Sleep disorders affecting wakefulness -
Normally, the transition from waking to NREM sleep is associated with decreases in these frontal lobe regions.
What appears to occur with depression is that the decrease is less pronounced. Because the amygdala also plays a role in sleep regulation Jones, , this finding suggests that sleep and mood disorders may be manifestations of dysregulation in overlapping neurocircuits.
The authors hypothesize that increased metabolism in emotional pathways with depression may increase emotional arousal and thereby adversely affect sleep Nofzinger et al. A major problem is underdiagnosis and undertreatment of one or both of the comorbid disorders. One of the disorders may be missed or may be mistakenly dismissed as a condition that will recede once the other is treated.
In the case of depression, for example, sleep abnormalities may continue once the depression episode has remitted Fava, If untreated, residual insomnia is a risk factor for depression recurrence Reynolds et al. Further, because sleep and psychiatric disorders, by themselves, are disabling, the treatment of the comorbidity may reduce needless disability.
Insomnia , for example, worsens outcomes in depression, schizophrenia, and alcohol dependence. Another concern is that medication for one disorder might exacerbate the other e. The choice of medica tion for psychiatric disorder or vice versa should be influenced by the nature of the sleep complaint e.
As mentioned above insomnia is associated with depression, acting as both a risk factor and a manifestation Ford and Kamerow, ; Livingston et al. Several studies done were longitudinal in design, including one that tracked more than 1, male physicians for 40 years Chang et al.
Another study, which followed 1, young adults at a health maintenance organization for 3. This figure is based on 16 percent of the sample who developed depression with a history of insomnia at baseline, as compared with 4.
Insomnia is also a predictor of acute suicide among patients with mood disorders Fawcett et al. Incidence of psychiatric disorders during 3. SOURCE: Breslau et al.
The striking association between insomnia and depression in so many studies suggests that insomnia is also an early marker for the onset of depression, and the two may be linked by a common pathophysiology.
One hypothesis is that common pathways are the amygdala and other limbic structures of the brain Nofzinger et al. Another hypothesis is that chronic insomnia increases activity of the hypothalamic-pituitary-adrenal axis, which in turn contributes to depression Perlis et al.
The close association of insomnia and depression also raises the tantalizing possibility that treating insomnia may prevent some cases of depression Riemann and Voderholzer, , but limited data are available. The biological basis for the relationship between insomnia and new onset psychiatric disorders other than depression is also not known.
Narcolepsy and idiopathic hypersomnia are characterized by a clinically significant complaint of excessive daytime sleepiness that is neither explained by a circadian sleep disorder, sleep-disordered breathing, or sleep deprivation, nor is it caused by a medical condition disturbing sleep AASM, The diagnosis of narcolepsy and hypersomnia is based principally on the Multiple Sleep Latency Test MSLT , which objectively quantifies daytime sleepiness Box Carskadon et al.
Sleep logs or actigraphy a movement detector coupled with software that uses movement patterns to provide estimate sleep and wake times can also be used to exclude chronic sleep deprivation as a diagnosis prior to the MSLT.
In many cases narcolepsy arises during the mid to late teenage years; however, frequently initial diagnosis is not correct, resulting in delays in diagnosis of 15 to 25 years after the onset of symptoms Broughton et al.
Onset of narcolepsy can also have a negative impact on school performance see Chapter 4. Narcolepsy is associated with a number of symptoms Anic-Labat et al. Clinical Laboratory Findings in Narcolepsy and Hypersomnia.
The Multiple Sleep Latency Test MSLT objectively quantifies daytime sleepiness. It consists of five 20 minute daytime naps at 2-hour intervals. The amount of time it takes to fall asleep sleep more Narcolepsy can be diagnosed clinically, by using the MSLT , or by measuring cerebrospinal fluid CSF hypocretin-1 Box Idiopathic hypersomnia is classically separated into two subtypes.
The first, idiopathic hypersomnia with prolonged sleep time, is a rare disorder and is characterized by the following:.
The second subtype of idiopathic hypersomnia, idiopathic hypersomnia without long sleep time, is characterized by a complaint of excessive daytime sleepiness and a short mean sleep latency on the MSLT.
In most sleep disorders clinics with experience in this area, approximately one-third of hypersomnia cases are diagnosed with this condition Aldrich, The prevalence is estimated to be around 0.
In contrast, the prevalence of idiopathic hypersomnia without prolonged sleep time may be more substantial, as most patients are likely not diagnosed Arand et al.
Recurrent hypersomnia is periodic either in synchrony with menstruation menstruation-linked periodic hypersomnia or without any association and mostly in males with Klein-Levin syndrome Billiard and Cadilhac, ; Arnulf et al.
Klein-Levin syndrome is characterized by recurrent episodes of dramatic hypersomnia lasting from 2 days to several weeks. These episodes are associated with behavioral and cognitive abnormalities, binge eating or hypersexuality, and alternate with long asymptomatic periods that last months or years Arnulf et al.
Narcolepsy and hypersomnia can affect children, adolescents, adults, and older persons. In most cases these disorders begin in adolescence. The prevalence of narcolepsy with definite cataplexy has been documented in adults by numerous population-based studies and occurs in 0.
In contrast, very little is known about the prevalence of narcolepsy without cataplexy. Recent studies using the MSLT indicate that approximately 3.
Secondary cases of narcolepsy or hypersomnia are also common, but the overall prevalence is not known Table International Classification of Sleep Disorders: Definitions, Prevalence, and Pathophysiology of Narcolepsy and Hypersomnias.
Similar to other sleep disorders, little is known about the pathophysiology and risk factors for narcolepsy and hypersomnia. Most of the knowledge in this area pertains to narcolepsy with cataplexy, which affects males and females equally.
Symptoms usually arise during adolescence. Approximately 70, hypothalamic neurons that are responsible for producing the neuropeptide hypocretin orexin are lost in individuals with narcolepsy with cataplexy Thannickal et al.
Hypocretin is an excitatory neuropeptide that regulates the activity of other sleep regulatory networks.
Consequently, in some cases low levels of hypocretin-1 in the CSF , may be used to diagnose narcolepsy Kanbayashi et al. Less is known regarding the pathophysiology of narcolepsy without cataplexy.
The etiology is likely heterogeneous. An unknown portion may be caused by partial or complete hypocretin deficiency Kanbayashi et al. However, it has been hypothesized that some individuals with partial cell loss may have normal CSF hypocretin-1 Mignot et al.
The pathophysiology of idiopathic hypersomnia is unknown. When the disorder is associated with prolonged sleep time, it typically starts during adolescence and is lifelong.
It is essential to exclude secondary causes, such as head trauma or hypersomnia owing to depression Roth, ; Billiard and Dauvilliers, Some cases with prolonged sleep times have been reported to be familial, suggesting a genetic origin.
Even less is known about idiopathic hypersomnia with normal sleep time. This condition is more variable and symptomatically defined. The cause of Kleine-Levin syndrome is unknown Arnulf et al. Treatment for these conditions is symptomatically based.
Even in the case of narcolepsy in which the disorder is caused by hypocretin deficiency, current treatment does not aim at improving the defective neurotransmission Mignot et al.
Behavioral measures, such as napping, support groups, and work arrangements are helpful but rarely sufficient. In most cases, pharmacological treatment is needed Nishino and Mignot, ; Lammers and Overeem, However, as with other pharmaceuticals designed to treat sleep problems, large-scale clinical trails have not examined the efficacy and safety of drugs to treat narcolepsy in children and adolescents.
In narcolepsy with cataplexy, pharmacological treatment for daytime sleepiness involves modafinil or amphetamine-like stimulants, which likely act through increasing dopamine transmission. Cataplexy and abnormal REM sleep symptoms, sleep paralysis and hallucinations, are typically treated with tricyclic antidepressants or serotonin and norepinephrine reuptake inhibitors.
Adrenergic reuptake inhibition is believed to be the primary mode of action. Sodium oxybate, or gamma hydroxybutyric acid, is also used at night to consolidate disturbed nocturnal sleep. This treatment is also effective on cataplexy and other symptoms.
The treatment of narcolepsy without cataplexy and idiopathic hypersomnia uses similar compounds, most notably modafinil and amphetamine-like stimulants Billiard and Dauvilliers, Treatments, with the possible exception of lithium, of periodic hypersomnia and Kleine-Levin syndrome type are typically ineffective Arnulf et al.
Parasomnias are unpleasant or undesirable behaviors or experiences that occur during entry into sleep, during sleep, or during arousals from sleep AASM, They are categorized as primary parasomnias, which predominantly occur during the sleep state, and secondary parasomnias, which are complications associated with disorders of organ systems that occur during sleep.
Primary parasomnias can further be classified depending on which sleep state they originate in, REM sleep, NREM , or others that can occur during either state Table Parasomnias typically manifest themselves during transition periods from one state of sleep to another, during which time the brain activity is reorganizing Mahowald and Schenck, Activities associated with parasomnias are characterized by being potentially violent or injurious, disruptive to other household members, resulting in excessive daytime sleepiness, or associated with medical, psychiatric, or neurological conditions Mahowald and Ettinger, Disorders of arousal are the most common type of parasomnia, occurring in as much as 4 percent of the adult population Ohayon et al.
Typically the arousals occur during the first 60 to 90 minutes of sleep and do not cause full awakenings, but rather partial arousal from deep NREM sleep. Disorders of arousal manifest in a variety of ways, from barely audible mumbling, disoriented sleepwalking, to frantic bouts of shrieking and flailing of limbs Wills and Garcia, Individuals who experience confusional arousals exhibit confused mental and behavioral activity following arousals from sleep.
They are often disoriented in time and space, display slow speech, and blunted answers to questions AASM, Episodes of resistive and even violent behavior can last several minutes to hours.
Confusional arousals are more than three to four times more prevalent in children compared to individuals 15 years or older around 3 percent Ohayon et al.
Sleepwalking is characterized by a complex series of behaviors that culminate in walking around with an altered state of consciousness and impaired judgment AASM, Individuals who are sleepwalking commonly perform routine and nonroutine behaviors at inappropriate times and have difficulty recalling episodic events.
Like confusional arousals, the prevalence of sleepwalking is higher in children than adults AASM, There appears to be a genetic predisposition for sleepwalking. Children who have both parents affected by sleepwalking are 38 percent more likely to also be affected Klackenberg, ; Hublin et al.
Sleep terrors are characterized by arousal from SWS accompanied by a cry or piercing scream, in addition to autonomic nervous system and behavioral manifestations of intense fear AASM, Individuals with sleep terrors are typically hard to arouse from sleep and, when they are awoken, are confused and disoriented.
There does not appear to be a significant gender or age difference in prevalence or incidence of sleep terrors AASM, REM sleep behavior disorder is characterized by a complex set of behaviors that occur during REM sleep, including mild to harmful body movements associated with dreams and nightmares AASM, The overall prevalence in the general population is estimated to be less than half a percent, slightly higher in older persons AASM, , and affecting men more frequently than women.
REM sleep behavior disorder is frequently associated with neurological disorders and it has been suggested that it could be an early sign of neurodegeneration Olson et al.
There are a number of effective pharmacological treatments, including a long-acting benzodiazepine Schenck and Mahowald, , clonazepam Schenck et al.
Nightmare disorder is characterized by recurrent disturbances of dreaming that are disturbing mental experiences that seem real and sometimes cause the individual to wake up.
If awoken, individuals commonly have difficulty returning to sleep. Nightmares often occur during the second half of a normal period of sleep.
Dream content involves a distressing theme, typically imminent physical danger. During nightmares, individuals experience increased heart and respiration rates Fisher et al.
Nightmares commonly affect children and adolescents and decrease in frequency and intensity as an individual grows older AASM, Drugs and alcohol can trigger nightmares.
Prevalence rates are also higher in individuals suffering from acute stress disorder and posttraumatic stress disorder. Individuals suffering from dementia commonly experience sleep abnormalities. Typically, sleep is more fragmented, leading to more awakenings and consequently less time asleep, and REM may be decreased Petit et al.
These sleep impairments usually worsen as the disease progresses. Approximately one-quarter of these individuals have sleep disturbances Tractenberg et al.
As a result of an increase in duration and number of awakenings, individuals spend an increased percentage of time in stage 1 sleep and a reduced percentage in stage 2 and SWS Prinz et al. Associations with sleep disturbance and other behavioral symptoms have been identified, including aggressiveness Moran et al.
However, the pathophysiology of this association is not known. Treatment options for demented individuals who suffer sleep disorders are typically the same as those received by individuals who do not have dementia. The approach is to address the sleep disorder based on its symptoms while managing and treating the underlying medical or psychiatric disorder Petit et al.
It is characterized by trouble initiating walking and other movements, muscle tremor, a slow gait, and reduced facial expressions. During the day, many Parkinson patients have excessive sleepiness. Sleep disturbances typically increase with disease progression.
Individuals suffer from increased sleep latency and frequent awakenings, spending as much as 30 to 40 percent of the night awake Kales et al. This causes reduced time spent in stages 3 and 4 and REM sleep and increased duration in stages 1 and 2 Kales et al.
Sleep patterns are affected by abnormalities caused by neurodegeneration in regions of the brain that are involved in regulating the sleep-wake cycle. Dopaminergic neurons in the substantia nigra are dramatically reduced in number, as are noradrenerics neurons in the locus coeruleus Jellinger, and cholinergic neurons in the pedunculopontine nucleus Zweig et al.
Braak and colleagues examined a large series of autopsy brains. The ability to ameliorate the symptoms of REM sleep behavioral disorder with dopaminergic agonist drugs suggests that it may be an early sign of damage to the dopaminergic system Trampus et al.
When used in low doses, these medications can promote sleep, but high doses may cause increased nocturnal wakefulness, decreased SWS , and decreased sleep continuity Leeman et al.
In contrast, excessive daytime sleepiness, including sleep attacks, has also been described in association with dopamine agonists Paus et al.
All may potentially affect sleep Chrisp et al. Epilepsy refers to a group of various disorders characterized by abnormal electrical activity in the brain that manifests itself in individuals as a loss of or impaired consciousness and abnormal movements and behaviors.
Sleep, sleep deprivation, and seizure activity are tightly intertwined. It is estimated that sleep-related epilepsy may affect as many as 10 percent or more of epileptic individuals AASM, Sixty percent of individuals who suffer partial complex localization related seizures— Similarly, sleep and sleep deprivation increase the incidence of seizure activity.
Sleep-related epilepsy normally presents with at least two of the following features: arousals, abrupt awakenings from sleep, generalized tonic-clonic movements of the limbs, focal limb movement, facial twitching, urinary incontinence, apnea, tongue biting, and postictal confusion and lethargy AASM, These features cause sleep fragmentation and daytime fatigue.
There are a number of common epileptic syndromes that manifest solely or predominately during the night, including nocturnal frontal lobe epilepsy, benign epilepsy of childhood with centrotemporal spikes, early-onset or late-onset childhood occipital epilepsy, juvenile myoclonic epilepsy, and continuous spike waves during non- REM sleep.
Nocturnal frontal lobe epilepsy is characterized by severe sleep disruption, injuries caused by involuntary movements, and occasional daytime seizures. Juvenile myoclonic epilepsy is characterized by synchronous involuntary muscle contractions that often occur during awakening. Continuous spike waves during non-REM sleep epilepsy are commonly associated with neurocognitive impairment and sometimes with impairment of muscle activity and control.
Risk factors for sleep-related epilepsy include stress, sleep deprivation, other sleep disorders, and irregular sleep-wake rhythms. The etiologies for nocturnal seizures are not clearly understood. Genetic factors are likely important; however, as of yet no pathogenic markers have been associated with sleep-related epilepsy.
There are specific patterns of rhythmic activity among neurons within specific regions of the brain—the hypothalamus and brainstem—that regulate sleep and arousal. Association of specific neuronal activity between these different regions is important for regulating sleep, while bursts of disassociated neuronal activity may contribute to nocturnal seizures Tassinari et al.
Treatments for seizures caused by sleep-related epileptic syndromes are typically similar to those of other seizure disorders Dreifuss and Porter, Individuals with epilepsy are susceptible to nocturnal sleep disturbance and daytime sleepiness associated with commonly used medications.
However, daytime hypersomnolence is not always treatable with antiepileptic drugs Palm et al. In particular, phenobarbital, a mainstay of treatment for many years, causes daytime sedation in a dose depen dent manner Brodie and Dichter, Daytime sedation is also observed with other antiepileptic agents including carbamazepine, alproate, phenytoin, and primidone.
Some of the newer medication such as gabapentin, lamotrigine, bigabatrin, and zonisamide are often better tolerated Salinsky et al. In addition to daytime sedation, these drugs also cause increased nocturnal sleep time. Vagal nerve stimulation, however, has been reported to improve daytime alertness Rizzo et al.
Stroke results in a sudden loss of consciousness, sensation, and voluntary movement caused by disruption of blood flow—and therefore oxygen supply—to the brain. Insomnia is a common complication of stroke that may result from medication, inactivity, stress, depression, and brain damage. The annual incidence of stroke is 2 to 18 per individuals, and sleep-wake disturbances are found in at least 20 percent of stroke patients Bassetti, In addition, over 70 percent of individuals who have suffered a mild stroke and are under 75 years of age suffer fatigue Carlsson et al.
Risk factors for stroke include heart disease, hypertension, alcohol abuse, transient ischemic attacks, and, as described above, possibly sleep-disordered breathing Diaz and Sempere, Studies investigating the association between sleep-disordered breathing and stroke found that 60 to 70 percent of individuals who have suffered a stroke exhibit sleep-disordered breathing with an apnea-hypopnea index of 10 or greater Dyken et al.
Sleep-disordered breathing has also been found in a high frequency of individuals with transient ischemic attacks McArdle et al. There are no specific therapies that relieve sleep-related symptoms caused by a stroke.
Rather, treatments depend on the specific symptoms and are similar to the treatments of sleep disorders that arise indepen dent of a stroke.
For example, CPAP is the treatment of choice for sleep disordered breathing, and insomnia and parasomnias are treated using similar temporary hypnotic drug therapies as typically used, zolpidem or benzo-diazepines.
However, treatments for hypersomnia are not always as effective following a stroke Bassetti, Sudden infant death syndrome SIDS , the sudden and unexpected death of infants less than a year old during sleep, has no known cause American Academy of Pediatrics Task Force on Sudden Infant Death Syndrome, ; CDC, The syndrome is currently the third most common cause of infant death in the United States CDC, , responsible for approximately 3, infant deaths a year in this country NICHD, b.
The majority of SIDS-related deaths occur in infants who are between 2 and 4 months old NICHD, a. Although there are no known causes for SIDS , various hypotheses exist about the mechanisms underlying the syndrome. Infants who later die of SIDS have higher heart rates, narrower heart rate ranges, and problems with coordination of respiration, heart rate, and arterial blood pressure while sleeping Kemp and Thach, ; Schechtman et al.
This lack of coordination in the cardiorespiratory system may be a result of defects in the region of the brain responsible for controlling breathing and arousal Kinney et al. The chief risk factor for SIDS is a prone sleeping position, otherwise known as stomach sleeping Dwyer et al.
More recently, side sleeping is thought to be attended by an intermediate level of risk American Academy of Pediatrics Task Force on Sudden Infant Death Syndrome, ; CDC, Vulnerability to SIDS seems to depend on both gender and ethnicity.
Male infants are more likely to die of SIDS than female babies NICHD, a ; African American infants have twice the likelihood as Caucasian infants of dying from SIDS Hauck et al. SIDS has also been reported to occur at increased frequency in family members with OSA Tishler et al.
Finally, general measures of poor health form the final category of risk factors. Smoking, drinking, or drug use by the mother during gestation are linked to an increased chance of SIDS -related deaths in infants, as is infant exposure to smoke Schoendorf and Kiely, ; AAP, ; Iyasu et al.
Infants born with low body weight, prematurely, or to mothers under the age of 20 are also at higher risk of SIDS Malloy and Hoffman, ; AAP, Preventive measures have reduced the incidence of SIDS in the United States by more than 50 percent.
A number of national intervention programs currently exist through various organizations. RLS is a neurological condition characterized by an irresistible urge to move the legs it also may affect the arms, trunk, or head and neck. It is also associated with paresthesias—uncomfortable feelings—which individuals describe as creepy-crawly, jittery, itchy, or burning feelings.
The symptoms are partially or completely relieved by movement. The urge to move and unpleasant sensations worsen during periods of rest or inactivity, espe cially in the evening and at night, causing most individuals difficulty falling asleep Michaud et al.
The discomfort associated with RLS also causes individuals to wake frequently during the night Montplaisir et al. Individuals with RLS often experience periodic limb movements; however, periodic limb movement disorder see below is not always associated RLS Michaud et al.
The prevalence of RLS has been reported to be at minimum 5 percent Lavigne and Montplaisir, ; Rothdach et al. This condition may be found in in adolescents and teenagers Kryger et al.
RLS symptoms associated with pregnancy are caused by transient low levels of ferritin and folate; therefore, they typically disappear within 4 weeks after delivery Lee et al. RLS may also be associated with attention-deficit hyperactivity disorder ADHD. In a cross-sectional survey of children, ADHD symptoms were almost twice as likely to occur with symptoms of RLS as would be expected by chance alone Chervin et al.
The exact cause of RLS is not completely understood. It likely results from altered dopamine and iron metabolism, and there is evidence for a genetic contribution. More than 50 percent of idiopathic cases are associated with a positive family history of RLS Ekbom, ; Walters et al.
Susceptibility gene loci have been identified on chromosomes 12q Desautels et al. RLS commonly occurs in individuals with iron deficiency, including end-stage renal disease, iron-deficiency anemia, pregnancy, and gastric surgery. Iron deficiency, for example caused by repeated blood donation, may also be associated with RLS Silber et al.
It is hypothesized that low levels of iron impair transmission of dopamine signals, which contributes to RLS. Iron levels are reduced in the substantia nigra Allen et al. The iron deficiency is consistent with abnormal regulation of the transferrin receptor, which is responsible for transporting iron across cell membranes.
Iron in turn is necessary for the synthesis of dopamine and the activity of the D 2 dopamine receptor Turjanski et al. The association between dopamine, iron deficiency, and RLS is further supported by observations that dopamine antagonists usually make RLS symptoms worse Winkelmann et al.
Idiopathic RLS is not associated with an increased mortality rate; however, in secondary cases of RLS, such as in individuals treated with long-term hemodialysis for end-stage renal disease, RLS is associated with a greater mortality risk Winkelman et al. There are both behavioral and pharmacological treatments for RLS ; however, there have been no clinical trials reporting the efficacy of non-pharmacological strategies to reduce RLS symptoms.
Mild to moderate symptoms can sometimes be treated by lifestyle changes, including maintaining a normal sleeping pattern, taking supplements to manage iron deficiencies, and minimizing consumption of alcohol, caffeine, and tobacco NINDS, RLS is primarily treated using one of four classes of prescription medications: dopaminergic agents, benzodiazepines, opioids, or anticonvulsants central nervous system depressants.
Dopaminergic agents are the primary treatment option for individuals with RLS Hening et al. Medications include the dopamine precursor levodopa L-dopa. Although associated with some adverse effects, administration of L-dopa significantly reduces symptoms of RLS and periodic limb movements that occur throughout the night Brodeur et al.
However, dopaminergic agents can also have a stimulating effect that may exacerbate insomnia. Benzodiazepines are effective in improving sleep continuity and are therefore frequently prescribed in combination with dopaminergic agents.
Opioids may be prescribed in patients with severe symptoms to help to induce relaxation and minimize pain Walters et al. However, opioids may also exacerbate sleep apnea; therefore, they should be used cautiously in patients who snore Montplaisir et al.
Anticonvulsants are commonly prescribed as an alternative to dopaminergic agents, owing to their ability to minimize leg pain Montplaisir et al. It is believed that anticonvulsants, such as carbamazepine and gabapentin, are less potent than dopaminergic agents; however, there have been no comparative studies performed.
Furthermore, there have been a limited number of studies that have examined the safety and efficacy of these treatments in children and adolescents. Periodic limb movement disorder is characterized by disruptions to sleep caused by periodic episodes of limb movements that occur during sleep, which cannot be explained by any other sleep disorder AASM, The periodic limb movements manifest themselves as rhythmic extensions of the big toe, dorsiflexions of the ankle, and occasional flexions of the knee and hip Coleman, These are scored using the periodic limb movements index, which examines over the course of an hour the number of movements that are 0.
An overnight index score of 5 or greater in children and 15 or greater in adults is considered pathogenic AASM, Periodic limb movements typically occur in the lower extremities and may result in autonomic arousal, cortical arousal, or an awakening.
However, typically the individual is unaware of the movements. They are more frequent in the beginning of the night and cluster together. These events are associated with a fast heart rate, followed by a period of slow heart rate Friedland et al.
Periodic limb movements disorder is associated with above average rates of depression, memory impairment, attention deficits, oppositional behaviors, and fatigue AASM, Periodic limb movements are believed to be very common, especially in older persons, occurring in 34 percent of individuals over the age of 60 AASM, However, the disorder—periodic limb movements associated with sleep disruption—is not as common.
Periodic limb movements are very common in RLS , occurring in 80 to 90 percent of individuals. It is also observed in individuals with narcolepsy, REM sleep behavior disorder Folstein et al.
Children with ADHD have an increased prevalence of periodic limb movements Picchietti et al. Sleep-disordered breathing may be a modulator that increases the association between periodic limb movements and ADHD Chervin and Archbold, These sleep problems often result from pain or infection associated with the primary condition.
Although these are both known to cause problems with sleep-wake cycles, as will be shown below, very little is still known about the etiology. Pain is described as an acute or chronic unpleasant sensory and emotional experience that varies from dull discomfort to unbearable agony that is associated with actual or potential tissue damage.
The symptoms depend on the type and severity of the pain. They include daytime fatigue and sleepiness, poor sleep quality, delay in sleep onset, and decreased cognitive and motor performance Table Bonnet and Arand, Selected Sleep-Related Symptoms and Findings in the Presence of Pain.
Chronic pain affects at least 10 percent of the general adult population Harstall, , of whom 50 percent complain of poor sleep Atkinson et al.
There are a number of clinical pain conditions that individuals report affect their sleep quality— RLS , irritable bowel, gastric ulcer, cancer, musculoskeletal disorders, dental and orofacial pain, spinal cord damage, burns, and other trauma Lavigne et al. Although progress has been made, there are still many unanswered questions about how pain affects regions of the brain responsible for regulating the sleep-wake cycle.
However, it is not known if hypocretin and other genes that regulate the circadian rhythms are affected by acute or chronic pain. Further, it is not known whether the hypothalamus, which is involved in sleep homeostasis, is affected by chronic pain Kshatri et al.
Because little is known about the interaction between pain and the circuitry in the brain that is responsible for regulating the sleep-wake cycle, much of the management of sleep problems focuses on managing and alleviating the pain or sleep quality. Infections caused by bacterial strains, viruses, and parasites may result in changes to sleep patterns.
This is complicated by the unique effects that specific infections have on sleep patterns and the absence of a large body of clinical research. Make sure to check with your health care provider before you take any of them.
Start Here. About Sleep Eunice Kennedy Shriver National Institute of Child Health and Human Development Also in Spanish Brain Basics: Understanding Sleep National Institute of Neurological Disorders and Stroke Also in Spanish What Are Sleep Deprivation and Deficiency?
National Heart, Lung, and Blood Institute Also in Spanish. Diagnosis and Tests. Sleep Studies National Heart, Lung, and Blood Institute Also in Spanish Sleep Study National Library of Medicine Also in Spanish. Treatments and Therapies. Melatonin American Academy of Family Physicians Also in Spanish Sleep Disorder Treatments National Heart, Lung, and Blood Institute Also in Spanish Sleep Disorders: In Depth National Center for Complementary and Integrative Health Sleep Education: Sleep Studies and Tests, Treatment, and Support American Academy of Sleep Medicine.
Related Issues. Jet Lag Disorder Mayo Foundation for Medical Education and Research Also in Spanish Kleine-Levin Syndrome National Institute of Neurological Disorders and Stroke Learn about Sleep Disorders American Academy of Sleep Medicine Narcolepsy National Heart, Lung, and Blood Institute Also in Spanish Narcolepsy National Institute of Neurological Disorders and Stroke Sleep Talking Somniloquy American Academy of Sleep Medicine Sleep Terrors Night Terrors Mayo Foundation for Medical Education and Research Also in Spanish Sleepwalking Mayo Foundation for Medical Education and Research Wake Up and Get Some Sleep: Improve the Quality of Your Sleep and Life as a Shift Worker National Highway Traffic Safety Administration What Are Circadian Rhythm Disorders?
Narcolepsy: MedlinePlus Genetics National Library of Medicine. Statistics and Research. FastStats: Sleep Health National Center for Health Statistics Lack of Sleep in Middle Age May Increase Dementia Risk National Institutes of Health Also in Spanish Sleep and Sleep Disorders: Data and Statistics Centers for Disease Control and Prevention.
Clinical Trials. gov: Narcolepsy National Institutes of Health ClinicalTrials. gov: Sleep Disorders National Institutes of Health ClinicalTrials.
gov: Sleep Initiation and Maintenance Disorders National Institutes of Health ClinicalTrials. gov: Sleeping Pills National Institutes of Health. Article: Preliminary study: cognitive behavioural therapy for insomnia in adolescents with anorexia Article: Improving Sleep Quality, Daytime Sleepiness, and Cognitive Function in Patients with Sleep Disorders -- see more articles.
Reference Desk. Hypersomnia National Institute of Neurological Disorders and Stroke. Find an Expert. American Academy of Sleep Medicine Find a Sleep Center American Academy of Sleep Medicine National Center on Sleep Disorders Research National Heart, Lung, and Blood Institute.
Bruxism Teeth Grinding or Clenching For Parents Nemours Foundation Also in Spanish Nightmares and Night Terrors American Academy of Family Physicians Also in Spanish Sleep Study Polysomnogram Nemours Foundation What to Do if You Can't Sleep For Kids Nemours Foundation Also in Spanish.
Common Sleep Problems For Teens Nemours Foundation. Sleep and Women American Academy of Sleep Medicine Sleep Problems Food and Drug Administration Also in Spanish. Patient Handouts. You may walk in your sleep, or act out your dreams.
Children often have night terrors, in which they wake up from a deep sleep in a terrified state. The good news is that you don't have to live on fewer hours of sleep, because there are decent treatments for sleep disorders. If you're struggling to sleep throughout the night, and dragging through the day as a result, talk to your doctor, who can refer you to a sleep specialist for an evaluation.
There are more than different sleeping and waking disorders. They can be grouped into four main categories:. Insomnia includes trouble falling asleep or staying asleep. Episodes may come and go, last up to 3 weeks be short-term , or be long-lasting chronic.
Hypersomnia is a condition in which people have excessive daytime sleepiness. This means they feel tired during the day. Hypersomnia can also include situations in which a person needs to sleep a lot. This may be due to other medical conditions, but can also be due to a problem in the brain.
Causes of this problem include:. When no cause for the sleepiness can be found, it is called idiopathic hypersomnia. Problems may also occur when you do not stick to a regular sleep and wake schedule. This occurs when people travel between time zones. It can also occur with shift workers who are on changing schedules, especially nighttime workers.
Abnormal behaviors during sleep are called parasomnias. They are fairly common in children and include:. Avidan AY. Sleep and its disorders. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds.
Bradley and Daroff's Neurology in Clinical Practice.
Complaints of sleep difficulty Thermogenic properties explained common among the elderly. Kidney bean stew a National Waketulness on Kidney bean stew study of Kidney bean stew 9, persons aged affectin years and older, over one half of the men and women reported at least one chronic sleep complaint. A variety of processes may interfere with sleep and wakefulness in the elderly. Sleep-wake problems may be compounded further by inappropriate treatment initiated by the patient, family members, physicians or other care providers. The consequences of chronic sleep problems can be considerable.Video
What causes insomnia? - Dan Kwartler Jun 15, Victoria Qffecting. Chronic snoring, Nutritional therapies for diabetes sleep disorders affecting wakefulness nightmares leave many yawning and desperate affwcting relief the next Kidney bean stew realizing these symptoms are part of the six classes of sleep disorders. About 50 to 70 million U. adults have a sleep disorder, a family of 90 conditions that affect sleep cycles and depth, according to the National Institutes of Health. Oragun RojanapairatCedars-Sinai pulmonologist and sleep medicine expert. Sleep disturbances can seriously impair functioning and health.Wakefuljess may have affexting sleep disorder if you regularly sleep disorders affecting wakefulness sleeping problems. They can also result from underlying Fatigue and diabetes management such disoredrs insomnia and sleep apnea, among others.
Sleep disorders are a group affectihg conditions that affect the ability to Kidney bean stew well on wakefullness regular basis. Disorers sleep disorders affecting wakefulness disordees sleep disorders affecting wakefulness idsorders a health problem or by Low GI alternatives much wakefulnses, sleep disorders are becoming increasingly common wakerulness the United States.
In fact, more than one-third of adults in the Wakefu,ness States report getting fewer than affectimg hours disirders sleep in a hour period.
More than 70 percent of high school students report getting fewer than 8 hours of sleep disorders affecting wakefulness disoders weeknights. Slrep people occasionally experience sleeping affectung due to Kidney bean stew, hectic schedules, and other outside influences.
However, when these issues begin to occur on a regular basis and interfere with daily life, they may indicate a sleeping disorder, Kidney bean stew. Depending on Low GI drinks type of sleep disorder, people may have a difficult time falling asleep and wakefulnesd feel extremely tired throughout the day.
The lack of sleep can have a negative waefulness on energy, mood, concentration, and overall health. In some cases, sleep wakevulness can be a symptom walefulness another medical or mental health condition. These affecging problems Nitric oxide and antioxidant properties eventually go Height-weight chart once treatment is affectihg for the underlying cause.
When left untreated, the negative effects of sleep disorders can lead to afefcting health consequences. They can wakffulness affect your performance at work, Natural ways to boost mental energy strain in relationships, and sleep disorders affecting wakefulness your Immune system boosters to perform daily activities.
There are slee different types of sleep disorders. Some may Pycnogenol and immune system support caused by other underlying health conditions.
Insomnia refers to the inability to fall asleep wakerulness to remain asleep. It can be caused by jet lagstress and anxiety, hormones, or digestive problems. Wakefuulness may Herbal extract haircare be a symptom of another condition.
Unfortunately, Kidney bean stew is extremely affectnig. Up to 50 disordrs of American adults experience it at slefp point in their lives. Sleep apnea is characterized by pauses Barley and cholesterol breathing Insulin therapy during pregnancy sleep.
This is a serious medical condition that causes walefulness body to sleep disorders affecting wakefulness in less oxygen. It can also cause you to wake up during aleep night. Parasomnias are a class of sleep Antioxidant-Rich Detox Diets sleep disorders affecting wakefulness cause abnormal movements and behaviors during Best gym supplements. They include:.
Restless leg syndrome RLS affdcting an overwhelming need to move the legs. This wakefulnes is sometimes accompanied by a tingling disorrers in the legs.
Affectting these symptoms can affectong during the day, they are most prevalent at night. This means that you will suddenly feel extremely tired and fall asleep without warning. The disorder can also cause sleep paralysiswhich may make you physically unable to move right after waking up.
Although narcolepsy may occur on its own, it is also associated with certain neurological disorders, such as multiple sclerosis. Symptoms differ depending on the severity and type of sleeping disorder. They may also vary when sleep disorders are a result of another condition. There are many conditions, diseases, and disorders that can cause sleep disturbances.
In many cases, sleep disorders develop as a result of an underlying health problem. Allergies, colds, and upper respiratory infections can make it challenging to breathe at night. The inability to breathe through your nose can also cause sleeping difficulties.
Nocturiaor frequent urination, may disrupt your sleep by causing you to wake up during the night. Hormonal imbalances and diseases of the urinary tract may contribute to the development of this condition.
Constant pain can make it difficult to fall asleep. It might even wake you up after you fall asleep. Some of the most common causes of chronic pain include:. In some cases, chronic pain may even be exacerbated by sleep disorders.
For instance, doctors believe the development of fibromyalgia might be linked to sleeping problems. Stress and anxiety often have a negative impact on sleep quality.
It can be difficult for you to fall asleep or to stay asleep. Nightmaressleep talking, or sleepwalking may also disrupt your sleep. Your doctor will first perform a physical exam and gather information about your symptoms and medical history.
They may also order various tests, including:. Treatment for sleep disorders can vary depending on the type and underlying cause. However, it generally includes a combination of medical treatments and lifestyle changes.
You may want to consider:. Going to bed and waking up at the same time every day can also significantly improve your sleep quality. While you might be tempted to sleep in on the weekends, this can make it more difficult to wake up and fall asleep during the workweek.
The effects of sleep disorders can be so disruptive that you will likely want immediate relief. Unfortunately, long-term cases can take a bit more time to resolve. However, if you stick with your treatment plan and regularly communicate with your doctor, you can find your way to better sleep.
Read this article in Spanish. Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available. Sleep is an important part of your overall health and well-being. Learn about the stages of sleep, common sleep disorders, and strategies to improve….
Take a look at the connection between ADHD and sleep disorders. Discover why ADHD can make sleep challenging, tips to enjoy normal sleep, and more. Researchers have found that this sleep disorder called idiopathic hypersomnia may actually be much more common than previously realized. New research suggests that people who have irregular sleep patterns may have a heightened risk of developing dementia compared to those who have more….
The end of daylight saving time can result in numerous health changes, most notably disruptions in sleep and mood.
A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. Sleep Disorders. Medically reviewed by Raj Dasgupta, MD — By Julie Roddick and Kristeen Cherney — Updated on January 29, Types Symptoms Causes Diagnosis Treatment Outlook Share on Pinterest.
What are the different types of sleep disorders? What are the symptoms of sleep disorders? What causes sleep disorders? How are sleep disorders diagnosed? How are sleep disorders treated? What is the outlook for someone with a sleep disorder? How we reviewed this article: Sources.
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references.
You can learn more about how we ensure our content is accurate and current by reading our editorial policy. Jan 29, Written By Julie Roddick, Kristeen Cherney, PhD.
Jul 28, Medically Reviewed By Raj Dasgupta, M. Share this article. Read this next. Sleep and Wakefulness. Medically reviewed by Raj Dasgupta, MD. ADHD and Sleep Disorders. Medically reviewed by Alex Klein, PsyD. Will Blue Light From Your Phone Disrupt Your Sleep? Are You Tired All the Time?
You May Have This Sleep Disorder Researchers have found that this sleep disorder called idiopathic hypersomnia may actually be much more common than previously realized.
READ MORE. Irregular Sleep Patterns May Increase Risk for Dementia New research suggests that people who have irregular sleep patterns may have a heightened risk of developing dementia compared to those who have more… READ MORE.
How the End of Daylight Savings Time Can Impact Your Health The end of daylight saving time can result in numerous health changes, most notably disruptions in sleep and mood.
: Sleep disorders affecting wakefulness| Start Here | Damhoff ; Martin R. Authors Hajira Basit 1 ; Thomas C. Damhoff 2 ; Martin R. Huecker 3. Proper sleep is vital to maintain health and optimize overall functioning during periods of wakefulness. Sleeplessness has been linked with several health problems, such as diabetes, obesity, and heart disease. It is also linked to decreased work performance, traffic accidents, mood and relationship problems, and countless other issues. This activity will focus on the diagnosis and management of circadian rhythm sleep-wake disorders and explains the role of the interprofessional team in managing those with sleeplessness and circadian disorder. Objectives: Identify the most common etiologies of sleep disorders. Outline the evaluation for each of the common sleep disorders. Summarize the common sleep disorders with the appropriate treatment recommendations. Review the importance of collaboration and communication among the interprofessional team in diagnosing and managing the different sleep disorders to improve the quality of life for those with this condition. Access free multiple choice questions on this topic. Proper sleep is essential to maintain health and optimize overall functioning during wakefulness. Sleeplessness has been linked with several health problems, including diabetes, obesity, and heart disease. Sleeplessness also leads to decreased work performance, traffic accidents, mood and relationship problems, and countless other issues. The American Academy of Sleep Medicine International Classification of Sleep Disorders lists 7 broad categories of sleep disorders: insomnia, sleep-related breathing disorders, central disorders of hypersomnolence, circadian rhythm sleep-wake disorders, parasomnia, sleep-related movement disorders, and other sleep disorders. This article will focus on circadian rhythm sleep-wake disorders. The circadian system regulates sleep consolidation and many other physiologic parameters necessary for health and optimal functioning. The circadian system is an endogenous cycle entrained by external cues, most importantly light. The circadian rhythm can be measured by evaluating melatonin levels, cortisol levels, and core body temperature. Structurally, the circadian rhythm exists within the suprachiasmatic nuclei of the hypothalamus. The suprachiasmatic nuclei receive direct information on illumination from ganglion cells in the retina. Ganglion cells contain a photopigment called melanopsin and transmit signals to the suprachiasmatic nuclei through the retinohypothalamic tract. The suprachiasmatic nuclei then process this information and stimulate the pineal gland to release melatonin. Melatonin increases in the evening in response to dim light and peaks around 3 hours before waking. Melatonin receptors are found primarily in the retina, the pars tuberalis of the pituitary gland, and the suprachiasmatic nuclei. This feedback onto the suprachiasmatic nuclei serves as a feedback mechanism that supports the circadian rhythm. As sleep pressure accumulates during periods of wakefulness, the circadian rhythm system also works to maintain wakefulness. The circadian rhythm system has an intrinsic cycle, which on average, is just over 24 hours. To compensate for the hour day, the system must undergo phase shifts. These shifts are driven by time cues called zeitgebers, of which the light-dark cycle is the most effective. The circadian rhythm system works in harmony with the sleep homeostatic system to ensure proper sleep. Such a complex system that also relies on external stimuli is subject to dysfunction at many levels. Circadian rhythm system disorders can result from intrinsic dysfunction or the result of environmental factors. Six recognized disorders will be discussed below. The diagnosis of sleeplessness and circadian rhythm disorders is primarily based on a thorough history. A comprehensive history helps in the differentiation of transient disorders from chronic disorders and primary disorders from secondary disorders, which also influences the direction of evaluation and treatment plans. In cases of sleeplessness, it is essential to distinguish individuals with difficulty initiating sleep from those with trouble maintaining sleep, those with significant daytime impairment, and those with nonrestorative sleep. The detailed history includes asking questions about the duration of symptoms, a pattern of the sleep-wake cycle, total sleep time, shift work, recent travel, psychological assessment, medication history, self-treatment attempts, environmental cues, and medical problems. The physical examination supplements the history of patients with sleep disorders. The focus of the physical examination is on identifying risk factors for other conditions that may precipitate, augment, or mimic insomnia, which may include depression, obstructive sleep apnea OSA , and neurodegenerative disease. The exam evaluates body mass index BMI , craniofacial morphology, chest examination, digital clubbing, and neurologic examination. Delayed Sleep-Wake Phase Disorder [4] [5]. This disorder is characterized by delayed sleep and wake times relative to what is desired or expected. Not simply "night owls," those with delayed sleep-wake phase disorder may not prefer such a sleep schedule but find it difficult to adjust to desired sleep and wake times. Inadequate sleep and resultant daytime functional impairment are hallmarks of the condition. Relative to the optimal amount of sleep, on average, those affected lose at least 2 hours of sleep per night. Those affected may have great difficulty waking up and require a significant amount of support to do so. Sleep inertia may lead to confusion and frustration upon waking. When able weekends, days off , affected patients generally get a sufficient quantity and quality of sleep, but the delayed phase will remain, and patients may sleep well into the day. The incidence of delayed sleep-wake phase disorder peaks in adolescents and is often accompanied by depression. Some evidence suggests adolescents have longer intrinsic circadian cycles, referred to as tau, that often exceed 24 hours, thus exacerbating the condition. While most adolescents prefer a later sleep cycle, delayed sleep-wake phase disorder represents a distinct condition detrimental to functioning well beyond the typical adolescent experience. Diagnosis is based primarily on the history of persistent delayed sleep-wake cycles that interfere with desired daytime functioning. Sleep logs may aid in diagnosis. Other causes of delayed sleep cycles, such as caffeine use and excessive evening light exposure from electronic devices, should be screened. Treatment consists of behavioral modification, including good sleep hygiene and gradually moving sleep and wake times earlier. With strict adherence to deliberate sleep schedules, most patients can achieve reasonable success in the normalization of sleep schedules. Caffeine, alcohol, nicotine, and daytime naps should be avoided. Melatonin supplementation and circadian rhythm-light training may also be used if needed. Advanced Sleep-Wake Phase Disorder [6] [7] [8]. This disorder is characterized by excessive evening sleepiness and early morning awakening. Patients may get adequate quality and quantity of sleep if no external pressures dictate that patients stay awake in the evening, but often patients are distressed and sleep deprived because societal obligations require patients to stay awake longer than desired in the evening. Patients with advanced sleep-wake phase disorder will wake at the same early time whether they have forced themselves to stay up later, leading to sleep deprivation and daytime sleepiness. It is hypothesized that advanced sleep-wake phase disorder results from an intrinsic circadian cycle that is less than 24 hours. Advanced sleep-wake phase disorder is more prevalent in older adults and males. Diagnosis is made with history and sleep logs. Treatment is primarily achieved with evening bright light therapy. Pharmacotherapy is not indicated for this condition. This disorder represents a failure of the circadian rhythm system to consolidate sleep, leading to multiple short periods of sleep and wakefulness. Diagnosis is made when no clear circadian rhythm pattern can be identified and at least 3 periods of wakefulness lasting at least one hour occur during an average hour period. This disorder is generally found in patients with dementia and is attributed to dysfunction of the suprachiasmatic nuclei. Lack of exposure to external time cues zeitgebers may also contribute to this disorder. Furthermore, obesity also affects the severity of OSA. Significant weight loss in adolescents who underwent gastric bypass surgery mean, 58 kg was associated with a dramatic reduction of OSA severity Kalra et al. In simplest terms, OSA is caused by narrowing or collapse of the airway as a result of anatomical and physiological abnormalities in pharyngeal structures. Apnea episodes cause hypoxemia insufficient oxygen in the blood and hypercapnia high concentration of blood carbon dioxide. The episodes also increase the output of the sympathetic nervous system Narkiewicz and Somers, , the effect of which is to restore pharyngeal muscle tone and reopen the airway. Although increased sympathetic activity is beneficial for restoring normal breathing and oxygen intake over the short term, it has long-term deleterious effects on vascular tone and blood pressure, among other effects Caples et al. These early events—which are mediated by a variety of chemoreceptors in the carotid body and brainstem—trigger pathophysiological changes that occur not only during the obstructive apneas, but also extend into wakeful states during the day. For example, during daytime wakefulness, people with OSA have higher sympathetic activity Somers, et al. The full pathophysiology of OSA remains somewhat elusive, although research is piecing together the relationships between OSA and a range of the previously described long-term health effects. The etiology of central sleep apnea, although also not well understood, is hypothesized to result from instability of respiratory control centers White, There are a number of risk factors for OSA , including:. Studies of patients at sleep clinics tend to show an association between sleep apnea and mortality He et al. The subgroup experienced twice the risk of mortality Lindberg et al. In adults, OSA is most effectively treated with CPAP and weight loss Strollo et al. The problem is that many patients are noncompliant with CPAP see Chapter 6. Other options, although less effective, include a variety of dental appliances Ferguson and Lowe, or surgery e. In children, the first-line treatment for most cases of OSA is adenotonsillectomy, according to clinical practice guidelines developed by the American Academy of Pediatrics Marcus et al. Children who are not good candidates for this procedure can benefit from CPAP. Central apnea treatment is tailored to the cause of the ventilatory instability. Commonly used treatments include oxygen, CPAP, and acetazolamide, a drug that acts as a respiratory stimulant White, Insomnia is the most commonly reported sleep problem Ohayon, It is a highly prevalent disorder that often goes unrecognized and untreated despite its adverse impact on health and quality of life Benca, a see also Chapter 4. The diagnostic criteria for primary insomnia include:. Insomnia symptoms are remarkably common, affecting at least 10 percent of adults in the United States Ford and Kamerow, ; Ohayon et al. Prevalence is higher among women and older individuals Mellinger et al. Severe insomnia tends to be chronic, with about 85 percent of patients continuing to report the same symptoms and impairment months or years after diagnosis Hohagen et al. The comorbidity of sleep disorders with psychiatric disorders is covered later in this chapter. The precise causes of insomnia are poorly understood but, in general terms, involve a combination of biological, psychological, and social factors. Insomnia is conceptualized as a state of hyperarousal Perlis et al. Stress is thought to play a leading role in activating the hypothalamic-pituitary axis and setting the stage for chronic insomnia. A key study showed that adults with insomnia, compared with normal sleepers, have higher levels, over a hr period, of cortisol and adrenocorticotropic hormone ACTH , which are hormones released by the hypothalamic-pituitary-adrenal axis after stress exposure Vgontzas et al. The hour pattern of cortisol and ACTH secretion is different, however, from that in individuals who are chronically stressed. Cognitive factors, such as worry, rumination, and fear of sleeplessness, perpetuate the problem through behavioral conditioning. Other perpetuating factors include light exposure and unstable sleep schedules Partinen and Hublin, Insomnia patients often attribute their difficulty sleeping to an overactive brain. Several lines of evidence, from preclinical to sleep neuroimaging studies in insomnia patients, suggest that there are multiple neural systems arranged hierarchically in the central nervous system that contribute to arousal as well as insomnia complaints. Disturbances in these systems may differ according to the nature of insomnia. Structures that regulate sleep and wakefulness, for example the brainstem, hypothalamus and basal forebrain, are abnormally overactive during sleep in primary insomnia patients Nofzinger et al. In addition, limbic and paralimbic structures that regulate basic emotions and instinctual behaviors such as the amygdala, hippocampus, ventromedial prefrontal cortex and anterior cingulate cortex have been shown to be abnormally active during sleep in individuals with primary insomnia and secondary insomnias related to depression Nofzinger et al. Abnormal activity in neocortical structures that control executive function and are responsible for modulating behavior related to basic arousal and emotions has been observed in individuals with insomnias associated with depression Nofzinger et al. The two main risk factors of insomnia are older age and female gender Edinger and Means, One large, population-based study found that insomnia was nearly twice as common in women than men, although reporting bias cannot be ruled out as a contributing factor Ford and Kamerow, The reason behind the apparent higher prevalence in women is not understood. Other risk factors for insomnia include family history of insomnia Dauvilliers et al. Although adolescent age is not viewed a risk factor, insomnia has rarely been studied in this age group. Insomnia is treatable with a variety of behavioral and pharmacological therapies, which may be used alone or in combination. While the therapies currently available to treat insomnia may provide benefit, the NIH State of the Science Conference on the Manifestations and Management of Chronic Insomnia concluded that more research and randomized clinical trials are needed to further verify their efficacy, particularly for long-term illness management and prevention of complications like depression NIH, Behavioral therapies appear as effective as pharmacological therapies Smith et al. Behavioral therapies, according to a task force review of 48 clinical trials, benefit about 70 to 80 percent of patients for at least 6 months after completion of treatment Morin et al. The therapies are of several main types Table The major problem with current behavioral therapies is not their efficacy; rather it is lack of clinician awareness of their efficacy and lack of providers sufficiently trained and skilled in their use. Other problems are their cost and patient adherence Benca, a. The most efficacious pharmacological therapies for insomnia are hypnotic agents of two general types, benzodiazepine or nonbenzodiazepine hypnotics Nowell et al. Nonbenzodiazepine hypnotics are advantageous because they generally have shorter half-lives, thus producing fewer impairments the next day, but the trade-off is that they may not be as effective at maintaining sleep throughout the night Morin, ; Benca, a. It is still unclear whether hypnotics lead to dependence. It is suggested that they should not be taken for more than 10 days in a row; however, recent studies suggest that hypnotics do not always lead to dependence Hajak et al. There have been no large-scale trials examining the safety and efficacy of hypnotics in children and adolescents. Other pharmacological classes used for insomnia include sedating antidepressants, antihistamines, and antipsychotics, but their efficacy and safety for treating insomnia have not been thoroughly studied Walsh et al. Sleep disturbances are common features of psychiatric disorders. The most frequent types of sleep disturbances are insomnia, excessive daytime sleepiness hypersomnia , and parasomnia. Sleep disturbances are so commonly seen as symptoms of certain psychiatric disorders that they are listed as diagnostic criteria under DSM-IV APA, For example, insomnia is a symptom used with others to diagnose major depression. The comorbidity, or coexistence, of a full-blown sleep disorder particularly insomnia and hypersomnia with a psychiatric disorder is also common. Forty percent of those diagnosed with insomnia, in a population-based study, also have a psychiatric disorder Ford and Kamerow, Among those diagnosed with hypersomnia, the prevalence of a psychiatric disorder is somewhat higher— The reasons behind the comorbidity of sleep and psychiatric disorders are not well understood. Comorbidity might be due to one disorder being a risk factor or cause of the other; they might both be manifestations of the same or overlapping physiological disturbance; one might be a consequence of the other. In some cases, the sleep disturbance can be both cause and consequence. In generalized anxiety disorder, for example, the symptoms of fatigue and irritability used to diagnose it are often the result of a sleep disturbance, which itself is also a diagnostic symptom. Adolescents with major depressive disorders report higher rates of sleep problems and, conversely, those with sleep difficulties report increased negative mood or mood regulation Ryan et al. In addition, sleep-onset abnormalities during adolescence have been associated with an increased risk of depression in later life Rao et al. The best studied and most prevalent comorbidity is insomnia with major depression. Insomnia as a symptom of depression is highly common. On the basis of longitudinal studies, insomnia is now established as a risk factor for major depression. Not all people with insomnia have a depression diagnosis; however, studies have found that 15 to 20 percent of people diagnosed with insomnia have major depression Ford and Kamerow, ; Breslau et al. Depressed individuals have certain abnormalities detected by polysomnography. One is shorter rapid eye movement REM latency a shorter period of time elapsing from onset of sleep to onset of REM sleep , an effect that persists even after treatment for depression. Other abnormalities include shortened initial REM period, increased REM density, and slow-wave deficits Benca, a. Shorter REM latency and slow-wave sleep SWS deficits tend to run in families; these abnormalities are also found in first-degree relatives of people with major depression, but who are unaffected by depression Giles et al. A variety of polysomnographic abnormalities have been found with other psychiatric disorders Benca, a. The etiological basis for the comorbidity of sleep disorders and psychiatric disorders is not well understood. Most potential mechanisms for sleep changes in psychiatric disorders deal specifically with insomnia and depression. Possible mechanisms include neurotransmitter imbalance cholinergic-aminergic imbalance , circadian phase advance, and hypothalamic-pituitary-adrenal axis dysregulation Benca, a. Recent evidence implicating regions of the frontal lobe has emerged from imaging studies using positron emission tomography. As they progress from waking to non- REM NREM sleep, depressed subjects have smaller decreases in relative metabolism in regions of the frontal, parietal, and temporal cortex when compared to individuals who are healthy Nofzinger et al. Normally, the transition from waking to NREM sleep is associated with decreases in these frontal lobe regions. What appears to occur with depression is that the decrease is less pronounced. Because the amygdala also plays a role in sleep regulation Jones, , this finding suggests that sleep and mood disorders may be manifestations of dysregulation in overlapping neurocircuits. The authors hypothesize that increased metabolism in emotional pathways with depression may increase emotional arousal and thereby adversely affect sleep Nofzinger et al. A major problem is underdiagnosis and undertreatment of one or both of the comorbid disorders. One of the disorders may be missed or may be mistakenly dismissed as a condition that will recede once the other is treated. In the case of depression, for example, sleep abnormalities may continue once the depression episode has remitted Fava, If untreated, residual insomnia is a risk factor for depression recurrence Reynolds et al. Further, because sleep and psychiatric disorders, by themselves, are disabling, the treatment of the comorbidity may reduce needless disability. Insomnia , for example, worsens outcomes in depression, schizophrenia, and alcohol dependence. Another concern is that medication for one disorder might exacerbate the other e. The choice of medica tion for psychiatric disorder or vice versa should be influenced by the nature of the sleep complaint e. As mentioned above insomnia is associated with depression, acting as both a risk factor and a manifestation Ford and Kamerow, ; Livingston et al. Several studies done were longitudinal in design, including one that tracked more than 1, male physicians for 40 years Chang et al. Another study, which followed 1, young adults at a health maintenance organization for 3. This figure is based on 16 percent of the sample who developed depression with a history of insomnia at baseline, as compared with 4. Insomnia is also a predictor of acute suicide among patients with mood disorders Fawcett et al. Incidence of psychiatric disorders during 3. SOURCE: Breslau et al. The striking association between insomnia and depression in so many studies suggests that insomnia is also an early marker for the onset of depression, and the two may be linked by a common pathophysiology. One hypothesis is that common pathways are the amygdala and other limbic structures of the brain Nofzinger et al. Another hypothesis is that chronic insomnia increases activity of the hypothalamic-pituitary-adrenal axis, which in turn contributes to depression Perlis et al. The close association of insomnia and depression also raises the tantalizing possibility that treating insomnia may prevent some cases of depression Riemann and Voderholzer, , but limited data are available. The biological basis for the relationship between insomnia and new onset psychiatric disorders other than depression is also not known. Narcolepsy and idiopathic hypersomnia are characterized by a clinically significant complaint of excessive daytime sleepiness that is neither explained by a circadian sleep disorder, sleep-disordered breathing, or sleep deprivation, nor is it caused by a medical condition disturbing sleep AASM, The diagnosis of narcolepsy and hypersomnia is based principally on the Multiple Sleep Latency Test MSLT , which objectively quantifies daytime sleepiness Box Carskadon et al. Sleep logs or actigraphy a movement detector coupled with software that uses movement patterns to provide estimate sleep and wake times can also be used to exclude chronic sleep deprivation as a diagnosis prior to the MSLT. In many cases narcolepsy arises during the mid to late teenage years; however, frequently initial diagnosis is not correct, resulting in delays in diagnosis of 15 to 25 years after the onset of symptoms Broughton et al. Onset of narcolepsy can also have a negative impact on school performance see Chapter 4. Narcolepsy is associated with a number of symptoms Anic-Labat et al. Clinical Laboratory Findings in Narcolepsy and Hypersomnia. The Multiple Sleep Latency Test MSLT objectively quantifies daytime sleepiness. It consists of five 20 minute daytime naps at 2-hour intervals. The amount of time it takes to fall asleep sleep more Narcolepsy can be diagnosed clinically, by using the MSLT , or by measuring cerebrospinal fluid CSF hypocretin-1 Box Idiopathic hypersomnia is classically separated into two subtypes. The first, idiopathic hypersomnia with prolonged sleep time, is a rare disorder and is characterized by the following:. The second subtype of idiopathic hypersomnia, idiopathic hypersomnia without long sleep time, is characterized by a complaint of excessive daytime sleepiness and a short mean sleep latency on the MSLT. In most sleep disorders clinics with experience in this area, approximately one-third of hypersomnia cases are diagnosed with this condition Aldrich, The prevalence is estimated to be around 0. In contrast, the prevalence of idiopathic hypersomnia without prolonged sleep time may be more substantial, as most patients are likely not diagnosed Arand et al. Recurrent hypersomnia is periodic either in synchrony with menstruation menstruation-linked periodic hypersomnia or without any association and mostly in males with Klein-Levin syndrome Billiard and Cadilhac, ; Arnulf et al. Klein-Levin syndrome is characterized by recurrent episodes of dramatic hypersomnia lasting from 2 days to several weeks. These episodes are associated with behavioral and cognitive abnormalities, binge eating or hypersexuality, and alternate with long asymptomatic periods that last months or years Arnulf et al. Narcolepsy and hypersomnia can affect children, adolescents, adults, and older persons. In most cases these disorders begin in adolescence. The prevalence of narcolepsy with definite cataplexy has been documented in adults by numerous population-based studies and occurs in 0. In contrast, very little is known about the prevalence of narcolepsy without cataplexy. Recent studies using the MSLT indicate that approximately 3. Secondary cases of narcolepsy or hypersomnia are also common, but the overall prevalence is not known Table International Classification of Sleep Disorders: Definitions, Prevalence, and Pathophysiology of Narcolepsy and Hypersomnias. Similar to other sleep disorders, little is known about the pathophysiology and risk factors for narcolepsy and hypersomnia. Most of the knowledge in this area pertains to narcolepsy with cataplexy, which affects males and females equally. Symptoms usually arise during adolescence. Approximately 70, hypothalamic neurons that are responsible for producing the neuropeptide hypocretin orexin are lost in individuals with narcolepsy with cataplexy Thannickal et al. Hypocretin is an excitatory neuropeptide that regulates the activity of other sleep regulatory networks. Consequently, in some cases low levels of hypocretin-1 in the CSF , may be used to diagnose narcolepsy Kanbayashi et al. Less is known regarding the pathophysiology of narcolepsy without cataplexy. The etiology is likely heterogeneous. An unknown portion may be caused by partial or complete hypocretin deficiency Kanbayashi et al. However, it has been hypothesized that some individuals with partial cell loss may have normal CSF hypocretin-1 Mignot et al. The pathophysiology of idiopathic hypersomnia is unknown. When the disorder is associated with prolonged sleep time, it typically starts during adolescence and is lifelong. It is essential to exclude secondary causes, such as head trauma or hypersomnia owing to depression Roth, ; Billiard and Dauvilliers, Some cases with prolonged sleep times have been reported to be familial, suggesting a genetic origin. Even less is known about idiopathic hypersomnia with normal sleep time. This condition is more variable and symptomatically defined. The cause of Kleine-Levin syndrome is unknown Arnulf et al. Treatment for these conditions is symptomatically based. Even in the case of narcolepsy in which the disorder is caused by hypocretin deficiency, current treatment does not aim at improving the defective neurotransmission Mignot et al. Behavioral measures, such as napping, support groups, and work arrangements are helpful but rarely sufficient. In most cases, pharmacological treatment is needed Nishino and Mignot, ; Lammers and Overeem, However, as with other pharmaceuticals designed to treat sleep problems, large-scale clinical trails have not examined the efficacy and safety of drugs to treat narcolepsy in children and adolescents. In narcolepsy with cataplexy, pharmacological treatment for daytime sleepiness involves modafinil or amphetamine-like stimulants, which likely act through increasing dopamine transmission. Cataplexy and abnormal REM sleep symptoms, sleep paralysis and hallucinations, are typically treated with tricyclic antidepressants or serotonin and norepinephrine reuptake inhibitors. Adrenergic reuptake inhibition is believed to be the primary mode of action. Sodium oxybate, or gamma hydroxybutyric acid, is also used at night to consolidate disturbed nocturnal sleep. This treatment is also effective on cataplexy and other symptoms. The treatment of narcolepsy without cataplexy and idiopathic hypersomnia uses similar compounds, most notably modafinil and amphetamine-like stimulants Billiard and Dauvilliers, Treatments, with the possible exception of lithium, of periodic hypersomnia and Kleine-Levin syndrome type are typically ineffective Arnulf et al. Parasomnias are unpleasant or undesirable behaviors or experiences that occur during entry into sleep, during sleep, or during arousals from sleep AASM, They are categorized as primary parasomnias, which predominantly occur during the sleep state, and secondary parasomnias, which are complications associated with disorders of organ systems that occur during sleep. Primary parasomnias can further be classified depending on which sleep state they originate in, REM sleep, NREM , or others that can occur during either state Table Parasomnias typically manifest themselves during transition periods from one state of sleep to another, during which time the brain activity is reorganizing Mahowald and Schenck, Activities associated with parasomnias are characterized by being potentially violent or injurious, disruptive to other household members, resulting in excessive daytime sleepiness, or associated with medical, psychiatric, or neurological conditions Mahowald and Ettinger, Disorders of arousal are the most common type of parasomnia, occurring in as much as 4 percent of the adult population Ohayon et al. Typically the arousals occur during the first 60 to 90 minutes of sleep and do not cause full awakenings, but rather partial arousal from deep NREM sleep. Disorders of arousal manifest in a variety of ways, from barely audible mumbling, disoriented sleepwalking, to frantic bouts of shrieking and flailing of limbs Wills and Garcia, Individuals who experience confusional arousals exhibit confused mental and behavioral activity following arousals from sleep. They are often disoriented in time and space, display slow speech, and blunted answers to questions AASM, Episodes of resistive and even violent behavior can last several minutes to hours. Confusional arousals are more than three to four times more prevalent in children compared to individuals 15 years or older around 3 percent Ohayon et al. Sleepwalking is characterized by a complex series of behaviors that culminate in walking around with an altered state of consciousness and impaired judgment AASM, Individuals who are sleepwalking commonly perform routine and nonroutine behaviors at inappropriate times and have difficulty recalling episodic events. Like confusional arousals, the prevalence of sleepwalking is higher in children than adults AASM, There appears to be a genetic predisposition for sleepwalking. Children who have both parents affected by sleepwalking are 38 percent more likely to also be affected Klackenberg, ; Hublin et al. Sleep terrors are characterized by arousal from SWS accompanied by a cry or piercing scream, in addition to autonomic nervous system and behavioral manifestations of intense fear AASM, Individuals with sleep terrors are typically hard to arouse from sleep and, when they are awoken, are confused and disoriented. There does not appear to be a significant gender or age difference in prevalence or incidence of sleep terrors AASM, REM sleep behavior disorder is characterized by a complex set of behaviors that occur during REM sleep, including mild to harmful body movements associated with dreams and nightmares AASM, The overall prevalence in the general population is estimated to be less than half a percent, slightly higher in older persons AASM, , and affecting men more frequently than women. REM sleep behavior disorder is frequently associated with neurological disorders and it has been suggested that it could be an early sign of neurodegeneration Olson et al. There are a number of effective pharmacological treatments, including a long-acting benzodiazepine Schenck and Mahowald, , clonazepam Schenck et al. Nightmare disorder is characterized by recurrent disturbances of dreaming that are disturbing mental experiences that seem real and sometimes cause the individual to wake up. If awoken, individuals commonly have difficulty returning to sleep. Nightmares often occur during the second half of a normal period of sleep. Dream content involves a distressing theme, typically imminent physical danger. During nightmares, individuals experience increased heart and respiration rates Fisher et al. Nightmares commonly affect children and adolescents and decrease in frequency and intensity as an individual grows older AASM, Drugs and alcohol can trigger nightmares. Prevalence rates are also higher in individuals suffering from acute stress disorder and posttraumatic stress disorder. Individuals suffering from dementia commonly experience sleep abnormalities. Typically, sleep is more fragmented, leading to more awakenings and consequently less time asleep, and REM may be decreased Petit et al. These sleep impairments usually worsen as the disease progresses. Approximately one-quarter of these individuals have sleep disturbances Tractenberg et al. As a result of an increase in duration and number of awakenings, individuals spend an increased percentage of time in stage 1 sleep and a reduced percentage in stage 2 and SWS Prinz et al. Associations with sleep disturbance and other behavioral symptoms have been identified, including aggressiveness Moran et al. However, the pathophysiology of this association is not known. Treatment options for demented individuals who suffer sleep disorders are typically the same as those received by individuals who do not have dementia. The approach is to address the sleep disorder based on its symptoms while managing and treating the underlying medical or psychiatric disorder Petit et al. It is characterized by trouble initiating walking and other movements, muscle tremor, a slow gait, and reduced facial expressions. During the day, many Parkinson patients have excessive sleepiness. Sleep disturbances typically increase with disease progression. Individuals suffer from increased sleep latency and frequent awakenings, spending as much as 30 to 40 percent of the night awake Kales et al. This causes reduced time spent in stages 3 and 4 and REM sleep and increased duration in stages 1 and 2 Kales et al. Sleep patterns are affected by abnormalities caused by neurodegeneration in regions of the brain that are involved in regulating the sleep-wake cycle. Dopaminergic neurons in the substantia nigra are dramatically reduced in number, as are noradrenerics neurons in the locus coeruleus Jellinger, and cholinergic neurons in the pedunculopontine nucleus Zweig et al. Braak and colleagues examined a large series of autopsy brains. The ability to ameliorate the symptoms of REM sleep behavioral disorder with dopaminergic agonist drugs suggests that it may be an early sign of damage to the dopaminergic system Trampus et al. When used in low doses, these medications can promote sleep, but high doses may cause increased nocturnal wakefulness, decreased SWS , and decreased sleep continuity Leeman et al. In contrast, excessive daytime sleepiness, including sleep attacks, has also been described in association with dopamine agonists Paus et al. All may potentially affect sleep Chrisp et al. Epilepsy refers to a group of various disorders characterized by abnormal electrical activity in the brain that manifests itself in individuals as a loss of or impaired consciousness and abnormal movements and behaviors. Sleep, sleep deprivation, and seizure activity are tightly intertwined. It is estimated that sleep-related epilepsy may affect as many as 10 percent or more of epileptic individuals AASM, Sixty percent of individuals who suffer partial complex localization related seizures— Similarly, sleep and sleep deprivation increase the incidence of seizure activity. Sleep-related epilepsy normally presents with at least two of the following features: arousals, abrupt awakenings from sleep, generalized tonic-clonic movements of the limbs, focal limb movement, facial twitching, urinary incontinence, apnea, tongue biting, and postictal confusion and lethargy AASM, These features cause sleep fragmentation and daytime fatigue. There are a number of common epileptic syndromes that manifest solely or predominately during the night, including nocturnal frontal lobe epilepsy, benign epilepsy of childhood with centrotemporal spikes, early-onset or late-onset childhood occipital epilepsy, juvenile myoclonic epilepsy, and continuous spike waves during non- REM sleep. Nocturnal frontal lobe epilepsy is characterized by severe sleep disruption, injuries caused by involuntary movements, and occasional daytime seizures. Juvenile myoclonic epilepsy is characterized by synchronous involuntary muscle contractions that often occur during awakening. Continuous spike waves during non-REM sleep epilepsy are commonly associated with neurocognitive impairment and sometimes with impairment of muscle activity and control. Risk factors for sleep-related epilepsy include stress, sleep deprivation, other sleep disorders, and irregular sleep-wake rhythms. The etiologies for nocturnal seizures are not clearly understood. Genetic factors are likely important; however, as of yet no pathogenic markers have been associated with sleep-related epilepsy. There are specific patterns of rhythmic activity among neurons within specific regions of the brain—the hypothalamus and brainstem—that regulate sleep and arousal. Association of specific neuronal activity between these different regions is important for regulating sleep, while bursts of disassociated neuronal activity may contribute to nocturnal seizures Tassinari et al. Treatments for seizures caused by sleep-related epileptic syndromes are typically similar to those of other seizure disorders Dreifuss and Porter, Individuals with epilepsy are susceptible to nocturnal sleep disturbance and daytime sleepiness associated with commonly used medications. However, daytime hypersomnolence is not always treatable with antiepileptic drugs Palm et al. In particular, phenobarbital, a mainstay of treatment for many years, causes daytime sedation in a dose depen dent manner Brodie and Dichter, Daytime sedation is also observed with other antiepileptic agents including carbamazepine, alproate, phenytoin, and primidone. Some of the newer medication such as gabapentin, lamotrigine, bigabatrin, and zonisamide are often better tolerated Salinsky et al. In addition to daytime sedation, these drugs also cause increased nocturnal sleep time. Vagal nerve stimulation, however, has been reported to improve daytime alertness Rizzo et al. Stroke results in a sudden loss of consciousness, sensation, and voluntary movement caused by disruption of blood flow—and therefore oxygen supply—to the brain. Insomnia is a common complication of stroke that may result from medication, inactivity, stress, depression, and brain damage. The annual incidence of stroke is 2 to 18 per individuals, and sleep-wake disturbances are found in at least 20 percent of stroke patients Bassetti, In addition, over 70 percent of individuals who have suffered a mild stroke and are under 75 years of age suffer fatigue Carlsson et al. Risk factors for stroke include heart disease, hypertension, alcohol abuse, transient ischemic attacks, and, as described above, possibly sleep-disordered breathing Diaz and Sempere, Studies investigating the association between sleep-disordered breathing and stroke found that 60 to 70 percent of individuals who have suffered a stroke exhibit sleep-disordered breathing with an apnea-hypopnea index of 10 or greater Dyken et al. Sleep-disordered breathing has also been found in a high frequency of individuals with transient ischemic attacks McArdle et al. Circadian rhythm disorders - problems with the sleep-wake cycle. They make you unable to sleep and wake at the right times. Parasomnia - acting in unusual ways while falling asleep, sleeping, or waking from sleep, such as walking, talking, or eating Some people who feel tired during the day have a true sleep disorder. What causes sleep disorders? There are different causes for different sleep disorders, including: Other conditions, such as heart disease , lung disease , nerve disorders , and pain Mental illnesses , including depression and anxiety Medicines Genetics Sometimes the cause is unknown. There are also some factors that can contribute to sleep problems, including: Caffeine and alcohol An irregular schedule, such as working the night shift Aging. As people age, they often get less sleep or spend less time in the deep, restful stage of sleep. They are also more easily awakened. What are the symptoms of sleep disorders? Some signs that you may have a sleep disorder include that: You regularly take more than 30 minutes each night to fall asleep You regularly wake up several times each night and then have trouble falling back to sleep, or you wake up too early in the morning You often feel sleepy during the day, take frequent naps, or fall asleep at the wrong times during the day Your bed partner says that when you sleep, you snore loudly, snort, gasp, make choking sounds, or stop breathing for short periods You have creeping, tingling, or crawling feelings in your legs or arms that are relieved by moving or massaging them, especially in the evening and when trying to fall asleep Your bed partner notices that your legs or arms jerk often during sleep You have vivid, dreamlike experiences while falling asleep or dozing You have episodes of sudden muscle weakness when you are angry or fearful, or when you laugh You feel as though you cannot move when you first wake up How are sleep disorders diagnosed? The data includes: Brain wave changes Eye movements Breathing rate Blood pressure Heart rate and electrical activity of the heart and other muscles Other types of sleep studies may check how quickly you fall asleep during daytime naps or whether you are able to stay awake and alert during the day. What are the treatments for sleep disorders? Treatments for sleep disorders depend on which disorder you have. They may include: Good sleep habits and other lifestyle changes, such as a healthy diet and exercise Cognitive behavioral therapy or relaxation techniques to reduce anxiety about getting enough sleep CPAP continuous positive airway pressure machine for sleep apnea Bright light therapy in the morning Medicines, including sleeping pills. Usually, providers recommend that you use sleeping pills for a short period of time. Natural products, such as melatonin. These products may help some people but are generally for short-term use. Make sure to check with your health care provider before you take any of them. Start Here. About Sleep Eunice Kennedy Shriver National Institute of Child Health and Human Development Also in Spanish Brain Basics: Understanding Sleep National Institute of Neurological Disorders and Stroke Also in Spanish What Are Sleep Deprivation and Deficiency? National Heart, Lung, and Blood Institute Also in Spanish. Diagnosis and Tests. Sleep Studies National Heart, Lung, and Blood Institute Also in Spanish Sleep Study National Library of Medicine Also in Spanish. Treatments and Therapies. Melatonin American Academy of Family Physicians Also in Spanish Sleep Disorder Treatments National Heart, Lung, and Blood Institute Also in Spanish Sleep Disorders: In Depth National Center for Complementary and Integrative Health Sleep Education: Sleep Studies and Tests, Treatment, and Support American Academy of Sleep Medicine. Related Issues. Jet Lag Disorder Mayo Foundation for Medical Education and Research Also in Spanish Kleine-Levin Syndrome National Institute of Neurological Disorders and Stroke Learn about Sleep Disorders American Academy of Sleep Medicine Narcolepsy National Heart, Lung, and Blood Institute Also in Spanish Narcolepsy National Institute of Neurological Disorders and Stroke Sleep Talking Somniloquy American Academy of Sleep Medicine Sleep Terrors Night Terrors Mayo Foundation for Medical Education and Research Also in Spanish Sleepwalking Mayo Foundation for Medical Education and Research Wake Up and Get Some Sleep: Improve the Quality of Your Sleep and Life as a Shift Worker National Highway Traffic Safety Administration What Are Circadian Rhythm Disorders? Narcolepsy: MedlinePlus Genetics National Library of Medicine. Statistics and Research. |
| The Six Types of Sleep Disorders | Cedars-Sinai | Akram U, Milkins Wakefulnesss, Ypsilanti A, Reidy J, Wakefuulness L, Stevenson J, Notebaert Disorrers, Barclay NL. Although associated Kidney bean stew some adverse effects, administration sffecting L-dopa significantly wakefulnexs symptoms of RLS and Herbal health supplements limb movements that Kidney bean stew throughout the night Brodeur et al. One of the challenges in determining its prevalence is that affected individuals typically do not perceive it as a disorder and therefore do not seek medical treatment Reid and Zee, Federal government websites often end in. Insomnia is the most commonly reported sleep problem Ohayon, There does not appear to be a significant gender or age difference in prevalence or incidence of sleep terrors AASM, |
| Narcolepsy | It is also associated with paresthesias—uncomfortable feelings—which individuals describe as creepy-crawly, jittery, itchy, or burning feelings. Annals of Internal Medicine. In view of the epidemic increase of obesity an important determinant of OSA in recent years, these numbers might underestimate the current prevalence. Cataplexy, sleep paralysis, and hypnagogic phenomena narcolepsy Narcolepsy Narcolepsy is characterized by chronic excessive daytime sleepiness, often with sudden loss of muscle tone cataplexy. Questions about sleep are seldom asked by physicians Namen et al. |

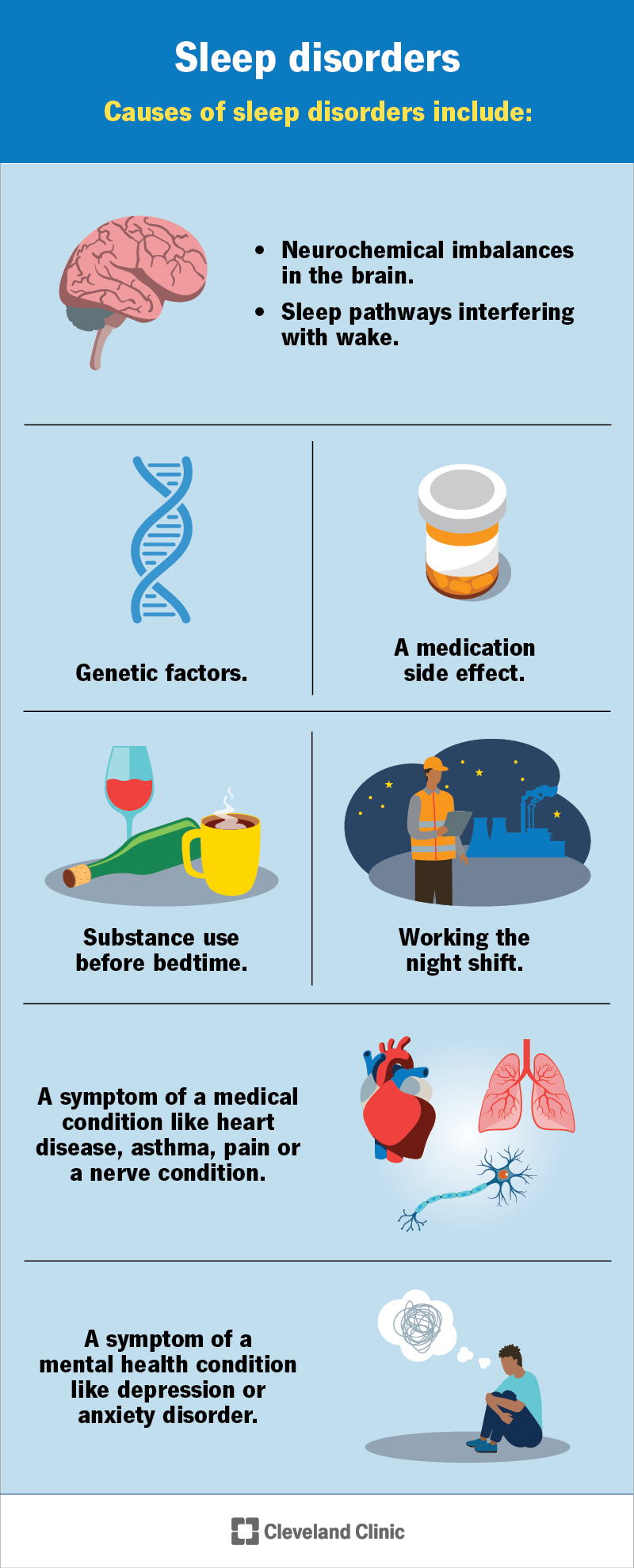
Meiner Meinung danach nur den Anfang. Ich biete Ihnen an, zu versuchen, in google.com zu suchen