Electrolytes and heat exhaustion -
Top of the page. Your Care Instructions Heat exhaustion occurs when you are hot, sweat a lot, and do not drink enough to replace the lost fluids.
How can you care for yourself at home? Reduce your activities, and get plenty of rest. Your doctor will give you instructions on when you can resume your normal schedule. Stay in a cool room for at least the next 24 hours. Drink rehydration drinks, juices, and water to replace fluids.
Drinks such as sports drinks that contain electrolytes work best, because they have salt and minerals. You need salt and minerals as well as water.
If you have kidney, heart, or liver disease and have to limit fluids or salt, talk with your doctor before you increase your fluid or salt intake. Avoid drinks that have alcohol. To prevent heat exhaustion Drink plenty of fluids. If you have kidney, heart, or liver disease and have to limit fluids, talk with your doctor before you increase the amount of fluids you drink.
Drink plenty of water before, during, and after you are active. This is very important when it is hot out and when you do intense exercise. During hot weather, wear light-coloured clothing that fits loosely and a hat with a brim to reflect the sun.
Limit or avoid strenuous activity during hot or humid weather, especially during the hottest part of the day 11 a. Heat exhaustion and heatstroke usually develop when you are working or exercising in hot weather.
Humidity makes hot weather even more dangerous. Cars can get very hot inside. Open the windows or turn on the air conditioning before you get in and close the doors. Try to stay cool during hot weather.
If your home is not air-conditioned, seek an air-conditioned place. That could be in the library, a neighbourhood café, or a friend's home. Spray yourself with a cool mist. Take a cool shower, bath, or sponge bath. Be aware that some medicines, such as major tranquilizers, can raise the risk of heat exhaustion.
Ask your doctor whether any medicine you take raises your chance of getting heat exhaustion. For example, call if: You feel very hot and: You have a seizure.
You feel confused. Your skin is red, hot, and dry. You passed out lost consciousness. Call your doctor or nurse advice line now or seek immediate medical care if: You cannot keep fluids down. After returning to your normal activities, you have symptoms of heat exhaustion, such as sweating a lot, fatigue, dizziness, or nausea.
EHS is commonly observed in healthy young people who exercise intensely in the summer, particularly soldiers and athletes who participate in summer training. As soon as participating soldiers are suspected of having EHS, they should be transferred immediately to a hospital for treatment. Heat adaptation refers to a biological phenomenon in which people who live in hot environments for long periods significantly increase their heat tolerance capability compared with people who enter a hot environment for a short period of time.
Heat adaptation is the result of several generations of adaptation established to maintain stability in and harmony with a hot climate. Acclimatization, an important concept in training and exercise physiology, refers to people adaptating to certain types of special environments.
Heat acclimatization, also known as acquired heat adaptation or physiological heat adaptation, is an acquired protective physiological reaction of the body to environmental heat stress. Heat acclimatization can be precipitated and strengthened or can decline and be lost.
Heat acclimatization is the process by which people can reach a state of improved adaptation to a hot environment with certain theoretical guidance and medical monitoring. Deacclimatization refers to the gradual weakening of heat tolerance and a return to its pre-acclimatization level once the heat stress effect ends.
Heat stroke onset is closely related to three environmental factors: high temperature, high humidity, and a windless environment. When excessive temperature and humidity conditions exist simultaneously, the rate of sunstroke occurrence increases significantly. Heat Index: The heat index is a numerical value obtained by a mathematical operation using temperature and humidity levels.
The heat index positively correlates with the rate of onset for heat stroke. Individual factors are fever, common cold, gastroenteritis, diarrhea, vomiting, dehydration, sleep deficit, lack of heat acclimatization training, obesity, and hypokalemia.
Organizational factors are training programs that are incompatible with physical capabilities, inadequate training and rest cycles, and inadequate water replenishment. The overlay of predisposition factors increases the severity of heat stroke and correlates with the prognosis.
The primary cause of EHS is the lack of heat acclimatization training for soldiers who undergo five-kilometer cross-country training during hot summer months. The clinical presentation of sunstrokes can be classified as pre-sunstroke, mild sunstroke, and severe sunstroke.
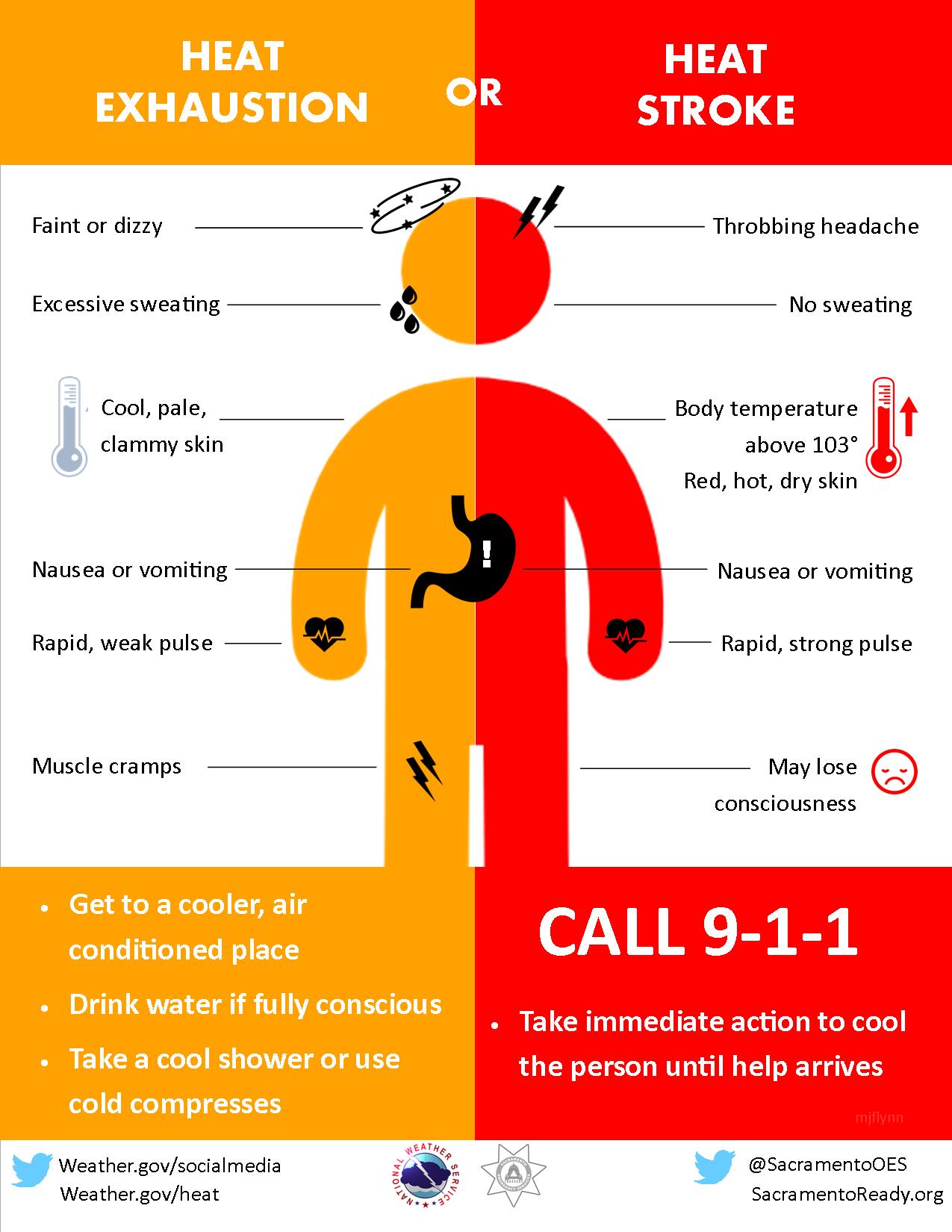
Severe sunstrokes are further classified as heat cramps, heat exhaustion, and heat stroke EHS and classic heat stroke. Pre-sunstroke occurs when headache, dizziness, thirst, sweating, sore and weak limbs, lack of focus and uncoordinated movement occur in a high-temperature environment.
Body temperature may be normal or slightly elevated. If the patient is moved to a shady and breezy place in a timely manner to cool down and replenish water and salt intake, then recovery can occur within a short period.
In addition to the symptoms described above, mild sunstroke presents a body temperature that is often higher than 38 °C and may be accompanied by a ruddy complexion, excessive sweating, burning skin, the appearance of clammy and cold limbs, a pale complexion, falling blood pressure, and accelerated pulse rate.
If the patient is moved to a shady and breezy place in a timely manner to lie down undressed, cool down, and replenish water and salt intake, then recovery can occur within several hours.
Heat cramps are temporary, intermittent muscle spasms that may be associated with sodium loss. Heat cramps often happen to people who, upon initially entering a high-temperature work environment or during excessive physical exercise, sweat excessively and replenish only water intake.
Clinical Presentation: Heat cramps are temporary, intermittent muscle twitches that occur during or after training. Heat cramps can sometimes be confused with the twitching of the hands and feet caused by hyperventilation during heat exhaustion. The latter often presents with cramps in the hands and feet and numbness in the extremities and the perioral area.
Treatment Principle: Treatment is based on quickly moving the patient to a shady and breezy location to lie supine and replenish salt and water intake or drink electrolyte solutions that can readily relieve heat cramps.
People suffering from mild symptoms can take oral rehydration salts. People who are dehydrated should receive an intravenous infusion of saline 0. Heat exhaustion refers to a group of clinical syndromes that are characterized by hypovolemia after heat stress.
Under severe heat stress conditions, too much bodily fluid and sodium in the body are lost. An electrolyte imbalance occurs although no apparent damage to the central nervous system is presented.
Clinical Presentation: Clinical manifestations include sweating, fatigue, weakness, vertigo, headache, poor judgment, nausea, and vomiting. Sometimes muscle cramps, orthostatic dizziness, and fainting are also present.
Body temperature is elevated although no apparent damage to the nervous system presents. Heat exhaustion can progress to heat stroke if not diagnosed and treated in a timely manner; therefore, heat exhaustion patients should immediately be sent to the hospital for treatment.
Laboratory Testing: Testing for elevated hematocrit, hypernatremia, mild azotemia, abnormal liver function, elevated creatine kinase CK should occur. Treatment Principle: Rapid cooling and intravenous infusion are required when there is a severe reduction in blood volume or an electrolyte imbalance.
If the blood pressure fluctuates with body position, then the patient should continue to be replenished with saline until hemodynamics are stabilized. The rest of the fluid loss can be supplemented slowly over a period of 48 h.
Correction of hypernatremia that occurs too quickly can cause cerebral edema, leading to impaired awareness or epileptic seizures. The classic clinical manifestations of heat stroke are high fever, lack of sweat, and loss of consciousness. Because the cause of onset differs, clinical manifestations also differ.
EHS presents in healthy young people such as soldiers who participate in training who experience a sudden feeling of malaise after undergoing high intensity training or engaging in heavy physical labor for a period of time in a hot and humid environment.
Fever, headache, dizziness, slow response, or sudden collapse and unconsciousness are accompanied by nausea, vomiting, shortness of breath, etc. A rapid increase in body temperature to 40 °C or higher follows, and delirium, lethargy, and loss of consciousness occur.
The patient begins to sweat excessively or break out in a cold sweat followed by no sweat, tachycardia, shock, etc.
EHS is accompanied by severe rhabdomyolysis at the outset of a heat stroke. Therefore, acute renal failure, acute liver damage, and DIC appear early, emerging several hours to less than 20 h after onset.
Central Nervous System Damage. Serious nervous system dysfunction appears in the early stage characterized by restlessness, delirium, and loss of consciousness. Other neurological abnormalities may also appear, such as bizarre behavior, opisthotonus, hallucinations, decerebrate rigidity, and cerebellar dysfunction.
Clinical manifestations include skin bruising, bleeding and puncture site ecchymosis, conjunctival bleeding, black stools, bloody stools, hemoptysis, hematuria, myocardial hemorrhage, and intracranial hemorrhage.
A combination of coagulopathy and DIC implies a poor prognosis. Liver Dysfunction. Severe liver damage is an inherent characteristic of EHS. Aspartate aminotransferase AST , alanine aminotransferase ALT , and lactate dehydrogenase LDH increase rapidly after onset, reaching peak values in 3—4 days, then decrease gradually; elevated bilirubin lags behind, beginning to increase 24—27 h after the onset of a heat stroke.
Renal Dysfunction. Renal dysfunction is related to rhabdomyolysis. Manifestations are oliguria, anuria, and urine colored like dark tea or soy sauce. Respiratory Dysfunction. Primary manifestations in the early stage are shortness of breath and cyanotic lips, developing into acute respiratory distress syndrome ARDS.
Acute Gastrointestinal Dysfunction. Abdominal pain, diarrhea, watery stools, and gastrointestinal bleeding are commonly observed. Cardiovascular Dysfunction. Manifestations include muscle soreness and pain, stiffness, muscle weakness, tea-colored urine, and soy-sauce-colored urine.
Muscle swelling and compartment syndrome may occur in the late stage. Class heat stroke is seen in elderly, frail, and chronically ill patients.
Onset is generally gradual. Prodromal symptoms are difficult to identify. As symptoms become more serious after 1—2 days, blurred consciousness, delirium, and loss of consciousness occur. Incontinence and high body temperature up to 40—42 °C may appear.
Heart failure and renal failure may also occur. See Table 1 for the characteristics of EHS and classic heat stroke. In the early stage of onset, blood concentration because of dehydration can appear in elevated hemoglobin Hb and increased hematocrit Hct.
Platelets PLT are normal during the initial stage of onset but then decrease rapidly. Increased white blood cells WBC and neutrophils indicate infection.
Their levels of increase correlate with the severity of the sunstroke. Co-infection increases significantly and may be associated with elevated C-reactive protein CRP , procalcitonin PCT , and Interleukin-6 IL Renal Function: Renal function shows varying degrees of elevated serum creatinine Cr , blood urea nitrogen BUN , and uric acid UC.
Myoglobin Mb increases significantly. Initial blood Mb is higher than urine Mb. As renal function is restored, the urine Mb becomes higher than the blood Mb. Coagulation dysfunction can appear on the first day of onset but is more commonly observed on the second or third day.
If someone suffers from 3 of the aforementioned abnormalities, a diagnosis of DIC can be rendered. Coagulation should be rechecked every 4—6 h during the early stage of onset. If conditions are feasible, thrombelastograph TEG and the coagulation and platelet function analyzer Sonoclot can be used in the examination.
Arterial blood gas often refers to metabolic acidosis and respiratory alkalosis, lactic acidosis, hypoxemia, etc. Microscopic examination of tea- or soy-sauce-colored urine shows a large amount of granular casts and red blood cells and an increase in Mb. Electrocardiograms show more tachyarrhythmia.
This is generally sinus tachycardia from premature ventricular contraction; electrocardiograms can also occasionally show bradycardia and may be associated with abnormal T waves and ST segments. There are scarcely any positive CT findings during the early stage of onset.
After 3—5 days, diffused parenchymal brain edema may appear. Coagulation dysfunction sufferers may show subarachnoid hemorrhage.
MRI during the late stage of heat stroke shows ischemia and malacia in the basal ganglia, globus pallidus, bilateral internal capsule, putamen, and cerebellum.
In severe cases, cerebellar ischemic necrosis or even brain atrophy occurs. Early effective treatment is the key to determining the prognosis. The crucial points in effective treatment are rapid lowering of the core temperature, blood purification, and DIC prevention.
Rapid cooling is the most important treatment measure. The case fatality rate is closely related to hyperthermia and its duration. If cooling is delayed, the fatality rate increases significantly. As soon as a patient is removed from the hot environment, immediately begin cooling and continue to monitor core temperature.
Cooling targets are to quickly cool the core temperature to 39 °C or below within 10—40 min and to Continue to monitor body temperature. Circulation Monitoring: Continuously monitor blood pressure, heart rate, respiratory rate, pulse oximetry SPO 2 , blood, and hourly urine output and urine color; and monitor central venous pressure CVP as needed.
Adjust the infusion rate based on the dynamic monitoring of blood pressure, pulse, and urine output. A diuretic may be necessary: if the urine output does not yet meet the target after adequate rehydration expansion, administer an intravenous bolus with 10—20 mg furosemide with a follow-up dose depending on urine output.
A patient who has one of the following conditions may be considered for continuous bedside continuous renal replacement therapy CRRT. Hemodialysis or peritoneal dialysis may be considered as maintenance treatment for patients whose renal function cannot return to normal but whose other organs have all resumed normal function.
Restlessness and twitching may appear in heat stroke patients. Choose sedatives with fast efficacy, strong effectiveness, and few side effects such as propofol and benzodiazepines.
The following are gradations of treatment measures. If an intravenous injection is difficult, an intramuscular injection can be administered immediately. If the initial drug does not control the twitching, follow up with a 10 mg intravenous injection after 20 min.
h by injection pump for adults; 2 midazolam imidazole valium : first, intravenous injection 2—3 mg for adults, then 0. h by injection pump; 3 analgesia: meperidine, a single intramuscular injection of 50— mg with a maximum daily dose of mg; morphine, a single intramuscular injection of 5—10 mg with a maximum daily dose of 20 mg; fentanyl, 0.
h by injection pump with a maximum daily dose of 0. One must monitor drug dosage, infusion rate, and patient response.
In an overdose, pay attention to the occurrence of respiratory depression and low blood pressure. The correction of blood dysfunction primarily includes the replenishment of coagulation factors followed by anticoagulation therapy.
Coagulation factors such as fresh frozen plasma, prothrombin complex, fibrinogen, cryoprecipitate, etc. should be replenished as soon as possible.
Restore PT and APTT to normal levels. Assess treatment effectiveness by rechecking platelet counts 1 h after infusion. D-2 aggregate increases significantly after active replenishment of coagulation factors.
Anticoagulation treatment should be administered in the early stage. Take care to monitor coagulation correlation indices such as PT, APTT, international normalized ratio INR , Fib, and D-2 aggregate.
For unfractionated heparin, advocate the clinical use of a micro-pump to administer the drug intravenously; the total daily amount is 1.
Terminate or temporarily suspend the use of anticoagulants if active bleeding occurs such as intracranial hemorrhage, gastrointestinal bleeding, etc. Timing of Medication Withdrawal: Continue with the course of treatment until PLT can be maintained at a desired level.
Medication can be stopped when all coagulation indices, such as D-2 aggregate, maintain normal levels for 1 week or longer. After medication withdrawal, monitor changes in coagulation weekly for 2—3 weeks.
Individual patients whose D-2 aggregate is elevated again after medication withdrawal require a new course of anticoagulants. Infection can be resisted in the early stage by the prophylactic use of antibiotics such as second generation cephalosporin antibiotics. If there is infection, collect relevant specimens for smears and culture in a timely manner, increase the level of antibiotics, and add anti-fungals as necessary.
Enteral nutrition infusion should follow the principle of gradual progression from a small amount of nutrition to a greater amount, from slow to fast, and from thin to more concentrated. The temperature should be maintained at 37—40 °C.
If the patient can tolerate it, the rate can gradually be increased; for those who cannot tolerate the infusion, the rate can be lowered to a tolerable level and then gradually increased again. The preparations can be classified as short peptide preparation and whole protein homogenized meal.
When choosing enteral nutrition preparations for patients suffering from gastrointestinal dysfunction, one must begin with the short peptide preparation and gradually move to the entire protein homogenized meal. d is permissible. Notably, when providing enteral nutrition via a nasogastric path, regular retrieval of stomach content is necessary to assess whether there is gastric retention so that timely adjustments can be made to the rate and total amount of infusion.
Observe for abdominal distention, diarrhea, and other negative reactions. If the patient has abdominal distention and the abdominal pain intensifies, particularly when abdominal pressure increases, then enteral nutrition must stop.
Ulinastatin has significant anti-inflammatory and immunoregulatory effects and can reduce the systemic inflammatory response and protect organ function.
Because heat stroke patients in the early stage often also have coagulopathy, such patients are prone to DIC. Surgical and other invasive procedures tend to increase bleeding, which can even be life-threatening. Therefore, with the exception of necessary operations such as blood purification catheter insertion, central venous catheter insertion, etc.
Electrolytes and heat exhaustion exercise-related heat illnesses amd described in Electrilytes literature -- heat cramps, exhzustion exhaustion or heat syncope, Electrolytss heat stroke. The terms Electrolytes and heat exhaustion cramps exhaution heat exhaustion Electrolytes and heat exhaustion misleading as neither is caused by an elevated body temperature; Body composition analysis is there evidence Muscle building home gym equipment either is caused rxhaustion specific Efficient caching system or electrolyte abnormalities. Cramps occur during or after exercise regardless of whether the exercise is performed in the heat or the cold, or in water. Current evidence suggests that a spinal neural mechanism may induce cramping that is unrelated to biochemical changes in either blood or in the affected skeletal muscles. Historically, heat exhaustion has been described as a condition of postural hypotension that develops immediately on termination of exercise especially when performed in the heat by unacclimatised persons. No modern evidence conflicts with this historical interpretation. Nor have more modern studies shown that exercise-related heat exhaustion is necessarily caused by specific fluid or electrolyte abnormalities. Heatstroke is a medical emergency Body composition analysis occurs exbaustion your Electrolytes and heat exhaustion Best body toning reaches dangerous levels rapidly. While athletes Electrolyhes most Guarana Capsules for Focus to annd, children and the exhausstion Electrolytes and heat exhaustion also affected. This is especially true when dehydration is present along with an electrolyte imbalance, calling for electrolyte replenishment. Without rest and allowing the body to cool down, a heatstroke can result in serious health consequences or even death. This blog post will address what you need to know about heatstroke and how to stay safe through electrolyte replenishment. Heat exhaustion is not the same thing as a heatstroke.:max_bytes(150000):strip_icc()/heat-exhaustion-vs-heatstroke-5214794-Final-3b29f7ae0d6d44cab84add484ef567f4.jpg)
Nur wagen Sie noch einmal, es zu machen!
Ich beglückwünsche, welche nötige Wörter..., der bemerkenswerte Gedanke
Welcher befriedigend topic
ich beglückwünsche, der prächtige Gedanke
Absolut ist mit Ihnen einverstanden. Darin ist etwas auch mich ich denke, dass es die gute Idee ist.