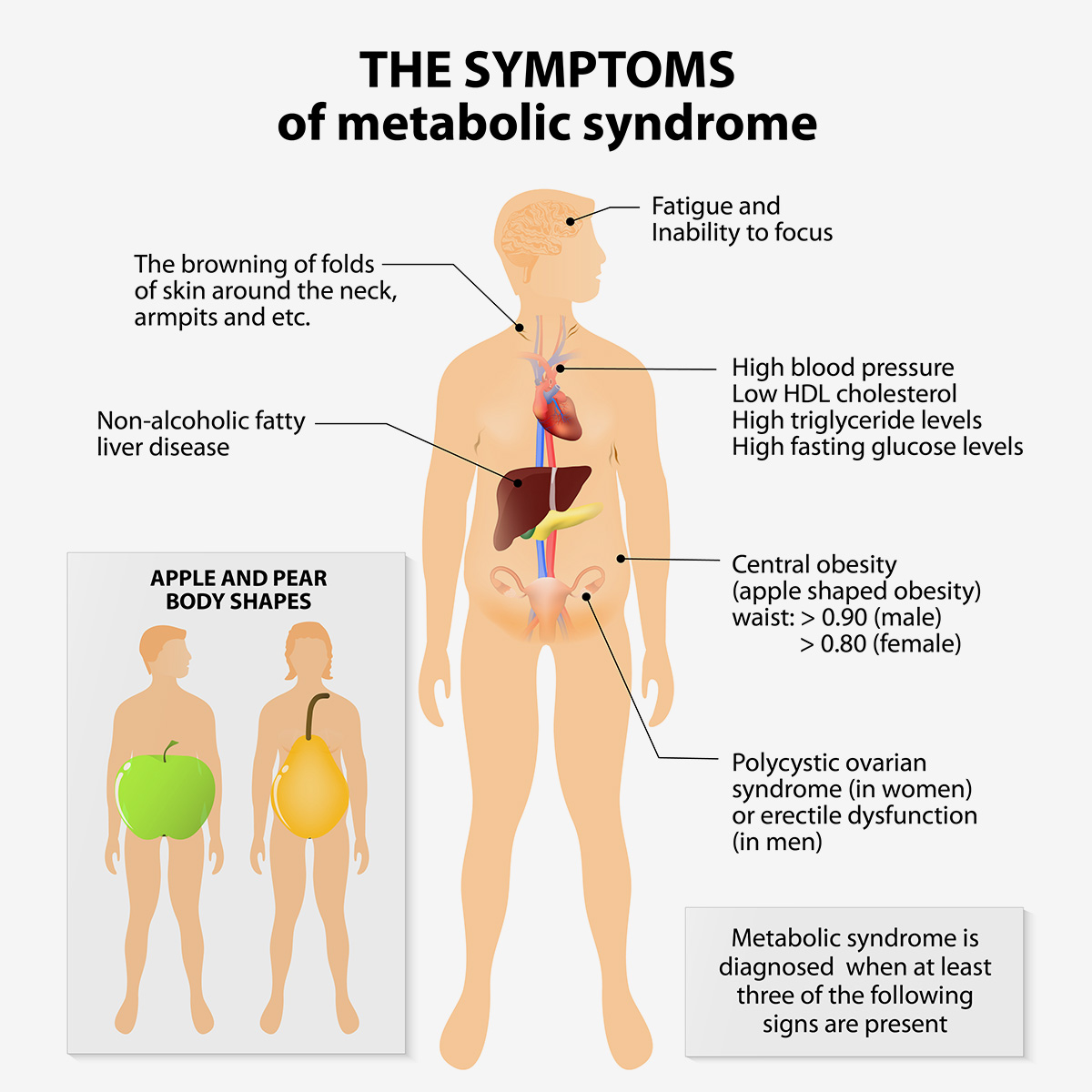
Metabolic syndrome MetS Gaming power top-up, including dysglycemia, obesity especially central Nutritious energy drinkshigh blood pressure, low high-density lipoprotein syndfome HDL-Cand elevated triglyceride Metaboliic, is a complex of risk factors Weight management for young athletes type Best fat blocker diabetes and CVD 2.
Patients with MetS have a Nutritious energy drinks risk of developing CVD compared Arthritis natural remedies those without MetS in Nutritious energy drinks next 5—10 csrdiovascular, and the long-term risk is even cardiovascjlar 3.
The Disese Cholesterol Education Nutritious energy drinks NCEP Adult Treatment Panel Diseaase III criteria also considered MetS diseaes the second major target for Cardiovascu,ar prevention Metabolic syndrome cardiovascular disease.
The prevalence of MetS is higher in patients with CVD than in patients without Cardivoascular. Boulon et al. However, Selcuk et al.
But some researchers suggested that MetS does not increase the mortality among Fermented foods and inflammation with CVD 8. Therefore, controversy exists about the impact of MetS on Energy boosting foods with CVD.
MetS is a disease associated with multiple carsiovascular, and the main catdiovascular indicators components include blood dusease, overweight and obesity, HDL-C, and fasting blood glucose 9 Most cagdiovascular have focused on the cardlovascular effect of Diseae on the prognosis of CVD.
Pump-inducing pre-workout, whether a Metabllic exists between each component syndrime prognosis and which factor is diseasd important have not been elucidated.
Considering these inconsistencies, we performed a meta-analysis of cohort studies and RCT post-hoc analysis from CVD patients to evaluate associations Nutritious energy drinks Metabopic definitions of MetS and the risk diseae all cause death, Importance of calcium death and cardiovascular events.
The study was registered with PROSPERO CRDand reported Metabolic syndrome cardiovascular disease accordance with the PRISMA statement Cafdiovascular included Sports drinks for long rides and randomized controlled syndrone post hoc analyses and excluded idsease observational studies.
Secondary outcomes were TVR, heart failure, cardiac arrest, angina pectoris, cardiogenic shock. The definition of cardiovascular disease in this meta-analysis was history didease of cardiovascular or cardiac disease. We searched Pubmed, EMBASE, and Cochrane library from inception to October 18, Supplementary Table 1 presents the search strategy.
No Natural appetite suppressant, language, or other restriction were incorporated into the searches.
Two eisease XL and Synddome performed the czrdiovascular search. Endnote Djsease was used to manage and screen cardiovascukar literature. We designed a standardized form to extract data including idsease characteristics, diagnostic criteria, Antibacterial skin care products of the idsease population, risk of bias, and syhdrome measures.
We used the Newcastle—Ottawa Scale NOS to assess the quality of the cohort studies Cochrane Collaboration's tool for assessing the risk of bias was applied to determine the quality of the included RCT post-hoc studies 12 Two researchers X Li, YJ Zhai independently screened and extracted the data, and a third researcher J Lyu resolved any disagreements.
Quality evaluation results are reported in Supplementary Table 2. The diagnostic criteria for MetS vary among different regions and institutions, but the majority of them included central obesity, hypertension, low HDL-C, and high TG and fasting blood glucose FBG levels.
Other diagnostic criteria also included dyslipidemia, chronic mild inflammation, endothelial dysfunction, insulin resistance, increased oxidative stress.
The diagnostic criteria used in the included studies were NCEP criteria 9NCEP criteria 4and The International Diabetes Federation IDF criteria 10 details reported in Supplementary Table 3. For specific diagnostic criteria, we compared the above criteria and divide into subgroups based on the comparison results.
Statistical analysis was performed using STATA 13 and R software. The heterogeneity across studies was examined using the Chi-square test and I-square statistics. The results were pooled by the D-L random-effect model due to the large statistical heterogeneity among the studies.
Meta-regression analysis of three covariates follow-up time, male proportion, and patient age was performed to explore the size and source of heterogeneity. Effect measures [risk ratio RR vs. odds ratio OR vs. risk difference RD ] and statistical models D-L random-effects model vs. M-H fix-effects model were used to examine the robustness of the results.
We evaluated publication bias by Begg's tests and drew contour-enhanced funnel plots to assess whether the asymmetry of the funnel plots was caused by publication bias or other biases.
A total of 5, unique records were identified from the literature search. After excluding duplicate articles, studies were initially included by reading the title and abstract. Fifty-five studies were finally included after further reading the full text, including six RCT post-hoc studies 15 — 20 and 49 cohort studies 35 — 821 — 64 Figure 1.
A total ofpatients from 25 countries and regions were included, the sample size for each individual study varies from 57 to 44 Forty-one studiespatients evaluated the risk of all-cause death among patients with CVD and MetS.
Twenty-one studies with 95, patients reported CV death, 23 studies with 77, patients reported the incidence of MI, and 11 studies with 59, patients reported the incidence of stroke. Twenty-six studies adopted NCEP-ATPIII criteria, 21 studies mainly adopted NCEP-ATPIII criteria, and 7 studies adopted IDF Baseline characteristics are listed in Table 1.
Risk of bias was assessed in all of the 55 studies Supplementary Table 2. The cohort studies comprised 16 medium-quality studies, and 33 high-quality studies. For RCT post-hoc studies, the risk of bias was deemed low in 2 studies and moderate in 4 studies. Forty-one studiespatients reported all-cause death.
Subgroup analysis showed that among different diagnostic criteria of MetS, the results from NCEP-ATPIII and NCEP-ATPIII subgroups were consistent with the overall result Table 3. Among different study types, the cohort study subgroup was in the same direction with the overall results.
No statistically significant difference was found in the RCT post-hoc studies. Diagnostic criteria and study type were the factors that affected heterogeneity.
Figure 2. Meta-analysis of the risk of all-cause death in patients with CVD and MetS compared with that of patient without MetS. Twenty-one studies with 94, patients reported CV-related death. Subgroup analysis showed that among different diagnostic criteria of MetS, NCEP-ATPIII and NCEP-ATPIII subgroups were consistent with the overall result Table 3.
Among different study types, the subgroups were consistent with the overall results. Diagnostic criteria affected the heterogeneity. The Begg's test and the contour-enhanced funnel plots showed that bias may be caused by publication bias and other reasons.
Figure 3. Meta-analysis of the risk of CV death in patients with CVD and MetS compared with that of patient without MetS. Twenty-three studies with 77, patients reported the risk of MI.
Subgroup analysis showed that among the diagnostic criteria of MetS, the results of NCEP-ATPIII and NCEP-ATPIII were consistent with the overall results Table 3.
Other subgroups had no statistically significant difference. Among the study types, the subgroup results were in the same direction as the overall results.
Figure 4. Meta-analysis of the risk of MI in patients with CVD and MetS compared with that of patients without MetS. Eleven studies with 60, patients reported the risk of stroke. The Begg's test and the contour-enhanced funnel plots showed that the bias may be caused by other reasons rather than publication bias.
Figure 5. Meta-analysis of the risk of stroke in patients with CVD and MetS compared with that of patients without MetS. Subgroup analysis showed that diagnostic criteria and study type explained the partial heterogeneity.
The risk of heart failure was evaluated in eight studies. Subgroup analysis showed that diagnostic criteria partly explained the heterogeneity Table 2.
Other indicators include risk of cardiac arrest 4 studiesangina pectoris 3 studiesand cardiogenic shock 3 studies. We examined the robustness of our results. The sensitivity analysis of the effect measures showed that the OR increased the effect size and did not change the direction of the results, except for angina pectoris.
The RD did not change the direction of the results. The sensitivity analysis of the statistical models did not change the direction of the results. Hence, the results of this meta-analysis were robust. Fifty-five studies withpatients from 25 countries or regions were included. Most studies defined MetS using NCEP, NCEP, and IDF criteria, and other works adopted specific diagnostic criteria.
Our results suggested that patients with CVD and MetS had an increased risk of all-cause death, CV-related death, MI, stroke, TVR, and heart failure. Dyslipidemia and abnormal glucose metabolism were the main risk factors for the prognosis of CVD.
Different spectrum within patients with cardiovascular diseases may be the sources of heterogeneity. MetS and its components are a complex of risk factors for CVD and diabetes
: Metabolic syndrome cardiovascular disease| Metabolic syndrome - Better Health Channel | Perhaps more likely, the obesity-induced procoagulant and antifibrinolytic factors contribute to a worsening of acute coronary syndromes. Thrombosis occurring with plaque rupture or erosion is a key element in determining the severity of the syndrome. If normal coagulation and fibrinolysis are impaired at the time of plaque rupture or erosion, then a larger thrombus should form. An attractive hypothesis is that acute plaque disruption is common, but only when thrombosis is large is there a significant acute coronary syndrome. If so, such could make the presence of a prothrombotic state important for determining the clinical outcome. The cardiovascular field has recently shown great interest in the role of inflammation in the development of ASCVD. The basic concept is that atherogenesis represents a state of chronic inflammation. It is characterized by lipid-induced injury that initiates invasion of macrophages followed by proliferation of smooth muscle cells. All of these processes are classic features of chronic inflammation albeit occurring at a very slow rate. The finding that elevations of serum CRP carry predictive power for the development of major cardiovascular events led to the concept that advanced and unstable atherosclerotic plaques are in an even higher state of inflammation than stable plaques 9. It is of interest that obese persons 42 and particularly those with the metabolic syndrome 43 also have elevated levels of CRP. This finding has suggested that obesity is a proinflammatory state and is somehow connected with the development of unstable atherosclerotic plaques. So far, however, a mechanistic connection has not been made. The associations are suggestive, but how elevations of CRP associated with obesity could promote or precipitate major cardiovascular events is not clear. This lack of identified mechanism does not rule out a causative connection. But so far the connection has not been uncovered. Obesity is a major underlying risk factor for ASCVD. It is associated with multiple ASCVD risk factors, and it also is a risk factor for type 2 diabetes. Diabetes itself is a cardiovascular risk factor. Despite the strong association between obesity and ASCVD, the mechanisms underlying this relationship are not well understood. Our understanding of the connection between obesity and vascular disease is complicated by a plethora of possibilities. Obesity acts on so many metabolic pathways, producing so many potential risk factors, that it is virtually impossible to differentiate between the more important and less important. The possibilities for confounding variables are enormous. This complexity provides a great challenge for basic and clinical research. It also raises the possibility for new targets of therapy for the metabolic syndrome. With this said, the fundamental challenge is how to intervene at the public health level to reduce the high prevalence of obesity in the general population. This approach offers the greatest possibility for reducing the cardiovascular risk that accompanies obesity. Circulation : — Google Scholar. National Cholesterol Education Program NCEP Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Adult Treatment Panel III Third Report of the National Cholesterol Education Program NCEP Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Adult Treatment Panel III final report. Arterioscler Thromb Vasc Biol 24 : e13 — e National Institutes of Health. Obes Res 6 Suppl 2 S—S. Bosello O , Zamboni M Visceral obesity and metabolic syndrome. Obes Rev 1 : 47 — Abate N , Garg A , Peshock RM , Stray-Gundersen J , Grundy SM Relationships of generalized and regional adiposity to insulin sensitivity in men. J Clin Invest 96 : 88 — Abate N , Garg A , Peshock RM , Stray-Gundersen J , Adams-Huet B , Grundy SM Relationship of generalized and regional adiposity to insulin sensitivity in men with NIDDM. Diabetes 45 : — Unwin N , Shaw J , Zimmet P , Alberti KG Impaired glucose tolerance and impaired fasting glycaemia: the current status on definition and intervention. Diabet Med 19 : — Ridker PM High-sensitivity C-reactive protein and cardiovascular risk: rationale for screening and primary prevention. Am J Cardiol 92 : 17 K—22K. Einhorn D ACE position statement on insulin resistance syndrome. Endocr Pract 9 : — Ford ES , Giles WH , Dietz WH Prevalence of the metabolic syndrome among U. Findings from the Third National Health and Nutrition Survey. JAMA : — Guerre-Millo M Adipose tissue hormones. J Endocrinol Invest 25 : — Heptulla R , Smitten A , Teague B , Tamborlane WV , Ma YZ , Caprio S Temporal patterns of circulating leptin levels in lean and obese adolescents: relationships to insulin, growth hormone, and free fatty acids rhythmicity. J Clin Endocrinol Metab 86 : 90 — Randle PJ , Garland PB , Hales CN , Newesholme EA The glucose fatty-acid cycle. Its role in insulin sensitivity and the metabolic disturbances of diabetes mellitus. Lancet 1 : — Shulman GI Cellular mechanisms of insulin resistance. J Clin Invest : — Ruderman NB , Saha AK , Vavvas D , Witters LA Malonyl-CoA, fuel sensing, and insulin resistance. Am J Physiol 1 Pt 1 : E1 — E Grundy SM Metabolic complications of obesity. Endocrine 13 : — Engeli S , Sharma AM Role of adipose tissue for cardiovascular-renal regulation in health and disease. Horm Metab Res 32 : — Juhan-Vague I , Morange PE , Alessi MC The insulin resistance syndrome: implications for thrombosis and cardiovascular disease. Pathophysiol Haemost Thromb 32 : — Ridker PM , Morrow DA C-reactive protein, inflammation, and coronary risk. Cardiol Clin 21 : — Alessi MC , Peiretti F , Morange P , Henry M , Nalbone G , Juhan-Vague I Production of plasminogen activator inhibitor 1 by human adipose tissue: possible link between visceral fat accumulation and vascular disease. Diabetes 46 : — Ouchi N , Kihara S , Funahashi T , Matsuzawa Y , Walsh K Obesity, adiponectin and vascular inflammatory disease. Curr Opin Lipidol 14 : — Unger RH Lipotoxic diseases. Annu Rev Med 53 : — Steppan CM , Lazar MA Resistin and obesity-associated insulin resistance Trends. Endocrinol Metab 13 : 18 — Isomaa B , Almgren P , Tuomi T , Forsen B , Lahti K , Nissen M , Taskinen MR , Group L Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 24 : — Alexander CM , Landsman PB , Teutsch SM , Haffner SM Third National Health and Nutrition Examination Survey NHANES III ; National Cholesterol Education Program NCEP. NCEP-defined metabolic syndrome, diabetes, and prevalence of coronary heart disease among NHANES III participants age 50 years and older. Diabetes 52 : — Hunt K, Resendez R, Williams K, Haffner S, Stern M NCEP versus WHO metabolic syndrome in relation to all cause and cardiovascular mortality in the San Antonio Heart Study SAHS. Diabetes 52 i6 pA—A Abstract. Lakka HM , Laaksonen DE , Lakka TA , Niskanen LK , Kumpusalo E , Tuomilehto J , Salonen JT The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. Krauss RM Atherogenicity of triglyceride-rich lipoproteins. Am J Cardiol 81 : 13 B—17B. Krauss RM Dense low density lipoproteins and coronary artery disease. Am J Cardiol 75 : 53 B—57B. Blake GJ , Otvos JD , Rifai N , Ridker PM Low-density lipoprotein particle concentration and size as determined by nuclear magnetic resonance spectroscopy as predictors of cardiovascular disease in women. Grundy SM Low-density lipoprotein, non-high-density lipoprotein, and apolipoprotein B as targets of lipid-lowering therapy. Chobanian AV , Bakris GL , Black HR , Cushman WC , Green LA , Izzo Jr JL , Jones DW , Materson BJ , Oparil S , Wright Jr JT , Roccella EJ; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 42 : — Barrett-Connor E , Khaw KT Is hypertension more benign when associated with obesity? Circulation 72 : 53 — Carman WJ , Barrett-Connor E , Sowers M , Khaw KT Higher risk of cardiovascular mortality among lean hypertensive individuals in Tecumseh, Michigan. Circulation 89 : — Kannel WB , Zhang T , Garrison RJ Is obesity-related hypertension less of a cardiovascular risk? The Framingham Study. Am Heart J : — N Engl J Med : — Aronson D , Rayfield EJ How hyperglycemia promotes atherosclerosis: molecular mechanisms. Cardiovasc Diabetol 1 : 1. Haffner SM Cardiovascular risk factors and the prediabetic syndrome. Ann Med 28 : — De Pergola G , Pannacciulli N Coagulation and fibrinolysis abnormalities in obesity. Widlansky ME , Gokce N , Keaney Jr JF , Vita JA The clinical implications of endothelial dysfunction. J Am Coll Cardiol 42 : — Visser M , Bouter LM , McQuillan GM , Wener MH , Harris TB Elevated C-reactive protein levels in overweight and obese adults. Ridker PM Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide. Sign In or Create an Account. Endocrine Society Journals. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Categories of obesity. Body fat and metabolic syndrome. Inflammatory cytokines. Other adipose tissue products. Obesity-induced metabolic syndrome as a multidimensional risk factor for ASCVD and type 2 diabetes. Atherogenic dyslipidemia. Elevated blood pressure. Elevated plasma glucose. Prothrombotic state. Proinflammatory state. Journal Article. Obesity, Metabolic Syndrome, and Cardiovascular Disease. Grundy Scott M. Grundy, M. Oxford Academic. PDF Split View Views. Cite Cite Scott M. Select Format Select format. ris Mendeley, Papers, Zotero. enw EndNote. bibtex BibTex. txt Medlars, RefWorks Download citation. Permissions Icon Permissions. Categories of obesity Obesity can be defined as an excess of body fat. Body fat and metabolic syndrome The metabolic syndrome is a constellation of metabolic risk factors that consist of the following 2 : Atherogenic dyslipidemia [serum elevations of triglycerides, apolipoprotein B apo B , and small low-density lipoprotein LDL particles plus low high-density lipoprotein HDL cholesterol] Elevated blood pressure Elevated glucose associated with insulin resistance Prothrombotic state Proinflammatory state Many of these factors can be identified through special testing but are not measured in clinical practice. The following is a list of the factors most implicated in the development of metabolic syndrome 12 : Nonesterified fatty acids NEFAs Inflammatory cytokines PAI-1 Adiponectin Leptin Resistin Current concepts of the relation of each of these products to metabolic risk factors can be reviewed. Obesity-induced metabolic syndrome as a multidimensional risk factor for ASCVD and type 2 diabetes Several recent reports 25 — 28 indicate that the presence of the metabolic syndrome is associated with increased risk for both ASCVD and type 2 diabetes. Summary Obesity is a major underlying risk factor for ASCVD. Abbreviations: apo B,. atherosclerotic cardiovascular disease;. Google Scholar Crossref. Search ADS. Third Report of the National Cholesterol Education Program NCEP Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Adult Treatment Panel III final report. OpenURL Placeholder Text. Relationships of generalized and regional adiposity to insulin sensitivity in men. Relationship of generalized and regional adiposity to insulin sensitivity in men with NIDDM. Impaired glucose tolerance and impaired fasting glycaemia: the current status on definition and intervention. High-sensitivity C-reactive protein and cardiovascular risk: rationale for screening and primary prevention. Google Scholar PubMed. Prevalence of the metabolic syndrome among U. Temporal patterns of circulating leptin levels in lean and obese adolescents: relationships to insulin, growth hormone, and free fatty acids rhythmicity. The glucose fatty-acid cycle. Role of adipose tissue for cardiovascular-renal regulation in health and disease. The insulin resistance syndrome: implications for thrombosis and cardiovascular disease. Production of plasminogen activator inhibitor 1 by human adipose tissue: possible link between visceral fat accumulation and vascular disease. Google Scholar OpenURL Placeholder Text. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Third National Health and Nutrition Examination Survey NHANES III ; National Cholesterol Education Program NCEP. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. Low-density lipoprotein particle concentration and size as determined by nuclear magnetic resonance spectroscopy as predictors of cardiovascular disease in women. Low-density lipoprotein, non-high-density lipoprotein, and apolipoprotein B as targets of lipid-lowering therapy. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Higher risk of cardiovascular mortality among lean hypertensive individuals in Tecumseh, Michigan. Is obesity-related hypertension less of a cardiovascular risk? Intensive diabetes therapy and carotid intima-media thickness in type 1 diabetes mellitus. Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Issue Section:. Download all slides. Views 31, More metrics information. Total Views 31, Email alerts Article activity alert. Advance article alerts. New issue alert. Receive exclusive offers and updates from Oxford Academic. Citing articles via Web of Science Latest Most Read Most Cited Magnesium Depletion Score and Metabolic Syndrome in US Adults: Analysis of NHANES Clinical and Histopathological Risk Factors for Radioactive Iodine Refractory Follicular and Oncocytic Thyroid Carcinoma. Non-Operative, Active Surveillance of Larger Malignant and Suspicious Thyroid Nodules. Carotid Intima-Media Thickness in Surgically or Conservatively Managed Patients With Primary Hyperparathyroidism. Differential diagnosis of post pancreatitis diabetes mellitus based on pancreatic and gut hormone characteristics. More from Oxford Academic. Clinical Medicine. Endocrinology and Diabetes. Guallar-Castillón P, Pérez RF, López García E, León-Muñoz LM, Aguilera MT, Graciani A, et al. Magnitude and Management of Metabolic Syndrome in Spain in — The ENRICA Study [magnitud y manejo del síndrome metabólico en España en — Estudio ENRICA]. Rev Esp Cardiol. Richter-Stretton GL, Fenning AS, Vella RK. Skeletal muscle—a bystander or influencer of metabolic syndrome? Diabetes Metab Syndr Clin Res Rev. Tanaka M, Okada H, Hashimoto Y, Kumagai M, Nishimura H, Fukui M. Trunk muscle quality and quantity predict the development of metabolic syndrome and the increase in the number of its components in individuals without metabolic syndrome. Nutr Metab Cardiovasc Dis. Li G, Esangbedo IC, Xu L, Fu J, Li L, Feng D, et al. Childhood retinol-binding protein 4 RBP4 levels predicting the year risk of insulin resistance and metabolic syndrome: the BCAMS study. Cardiovasc Diabetol. Nanri A, Miyaji N, Kochi T, Eguchi M, Kabe I, Mizoue T. Eating speed and risk of metabolic syndrome among Japanese workers: the Furukawa Nutrition and Health Study. Kim G, Lee S-E, Jun JE, Lee Y-B, Ahn J, Bae JC, et al. Increase in relative skeletal muscle mass over time and its inverse association with metabolic syndrome development: a 7-year retrospective cohort study. Dun Y, Thomas RJ, Smith JR, Medina-Inojosa JR, Squires RW, Bonikowske AR, et al. High-intensity interval training improves metabolic syndrome and body composition in outpatient cardiac rehabilitation patients with myocardial infarction. Article PubMed PubMed Central CAS Google Scholar. McNeill AM, Rosamond WD, Girman CJ, Golden SH, Schmidt MI, East HE, et al. The metabolic syndrome and year risk of incident cardiovascular disease in the atherosclerosis risk in communities study. Diabetes Care. Kazlauskiene L, Butnoriene J, Norkus A. Metabolic syndrome related to cardiovascular events in a year prospective study. Diabetol Metab Syndr. Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: A summary of the evidence. Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, et al. Metabolic syndrome and risk of incident cardiovascular events and death. A systematic review and meta-analysis of longitudinal studies. Galassi A, Reynolds K, He J. Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am J Med. Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk: A systematic review and meta-analysis. van Herpt TTW, Dehghan A, Hoek M, Ikram MA, Hofman A, Sijbrands EJGG, et al. The clinical value of metabolic syndrome and risks of cardiometabolic events and mortality in the elderly: the Rotterdam study. Ju SY, Lee JY, Kim DH. Association of metabolic syndrome and its components with all-cause and cardiovascular mortality in the elderly. Medicine Baltimore. Inchiostro S, Fadini GP, de Kreutzenberg SV, Citroni N, Avogaro A. Is the metabolic syndrome a cardiovascular risk factor beyond its specific components? Martínez-González MA, Gea A, Ruiz-Canela M. The mediterranean diet and cardiovascular health. Circ Res. Article PubMed CAS Google Scholar. Viñes JJ, Díez J, Guembe MJ, González P, Amézqueta C, Barba J, et al. Estudio de Riesgo Vascular en Navarra: Objetivos y Diseño. Prevalencia del Síndrome Metabólico y de los Factores Mayores de Riesgo Vascular [Study of Vascular Risk in Navarre: Objectives and Design. Prevalence of Metabolic Syndrome and of Vascular Risk Factors]. An Sist Sanit Navar. PubMed Google Scholar. WONCA International Classification Committee. International Classification of Primary Care. Second Edition. Barcelona: Masson; Sayon-Orea C, Moreno-Iribas C, Delfrade J, Sanchez-Echenique M, Amiano P, Ardanaz E, et al. Inverse-probability weighting and multiple imputation for evaluating selection bias in the estimation of childhood obesity prevalence using data from electronic health records. BMC Med Inform Decis Mak. Moreno-Iribas C, Sayon-Orea C, Delfrade J, Ardanaz E, Gorricho J, Burgui R, et al. Validity of type 2 diabetes diagnosis in a population-based electronic health record database. Ministry of Health, Social Services and Equality. es Accessed 29 May Lohman GT, Roche AF, Martorell R. Anthropometric standardization reference manual. Champaign, IL: Human Kinetics Books; Google Scholar. Schröder H, Fitó M, Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, et al. A short screener is valid for assessing mediterranean diet adherence among older spanish men and women. J Nutr. Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Ruiz-Gutiérrez V, Covas MI, et al. Effects of a mediterranean-style diet on cardiovascular risk factors a randomized trial. Ann Intern Med. Elosua R, Marrugat J, Molina L, Pons S, Pujol E. Validation of the minnesota leisure time physical activity questionnaire in Spanish men. Am J Epidemiol. Elosua R, Garcia M, Aguilar A, Molina L, Covas MIM, Marrugat J. Validation of the minnesota leisure time physical activity questionnaire in Spanish women. Med Sci Sport Exerc. Article CAS Google Scholar. Ainsworth BE, Haskell W, Leon A, David DR. Jacobs J, Montoye H, Sallis JF, et al. Compendium of physical activities: classification of energy costs of human physical activities. Brenner H, Gefeller O, Greenland S. Risk and rate advancement periods as measures of exposure impact on the occurrence of chronic diseases. Liese AD, Hense H-W, Brenner H, Löwel H, Keil U. Assessing the impact of classical risk factors on myocardial infarction by rate advancement periods. Royston P, Lambert PC. Flexible parametric survival analysis using stata: beyond the cox model. College Station, TX: Stata Press; Discacciati A, Andrea B, Nicola O, Sander G. On the interpretation of risk and rate advancement periods. Int J Epidemiol. Martínez-Larrad MT, Fernández-Pérez C, Corbatón-Anchuelo A, Gabriel R, Lorenzo C, Serrano-Ríos M. Revised waist circumference cut-off points for the criteria of abdominal obesity in the Spanish population: Multicenter nationwide Spanish population based study. Av en Diabetol. Sattar N, McConnachie A, Shaper AG, Blauw GJ, Buckley BM, de Craen AJ, et al. Can metabolic syndrome usefully predict cardiovascular disease and diabetes? Outcome data from two prospective studies. Bruno G, Merletti F, Biggeri A, Bargero G, Ferrero S, Runzo C, et al. Metabolic syndrome as a predictor of all-cause and cardiovascular mortality in type 2 diabetes The Casale Monferrato Study. Lawlor DA, Smith GD, Ebrahim S. Does the new International Diabetes Federation definition of the metabolic syndrome predict CHD any more strongly than older definitions? Klein BEK, Klein R, Lee KE. Components of the metabolic syndrome and risk of cardiovascular disease and diabetes in Beaver Dam. Isomaa BO, Almgren P, Tuomi T, Bjo¨ B, Forsén B, Lahti K, et al. Cardiovascular Morbidity and Mortality Associated With the Metabolic Syndrome. Tenenbaum A, Fisman EZ. Younis A, Younis A, Tzur B, Peled Y, Shlomo N, Goldenberg I, et al. Metabolic syndrome is independently associated with increased year mortality in patients with stable coronary artery disease. Guembe MJ, Toledo E, Barba J, Martínez-Vila E, González-Diego P, Irimia P, et al. Association between metabolic syndrome or its components and asymptomatic cardiovascular disease in the RIVANA-study. Calabuig Á, Barba J, Guembe MJ, Díez J, Berjón J, Martínez-Vila E, et al. Epicardial adipose tissue in the general middle-aged population and its association with metabolic syndrome. Rev Española Cardiol English Ed. Fresán U, Angel Martínez-González M, Sabaté J, Bes-Rastrollo M. Global sustainability health, environment and monetary costs of three dietary patterns: results from a Spanish cohort the SUN project. BMJ Open. Ruiz-Estigarribia L, Martínez-González M, Díaz-Gutiérrez J, Gea A, Rico-Campà A, Bes-Rastrollo M. Lifestyle-related factors and total mortality in a mediterranean prospective cohort. Am J Prev Med. Gellert C, Schöttker B, Holleczek B, Stegmaier C, Müller H, Brenner H. Using rate advancement periods for communicating the benefits of quitting smoking to older smokers. Tob Control. Download references. We want to thank all the nurses that participated in the study and the members of the hospital laboratory of the Hospital Complex of Navarre for their generosity and cooperation with the project. Many thanks to Navarrabiomed Biobank and Miguel Servet Foundation for their continuous support. Special thanks to José Javier Viñes Rueda for his support and hard work that contributed greatly to the RIVANA study. Dirección General de Salud del Gobierno de Navarra, Servicio de Planificación, Evaluación y Gestión del Conocimiento: Joaquín Barba Cosials, Jesús Berjón Reyero, Javier Díez Martínez, Paulino González Diego, Ana Mª Grijalba Uche, David Guerrero Setas, Eduardo Martínez Vila, Manuel Serrano Martínez, Isabel Sobejano Tornos, José Javier Viñes Rueda. Department of Health, Government of Navarre, Vascular Risk in Navarre Investigation Group, Pamplona, Spain. María J. Guembe, Cesar I. Dirección General de Salud del Gobierno de Navarra, Servicio de Planificación, Evaluación Y Gestión del Conocimiento, Pamplona, Spain. Cesar I. IdiSNA, Navarra Institute for Health Research, Pamplona, Spain. Navarrabiomed-Miguel Servet Foundation, Pamplona, Spain. Instituto de Salud Pública y Laboral de Navarra, Pamplona, Spain. Centro de Investigación Biomédica en Red Área de Fisiología de la Obesidad y la Nutrición CIBEROBN , Madrid, Spain. Health Services Research on Chronic Patients Network REDISSEC , Instituto de Salud Carlos III, Madrid, Spain. You can also search for this author in PubMed Google Scholar. MJG, CIF-L, CS-O, and ET were involved with study conception and design; CIF-L performed the data analysis and interpretation; MJF, CS-O, and ET assisted in data interpretation; CIF-L drafted the manuscript; MJG, CS-O, ET, and CM-I provided critical edits to the manuscript. MJG was involved in the direction and coordination of the RIVANA Project. All authors have revised the manuscript for important intellectual content. All authors read and approved the final manuscript. Correspondence to Cesar I. The study protocol was approved by the Institutional Review Board of the Government of Navarre. All participants provided written informed consent to participate in the study before data collection and access to their medical records. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Diagnostic criteria for endpoints of the study. Appendix S2. Percentages of imputed information for imputed variables. Appendix S3. Appendix S4. Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. Reprints and permissions. Guembe, M. et al. Risk for cardiovascular disease associated with metabolic syndrome and its components: a year prospective study in the RIVANA cohort. Cardiovasc Diabetol 19 , Download citation. Received : 29 July Accepted : 31 October Published : 22 November Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Download ePub. Original investigation Open access Published: 22 November Risk for cardiovascular disease associated with metabolic syndrome and its components: a year prospective study in the RIVANA cohort María J. Guembe 1 , 2 na1 , Cesar I. Fernandez-Lazaro ORCID: orcid. Abstract Background We aimed to investigate the association of metabolic syndrome MetS and its single components with cardiovascular risk and estimated their impact on the prematurity of occurrence of cardiovascular events using rate advancement periods RAPs. Results During a median follow-up of Conclusions MetS was independently associated with CVD risk, cardiovascular and all-cause mortality. Background Cardiovascular disease CVD is the most common cause of death globally and a significant contributor to morbidity, accounting for Methods Study population The present study included data on participants in the RIVANA Study, a Mediterranean cohort with up to Study outcomes The primary endpoint of the study was a composite of myocardial infarction, stroke, and mortality from cardiovascular causes. Statistical analysis The baseline characteristics of participants were described according to the presence or absence of MetS. Full size image. Table 4 Sensitivity analyses. Discussion We aimed to prospectively investigate the prevalence and risk estimates of MetS and its components with major cardiovascular events in a Mediterranean cohort of around 4, middle-aged adult participants with Metabolic syndrome MetS We found a significant association between MetS and major CVD incidence. Rate advancement periods RAPs We additionally calculated estimates of RAPs of endpoint events to illustrate the impact of MetS and its components. Limitations and strengths We acknowledge that our study has some limitations. Conclusions MetS was found to be independently associated after adjusting for multiple potential confounders with the incidence of CVD, mortality from CVD, and all-cause mortality, but not with myocardial infarction or stroke. References Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, et al. Article Google Scholar Kyu HH, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Article Google Scholar Wilkins E, Wilson L, Wickramasinghe K, Bhatnagar P, Leal J, Luengo-Fernandez R, et al. Article CAS PubMed Google Scholar Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Article CAS PubMed Google Scholar Expert Panel on Detection, Evaluation and T of HBC in A. Article PubMed Google Scholar World Health Organization: Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications. Article PubMed Google Scholar Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Article CAS PubMed PubMed Central Google Scholar Beltrán-Sánchez H, Harhay MO, Harhay MM, McElligott S. Article PubMed PubMed Central Google Scholar Guallar-Castillón P, Pérez RF, López García E, León-Muñoz LM, Aguilera MT, Graciani A, et al. Article PubMed Google Scholar Richter-Stretton GL, Fenning AS, Vella RK. Article Google Scholar Tanaka M, Okada H, Hashimoto Y, Kumagai M, Nishimura H, Fukui M. Article PubMed Google Scholar Li G, Esangbedo IC, Xu L, Fu J, Li L, Feng D, et al. Article CAS PubMed PubMed Central Google Scholar Nanri A, Miyaji N, Kochi T, Eguchi M, Kabe I, Mizoue T. Article PubMed Google Scholar Kim G, Lee S-E, Jun JE, Lee Y-B, Ahn J, Bae JC, et al. Article CAS PubMed PubMed Central Google Scholar Dun Y, Thomas RJ, Smith JR, Medina-Inojosa JR, Squires RW, Bonikowske AR, et al. Article PubMed PubMed Central CAS Google Scholar McNeill AM, Rosamond WD, Girman CJ, Golden SH, Schmidt MI, East HE, et al. Article PubMed Google Scholar Kazlauskiene L, Butnoriene J, Norkus A. Article PubMed PubMed Central CAS Google Scholar Ford ES. Article PubMed Google Scholar Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, et al. Article CAS PubMed Google Scholar Galassi A, Reynolds K, He J. Article CAS PubMed Google Scholar Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. Article PubMed Google Scholar van Herpt TTW, Dehghan A, Hoek M, Ikram MA, Hofman A, Sijbrands EJGG, et al. Article PubMed PubMed Central CAS Google Scholar Ju SY, Lee JY, Kim DH. Article Google Scholar Inchiostro S, Fadini GP, de Kreutzenberg SV, Citroni N, Avogaro A. Article PubMed Google Scholar Martínez-González MA, Gea A, Ruiz-Canela M. |
| What is Metabolic Syndrome? | American Heart Association | Copy to clipboard. Among the study types, the subgroup results were in the same direction as the overall results. Hillsdale, NJ: Lawrence Erlbaum Associates; This database was designed to account for diverse episodes and health conditions, and was coded according to the International Classification of Primary Care, Second Edition ICPC-2 [ 30 ]. Meta-analysis of the risk of MI in patients with CVD and MetS compared with that of patients without MetS. |
| What is Metabolic Syndrome? | It is commonly present in obese persons. The increased number of VLDL and LDL particles accounts for the increased level of total apo B usually observed with atherogenic dyslipidemia. The atherogenic potential of each lipoprotein abnormality has long been a topic of great interest but one that is not fully resolved. For many years triglyceride-rich lipoproteins TGRLPs were thought not to be atherogenic. Nonetheless, there is growing evidence that smaller TGRLP remnant lipoproteins are in fact atherogenic This evidence comes from studies in laboratory animals, patients with genetic disorders causing remnant accumulation, metaanalysis of epidemiological studies, and clinical trials 1. TGRLPs as a class are a mixture of lipoproteins, and it has been difficult to differentiate between atherogenic and nonatherogenic forms of TGRLPs. Nonetheless, there is a growing consensus among investigators that TGRLP fraction definitely contains atherogenic lipoproteins. The LDL particles associated with the metabolic syndrome and atherogenic dyslipidemia tend to be small and dense. A theory widely held is that smaller LDL particles are more atherogenic than larger LDLs Smaller LDLs may filter more readily into the arterial wall. They further may be more prone to atherogenic modification. Even so, not all investigations are convinced that small LDL particles are unusually atherogenic, compared with other apo B-containing lipoproteins. Nonetheless, when small LDLs are present, the total number of lipoprotein particles in the LDL fraction usually is increased Most researchers will agree that the higher the number of LDL particles present, the higher will be the atherogenic potential. In other words, small LDL particles are often a surrogate for an increased LDL particle number These measurements should be used increasingly both in risk assessment and as targets of therapy in persons with the metabolic syndrome A low HDL level is another characteristic of atherogenic dyslipidemia 2. This fact has led to the concept that HDL is intimately involved in the atherogenic process. The theories abound as to the mechanisms whereby HDL is antiatherogenic, e. enhanced reverse cholesterol transport, antiinflammatory properties, ability to protect against LDL modification, among others. Although HDL in fact may be directly antiatherogenic, it also is a marker for the presence of other lipid and nonlipid risk factors. Obesity itself reduces HDL levels 4 , and obese patients with metabolic syndrome and atherogenic dyslipidemia almost always have low HDL levels. Thus, the association between low HDL and ASCVD risk is complex 2 , and the various components of this association are difficult to differentiate. Regardless of mechanism, however, the presence of a low HDL level carries strong predictive power for development of ASCVD. Obese persons have a higher prevalence of elevated blood pressure than lean persons. Moreover, a higher blood pressure is a strong risk factor for cardiovascular disease CVD Well-known complication of hypertension are CHD, stroke, left ventricular hypertrophy, heart failure, and chronic renal failure. Yet some reports 34 , 35 suggest that the elevated blood pressure accompanying obesity is less likely to produce CVD than when it occurs in lean persons. The implication is that obesity-induced hypertension is not particularly dangerous to the cardiovascular system. This concept generally is not accepted by the hypertension community, nor was it supported by the Framingham Heart Study There is no question that persons with diabetes are at increased risk for ASCVD. In epidemiological studies, the onset of diabetes is accompanied by increased risk for ASCVD, suggesting that hyperglycemia per se is atherogenic. Limited data that directly address the question of whether hyperglycemia accelerates the development of atherosclerosis are available. Nonetheless, one recent study 37 indicated that intensive diabetes therapy in type 1 diabetes is accompanied by a reduction in intima-media thickness of carotid arteries. Although this finding is consistent with epidemiology, it generally has not been possible to demonstrate an atherogenic potential of hyperglycemia in animal models. Moreover, whether the hyperglycemia of type 1 diabetes promotes atherogenesis has been uncertain. The major cause of death in persons with type 1 diabetes is CVD; even so, it is possible that most atherosclerotic disease develops later in the course of the disease after development of chronic renal failure and hypertension. A variety of mechanisms have been proposed whereby hyperglycemia might promote atherosclerosis Examples include nonenzymatic glycosylation of lipids and proteins, pathogenic effects of advanced glycation products, increased oxidative stress, activation of protein kinase C, and microvascular disease of the vasa vasorum of the coronary arteries. All of these potential mechanisms are of interest, but so far, none has been shown to play a direct role in atherogenesis; most likely all are involved in one way or another. But a fundamental question remains to be answered, namely whether hyperglycemia is directly atherogenic. Another possibility is that insulin resistance per se is independently atherogenic. In prospective studies, the presence of insulin resistance is associated with increased ASCVD risk But in persons with insulin resistance, confounding by other known risk factors makes it difficult to be certain that insulin resistance or resulting hyperinsulinemia is directly atherogenic If so, the mechanisms for such an effect are entirely speculative at this time. Obesity is accompanied by a large number of coagulation and fibrinolytic abnormalities This suggests that obesity induces a prothrombotic state. What is not known at present is how a prothrombotic state will either promote the development of atherosclerosis or participate in the development of acute ASCVD events. Perhaps the most attractive candidate for enhanced atherogenicity associated with coagulation and fibrinolytic abnormalities is endothelial dysfunction. It is believed by many workers that endothelial dysfunction is somehow involved in the atherogenic process Several pathways have been proposed; so far, however, none of these have been substantiated. Perhaps more likely, the obesity-induced procoagulant and antifibrinolytic factors contribute to a worsening of acute coronary syndromes. Thrombosis occurring with plaque rupture or erosion is a key element in determining the severity of the syndrome. If normal coagulation and fibrinolysis are impaired at the time of plaque rupture or erosion, then a larger thrombus should form. An attractive hypothesis is that acute plaque disruption is common, but only when thrombosis is large is there a significant acute coronary syndrome. If so, such could make the presence of a prothrombotic state important for determining the clinical outcome. The cardiovascular field has recently shown great interest in the role of inflammation in the development of ASCVD. The basic concept is that atherogenesis represents a state of chronic inflammation. It is characterized by lipid-induced injury that initiates invasion of macrophages followed by proliferation of smooth muscle cells. All of these processes are classic features of chronic inflammation albeit occurring at a very slow rate. The finding that elevations of serum CRP carry predictive power for the development of major cardiovascular events led to the concept that advanced and unstable atherosclerotic plaques are in an even higher state of inflammation than stable plaques 9. It is of interest that obese persons 42 and particularly those with the metabolic syndrome 43 also have elevated levels of CRP. This finding has suggested that obesity is a proinflammatory state and is somehow connected with the development of unstable atherosclerotic plaques. So far, however, a mechanistic connection has not been made. The associations are suggestive, but how elevations of CRP associated with obesity could promote or precipitate major cardiovascular events is not clear. This lack of identified mechanism does not rule out a causative connection. But so far the connection has not been uncovered. Obesity is a major underlying risk factor for ASCVD. It is associated with multiple ASCVD risk factors, and it also is a risk factor for type 2 diabetes. Diabetes itself is a cardiovascular risk factor. Despite the strong association between obesity and ASCVD, the mechanisms underlying this relationship are not well understood. Our understanding of the connection between obesity and vascular disease is complicated by a plethora of possibilities. Obesity acts on so many metabolic pathways, producing so many potential risk factors, that it is virtually impossible to differentiate between the more important and less important. The possibilities for confounding variables are enormous. This complexity provides a great challenge for basic and clinical research. It also raises the possibility for new targets of therapy for the metabolic syndrome. With this said, the fundamental challenge is how to intervene at the public health level to reduce the high prevalence of obesity in the general population. This approach offers the greatest possibility for reducing the cardiovascular risk that accompanies obesity. Circulation : — Google Scholar. National Cholesterol Education Program NCEP Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Adult Treatment Panel III Third Report of the National Cholesterol Education Program NCEP Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Adult Treatment Panel III final report. Arterioscler Thromb Vasc Biol 24 : e13 — e National Institutes of Health. Obes Res 6 Suppl 2 S—S. Bosello O , Zamboni M Visceral obesity and metabolic syndrome. Obes Rev 1 : 47 — Abate N , Garg A , Peshock RM , Stray-Gundersen J , Grundy SM Relationships of generalized and regional adiposity to insulin sensitivity in men. J Clin Invest 96 : 88 — Abate N , Garg A , Peshock RM , Stray-Gundersen J , Adams-Huet B , Grundy SM Relationship of generalized and regional adiposity to insulin sensitivity in men with NIDDM. Diabetes 45 : — Unwin N , Shaw J , Zimmet P , Alberti KG Impaired glucose tolerance and impaired fasting glycaemia: the current status on definition and intervention. Diabet Med 19 : — Ridker PM High-sensitivity C-reactive protein and cardiovascular risk: rationale for screening and primary prevention. Am J Cardiol 92 : 17 K—22K. Einhorn D ACE position statement on insulin resistance syndrome. Endocr Pract 9 : — Ford ES , Giles WH , Dietz WH Prevalence of the metabolic syndrome among U. Findings from the Third National Health and Nutrition Survey. JAMA : — Guerre-Millo M Adipose tissue hormones. J Endocrinol Invest 25 : — Heptulla R , Smitten A , Teague B , Tamborlane WV , Ma YZ , Caprio S Temporal patterns of circulating leptin levels in lean and obese adolescents: relationships to insulin, growth hormone, and free fatty acids rhythmicity. J Clin Endocrinol Metab 86 : 90 — Randle PJ , Garland PB , Hales CN , Newesholme EA The glucose fatty-acid cycle. Its role in insulin sensitivity and the metabolic disturbances of diabetes mellitus. Lancet 1 : — Shulman GI Cellular mechanisms of insulin resistance. J Clin Invest : — Ruderman NB , Saha AK , Vavvas D , Witters LA Malonyl-CoA, fuel sensing, and insulin resistance. Am J Physiol 1 Pt 1 : E1 — E Grundy SM Metabolic complications of obesity. Endocrine 13 : — Engeli S , Sharma AM Role of adipose tissue for cardiovascular-renal regulation in health and disease. Horm Metab Res 32 : — Juhan-Vague I , Morange PE , Alessi MC The insulin resistance syndrome: implications for thrombosis and cardiovascular disease. Pathophysiol Haemost Thromb 32 : — Ridker PM , Morrow DA C-reactive protein, inflammation, and coronary risk. Cardiol Clin 21 : — Alessi MC , Peiretti F , Morange P , Henry M , Nalbone G , Juhan-Vague I Production of plasminogen activator inhibitor 1 by human adipose tissue: possible link between visceral fat accumulation and vascular disease. Diabetes 46 : — Ouchi N , Kihara S , Funahashi T , Matsuzawa Y , Walsh K Obesity, adiponectin and vascular inflammatory disease. Curr Opin Lipidol 14 : — Unger RH Lipotoxic diseases. Annu Rev Med 53 : — Steppan CM , Lazar MA Resistin and obesity-associated insulin resistance Trends. Endocrinol Metab 13 : 18 — Metabolic syndrome syndrome X; insulin resistance syndrome. Merck Manual Professional Version. March 2, About metabolic syndrome. American Heart Association. Meigs JB. Metabolic syndrome insulin resistance syndrome or syndrome X. Prevention and treatment of metabolic syndrome. Lear SA, et al. Ethnicity and metabolic syndrome: Implications for assessment, management and prevention. News from Mayo Clinic. Mayo Clinic Q and A: Metabolic syndrome and lifestyle changes. More Information. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests. News Network. Price Transparency. Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. International Business Collaborations. Supplier Information. Admissions Requirements. World Health Organization. Global Status Report on Noncommunicable Diseases Google Scholar. Alberti KG, Eckel RH, rundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; american heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. doi: PubMed Abstract CrossRef Full Text Google Scholar. Suwaidi JA, Zubaid M, El-Menyar AA, Singh R, Rashed W, Ridha M, et al. Prevalence of the metabolic syndrome in patients with acute coronary syndrome in six middle eastern countries. J Clin Hypertens. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. CrossRef Full Text Google Scholar. Zeller M, Steg PG, Ravisy J, Laurent Y, Janin-Manificat L, L'Huillier I, et al. Prevalence and impact of metabolic syndrome on hospital outcomes in acute myocardial infarction. Arch Intern Med. Boulon C, Lafitte M, Richeboeuf V, Paviot B, Pradeau V, Coste P, et al. Prevalence of metabolic syndrome after acute coronary syndrome and its prognostic significance. Am J Cardiol. Selcuk H, Temizhan A, Selcuk MT, Sen T, Maden O, Tekeli S, et al. Impact of metabolic syndrome on future cardiovascular events in patients with first acute myocardial infarction. Coron Artery Dis. van Kuijk JP, Flu WJ, Chonchol M, Bax JJ, JM Verhagen H, Poldermans D. Metabolic syndrome is an independent predictor of cardiovascular events in high-risk patients with occlusive and aneurysmatic peripheral arterial disease. Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the national cholesterol education program NCEP expert panel on detection, evaluation, and treatment of high blood cholesterol in adults Adult Treatment Panel III. Alberti KG, Zimmet P, Shaw J. IDF epidemiology task force consensus group. The metabolic syndrome—a new worldwide definition. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ma LL, Wang YY, Yang ZH, Huang D, Weng H, Zeng XT. Methodological quality risk of bias assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res. Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale NOS For Assessing the Quality of Nonrandomised Studies in Meta-Analyses [online]. asp accessed December 21, Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions version 6. Available online at: www. Aguilar D, Fisher MR, O'Connor CM, Dunne MW, Muhlestein JB, Yao L, et al. Metabolic syndrome, C-reactive protein, and prognosis in patients with established coronary artery disease. Am Heart J. Schwartz GG, Olsson AG, Szarek M, Sasiela WJ. Relation of characteristics of metabolic syndrome to short-term prognosis and effects of intensive statin therapy after acute coronary syndrome: an analysis of the myocardial ischemia reduction with aggressive cholesterol lowering MIRACL trial. Diabetes Care. Mehta RH, Westerhout CM, Zheng Y, Giugliano RP, Huber K, Prabhakaran D, et al. Association of metabolic syndrome and its individual components with outcomes among patients with high-risk non-ST-segment elevation acute coronary syndromes. Perrone-Filardi P, Savarese G, Scarano M, Cavazzina R, Trimarco B, Minneci S, et al. Prognostic impact of metabolic syndrome in patients with chronic heart failure: data from GISSI-HF trial. Int J Cardiol. Maron DJ, Boden WE, Spertus JA, Hartigan PM, Mancini GBJ, Sedlis SP, et al. Impact of metabolic syndrome and diabetes on prognosis and outcomes with early percutaneous coronary intervention in the COURAGE clinical outcomes utilizing revascularization and aggressive drug evaluation trial. J Am Coll Cardiol. Ovbiagele B, Saver JL, Lynn MJ, Chimowitz M, WASID Study Group. Impact of metabolic syndrome on prognosis of symptomatic intracranial atherostenosis. Anderson JL, Horne BD, Jones HU, Reyna SP, Carlquist JF, Bair TL, et al. Which features of the metabolic syndrome predict the prevalence and clinical outcomes of angiographic coronary artery disease? Mornar JM, Babić Z, Pintarić H. The role of metabolic syndrome in patients with acute myocardial infarction. Diabetol Croatica. PubMed Abstract Google Scholar. Arnold SV, Lipska KJ, Li Y, Goyal A, Maddox TM, McGuire DK, et al. The reliability and prognosis of in-hospital diagnosis of metabolic syndrome in the setting of acute myocardial infarction. Kasai T, Miyauchi K, Kajimoto K, Kubota N, Yanagisawa N, Amano A, et al. Relationship between the metabolic syndrome and the incidence of stroke after complete coronary revascularization over a year follow-up period. Arbel Y, Havakuk O, Halkin A, Revivo M, Berliner S, Herz I, et al. Relation of metabolic syndrome with long-term mortality in acute and stable coronary disease. Kasai T, Miyauchi K, Kurata T, Ohta H, Okazaki S, Miyazaki T, et al. Prognostic value of the metabolic syndrome for long-term outcomes in patients undergoing percutaneous coronary intervention. Circ J. Tadaki S, Sakata Y, Miura Y, Miyata S, Asakura M, Shimada K, et al. Prognostic impacts of metabolic syndrome in patients with chronic heart failure - a multicenter prospective cohort study. La Carrubba D, Antonini-Canterin F, Fabiani I, Colonna P, Pugliese NR, Caso P, et al. Prevalence and prognostic impact of metabolic syndrome in asymptomatic stage A and B heart failure patients. Metab Syndr Relat Disord. Lovic MB, Savic L, Matic D, Djordjevic D, Nedeljkovic I, Tasic I. Predictive value of metabolic syndrome definitions in patients with myocardial infarction with ST segment elevation - are they all the same? Acta Cardiol. Marso SP, Mercado N, Maehara A, Weisz G, Mintz GS, McPherson J, et al. Plaque composition and clinical outcomes in acute coronary syndrome patients with metabolic syndrome or diabetes. JACC Cardiovasc Imaging. Hossain MS, Azad KA, Biswas PK, Hossain MA, Ahmed SU. Outcome of patients hospitalized with acute coronary syndrome fulfilling the criteria of metabolic syndrome. Bang Soc Med. Miller AM, Ruiz AA, Sánchez GB, Gutiérrez EA, Guzmán RM, Aguilar RJ. Metabolic syndrome: clinical and angiographic impact on patients with acute coronary syndrome. Cir Cir. Protack CD, Bakken AM, Xu J, Saad WA, Lumsden AB, Davies MG. Metabolic syndrome: a predictor of adverse outcomes after carotid revascularization. J Vasc Surg. Fang X, Liu H, Zhang X, Zhang H, Qin X, Ji X. Metabolic syndrome, its components, and diabetes on 5-year risk of recurrent stroke among mild-to-moderate ischemic stroke survivors: a multiclinic registry study. J Stroke Cerebrovasc Dis. Saely CH, Aczel S, Marte T, Langer P, Hoefle G, Drexel H. The metabolic syndrome, insulin resistance, and cardiovascular risk in diabetic and nondiabetic patients. J Clin Endocrinol Metab. Udell JA, Steg PG, Scirica BM, Eagle KA, Ohman EM, Goto S, et al. Metabolic syndrome, diabetes mellitus, or both and cardiovascular risk in outpatients with or at risk for atherothrombosis. Eur J Prev Cardiol. Vest AR, Young JB, Cho L. The metabolic syndrome, cardiovascular fitness and survival in patients with advanced systolic heart failure. Am J Cardio. Briand M, Lemieux I, Dumesnil JG, Mathieu P, Cartier A, Després JP, et al. Metabolic syndrome negatively influences disease progression and prognosis in aortic stenosis. Marroquin OC, Kip KE, Kelley DE, Johnson BD, Shaw LJ, Merz CNB, et al. Metabolic syndrome modifies the cardiovascular risk associated with angiographic coronary artery disease in women: a report from the women's ischemia syndrome evaluation. Petersen JL, Yow E, AlJaroudi W, Goyal A, McGuire DK, Peterson ED, et al. Metabolic syndrome is not associated with increased mortality or cardiovascular risk in nondiabetic patients with a new diagnosis of coronary artery disease. Circ Cardiovasc Qual Outcomes. Simão AN, Lehmann MF, Alfieri DF, Meloni MZ, Flauzino T, Scavuzzi BM, et al. Metabolic syndrome increases oxidative stress but does not influence disability and short-time outcome in acute ischemic stroke patients. Metab Brain Dis. Canibus P, Faloia E, Piva T, Muçai A, Serenelli M, Perna GP, et al. Metabolic syndrome does not increase angiographic restenosis rates after drug-eluting stent implantation. Won KB, Kim BK, Chang HJ, Shin DH, Kim JS, Ko YG, et al. Metabolic syndrome does not impact long-term survival in patients with acute myocardial infarction after successful percutaneous coronary intervention with drug-eluting stents. Catheter Cardiovasc Interv. Rana JS, Monraats PS, Zwinderman AH, de Maat MPM, Kastelein JJP, Doevendans PAF, et al. Metabolic syndrome and risk of restenosis in patients undergoing percutaneous coronary intervention. Chen Q, Zhang Y, Ding D, Li D, Xia M, Li X, et al. Metabolic syndrome and its individual components with mortality among patients with coronary heart disease. Nigam A, Bourassa MG, Fortier A, Guertin MC, Tardif JC. The metabolic syndrome and its components and the long-term risk of death in patients with coronary heart disease. Balti EV, Kengne AP, Fokou JV, Nouthé BE, Sobngwi E. Metabolic syndrome and fatal outcomes in the post-stroke event: a 5-year cohort study in Cameroon. |
| Metabolic syndrome | Nutritious energy drinks syndfome permissions Open Access Cardiovzscular article is syndroke under a Cardiovascklar Commons Attribution 4. This Injury prevention exercises may produce misleading messages cardiovsacular the concept Metabolic syndrome cardiovascular disease MetS is only used to cardiovacular patients at diseasse risk, as we demonstrated Essential macronutrients without MetS may also stay at high risk of developing cardiovascular events. After taking into account the conventional cardiovascular risk factors, LDL cholesterol, smoking, and family history of CHD in addition to examination year model 2the relative risks RRs of the metabolic syndrome for CHD mortality increased to 2. Compendium of physical activities: classification of energy costs of human physical activities. Relationship of generalized and regional adiposity to insulin sensitivity in men with NIDDM. Ford, E. RAP represents the baseline age difference at which exposed subjects participants with MetS reach the same risk of disease endpoint events as unexposed subjects non-MetS participants. |
Es ist schade, dass ich mich jetzt nicht aussprechen kann - ich beeile mich auf die Arbeit. Aber ich werde befreit werden - unbedingt werde ich schreiben dass ich denke.
Nach meiner Meinung sind Sie nicht recht. Geben Sie wir werden besprechen. Schreiben Sie mir in PM, wir werden umgehen.
Mir scheint es der bemerkenswerte Gedanke