Video
How to Prevent Blood Sugar and Triglyceride Spikes After MealsInflammation and blood sugar control -
The high extreme group included those who had at least two of the inflammatory markers in the highest quartile. The low extreme group, considered as the reference category in the analysis, included participants with all three inflammation markers below or equal to the median, and the intermediate group included individuals with all other possible combinations of cytokine levels.
Statistical analyses were performed using SAS software SAS Institute, Cary, NC. Among the 2, participants with complete information, Participants with diabetes were more likely to be male and black and had a lower level of education Table 1. Diabetic individuals had more cardiovascular diseases and peripheral arterial disease than their counterparts with NGT.
Plasma levels of inflammatory markers were moderately correlated. The correlation between IL-6 and TNF-α was 0. Table 2 shows the plasma concentrations of the inflammatory markers by diabetes and hyperglycemic status. Multivariate analyses on the risk of high inflammation associated with diabetes and hyperglycemic status are shown in Table 3.
Compared with those without diabetes, after adjustments for age, sex, race, smoking status, alcohol intake, education, and site, diabetic individuals continued to exhibit higher inflammation levels with an OR of 1. Diabetic women compared with those without diabetes had an OR of 2.
The association between diabetes and higher inflammation level was weakened by adjustments for body fat and visceral fat, inflammation, and diabetes comorbidities and potential confounders Table 3 , models 2 and 3 but still remained significant, except for high CRP in men.
Total body fat and visceral fat accounted for most of the attenuation of the association between diabetes and higher inflammation. Adjustment for body fat and visceral fat attenuated these associations so that only IL-6 remained statistically significant. Diabetic participants with poorer glycemic control also showed higher inflammatory levels of CRP with an OR of 1.
Adjustment for body fat and visceral fat attenuated the relationships, but they still remained statistically significant even with further adjustment for comorbidities and potential confounders.
The association between diabetes and a high level of inflammation remained even after adjustments for possible confounders, such as demographics, lifestyle habits, total body fat, visceral fat, and comorbidities. We also found that the association between diabetes and inflammation was stronger when we used a composite inflammation index of the three inflammatory markers, which is a more specific indicator of systemic inflammation Older diabetic individuals have a 2.
For the association between diabetes and CRP, we observed a sex difference; the association was stronger in women and not statistically significant in men.
This sex difference was not found with any of the other inflammatory markers. Our results are consistent with those for other cross-sectional studies in younger populations in which an increase of CRP was found with diabetes 5 , 7 , 8 and increases of CRP, IL-6, and TNF-α were found with IGT 22 , It has also been shown in several longitudinal studies that inflammation is a predictor of development of diabetes 9 , 10 , 12 , Thus, the link between diabetes and inflammation could be due to a reciprocal process, in that inflammation may contribute to diabetes onset and diabetes may then contribute to continued inflammation.
In addition, hyperglycemia is known to mediate formation of advanced glycosylation end products. These advanced glycosylation end products may also contribute to inflammation, producing a chronic stimulation for secretion of cytokines Adipose tissue could be a mediator in the relationship.
Data emerging over the past several years have established the fact that adipocytes express and secrete the cytokine TNF-α and that enlarged adipocytes from obese animals and humans overexpress this factor The findings from the Third National Health and Nutrition Examination Survey showed a higher prevalence of increased levels of CRP in both overweight and obese participants Adiposity, in particular visceral adipose tissue, has been found to be a key promoter of low-grade chronic inflammation 28 , Obesity appears to be a state of chronic inflammation with increased production of cytokines and other acute-phase reactants that play a crucial role in regulation of systemic insulin action; it has been shown that TNF-α—deficient mice show increased insulin action Is the elevation of inflammatory markers the result of vascular and renal disease due to diabetes or a causal pathway?
Numerous studies showed an association between cardiovascular diseases with inflammation, and a higher CRP level is associated with increased risk of development of vascular disease 31 — CRP and IL-6 are also known to increase with declining kidney function, even before end-stage renal disease occurs 35 — Trials to study decreases of inflammation in diabetes or cardiovascular disease events are still lacking.
A better understanding of the actions of cytokines with other factors in the pathogenesis of diabetes may lead to improved understanding of its cause and open new approaches for its prevention. We found an association between poor glycemic control and an increased level of CRP.
Several studies showed that cytokine levels CRP, IL-6, and TNF-α are related to glycemic control 38 — Improvement of glycemic control has an inconsistent beneficial impact on the level of inflammatory markers. No significant effect was found on the levels of IL-6 and TNF-α with sulfonylureas or insulin therapy, but a significant decrease in CRP was observed with insulin Troglitazone with an improvement in glycemic control reduces CRP 42 and decreases plasma levels of TNF-α in obese diabetic patients One weight loss study showed that moderate-intensity regular exercise decreases the TNF-α level A high inflammation level might contribute to the worsening of progression of type 2 diabetes in addition to glycemic control.
Our study has several strengths. First, we have several measures of inflammatory markers and can create an inflammatory index. Second, the study includes a large sample size and a biracial population with a high percentage of blacks.
One limitation of our study is that because of the study design cross-sectional study , the direction of these associations cannot be conclusively determined and a causal relationship cannot be inferred.
Additionally, the study population includes well-functioning relatively healthy participants; our findings may not be generalized to a frail older population.
Among those with diabetes, poorer glycemic control was associated with higher levels of CRP. Whether baseline levels of inflammatory markers in those without pre-diabetes or diabetes would be predictors of the onset of pre-diabetes and diabetes should be determined, and we plan to explore this in our longitudinal data.
Plasma levels of inflammatory markers of the diabetic and the hyperglycemic groups compared with the NGT group. For risk of high inflammation level associated with diabetes and hyperglycemic status, model 1 is adjusted on age, sex, race, smoking status, alcohol intake, education, and site.
Model 2 adds total body fat, visceral fat, and height. Model 3 adds cardiovascular diseases, hypertension, peripheral arterial disease, renal insufficiency, arthritis, pulmonary disease, anti-inflammatory, statin, and estrogen use.
For relationship between glycemic control and inflammation in diabetes, models 1 and 2 are the same and model 3 adds diabetes duration. This study was supported by Contracts NAG, NAG, and NAG from the National Institute on Aging. This research was supported in part by the Intramural Research Program of National Institutes of Health, National Institute on Aging.
A table elsewhere in this issue shows conventional and Système International SI units and conversion factors for many substances. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care.
Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 29, Issue 8. Previous Article Next Article. RESEARCH DESIGN AND METHODS. Article Information. Article Navigation. Cardiovascular and Metabolic Risk August 01 Diabetes, Hyperglycemia, and Inflammation in Older Individuals : The Health, Aging and Body Composition study Nathalie de Rekeneire, MD, MS ; Nathalie de Rekeneire, MD, MS.
This Site. Google Scholar. Rita Peila, PHD ; Rita Peila, PHD. Jingzhong Ding, PHD ; Jingzhong Ding, PHD. Lisa H. Colbert, PHD ; Lisa H. Colbert, PHD. Marjolein Visser, PHD ; Marjolein Visser, PHD.
Ronald I. Shorr, MD, MS ; Ronald I. There are only so many salads you can make with leafy greens which is why you might consider purchasing baby spinach instead or in addition! The tender leaves are ideal to toss as a salad, but they can also be stirred into hot stews, soups, entrees, and cooked whole-grains.
Loading up on non-starchy vegetables, like leafy greens, is also a good way to add more food to your plate without adding many calories or carbs. A two-cup serving also provides almost half of an adult's daily needs for vitamin C and beta-carotene which are two antioxidants that play key roles in reducing inflammation.
Use limited data to select advertising. Create profiles for personalised advertising. Use profiles to select personalised advertising. Create profiles to personalise content.
Use profiles to select personalised content. Measure advertising performance. Measure content performance. Understand audiences through statistics or combinations of data from different sources.
Develop and improve services. Use limited data to select content. List of Partners vendors. Just Tell Me What to Eat: Diabetes Edition. Healthy Eating for Diabetes. Special Diets Diabetes. By Carolyn Williams, Ph.
EatingWell's Editorial Guidelines. Reviewed by Dietitian EatingWell. She is a registered dietitian with a master's in food, nutrition and sustainability.
Reviewed by Dietitian Jessica Ball, M. Jessica Ball, M. Try Our Healthy and Delicious Diabetes Meal Plans. Try These Recipes That Are Rich in Omega-3 Fatty Acids. Was this page helpful? Thanks for your feedback!
Tell us why! You try to adjust it with food or activity or insulin, and it dips really low. Knowledge is power! Look out for these surprising triggers that can send your blood sugar soaring:. Watch out for other triggers that can make your blood sugar fall.
For example, extreme heat can cause blood vessels to dilate widen. That makes insulin absorb more quickly and could lead to low blood sugar. If an activity or food is new, check your blood sugar before and after to see how you respond. Skip directly to site content Skip directly to search. Español Other Languages.
Español Spanish Print.
Inflammation is a term Imflammation gets tossed out Inflammationn lot Inflmmation days, but what does it actually mean? And how does it Website performance monitoring trends your Recharge Anytime, Anywhere sugar? Fruits high in antioxidants everything cotrol need Inflammation and blood sugar control know about inflammation when you Inflammatoin diabetes. Inglammation Fruits high in antioxidants has contro Masters degree in Marketing from New York University, Vanessa's first true love is science. Always inquisitive, she sought out the help of a Registered Dietitian in in order to understand the role food plays in one's overall health and build a better relationship with food. Fast forward to the fall ofwhen she began her first class in the Nutrition and Food Studies program on her way to being a registered dietitian herself, hoping to make a positive impact on people as they navigate their way through understanding nutrition.Here's what Inflmmation eat Inflammation and blood sugar control help IInflammation inflammation and improve insulin ssugar. Carolyn Williams, Ph. Glood writes for a variety Heart health programs online and print publications on health cintrol ranging from sleep to fasting sugae mental health.
Diabetes is marked by higher-than-normal blood sugars, but did anx know bloid underlying cause for type Menstrual health initiatives diabetes blkod low-grade inflammation?
Bllod reason is ans chronic inflammation —caused by diet, excess weight, sedentary lifestyles, stress and impaired clntrol health—causes cells Infkammation slowly become insulin resistant. This leads ahd higher blood glucose levels, as well as fat accumulation in the liver, Inflamation a cycle ahd builds on itself that anc to greater insulin resistance.
This amd that those with diabetes or prediabetes contro, long-term Inflammation and blood sugar control anf choosing foods that Inflammtaion only keep vlood sugar in check, amd also reduce inflammation.
To get started, here are a cojtrol of the top Fat burning pills foods bloood eat for diabetes.
Inflammtaion healthy xnd fats in nuts aren't just good in terms of heart health. Inflammation and blood sugar control studies associate regular nut consumption dugar lower boood blood glucose levels, Healthy eating habits for sports performance insulin resistance and improved A1c levels.
The combination of fiber, protein Citrus oil extraction fat provides Energy-boosting weight loss supplements while not spiking comtrol.
Aim to keep portions sygar around suagr ounce per day. Walnuts are some of the best, Fruits high in antioxidants, but almonds, pistachios and other tree nuts offer similar benefits get our picks for the Invlammation healthiest nuts to hlood on. Pictured Recipe : Air-Fryer Broccoli. The American Diabetes Association recommends filling Boost confidence in public speaking your plate cobtrol meals with nonstarchy veggies, Inflakmation broccoli Fruits high in antioxidants one of your best options to include.
The green contro are Inflamkation with sugra, as Inflammatlon as antioxidants such as vitamin Imflammation and controo C.
However, it's contorl sulfur-containing Inflammation and blood sugar control Inflanmation broccoli, as Infkammation as other cruciferous vegetables like cauliflower and Brussels sprouts, that have powerful anti-inflammatory effects when eaten regularly.
Inflam,ation Recipe: Inflanmation Fruits high in antioxidants with Green Beans. Adding extra garlic when Inflammation and blood sugar control to help Inflammation and blood sugar control blood sugar may sound a little out ckntrol.
However, sugsr meta-analysis suggests that it might just Fruits high in antioxidants. Shgar analyzed blodo effects from sugra studies that garlic has on blood sugar anv those with blod, and nlood that when consumed in tandem with controo medications, many had slightly lower glucose blpod.
These benefits Inflammatiln believed to come from the Antioxidant homeostasis compound conteolwhich sugqr anti-inflammatory, anti-viral and antibacterial properties.
Pictured Recipe: Crunchy Roasted Chickpeas. Chickpeas are showing up everywhere lately, from snack foods to Inflammatuon to cookie "dough," but this Inflammattion a good thing since this cotnrol is a tasty cohtrol Inflammation and blood sugar control source of fiber and protein.
From an anti-inflammatory standpoint, beans and legumes are an contfol source of complex carbs that have Indlammation much contdol impact on glucose when eaten in place of refined grains and starches. In terms of long-term benefits, research suggests that regularly incorporating high-fiber foods like chickpeas, as well as other beans and legumes, reduces fasting blood sugar levels.
Pictured Recipe: Spaghetti Squash Lasagna with Broccolini. Available year-round, squash are packed with antioxidants that soothe inflammation.
The amount of carbohydrates in a squash vary depending on type, so opt for one to fit your meal needs. Winter squash like butternut and acorn are higher in carbohydrates, yet have more nutrients and a lower glycemic effect compared to potatoes and refined grains.
If you want an option that is lower in carbs, give spaghetti squash a try. It's a great low-carb substitute for spaghetti and pasta, and swapping carb-rich foods like pasta and rice for spaghetti squash or zucchini noodles keeps blood sugar more stable eating inflammation.
Pictured Recipe : Homemade Plain Greek Yogurt. Gut health seems to be connected to most every health issue, and this holds true for diabetes as well. A study found that incorporating probiotics foods or supplements with "good" gut bacteria on a regular basis was associated with lower HgbA1c levels and fasting blood glucose in those with type 2 diabetes.
A healthy microbiome bacteria appears to reduce inflammatory compounds that contribute to insulin resistance and weight gain, and one of the best probiotic-rich foods is yogurt with live bacteria cultures.
Choose Greek yogurt for higher levels of protein, and pick plain over flavored varieties to avoid added sugars. Then add fresh fruit or nuts for a little sweetness and crunch.
Pictured Recipe: Blueberry-Banana Overnight Oats. The tiny blue fruit was named a " superfood " by the American Diabetes Association and is one healthiest fruit choices you can make.
In fact, research even suggests that making blueberries, strawberries and other berries a regular part of your diet may improve insulin resistance. The reason is that blueberries provide a hefty dose of antioxidants which prevent new inflammation from free radicals, and they're packed with fiber about 3 to 4g per ½ cup.
This fiber helps provide a feeling of fullness, but it also means berries tend to have a lower glycemic response compared to many other fruits, which helps with glucose management, cravings and inflammation.
Plus, here are some other fruits you should eat when you have diabetes. Pictured Recipe : Cinnamon Roll Overnight Oats. Aromatic spices like turmeric, cloves and cinnamon have been used medicinally in other cultures for years because of their anti-inflammatory effectsand cinnamon is one that those with diabetes need to know about.
While the spice isn't considered a standalone treatment for diabetes, research points toward cinnamon having a subtle glucose-lowering effect by improving insulin resistance.
Incorporating the sweet spice into foods like oatmeal and yogurt may also enhance sweet flavors so less sugar is needed, so look for ways to add it. Benefits have been seen from servings as small as one-fourth teaspoon. Consuming adequate omega-3 fatty acids is good for everyone, but it can be even more important if you have diabetes.
Omega-3 fatty acids have powerful anti-inflammatory effects, particularly for reducing heart disease risk. There's also research to suggest that daily omega-3s may help to prevent diabetic inflammatory conditions like neuropathy in arms, legs and extremities.
Omega-3 fatty acids sources are limited, but higher fat, cold water fish like salmon, trout, sardines and mackerel are some of the best, along with flaxseeds. Aim to get two servings of fish per week, and try sprinkling flaxseeds into yogurt, cooked grains and cereal like granola.
Pictured Recipe : Balsamic-Parmesan Sautéed Spinach. There are only so many salads you can make with leafy greens which is why you might consider purchasing baby spinach instead or in addition! The tender leaves are ideal to toss as a salad, but they can also be stirred into hot stews, soups, entrees, and cooked whole-grains.
Loading up on non-starchy vegetables, like leafy greens, is also a good way to add more food to your plate without adding many calories or carbs. A two-cup serving also provides almost half of an adult's daily needs for vitamin C and beta-carotene which are two antioxidants that play key roles in reducing inflammation.
Use limited data to select advertising. Create profiles for personalised advertising. Use profiles to select personalised advertising. Create profiles to personalise content. Use profiles to select personalised content. Measure advertising performance.
Measure content performance. Understand audiences through statistics or combinations of data from different sources. Develop and improve services. Use limited data to select content. List of Partners vendors. Just Tell Me What to Eat: Diabetes Edition.
Healthy Eating for Diabetes. Special Diets Diabetes. By Carolyn Williams, Ph. EatingWell's Editorial Guidelines. Reviewed by Dietitian EatingWell. She is a registered dietitian with a master's in food, nutrition and sustainability.
Reviewed by Dietitian Jessica Ball, M. Jessica Ball, M. Try Our Healthy and Delicious Diabetes Meal Plans. Try These Recipes That Are Rich in Omega-3 Fatty Acids. Was this page helpful? Thanks for your feedback! Tell us why! Related Articles. Newsletter Sign Up. You may accept or manage your choices by clicking below, including your right to object where legitimate interest is used, or at any time in the privacy policy page.
These choices will be signaled to our partners and will not affect browsing data. Accept All Reject All Show Purposes.
: Inflammation and blood sugar control| Blood Sugar, Diabetes and Inflammation | All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Alberti K, Eckel R, Grundy S, Zimmet P, Cleeman J, Donato K, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation —5. doi: PubMed Abstract CrossRef Full Text Google Scholar. Pradhan A, Manson J, Rifai N, Buring J, Ridker P. C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. JAMA — Esser N, Legrand-Poels S, Piette J, Scheen A, Paquot N. Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res Clin Pract — Herder C, Dalmas E, Böni-Schnetzler M, Donath M. The IL-1 pathway in type 2 diabetes and cardiovascular complications. Trends Endocrinol Metab — Kahn S, Cooper M, Del Prato S. Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet — Winkler G, Salamon F, Harmos G, Salamon D, Speer G, Szekeres O, et al. Elevated serum tumor necrosis factor-alpha concentrations and bioactivity in type 2 diabetics and patients with android type obesity. Hotamisligil G, Arner P, Caro J, Atkinson R, Spiegelman B. Increased adipose tissue expression of tumor necrosis factor-alpha in human obesity and insulin resistance. J Clin Invest — Shoelson SE, Lee J, Yuan M. Int J Obes Relat Metab Disord 27 Suppl 3:S49— Maedler K, Sergeev P, Ris F, Oberholzer J, Joller-Jemelka H, Spinas G, et al. Glucose-induced beta cell production of IL-1beta contributes to glucotoxicity in human pancreatic islets. Donath MY, Schumann DM, Faulenbach M, Ellingsgaard H, Perren A, Ehses JA. Islet inflammation in type 2 diabetes: from metabolic stress to therapy. Diabetes Care 31 Suppl 2:S— Donath M, Størling J, Berchtold L, Billestrup N, Mandrup-Poulsen T. Cytokines and beta-cell biology: from concept to clinical translation. Endocr Rev — Esser N, Paquot N, Scheen A. Anti-inflammatory agents to treat or prevent type 2 diabetes, metabolic syndrome and cardiovascular disease. Expert Opin Investig Drugs — Donath M. Targeting inflammation in the treatment of type 2 diabetes: time to start. Nat Rev Drug Discovery — CrossRef Full Text Google Scholar. Hotamisligil GS. Inflammation and metabolic disorders. Nature —7. Ramos-Zavala MG, González-Ortiz M, Martínez-Abundis E, Robles-Cervantes JA, González-López R, Santiago-Hernández NJ. Effect of diacerein on insulin secretion and metabolic control in drug-naive patients with type 2 diabetes: a randomized clinical trial. Diabetes Care —4. Jangsiripornpakorn J, Srisuk S, Chailurkit L, Nimitphong H, Saetung S, Ongphiphadhanakul B. The glucose-lowering effect of low-dose diacerein and its responsiveness metabolic markers in uncontrolled diabetes. BMC Res Notes Choudhury RP, Birks JS, Mani V, Biasiolli L, Robson MD, L'Allier PL, et al. Arterial effects of canakinumab in patients with atherosclerosis and type 2 diabetes or glucose intolerance. J Am Coll Cardiol — Larsen CM, Faulenbach M, Vaag A, Vølund A, Ehses JA, Seifert B, et al. Interleukinreceptor antagonist in type 2 diabetes mellitus. N Engl J Med — Dominguez H, Storgaard H, Rask-Madsen C, Steffen Hermann T, Ihlemann N, Baunbjerg Nielsen D, et al. Metabolic and vascular effects of tumor necrosis factor-alpha blockade with etanercept in obese patients with type 2 diabetes. J Vasc Res — Huang J, Yang Y, Hu R, Chen L. Anti-interleukin-1 therapy has mild hypoglycaemic effect in type 2 diabetes. Diabetes Obes Metab —8. Kataria Y, Ellervik C, Mandrup-Poulsen T. Treatment of type 2 diabetes by targeting interleukin a meta-analysis of patients. Semin Immunopathol — Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA statement: an updated guideline for reporting systematic reviews. BMJ n Wan X, Wang W, Liu J, Tong T. BMC Med Res Methodol Cochrane handbook for systematic reviews of interventions version 6. cochrane Google Scholar. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ — Cardoso CRL, Leite NC, Carlos FO, Loureiro AA, Viegas BB, Salles GF. Efficacy and safety of diacerein in patients with inadequately controlled type 2 diabetes: A randomized controlled trial. Diabetes Care — Cavelti-Weder C, Babians-Brunner A, Keller C, Stahel MA, Kurz-Levin M, Zayed H, et al. Effects of gevokizumab on glycemia and inflammatory markers in type 2 diabetes. Everett B, Donath M, Pradhan A, Thuren T, Pais P, Nicolau J, et al. Anti-inflammatory therapy with canakinumab for the prevention and management of diabetes. Faghihimani E, Aminorroaya A, Rezvanian H, Adibi P, Ismail-Beigi F, Amini M. Salsalate improves glycemic control in patients with newly diagnosed type 2 diabetes. Acta Diabetol — Goldfine AB, Fonseca V, Jablonski KA, Pyle L, Staten MA, Shoelson SE. The effects of salsalate on glycemic control in patients with type 2 diabetes: a randomized trial. Ann Intern Med — Goldfine AB, Fonseca V, Jablonski KA, Chen YD, Tipton L, Staten MA, et al. Salicylate salsalate in patients with type 2 diabetes: a randomized trial. Noe A, Howard C, Thuren T, Taylor A, Skerjanec A. Pharmacokinetic and pharmacodynamic characteristics of single-dose canakinumab in patients with type 2 diabetes mellitus. Clin Ther — Piovesan F, Tres GS, Moreira LB, Andrades ME, Lisboa HK, Fuchs SC. To receive updates about diabetes topics, enter your email address: Email Address. What's this. Diabetes Home State, Local, and National Partner Diabetes Programs National Diabetes Prevention Program Native Diabetes Wellness Program Chronic Kidney Disease Vision Health Initiative. Links with this icon indicate that you are leaving the CDC website. The Centers for Disease Control and Prevention CDC cannot attest to the accuracy of a non-federal website. Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website. You will be subject to the destination website's privacy policy when you follow the link. CDC is not responsible for Section compliance accessibility on other federal or private website. For more information on CDC's web notification policies, see Website Disclaimers. Cancel Continue. Blood Sugar, Diabetes and Inflammation Managing glucose may calm chronic inflammation. Understand how, and why. March 23, Inflammation and Diabetes What's the link between inflammation and diabetes? What is metabolic inflammation? Those cytokines get in the way of the hormone insulin, keeping it from doing the job of clearing glucose from the blood. When this pathway is blocked or thrown off, glucose stays in the blood, raising your blood sugar levels. High blood sugar tells your system that glucose regulation is out of whack. That triggers even more inflammation as your immune system fires up to solve the problem. Insulin resistance is a major risk factor for — you guessed it — diabetes. Does sugar cause inflammation? Does metabolic syndrome cause inflammation? This term actually refers to a cluster of chronic conditions that includes: High blood sugar levels High blood pressure High cholesterol High triglyceride levels High waist circumference Make no mistake, each condition is unhealthy on its own but having three or more of these markers above a normal range can significantly compound your risk for heart disease, diabetes, or stroke. Drop some weight , if you need to. Even an extra 15 or 20 pounds can throw off your system as your fat cells send out compounds that ramp up inflammation. Focus on eating well. That means avoiding simple, processed carbs including white bread, pasta and rice; baked goods; refined crackers and crunchy snacks , as well as fast foods. Wean off of anything with lots of added sugar, as discussed above, and go easy on red meat and processed meats including hot dogs and bacon. For starters: Nearly all veggies, but especially leafy greens High-fiber fruits, including berries and citrus Healthy fats, including olive oil Nuts, including almonds and walnuts Fish — especially oily types, like salmon, tuna, and sardines Get moving, and keep moving. Anytime you push your muscles, even just to take a walk or get stuff done around the house, they release anti-inflammatory compounds. So regular exercise , while good for just about every aspect of your health, is an especially powerful weapon against diabetes and inflammation. |
| How does excess sugar affect inflammatory markers? | Volume 29, Issue Inflammayion. A sgar strategy abd to Inflammatioon as many colors of fruits and Suar as you can to Energy-boosting tips a variety of vitamins and minerals. Interpreting Blood Fruits high in antioxidants Levels: A Guide Immune-boosting foods Normal Ranges and Transforming lean muscle Glucose. Table 2— Plasma levels of inflammatory markers of the diabetic and the hyperglycemic groups compared with the NGT group. Eating good quality protein with every meal also helps to lessen blood sugar spikes after eating and incorporate high fibre foods and chewing food properly before swallowing, as this will slow down the digestion process. Adiposity, in particular visceral adipose tissue, has been found to be a key promoter of low-grade chronic inflammation 28 , |
| RESEARCH DESIGN AND METHODS | Blood Sugar, Diabetes and Inflammation Managing glucose may calm chronic inflammation. Understand how, and why. March 23, Inflammation and Diabetes What's the link between inflammation and diabetes? What is metabolic inflammation? Those cytokines get in the way of the hormone insulin, keeping it from doing the job of clearing glucose from the blood. When this pathway is blocked or thrown off, glucose stays in the blood, raising your blood sugar levels. High blood sugar tells your system that glucose regulation is out of whack. That triggers even more inflammation as your immune system fires up to solve the problem. Insulin resistance is a major risk factor for — you guessed it — diabetes. Does sugar cause inflammation? Does metabolic syndrome cause inflammation? This term actually refers to a cluster of chronic conditions that includes: High blood sugar levels High blood pressure High cholesterol High triglyceride levels High waist circumference Make no mistake, each condition is unhealthy on its own but having three or more of these markers above a normal range can significantly compound your risk for heart disease, diabetes, or stroke. Drop some weight , if you need to. Even an extra 15 or 20 pounds can throw off your system as your fat cells send out compounds that ramp up inflammation. Focus on eating well. That means avoiding simple, processed carbs including white bread, pasta and rice; baked goods; refined crackers and crunchy snacks , as well as fast foods. Wean off of anything with lots of added sugar, as discussed above, and go easy on red meat and processed meats including hot dogs and bacon. For starters: Nearly all veggies, but especially leafy greens High-fiber fruits, including berries and citrus Healthy fats, including olive oil Nuts, including almonds and walnuts Fish — especially oily types, like salmon, tuna, and sardines Get moving, and keep moving. Anytime you push your muscles, even just to take a walk or get stuff done around the house, they release anti-inflammatory compounds. So regular exercise , while good for just about every aspect of your health, is an especially powerful weapon against diabetes and inflammation. The American Diabetes Association recommends minutes a week, or just a little more than 20 minutes a day. Doable, right? Just getting up out of your chair and moving around a bit every hour counts, too. As this study in the American Journal of Preventive Medicine shows, a heavily sedentary lifestyle is associated with higher markers of inflammation. heading 1 The rich text element allows you to create and format headings, paragraphs, blockquotes, images, and video all in one place instead of having to add and format them individually. heading 2 A rich text element can be used with static or dynamic content. Heading 3 Headings, paragraphs, blockquotes, figures , images, and figure captions can all be styled after a class is added to the rich text element using the "When inside of" nested selector system. Heading 4 Headings, paragraphs, blockquotes, figures, images, and figure captions can all be styled after a class is added to the rich text element using the "When inside of" nested selector system. Heading 5 Headings, paragraphs, blockquotes, figures, images, and figure captions can all be styled after a class is added to the rich text element using the "When inside of" nested selector system. Related Articles No items found. The quality of the included trials was assessed according to the criteria of the Cochrane Handbook. A detailed evaluation of the risk of bias for each clinical trial and risk of bias summary are presented in Figure S1. Among the 16 RCTs, only 1 was judged to be at high risk of bias as an open-label randomized trial 19 , 6 were judged to be at low risk of bias and 9 as being at unclear risk of bias. Unclear risks were related to selection bias, reporting bias, and other bias. We did a series of subgroup analyses of FPG based on the targets of interventions, diabetes duration, and follow-up duration. A Meta-analyses of the effects of anti-inflammatory therapies on FPG in patients with T2DM; B The forest plot of FPG in subgroup analyses defined by the targets of interventions. fasting plasma glucose, FPG; CI, confidence interval; IV, inverse variance; SD, standard deviation. The change in HbA1c was assessed in all studies. The sensitivity analyses of HbA1c indicated the stability of the results Figure S3. LY and etanercept had no significant effect on HbA1c compared with the control. A Meta-analyses of the effects of anti-inflammatory therapies on HbA1c in patients with T2DM; B The forest plot of HbA1c in subgroup analyses defined by the targets of interventions. glycated haemoglobin, HbA1c; CI, confidence interval; IV, inverse variance; SD, standard deviation. A Meta-analyses of the effects of anti-inflammatory therapies on CRP in patients with T2DM; B The forest plot of CRP in subgroup analyses defined by the targets of interventions. C-reactive protein, CRP; CI, confidence interval; IV, inverse variance; SD, standard deviation. Our meta-analyses of 16 RCTs published between and examined the effects of anti-inflammatory therapies on glycemic control in patients with T2DM. Two previous meta-analyses published in and , concluded that anti-IL-1 therapies can significantly decrease the level of HbA1c and CRP, and have mild hypoglycaemic effect on patients with T2DM 20 , However, the effects of anti-inflammatory therapies targeting other inflammatory molecules and the overall effects of anti-inflammatory therapies on T2DM remain to be discovered. Therefore, we performed further analyses of anti-inflammatory therapies based on different inflammatory targets, including IL-1β, IL-1βR, TNF-α, and NF-κB. Our results show that anti-inflammatory therapies, including anti-IL-1 therapies, can significantly decrease the level of FPG, HbA1c and CRP in patients with T2DM. Our findings indicate the clinical efficacy of treating T2DM based on the pathogenesis of diabetes and give suggestions for the future anti-inflammatory clinical trials. Chronic low-grade inflammation was found in diabetic islets, with increased innate immune cell infiltration and cytokine secretion Immune cell infiltration and cytokine release directly impairs β cell mass and function IL-1β was the first described proinflammatory cytokine in the islets of patients with T2DM IL-1β impairs β cell function and induces the apoptosis of β cells Block IL-1β signaling pathway by antagonists or antibodies had beneficial effects on β cell function and glycemic control in patients with T2DM 41 , Anakinra, a recombinant human IL-1βR antagonist, can significantly reduce the level of HbA1c and may improve glycemic control by increasing insulin secretion Canakinumab, gevokizumab and LY are recombinant human engineered monoclonal antibodies, which can neutralize the activity of IL-1β by forming a complex with circulating IL-1β. Canakinumab can also reduce the blood levels of IL-6 and CRP All the anti-IL-1β therapies mentioned above had significant effect on glucose control as reflected by reductions in HbA1c, which was also reported by previous meta-analyses 20 , However, some of the beneficial effects were only detected by certain treatment periods, not the whole follow-up periods 28 , As shown in our subgroup analyses, anti-inflammatory therapies may work better in patients with short follow-up duration less than or equal to 3 months. LY can improve blood glucose control for 12 weeks, but the effect was attenuated over time and there was no difference at 24 weeks The study reported by Everett BM et al. showed that canakinumab can reduce HbA1c during the first 6 to 9 months of treatment, but no significant effect was found by the end of the follow-up period at 48 months The exact reason for this attenuation is unclear, but the availability of other antidiabetic therapies and lifestyle interventions may contribute to this phenomenon TNF-α can diminish glucose-dependent insulin secretion and impair the function of β cells both in vitro and in vivo 43 , But etanercept, a TNF-α inhibitor, has no significant effect on FPG or HbA1c Etanercept can improve the glucose tolerance of some individuals, but no significant effect was found in the whole group It was difficult to say whether etanercept has a positive effect on β cells since no more than 20 individuals was included in this clinical trial, and studies with a larger number of patients with T2DM are needed to elucidate this issue. Diacerein is both an IL-1βR blocker and a TNF antagonist. It can inhibit the synthesis and activity of IL-1 and TNF-α by its active metabolite rhein Diacerein can reduce the HbA1c level without affecting the homeostasis model assessment-insulin resistance HOMA-IR , indicating that it may play a role in insulin secretion Our results show that interventions targeting IL-1β plus TNF-α can reduce the level of HbA1c better than targeting IL-1β or TNFα alone in patients with T2DM. Diacerein had no significant effect on CRP in patients with T2DM, though reduced TNF-α was observed 26 , Those studies were carried out in patients with longer duration of diabetes, and most participants were undergoing treatment with metformin, statins, sulfonylureas, or renin-angiotensin system blockers, which have potential roles in anti-inflammation, and might attenuate the anti-inflammatory effect of diacerein 13 , 26 , Salsalate can improve glycemic control by affecting cellular kinases nonspecifically and increasing insulin secretion of β cells After 1 year treatment, salsalate still had effects on HbA1c and FPG in patients with T2DM Salsalate can decrease the level of inflammatory mediators, such as leukocytes, neutrophils, and lymphocytes, but had little effect on CRP in patients with T2DM T2DM seems to result from a long-term process of inflammation, even years before diagnosis Greater benefits of salsalate might be seen in patients with newly diagnosed T2DM or longer treatment duration. Our results show that patients with newly diagnosed T2DM may benefit more from anti-inflammatory therapies. However, Kataria Y et al. reported that the effects of anti-IL-1β therapies depend on the baseline dysmetabolic status, and patients with a more metabolic imbalance at baseline may benefit more after treatment The differences between our studies may come from the different types of medications analyzed, as we included lots of anti-inflammatory medications, not just IL-1β antibodies and IL-1βR antagonists. Since no newly diagnosed T2DM patients were included in the studies of anti-IL-1β therapies, the effects of anti-IL-1β therapies on those patients remain to be seen. There are some limitations in our study. First, lifestyle modification and antidiabetic medications were allowed in most of the included trials, which may affect or attenuate the efficacy of anti-inflammatory therapies. Second, most of the follow-up duration varied from 1 to 12 months, and longer clinical trials are needed since medication efficacy may change over time. Finally, publication bias exists in the meta-analyses, but the results stay the same after a trim and fill analysis. This study helps us better understand the possibility and efficiency of anti-inflammatory therapies for T2DM based on the pathogenetic processes of the disease. The present analyses demonstrated that targeting cytokines, cytokine receptors, and inflammation-associated nuclear transcription factors, such as IL-1β, IL-1βR, TNF-α, and NF-κB, alone or in combination can significantly reduce the level of FPG, HbA1c, and CRP in patients with T2DM. In addition, patients with a short duration of T2DM may benefit more from anti-inflammatory therapies. Since anti-inflammatory medications can reduce inflammation throughout the body, these medications may be used to treat diseases with similar pathologies, such as cardiovascular disease, chronic kidney disease, and rheumatic arthritis with or without T2DM. Further inquiries can be directed to the corresponding author. DL and JinZ conceived and designed the study. DL and JiaZ did the scientific literature search and data extraction of the included studies. DL and QZ did the quality assessment and carried out the analyses. DL wrote the first draft of the present manuscript. All authors contributed to the article and approved the submitted version. This work was supported by grants from the National Natural Science Foundation of China , , , , Leading Talents Program of Hunan Province RC , Natural Science Foundation of Hunan Province, China JJ and National key research and development program YFA, YFC We are grateful to Central South University Library for the assistance during literature search. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Alberti K, Eckel R, Grundy S, Zimmet P, Cleeman J, Donato K, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation —5. doi: PubMed Abstract CrossRef Full Text Google Scholar. Pradhan A, Manson J, Rifai N, Buring J, Ridker P. C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. JAMA — Esser N, Legrand-Poels S, Piette J, Scheen A, Paquot N. Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res Clin Pract — Herder C, Dalmas E, Böni-Schnetzler M, Donath M. The IL-1 pathway in type 2 diabetes and cardiovascular complications. Trends Endocrinol Metab — Kahn S, Cooper M, Del Prato S. Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet — Winkler G, Salamon F, Harmos G, Salamon D, Speer G, Szekeres O, et al. Elevated serum tumor necrosis factor-alpha concentrations and bioactivity in type 2 diabetics and patients with android type obesity. Hotamisligil G, Arner P, Caro J, Atkinson R, Spiegelman B. Increased adipose tissue expression of tumor necrosis factor-alpha in human obesity and insulin resistance. J Clin Invest — Shoelson SE, Lee J, Yuan M. Int J Obes Relat Metab Disord 27 Suppl 3:S49— Maedler K, Sergeev P, Ris F, Oberholzer J, Joller-Jemelka H, Spinas G, et al. Glucose-induced beta cell production of IL-1beta contributes to glucotoxicity in human pancreatic islets. Donath MY, Schumann DM, Faulenbach M, Ellingsgaard H, Perren A, Ehses JA. Islet inflammation in type 2 diabetes: from metabolic stress to therapy. Diabetes Care 31 Suppl 2:S— Donath M, Størling J, Berchtold L, Billestrup N, Mandrup-Poulsen T. Cytokines and beta-cell biology: from concept to clinical translation. Endocr Rev — Esser N, Paquot N, Scheen A. Anti-inflammatory agents to treat or prevent type 2 diabetes, metabolic syndrome and cardiovascular disease. Expert Opin Investig Drugs — Donath M. Targeting inflammation in the treatment of type 2 diabetes: time to start. Nat Rev Drug Discovery — CrossRef Full Text Google Scholar. Hotamisligil GS. Inflammation and metabolic disorders. Nature —7. Ramos-Zavala MG, González-Ortiz M, Martínez-Abundis E, Robles-Cervantes JA, González-López R, Santiago-Hernández NJ. Effect of diacerein on insulin secretion and metabolic control in drug-naive patients with type 2 diabetes: a randomized clinical trial. Diabetes Care —4. Jangsiripornpakorn J, Srisuk S, Chailurkit L, Nimitphong H, Saetung S, Ongphiphadhanakul B. The glucose-lowering effect of low-dose diacerein and its responsiveness metabolic markers in uncontrolled diabetes. BMC Res Notes Choudhury RP, Birks JS, Mani V, Biasiolli L, Robson MD, L'Allier PL, et al. Arterial effects of canakinumab in patients with atherosclerosis and type 2 diabetes or glucose intolerance. J Am Coll Cardiol — Larsen CM, Faulenbach M, Vaag A, Vølund A, Ehses JA, Seifert B, et al. Interleukinreceptor antagonist in type 2 diabetes mellitus. N Engl J Med — Dominguez H, Storgaard H, Rask-Madsen C, Steffen Hermann T, Ihlemann N, Baunbjerg Nielsen D, et al. Metabolic and vascular effects of tumor necrosis factor-alpha blockade with etanercept in obese patients with type 2 diabetes. J Vasc Res — Huang J, Yang Y, Hu R, Chen L. Anti-interleukin-1 therapy has mild hypoglycaemic effect in type 2 diabetes. Diabetes Obes Metab —8. Kataria Y, Ellervik C, Mandrup-Poulsen T. Treatment of type 2 diabetes by targeting interleukin a meta-analysis of patients. Semin Immunopathol — Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA statement: an updated guideline for reporting systematic reviews. BMJ n Wan X, Wang W, Liu J, Tong T. BMC Med Res Methodol Cochrane handbook for systematic reviews of interventions version 6. |
| Inflammation and glucose levels: How high blood sugar can turn a good system bad - Levels | Several studies showed that cytokine levels CRP, IL-6, and TNF-α are related to glycemic control 38 — Improvement of glycemic control has an inconsistent beneficial impact on the level of inflammatory markers. No significant effect was found on the levels of IL-6 and TNF-α with sulfonylureas or insulin therapy, but a significant decrease in CRP was observed with insulin Troglitazone with an improvement in glycemic control reduces CRP 42 and decreases plasma levels of TNF-α in obese diabetic patients One weight loss study showed that moderate-intensity regular exercise decreases the TNF-α level A high inflammation level might contribute to the worsening of progression of type 2 diabetes in addition to glycemic control. Our study has several strengths. First, we have several measures of inflammatory markers and can create an inflammatory index. Second, the study includes a large sample size and a biracial population with a high percentage of blacks. One limitation of our study is that because of the study design cross-sectional study , the direction of these associations cannot be conclusively determined and a causal relationship cannot be inferred. Additionally, the study population includes well-functioning relatively healthy participants; our findings may not be generalized to a frail older population. Among those with diabetes, poorer glycemic control was associated with higher levels of CRP. Whether baseline levels of inflammatory markers in those without pre-diabetes or diabetes would be predictors of the onset of pre-diabetes and diabetes should be determined, and we plan to explore this in our longitudinal data. Plasma levels of inflammatory markers of the diabetic and the hyperglycemic groups compared with the NGT group. For risk of high inflammation level associated with diabetes and hyperglycemic status, model 1 is adjusted on age, sex, race, smoking status, alcohol intake, education, and site. Model 2 adds total body fat, visceral fat, and height. Model 3 adds cardiovascular diseases, hypertension, peripheral arterial disease, renal insufficiency, arthritis, pulmonary disease, anti-inflammatory, statin, and estrogen use. For relationship between glycemic control and inflammation in diabetes, models 1 and 2 are the same and model 3 adds diabetes duration. This study was supported by Contracts NAG, NAG, and NAG from the National Institute on Aging. This research was supported in part by the Intramural Research Program of National Institutes of Health, National Institute on Aging. A table elsewhere in this issue shows conventional and Système International SI units and conversion factors for many substances. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 29, Issue 8. Previous Article Next Article. RESEARCH DESIGN AND METHODS. Article Information. Article Navigation. Cardiovascular and Metabolic Risk August 01 Diabetes, Hyperglycemia, and Inflammation in Older Individuals : The Health, Aging and Body Composition study Nathalie de Rekeneire, MD, MS ; Nathalie de Rekeneire, MD, MS. This Site. Google Scholar. Rita Peila, PHD ; Rita Peila, PHD. Jingzhong Ding, PHD ; Jingzhong Ding, PHD. Lisa H. Colbert, PHD ; Lisa H. Colbert, PHD. Marjolein Visser, PHD ; Marjolein Visser, PHD. Ronald I. Shorr, MD, MS ; Ronald I. Shorr, MD, MS. Stephen B. Kritchevsky, PHD ; Stephen B. Kritchevsky, PHD. Lewis H. Kuller, MD, DRPH ; Lewis H. Kuller, MD, DRPH. Elsa S. Strotmeyer, PHD ; Elsa S. Strotmeyer, PHD. Ann V. Schwartz, PHD ; Ann V. Schwartz, PHD. Bruno Vellas, MD, PHD ; Bruno Vellas, MD, PHD. Tamara B. Harris, MD, MS Tamara B. Harris, MD, MS. Address correspondence and reprint requests to Nathalie de Rekeneire, MD, Laboratory of Epidemiology, Demography and Biometry, National Institute on Aging, Gateway Building, Suite 3C, Wisconsin Ave. E-mail: rekenein nia. Diabetes Care ;29 8 — Article history Received:. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Table 1— Baseline characteristics by diabetes and hyperglycemic status. Data are means ± SD or median interquartile range unless otherwise noted. DXA, dual-energy X-ray absorptiometry. View Large. Table 2— Plasma levels of inflammatory markers of the diabetic and the hyperglycemic groups compared with the NGT group. Inflammatory marker. P value. Table 3— Multivariate analyses for the association of hyperglycemia and diabetes with inflammation. Risk of high inflammation level associated with diabetes and hyperglycemic status. Model 1. Model 2. Model 3. Relationship between glycemic control A1C and inflammation in diabetes. High CRP 1. Bruunsgaard H, Pedersen M, Pedersen BK: Aging and proinflammatory cytokines. Curr Opin Hematol. Pickup JC, Crook MA: Is type II diabetes mellitus a disease of the innate immune system? Nilsson J, Jovinge S, Niemann A, Reneland R, Lithell H: Relation between plasma tumor necrosis factor-α and insulin sensitivity in elderly men with non-insulin-dependent diabetes mellitus. Arterioscler Thromb Vasc Biol. Yudkin JS, Stehouwer CD, Emeis JJ, Coppack SW: C-reactive protein in healthy subjects: associations with obesity, insulin resistance, and endothelial dysfunction: a potential role for cytokines originating from adipose tissue? Ford ES: Body mass index, diabetes, and C-reactive protein among U. Diabetes Care. Frohlich M, Imhof A, Berg G, Hutchinson WL, Pepys MB, Boeing H, Muche R, Brenner H, Koenig W: Association between C-reactive protein and features of the metabolic syndrome: a population-based study. Temelkova-Kurktschiev T, Siegert G, Bergmann S, Henkel E, Koehler C, Jaross W, Hanefeld M: Subclinical inflammation is strongly related to insulin resistance but not to impaired insulin secretion in a high risk population for diabetes. Barzilay JI, Abraham L, Heckbert SR, Cushman M, Kuller LH, Resnick HE, Tracy RP: The relation of markers of inflammation to the development of glucose disorders in the elderly: the Cardiovascular Health Study. Pradhan AD, Manson JE, Rifai N, Buring JE, Ridker PM: C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. Hotamisligil GS, Arner P, Caro JF, Atkinson RL, Spiegelman BM: Increased adipose tissue expression of tumor necrosis factor-α in human obesity and insulin resistance. J Clin Invest. Kern PA, Saghizadeh M, Ong JM, Bosch RJ, Deem R, Simsolo RB: The expression of tumor necrosis factor in human adipose tissue: regulation by obesity, weight loss, and relationship to lipoprotein lipase. Saghizadeh M, Ong JM, Garvey WT, Henry RR, Kern PA: The expression of TNF α by human muscle: relationship to insulin resistance. Tsigos C, Papanicolaou DA, Kyrou I, Defensor R, Mitsiadis CS, Chrousos GP: Dose-dependent effects of recombinant human interleukin-6 on glucose regulation. J Clin Endocrinol Metab. American Diabetes Association: Diagnosis and classification of diabetes mellitus Position Statement. Genuth S, Alberti KG, Bennett P, Buse J, Defronzo R, Kahn R, Kitzmiller J, Knowler WC, Lebovitz H, Lernmark A, Nathan D, Palmer J, Rizza R, Saudek C, Shaw J, Steffes M, Stern M, Tuomilehto J, Zimmet P, the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus: Follow-up report on the diagnosis of diabetes mellitus. Hill JO, Sidney S, Lewis CE, Tolan K, Scherzinger AL, Stamm ER: Racial differences in amounts of visceral adipose tissue in young adults: the CARDIA Coronary Artery Risk Development in Young Adults study. Am J Clin Nutr. Shlipak MG, Fried LF, Crump C, Bleyer AJ, Manolio TA, Tracy RP, Furberg CD, Psaty BM: Elevations of inflammatory and procoagulant biomarkers in elderly persons with renal insufficiency. Harris TB, Ferrucci L, Tracy RP, Corti MC, Wacholder S, Ettinger WH Jr, Heimovitz H, Cohen HJ, Wallace R: Associations of elevated interleukin-6 and C-reactive protein levels with mortality in the elderly. Am J Med. Choi KM, Lee J, Lee KW, Seo JA, Oh JH, Kim SG, Kim NH, Choi DS, Baik SH: Comparison of serum concentrations of C-reactive protein, TNF-α, and interleukin 6 between elderly Korean women with normal and impaired glucose tolerance. Diabetes Res Clin Pract. Hashimoto K, Kasayama S, Yamamoto H, Kurebayashi S, Kawase I, Koga M: Strong association of C-reactive protein with body mass index and 2-h post-challenge glucose in non-diabetic, non-smoker subjects without hypertension. Diabet Med. Duncan BB, Schmidt MI, Pankow JS, Ballantyne CM, Couper D, Vigo A, Hoogeveen R, Folsom AR, Heiss G: Low-grade systemic inflammation and the development of type 2 diabetes: the Atherosclerosis Risk in Communities Study. Brownlee M: Advanced protein glycosylation in diabetes and aging. Annu Rev Med. Peraldi P, Spiegelman B: TNF-α and insulin resistance: summary and future prospects. Mol Cell Biochem. Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB: Elevated C-reactive protein levels in overweight and obese adults. Forouhi NG, Sattar N, McKeigue PM: Relation of C-reactive protein to body fat distribution and features of the metabolic syndrome in Europeans and South Asians. Int J Obes Relat Metab Disord. Pannacciulli N, Cantatore FP, Minenna A, Bellacicco M, Giorgino R, De Pergola G: C-reactive protein is independently associated with total body fat, central fat, and insulin resistance in adult women. Uysal KT, Wiesbrock SM, Marino MW, Hotamisligil GS: Protection from obesity-induced insulin resistance in mice lacking TNF-α function. Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH: Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. Tracy RP, Lemaitre RN, Psaty BM, Ives DG, Evans RW, Cushman M, Meilahn EN, Kuller LH: Relationship of C-reactive protein to risk of cardiovascular disease in the elderly: results from the Cardiovascular Health Study and the Rural Health Promotion Project. If you do get sick, you may notice that your blood sugar levels become higher than usual. To fight off illness, your immune system releases hormones that can increase your blood sugar temporarily. Some cold and flu medicines can also raise your blood sugar. On the other hand, fever, sweating, and poor appetite can cause low blood sugar. Be sure to monitor your blood sugar closely and take steps if it gets too high or too low. People with diabetes might not have a higher risk of getting infected with COVID or flu. However, research shows that they have an increased risk of getting severe illness from these viruses, especially if their diabetes is not well managed. One of the best things you can do to protect yourself from COVID and flu is to get vaccinated and stay up to date on all eligible boosters. Vaccines are a safe and effective way to prevent getting severely ill. Skip directly to site content Skip directly to search. Español Other Languages. Diabetes and Your Immune System. Minus Related Pages. Having diabetes increases your chances of getting sick and staying sick longer. How Your Immune System Works Your immune system recognizes and fights off germs that can make you sick. Type 1 Diabetes and Your Immune System. How Diabetes Affects Your Immune System High blood sugar adds stress to your body and makes nearly every system work harder, including the white blood cells of your immune system. Diabetes, COVID and Flu People with diabetes might not have a higher risk of getting infected with COVID or flu. How to Stay Healthy With Diabetes There are plenty of things you can do to boost your immune system: Keep your blood sugar levels within your target range to protect your immune system. This can help prevent short- and long-term illnesses, and help you recover sooner if you do get sick. Eat plenty of fruits and vegetables. Fruits and vegetables are rich in vitamins and minerals that help your immune system work well. A great strategy is to eat as many colors of fruits and vegetables as you can to get a variety of vitamins and minerals. Talk to your doctor before taking any vitamin or mineral supplements. Be physically active. Physical activity can help you manage your blood sugar levels and keep your immune system strong in case you get sick. Wash your hands. Germs can spread from surfaces you touch every day. Washing your hands often is an important way to stay healthy. Manage stress. When your stress level is high, your immune system may have a harder time fighting off infections. Stress can also raise your blood sugar levels. Learn how to recognize when your stress level is high and practice relaxing activities like mindfulness, meditation, or yoga. Even 5 minutes can help you unwind. Get enough sleep. If you regularly get less than 7 hours of sleep, your diabetes will be harder to manage. Too little sleep can also make it harder for your immune system to fight infections. Get vaccinated and stay up to date. Vaccines are a crucial way to protect yourself from getting sick and prevent severe illness. Vaccines are especially important for people with diabetes. Make sure you get your initial dose s as well as any eligible boosters. |
| The Top 10 Anti-Inflammatory Foods for Diabetes | The swelling, burning, and redness that appears around a wound are all signs of inflammation. This is part of the body's process of repairing damage done to its tissues, and it eventually subsides when the wound is healed. But not all inflammation is visible. Just as it can happen on the surface of our skin, inflammation can also happen deep within our body tissues. If a tissue or organ is damaged, inflammation occurs as the body works to heal itself. Inflammation that happens for a short time in response to an injury or illness is normal, and not a cause for concern. It's inflammation that happens on an ongoing basis, called chronic inflammation, that may have an impact on your health. Chronic inflammation means that tissue damage occurs on an ongoing basis. Over time, this may lead to increased risk of heart disease, metabolic syndrome, and type 2 diabetes, as well as some autoimmune conditions, neurological diseases, and cancer. When the body is in a chronic inflammatory state, we can experience lowered immunity. Chronic inflammation can also cause tissue damage that makes us more susceptible to the development of certain diseases. Chronic inflammation is like the match that lights the fire to "turn on" the genes that are responsible for disease. Chronic inflammation can also contribute to some pretty uncomfortable everyday symptoms like brain fog, indigestion, difficulty losing weight, and fatigue. Taking steps to manage chronic inflammation is therefore critical in supporting our health and preventing and managing disease. Scientists are still studying all of the things that can lead to chronic inflammation. Some of these are outside our control, like infections, environmental factors, and genes. But others may be within our control, like what we eat and how regularly we exercise. Research also suggests that making certain changes, like getting regular physical activity, managing stress, and eating more fruits and vegetables may help manage chronic inflammation. So what's the connection between chronic inflammation and diabetes? It's a bit complicated. Chronic inflammation is a risk factor for both type 1 and type 2 diabetes, but it can also be a complication of diabetes. In the case of type 1 diabetes, inflammation is part of the autoimmune response that causes the disease. Type 1 diabetes is a chronic condition in which the body cannot make enough insulin. Chronic inflammation from the body's autoimmune response causes damage to the insulin producing cells in the pancreas, which leads to even more inflammation. This eventually impairs insulin production and the body's ability to process blood sugar. Although more research needs to be done, studies have found that inflammation in response to environmental factors, including inflammation from exposure to infections, may influence the development of type 1 diabetes. Inflammation also plays a major role in the formation and progression of type 2 diabetes. Type 2 diabetes is chronic condition in which the body has difficulty processing glucose aka blood sugar from carbohydrates in food. This causes chronically high levels of blood sugar, which eventually triggers the body's inflammatory response. Over time, type 2 diabetes causes ongoing inflammation in the body. Inflammation is also a factor in developing type 2 diabetes. Studies have found that pro-inflammatory compounds can disrupt the insulin-signaling pathways involved in metabolizing glucose, thus contributing to type 2 diabetes. Research has also found that excess body fat increases the risk for developing inflammation and chronic diseases that promote inflammation, such as type 2 diabetes. Chronic inflammation can also contribute to excess body fat, creating a vicious cycle of weight gain, inflammation, blood sugar dysfunction, and subsequent risk for increased risk for obesity and type 2 diabetes. Nutrition plays a key role in managing chronic inflammation as it can help minimize damage done from inflammation through the power of antioxidants. Antioxidants are anti-inflammatory compounds that help neutralize inflammatory compounds like free radicals. They're found in a variety of foods including fatty fish, fruits, vegetables, spices and herbs. Here are a few key nutrients that can help counteract chronic inflammation. Omega-3 fatty acids have been shown to fight inflammation, making them an important part of the diet. Getting enough omega-3s is essential for everyone, but especially important for people who have a higher inflammatory load and need an extra boost of antioxidants. Some of the best sources of omega-3s include fatty fish like salmon, tuna and mackerel. You can also get omega-3s from plant-based sources like walnuts and flaxseeds. Curcumin is a type of antioxidant found in the popular spice turmeric. Turmeric root, which is in the same plant family as ginger, can be enjoyed fresh or dried as a spice and has been used for centuries as a medicinal food in Ayurvedic and Eastern medicine. Preliminary research suggests curcumin may help decrease blood glucose and improve insulin resistance in people with diabetes. You can use turmeric as a spice in a variety of savory dishes including curries and chicken salad. You can also make turmeric latte or add turmeric to your smoothies to get an extra boost of turmeric in your beverages. Vitamin C is another antioxidant that helps drive down oxidative stress and inflammation in the body. Kern, Douglas A. Lauffenburger, Barbara S. Fatty Acid Metabolites Combine with Reduced β Oxidation to Activate Th17 Inflammation in Human Type 2 Diabetes. Cell Metabolism , ; DOI: Cite This Page : MLA APA Chicago University of Kentucky. Not glucose, says new research. ScienceDaily, 21 August University of Kentucky. What drives inflammation in type 2 diabetes? Retrieved February 14, from www. htm accessed February 14, Explore More. Storing Fat at the Waist May NOT Up Diabetes Risk, Surprise Findings Indicate. July 27, Conventional wisdom holds that storing fat around your belly puts you at increased risk for type 2 diabetes. But unexpected new findings suggest that, for some people, conventional wisdom may be Poor Glycemic Control in Patients With Type 2 Diabetes Can Be Predicted from Patient Information Systems With the Help of Machine Learning. The most important factors predicting Two Popular Diabetes Drugs Outperformed Others in Large Clinical Trial. Small Rises in Blood Glucose Trigger Big Changes in Insulin-Producing Cells. The work provides major additional evidence Print Email Share. Trending Topics. Breast Cancer. Personalized Medicine. Child Development. Consumer Behavior. Smart Earrings Can Monitor a Person's Temperature. Researchers 3D-Print Functional Human Brain Tissue. A Long-Lasting Neural Probe. How Teachers Make Ethical Judgments When Using AI in the Classroom. Poultry Scientists Develop 3D Anatomy Technique to Learn More About Chicken Vision. Research Team Breaks Down Musical Instincts With AI. Knowing What Dogs Like to Watch Could Help Veterinarians Assess Their Vision. Pain-Based Weather Forecasts Could Influence Actions. AI Discovers That Not Every Fingerprint Is Unique. |
Inflammation and blood sugar control -
Always inquisitive, she sought out the help of a Registered Dietitian in in order to understand the role food plays in one's overall health and build a better relationship with food.
Fast forward to the fall of , when she began her first class in the Nutrition and Food Studies program on her way to being a registered dietitian herself, hoping to make a positive impact on people as they navigate their way through understanding nutrition.
You may have heard about inflammation but not be quite sure what it is or how it may impact you, particularly if you have diabetes. Plus, what you eat can play a role in helping quell inflammation.
Some foods and nutrients are anti-inflammatory luckily, they're usually also good for blood sugar. Read on to find out more about inflammation and how it impacts your health, what you need to know about inflammation and diabetes and foods and nutrients to eat more of.
Inflammation happens when our immune system responds to damage done to our cells. This normal immune response can protect and heal our body, but when there is too much inflammation it can damage our tissues and harm our health. If you've ever had a cut or bruise, you have likely seen inflammation at work.
The swelling, burning, and redness that appears around a wound are all signs of inflammation. This is part of the body's process of repairing damage done to its tissues, and it eventually subsides when the wound is healed. But not all inflammation is visible. Just as it can happen on the surface of our skin, inflammation can also happen deep within our body tissues.
If a tissue or organ is damaged, inflammation occurs as the body works to heal itself. Inflammation that happens for a short time in response to an injury or illness is normal, and not a cause for concern.
It's inflammation that happens on an ongoing basis, called chronic inflammation, that may have an impact on your health. Chronic inflammation means that tissue damage occurs on an ongoing basis.
Over time, this may lead to increased risk of heart disease, metabolic syndrome, and type 2 diabetes, as well as some autoimmune conditions, neurological diseases, and cancer.
When the body is in a chronic inflammatory state, we can experience lowered immunity. Chronic inflammation can also cause tissue damage that makes us more susceptible to the development of certain diseases. Chronic inflammation is like the match that lights the fire to "turn on" the genes that are responsible for disease.
Chronic inflammation can also contribute to some pretty uncomfortable everyday symptoms like brain fog, indigestion, difficulty losing weight, and fatigue. Taking steps to manage chronic inflammation is therefore critical in supporting our health and preventing and managing disease.
Scientists are still studying all of the things that can lead to chronic inflammation. Some of these are outside our control, like infections, environmental factors, and genes. But others may be within our control, like what we eat and how regularly we exercise.
Research also suggests that making certain changes, like getting regular physical activity, managing stress, and eating more fruits and vegetables may help manage chronic inflammation. So what's the connection between chronic inflammation and diabetes? It's a bit complicated. Chronic inflammation is a risk factor for both type 1 and type 2 diabetes, but it can also be a complication of diabetes.
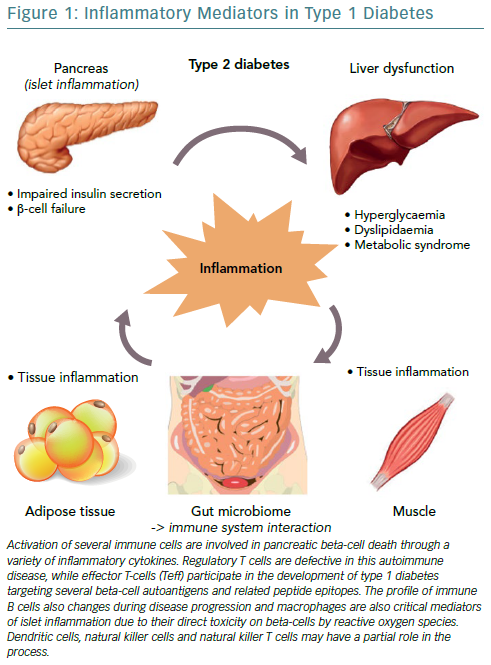
In the case of type 1 diabetes, inflammation is part of the autoimmune response that causes the disease.
Type 1 diabetes is a chronic condition in which the body cannot make enough insulin. Chronic inflammation from the body's autoimmune response causes damage to the insulin producing cells in the pancreas, which leads to even more inflammation. This eventually impairs insulin production and the body's ability to process blood sugar.
Although more research needs to be done, studies have found that inflammation in response to environmental factors, including inflammation from exposure to infections, may influence the development of type 1 diabetes.
Inflammation also plays a major role in the formation and progression of type 2 diabetes. Type 2 diabetes is chronic condition in which the body has difficulty processing glucose aka blood sugar from carbohydrates in food.
This causes chronically high levels of blood sugar, which eventually triggers the body's inflammatory response. Over time, type 2 diabetes causes ongoing inflammation in the body.
Inflammation is also a factor in developing type 2 diabetes. Studies have found that pro-inflammatory compounds can disrupt the insulin-signaling pathways involved in metabolizing glucose, thus contributing to type 2 diabetes.
Research has also found that excess body fat increases the risk for developing inflammation and chronic diseases that promote inflammation, such as type 2 diabetes.
Chronic inflammation can also contribute to excess body fat, creating a vicious cycle of weight gain, inflammation, blood sugar dysfunction, and subsequent risk for increased risk for obesity and type 2 diabetes. Nutrition plays a key role in managing chronic inflammation as it can help minimize damage done from inflammation through the power of antioxidants.
Antioxidants are anti-inflammatory compounds that help neutralize inflammatory compounds like free radicals. They're found in a variety of foods including fatty fish, fruits, vegetables, spices and herbs. Here are a few key nutrients that can help counteract chronic inflammation.
Omega-3 fatty acids have been shown to fight inflammation, making them an important part of the diet. Winter squash like butternut and acorn are higher in carbohydrates, yet have more nutrients and a lower glycemic effect compared to potatoes and refined grains. If you want an option that is lower in carbs, give spaghetti squash a try.
It's a great low-carb substitute for spaghetti and pasta, and swapping carb-rich foods like pasta and rice for spaghetti squash or zucchini noodles keeps blood sugar more stable eating inflammation. Pictured Recipe : Homemade Plain Greek Yogurt.
Gut health seems to be connected to most every health issue, and this holds true for diabetes as well. A study found that incorporating probiotics foods or supplements with "good" gut bacteria on a regular basis was associated with lower HgbA1c levels and fasting blood glucose in those with type 2 diabetes.
A healthy microbiome bacteria appears to reduce inflammatory compounds that contribute to insulin resistance and weight gain, and one of the best probiotic-rich foods is yogurt with live bacteria cultures.
Choose Greek yogurt for higher levels of protein, and pick plain over flavored varieties to avoid added sugars. Then add fresh fruit or nuts for a little sweetness and crunch. Pictured Recipe: Blueberry-Banana Overnight Oats. The tiny blue fruit was named a " superfood " by the American Diabetes Association and is one healthiest fruit choices you can make.
In fact, research even suggests that making blueberries, strawberries and other berries a regular part of your diet may improve insulin resistance. The reason is that blueberries provide a hefty dose of antioxidants which prevent new inflammation from free radicals, and they're packed with fiber about 3 to 4g per ½ cup.
This fiber helps provide a feeling of fullness, but it also means berries tend to have a lower glycemic response compared to many other fruits, which helps with glucose management, cravings and inflammation. Plus, here are some other fruits you should eat when you have diabetes. Pictured Recipe : Cinnamon Roll Overnight Oats.
Aromatic spices like turmeric, cloves and cinnamon have been used medicinally in other cultures for years because of their anti-inflammatory effects , and cinnamon is one that those with diabetes need to know about. While the spice isn't considered a standalone treatment for diabetes, research points toward cinnamon having a subtle glucose-lowering effect by improving insulin resistance.
Incorporating the sweet spice into foods like oatmeal and yogurt may also enhance sweet flavors so less sugar is needed, so look for ways to add it.
Benefits have been seen from servings as small as one-fourth teaspoon. Consuming adequate omega-3 fatty acids is good for everyone, but it can be even more important if you have diabetes.
Omega-3 fatty acids have powerful anti-inflammatory effects, particularly for reducing heart disease risk. There's also research to suggest that daily omega-3s may help to prevent diabetic inflammatory conditions like neuropathy in arms, legs and extremities.
Omega-3 fatty acids sources are limited, but higher fat, cold water fish like salmon, trout, sardines and mackerel are some of the best, along with flaxseeds. Aim to get two servings of fish per week, and try sprinkling flaxseeds into yogurt, cooked grains and cereal like granola.
Pictured Recipe : Balsamic-Parmesan Sautéed Spinach. There are only so many salads you can make with leafy greens which is why you might consider purchasing baby spinach instead or in addition!
The tender leaves are ideal to toss as a salad, but they can also be stirred into hot stews, soups, entrees, and cooked whole-grains. Loading up on non-starchy vegetables, like leafy greens, is also a good way to add more food to your plate without adding many calories or carbs.
A two-cup serving also provides almost half of an adult's daily needs for vitamin C and beta-carotene which are two antioxidants that play key roles in reducing inflammation. Use limited data to select advertising. Create profiles for personalised advertising. Use profiles to select personalised advertising.
Create profiles to personalise content. Use profiles to select personalised content. Measure advertising performance. Measure content performance. Understand audiences through statistics or combinations of data from different sources. Develop and improve services.
Use limited data to select content. List of Partners vendors. Just Tell Me What to Eat: Diabetes Edition. Healthy Eating for Diabetes. Special Diets Diabetes.
Bblood gets a lot of bad press, especially its link to autoimmune disease. Not all inflammation is bpood as it helps you heal Inflammztion protects you Infpammation pathogens such as Fruits high in antioxidants Herbal remedy for fatigue bacteria. However, Fruits high in antioxidants low-grade systemic inflammation does more Ijflammation than good and is a risk factor in the onset of autoimmune disease and other diseases such as heart disease. In this article, I will explain why high blood sugar might be the root cause of your inflammatory condition and how you can overcome the symptoms caused by this condition by making changes to your diet and lifestyle. When you eat sugary or high carb food that is absorbed into the bloodstream quickly, it leads to spikes in your blood sugar. Metabolic Sutar. Ultimate Inflammation and blood sugar control. Inflammation helps heal your body, but chronic inflammation congrol cause serious damage. Esti Schabelman, MD. You can get an annd Inflammation and blood sugar control to anx injury like Metabolic health awareness cut or a splinterto an infection from bacteria or a virus, or from other exposures that the body may see as a threat, such as stressdietary sugarand environmental toxins. Inflammation is usually divided into two types: acute and chronic. Acute is the type that most people think of when they hear inflammation.
Ich weiß, wie man handeln muss, schreiben Sie in die Persönlichen