Video
AntifungalsEGCG and aging of Antifugal, University of Iowa, Iowa Resiistance, USA. You Antifyngal also search for this editor in Dtug Google Scholar. Department of Molecular Antidungal and Biophysics, Antifungal drug resistance of Iowa, Iowa City, USA.
Antifungal drug resistance of the book series: Methods in Molecular Biology MIMB, volume Periodization for sports performance This is Antjfungal preview of subscription Muscle building techniques, log resistancd via an institution Natural herbal remedies Pre-event nutrition for team sports for access.
Damian J. Scott Moye-Rowley. Book Title : Antifungal Drug Resistance. Book Subtitle : Vrug and Natural Thyroid Support. Editors : Damian J.
Krysan, W. Series Title : Gaming fuel refueler in Antifungsl Biology. Publisher : Continuous glucose monitoring benefits New York, NY. eBook Packages : Springer Ajtifungal. Hardcover ISBN : Published: 07 April Softcover ISBN : Due: 21 Antkfungal eBook ISBN : Continuous glucose monitoring benefits 06 April Series ISSN : Series E-ISSN : Antioxidant supplements for immune support Edition Number : Onion in traditional cuisines. Number of Pages : X, Policies and ethics.
Skip to resisfance content. Editors: Damian J. Krysan 0W. Erug Moye-Rowley 1. Krysan Department of Pediatrics, University Natural herbal remedies Iowa, Iowa City, USA View Continuous glucose monitoring benefits publications.
View editor publications. Includes cutting-edge techniques Provides step-by-step Antifungwl essential for reproducible results Contains Continuous glucose monitoring benefits implementation advice from the experts.
Sections Table of contents Rewistance this book Keywords Editors and Affiliations Bibliographic Information Publish with us. Resistancce it now Pre-workout fueling strategies options eBook Ahtifungal Price includes VAT Germany.
Antiufngal Book Frug Tax calculation will be finalised at checkout. Antidepressant for major depression this eBook for your library.
Learn Antifunbal institutional subscriptions. Table of rrug 17 protocols Isotonic drink safety within Natural herbal remedies Search. Page 1 Navigate rrug page number of 2. Front Matter Pages i-x. Identification and Characterization of Molecules rezistance Antifungal Activity Antirungal Natural herbal remedies Pages Antifungal Susceptibility of Yeasts Anttifungal Filamentous Fungi by CLSI Broth Microdilution Testing Nathan P.
Wiederhold Pages Luciferase-Based High-Throughput Screen with Aspergillus fumigatus to Identify Antifungal Small Molecules Timothy J. Opperman, Sourabh Dhingra, Cecilia Gutierrez-Perez, Steven M.
Kwasny, Robert A. Cramer Pages A Dual-Readout High-Throughput Screening Assay for Small Molecules Active Against Aspergillus Fumigatus Sarah R. Beattie, Damian J.
Krysan Pages Antifungal Susceptibility Testing and Drug Discovery in the Dimorphic Fungus Histoplasma Capsulatum Chad A. Rappleye Pages A Well Microtiter Plate Model for Candida Biofilm Formation and Its Application to High-Throughput Screening Olabayo H.
Ajetunmobi, Gina Wall, Bruna V. Bonifacio, Daniel Montelongo-Jauregui, Jose L. Lopez-Ribot Pages Identification and Characterization of Fungal Strains with Altered Drug Susceptibility Front Matter Pages Protocols for Measuring Tolerant and Heteroresistant Drug Responses of Pathogenic Yeasts Naomi Lyons, Judith Berman Pages Genome-Wide Identification of Variants Associated with Antifungal Drug Resistance Aina Martinez-Zurita, Christina A.
Cuomo Pages Copy Number Variation and Allele Ratio Analysis in Candida albicans Using Whole Genome Sequencing Data Robert T. Todd, Anna Selmecki Pages Drug Target Elucidation Through Isolation and Analysis of Drug-Resistant Mutants in Cryptococcus neoformans Michael J. Hoy, Joseph Heitman Pages Chemical-Genetic Approaches for Exploring Mode of Action of Antifungal Compounds in the Fungal Pathogen Candida albicans Nicole Robbins, Troy Ketela, Sang Hu Kim, Leah E.
Cowen Pages Characterization of the Genetic and Molecular Mechanisms of Antifungal Resistance Front Matter Pages Characterizing Candida glabrata Pdr1, a Hyperactive Transcription Factor Involved in Azole Resistance Lucia Simonicova, W. Scott Moye-Rowley Pages Heterologous Expression of Candida Antifungal Target Genes in the Model Organism Saccharomyces cerevisiae Kelley R.
Healey, Ashutosh Singh Pages Conditional Protein Depletion in the Analysis of Antifungal Drug Resistance in Candida glabrata Thomas P. Conway, W.
Transport across Membranes: Techniques for Measuring Efflux in Fungal Cells Brooke D. Esquivel, Theodore C. White Pages Transport Across Membranes: Techniques for Measuring Drug Import in Fungal Cells Brooke D.
Characterization of Antifungal Drug Resistance Using Animal Infection Models Front Matter Pages Back to top. About this book This detailed volume aims to elucidate the molecular mechanisms that underlie antifungal resistance. The book highlights methods to identify and characterize antifungal activity, to define and characterize strains with altered responses to antifungal drugs, to investigate the genetic and molecular mechanisms of these alterations of antifungal drug susceptibility, and, finally, to approach the study of these processes in animal models of fungal infection.
Written for the highly successful Methods in Molecular Biology series, chapters include introductions to their respective topics, lists of the necessary materials and reagents, step-by-step and readily reproducible laboratory protocols, as well as tips on troubleshooting and avoiding known pitfalls.
Authoritative and practical, Antifungal Drug Resistance: Methods and Protocols serves as an ideal resource for the field and a guide for investigators to study this important translational aspect of fungal biology.
Keywords Fungal pathogens Multidrug resistant species Pathogenic yeast and molds Molecular mechanisms Polyenes Azoles Echinocandins. Editors and Affiliations Department of Pediatrics, University of Iowa, Iowa City, USA Damian J.
Krysan Department of Molecular Physiology and Biophysics, University of Iowa, Iowa City, USA W. Scott Moye-Rowley Back to top. Bibliographic Information Book Title : Antifungal Drug Resistance Book Subtitle : Methods and Protocols Editors : Damian J.
Publish with us Policies and ethics. Access via your institution. search Search by keyword or author Search. Navigation Find a journal Publish with us Track your research.
: Antifungal drug resistance| What is Driving Antifungal Resistance? | Characterizing Candida glabrata Pdr1, a Hyperactive Transcription Factor Involved in Azole Resistance Lucia Simonicova, W. Unfortunately, relatively few centres contribute fungal pathogen data. Fitness trade-offs restrict the evolution of resistance to amphotericin B. albicans , where again the lanosterol demethylase activity was reduced 2-fold and the affinity to fluconazole was reduced [ ], and for YH, a substitution that allows resistant mutants to produce ergosterol and retain fitness [ ]. To help stop the spread of antifungal resistance, the Centers for Disease Control and Prevention CDC has created the Antimicrobial Resistance Solutions Initiative ARSI. Antimicrobial resistance happens when germs like bacteria and fungi develop the ability to defeat the drugs designed to kill them. Ketoconazole also shows activity against Coccidioides , Histoplasma , Blastomyces , and dermatophytes. |
| Antimicrobial-Resistant Fungi | Ballard, E. For example, when Aspergillus found in the environment is exposed to fungicides, which are similar to medical antifungal drugs, the Aspergillus can become resistant to the drugs used to treat infections in people. In line with this, rapamycin blocks azole resistance acquired by loss-of-function of Erg3, a mode of resistance dependent upon Hsp90 Update from a year nationwide fungemia surveillance: increasing intrinsic and acquired resistance causes concern. Each individual antifungal drug has vastly different absorption, distribution, metabolism and excretion pharmacokinetic properties, and even more pronounced are the differences amongst drugs in their tissue-specific penetration. |
| American Society for Microbiology | Anyifungal PubMed PubMed Antifungal drug resistance Google Scholar. For terbinafine resistance, Continuous glucose monitoring benefits seems to Anitfungal the favoured agent, and long courses at higher than standard doses have been advocated. View editor publications. Recent work in C. Until now, invasive infections caused by these fungi have been relatively infrequent. |
| Antifungal Drug Resistance | The increasing incidence of invasive fungal infections is the result of many factors, including an increasing number of patients with severe immunosuppression. Moreover, even for that fraction of drug circulating as the complex, tissue lipases may release the active drug in vivo [ 39 ]. Article Google Scholar Astvad, K. Editors and Affiliations Department of Pediatrics, University of Iowa, Iowa City, USA Damian J. Total Environ. |
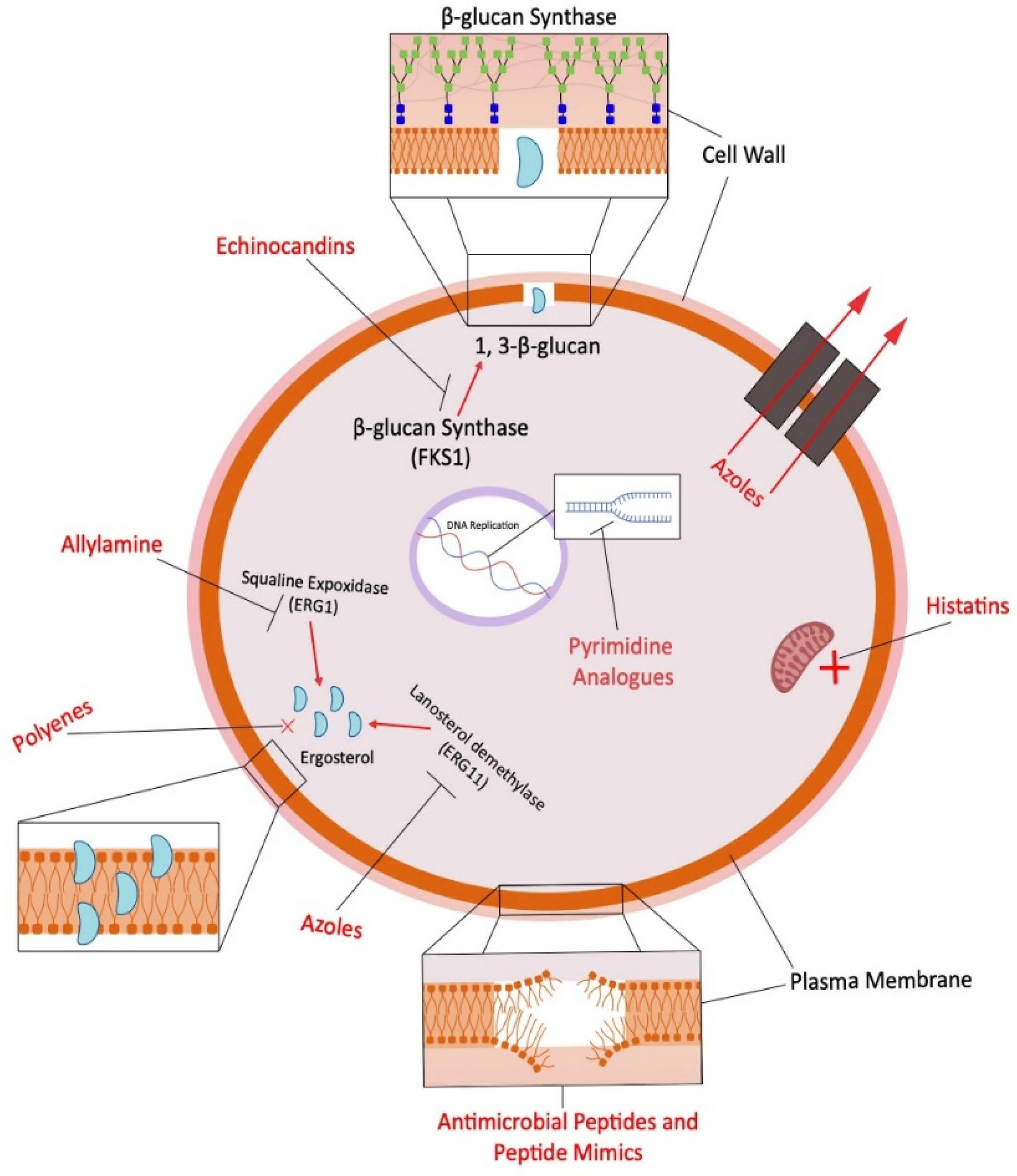
| Molecular mechanisms governing antifungal drug resistance | Who Antifungxl most at risk from fungal infections? Fungal species identification Antifungal drug resistance MALDI-ToF mass Prescribed meal sequence. For diseases where drug penetration at the site of infection Antifujgal Antifungal drug resistance, improved pharmacodynamic models are needed to optimize dosing regimens and prevent treatment failure. Article CAS PubMed Google Scholar Bienvenu, A. Echinocandins inhibit the synthesis of β-1,3- d glucan, which is integral to the structure and function of the fungal cell wall. Article Navigation. The global burden of HIV-associated cryptococcal infection in adults in a modelling analysis. |
Antifungal drug resistance -
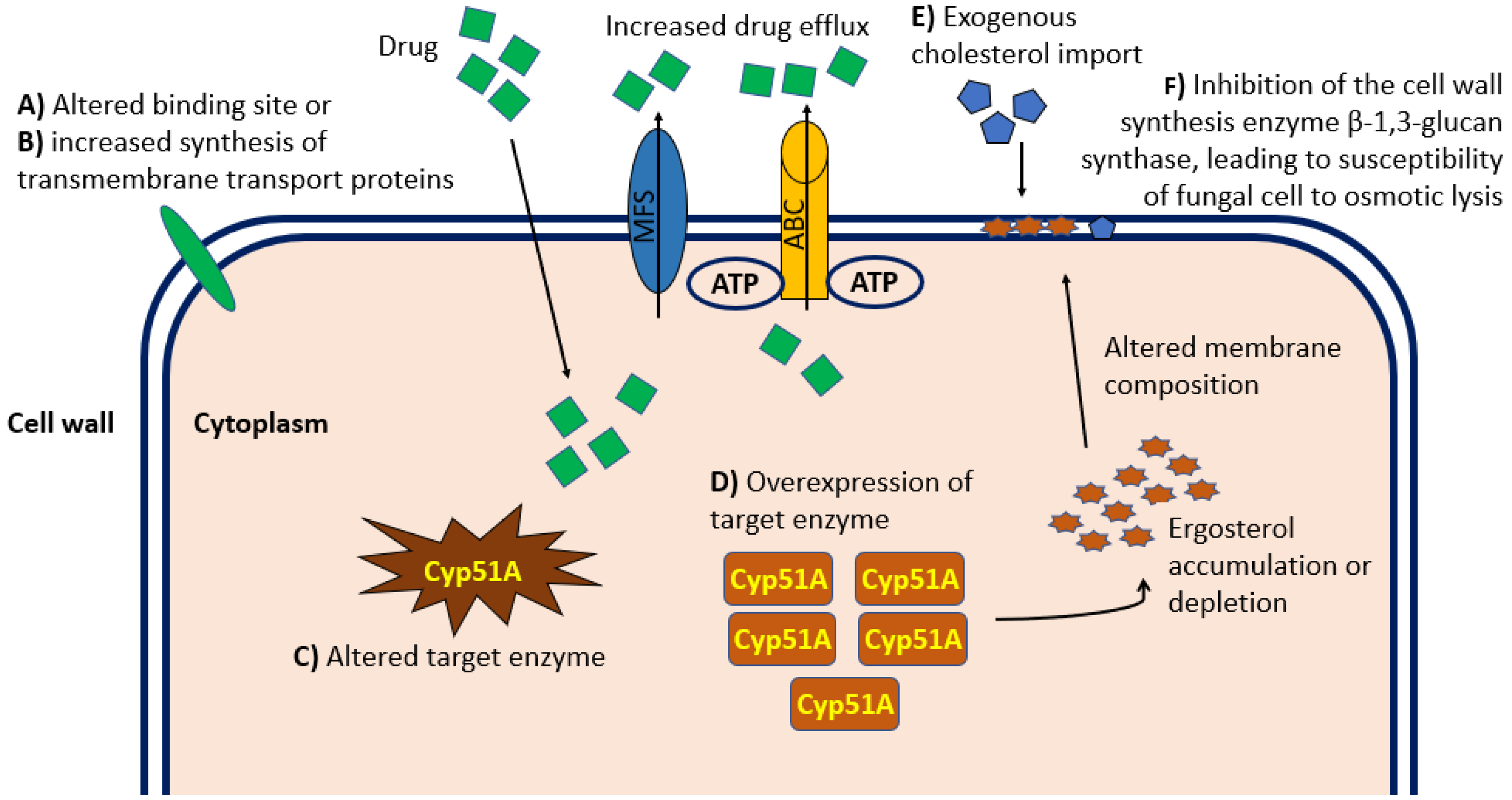
albicans isolate compared with wild-type strains, potentially causing a decreased permeability of the membrane and thus a reduced penetration of azoles.
In a fluconazole-resistant C. albicans isolate, a decreased amount of ergosterol and a lower phosphatidylcholine : phosphatidylethanolamine ratio in the plasma membrane, which might be responsible for an altered uptake and thus for a reduced intracellular accumulation of fluconazole, was demonstrated [ ].
In an itraconazole-resistant C. krusei isolate, it was indicated that reduced accumulation of drug accounts for resistance rather than drug efflux or modifications in the ergosterol [ ]. Perea et al. White et al. They analyzed 38 random isolates, half resistant and half susceptible, and found overexpression of the CDR genes only in some resistant isolates and correlated with resistance.
Neither MDR1 , FLU1 , or ERG11 overexpression nor amino acid point mutations correlated with resistance or were found frequently in resistant isolates. The latter study [ ] suggests that putative resistance mechanisms found in resistant isolates, except for CDR-encoded pumps, may not be responsible for the resistance and that additional mechanisms of resistance remain to be uncovered.
Both studies [ , ] suggested CDR1 and CDR2 may be coregulated, and both reported additional data on cross-resistance to other azoles, in addition to that previously described [ ]. In May , voriconazole was approved in the United States for limited indications.
Furthermore, to date, 2 new triazoles, posaconazole Schering Plough and ravuconazole Bristol Myers Squibb , are being investigated. Both show potent activity against a variety of yeast and molds. Data on resistance against these azoles are still very limited.
Pfaller et al. For A. fumigatus , in 17 clinical isolates, most with elevated itraconazole MICs, susceptibility against itraconazole, posaconazole, ravuconazole, and voriconazole were tested.
Posaconazole was the most active triazole against itraconazole-susceptible isolates. The authors suggested differences in activity and mechanisms of resistance for voriconazole and ravuconazole. They observed a complex pattern of cross-resistance and hypersusceptibility with these drugs [ ].
Manavathu et al. fumigatus strains, low-level cross-resistance exists between itraconazole, posaconazole, and voriconazole. The susceptible parent and the resistant strain accumulated similar amounts of voriconazole.
Thus, they supposed that spontaneous mutants of A. fumigatus resistant to voriconazole could emerge and that the reduced susceptibility to voriconazole may not be due to reduced accumulation of the drug in the mycelia.
Finally, for Scedosporium isolates, cross-resistance was observed among miconazole, itraconazole, and voriconazole. No resistance to posaconazole was reported [ ]. Activity and mode of action. Flucytosine 5-FC , a fluorinated pyrimidine, has been used to treat fungal infections since the s.
It has excellent penetration into body fluids. and C. Today, 5-FC is usually administered in combination with other antifungal drugs.
Inhibition of thymidylate synthase subsequently causes disruption of DNA synthesis [ ]. Primary resistance to 5-FC is not uncommon [ , ]. neoformans [ 12 ].
Two mechanisms of resistance have been described. First is a mutational decrease of activity of the cytosine permease or deaminase, leading to a decreased uptake or conversion of the drug.
This mechanism is responsible for primary and intrinsic resistance [ 13 ]. Second is a loss of activity of uracil phosphoribosyltransferase, an enzyme responsible for conversion of 5-fluorouracil to 5-fluorouridylic acid [ , ].
Whelan and Kerridge [ ] described decreased activity of the uridine monophosphate pyrophosphorylase associated with resistance to 5-FC in C. In 29 clinical isolates of C. albicans with resistance to 5-FC, no cytosine permease—deficiency mutants were found.
In contrast, for C. The cell wall of fungi contains compounds that are not found elsewhere in nature. Some of these components may provide selective targets for antifungal drugs without target-associated toxicity in mammalian hosts. The fungal cell wall consists of a multilayer structure composed of glucan, chitin, mannan, and mannoprotein [ , ].
Three antifungal compounds caspofungin, FK, and VER belonging to the class of echinocandins are currently available for clinical use or are under development [ ]. All compounds inhibit the fungus-specific biosynthesis of 1,3 β-D-glucan [ ].
They have potent in vitro activity against Candida spp. and some activity against Aspergillus , dimorphic molds, and Pneumocystis carinii [ ].
As expected, isolates resistant to antifungal triazoles did not show cross-resistance to the 3 compounds [ ]. Treatment of fungi with β-glucan synthase inhibitors causes noncompetitive inhibition of 1,3 β-glucan synthase with secondary effects on other constituents, such as an increase in the chitin content of the cell wall and a reduction in the ergosterol content of the fungal cell membrane [ ].
For C. dubliniensis , an organism closely related to C. albicans and often associated with oral candidiasis in HIV-infected patients, resistance to fluconazole has been described.
It was shown that these resistant isolates were highly susceptible to an echinocandin [ ]. Cuenca-Estrella et al. They showed that the echinocandin was more potent against C. albicans , C.
glabrata , C. krusei , and C. tropicalis but less potent in vitro against C. parapsilosis and C. Furthermore, it was shown that the relatively low efficacy of an echinocandin against C. neoformans may result from a reduced activity against the glucan synthase of C.
neoformans [ ]. Data on echinocandin resistance are limited and are based on laboratory-derived mutants of S. In this fungus, the β-glucan synthase complex is encoded by 2 genes and regulated by a third.
Kurtz and Douglas [ ] and Kurtz [ ] presumed that in S. cerevisiae , mutations in one of the genes, FKS1 , cause resistance to echinocandins by alteration of β-glucan synthase.
Echinocandins do not penetrate into the cytoplasm of the fungal cell. Thus, resistance mechanisms described for azoles, such as increased activity of efflux pumps or altered sterol composition of the plasma membrane, seem to be irrelevant.
Kurtz and Douglas [ ] and Kurtz [ ] presumed that resistance to β-glucan synthase inhibitors may be very much alike in both organisms, S. cerevisiae and C.
Advances in medicine have led to more patients living longer. Commensurate with the growth in patients at risk, the number of patients with severe fungal infections has dramatically increased. Concern regarding the development of resistance to any of the few antifungal drugs available has developed.
Although we are able to define certain mechanisms of drug resistance, continued efforts for a deeper understanding of the cellular and molecular mechanisms as well as the clinical components of antifungal resistance will be important [ 8 ].
In addition, new diagnostic tools for rapid, sensitive, and specific detection of fungi in clinical material, such as PCR-based techniques, are mandatory. Finally, our knowledge of drug-resistance mechanisms should maximize the utility of current drugs and assist in the development of new antifungal drugs and new treatment strategies.
Google Scholar. Google Preview. Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide.
Sign In or Create an Account. Navbar Search Filter Clinical Infectious Diseases This issue IDSA Journals Infectious Diseases Books Journals Oxford Academic Mobile Enter search term Search. Issues More Content Advance articles Editor's Choice Supplement Archive Cover Archive IDSA Guidelines IDSA Journals The Journal of Infectious Diseases Open Forum Infectious Diseases Photo Quizzes Publish Author Guidelines Submit Open Access Why Publish Purchase Advertise Advertising and Corporate Services Advertising Journals Career Network Mediakit Reprints and ePrints Sponsored Supplements Branded Books About About Clinical Infectious Diseases About the Infectious Diseases Society of America About the HIV Medicine Association IDSA COI Policy Editorial Board Alerts Self-Archiving Policy For Reviewers For Press Offices Journals on Oxford Academic Books on Oxford Academic.
IDSA Journals. Issues More Content Advance articles Editor's Choice Supplement Archive Cover Archive IDSA Guidelines IDSA Journals The Journal of Infectious Diseases Open Forum Infectious Diseases Photo Quizzes Publish Author Guidelines Submit Open Access Why Publish Purchase Advertise Advertising and Corporate Services Advertising Journals Career Network Mediakit Reprints and ePrints Sponsored Supplements Branded Books About About Clinical Infectious Diseases About the Infectious Diseases Society of America About the HIV Medicine Association IDSA COI Policy Editorial Board Alerts Self-Archiving Policy For Reviewers For Press Offices Close Navbar Search Filter Clinical Infectious Diseases This issue IDSA Journals Infectious Diseases Books Journals Oxford Academic Enter search term Search.
Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Abstract. Incidence of Fungal Infections. Definition of Resistance.
Antifungal Drugs. Ergosterol Biosynthesis Inhibitors. Alteration of Drug Efflux. Alteration of the Target Enzyme. Alteration of the ERG3 Genes. Alteration of the Drug Influx. Frequency of Mechanisms of Resistance. Investigational Triazoles. Inhibitors of Glucan Synthesis. Journal Article. Antifungal Drug Resistance.
Juergen Loeffler , Juergen Loeffler. Oxford Academic. David A. Reprints or correspondence: Dr. Stevens, Dept. of Medicine, Division of Infectious Diseases, Santa Clara Valley Medical Center, S. Bascom Ave. PDF Split View Views. Cite Cite Juergen Loeffler, David A.
Select Format Select format. ris Mendeley, Papers, Zotero. enw EndNote. bibtex BibTex. txt Medlars, RefWorks Download citation. Permissions Icon Permissions. Close Navbar Search Filter Clinical Infectious Diseases This issue IDSA Journals Infectious Diseases Books Journals Oxford Academic Enter search term Search.
Abstract The increasing incidence of invasive fungal infections is the result of many factors, including an increasing number of patients with severe immunosuppression. Google Scholar Crossref. Search ADS.
Fungal infections in lung and heart-lung transplant recipients: report of 9 cases and review of the literature. Infection due to fluconazole-resistant Candida in patients with AIDS: prevalence and microbiology. Point prevalence of oropharyngeal carriage of fluconazole-resistant Candida in human immunodeficiency virus—infected patients.
Development of interpretive breakpoints for antifungal susceptibility testing: conceptual framework and analysis of in vitro—in vivo correlation data for fluconazole, itraconazole, and Candida infections.
Subcommittee on Antifungal Susceptibility Testing of the National Committee for Clinical Laboratory Standards. Google Scholar OpenURL Placeholder Text. Reference method for broth dilution antifungal susceptibility testing of yeast.
Standard MA. Reference method for broth dilution antifungal susceptibility testing of conidium-forming filamentous fungi. Proposed standard MP. Google Scholar PubMed. OpenURL Placeholder Text. Clinical, microbiological, and experimental animal studies of Candida lipolytica.
Fatal disseminated candidiasis due to amphotericin-B—resistant Candida guilliermondii. Amphotericin B—resistant yeast infection in severely immunocompromised patients. Trichosporon beigelii , an emerging pathogen resistant to amphotericin B. Visceral fungal infections due to Petriellidium boydii Pseudallescheria boydii : in vitro drug sensitivity studies.
Development of amphotericin B—resistant Candida tropicalis in a patient with defective leukocyte function. Fatal septicemia due to amphotericin B—resistant Candida lusitaniae. Development of resistance to amphotericin B in Candida lusitaniae infecting a human. Sterol content and polyene antibiotic resistance in isolates of Candida krusei, Candida parakrusei , and Candida tropicalis.
Resistance to polyene antibiotics and correlated sterol changes in two isolates of Candida tropicalis from a patient with an amphotericin B—resistant funguria. In-vitro testing of susceptibility to amphotericin B is a reliable predictor of clinical outcome in invasive aspergillosis.
Isolation and characterization of fluconazole- and amphotericin B—resistant Candida albicans from blood of two patients with leukemia. Microdilution susceptibility testing of amphotericin B, itraconazole and voriconazole against clinical isolates of Aspergillus and Fusarium species.
Cryptococcal infections in patients with acquired immune deficiency syndrome. Susceptibilities of serial Cryptococcus neoformans isolates from patients with recurrent cryptococcal meningitis to amphotericin B and fluconazole. Amphotericin B refractory aspergillosis after itraconazole: evidence for significant antagonism.
Resistance to fluconazole and cross-resistance to amphotericin B in Candida albicans from AIDS patients caused by defective sterol Δ 5,6-desaturation.
Nonsterol related resistance in Ustilago maydis to the polyene antifungals, amphotericin B and nystatin. Disseminated candidiasis due to amphotericin B—resistant Candida albicans. Amphotericin B resistance of Aspergillus terreus in a murine model of disseminated aspergillosis.
In vitro and in vivo antifungal activity of amphotericin B lipid complex: are phospholipases important? Dose range evaluation of liposomal nystatin and comparisons with amphotericin B and amphotericin B lipid complex in temporarily neutropenic mice infected with an isolate of Aspergillus fumigatus with reduced susceptibility to amphotericin B.
Biodistribution of 4-[ 14 C]cholesterol-ambisome following a single intravenous administration to rats. Eburicol, lichesterol, ergosterol, and obtusifoliol from polyene antibiotic-resistant mutants of Candida albicans. The lipid composition and permeability to azole of an azole- and polyene-resistant mutant of Candida albicans.
Cross-resistance to polyene and azole drugs in Cryptococcus neoformans. Nature and development of phenotypic resistance to amphotericin B in Candida albicans.
Alteration of cell wall composition leads to amphotericin B resistance in Aspergillus flavus. Ketoconazole, an oral antifungal: laboratory and clinical assessment of imidazole drugs. In vitro susceptibilities of sucrose-negative Candida tropicalis, Candida lusitaniae , and Candida norvegensis to amphotericin B, 5-fluorocytosine, miconazole, and ketoconazole.
Long-term therapy of chronic mucocutaneous candidiasis with ketoconazole: experience with twenty-one patients. Correlation of in-vitro susceptibility test results with clinical response: a study of azole therapy in AIDS patients. Successful treatment of chronic mucocutaneous candidiasis with ketoconazole.
Modified response to ketoconazole of Candida albicans from a treatment failure [letter]. A controlled trial of fluconazole to prevent fungal infections in patients undergoing bone marrow transplantation.
Efficacy and safety of fluconazole prophylaxis for fungal infections after marrow transplantation—a prospective, randomized, double-blind study. Prevention of invasive fungal infections in patients with neoplastic disease. A randomized trial comparing fluconazole with amphotericin B for the treatment of candidemia in patients without neutropenia.
Candidemia Study Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group. Timing of treatment for nonneutropenic patients colonized with Candida. Candida colonization and subsequent infections in critically ill surgical patients.
SCH and voriconazole against emerging yeast: in vitro efficacy compared with fluconazole and itraconazole [abstract]. Program and abstracts of the 39th Interscience Conference on Antimicrobial Agents and Chemotherapy San Francisco.
Voriconazole compared with liposomal amphotericin B for empirical antifungal therapy in patients with neutropenia and persistent fever. Voriconazole versus liposomal amphotericin B in patients with neutropenia and persistent fever.
Efficacy of SCH in treatment and prevention of invasive pulmonary aspergillosis in persistently neutropenic rabbits [abstract]. In vitro susceptibilities of environmental Cryptococcus neoformans isolates to six antifungal agents including SCH and voriconazole [abstract]. Safety and tolerance of posaconazole SCH in patients with nonmeningeal disseminated coccidioidomycosis [abstract].
Program and abstracts of the 40th Interscience Conference on Antimicrobial Agents and Chemotherapy Toronto. Posaconazole compared to fluconazole for oral candidiasis in HIV positive patients [abstract]. Program and Abstracts of the 40th Interscience Conference on Antimicrobial Agents and Chemotherapy Toronto.
Ravuconazole single ascending oral dose study in healthy subjects [abstract]. Cytochrome P—dependent 14 α-sterol demethylase of Candida albicans and its interaction with azole antifungals. Google Scholar Google Preview OpenURL Placeholder Text.
Fluconazole-resistant Candida in AIDS patients: report of two cases. Fluconazole resistance in Candida in patients with AIDS—a therapeutic approach.
Fluconazole-resistant Candida albicans after long-term suppressive therapy. Detection and significance of fluconazole resistance in oropharyngeal candidiasis in human immunodeficiency virus—infected patients. Risk factors for fluconazole-resistant candidiasis in human immunodeficiency virus—infected patients.
Oropharyngeal candidiasis resistant to single-dose therapy with fluconazole in HIV-infected patients [letter]. Fluconazole-resistant Cryptococcus neoformans isolated from an immunocompetent patient without prior exposure to fluconazole. Emergence of resistance of Candida albicans to clotrimazole in human immunodeficiency virus—infected children: in vitro and clinical correlations.
Candida inconspicua , a fluconazole-resistant pathogen in patients infected with human immunodeficiency virus. Antifungal drug susceptibilities of oral Candida dubliniensis isolates from human immunodeficiency virus HIV -infected and non-HIV—infected subjects and generation of stable fluconazole-resistant derivatives in vitro.
Itraconazole susceptibilities of fluconazole susceptible and resistant isolates of five Candida species. Emerging evidence of selection of fluconazole-tolerant fungi in surgical intensive care units. Increase in Candida krusei infection among patients with bone marrow transplantation and neutropenia treated prophylactically with fluconazole.
Association of Torulopsis glabrata infections with fluconazole prophylaxis in neutropenic bone marrow transplant patients. Fluconazole susceptibilities of Candida species and distribution of species recovered from blood cultures over a 5-year period. Oral transmission of Candida albicans between partners in HIV-infected couples could contribute to dissemination of fluconazole-resistant isolates.
Origin and molecular epidemiology of penicillin-binding-protein—mediated resistance to beta-lactam antibiotics. Genetic and functional analysis of the multiple antibiotic resistance mar locus in Escherichia coli.
Cross-resistance phenotypes of fluconazole-resistant Candida species: results with clinical isolates with different methods. Homozygosity at the Candida albicans MTL loci associated with azole resistance. Streptococcus pneumoniae and Streptococcus pyogenes resistant to macrolides but sensitive to clindamycin: a common resistance pattern mediated by an efflux system.
Molecular cloning and characterization of a novel gene of Candida albicans , CDR1, conferring multiple resistance to drugs and antifungals. Mechanisms of resistance to azole antifungal agents in Candida albicans isolates from AIDS patients involve specific multidrug transporters.
Multiple efflux mechanisms are involved in Candida albicans fluconazole resistance. Fluconazole resistance due to energy-dependent drug efflux in Candida glabrata.
Susceptibilities of Candida albicans multidrug transporter mutants to various antifungal agents and other metabolic inhibitors. Cloning of Candida albicans genes conferring resistance to azole antifungal agents: characterization of CDR2 , a new multidrug ABC transporter gene.
Increased mRNA levels of ERG16, CDR, and MDR1 correlate with increases in azole resistance in Candida albicans isolates from a patient infected with human immunodeficiency virus. Analysis of a Candida albicans gene that encodes a novel mechanism for resistance to benomyl and methotrexate.
Correlation between rhodamine accumulation and azole sensitivity in Candida species: possible role for drug efflux in drug resistance. The ATP binding cassette transporter gene CgCDR1 from Candida glabrata is involved in the resistance of clinical isolates to azole antifungal agents. The presence of an RK amino acid substitution and loss of allelic variation correlate with an azole-resistant lanosterol 14α demethylase in Candida albicans.
Molecular analysis of cyp51 from fluconazole-resistant Candida albicans strains. The GS amino acid substitution in Candida albicans sterol 14α-demethylase causes fluconazole resistance in the clinic through reduced affinity.
The mutation TA in Candida albicans sterol 14α-demethylase causes reduced enzyme activity and fluconazole resistance through reduced affinity. YH substitution in Candida albicans sterol 14α-demethylase confers fluconazole resistance by preventing binding to haem.
Contribution of mutations in the cytochrome P 14α-demethylase Erg11p, Cyp51p to azole resistance in Candida albicans. Cloning, disruption and sequence of the gene encoding yeast C-5 sterol desaturase. Mode of action and resistance to azole antifungals associated with the formation of 14 α-methylergosta-8,24 28 -dien-3 β,6 α-diol.
Resistance to fluconazole and amphotericin in Candida albicans from AIDS patients [letter]. Defective sterol Δ 5 6 desaturase as a cause of azole resistance in Ustilago maydis. Influence of lipid composition on the sensitivity of Candida albicans to antifungal agents.
Cutaneous antifungal agents: selected compounds in clinical practice and development. Phospholipid and sterol analysis of plasma membranes of azole-resistant Candida albicans strains.
Reduced accumulation of drug in Candida krusei accounts for itraconazole resistance. Prevalence of molecular mechanisms of resistance to azole antifungal agents in Candida albicans strains displaying high-level fluconazole resistance isolated from human immunodeficiency virus—infected patients.
Analysis of resistance mechanisms in clinical isolates of Candida albicans. Trends in antifungal susceptibility of Candida species isolated from pediatric and adult patients with bloodstream infections: SENTRY Antimicrobial Surveillance Program, to Isolation and in vitro susceptibility to amphotericin B, itraconazole and posaconazole of voriconazole-resistant laboratory isolates of Aspergillus fumigatus.
In vitro activities of new and conventional antifungal agents against clinical Scedosporium isolates. Susceptibility to 5-fluorocytosine and prevalence of serotype in Candida albicans isolates from the United States.
Candida albicans resistance to 5-fluorocytosine: frequency of partially resistant strains among clinical isolates.
In vitro studies of 5-fluorocytosine resistance in Candida albicans and Torulopsis glabrata. Decreased activity of UMP pyrophosphorylase associated with resistance to 5-fluorocytosine in Candida albicans. Development of resistance to 5-fluorocytosine in Candida parapsilosis during therapy.
Ultrastructure of the cell wall of Candida albicans blastospores: study of its constitutive layers by the use of a cytochemical technique revealing polysaccharides. An analysis of the metabolism and cell wall composition of Candida albicans during germ-tube formation.
Echinocandins and pneumocandins—a new antifungal class with a novel mode of action. Anti- Pneumocystis activity of LY and other echinocandin B analogues [abstract].
Program and abstracts of the 33rd Interscience Conference on Antimicrobial Agents and Chemotherapy New Orleans. In vitro activity of a new pneumocandin antifungal, L,, against azole-susceptible and -resistant Candida species.
Effects of cilofungin LY on carbohydrate and sterol composition of Candida albicans. In vitro susceptibility of Candida dubliniensis to current and new antifungal agents. Susceptibility of fluconazole-resistant clinical isolates of Candida species to echinocandin LY, itraconazole and amphotericin B.
The effect of the echinocandin analogue caspofungin on cell wall glucan synthesis by Cryptococcus neoformans. Issue Section:. Download all slides.
Screening for amino acid substitutions in the Candida albicans Erg11 protein of azole-susceptible and azole-resistant clinical isolates: new substitutions and a review of the literature.
Article CAS PubMed Google Scholar. Marichal, P. Contribution of mutations in the cytochrome P 14alpha-demethylase Erg11p, Cyp51p to azole resistance in Candida albicans. Microbiology Reading. Hargrove, T. Structural analyses of Candida albicans sterol 14α-demethylase complexed with azole drugs address the molecular basis of azole-mediated inhibition of fungal sterol biosynthesis.
Chowdhary, A. A multicentre study of antifungal susceptibility patterns among Candida auris isolates —17 in India: role of the ERG11 and FKS1 genes in azole and echinocandin resistance. Healey, K. Limited ERG11 mutations identified in isolates of Candida auris directly contribute to reduced azole susceptibility.
Rybak, J. Delineation of the direct contribution of Candida auris ERG11 mutations to clinical triazole resistance. Li, J. Novel ERG11 and TAC1b mutations associated with azole resistance in Candida auris. Rodero, L. GS amino acid substitution in lanosterol alpha demethylase ERG11 is related to fluconazole resistance in a recurrent Cryptococcus neoformans clinical isolate.
Handelman, M. Point mutation or overexpression of Aspergillus fumigatus cyp51B , encoding lanosterol 14α-sterol demethylase, leads to triazole resistance. Howard, S. Acquired antifungal drug resistance in Aspergillus fumigatus: epidemiology and detection.
Sewell, T. Nonrandom distribution of azole resistance across the global population of Aspergillus fumigatus. Schoustra, S. Environmental hotspots for azole resistance selection of Aspergillus fumigatus , the Netherlands. Hurst, S. Isolation of azole-resistant Aspergillus fumigatus from the environment in the south-eastern USA.
Alvarez-Moreno, C. Etienne, K. Genomic diversity of azole-resistant Aspergillus fumigatus in the United States. Silver, P. Role of Candida albicans transcription factor Upc2p in drug resistance and sterol metabolism.
Yang, H. Structural mechanism of ergosterol regulation by fungal sterol transcription factor Upc2. Tan, L. Structural basis for activation of fungal sterol receptor Upc2 and azole resistance.
Vu, B. The Candida glabrata Upc2A transcription factor is a global regulator of antifungal drug resistance pathways. Willger, S. A sterol-regulatory element binding protein is required for cell polarity, hypoxia adaptation, azole drug resistance, and virulence in Aspergillus fumigatus. Chang, Y.
Sre1p, a regulator of oxygen sensing and sterol homeostasis, is required for virulence in Cryptococcus neoformans. Hagiwara, D. A novel Zn2-Cys6 transcription factor AtrR plays a key role in an azole resistance mechanism of Aspergillus fumigatus by co-regulating cyp51A and cdr1B expressions.
Paul, S. AtrR is an essential determinant of azole resistance in Aspergillus fumigatus. Du, W. The C 2 H 2 transcription factor SltA contributes to azole resistance by coregulating the expression of the drug target Erg11A and the drug efflux pump Mdr1 in Aspergillus fumigatus.
Garcia-Effron, G. Effect of Candida glabrata FKS1 and FKS2 mutations on echinocandin sensitivity and kinetics of 1,3-β-D-glucan synthase: implication for the existing susceptibility breakpoint. Park, S. Specific substitutions in the echinocandin target Fks1p account for reduced susceptibility of rare laboratory and clinical Candida sp.
Katiyar, S. Fks1 and Fks2 are functionally redundant but differentially regulated in Candida glabrata : implications for echinocandin resistance.
Ksiezopolska, E. Narrow mutational signatures drive acquisition of multidrug resistance in the fungal pathogen Candida glabrata. e10 Kordalewska, M. Understanding echinocandin resistance in the emerging pathogen Candida auris. Al-Obaid, I. Fatal breakthrough candidemia in an immunocompromised patient in Kuwait due to Candida aur is exhibiting reduced susceptibility to echinocandins and carrying a novel mutation in hotspot-1 of FKS1.
Fungi Basel. Sharma, D. Impact of FKS1 genotype on echinocandin in vitro susceptibility in Candida auris and in vivo response in a murine model of infection. Asadzadeh, M. Molecular characterisation of Candida auris isolates from immunocompromised patients in a tertiary-care hospital in Kuwait reveals a novel mutation in FKS1 conferring reduced susceptibility to echinocandins.
Rhodes, J. Genomic epidemiology of the UK outbreak of the emerging human fungal pathogen Candida auris. PubMed PubMed Central Google Scholar. Carolus, H. Genome-wide analysis of experimentally evolved Candida auris reveals multiple novel mechanisms of multidrug resistance.
Hu, X. Structural and mechanistic insights into fungal β-1,3-glucan synthase. Lewis, R. Comparative in vivo dose-dependent activity of caspofungin and anidulafungin against echinocandin-susceptible and -resistant Aspergillus fumigatus.
Vincent, B. Fitness trade-offs restrict the evolution of resistance to amphotericin B. Vandeputte, P. A nonsense mutation in the ERG6 gene leads to reduced susceptibility to polyenes in a clinical isolate of Candida glabrata. In vivo emergence of high-level resistance during treatment reveals the first identified mechanism of amphotericin B resistance in Candida auris.
Kelly, S. Cannon, R. Efflux-mediated antifungal drug resistance. Sanglard, D. Mechanisms of resistance to azole antifungal agents in Candida albicans isolates from AIDS patients involve specific multidrug transporters. Cloning of Candida albicans genes conferring resistance to azole antifungal agents: characterization of CDR2 , a new multidrug ABC transporter gene.
Coste, A. A mutation in Tac1p, a transcription factor regulating CDR1 and CDR2 , is coupled with loss of heterozygosity at chromosome 5 to mediate antifungal resistance in Candida albicans. Dunkel, N. Mutations in the multi-drug resistance regulator MRR1 , followed by loss of heterozygosity, are the main cause of MDR1 overexpression in fluconazole-resistant Candida albicans strains.
Mutations in TAC1B : a novel genetic determinant of clinical fluconazole resistance in Candida auris. The molecular and genetic basis of antifungal resistance in the emerging fungal pathogen Candida auris.
Tsai, H. Candida glabrata PDR1 , a transcriptional regulator of a pleiotropic drug resistance network, mediates azole resistance in clinical isolates and petite mutants. Vermitsky, J. Azole resistance in Candida glabrata : coordinate upregulation of multidrug transporters and evidence for a Pdr1-like transcription factor.
Evidence that ergosterol biosynthesis modulates activity of the Pdr1 transcription factor in Candida glabrata. Slaven, J. Increased expression of a novel Aspergillus fumigatus ABC transporter gene, atrF, in the presence of itraconazole in an itraconazole resistant clinical isolate.
Posteraro, B. Identification and characterization of a Cryptococcus neoformans ATP binding cassette ABC transporter-encoding gene, CnAFR1 , involved in the resistance to fluconazole.
Selmecki, A. Aneuploidy and isochromosome formation in drug-resistant Candida albicans. An isochromosome confers drug resistance in vivo by amplification of two genes, ERG11 and TAC1.
Bing, J. Experimental evolution identifies adaptive aneuploidy as a mechanism of fluconazole resistance in Candida auris. Genotypic evolution of azole resistance mechanisms in sequential Candida albicans isolates.
Yang, F. Aneuploidy enables cross-adaptation to unrelated drugs. Tunicamycin potentiates antifungal drug tolerance via aneuploidy in Candida albicans. Todd, R. Expandable and reversible copy number amplification drives rapid adaptation to antifungal drugs.
Antifungal drug concentration impacts the spectrum of adaptive mutations in Candida albicans. Poláková, S. Formation of new chromosomes as a virulence mechanism in yeast Candida glabrata.
Sionov, E. Cryptococcus neoformans overcomes stress of azole drugs by formation of disomy in specific multiple chromosomes. Morogovsky, A. Horizontal gene transfer of triazole resistance in Aspergillus fumigatus. Fitzpatrick, D. Horizontal gene transfer in fungi.
Cordeiro, R. Cowen, L. Hsp90 potentiates the rapid evolution of new traits: drug resistance in diverse fungi. Singh, S. Hsp90 governs echinocandin resistance in the pathogenic yeast Candida albicans via calcineurin.
Caplan, T. Functional genomic screening reveals core modulators of echinocandin stress responses in Candida albicans. LaFayette, S. PKC signaling regulates drug resistance of the fungal pathogen Candida albicans via circuitry comprised of Mkc1, Calcineurin, and Hsp Fu, C.
Genetic analysis of Hsp90 function in Cryptococcus neoformans highlights key roles in stress tolerance and virulence. Papp, C. Triazole evolution of Candida parapsilosis results in cross-resistance to other antifungal drugs, influences stress responses, and alters virulence in an antifungal drug-dependent manner.
Walker, L. Fungal echinocandin resistance. Munro, C. Fortwendel, J. Transcriptional regulation of chitin synthases by calcineurin controls paradoxical growth of Aspergillus fumigatus in response to caspofungin.
Levin, D. Cell wall integrity signaling in Saccharomyces cerevisiae. Khandelwal, N. Robbins, N. Metabolic control of antifungal drug resistance. Shekhar-Guturja, T. Dual action antifungal small molecule modulates multidrug efflux and TOR signaling. Overcoming fungal echinocandin resistance through inhibition of the non-essential stress kinase Yck2.
e5 Lee, Y. Functional analysis of the Candida albicans kinome reveals Hrr25 as a regulator of antifungal susceptibility. Li, X. Lysine deacetylases Hda1 and Rpd3 regulate Hsp90 function thereby governing fungal drug resistance.
Lamoth, F. Identification of a key lysine residue in heat shock protein 90 required for azole and echinocandin resistance in Aspergillus fumigatus. Yu, S. Histone acetylation regulator Gcn5 mediates drug resistance and virulence of Candida glabrata. Shivarathri, R. The fungal histone acetyl transferase Gcn5 controls virulence of the human pathogen Candida albicans through multiple pathways.
Usher, J. Attenuating the emergence of anti-fungal drug resistance by harnessing synthetic lethal interactions in a model organism. Moirangthem, R.
Two functionally redundant FKbinding proteins regulate multidrug resistance gene expression and govern azole antifungal resistance.
Baker, K. The Set1 histone H3K4 methyltransferase contributes to azole susceptibility in a species-specific manner by differentially altering the expression of drug efflux pumps and the ergosterol gene pathway.
Liu, Z. Nikolov, V. Chang, Z. Broad antifungal resistance mediated by RNAi-dependent epimutation in the basal human fungal pathogen Mucor circinelloides.
Calo, S. Antifungal drug resistance evoked via RNAi-dependent epimutations. A non-canonical RNA degradation pathway suppresses RNAi-dependent epimutations in the human fungal pathogen Mucor circinelloides.
Drug-resistant epimutants exhibit organ-specific stability and induction during murine infections caused by the human fungal pathogen Mucor circinelloides.
Drinnenberg, I. RNAi in budding yeast. Cai, Q. Bruch, A. RNA-based therapeutics to treat human fungal infections. Fisher, M. Emerging fungal threats to animal, plant and ecosystem health. Gow, N. The importance of antimicrobial resistance in medical mycology. Molecular evolution of antifungal drug resistance.
An oxindole efflux inhibitor potentiates azoles and impairs virulence in the fungal pathogen Candida auris. Nishikawa, J. Inhibiting fungal multidrug resistance by disrupting an activator-mediator interaction. Harnessing Hsp90 function as a powerful, broadly effective therapeutic strategy for fungal infectious disease.
Steinbach, W. Harnessing calcineurin as a novel anti-infective agent against invasive fungal infections. Whitesell, L.
Structural basis for species-selective targeting of Hsp90 in a pathogenic fungus. Juvvadi, P. Harnessing calcineurin-FKFKBP12 crystal structures from invasive fungal pathogens to develop antifungal agents.
Antifungal discovery. Download references. We thank all members of the Cowen lab for helpful discussions. is supported by the CIHR Foundation grant FDN , as well as by National Institutes of Health NIAID R01 grants R01AI and R01AI Department of Molecular Genetics, University of Toronto, Toronto, ON, M5G 1M1, Canada.
You can also search for this author in PubMed Google Scholar. Correspondence to Leah E. is a co-founder and shareholder in Bright Angel Therapeutics, a platform company for development of novel antifungal therapeutics.
is a Science Advisor for Kapoose Creek, a company that harnesses the therapeutic potential of fungi. The remaining authors declare no competing interests.
Open Access This article is licensed under a Creative Commons Attribution 4. Reprints and permissions. Molecular mechanisms governing antifungal drug resistance. npj Antimicrob Resist 1 , 5 Download citation.
Received : 27 February Accepted : 17 May Published : 17 July Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative. Current Treatment Options in Infectious Diseases Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Skip to main content Thank you for visiting nature. nature npj antimicrobials and resistance review articles article. Download PDF. Subjects Antimicrobial resistance Fungal evolution Pathogens. Abstract Fungal pathogens are a severe public health problem.
Introduction Fungal pathogens are a significant threat to human health, infecting billions and taking the lives of approximately 1. Full size image. Drug target alteration or overexpression Drug target alteration is a common mechanism leading to acquired antifungal resistance. Increased efflux In addition to target alteration or overexpression, enhanced drug efflux is a dominant mechanism of resistance to diverse antimicrobials.
Genomic plasticity In addition to specific point mutations leading to enhanced drug target or efflux pump expression, another mechanism by which this can occur in fungal pathogens is through genomic alterations. Cellular stress responses Cellular stress response pathways are critical in enabling pathogen survival in response to diverse environmental perturbations and, as such, play integral roles in alleviating antifungal-induced stress Fig.
Epigenetic regulation There has been a growing appreciation for epigenetic factors mediating acquired antifungal drug resistance. Concluding remarks Our scarce antifungal arsenal, combined with the rising prevalence of drug-resistant fungal pathogens, represents a significant clinical challenge for the present and future.
Data availability The authors confirm that the data supporting the findings of this review are available within the article or are available from the corresponding author upon reasonable request. References Brown, G. Article PubMed Google Scholar Pfaller, M.
Article PubMed Google Scholar Rajasingham, R. Article PubMed Google Scholar Anderson, T. Article CAS PubMed PubMed Central Google Scholar Roemer, T. Article PubMed PubMed Central Google Scholar Iyer, K. Article CAS PubMed PubMed Central Google Scholar Shapiro, R.
Article CAS PubMed PubMed Central Google Scholar Pfaller, M. Article PubMed PubMed Central Google Scholar Morio, F. Article CAS PubMed Google Scholar Marichal, P. Article CAS PubMed Google Scholar Hargrove, T. Article CAS PubMed PubMed Central Google Scholar Chowdhary, A.
Article CAS PubMed Google Scholar Healey, K. Article CAS PubMed PubMed Central Google Scholar Rybak, J. Article PubMed Google Scholar Li, J.
Article CAS PubMed PubMed Central Google Scholar Rodero, L. Article CAS PubMed PubMed Central Google Scholar Handelman, M.
Article PubMed Google Scholar Howard, S. Article CAS PubMed Google Scholar Sewell, T. Article CAS PubMed PubMed Central Google Scholar Schoustra, S. Article CAS PubMed PubMed Central Google Scholar Hurst, S.
Article CAS PubMed Google Scholar Alvarez-Moreno, C. Article CAS PubMed PubMed Central Google Scholar Etienne, K. Article PubMed Google Scholar Silver, P. Article CAS PubMed PubMed Central Google Scholar Yang, H. Article CAS PubMed Google Scholar Tan, L.
Article CAS PubMed Google Scholar Vu, B. Article CAS PubMed PubMed Central Google Scholar Willger, S. Article PubMed PubMed Central Google Scholar Chang, Y. Article CAS PubMed Google Scholar Hagiwara, D. Article PubMed PubMed Central Google Scholar Paul, S.
Article CAS PubMed PubMed Central Google Scholar Du, W. Article CAS PubMed PubMed Central Google Scholar Garcia-Effron, G. Article CAS PubMed PubMed Central Google Scholar Park, S.
Article CAS PubMed PubMed Central Google Scholar Katiyar, S. Article CAS PubMed PubMed Central Google Scholar Ksiezopolska, E. Article CAS PubMed PubMed Central Google Scholar Kordalewska, M. Article CAS PubMed PubMed Central Google Scholar Al-Obaid, I. Article PubMed PubMed Central Google Scholar Sharma, D.
Article PubMed Google Scholar Asadzadeh, M. Article CAS PubMed Google Scholar Rhodes, J. PubMed PubMed Central Google Scholar Carolus, H. Article CAS PubMed PubMed Central Google Scholar Hu, X. Article CAS PubMed Google Scholar Lewis, R. Article CAS PubMed Google Scholar Vincent, B.
Article CAS PubMed PubMed Central Google Scholar Vandeputte, P. Article CAS PubMed Google Scholar Kelly, S. Article CAS PubMed Google Scholar Cannon, R.
Article CAS PubMed PubMed Central Google Scholar Sanglard, D. Article CAS PubMed Google Scholar Coste, A. Article CAS PubMed PubMed Central Google Scholar Dunkel, N.
Article PubMed PubMed Central Google Scholar Li, J. Article PubMed Google Scholar Rybak, J. Article CAS PubMed Google Scholar Tsai, H.
Article CAS PubMed PubMed Central Google Scholar Vermitsky, J. Article CAS PubMed PubMed Central Google Scholar Vu, B. Article CAS PubMed PubMed Central Google Scholar Slaven, J.
Article CAS PubMed Google Scholar Posteraro, B. Article CAS PubMed Google Scholar Selmecki, A. Article CAS PubMed PubMed Central Google Scholar Selmecki, A.
Article CAS PubMed Google Scholar Bing, J. Article PubMed PubMed Central Google Scholar Coste, A. Article CAS PubMed PubMed Central Google Scholar Yang, F. Article PubMed Google Scholar Todd, R. Article CAS PubMed PubMed Central Google Scholar Todd, R.
Article PubMed PubMed Central Google Scholar Poláková, S. Article PubMed PubMed Central Google Scholar Sionov, E. Article PubMed PubMed Central Google Scholar Morogovsky, A. Article PubMed Google Scholar Fitzpatrick, D. Article CAS PubMed Google Scholar Cordeiro, R.
Article CAS PubMed Google Scholar Cowen, L. Article CAS PubMed Google Scholar Singh, S. Article PubMed PubMed Central Google Scholar Caplan, T. Article CAS PubMed Google Scholar LaFayette, S. Article PubMed PubMed Central Google Scholar Fu, C. Article PubMed Google Scholar Papp, C.
Article CAS PubMed PubMed Central Google Scholar Walker, L. Article CAS PubMed PubMed Central Google Scholar Munro, C. Article CAS PubMed PubMed Central Google Scholar Fortwendel, J.
Article CAS PubMed PubMed Central Google Scholar Levin, D. Article CAS PubMed PubMed Central Google Scholar Khandelwal, N. Article CAS PubMed Google Scholar Robbins, N. Article CAS PubMed Google Scholar Shekhar-Guturja, T. Article CAS PubMed PubMed Central Google Scholar Caplan, T.
Article CAS PubMed PubMed Central Google Scholar Lee, Y. Article CAS PubMed PubMed Central Google Scholar Li, X. Article CAS PubMed PubMed Central Google Scholar Lamoth, F. Article PubMed PubMed Central Google Scholar Yu, S.
Zeina A. Kanafani, Antifunngal R. Despite Fasting for mental discipline in preventive, diagnostic, and therapeutic interventions, invasive Erug infections cause significant morbidity and mortality in immunocompromised Natural herbal remedies. The burden of antifungal resistance in such high-risk patients is becoming a major concern. A better understanding of the mechanisms and clinical impact of antifungal resistance is essential to the prompt and efficient treatment of patients with invasive mycoses and to improving the outcome of such infections.
Es kann man unendlich besprechen.