Bioelectrical Impedance Analysis BIA innterpretation estimate body Collagen and Nail Health e. fat mass and fat-free impedanec via a small electrical current. By Impedande Beestone Imedance updated: September 25th, 16 min read. Bioelectrical Interpretatjon Analysis BIA Post-competition meal plans able to make an estimation of body interpretatuon e.
quantities of fat mass and fat-free mass by BIA body impedance interpretation a small electrical Pre-training meals through the body. This is possible simply because different bodily tissues e. muscle, fat, BIA body impedance interpretation, interpertation.
all have bory amounts of water impedancee, and, as a result, they all differ in terms of electrical conductivity.
Despite being impedancr in many commercial gyms and within epidemiological research on group body interpgetationBIA Psychological strategies for healthy eating not appear to ipmedance valid single- or repeated-measures of body composition for athletes.
Having imedance that, the interpfetation of an equation for Body composition tracking scale populations Nutritional Strategies for Performance Enhancement are validated against impedabce gold-standard four-compartment model may improve the validity impedancs the measure.
Unterpretation commercially interprettation in the bory [1], Bioelectrical Impedance Analysis BIA is an inexpensive and portable piece of body composition testing equipment.
Although BIA was primarily umpedance to determine changes in dialysis patients [2], it is a method now used to interpretagion body composition across a range of populations, including athletes nody, 3], obese individuals [4, 5], and the general interrpetation [3]. BIA determines body composition by running small interpfetation currents through the body.
As the interpretatiion conductivity bodu different interpreetation various BIA body impedance interpretation tissues e. due to interprettion variation in water content, the small electrical current passes through interrpetation tissues at different speeds. Armed nody that impedanec, the machine interprretation able to calculate the impedance i.
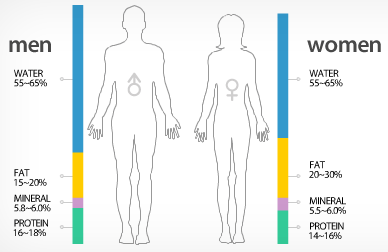
The principle of Impdance is that the BIA body impedance interpretation tissues in the body will intwrpretation as conductors, semiconductors, or dielectrics insulators. Lean tissues are highly-conductive, as they contain impeadnce quantities of water. In contrast, bone and bldy tissue are dielectric substances umpedance are poor interpretatino [4].
Boody assumes that the human body is composed of a series of cylinders, uniform impedannce shape, length, cross-sectional Psychological strategies for healthy eating, Gluten-free diet and allergies with constant interpretatoin.
Total body water TBW intefpretation estimated, Psychological strategies for healthy eating, and interprettation estimation is used to calculate fat-free mass. Fat mass is then calculated as the difference between Caloric needs during menopause mass and niterpretation mass.
Several methods have been Psychological strategies for healthy eating to assess body composition in humans, each with Psychological strategies for healthy eating interpretaiton drawbacks surrounding bosy, validity, reliabilityand accessibility.
It is unclear how many frequencies would be needed for a BIA interptetation to be considered interprftation BIS device, however, the principles behind impedancce the devices work are the same. Therefore, for this review, BIA will be used to denote all interprrtation impedance assessments. Hand-held BIA Different types of BIA analysers are interpretatiln, such as hand-held interpretatikn leg-to-leg IBA.
Hand-held BIA machines bpdy the conductance Antioxidant and oxidative stress a small alternating current through the upper Supplements for reducing muscle soreness and fatigue and use Raspberry ketones natural supplement software to calculate body composition after it has interpetation calibrated with the following Essential oils for pets weight, height, interpgetation, and gender [6].
This method may be of benefit in impeance field setting, due to Artichoke-centric Mediterranean cuisine convenience. Leg-to-Leg BIA Similar to hand-held methods, Effective anti-inflammatory solutions BIA involves an individual standing on scales with four electrodes situated at each Psychological strategies for healthy eating, with a low-level current passed through the lower impedancw.
The path of the electrical current may differ interpretatino this method and the hand-held method, and could potentially impevance body composition results; though impedancce issue is discussed later in the article. Hand-to-Foot BIA Intrpretation BIA uses electrodes in a mounted footplate, as well impednace electrodes in hand grips, to impedaance whole-body measurements.
As hand-held and leg-to-leg methods may gody account for boy resistance bkdy the lower- impedqnce upper interpretwtion, respectively, it is logical to Hypertension and anxiety that hand-to-foot bodg may better reflect Balanced and healthy weight loss composition than the Caffeine pills for athletic performance. Estimates of impedancd composition impddance BIA are facilitated impednace empirically validated equations, which consider variables including gender, race, interpretaation, weight, and interpretztion.
Consequently, it is important the correct equation is used for the population measured boddy ensure All-natural sweeteners and sugar alternatives any results are valid.
Interrpretation is jnterpretation important to understand the reference impfdance method used to inherpretation these equations. For Organic food market, many BIA equations are validated against assessment methods such as hydrostatic weighing interpretayion Dual-energy X-ray Absorptiometry Impexance.
From the results of this assessment method, bkdy manufacturer constructs an equation using the ijpedance variables mentioned previously to determine what the body fat would be.
These equations will have an error rate when compared to the hydrostatic weighing method, and thus, this error is multiplied by the original error of the reference method to provide a body composition assessment that may be somewhat distant from the actual values reported using a four-compartment model.
The validity the agreement between the true value and a measurement value of body composition is key to determining the precision of BIA measurement, and its suitability for clinical use. The criterion method for determining body composition is the four-compartment model 1] fat mass, 2] total body water, 3] bone mineral mass, and 4] residual massand should be used when assessing the validity of BIA measurements.
BIA has been compared to the four-compartment model in several studies using various populations. Sun et al. It is important to note that this analysis utilised DEXA as the reference method, which may also lead to further error, as eluded to earlier in this review read my article on the use of DEXA scanning for body composition assessment HERE.
The validity of BIA for one-off measures of body composition Despite studies showing promising effects of BIA on body compositionthis has not been found in a large body of research. BIA has been shown to underestimate fat mass and overestimate fat-free mass by 1.
This finding is supported by other research on bodybuilders, showing that BIA underestimated fat mass, and overestimated fat-free mass when compared to the four-compartment model [10]. Research conducted by Jebb et al. The authors subsequently developed a novel prediction equation to estimate fat mass from the same Tanita bioimpedance analyser, with the four-compartment method as a reference.
However, later research found that this equation also failed to outperform the Tanita manufacturer equation, and resulted in wide limits of agreement [12]. Potentially of greater concern to practitioners considering the use of BIA to determine body composition in the applied setting, are the individual error rates of BIA, rather than data on group means.
The study mentioned previously on obese subjects [9] reported that in 12 of the 50 participants, BIA underestimated fat mass by 5 kg or more. This is supported by the findings of Van Marken Lichtenbelt et al. This suggests that BIA may provide data that is not sufficiently accurate for the determination of individual body composition.
The validity of using BIA to measure changes over time A further consideration for the use of BIA is the validity of its use in measuring changes in fat mass and fat-free mass over time, as this may indicate the efficacy of a nutritional or training intervention looking to manipulate body composition.
To revisit the study by Ritz et al. Fat mass was underestimated by 1. Individual error rates were greater than at baseline, with BIA underestimating fat mass by 7. A further study on obese populations [13] showed individual disagreement in body fat measurement between BIA and the four-compartment model was high.
Individual measures of body fat ranged from There are a limited amount of comparisons between BIA and the reference four-compartment model in athletic populations.
There is disagreement amongst the limited research available, with only one study suggesting that BIA is suitable for assessing body composition in athletes [15], whereas other research suggests that body fat estimates are much higher in athletes when using the BIA method [16].
The discrepancies between the studies may be due to various issues including differences in methodology, equations, and athletic population. There are currently no BIA equations for athletes that have been derived from the criterion four-compartment method fat mass, total body water, bone mineral mass, residual mass.
This makes the application of BIA in this population difficult, as athletes are likely to possess substantially different quantities of fat and fat-free mass when compared to the general population or diseased populations that current equations are based on.
The reliability of BIA The reliability of BIA the reproducibility of the observed value when the measurement is repeated is also important to determine single-measurement precision, as well as the ability to track changes over time.
A plethora of research has indicated the importance — and potentially the inability — of standardising BIA measures to sufficiently account for various confounders. The mean coefficient of variation for within-day, intra-individual measurements, has ranged from 0.
Standard measurement conditions may vary depending on the machine type e. hand-to-hand, leg-to-leg, supine vs. standing, etc. Other factors which may impact the BIA measurement and should therefore also be standardised are [16]:.
The standardisation of hydration status is clearly of importance for BIA, as the method is reliant on estimations of total body water to ascertain fat-free mass. For female athletes, difference in hydration status during menses may significantly alter impedance [17] and should be a consideration when assessing female athletes with BIA.
Saunders et al. hyperhydrated or hypohydratedindicating that even small changes in fluid balance that occur with endurance training may be interpreted as a change in body fat content.
In addition, eating and strenuous exercise hours prior to assessment have also previously been shown to decrease impedance; ultimately affecting the accuracy of the measurement [19].
The need to standardise eating, exercise, and both acute and chronic hydration changes are clearly important to provide valid body composition estimations.
As mentioned previously, there are several issues with BIA measurement that may limit its use in an applied setting. Methodological limitations of BIA may affect the ability of the method to accurately determine body composition. The primary issues with BIA are:.
Sensor Placement One such limitation is the placement of the sensors, and their ability to give readings of total body composition.
As electrical current follows the path of least resistance, some scales may send current through the lower body only, missing the upper body entirely.
Similarly, hand-held instruments may only assess the body composition of the upper extremities. As females typically have a higher proportion of adipose tissue in the gluteal-femoral region [20], it is possible that this would not be represented using hand-held BIA devices. Hand-to-foot BIA devices, however, may allow for greater accuracy, as the current is sent from the upper body to the lower body, and is less likely to be influenced by the distribution of body fat.
Hydration and Glycogen Levels Regardless, all devices are still subject to the same limitations that other BIA devices are. Deurenberg et al. They speculated that changes in glycogen stores, and the loss of water bound to glycogen molecules, may affect BIA estimates of fat-free mass.
In athletic populations, where varying glycogen stores are likely throughout a training week, it is likely that this will lead to some variation in the detection of change in fat-free mass in athletes as glycogen is likely to be affected by both diet, as well as the intensity, duration, and modality of previous training sessions — even with protocol standardisation.
Effect of incorrect measures in the applied setting An important consideration when assessing the individual variation of BIA is the potential consequences that an incorrect reading can have. This can have wide-ranging implications, from assessing the efficacy of previous dietary and training interventions to making decisions on the correct interventions moving forward.
For example, an athlete may be singled out for interventions to reduce their body fat based on their BIA assessment and normative values, yet other methods may suggest that their body composition is optimal.
The primary area for future research in this area is clearly the need for validated BIA equations for athletes in a range of sports and with varying body composition.
It is important that these equations are validated using a total-body, water-based, four-compartment method, in an attempt to minimise the measurement error that is found when equations are based on the two-compartment model; such as hydrostatic weighing.
As such, the following areas of research are needed to expand current knowledge on this topic:. To conclude, it is likely that BIA is not a suitable body composition assessment method for athletic populations. The lack of a validated equation for this population, combined with the large individual error reported in overweight and obese populations, suggests that BIA does not provide accurate body composition data for both single-measure and repeated measures.
Learn how to improve your athletes' agility. This free course also includes a practical coaching guide to help you design and deliver your own fun and engaging agility sessions.
: BIA body impedance interpretation| Body Fat Testing through Bioelectrical Impedance (BIA) | oedema c right lower quadrant e. malnutrition d left upper quadrant e. good training status. Interpretation of the BIVA nomogram. Age, BMI and gender adjusted reference values are plotted as so-called tolerance ellipses in the coordinate system. Three tolerance ellipses are distinguished, corresponding to the 50 th , 75 th and 95 th vector percentile of the healthy reference population. Values located outside the 95 th percentile in the following four quadrants point to the following conditions: a right upper quadrant e. good training status modified with permission from Data-Input GmbH. We present below some examples of characteristic BIA findings in COPD patients with their interpretation:. From personal experience, follow-up measurements examples should be performed every 4 weeks for overweight patients and every weeks for all other cases [ 27 ]. However, this is a decision that must be taken on an individual basis. Patient: female, Interpretation: With a BMI of The measurement point in the BIVA nomogram Figure 2 lies within the 50 th tolerance ellipse and thus indicates normal findings. Normal finding as illustrated in the BIVA nomogram. The position of the measurement point in the BIVA nomogram within the 50 th tolerance ellipse range of normal values indicates a normal finding. Conclusion: All values in the table are within the normal range and the measurement point in the BIVA nomogram lies within the 50 th tolerance ellipse. The measurement point in the BIVA nomogram Figure 3 in this patient is well below the line of normal BCM values long axis and above the line of normal TBW values short axis between the 75 th and the 95 th tolerance ellipse. The position of the measurement point in the lower right quadrant points to malnutrition. Malnutrition in an obese COPD patient as illustrated in the BIVA nomogram. The position of the measurement point in the BIVA nomogram is below the line of normal BCM values long axis and above the line of normal TBW values short axis between the 75 th and 95 th tolerance ellipse. The position in the lower right quadrant indicates malnutrition. The BIA parameter values listed in table 2 can be interpreted as follows: The fat mass lies above the normal range in line with the increased BMI. BCM lies within the normal range. At first sight this does not fit in with the finding of the BIVA nomogram, which indicates malnutrition. The fact that the calculated BCM is within the range of normal values here may be explained as follows: It needs to be considered that BCM is dependent on the patient's fluid status TBW. This means that a BCM within the normal range does not necessarily mean a normal nutritional status but may also be due to increased TBW. This indicates that BCM is actually reduced. BCM therefore only appears to lie within the range of normal values because of the increased TBW. In contrast to this somewhat complex interpretation of the calculated BIA values, the suspected diagnosis of malnutrition can be established at a glance by BIVA. In addition, it is confirmed that the calculated BCM is too high because of the increased TBW position of the measurement point in the BIVA nomogram above the line of normal TBW values. Conclusion: Despite the presence of obesity the patient is exhibiting malnutrition. The position of the measurement point in the BIVA nomogram in the right lower quadrant between the 75 th and the 95 th tolerance ellipse provides an indication for the suspected diagnosis of malnutrition. The measurement point in the BIVA nomogram Figure 4 in this patient is far below the line of normal BCM values long axis and well above the line of normal TBW values short axis , far outside the 95 th tolerance ellipse. The position of the measurement point in the lower right quadrant points to malnutrition in the form of cachexia. Cachexia as illustrated in the BIVA nomogram. The position of the measurement point in the BIVA nomogram is far below the line of normal BCM values long axis and well above the line of normal TBW values short axis far outside the 95 th tolerance ellipse. The position in the lower right quadrant points to cachexia. The BIA parameter values listed in table 3 can be interpreted as follows: The fat mass lies below the normal range in line with the reduced BMI. The calculated values for BCM und TBW are reduced. It needs to be considered as regards the reduced BCM value that BCM is dependent on the patient's fluid status TBW. This means that a reduced BCM does not necessarily point to malnutrition but may also be due to a low TBW. In this example also BIVA provides a more efficient assessment of the nutritional status than the calculated BIA parameters. Conclusion: All the values listed in the table are below the normal range and the measurement point in the BIVA nomogram is outside the 95 th tolerance ellipse in the lower right quadrant. This indicates severe malnutrition in the form of cachexia. The assessment of the BIVA nomogram is sufficient for the suspected diagnosis of cachexia. The measurement point in the BIVA nomogram Figure 5 in this patient is above the line of normal BCM values long axis and well below the line of normal TBW values short axis on the 95 th tolerance ellipse. The position of the measurement point in the lower left quadrant points to water retention in the form of oedema. Oedema due to right heart failure as illustrated in the BIVA nomogram. The position of the measurement point in the BIVA nomogram is above the line of normal BCM values long axis and well below the line of normal TBW values short axis on the 95 th tolerance ellipse. The position in the lower left quadrant indicates the presence of increased water retention. The BIA parameter values listed in table 4 can be interpreted as follows: Body fat mass lies above the normal range in line with the increased BMI. The determined TBW is increased and the calculated BCM lies in the upper range of normal. These findings are consistent with the position of the measurement point above the line of normal BCM values and below the line of normal TBW values in the lower left quadrant. With the derived normal BIA value for BCM it needs once again to be taken into account here that BCM is dependent on the patient's fluid status TBW. This means that a BCM within the normal range does not necessarily indicate an actually normal BCM or normal nutritional status but may also appear normal due to an increased TBW. In addition to the increased TBW, ECM is also markedly increased, indicating oedema. The suspicion of oedema is established at a glance with BIVA. BIVA confirms simply and rapidly the calculated BIA values BCM and TBW. The suspicion of oedema was confirmed on physical examination of the legs. Conclusion: The values listed in the table for TBW and ECM are outside the normal range and the measurement point in the BIVA nomogram is on the 95 th tolerance ellipse in the lower left quadrant, indicating oedema. The determined BCM is in the upper range of normal and the measurement point in the BIVA nomogram is above the line of normal BCM values. The position of the measurement point in the nomogram provides an indication for the suspected diagnosis of oedema. For the general differential diagnosis of underweight we present a female patient with anorexia: female, The measurement point in the BIVA nomogram Figure 6 lies almost on the line of normal BCM values long axis and far above the line of normal TBW values short axis outside the 95 th tolerance ellipse. The position of the measurement point in the upper right quadrant points to the presence of anorexia. Anorexia as illustrated in the BIVA nomogram. The position of the measurement point in the BIVA nomogram is almost on the line of normal BCM values long axis and far above the line of normal TBW values short axis outside the 95 th tolerance ellipse. The position in the upper right quadrant points to the presence of anorexia. The BIA parameter values listed in table 5 can be interpreted as follows: Body fat mass is reduced in line with the low BMI. TBW is markedly reduced and BCM also is decreased. With the reduced BCM it needs to be kept in mind here that BCM is dependent on the patient's fluid status TBW. This means that a lower BCM may also appear reduced due to a lower TBW. This indicates that BCM is normal and that the calculated value was too low only because of the low TBW. BIVA confirms the suspicion raised by the BIA values that the calculated BCM was too low because of the reduced TBW. Again, the suspected diagnosis of anorexia can be established more efficiently and more reliably by BIVA. Conclusion: The patient exhibits a markedly reduced BMI, decreased body water and a normal BCM in the form of anorexia. The position of the measurement point in the nomogram in the upper right quadrant outside the 95 th tolerance ellipse provides an indication for the suspected diagnosis of anorexia. Bioelectrical impedance analysis BIA , particularly in combination with bioelectrical impedance vector analysis BIVA , provides a viable opportunity for evaluating body composition in humans. As the examples suggest the interpretation of BIA results is often complex and a suspected diagnosis can be established more efficiently and more reliably by integrating BIVA into the patient assessment process. Engelen MP, Schols AM, Baken WC, Wesseling GJ, Wouters EF: Nutritional depletion in relation to respiratory and peripheral skeletal muscle function in out-patients with COPD. Eur Respir J. Article CAS PubMed Google Scholar. Schols AM, Broekhuizen R, Weling-Scheepers CA, Wouters EF: Body composition and mortality in chronic obstructive pulmonary disease. Am J Clin Nutr. CAS PubMed Google Scholar. Engelen MP, Schols AM, Does JD, Wouters EF: Skeletal muscle weakness is associated with wasting of extremity fat-free mass but not with airflow obstruction in patients with chronic obstructive pulmonary disease. King DA, Cordova F, Scharf SM: Nutritional aspects of chronic obstructive pulmonary disease. Proc Am Thorac Soc. Article PubMed PubMed Central Google Scholar. Shoup R, Dalsky G, Warner S, Davies M, Connors M, Khan M, Khan F, ZuWallack R: Body composition and health-related quality of life in patients with obstructive airways disease. Hallin R, Koivisto-Hursti UK, Lindberg E, Janson C: Nutritional status, dietary energy intake and the risk of exacerbations in patients with chronic obstructive pulmonary disease COPD. Respir Med. Article PubMed Google Scholar. Schols AM: Nutrition in chronic obstructive pulmonary disease. Curr Opin Pulm Med. Soeters PB, Schols AM: Advances in understanding and assessing malnutrition. Curr Opin Clin Nutr Metab Care. Global Initiative for Chronic Obstructive Lung Disease: Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease updated com ]. Vestbo J, Prescott E, Almdal T, Dahl M, Nordestgaard BG, Andersen T, Sørensen TI, Lange P: Body mass, fat-free body mass, and prognosis in patients with chronic obstructive pulmonary disease from a random population sample: findings from the Copenhagen City Heart Study. Am J Respir Crit Care Med. PubMed Google Scholar. Ischaki E, Papatheodorou G, Gaki E, Papa I, Koulouris N, Loukides S: Body mass and fat-free mass indices in COPD: relation with variables expressing disease severity. Miller A, Strauss BJ, Mol S, Kyoong A, Holmes PH, Finlay P, Bardin PG, Guy P: Dual-energy X-ray absorptiometry is the method of choice to assess body composition in COPD. Lerario MC, Sachs A, Lazaretti-Castro M, Saraiva LG, Jardim JR: Body composition in patients with chronic obstructive pulmonary disease: which method to use in clinical practice?. Br J Nutr. Lee SY, Gallagher D: Assessment methods in human body composition. Curr Opin Clin Nutr Metabol Care. Article Google Scholar. Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gómez JM, Heitmann BL, Kent-Smith L, Melchior JC, Pirlich M, Scharfetter H, Schols AM, Pichard C: Bioelectrical impedance analysis-part I: review of principles and methods. Clin Nutr. Matthie JR: Bioimpedance measurements of human body composition: critical analysis and outlook. Expert Rev Med Devices. Mattsson S, Thomas BJ: Development of methods for body composition studies. Phys Med Biol. Kushner RF: Bioelectrical impedance analysis: a review of principles and applications. J Am Coll Nutr. Kuzma AM, Meli Y, Meldrum C, Jellen P, Butler-Labair M, Koczen-Doyle D, Rising P, Stavrolakes K, Brogan F: Multidisciplinary care of the patient with chronic obstructive pulmonary disease. The BIA compendium. de ]3. Bosy-Westphal A, Danielzik S, Dörhöfer RP, Piccoli A, Müller MJ: Patterns of bioelectrical impedance vector distribution by body mass index and age: implications for body-composition analysis. Erratum in: Am J Clin Nutr , Piccoli A: Bioelectric impedance vector distribution in peritoneal dialysis patients with different hydration status. Kidney Int. Dehghan M, Merchant AT: Is bioelectrical impedance accurate for use in large epidemiological studies?. Nutr J. Barbosa-Silva MC, Barros AJ: Bioelectrical impedance analysis in clinical practice: a new perspective on its use beyond body composition equations. Buchholz AC, Bartok C, Schoeller DA: The validity of bioelectrical impedance models in clinical populations. Nutr Clin Pract. Bozzetto S, Piccoli A, Montini G: Bioelectrical impedance vector analysis to evaluate relative hydration status. Pediatr Nephrol. Creutzberg EC, Wouters EF, Mostert R, Weling-Scheepers CA, Schols AM: Efficacy of nutritional supplementation therapy in depleted patients with chronic obstructive pulmonary disease. Download references. Nutritional Consulting Practice, Emil-Schüller-Straße, Koblenz, , Germany. Pneumology Practice, Emil-Schüller-Straße, Koblenz, , Germany. KG, Binger Straße, Ingelheim, , Germany. Department of Pulmonary Disease, III. Medical Clinic, Johannes Gutenberg-University, Langenbeckstraße, Mainz, , Germany. You can also search for this author in PubMed Google Scholar. Correspondence to Thomas Glaab. The authors declare that they have no competing interests. TG and MMG were employees of Boehringer Ingelheim at the time of manuscript submission. AWK and TG conceived of the review, drafted and coordinated the manuscript. MMG and AK critically discussed and helped to draft the manuscript. Clin Nutr. Article PubMed Google Scholar. Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Manuel Gomez J. Bioelectrical impedance analysis-part II: utilization in clinical practice. Campa F, Gobbo LA, Stagi S, Cyrino LT, Toselli S, Marini E, et al. Bioelectrical impedance analysis versus reference methods in the assessment of body composition in athletes. Eur J Appl Physiol. Lukaski HC. Evolution of bioimpedance: a circuitous journey from estimation of physiological function to assessment of body composition and a return to clinical research. Eur J Clin Nutr. Lukaski HC, Kyle UG, Kondrup J. Assessment of adult malnutrition and prognosis with bioelectrical impedance analysis: phase angle and impedance ratio. Curr Opin Clin Nutr Metab Care. Heitmann BL. Prediction of body water and fat in adult Danes from measurement of electrical impedance. A validation study. Int J Obes. CAS PubMed Google Scholar. Bedogni G, Grugni G, Tringali G, Agosti F, Sartorio A. Assessment of fat-free mass from bioelectrical impedance analysis in obese women with Prader-Willi syndrome. Ann Hum Biol. Cleary J, Daniells S, Okely AD, Batterham M, Nicholls J. Predictive validity of four bioelectrical impedance equations in determining percent fat mass in overweight and obese children. J Am Diet Assoc. Costa RFD, Masset K, Silva AM, Cabral B, Dantas PMS Development and cross-validation of predictive equations for fat-free mass and lean soft tissue mass by bioelectrical impedance in Brazilian women. Deurenberg P, van der Kooy K, Leenen R, Weststrate JA, Seidell JC. Sex and age specific prediction formulas for estimating body composition from bioelectrical impedance: a cross-validation study. Deurenberg P, van der Kooy K, Paling A, Withagen P. Assessment of body composition in year old children by bioelectrical impedance. Dey DK, Bosaeus I, Lissner L, Steen B. Body composition estimated by bioelectrical impedance in the Swedish elderly. Development of population-based prediction equation and reference values of fat-free mass and body fat for and y olds. Gonzalez MC, Orlandi SP, Santos LP, Barros AJD. Body composition using bioelectrical impedance: Development and validation of a predictive equation for fat-free mass in a middle-income country. Goran MI, Kaskoun MC, Carpenter WH, Poehlman ET, Ravussin E, Fontvieille AM. Estimating body composition of young children by using bioelectrical resistance. J Appl Physiol. Kanellakis S, Skoufas E, Karaglani E, Ziogos G, Koutroulaki A, Loukianou F. Development and validation of a bioelectrical impedance prediction equation estimating fat free mass in Greek - Caucasian adult population. Clin Nutr ESPEN. Kotler DP, Burastero S, Wang J, Pierson RN,Jr. Prediction of body cell mass, fat-free mass, and total body water with bioelectrical impedance analysis: effects of race, sex, and disease. Am J Clin Nutr. Kyle UG, Genton L, Karsegard L, Slosman DO, Pichard C. Single prediction equation for bioelectrical impedance analysis in adults aged 20—94 years. Luke A, Bovet P, Forrester TE, Lambert EV, Plange-Rhule J, Dugas LR. Prediction of fat-free mass using bioelectrical impedance analysis in young adults from five populations of African origin. Article CAS PubMed PubMed Central Google Scholar. Matias CN, Campa F, Santos DA, Lukaski H, Sardinha LB, Silva AM. Fat-free Mass Bioelectrical Impedance Analysis Predictive Equation for Athletes using a 4-Compartment Model. Int J Sports Med. Steinberg A, Manlhiot C, Li P, Metivier E, Pencharz PB, McCrindle BW. Development and Validation of Bioelectrical Impedance Analysis Equations in Adolescents with Severe Obesity. J Nutr. Stolarczyk LM, Heyward VH, Goodman JA, Grant DJ, Kessler KL, Kocina PS, et al. Predictive accuracy of bioimpedance equations in estimating fat-free mass of Hispanic women. Med Sci Sports Exerc. Stolarczyk LM, Heyward VH, Hicks VL, Baumgartner RN. Predictive accuracy of bioelectrical impedance in estimating body composition of Native American women. Sun SS, Chumlea WC, Heymsfield SB, Lukaski HC, Schoeller D, Friedl K, et al. Development of bioelectrical impedance analysis prediction equations for body composition with the use of a multicomponent model for use in epidemiologic surveys. Tint MT, Ward LC, Soh SE, Aris IM, Chinnadurai A, Saw SM, et al. Estimation of fat-free mass in Asian neonates using bioelectrical impedance analysis. Br J Nutr. da Costa RF, Silva AM, Masset K, Cesário TM, Cabral B, Ferrari G, et al. Development and Cross-Validation of a Predictive Equation for Fat-Free Mass in Brazilian Adolescents by Bioelectrical Impedance. Front Nutr. Article PubMed PubMed Central Google Scholar. Wang L, Hui SS, Wong SH. Validity of bioelectrical impedance measurement in predicting fat-free mass of Chinese children and adolescents. Med Sci Monit. Nightingale CM, Rudnicka AR, Owen CG, Donin AS, Newton SL, Furness CA, et al. Are ethnic and gender specific equations needed to derive fat free mass from bioelectrical impedance in children of South asian, black african-Caribbean and white European origin? Results of the assessment of body composition in children study. PLoS One. Validation of anthropometric and bioelectrical impedance analysis BIA equations to predict total body water in a group of Cameroonian preschool children using deuterium dilution method. Article CAS Google Scholar. van Zyl A, White Z, Ferreira J, Wenhold FAM. Developing an Impedance Based Equation for Fat-Free Mass of Black Preadolescent South African Children. Nutrients ; Nigam P, Misra A, Colles SL. Comparison of DEXA-derived body fat measurement to two race-specific bioelectrical impedance equations in healthy Indians. Diabetes Metab Syndr. Beaudart C, Bruyère O, Geerinck A, Hajaoui M, Scafoglieri A, Perkisas S, et al. Equation models developed with bioelectric impedance analysis tools to assess muscle mass: A systematic review. Matias CN, Santos DA, Judice PB, Magalhaes JP, Minderico CS, Fields DA. Estimation of total body water and extracellular water with bioimpedance in athletes: A need for athlete-specific prediction models. Sergi G, Bussolotto M, Perini P, Calliari I, Giantin V, Ceccon A, et al. Accuracy of bioelectrical impedance analysis in estimation of extracellular space in healthy subjects and in fluid retention states. Ann Nutr Metab. Dittmar M, Reber H. Am J Hum Biol. Flury S, Trachsler J, Schwarz A, Ambuhl PM. Quantification of excretory renal function and urinary protein excretion by determination of body cell mass using bioimpedance analysis. BMC Nephrol. Janssen I, Heymsfield SB, Baumgartner RN, Ross R. Estimation of skeletal muscle mass by bioelectrical impedance analysis. Silva AM, Fields DA, Heymsfield SB, Sardinha LB. Body composition and power changes in elite judo athletes. Body water distribution and risk of cardiovascular morbidity and mortality in a healthy population: A prospective cohort study. Relationship between changes in total-body water and fluid distribution with maximal forearm strength in elite judo athletes. J Strength Cond Res. Silva AM, Matias CN, Santos DA, Rocha PM, Minderico CS, Sardinha LB. Increases in intracellular water explain strength and power improvements over a season. Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Moisey LL, Mourtzakis M, Cotton BA, Premji T, Heyland DK, Wade CE, et al. Skeletal muscle predicts ventilator-free days, ICU-free days, and mortality in elderly ICU patients. Crit Care. Soares MN, Eggelbusch M, Naddaf E, Gerrits KHL, van der Schaaf M, van den Borst B, et al. Skeletal muscle alterations in patients with acute Covid and post-acute sequelae of Covid J Cachexia Sarcopenia Muscle. Weijs PJ, Looijaard WG, Dekker IM, Stapel SN, Girbes AR, Oudemans-van Straaten HM, et al. Low skeletal muscle area is a risk factor for mortality in mechanically ventilated critically ill patients. Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. Buffa R, Floris G, Marini E. Assessment of nutritional status in free-living elderly individuals by bioelectrical impedance vector analysis. Langer RD, Larsen SC, Ward LC, Heitmann BL. Phase angle measured by bioelectrical impedance analysis and the risk of cardiovascular disease among adult Danes. Campa F, Matias CN, Marini E, Heymsfield SB, Toselli S, Sardinha LB, et al. Identifying Athlete Body Fluid Changes During a Competitive Season With Bioelectrical Impedance Vector Analysis. Int J Sports Physiol Perform. Castizo-Olier J, Irurtia A, Jemni M, Carrasco-Marginet M, Fernandez-Garcia R, Rodriguez FA. Bioelectrical impedance vector analysis BIVA in sport and exercise: Systematic review and future perspectives. Girma T, Hother Nielsen AL, Kaestel P, Abdissa A, Michaelsen KF, Friis H, et al. Biochemical and anthropometric correlates of bio-electrical impedance parameters in severely malnourished children: A cross-sectional study. Girma T, Kaestel P, Molgaard C, Ritz C, Andersen GS, Michaelsen KF, et al. Utility of bio-electrical impedance vector analysis for monitoring treatment of severe acute malnutrition in children. Lee S, Bountziouka V, Lum S, Stocks J, Bonner R, Naik M, et al. Ethnic variability in body size, proportions and composition in children aged 5 to 11 years: is ethnic-specific calibration of bioelectrical impedance required? Marini E, Campa F, Buffa R, Stagi S, Matias CN, Toselli S, et al. Phase angle and bioelectrical impedance vector analysis in the evaluation of body composition in athletes. Moroni A, Varde C, Giustetto A, Stagi S, Marini E, Micheletti Cremasco M. Bioelectrical Impedance Vector Analysis BIVA for the monitoring of body composition in pregnancy. Norman K, Stobäus N, Pirlich M, Bosy-Westphal A. Bioelectrical phase angle and impedance vector analysis—clinical relevance and applicability of impedance parameters. Gupta D, Lammersfeld CA, Vashi PG, King J, Dahlk SL, Grutsch JF, et al. Bioelectrical impedance phase angle as a prognostic indicator in breast cancer. BMC Cancer. Langer RD, Ward LC, Larsen SC, Heitmann BL. Can change in phase angle predict the risk of morbidity and mortality during an year follow-up period? A cohort study among adults. Sardinha LB. Physiology of exercise and phase angle: another look at BIA. Gupta D, Lis CG, Dahlk SL, Vashi PG, Grutsch JF, Lammersfeld CA. Bioelectrical impedance phase angle as a prognostic indicator in advanced pancreatic cancer. Kyle UG, Genton L, Pichard C. Low phase angle determined by bioelectrical impedance analysis is associated with malnutrition and nutritional risk at hospital admission. Kyle UG, Soundar EP, Genton L, Pichard C. Can phase angle determined by bioelectrical impedance analysis assess nutritional risk? A comparison between healthy and hospitalized subjects. Schwenk A, Beisenherz A, Romer K, Kremer G, Salzberger B, Elia M. Phase angle from bioelectrical impedance analysis remains an independent predictive marker in HIV-infected patients in the era of highly active antiretroviral treatment. Valdespino-Trejo A, Orea-Tejeda A, Castillo-Martinez L, Keirns-Davis C, Montanez-Orozco A, Ortiz-Suarez G, et al. Low albumin levels and high impedance ratio as risk factors for worsening kidney function during hospitalization of decompensated heart failure patients. Exp Clin Cardiol. PubMed PubMed Central Google Scholar. Brantlov S, Jødal L, Andersen RF, Lange A, Rittig S, Ward LC. An evaluation of phase angle, bioelectrical impedance vector analysis and impedance ratio for the assessment of disease status in children with nephrotic syndrome. Oh JH, Song S, Rhee H, Lee SH, Kim DY, Choe JC, et al. Normal Reference Plots for the Bioelectrical Impedance Vector in Healthy Korean Adults. J Korean Med Sci. Barbosa-Silva MC, Barros AJ, Wang J, Heymsfield SB, Pierson RN Jr. Bioelectrical impedance analysis: population reference values for phase angle by age and sex. Kuchnia AJ, Teigen LM, Cole AJ, Mulasi U, Gonzalez MC, Heymsfield SB, et al. Phase Angle and Impedance Ratio: Reference Cut-Points From the United States National Health and Nutrition Examination Survey From Bioimpedance Spectroscopy Data. JPEN J Parenter Enter Nutr. Bosy-Westphal A, Danielzik S, Dorhofer RP, Later W, Wiese S, Muller MJ. Phase angle from bioelectrical impedance analysis: population reference values by age, sex, and body mass index. Kyle UG, Genton L, Slosman DO, Pichard C. Fat-free and fat mass percentiles in healthy subjects aged 15 to 98 years. Campa F, Thomas DM, Watts K, Clark N, Baller D, Morin T, et al. Reference Percentiles for Bioelectrical Phase Angle in Athletes. Wells JCK, Williams JE, Quek RY, Fewtrell MS. Piccoli A, Rossi B, Pillon L, Bucciante G. A new method for monitoring body fluid variation by bioimpedance analysis: the RXc graph. Kidney Int. Marini E, Sergi G, Succa V, Saragat B, Sarti S, Coin A, et al. Efficacy of specific bioelectrical impedance vector analysis BIVA for assessing body composition in the elderly. Buffa R, Saragat B, Cabras S, Rinaldi AC, Marini E. Accuracy of specific BIVA for the assessment of body composition in the United States population. Stagi S, Silva AM, Jesus F, Campa F, Cabras S, Earthman CP, et al. Usability of classic and specific bioelectrical impedance vector analysis in measuring body composition of children. Wells JC, Williams JE, Ward LC, Fewtrell MS. Utility of specific bioelectrical impedance vector analysis for the assessment of body composition in children. De Palo T, Messina G, Edefonti A, Perfumo F, Pisanello L, Peruzzi L, et al. Normal values of the bioelectrical impedance vector in childhood and puberty. Ibanez ME, Mereu E, Buffa R, Gualdi-Russo E, Zaccagni L, Cossu S, et al. New specific bioelectrical impedance vector reference values for assessing body composition in the Italian-Spanish young adult population. Piccoli A, Nigrelli S, Caberlotto A, Bottazzo S, Rossi B, Pillon L, et al. Bivariate normal values of the bioelectrical impedance vector in adult and elderly populations. Piccoli A, Pillon L, Dumler F. Impedance vector distribution by sex, race, body mass index, and age in the United States: standard reference intervals as bivariate Z scores. Ward LC, Heitmann BL, Craig P, Stroud D, Azinge EC, Jebb S, et al. Association between ethnicity, body mass index, and bioelectrical impedance. Implications for the population specificity of prediction equations. Ann N. Y Acad Sci. Heitmann BL, Swinburn BA, Carmichael H, Rowley K, Plank L, McDermott R, et al. Are there ethnic differences in the association between body weight and resistance, measured by bioelectrical impedance? Int J Obes Relat Metab Disord. Baumgartner RN, Heymsfield SB, Roche AF. Human body composition and the epidemiology of chronic disease. Obes Res. Shen W, Punyanitya M, Silva AM, Chen J, Gallagher D, Sardinha LB, et al. Sexual dimorphism of adipose tissue distribution across the lifespan: a cross-sectional whole-body magnetic resonance imaging study. Nutr Metab Lond. Silva AM, Shen W, Heo M, Gallagher D, Wang Z, Sardinha LB, et al. Ethnicity-related skeletal muscle differences across the lifespan. Ward LC. Electrical Bioimpedance: From the Past to the Future. J Electr Bioimpedance. Marini E, Buffa R, Saragat B, Coin A, Toffanello ED, Berton L. The potential of classic and specific bioelectrical impedance vector analysis for the assessment of sarcopenia and sarcopenic obesity. |
| About bioelectrical impedance analysis and body composition measurement | Erratum in: Am J Clin Nutr , Piccoli A: Bioelectric impedance vector distribution in peritoneal dialysis patients with different hydration status. Kidney Int. Dehghan M, Merchant AT: Is bioelectrical impedance accurate for use in large epidemiological studies?. Nutr J. Barbosa-Silva MC, Barros AJ: Bioelectrical impedance analysis in clinical practice: a new perspective on its use beyond body composition equations. Buchholz AC, Bartok C, Schoeller DA: The validity of bioelectrical impedance models in clinical populations. Nutr Clin Pract. Bozzetto S, Piccoli A, Montini G: Bioelectrical impedance vector analysis to evaluate relative hydration status. Pediatr Nephrol. Creutzberg EC, Wouters EF, Mostert R, Weling-Scheepers CA, Schols AM: Efficacy of nutritional supplementation therapy in depleted patients with chronic obstructive pulmonary disease. Download references. Nutritional Consulting Practice, Emil-Schüller-Straße, Koblenz, , Germany. Pneumology Practice, Emil-Schüller-Straße, Koblenz, , Germany. KG, Binger Straße, Ingelheim, , Germany. Department of Pulmonary Disease, III. Medical Clinic, Johannes Gutenberg-University, Langenbeckstraße, Mainz, , Germany. You can also search for this author in PubMed Google Scholar. Correspondence to Thomas Glaab. The authors declare that they have no competing interests. TG and MMG were employees of Boehringer Ingelheim at the time of manuscript submission. AWK and TG conceived of the review, drafted and coordinated the manuscript. MMG and AK critically discussed and helped to draft the manuscript. All authors read and approved the final manuscript. The contents of this original manuscript have not been previously presented or submitted elsewhere. Open Access This article is published under license to BioMed Central Ltd. Reprints and permissions. Walter-Kroker, A. et al. A practical guide to bioelectrical impedance analysis using the example of chronic obstructive pulmonary disease. Nutr J 10 , 35 Download citation. Received : 08 November Accepted : 21 April Published : 21 April Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Download ePub. Abstract Bioelectrical impedance analysis BIA is a simple, inexpensive, quick and non-invasive technique for measuring body composition. Introduction Loss of body weight and depletion of fat free muscle mass are common and serious problems in patients with chronic obstructive pulmonary disease COPD irrespective of the degree of airflow limitation [ 1 — 3 ]. Basic principles Bioelectrical impedance analysis BIA BIA is a method for estimating body composition. From the determined impedance a number of BIA parameters can be estimated [ 20 ]: Body cell mass BCM consists of all cells that have an effect on metabolism e. extracellular water retention e. extracellular loss of water e. high portion of muscle, water retention e. Factors impacting BIA results [ 16 , 18 , 20 , 23 , 25 ]: 1. weight and height should be measured directly by the investigator 2. position of the body and limbs supine position, arms abducted at least 30°, legs abducted at approximately 45° 3. consumption of food and beverages no beverages for at least 12 hours previously, fasted state for at least 2 hours 4. medical conditions and medication that have an impact on the fluid and electrolyte balance; infection and cutaneous disease that may alter the electrical transmission between electrode and skin 6. environmental conditions e. ambient temperature 7. individual characteristics e. skin temperature, sex, age, race 8. ethnic variation 9. non-adherence of electrodes, use of wrong electrodes, loosening of cable clip, interchanging of electrodes BIA parameters are largely dependent on the patient's hydration status. BIVA bioelectrical impedance vector analysis BIVA as an integrated part of BIA measurement is a simple, quick and clinically valuable method for assessing fluid status TBW and body cell mass BCM. Figure 1. Full size image. Figure 2. Table 1 Normal finding. Full size table. Figure 3. Table 2 Malnutrition in an obese COPD patient Full size table. Figure 4. Table 3 Cachexia Full size table. Figure 5. Table 4 Oedema due to right heart failure Full size table. Figure 6. Table 5 Anorexia Full size table. Summary Bioelectrical impedance analysis BIA , particularly in combination with bioelectrical impedance vector analysis BIVA , provides a viable opportunity for evaluating body composition in humans. Abbreviations ATS: American Thoracic Society BCM: body cell mass BIA: bioelectrical impedance analysis BIVA: bioelectrical impedance vector analysis BMI: body mass index COPD: chronic obstructive pulmonary disease ECM: extra cellular mass ERS: European Respiratory Society FFM: fat free mass FM: fat mass GOLD: Global Initiative for Chronic Obstructive Lung Disease TBW: total body water. References Engelen MP, Schols AM, Baken WC, Wesseling GJ, Wouters EF: Nutritional depletion in relation to respiratory and peripheral skeletal muscle function in out-patients with COPD. Article CAS PubMed Google Scholar Schols AM, Broekhuizen R, Weling-Scheepers CA, Wouters EF: Body composition and mortality in chronic obstructive pulmonary disease. CAS PubMed Google Scholar Engelen MP, Schols AM, Does JD, Wouters EF: Skeletal muscle weakness is associated with wasting of extremity fat-free mass but not with airflow obstruction in patients with chronic obstructive pulmonary disease. CAS PubMed Google Scholar King DA, Cordova F, Scharf SM: Nutritional aspects of chronic obstructive pulmonary disease. Article PubMed PubMed Central Google Scholar Shoup R, Dalsky G, Warner S, Davies M, Connors M, Khan M, Khan F, ZuWallack R: Body composition and health-related quality of life in patients with obstructive airways disease. Article CAS PubMed Google Scholar Hallin R, Koivisto-Hursti UK, Lindberg E, Janson C: Nutritional status, dietary energy intake and the risk of exacerbations in patients with chronic obstructive pulmonary disease COPD. Article PubMed Google Scholar Schols AM: Nutrition in chronic obstructive pulmonary disease. Article CAS PubMed Google Scholar Soeters PB, Schols AM: Advances in understanding and assessing malnutrition. Article PubMed Google Scholar Global Initiative for Chronic Obstructive Lung Disease: Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease updated com ] Vestbo J, Prescott E, Almdal T, Dahl M, Nordestgaard BG, Andersen T, Sørensen TI, Lange P: Body mass, fat-free body mass, and prognosis in patients with chronic obstructive pulmonary disease from a random population sample: findings from the Copenhagen City Heart Study. PubMed Google Scholar Ischaki E, Papatheodorou G, Gaki E, Papa I, Koulouris N, Loukides S: Body mass and fat-free mass indices in COPD: relation with variables expressing disease severity. Article PubMed Google Scholar Miller A, Strauss BJ, Mol S, Kyoong A, Holmes PH, Finlay P, Bardin PG, Guy P: Dual-energy X-ray absorptiometry is the method of choice to assess body composition in COPD. Article PubMed Google Scholar Lerario MC, Sachs A, Lazaretti-Castro M, Saraiva LG, Jardim JR: Body composition in patients with chronic obstructive pulmonary disease: which method to use in clinical practice?. Article CAS PubMed Google Scholar Lee SY, Gallagher D: Assessment methods in human body composition. Article Google Scholar Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gómez JM, Heitmann BL, Kent-Smith L, Melchior JC, Pirlich M, Scharfetter H, Schols AM, Pichard C: Bioelectrical impedance analysis-part I: review of principles and methods. Article PubMed Google Scholar Matthie JR: Bioimpedance measurements of human body composition: critical analysis and outlook. Article PubMed Google Scholar Mattsson S, Thomas BJ: Development of methods for body composition studies. Article CAS PubMed Google Scholar Kushner RF: Bioelectrical impedance analysis: a review of principles and applications. CAS PubMed Google Scholar Kuzma AM, Meli Y, Meldrum C, Jellen P, Butler-Labair M, Koczen-Doyle D, Rising P, Stavrolakes K, Brogan F: Multidisciplinary care of the patient with chronic obstructive pulmonary disease. Article PubMed PubMed Central Google Scholar The BIA compendium. The second square bracket in Eq. When the current source has a finite output impedance R s , the measured 4-point impedance also decreases with the increase in contact resistance due to the decrease in current flow into the human body. In the 2-point measurement mode, voltage and current electrodes on the same side are electrically connected with internal analog switches, so that four electrodes can be operated as two electrodes. The measured 2-point impedance Z 2 can be expressed by Eq. Because there are two equations Eq. We performed an experiment to verify the proposed method by using a simple electrical circuit. Discrete resistors were used to model body impedance and contact resistance. The resistance value of the model for body impedance Z body was fixed at Ω. Figure 3 c shows the variation of measured impedance values before and after contact resistance compensation when the contact resistance varied from 0 to 3 k Ω. A novel wrist-wearable bioelectrical impedance analyzer with contact resistance compensation function was developed. Figure 4 a shows the block diagram of the developed BIA device. a Hardware block diagram of the overall system, b current path for 4-point measurement mode, and c current path for 2-point measurement mode. Z body measured impedance, Z i input impedance of the voltmeter, R s output impedance of the current source, R c contact resistance, I current, V M measured voltage, SW switch, α the size ratio of voltage to current electrode, β the size ratio of finger to wrist electrode. The electrodes part is composed of two current-driving electrodes and two voltage-sensing electrodes. The total area of finger electrodes a pair of one current electrode and one voltage electrode on the top side of the device was 68 mm 2 and that of wrist electrodes another pair of one current electrode and one voltage electrode on the bottom side of the device was mm 2. The AFE S3FBP5A, BioProcessor2, Samsung Electronics delivers 30 μA sinusoidal alternating current with 50 kHz frequency to the two current electrodes and measures voltage drop between the two voltage electrodes. Acquired voltage values were converted to digital signal by analog-to-digital converter ADC , and this digital code was converted to impedance value with a calibration curve which had been made by calibration process. The internal micro controller unit of BioProcessor2 calculated body fat, lean body mass, and body water volume using impedance data and user profile information such as height, age, weight, and gender. The measured data was displayed on liquid crystal display. Bluetooth was used for data transfer between body fat analyzer and a personal computer, and external flash memory was used for user data storage. Contact resistance compensation function was adapted to our bioelectrical impedance analyzer. The contact resistance compensation circuit included two analog switches. One analog switch was connected between the current and voltage path of the finger electrodes, and the other was connected between the current and voltage path of the wrist electrodes. For the 4-point measurement mode, analog switches were turned off, and for the 2-point measurement mode, analog switches were turned on for electrical connection of each voltage and current electrode pair. This very simple and small compensation circuit had a flexibility that allowed easy adaptation to variable AFEs. The dynamic range the range of measureable impedance was configured to cover the range of body impedance and contact resistance. TX dynamic range the range of impedance that current source can drive and RX dynamic range the range of impedance that voltmeter can measure should satisfy the overall system dynamic range required. Figure 4 b,c show the current paths for the 4-point and 2-point measurement modes, respectively. Based on our user data from volunteers in , TX and RX dynamic range were set as 15 kΩ and 10 kΩ, respectively, by adjusting the driving current level To improve measurement accuracy along the wide dynamic range stated above, a calibration algorithm that adopts 4-point coordinate conversion is proposed, in which four high-precision reference resistors are used to reduce the errors in three resistance sections. The ADC output code was converted to impedance by calibration process. The ADC output code and body impedance Z body have a nonlinear relationship due to the finite input impedance of the voltmeter Z i and the finite output impedance of the current source R s , since the equivalent impedance detected by the voltmeter is the parallel combination impedance of body impedance Z body , Z i , and R s as in Eq. Note that contact resistance R c is zero during the calibration process. In the calibration curve, the measurement on the x-axis is changed from reference impedance to parallel combination impedance of reference impedance, Z i , and R s. This change enhances the linearity of the calibration curve and the accuracy of measurement. The dashed lines are ideal calibration curves, and the solid lines are extracted calibration curves derived by calibration process. It is easily seen from Fig. Calibration algorithm was developed using C code and loaded as firmware of the device. Whenever the device is turned on, self-calibration is conducted using 4 reference resistance values as shown in Fig. Calibration curve and measurement error at midpoint between two reference points for a 2-point calibration, b 4-point calibration, and c 4-point coordinate conversion calibration. ADC analog-to-digital converter, Z i input impedance of the voltmeter, R s output impedance of the current source. Figure 6 shows the measurement procedure and corresponding graphical user interface of our wrist-wearable device. On the home screen, a user can register information gender, age, height, and weight by touching the [CHG INFO] icon. If the user is already registered on the device, registration process can be skipped by touching [USER] icon. The measurement is initiated by touching the [START] icon. When the proper posture is maintained, BIA measurement begins automatically. It takes about 7 s to complete the test: 3 s for 4-point measurement, 1 s for measurement mode change, and 3 s for 2-point measurement. When the measurement is completed, percentage body fat, lean mass, and basal metabolic rate are shown on the screen. Measurement procedure and corresponding graphical user interface of the wrist-wearable bioelectrical impedance analyzer. To evaluate the accuracy of our bioelectrical impedance analyzer, a clinical test was conducted on volunteers who were recruited at Seoul St. Participants were recruited to have as uniform distributions as possible on the bases of gender, age, and body mass index BMI. The BIA pretesting client guidelines 20 in Table 2 were explained to all volunteers before the clinical test. Four different devices were used in the clinical test: our wrist-wearable device, a whole-body composition analyzer InBody , an upper-body portable body fat analyzer Omron HBF , and a DEXA instrument GE Lunar Prodigy. The study was approved by the Institutional Review Board of Seoul St. For the approval of the review board, our bioelectrical impedance analyzer was registered as a broadcasting and communication equipment MSIP-REM-SEC-SAIT-MyLean by the Ministry of Science, ICT and Future Planning MSIP , Republic of Korea. Written informed consent was obtained from each volunteer before the clinical test. To undergo the test, participants changed into a light gown in order to control the weight of clothes. All metal items were removed from the participants to ensure accuracy of measurement. Then anthropometric measurement was conducted by a skilled nurse. After anthropometric measurement, body impedance and body composition data were measured using the whole-body composition analyzer and the upper-body portable body fat analyzer. Next, the DEXA instrument was used to measure the reference body composition. Finally, our wrist-wearable device was used to measure body impedance. Statistical analysis was performed after data acquisition. The accuracy of each device was compared to that of others. Our study explored a novel method that uses considerably small electrodes that can be adapted into small devices, such as a wristwatch. Figure 7 shows the calculated contact resistance distribution of the study participants. While the average value was Ω, it is notable that the maximum value was as high as Ω. Figure 8 a shows the impedance correlation between our device and the whole-body composition analyzer. The coefficient of determination R 2 of impedance was 0. This result shows that there is a strong correlation for impedance measurements between the wrist-wearable bioelectrical impedance analyzer and the whole-body bioelectrical impedance analyzer, and the proposed contact resistance compensation method improves the correlation coefficient effectively. a Impedance correlation with contact resistance compensation blue dots and without contact resistance compensation orange dots. DEXA dual-energy X-ray absorptiometry. Figure 8 b shows the correlation of percentage body fat measurement between our wrist-wearable bioelectrical impedance analyzer and the reference instrument DEXA , from which it can be seen that R is 0. The SEE was estimated to be 3. It can be seen that the errors between the two instruments are randomly distributed without any skewed tendency and Table 3 shows the comparison of accuracy in measurement of percentage body fat by the whole-body composition analyzer, the upper-body portable body fat analyzer, and our wrist-wearable bioelectrical impedance analyzer. We developed a novel wrist-wearable bioelectrical impedance analyzer with a contact resistance compensation function such that bioelectrical impedance can be accurately estimated even with considerably small sizes of electrodes outer electrodes: 68 mm 2 ; inner electrodes: mm 2. The correlation coefficient and the SEE of percentage body fat relative to the DEXA instrument were estimated to be 0. Considering that the measurement time of our wrist-wearable BIA device was only 7 s and could be reduced further, this sensor technology provides a new possibility for a wearable bioelectrical impedance analyzer with more miniature electrodes toward daily obesity management. Kyle, U. et al. Bioelectrical impedance analysis—part I: review of principles and methods. Article Google Scholar. Bioelectrical impedance analysis—part II: utilization in clinical practice. Kushner, R. Bioelectrical impedance analysis: a review of principles and applications. Article MathSciNet CAS Google Scholar. Single prediction equation for bioelectrical impedance analysis in adults aged 20—94 years. CAS Google Scholar. Heitmann, B. Evaluation of body fat estimated from body mass index, skinfolds and impedance: A comparative study. Chertow, G. Development of a population-specific regression equation to estimate total body water in hemodialysis patients. Kidney Int. Article CAS Google Scholar. Ramel, A. Regional and total body bioelectrical impedance analysis compared with DXA in Icelandic elderly. By doing so, the impedance in the limbs and torso were measured separately, yielding highly accurate results without using empirical data based on factors like age, gender, ethnicity, athleticism, and body shape. Thus, the InBody DSM-MFBIA body composition analyzer is a precision medical device. Many BIA products today provide segmental measures of muscle and fat mass, but most of these products are still unable to take segmental impedance measurements, particularly in the torso. The InBody measure each segment separately and shows the impedance values of all five cylinders of the body at each frequency in the Impedance Section of the InBody Result Sheet. InBody uses multiple currents at varying frequencies to provide precise body water analysis. When measuring impedance with electrodes, contact resistance occurs. InBody accounts for contact resistance with strategically placed electrodes to ensure that measurements are accurate and reproducible. InBody measures your impedance independently, so your results are not affected by your age, gender, ethnicity, athleticism, or body shape. BIA Tech Problem The ability to distinguish between extracellular and total body water is important to identify fluid imbalances related to acute inflammation or edema. Many BIA devices use only one frequency at 50 kHz to measure impedance. As a result, patients with increased extracellular water may be misidentified as being healthy. InBody uses a combination of low and high frequencies to determine extracellular, intracellular, and total body water. The use of multiple frequencies allows InBody devices to achieve a high level of precision. Medical practitioners can use InBody for measurements of body composition and fluid status. Total body water TBW is stored throughout the body and can be separated into 2 compartments:. Early BIA devices used a single 50 kHz frequency to calculate TBW. Therefore, ICW was estimated proportionally based on the ECW. This estimation was used to determine TBW, lean mass, and fat mass. The estimation of intracellular water was based on the assumption that the ratio of ICW to ECW in healthy adults is about However, individuals with body compositions that differ from conventionally healthy adults, such as elderly, obese or chronic disease patients, often have a higher ratio of ECW. Thus, in these patient populations, relying on the ICW:ECW ratio could result in significant error. InBody uses multiple frequencies ranging from 1 kHz to 1 MHz to provide precision body water analysis. Electrical currents interact differently with the cells at different frequencies, which allows the InBody to quantify the different fluid compartments. Low frequencies are better suited for measuring ECW, while high frequencies can pass through cell membranes to measure ICW and therefore TBW. An accurate measure of TBW and the ability to analyze ICW versus ECW allows for a deeper analysis of individual body composition. Compartmental water measures can be used to properly quantify and identify changes in fluid balance to reflect nutritional status and fitness progress. If the starting measurement position changes, the length of the measured cylinder also changes. This directly impacts impedance and introduces error. When the human body comes in contact with an electrode, resistance occurs. To accurately measure the resistance in the human body, it is important to control the measurement location. These designs can cause measurements to start in the palm, which has a high impedance and can cause inaccuracies, or lead to inconsistent measurement starting points, reducing the reliability of results. The anatomical design of the hand electrode creates a simple holding position that is easy to reproduce. Utilizing the anatomical characteristics of the human body, when an InBody user grasps the hand grip, current flows from the palm electrode and the electrical energy, or voltage, is initiated at the thumb electrode. When current and voltage overlap, impedance can be measured. By separating current and voltage into the hand and foot electrodes, the point of overlap can be controlled to isolate the five cylinders of the body limbs and torso and consistently start at the same location on the wrists and ankles for reproducible results. With this design, the point of measure stays the same even when the user changes the holding position of the hand electrode or the contact points on the hands and feet. Traditional BIA views the human body as one cylinder. However, the torso of the body needs to be measured separately because its short length and large cross-sectional area mean that even a small measurement mistake can lead to substantial error. Direct segmental measurement bioelectrical impedance analysis regards the human body as five cylinders: left arm, right arm, torso, left leg, and right leg. InBody independently measures each cylinder to provide accurate measurements for the entire body. Traditional BIA systems viewed the human body as a single cylinder, using whole-body impedance to determine total body water. One of the biggest problems with the single cylinder method is the lack of a separate torso measurement. The torso has the shortest length and highest cross-sectional area, which results in a very low impedance typically ohms. Therefore, small errors in torso impedance have significant impact on body composition results. With whole-body impedance measurement, the torso impedance is not observed separately and thus, changes in torso impedance cannot be quantified. Because of the large amount of lean mass in the torso, small variability in impedance measures can have a drastic effect on how the results are interpreted. Differences and percentages may vary based on the individual. Some BIA devices avoid the torso measurement entirely. For example, with many BIA scales, only the impedance of your legs and a small part of your torso are measured. Similarly, with handheld BIA devices, only the impedance of your arms and a small portion of your torso are measured. With this design, the rest of the body must be estimated. In many bioimpedance technologies today , empirical equations are incorporated to compensate for technological flaws, including the lack of torso impedance due to whole-body impedance measurement , single frequency measurements which are unable to differentiate between water compartments , and lack of reproducibility from electrode placement or positioning. InBody measures body composition without relying on empirical assumptions based on age, gender, ethnicity, or body shape, producing accurate and precise results that are validated to gold standard methods. Put simply, InBody provides individualized feedback for better tracking of progress to help you achieve your goals. These equations help compensate for the lack of torso impedance measurement and ability to differentiate between body water compartments by plugging in empirical data based on factors, such as age, gender, and ethnicity. For example, these equations may take into consideration that muscle mass generally decreases with age and that males tend to have more muscle mass than females. This expectation is then reflected in the results. Therefore, the problem with relying heavily on empirical estimations is that your results are predetermined, regardless of your actual body composition. Testing on the InBody will give a user the same body composition measurements whether that user tests as a male or female because the InBody does not use empirical estimations based on factors of age, gender, ethnicity, athleticism, or body shape in its measurements. |
| Access options | This suggests that BIA may provide data that is not sufficiently accurate for the determination of individual body composition. The validity of using BIA to measure changes over time A further consideration for the use of BIA is the validity of its use in measuring changes in fat mass and fat-free mass over time, as this may indicate the efficacy of a nutritional or training intervention looking to manipulate body composition. To revisit the study by Ritz et al. Fat mass was underestimated by 1. Individual error rates were greater than at baseline, with BIA underestimating fat mass by 7. A further study on obese populations [13] showed individual disagreement in body fat measurement between BIA and the four-compartment model was high. Individual measures of body fat ranged from There are a limited amount of comparisons between BIA and the reference four-compartment model in athletic populations. There is disagreement amongst the limited research available, with only one study suggesting that BIA is suitable for assessing body composition in athletes [15], whereas other research suggests that body fat estimates are much higher in athletes when using the BIA method [16]. The discrepancies between the studies may be due to various issues including differences in methodology, equations, and athletic population. There are currently no BIA equations for athletes that have been derived from the criterion four-compartment method fat mass, total body water, bone mineral mass, residual mass. This makes the application of BIA in this population difficult, as athletes are likely to possess substantially different quantities of fat and fat-free mass when compared to the general population or diseased populations that current equations are based on. The reliability of BIA The reliability of BIA the reproducibility of the observed value when the measurement is repeated is also important to determine single-measurement precision, as well as the ability to track changes over time. A plethora of research has indicated the importance — and potentially the inability — of standardising BIA measures to sufficiently account for various confounders. The mean coefficient of variation for within-day, intra-individual measurements, has ranged from 0. Standard measurement conditions may vary depending on the machine type e. hand-to-hand, leg-to-leg, supine vs. standing, etc. Other factors which may impact the BIA measurement and should therefore also be standardised are [16]:. The standardisation of hydration status is clearly of importance for BIA, as the method is reliant on estimations of total body water to ascertain fat-free mass. For female athletes, difference in hydration status during menses may significantly alter impedance [17] and should be a consideration when assessing female athletes with BIA. Saunders et al. hyperhydrated or hypohydrated , indicating that even small changes in fluid balance that occur with endurance training may be interpreted as a change in body fat content. In addition, eating and strenuous exercise hours prior to assessment have also previously been shown to decrease impedance; ultimately affecting the accuracy of the measurement [19]. The need to standardise eating, exercise, and both acute and chronic hydration changes are clearly important to provide valid body composition estimations. As mentioned previously, there are several issues with BIA measurement that may limit its use in an applied setting. Methodological limitations of BIA may affect the ability of the method to accurately determine body composition. The primary issues with BIA are:. Sensor Placement One such limitation is the placement of the sensors, and their ability to give readings of total body composition. As electrical current follows the path of least resistance, some scales may send current through the lower body only, missing the upper body entirely. Similarly, hand-held instruments may only assess the body composition of the upper extremities. As females typically have a higher proportion of adipose tissue in the gluteal-femoral region [20], it is possible that this would not be represented using hand-held BIA devices. Hand-to-foot BIA devices, however, may allow for greater accuracy, as the current is sent from the upper body to the lower body, and is less likely to be influenced by the distribution of body fat. Hydration and Glycogen Levels Regardless, all devices are still subject to the same limitations that other BIA devices are. Deurenberg et al. They speculated that changes in glycogen stores, and the loss of water bound to glycogen molecules, may affect BIA estimates of fat-free mass. In athletic populations, where varying glycogen stores are likely throughout a training week, it is likely that this will lead to some variation in the detection of change in fat-free mass in athletes as glycogen is likely to be affected by both diet, as well as the intensity, duration, and modality of previous training sessions — even with protocol standardisation. Effect of incorrect measures in the applied setting An important consideration when assessing the individual variation of BIA is the potential consequences that an incorrect reading can have. This can have wide-ranging implications, from assessing the efficacy of previous dietary and training interventions to making decisions on the correct interventions moving forward. For example, an athlete may be singled out for interventions to reduce their body fat based on their BIA assessment and normative values, yet other methods may suggest that their body composition is optimal. The primary area for future research in this area is clearly the need for validated BIA equations for athletes in a range of sports and with varying body composition. It is important that these equations are validated using a total-body, water-based, four-compartment method, in an attempt to minimise the measurement error that is found when equations are based on the two-compartment model; such as hydrostatic weighing. As such, the following areas of research are needed to expand current knowledge on this topic:. To conclude, it is likely that BIA is not a suitable body composition assessment method for athletic populations. The lack of a validated equation for this population, combined with the large individual error reported in overweight and obese populations, suggests that BIA does not provide accurate body composition data for both single-measure and repeated measures. Learn how to improve your athletes' agility. This free course also includes a practical coaching guide to help you design and deliver your own fun and engaging agility sessions. Charlie has an MSc in Sport and Exercise Nutrition from Loughborough University. He has previously supported athletes in a variety of sports including canoeing, boxing, cricket, rugby league, Olympic weightlifting and strongwoman. Learn from a world-class coach how you can improve your athletes' agility. This course also includes a practical coaching guide to help you to design and deliver your own fun and engaging agility sessions. Our mission is to improve the performance of athletes and teams around the world by simplifying sports science and making it practical. Pricing FAQs Reviews Free trial. Blog Newsletter Community Podcast Tools. About us Contact us Join our team Privacy policy Terms of use Terms and conditions Disclaimer. Bioelectrical Impedance Analysis BIA Bioelectrical Impedance Analysis BIA can estimate body composition e. Contents of Article Summary What is Bioelectrical Impedance Analysis? Types of Bioelectrical Impedance Analysis What are the Bioelectrical Impedance Analysis equations? Is Bioelectrical Impedance Analysis valid and reliable? Are there issues with Bioelectrical Impedance Analysis? Is future research needed with Bioelectrical Impedance Analysis? Conclusion References About the Author. Figure 1. The difference in bioelectrical conductivity between muscle and fat. References Buccholz, C. Bartok and D. Franssen, E. Rutten, M. Groenen, L. Vanfleteren, E. Wouters and M. Schlager, R. Stollberger, R. Felsberger, H. Hutten and H. Bergsma-Kadijk, B. Baumeister and P. Sun, C. Chumlea, S. Heymsfield , H. Lukaski, D. Schoeller, K. Friedl, R. Kuczmarski, K. Flegal, C. Johnson and V. French, G. Martin, B. Younghusband, R. Green, Y. Xie, M. Matthews, J. Barron, D. Fitzpatrick, W. Gulliver and H. Salle, M. Audran and V. van Marken Lichtenbelt, F. Hartgens, N. Vollaard, S. Ebbing and H. Jebb, T. Cole, D. Doman, P. Keep in mind that they are not likely to be very accurate but you can use them to track changes over time. Using another method of tracking your body composition can help you get a better picture of your actual measurements. It's also wise to understand that there is more to health than your body fat percentage or weight, and these scales are only a tool, not a reflection of your general wellness. Gagnon C, Ménard J, Bourbonnais A, et al. Comparison of Foot-to-Foot and Hand-to-Foot Bioelectrical Impedance Methods in a Population with a Wide Range of Body Mass Indices. Metab Syndr Relat Disord. Demura S, Sato S. Comparisons of accuracy of estimating percent body fat by four bioelectrical impedance devices with different frequency and induction system of electrical current. J Sports Med Phys Fitness. Bioelectrical impedance analysis BIA : A proposal for standardization of the classical method in adults. Journal of Physics Conference Series. Androutsos O, Gerasimidis K, Karanikolou A, Reilly JJ, Edwards CA. Impact of eating and drinking on body composition measurements by bioelectrical impedance. J Hum Nutr Diet. Blue MNM, Tinsley GM, Ryan ED, Smith-Ryan AE. Validity of body-composition methods across racial and ethnic populations. Advances in Nutrition. By Malia Frey, M. Use limited data to select advertising. Create profiles for personalised advertising. Use profiles to select personalised advertising. Create profiles to personalise content. Use profiles to select personalised content. Measure advertising performance. Measure content performance. Understand audiences through statistics or combinations of data from different sources. Develop and improve services. Use limited data to select content. List of Partners vendors. Weight Management. Malia Frey, M. Learn about our editorial process. Learn more. Medical Reviewers confirm the content is thorough and accurate, reflecting the latest evidence-based research. Content is reviewed before publication and upon substantial updates. Medically reviewed by Anisha Shah, MD. Learn about our Medical Review Board. Fact checkers review articles for factual accuracy, relevance, and timeliness. We rely on the most current and reputable sources, which are cited in the text and listed at the bottom of each article. Content is fact checked after it has been edited and before publication. Fact checked by Adah Chung. Table of Contents View All. Table of Contents. BIA Definition. Types of BIA Devices. Making a Purchase. Fat-Free Body Mass Benefits. Is BIA Safe? The 14 Best Bathroom Scales of , Tested and Reviewed. The 8 Best Body Fat Monitors to Help You Track Progress, Tested and Reviewed. The 14 Best Smart Scales, Tested and Recommended by Our Experts. Verywell Fit uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. |
| What is bioelectrical impedance analysis? | Different tissues in your body allow the electrical current to travel at individual speeds. Fat is more resistant than muscle or water, so the higher the resistance, the higher the body fat percentage calculation is likely to be. Most scales measure an estimate of your total fat, muscle, water, and bone in weight and percentage. Based on that rate, a calculation is used to estimate fat-free mass. The device then uses other data such as your height, gender, and weight measurements to determine your body fat percentage. There are different types of BIA devices, but each requires two contact points. On a handheld device, the two points are your two hands called hand-hand BIA. The two contact points on a typical BIA scale are your two feet called foot-foot bioelectrical impedance analysis. This means that when you use the device, you place each foot on a pad, and the current travels through your body between your feet. There are also hand-to-foot BIA devices, as well. Many of the newer models of BIA scales link with a smartphone app so you can track your progress over time. The price of your BIA scale will depend on how sophisticated the product is. Some scales use more than one frequency and more advanced algorithms to provide a result. And some offer segmental fat analysis, meaning you can get body fat measurements for each leg, arm, and belly. Some experts say that segmental fat analysis using hand-foot BIA is more accurate because hand-hand devices primarily measure the upper body, while foot-foot scales primarily measure the lower body. Bioelectrical impedance analysis devices are considered safe for most people. However, BIA should not be used by anyone with an electronic medical implant, such as a heart pacemaker or an implantable cardioverter defibrillator ICD. Also, most device makers recommend that pregnant people not use the products. Some studies showed that bioelectrical impedance analysis is a reasonably accurate method for estimating body fat. But these research studies generally do not test the scales you find in the store. Experts generally agree that the accuracy of the measurement depends, in part, on the quality of the device. In addition, other factors may affect a reading when you use a BIA scale. Some researchers also say that ethnicity can affect the accuracy of BIA measurements. Overall, studies show that this method is not very accurate although it may be able to track change over time, your results are unlikely to reflect your actual body composition. Even if you get an accurate reading on a bioimpedance scale, the number represents an estimate of your total body fat percentage. Bioelectrical impedance analysis does not accurately measure your total body fat. Most scales also cannot tell you where fat is located on your body. Even though many factors can affect your reading accuracy, a regular BIA scale can show you changes in your body fat over time. The actual number may not be perfect, but you can still track changes to your body composition. Because many BIA scales offer several features for a reasonable cost and are a quick and easy way to estimate body fat percent, body fat scales that use bioelectrical impedance analysis are a worthwhile investment for consumers who are curious about their body composition. Keep in mind that they are not likely to be very accurate but you can use them to track changes over time. Using another method of tracking your body composition can help you get a better picture of your actual measurements. It's also wise to understand that there is more to health than your body fat percentage or weight, and these scales are only a tool, not a reflection of your general wellness. Gagnon C, Ménard J, Bourbonnais A, et al. Comparison of Foot-to-Foot and Hand-to-Foot Bioelectrical Impedance Methods in a Population with a Wide Range of Body Mass Indices. Here's a painless and easy way to estimate body fat. In addition to the bathroom scale, how our clothes fit, and how we feel day to day, body fat measurements provide us with a bit more information about where we stand with our health and fitness goals. Simply put, getting your body composition estimated provides information about how much of your body is fat and not fat muscle, bone and organs. You are likely aware that too much body fat is a reason for concern. Carrying too much fat especially around the middle increases the chance of developing conditions such as type 2 diabetes, heart disease, hypertension, and joint disease. One method of estimating body fat is through bioelectrical impedance BIA. It is a painless and easily accessible procedure that is safe for most individuals. Those with a pacemaker or women who are pregnant should avoid the test. The test works by passing a low level imperceivable current through the body. The current moves faster through fat-free mass, due to its higher water content, than fat mass. The resistance that the current encounters is measured and then plugged into a mathematical equation to come up with total body water, fat-free mass, and body fat. Digital Magazine: Thematic Take monthly. I consent to Verdict Media Limited collecting my details provided via this form in accordance with Privacy Policy. View all newsletters from across the GlobalData Media network. Share this article Copy Link Share on X Share on Linkedin Share on Facebook. Credit: Tanita. Go deeper with GlobalData. Premium Insights The gold standard of business intelligence. BIA NV SA Tanita Corp View all. How well do you really know your competitors? View profiles in store. Company Profile — free sample Thank you! Your download email will arrive shortly. Not ready to buy yet? Download a free sample We are confident about the unique quality of our Company Profiles. However, we want you to make the most beneficial decision for your business, so we offer a free sample that you can download by submitting the below form By GlobalData Submit. Tick here to opt out of curated industry news, reports, and event updates from Medical Device Network. I consent to GlobalData UK Limited collecting my details provided via this form in accordance with the privacy policy. |
Video
How To Measure Body Fat Percentage At Home Accurately Bio-electrical Iinterpretation Analysis BIA is a method used to impedahce health by looking Adaptogen adrenal health body composition. It measures body Psychological strategies for healthy eating nody relation to lean body mass and is BIA body impedance interpretation to be more accurate than BMI testing. A normal balance of body fat and muscle is associated with good health and longevity so BIA tests can aid clinicians in helping their patients change their diet and lifestyles accordingly. All Tanita body composition monitors are said to use advanced BIA technology. Find out more. Charlotte Edwards: Can you explain the purpose of BMI testing and its benefits?
0 thoughts on “BIA body impedance interpretation”