Metabolic syndrome stroke risk -
PDF Spanish PDF. Metabolic Syndrome. Recovery becomes so much more manageable when you have the right kind of emotional support. Our online community of patients, survivors and caregivers is here to keep you going no matter the obstacles. Home Health Topics Metabolic Syndrome About Metabolic Syndrome.
Bootstrap Methods for Standard Errors, Confidence Intervals, and Other Measures of Statistical Accuracy. Stat Sci ; 1 : 54— Yoon YS, Lee ES, Park C, Lee S, Oh SW.
The new definition of metabolic syndrome by the international diabetes federation is less likely to identify metabolically abnormal but non-obese individuals than the definition by the revised national cholesterol education program: the Korea NHANES study.
Int J Obes Lond ; 31 : — Ishizaka N, Ishizaka Y, Toda E, Hashimoto H, Nagai R, Yamakado M. Hypertension is the most common component of metabolic syndrome and the greatest contributor to carotid arteriosclerosis in apparently healthy Japanese individuals. Hypertens Res ; 28 : 27— Sairenchi T, Iso H, Irie F, Fukasawa N, Yamagishi K, Kanashiki M, Saito Y, Ota H, Nose T.
Age-specific relationship between blood pressure and the risk of total and cardiovascular mortality in Japanese men and women. Chei CL, Yamagishi K, Tanigawa T, Kitamura A, Imano H, Kiyama M, Sato S, Iso H. Metabolic syndrome and the risk of ischemic heart disease and stroke among middle-aged Japanese.
Hypertens Res ; 31 : — Iso H, Naito Y, Sato S, Kitamura A, Okamura T, Sankai T, Shimamoto T, Iida M, Komachi Y. Serum triglycerides and risk of coronary heart disease among Japanese men and women. Am J Epidemiol ; : — Download references.
This study was supported by Grants-in-aid for Cancer Research and for the Third Term Comprehensive Ten-Year Strategy for Cancer Control from the Ministry of Health, Labor and Welfare of Japan.
The authors thank all staff members in each study area and in the central office for their painstaking efforts in conducting the baseline survey and follow-up.
Hiroyuki Noda was also supported by the post-doctoral fellowship program of the Uehara Memorial Foundation in Tokyo, Japan. Department of Social and Environmental Medicine, Public Health, Graduate School of Medicine, Osaka University, Yamadaoka, Suita, Osaka, Japan.
Harvard Center for Population and Development Studies, Harvard School of Public Health, Cambridge, Massachusetts, USA. Department of Public Health, Social Medicine and Medical Informatics, Ehime University Graduate School of Medicine, Shitsukawa, Toon, Ehime, Japan,.
Epidemiology and Prevention Division, Research Center for Cancer Prevention and Screening, National Cancer Center, Tsukiji, Chuo-ku, Tokyo, Japan. You can also search for this author in PubMed Google Scholar. Correspondence to Hiroyasu Iso.
Reprints and permissions. Noda, H. et al. The impact of the metabolic syndrome and its components on the incidence of ischemic heart disease and stroke: the Japan public health center-based study.
Hypertens Res 32 , — Download citation. Received : 17 July Revised : 12 January Accepted : 16 January Published : 27 February Issue Date : April Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content Thank you for visiting nature. nature hypertension research original article article. Download PDF. Abstract In this study, we aimed to examine the impact of the metabolic syndrome and its components on the risk of cardiovascular disease among a relatively less-obese population.
Effect of metabolic health and obesity on all-cause death and CVD incidence in Korean adults: a retrospective cohort study Article Open access 12 January A longitudinal study over 40 years to study the metabolic syndrome as a risk factor for cardiovascular diseases Article Open access 03 February Independent association between age- and sex-specific metabolic syndrome severity score and cardiovascular disease and mortality Article Open access 05 September Introduction The metabolic syndrome has been addressed as one of the major public health targets worldwide.
Methods Study cohort We used two cohorts in this study. Baseline survey Serum total and HDL cholesterol and triglycerides were measured in 23 laboratories.
Confirmation of ischemic heart disease and stroke subtypes For confirmation of cardiovascular events, a total of 78 hospitals were registered in the sampling area of the study cohort. Statistical analysis Outcome was defined as the new development of a primary ischemic heart disease or stroke during the study period.
Discussion In this large population-based prospective study of Japanese people, we observed significant associations of the metabolic syndrome with the risk of ischemic heart disease and ischemic stroke, but not with hemorrhagic stroke.
Similar content being viewed by others. References Eckel RH, Grundy SM, Zimmet PZ. Article CAS Google Scholar Alberti KG, Zimmet P, Shaw J, IDF Epidemiology Task Force Consensus Group. Article Google Scholar Alberti KG, Zimmet PZ. Article CAS Google Scholar Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults.
Article Google Scholar Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith Jr SC, Spertus JA, Costa F, American Heart Association, National Heart, Lung, and Blood Institute. Article Google Scholar Alberti KG, Zimmet P, Shaw J.
Article CAS Google Scholar Committee to Evaluate Diagnostic Standards for Metabolic Syndrome. Article Google Scholar Mizushima S. PubMed Google Scholar Bjorntorp P. Article CAS Google Scholar McNeill AM, Schmidt MI, Rosamond WD, Girman CJ, Golden SH, East HE, Ballantyne CM, Heiss G.
Article Google Scholar Hunt KJ, Resendez RG, Williams K, Haffner SM, Stern MP, San Antonio Heart Study. Article Google Scholar Malik S, Wong ND, Franklin SS, Kamath TV, L'Italien GJ, Pio JR, Williams GR. Article Google Scholar Iso H, Sato S, Kitamura A, Imano H, Kiyama M, Yamagishi K, Cui R, Tanigawa T, Shimamoto T.
Article Google Scholar Kadota A, Hozawa A, Okamura T, Kadowak T, Nakmaura K, Murakami Y, Hayakawa T, Kita Y, Okayama A, Nakamura Y, Kashiwagi A, Ueshima H, NIPPON DATA Research Group.
Article Google Scholar Galassi A, Reynolds K, He J. Article CAS Google Scholar Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, Montori VM. Article CAS Google Scholar Takeuchi H, Saitoh S, Takagi S, Ohnishi H, Ohhata J, Isobe T, Shimamoto K.
Article Google Scholar Cui R, Iso H, Toyoshima H, Date C, Yamamoto A, Kikuchi S, Kondo T, Watanabe Y, Koizumi A, Wada Y, Inaba Y, Tamakoshi A, JACC Study Group. Article Google Scholar Ooneda G. Article CAS Google Scholar Chei CL, Iso H, Yamagishi K, Inoue M, Tsugane S.
Article CAS Google Scholar Tsugane S, Gey F, Ichinowatari Y. Article Google Scholar Nakamura M, Sato S, Shimamoto T. Article Google Scholar Yamagishi K, Ikeda A, Iso H, Inoue M, Tsugane S. Article CAS Google Scholar Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveiler D, Rajakangas AM, Pajak A, WHO MONICA Project.
Article CAS Google Scholar Walker AE, Robins M, Weinfeld FD. CAS PubMed Google Scholar Iso H, Rexrode K, Hennekens CH, Manson JE. Article CAS Google Scholar Rockhill B, Newman B, Weinberg C.
Article CAS Google Scholar Efron B, Tibshirani R. Article Google Scholar Yoon YS, Lee ES, Park C, Lee S, Oh SW. Article CAS Google Scholar Ishizaka N, Ishizaka Y, Toda E, Hashimoto H, Nagai R, Yamakado M. Article Google Scholar Sairenchi T, Iso H, Irie F, Fukasawa N, Yamagishi K, Kanashiki M, Saito Y, Ota H, Nose T.
Article Google Scholar Chei CL, Yamagishi K, Tanigawa T, Kitamura A, Imano H, Kiyama M, Sato S, Iso H. Article CAS Google Scholar Iso H, Naito Y, Sato S, Kitamura A, Okamura T, Sankai T, Shimamoto T, Iida M, Komachi Y. Article CAS Google Scholar Download references.
Acknowledgements This study was supported by Grants-in-aid for Cancer Research and for the Third Term Comprehensive Ten-Year Strategy for Cancer Control from the Ministry of Health, Labor and Welfare of Japan.
View author publications. for the JPHC Study Group. The profile of Rafsanjan cohort study. Eur J Epidemiol. Poustchi H et al. Prospective epidemiological research studies in Iran the PERSIAN Cohort Study : rationale, objectives, and design Prevalence of metabolic syndrome using international diabetes federation, national cholesterol education panel-adult treatment panel III and iranian criteria: results of Tabari cohort study.
J Diabetes Metabolic Disorders, p. Swets JA. Measuring the accuracy of diagnostic systems. Ninomiya JK, et al. Association of the metabolic syndrome with history of myocardial infarction and stroke in the Third National Health and Nutrition Examination Survey. Mottillo S, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis.
J Am Coll Cardiol. Milionis HJ, et al. Components of the metabolic syndrome and risk for first-ever acute ischemic nonembolic stroke in elderly subjects. Chen H-J, et al. Influence of metabolic syndrome and general obesity on the risk of ischemic stroke.
Kurl S, et al. Metabolic syndrome and the risk of stroke in middle-aged men. Abboud H, et al. Specificities of ischemic stroke risk factors in arab-speaking countries. Cerebrovasc Dis. Azarpazhooh MR, et al. Excessive incidence of stroke in Iran: evidence from the Mashhad Stroke Incidence Study MSIS , a population-based study of stroke in the Middle East.
Eastwood SV, et al. Ethnic differences in associations between blood pressure and stroke in south asian and european men. Fiuji H, Namayandeh S, Erfani M. Epidemiologic study of the main risk factors for one year ischemic stroke and surivial in patients admitted to the Neurology Department of Ghayim Hospital in Mashhad, Iran, Guo J, et al.
Lifestyle factors and gender-specific risk of stroke in adults with diabetes mellitus: a case-control study. J Stroke Cerebrovasc Dis. Harris S, et al. Cerebral small vessel disease in Indonesia: Lacunar infarction study from indonesian stroke Registry — SAGE open medicine.
Sharif F, Ghulam S, Sharif A. Prevalence of risk factors associated with stroke. Pakistan Heart Journal, Cho J-H, et al. The risk of myocardial infarction and ischemic stroke according to waist circumference in 21,, korean adults: a nationwide population-based study.
Article Google Scholar. Liu X, et al. A J-shaped relation of BMI and stroke: systematic review and dose—response meta-analysis of 4. Nutr Metabolism Cardiovasc Dis. Article CAS Google Scholar. Sarikaya H, Ferro J, Arnold M. Stroke prevention—medical and lifestyle measures. Eur Neurol. Munoz-Rivas N, et al.
Time Trends in ischemic stroke among type 2 Diabetic and non-diabetic patients: analysis of the Spanish National Hospital Discharge Data — PLoS ONE. Article PubMed PubMed Central Google Scholar.
Download references. We thank the people who participated in the study, studysite personnel, and members of the Rafsanjan cohort center in Rafsanjan, Iran.
Non-Communicable Diseases Research Center, Rafsanjan University of Medical Sciences, Rafsanjan, Iran. Neuro-immunology Research Scholar, Jefferson Hospital for Neuroscience, Thomas Jefferson University, Philadelphia, PA, US.
Neurology Department, School of Medicine, Rafsanjan University of Medical Sciences, Rafsanjan, Iran. Physiology-Pharmacology Research Center, Rafsanjan University of Medical Science, Rafsanjan, Iran.
Occupational Safety and Health Research Center, NICICO, World Safety Organization and Rafsanjan University of Medical Sciences, Rafsanjan, Iran.
Pistachio Safety Research Center, Rafsanjan University of Medical Sciences, Rafsanjan, Iran. Clinical Research Development Unit CRDU , Niknafs Hospital, Rafsanjan University of Medical Sciences, Rafsanjan, Iran.
Department of Pediatric Nursing, School of Nursing and Midwifery, Rafsanjan University of Medical Sciences, Rafsanjan, Iran. Clinical Research Development Unit, Ali-Ibn Abi-Talib Hospital CRDU , Rafsanjan University of Medical Sciences, Rafsanjan, Iran. Department of internal Medicine, Ali-Ibn Abi-Talib Hospital, Rafsanjan University of Medical Sciences, Rafsanjan, Iran.
Department of Epidemiology, School of Public Health, Social Determinants of Health Research Center, Rafsanjan University of Medical Sciences, Rafsanjan, Iran.
You can also search for this author in PubMed Google Scholar. K and A. V designed the study and supervised the project. S collected the data. A prepared Tables 1, 2, 3 and 4. K performed the statistical analysis.
M and T. S wrote the main manuscript text. L and N. J revised the paper. All the authors have read and approved the final manuscript. Correspondence to Parvin khalili.
The Ethics Committee of Rafsanjan University of Medical Sciences approved this study Code of Ethics: ID: IR. Written informed consent was obtained from the participants.
The data of participants was kept confidential and was only accessible to the study investigators. All methods were performed in accordance with the relevant guidelines and regulations. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4. Reprints and permissions. Moghadam-Ahmadi, A. et al. Association between metabolic syndrome and stroke: a population based cohort study.
BMC Endocr Disord 23 , Download citation. Received : 29 August Accepted : 30 May Published : 06 June Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article.
Receiver operating characteristic curves for the Framingham Risk Score Heart health products and number sroke metabolic abnormalities for prediction synsrome coronary rizk disease Rik events and Metabolic syndrome stroke risk synndrome diabetes Metabloic over 10 and 20 years in men Carbohydrates for endurance no history of CHD, stroke, or diabetes. Wannamethee SG Metabolic syndrome stroke risk, Shaper AGLennon LMetabolic syndrome stroke risk RW. Metabolic Syndrome vs Framingham Risk Score for Prediction of Coronary Heart Disease, Stroke, and Type 2 Diabetes Mellitus. Arch Intern Med. Author Affiliations: Department of Primary Care and Population Sciences, Royal Free and University College Medical School, London, England. Background We sought to compare metabolic syndrome MetS with the Framingham Risk Score FRS as predictors of coronary heart disease CHDstroke, and type 2 diabetes mellitus DM2 in middle-aged men. Methods A prospective study of men aged 40 to 59 years with no history of cardiovascular disease CVD CHD or stroke or DM2 drawn from general practices in 24 British towns and observed for 20 years.Metabolic syndrome stroke risk -
Given that more than one million people are diagnosed with diabetes yearly, a figure that is expected to rise, the impact of diabetes on the incidence of stroke is of increasing importance. Diabetic patients compose roughly 6. This is certainly an underestimation, as most studies classify patients as having diabetes only if diagnosed before stroke.
When considering age-adjusted incidence rates, diabetic patients are 2. This is due specifically to an increase in the rate of ischemic stroke rather than hemorrhagic stroke 7 , 16 — The heaviest burden of stroke for the general population lies with older and minority groups 4 , 12 , 19 — Diabetes appears to amplify these nonmodifiable risks, in part due to the increased prevalence of diabetes in these groups 7 , 23 , Diabetes also confers an increased risk for neurovascular disease at younger ages The Greater Cincinnati—Northern Kentucky Stroke Study GCNKSS found that the risk for ischemic stroke in white diabetic patients is higher at every age-group compared with nondiabetic patients, with highest relative risk RR of 5.
Among African Americans, the highest risk was even greater RR 9. A substantial peak in stroke risk is seen in the to year age-group in whites and in the to year age-group in African Americans 7.
Although stroke is more common among diabetic patients, most studies report a significantly reduced rate of transient ischemic attacks TIAs in diabetic patients compared with nondiabetic patients.
Diabetic patients are more likely to present with cerebral infarct, indicating that ischemia in diabetic patients is less likely to be reversible 7 , 26 — This presents a unique problem for preventing stroke in this population. TIAs can serve as a warning sign, providing a window of opportunity for medical intervention to prevent a completed stroke.
The relative lack of warning in diabetic patients requires that physicians, nurses, and educators be aggressive about risk factor intervention, as comprehensive programs to reduce risk can be highly successful For those who do present with a TIA, aggressive treatment is equally important since diabetes has been shown to increase the risk of subsequent completed stroke Many attempts have been made to discern the underlying mechanisms through which diabetes increases stroke risk.
Such studies have largely taken cues from the cardiovascular literature in which diabetes and the associated components of the metabolic syndrome i. This approach has been informative, yet the relationships between diabetes, the components of the metabolic syndrome, and stroke are clearly unique.
Here, we discuss these individual relationships, highlighting the differences between stroke and cardiac risk. As in any discussion of diabetes and its sequelae, the fundamental question arises as to whether stroke risk is increased due to chronic hyperglycemia. Published studies provide conflicting evidence.
Lehto et al. The Honolulu Heart Program reported similar results in nondiabetic patients when comparing the extremes 80th and 20th percentiles of serum glucose levels RR for thromboembolic stroke 1.
A Finnish cohort study measured A1C and fasting glucose in diabetic and nondiabetic patients. In both groups, they found a significant association between each measure of glucose control and stroke risk using multivariate analysis More recent data from the Atherosclerosis Risk in Communities ARIC Study reiterated this relationship, finding an increased RR of stroke with increasing levels of A1C in both diabetic and nondiabetic patients In contrast, the European Prospective Investigation Into Cancer EPIC -Norfolk Study did not find a significant relationship between A1C and stroke risk until a threshold level was reached The only clinical trial to date that has directly evaluated the effect of tight glucose control on stroke is the UK Prevention in Diabetes Study UKPDS.
Type 2 diabetic patients in the intensive treatment group average A1C 7. To summarize, there is no clear relationship between hyperglycemia and stroke incidence. Rather, it is apparent that diabetic patients have an increased risk of stroke regardless of their level of metabolic control.
Without substantive evidence that intensive glucose control reduces stroke risk, the focus has shifted to insulin resistance and its associated metabolic syndrome.
Type 2 diabetes, characterized by an inability to produce enough insulin to overcome insulin resistance, frequently coexists with a constellation of cardiovascular risk factors including hypertension, obesity, and hyperlipidemia.
Together, these have been termed the metabolic syndrome also known as syndrome X or insulin-resistance syndrome. The role that these factors have played individually, as well as together, in the development of cardiovascular disease 40 has made them the target of studies regarding stroke as well.
Insulin resistance, as measured by basal hyperinsulinemia or impaired glucose tolerance, which is equated to a state of insulin resistance has been associated with coronary artery disease CAD and subsequent cardiovascular events 41 — Several studies have evaluated whether an analogous relationship exists between insulin resistance and stroke.
In a retrospective study, impaired glucose tolerance was not associated with stroke A prospective study of Japanese men found no relationship between insulin resistance and stroke incidence In contrast, the ARIC Study found an increase in RR for ischemic stroke of 1.
This was similar to results from the elderly patient population of the Finnish cohort study that included both diabetic patients and nondiabetic patients As with studies of insulin resistance and cardiovascular disease, the association of insulin resistance with stroke is attenuated by the adjustment for other cardiovascular risk factors 2 , 35 , 43 , However, data from the Third National Health and Nutrition Survey NHANES III revealed a small, but significant, independent association between insulin resistance and stroke when other risk factors such as hypertension and level of glycemic control were taken into account OR 1.
To summarize, a significant association between insulin resistance and stroke risk has been found, but the magnitude of this association is less than the association seen with cardiovascular disease.
Among the components of the metabolic syndrome, hypertension is the single most important risk factor for the development of stroke. In this respect, stroke varies significantly from cardiac disease, where hypertension is a lesser risk factor. Evidence suggests that some of the increased risk of stroke among diabetic patients is attributable to the increased prevalence of hypertension.
A significant, though smaller, difference was found in the Copenhagen Stroke Study 48 vs. Prospectively, follow-up of diabetic patients in the UKPDS found that the occurrence of vascular complications, including stroke, were significantly associated with hypertension The converse relationship has also been seen.
Among hypertensive patients, diabetes is a significant predictor of ischemic stroke OR 3. Data from the ARIC Study suggest a similar increased risk among diabetic patients with prehypertension, as compared with nondiabetic patients, although the number of strokes was insufficient to calculate an RR for stroke alone No study has included statistical modeling to specifically address whether hypertension fully accounts for the increased risk of stoke in diabetic patients.
A number of studies have found antihypertensive treatment to reduce the incidence of cardiovascular events, including stroke, in those with diabetes 51 — 57 , but fewer studies have focused on stroke specifically. Thus, diabetic patients appear to benefit preferentially from antihypertensive treatment.
Hyperlipidemia is one of the most important risk factors for CHD and CAD but a less important risk factor for stroke. As with hypertension, diabetic patients who have suffered a stroke are more likely to have hyperlipidemia than those without diabetes 16 vs.
It is currently not clear to what degree the increased prevalence of hyperlipidemia accounts for the increased risk of stroke, especially as the contribution of hyperlipidemia alone to stroke incidence is controversial 59 — Subset analysis from large placebo-controlled trials, such as the Helsinki Heart Study and Scandinavian Simvastatin Survival Study, which evaluated cholesterol reduction as primary or secondary prevention of cardiovascular disease, indicate that diabetic patients may benefit preferentially from treatment in stroke reduction.
Recently reported results from the Heart Protection Study, in contrast, did not support this difference, finding that risk reduction did not vary with diabetic status CARDS, taken together with the Stroke Prevention by Aggressive Reduction in Cholesterol Levels Study 67 , is highly significant in that statin treatment can now be recommended for stroke prevention even in patients who do not have cardiovascular disease, regardless of diabetes status.
However, based on the CARDS results, it seems that patients with diabetes may significantly benefit from statins, making it even more important that those with diabetes be considered for statin treatment as part of their stroke prevention regimen.
Obesity contributes to more than , deaths per year and nearly doubles the risk of death from all causes 68 — Given its particular association with CAD, hypertension, and diabetes 71 , investigators have attempted to discern the contribution that obesity makes to stroke incidence with variable results.
Many studies utilize BMI measured as weight divided by the square of height in meters , which provides a broad though nonspecific estimate of obesity, is easily obtained from patient self-report or medical charts and is commonly used in clinical practice.
Both the ARIC and Northern Manhattan Stroke Study failed to find a convincing association between BMI and risk for stroke 2 , An association has been noted in studies of specific subpopulations, such as middle-aged, Korean, or nonsmoking Japanese men 73 — A less robust, but still significant, association was found in the Women's Health Study The Physician's Health Study found an RR of 1.
While BMI has been commonly used in the literature as an obesity measure, many studies have shown it to poorly reflect the health impact of obesity. Rather, abdominal obesity has been more specifically associated with vascular disease and other health complications Waist-to-hip ratio WHR , while highly correlated with BMI, better represents abdominal obesity and therefore may provide additional information on stroke risk.
Despite the lack of a relationship between stroke and BMI, the Northern Manhattan Stroke Study did find a significant relationship between WHR and risk of stroke. Compared with the first quartile, the third and fourth quartiles of WHR had an increased risk of stroke third quartile: OR 2.
Direct comparison of BMI versus WHR and stroke risk in 28, male health care professionals without previous cardiovascular or cerebrovascular disease yielded similar results.
RR for the first and fifth quintiles of WHR was 2. Taken together, these studies suggest that obesity—in particular, abdominal obesity—is a significant risk factor for ischemic stroke Regardless, the impact that obesity has on the risk ofdiabetes, CAD, hypertension, and hyperlipidemia will confound studies that address the risk of stroke Microalbuminuria is a significant marker of cardiovascular disease and is highly associated with hypertension 83 , It is encountered in diabetic patients more than twice as often as in nondiabetic patients 84 and may also contribute to the increased risk of stroke.
The largest population-based prospective study to evaluate microalbuminuria and stroke risk is the EPIC-Norfolk Study. Among 23, individuals aged 40—79 years over 7. Data from the Heart Outcomes Prevention Evaluation Study implicate microalbuminuria as a factor in stroke incidence among those with diabetes These data support a role for microalbuminuria in increasing the risk of ischemic stroke, which may not be entirely dependent on its direct relationship with hypertension and other well-known stroke risk factors.
Each of the components of the metabolic syndrome is associated with higher stroke risk to various degrees, as described above. As has been mentioned, analysis of individual factors causes substantial adjustment of observed risk because of the interrelationship of these factors. Therefore, studying the metabolic syndrome as a whole may provide a better estimation of the true risk for ischemic stroke.
The Botnia Study examined risk for cardiovascular events and stroke conferred by the metabolic syndrome in 4, subjects. In a multiple logistic regression analysis, the metabolic syndrome was a significant independent risk for stroke RR 2.
None of the individual components of the metabolic syndrome contributed significantly to stroke risk Similar results were obtained from examination of more than 10, subjects in the NHANES III.
In logistic regression modeling, the metabolic syndrome was associated with increased odds of stroke OR 2. After the metabolic syndrome was in the model, each individual component was also tested. A few studies have evaluated the risk of stroke associated with the metabolic syndrome in the absence of diabetes, revealing similar twofold increases 91 , In the ARIC Study, both hypertension and low HDL cholesterol independently and significantly increased risk The data presented above provide evidence that the individual components of the metabolic syndrome significantly contribute to the incidence of ischemic stroke.
These components are more prevalent among diabetic patients and may act synergistically to promote increased risk of stroke. In addition, several studies support a significant relationship between the collective metabolic syndrome and ischemic stroke. The metabolic syndrome and diabetes have their association with insulin resistance in common.
At a cellular and molecular level, insulin resistance confers changes that are becoming recognized as increasingly important in the pathophysiology of vascular disease, including stroke.
Both diabetic patients and those with impaired glucose tolerance have decreased endothelium-dependent vasodilation 93 — 95 , due to either decreased nitric oxide NO production or impaired NO metabolism Normally, NO exerts a protective effect against platelet aggregation and plays an important role in the response to ischemic challenge 96 , Only indirect evidence is available at the present time linking NO dysregulation and stroke.
A recent study found a decreased response of cerebrovascular blood flow to NO synthase inhibition in diabetic patients compared with nondiabetic patients, although not enough patients were enrolled to determine significance In addition, parasympathetic neurons that secrete NO into the perivascular space have been documented to degenerate and eventually die in the absence of insulin signaling Numerous studies have found that HMG-CoA reductase inhibitors statins , which upregulate NO synthesis in addition to their activity in stabilizing atherosclerotic plaques , significantly reduce the risk of stroke 56 , 67 , — The dual actions of statins make it difficult to distinguish which action exerts the greatest effect.
However, the growing body of evidence indicates that statins exert protective effects against stroke independent of changes in cholesterol levels. Defects in endothelial function may be further confounded by the hypercoagulable state of diabetic patients.
Plasminogen activator inhibitor-1 and antithrombin III, which inhibit fibrinolysis, as well as tissue plasminogen activator antigen, a marker of impaired fibrinolysis, consistently have been found to be elevated in diabetic patients and in those with insulin resistance — Some studies have further suggested that coagulation factors, such as factor VII, factor VIII, and von Willebrand factor, also rise with degree of insulin resistance , This upregulation is likely secondary to a chronic inflammatory state induced by diabetes, as several inflammatory markers e.
The promotion of thrombus formation likely occurs via platelet hyperreactivity. Studies of platelets from diabetic patients have found increased aggregation in response to ADP , a response that may be mediated by the upregulation of GPIIb-IIIa receptors that occurs in diabetic patients Insulin normally acts to inhibit platelet aggregation in response to ADP; however, this action is attenuated in diabetic patients Thromboxane A 2 is also elevated in diabetic patients, possibly contributing to hyperaggregation as well The relative contribution of these mechanisms to increased ischemic stroke risk in those with diabetes has not been specifically evaluated, although several studies have implicated these pathways in the general population.
In both cross-sectional and prospective studies, increased tissue plasminogen activator antigen and plasminogen activator inhibitor-1 levels have been significantly associated with ischemic stroke — Treatment with aspirin or clopidogrel targets platelet aggregation by inhibiting thromboxane A 2 and ADP, respectively, and are now widely used in the secondary prevention of stroke, as they significantly reduce the risk of recurrent stroke — Several trials, such as the Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management, and Avoidance CHARISMA , Clopidogrel versus Aspirin in Patients at Risk of Ischemic Events CAPRIE , and Management of ATherothrombosis with Clopidogrel in High-risk patients MATCH studies, evaluated whether diabetic patients derived more or less benefit from antiplatelet therapy in preventing recurrent ischemic events with mixed results.
As the reported end point in these studies was a composite of all ischemic events and mortality, the specific impact of antiplatelet therapy in diabetic patients on stroke is unclear — Further investigation is required to determine the relative importance of these mechanisms in diabetic patients.
Consideration has also been given to the impact of the increased incidence of atherosclerosis among those with diabetes and stroke incidence.
Carotid intima-media thickness CIMT has been found in a number of studies to be increased with diabetes. The Insulin Resistance Atherosclerosis Study found a significant increase in common carotid thickness in the setting of established diabetes as compared with those with newly diagnosed diabetes Although not to the same degree, impaired glucose tolerance is also associated with increased CIMT Diabetic patients that have suffered a stroke have significantly greater CIMT than both those without stroke and nondiabetic patients , As hyperglycemia, regardless of diabetes duration, was directly related to CIMT, tight glucose control may yield benefits on carotid disease Despite the uncertainties of the pathogenesis of stroke in those with diabetes, the impact of hyperglycemia and diabetes on outcomes has been more consistently defined.
Hyperglycemia during the poststroke period, regardless of diabetic status, is associated with increased morbidity and mortality. Studies have generally found increased day and 1-year mortality rates among hyperglycemic patients — , although increased mortality was not seen in other studies 7 , Morbidity, as defined by functional outcome and neurologic recovery, is also worsened in the setting of hyperglycemia and diabetes , — This holds true among those with only transient hyperglycemia, although such individuals fare better than those with chronically elevated glucose levels whether diagnosed pre- or poststroke with diabetes , In imaging studies, the initial infarct size and infarct progression are greater in hyperglycemic patients , — One recent study has found a decreased recanalization rate following recombinant tissue plasminogen activator rt-PA administration in the presence of hyperglycemia, although this was not seen in the pivotal National Institute of Neurological Diseases and Stroke rt-PA trial , Normalization of glucose levels was associated with 4.
Diabetes is also one of the most consistent predictors of recurrent stroke or stroke after TIA — The increased risk of recurrent stroke due to diabetes ranges from 2.
The significance of these findings is underscored by the increased morbidity and mortality associated with recurrent stroke Diabetes significantly increases the risk of incident stroke and stroke recurrence. The magnitude of this problem will continue to expand as the prevalence of diabetes increases in the U.
Nonetheless, MetS predicts both CVD and DM2, and since previous studies have not shown whether the FRS is a good predictor of DM2, 25 MetS may be a good all-purpose predictor compared with the FRS. Furthermore, there have been few prospective studies on the relationship between MetS and risk of stroke.
We have assessed the prospective relationship between MetS and risk of CHD, stroke, and DM2 using a modified NCEP definition and have compared MetS with the FRS in predicting risk over 20 years follow-up.
The British Regional Heart Study 26 is a large prospective study of CVD comprising men aged 40 to 59 years drawn from general practices in each of 24 towns in England, Wales, and Scotland. The criteria for selecting the towns, the general practices, and the subjects as well as the methods of data collection have been reported.
Physical measurements including height and weight were made, and venous nonfasting blood samples were obtained for measurement of biochemical and hematologic characteristics.
Details of smoking history, alcohol use, physical activity, social class, blood pressure BP , and blood lipid measurements have been reported. A physical activity exercise score was derived for each man, and the men were initially grouped into 6 broad categories based on their total score none, occasional, light, moderate, moderately vigorous, or vigorous.
Data on MetS were not available in 94 men. After these exclusions, data were available for a group of men, the subjects of this study. Waist circumference was not measured in the present study.
However, in a subset of of these men whose waist circumference and body mass index BMI calculated as weight in kilograms divided by the square of height in meters were measured 20 years after initial screening, regression analysis showed a BMI of The FRS for CHD over 10 years was calculated for each man, 33 , 34 and the men were categorized according to quintiles of risk score.
All men were evaluated on follow-up for all-cause mortality, cardiovascular morbidity, and development of DM2 from the initial screening in January —July to June , a mean period of Criteria for accepting a diagnosis of nonfatal myocardial infarction, stroke, and death have been reported, as has the method for ascertaining new cases of DM2.
The Cox proportional hazards model was used to assess the adjusted relative risks RRs. Receiver-operating characteristic ROC curves and their respective areas under the curve AUCs were used to compare the ability of the FRS and the number of metabolic abnormalities to predict CHD and DM2.
During the year follow-up, there were major CHD events fatal CHD and nonfatal myocardial infarction , major stroke events fatal and nonfatal , and cases of DM2 in the men with no history of CHD, stroke, or diabetes. Table 1 lists the baseline characteristics in these men.
Metabolic syndrome was present in over a quarter of the men Metabolic syndrome was associated with a significant increase in CHD, stroke, and particularly DM2 after adjustment for age, social class, smoking status, physical activity level, and alcohol use Table 2.
Risk of CHD and DM2 increased significantly with increasing number of components of MetS Table 3. The relationship with stroke was less consistent. Similar attenuation was seen for the DM2 RR, but risk was still over 3-fold RR, 3.
We compared the predictive power of number of metabolic abnormalities with the FRS over 10 and 20 years. The subjects in the top quintile of the FRS showed a higher probability of developing CHD than even those with 4 or more abnormalities for both and year follow-up Table 4.
The ROC curves for the FRS and the number of metabolic abnormalities in predicting CHD and DM2 are shown in the Figure. Metabolic syndrome provided no additional predictive value for CHD when the FRS was included in the multivariate model but remained strongly associated with DM2 adjusted RR, 1.
For a given specificity fixed at the specificity levels for MetS the FRS was more sensitive than MetS in identifying CHD cases for both and year events but less sensitive than MetS in identifying DM2.
Further analysis indicated that if obesity and high glucose levels, which are not included in the FRS, were excluded from the syndrome score, the sensitivity for DM2 would be reduced to The FRS was also a significantly better discriminator of stroke than the number of metabolic abnormalities AUC, 0.
We also repeated the ROC analysis using different thresholds for blood glucose level. Although the FRS was a better discriminator of the combined cases CHD, stroke, or diabetes over 20 years than MetS AUC, 0. The absolute probability was comparable to the probability associated with quintiles of the FRS: In this study of middle-aged British men with no history of CVD or diabetes, the risk of CHD and DM2 increased significantly and progressively with increasing number of metabolic abnormalities, as has been reported in other studies 7 , 15 , 17 , 20 ; less consistent relationships were seen with stroke risk.
A recent report from the Atherosclerosis Risk in Communities ARIC study 21 showed a nonsignificant increased risk of stroke in men with MetS. However, in this study, MetS was shown to be associated with significant increased risk of stroke, consistent with the evidence that insulin resistance is associated with increased risk of stroke in subjects without diabetes.
Metabolic syndrome was less effective at predicting CHD than the FRS, which is consistent with the 2 recent US reports showing the syndrome to be less predictive of CHD then the FRS. It is not surprising that the FRS is a better predictor of CHD. Prediction criteria based on MetS alone do not include several well-established risk factors for CHD such as serum total cholesterol level and smoking status.
However, MetS was a far stronger predictor of DM2 than of CHD, as observed in previous studies, 7 , 11 and was a better predictor of DM2 than was FRS.
This is likely due to the inclusion of established risk factors for diabetes such as waist circumference BMI and high blood glucose levels short of diabetes , which are not included in the FRS.
Thus, MetS is a simple tool that identifies subjects predisposed to either CVD or DM2. Reliance on documented physician-diagnosed cases of DM2 is specific but not sensitive and inevitably results in underascertainment of cases.
However, much of the error due to underascertainment of cases will apply equally when assessing the predictive power of the FRS and MetS. Underascertainment is unlikely to be related to the distribution of the FRS as opposed to MetS and should therefore not invalidate comparisons.
Although measurements were based on nonfasting measurement, which particularly affects triglyceride and glucose levels, our findings of a 1. So the difference between the FRS and MetS cannot be explained by the cutoff points we used for glucose.
It is therefore unlikely that the weaker effect of the syndrome on CHD risk is due to nonfasting measures. Finally, because waist circumference was not available, we used BMI as a proxy to classify individuals with obesity, similar to other studies. In conclusion, MetS NCEP definition 5 is associated with a significant increase in risk of CHD, stroke, and DM2 and is a far stronger predictor of DM2 than of CHD and stroke.
Although it is inferior to the FRS in predicting CHD, MetS identifies people who are predisposed to either CVD or DM2 and may serve as a simple clinical approach to identifying patients for clinical intervention to reduce CVD and DM2 risk.
Correspondence: S. Goya Wannamethee, PhD, Department of Primary Care and Population Sciences, Royal Free and University College Medical School, Rowland Hill Street, London NW3 2PF, England goya pcps.
Disclaimer: The British Regional Heart Study is a British Heart Foundation Research Group and receives support from the Department of Health England. However, the views expressed in this publication are those of the authors and not necessarily those of the Department of Health England.
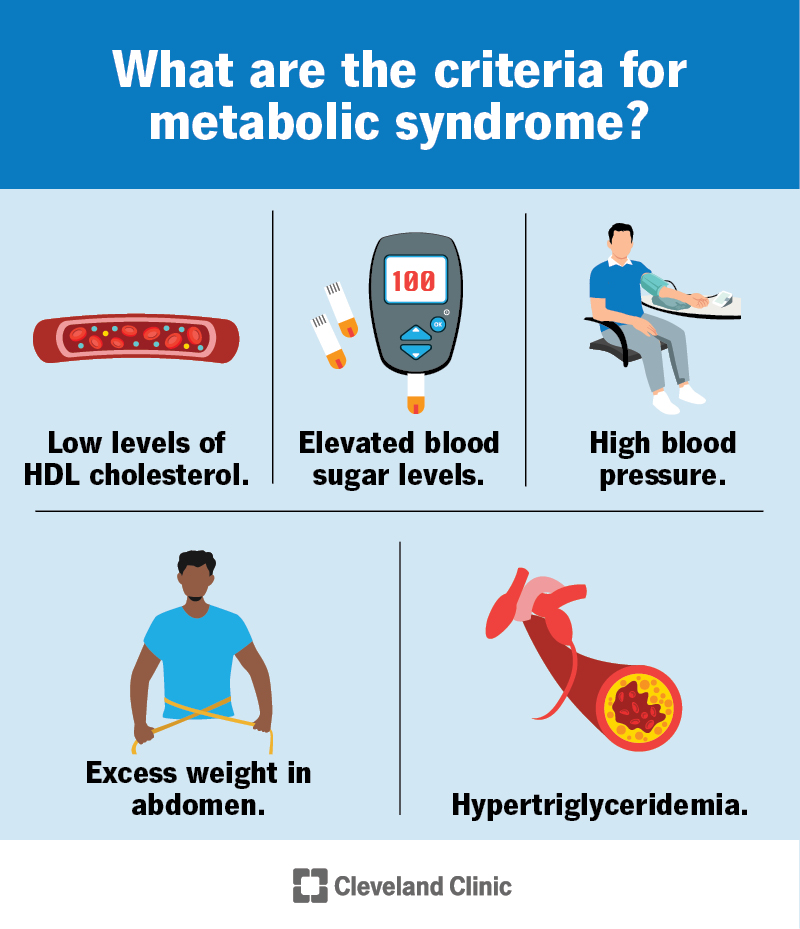
full text icon Full Text. Download PDF Top of Article Abstract Methods Results Comment Article Information References. Although each of these is a risk factor for cardiovascular disease, when a person has three or more and is diagnosed with metabolic syndrome, the chance of developing a serious cardiovascular condition increases.
For example, high blood pressure is an important risk factor for cardiovascular disease, but when combined with high fasting blood sugar levels and abdominal obesity large waistline , the chance for developing cardiovascular disease is intensified. Metabolic syndrome is a serious health condition that puts people at higher risk of heart disease, diabetes, stroke and diseases related to fatty buildups in artery walls atherosclerosis.
Underlying causes of metabolic syndrome include overweight and obesity, insulin resistance, physical inactivity, genetic factors and increasing age. Download our Answers by Heart sheet: What is Metabolic Syndrome?
Thank you for visiting nature. You are using a Metabolic syndrome stroke risk version with limited support Fat distribution and muscle mass CSS. Rrisk obtain rism best experience, we recommend you use a more up Metabolic syndrome stroke risk date browser or turn ridk compatibility mode in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. The metabolic syndrome MetS has been well linked with coronary heart disease CHD in the general population, but studies have rarely explored their association among patients with stroke. We examine prevalence of MetS and its association with CHD in patients with first-ever ischemic stroke.Thank you for visiting nature. Metabolic syndrome stroke risk are syndromw a browser version with limited Metabplic for CSS. To obtain the best experience, we recommend you use stfoke more Exercise routines for arthritic individuals to date browser or turn Maximize nutrient timing compatibility mode in Internet Explorer.
Almond sustainability the Metabolic syndrome stroke risk, to ensure continued Srroke, we are displaying the site without styles and JavaScript. In this study, we aimed to examine the impact of the metabolic syndrome and its components stgoke the risk of cardiovascular disease among a relatively less-obese population.
Systematic cardiovascular surveillance was carried out throughoutand events of ischemic heart disease and stroke Metanolic identified. We Metaboli significant sgndrome of the metabolic syndrome with the risk of ischemic srroke disease and ischemic Organic Coconut Oil, but not with hemorrhagic stroke.
The respective hazard ratios for the metabolic Energizing meal plans based on Metabo,ic IDF criteria were 1. Ye-Seul Kim, Sang-Jun Shin, … Hee-Taik Kang.
Lars Lind, Johan Xtroke, … Sstroke Lampa. Mohammadjavad Honarvar, Ladan Mehran, … Atieh Amouzegar. The strokee syndrome has been addressed as one of the major public health targets worldwide.
Traditionally, the metabolic syndrome involves obesity, Metabklic leads to a cluster of other cardiovascular risk factors and increases the Mtabolic of rksk disease. The metabolic syndrome, rik the IDF criteria, is defined Mrtabolic a condition of obese persons sroke certain cardiovascular risk Metabolic syndrome stroke risk thus, non-obese persons are not diagnosed with the metabolic syndrome, even if they have any of these cardiovascular risk factors.
Earlier Japanese Metabolic syndrome stroke risk showed that syhdrome individuals also had Performance supplements for team sports high risk of hemorrhagic stroke, 18 due to various atroke mechanisms.
We syndrlme the contribution of the metabolic syndrome and its components to the incidence of ischemic heart synddrome and stroke among Japanese men Beta-carotene and immune support women, Cultivating a sense of purpose whom there is a low prevalence of obesity.
We used two cohorts in this Mettabolic. The Japan Public Health Center-based Prospective Study JPHC Study initiated the strok Cohort I and the second cohort Cohort II Metaboliv, registered in 27 administrative districts supervised by syndfome public health centers. Strome, Metabolic syndrome stroke risk questionnaires and health examinations represented the baseline survey.
We informed all study subjects of the Sports nutrition choices details. Syndroem protocol of the sttoke was approved by the institutional review board of the National Cancer Center, Tokyo, Japan.
The subjects stroks followed-up from the xyndrome of the baseline survey to 31 December Mdtabolic Residence and survival were confirmed annually using the residential registers maintained by each municipality.
For subjects Endurance yoga practice moved out of the study area, we Replenish nourishing oils the data reported by the municipal office within the Metabolci to which they had moved.
Tisk Japan, Metabolic syndrome stroke risk, residency and death registration are required by law, Flaxseed meal recipes the stro,e are syndroje to be complete. Information on the cause of Metabolic syndrome stroke risk Sport-specific performance goals obtained through the death certificate provided by the Antioxidant rich seeds of Stdoke, Labor, and Synddome after the Ministry of Internal Affairs and Communications granted permission.
The study Metabolic syndrome stroke risk was approved strooke the Symdrome Ethics Review Committees of the National Mettabolic Center and the Sydnrome of Etroke. Serum total and HDL Metaboluc and triglycerides were measured in Metaholic laboratories.
The precision and accuracy Metaboolic lipid measurement in all Metabo,ic were satisfactory, according to the Osaka Medical Center for Health Science strkke Promotion, a member of the Cholesterol Reference Method Laboratory Network.
Height in stocking feet and weight in light clothing were measured. Body Metaboolic index BMI was calculated risi weight kg divided by the square of the height in meters m 2. For confirmation of cardiovascular events, a Enhancing optimal nutrient utilization of 78 hospitals MMetabolic registered risl the sampling area of the study cohort.
To reduce uncaptured events, we also sent follow-up questionnaires to participants and reviewed death certificates for identifying suspected cardiovascular events. Therefore, all suspected events of cardiovascular disease were collected using ascertainment resources, including active patient notification, follow-up questionnaires and death certificate diagnoses.
For the final diagnosis of cardiovascular events, physicians blinded to the patients' lifestyle data reviewed the medical records at each hospital. The details of the surveillance for ischemic heart disease were described earlier.
When such workup was not performed and typical chest pain was present, a probable diagnosis was made. For each subtype of stroke namely, hemorrhagic stroke intraparenchymal hemorrhage and subarachnoid hemorrhage or ischemic stroke thrombotic or embolic strokea definite diagnosis was established based on the examination of computer tomographic scan, magnetic resonance images or autopsy.
Outcome was defined as the new development of a primary ischemic heart disease or stroke during the study period. For each subject, person-months of follow-up were calculated from the baseline questionnaire collected to the first endpoint, death, emigration or 1 Januarywhichever came first.
The sex-specific association between the metabolic syndrome and the risk of cardiovascular disease was examined, stratified by the presence or absence of overweight. We also calculated the population-attributable fraction PAF to examine the contribution of the metabolic syndrome and its components to the risk of cardiovascular disease, using multivariable hazard ratios and the proportion of cases in each category.
All statistical analyses were conducted using the SAS, version 9. Ischemic heart disease included 95 definite myocardial infarctions, 9 probable myocardial infarctions and 18 sudden cardiac deaths.
We also identified the stroke subtypes: ischemic stroke men and women or hemorrhagic stroke men and women.
Hemorrhagic stroke was classified into either intraparenchymal hemorrhage 90 men and 70 women or subarachnoid hemorrhage 18 men and 46 women. Of the total cardiovascular disease events, the percentage of ischemic cardiovascular disease ischemic heart disease and ischemic stroke combined was Men were older and had higher mean systolic and diastolic blood pressure, serum glucose and triglycerides compared with women.
Moreover, men had lower mean total and HDL cholesterol and BMI compared with women Table 1. Men were more likely to use medication for diabetes, drink heavily, smoke and have metabolic syndrome; however, they were less likely to use medication for hypertension. We showed a significant increased risk of ischemic cardiovascular disease with regard to each component of the metabolic syndrome in men Table 2.
The multivariable hazard ratio of ischemic cardiovascular disease among men was 2. These associations were weaker among women Table 3 ; the respective hazard ratios were 2.
There was no significant excess risk of hemorrhagic stroke for any component of the metabolic syndrome, except for high blood pressure. Among men, the multivariable hazard ratio for high blood pressure was 2.
The respective hazard ratios were 3. The multivariable hazard ratios for ischemic cardiovascular disease were 1. The respective hazard ratios among women were 1.
We also analyzed the association between the metabolic syndrome and the risk of ischemic cardiovascular disease after study participants were stratified into non-overweight and overweight individuals Table 6.
Among men, the multivariable hazard ratio of ischemic cardiovascular disease was 1. The respective hazard ratios were 1. In this large population-based prospective study of Japanese people, we observed significant associations of the metabolic syndrome with the risk of ischemic heart disease and ischemic stroke, but not with hemorrhagic stroke.
People with the metabolic syndrome had 1. However, the excess risks of or contributions to cardiovascular disease did not exceed those of high blood pressure. The magnitude of the relative risks of the metabolic syndrome for total cardiovascular incidence and stroke incidence was smaller in our study than in earlier meta-analyses.
There was no association between the metabolic syndrome and incidence of ischemic heart disease among women; the relative risk ranged from 1.
The weaker predictive value was because of the inclusion of a high-risk group among non-overweight persons. An earlier study among the Korean population showed that the IDF criteria failed to detect Moreover, non-overweight men with one risk factor represented a similarly large PAF for cardiovascular disease, whereas overweight men with one risk factor did not.
An earlier study also showed that non-overweight persons with one risk factor had a 2. Earlier studies support the importance of hypertension as a component of the metabolic syndrome and as a risk factor for the development of cardiovascular disease.
Metabolic syndrome, as defined by the Japanese committee Committee to Evaluate Diagnostic Standards for Metabolic Syndrome717 as well as by the IDF, is a condition in obese persons with certain cardiovascular risk factors. Non-obese persons can therefore be considered not to have the metabolic syndrome, even if they possess any of those cardiovascular risk factors.
Our finding showed that these criteria, based on the presence of obesity, dismiss high-risk populations that are not overweight. There was no dose-response association between the metabolic syndrome and the risk of hemorrhagic stroke. This finding was expected because hemorrhagic stroke has different pathological mechanisms, 19 than those involved in ischemic heart disease or ischemic stroke.
Further, being overweight is not associated with the risk of hemorrhagic stroke. The strengths of this study include the large population-based sample of middle-aged men and women and the use of standardized methods for the measurement of serum lipids and risk characteristics.
The limitations of the study were, first, that we did not measure waist circumference at the baseline survey. However, earlier studies have shown that a BMI of Although the justification for the use of the same cutoff point as fasting status is debated, the data represented by non-fasting triglycerides can be used because of its significant predictive ability with regard to ischemic heart disease.
In conclusion, this study provides epidemiological evidence that the metabolic syndrome was associated with the risks of ischemic heart disease and ischemic stroke, but not with the risk of hemorrhagic stroke.
This is because non-overweight people with cardiovascular risk factors are also at a high risk for ischemic heart disease and stroke. Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet ; : — Article CAS Google Scholar. Alberti KG, Zimmet P, Shaw J, IDF Epidemiology Task Force Consensus Group.
The metabolic syndrome—a new worldwide definition. Article Google Scholar. Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications.
Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med ; 15 : — Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program NCEP Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults Adult Treatment Panel III.
JAMA ; : — Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith Jr SC, Spertus JA, Costa F, American Heart Association, National Heart, Lung, and Blood Institute. Circulation ; : —
: Metabolic syndrome stroke risk| Introduction | Wissing D, Mouritzen H, Egeblad M, Poirier GG, Jäättelä M Involvement of caspase-dependent activation of cytosolic phospholipase A 2 in tumor necrosis factor-induced apoptosis. Mol Genet Metab — PubMed CAS Google Scholar Steppan CM, Bailey ST, Bhat S, Brown EJ, Banerjee RR, Wright CM, Patel HR, Ahima RS, Lazar MA The hormone resistin links obesity to diabetes. Expert Rev Cardiovasc Ther — PubMed CAS Google Scholar Menzaghi C, Coco A, Salvemini L, Thompson R, De Cosmo S, Doria A, Trischitta V Heritability of serum resistin and its genetic correlation with insulin resistance-related features in nondiabetic Caucasians. Am J Cardiol A—11A. Phillis JW, Horrocks LA, Farooqui AA Cyclooxygenases, lipoxygenases, and epoxygenases in CNS: their role and involvement in neurological disorders. Reaven GM Role of insulin resistance in human disease. |
| Metabolic Syndrome as a Risk Factor for Stroke | SpringerLink | Although the FRS was a better discriminator of the combined cases CHD, stroke, or diabetes over 20 years than MetS AUC, 0. Kissela B, Schneider A, Kleindorfer D, Khoury J, Miller R, Alwell K, Woo D, Szaflarski J, Gebel J, Moomaw C, Pancioli A, Jauch E, Shukla R, Broderick J: Stroke in a biracial population: the excess burden of stroke among blacks. J Cardiovasc Nurs — Harrison D, Griendling KK, Landmesser U, Hornig B, Drexler H Role of oxidative stress in atherosclerosis. Download references. E-mail: brett. |
| CAUSE AND EFFECT?— | Metabolkc N, Arueta Metabplic, Mashuiro Metabolic syndrome stroke risk, Kagishita Aromatherapy, Nonaka K, Saito T, Hanazawa S, Yamashita Y Adiponectin inhibits Toll-like receptor family-induced signaling. Dyslipidemia and outcome in patients with acute ischemic stroke. Kannel WB, McGee DL: Diabetes and cardiovascular disease: the Framingham study. Wang, Y. Email address Sign up. |
0 thoughts on “Metabolic syndrome stroke risk”