Video
How To Increase Metabolism: Intermittent Fasting vs Calorie RestrictionCaloric restriction and fat metabolism -
Severely restricting your calories can decrease your metabolism and cause you to lose muscle mass. This makes it more difficult to maintain your weight loss in the long term.
Regularly eating fewer calories than your body requires can cause fatigue and make it more challenging for you to meet your daily nutrient needs.
For instance, calorie-restricted diets may not provide sufficient amounts of iron, folate or vitamin B This can lead to anemia and extreme fatigue 16 , 17 , In addition, the number of carbs you eat may play a role in fatigue.
Some studies suggest that calorie-restricted diets with low amounts of carbs may cause feelings of fatigue in some individuals 19 , 20 , 21 , However, other studies find that low-carb diets reduce fatigue. Therefore, this effect may depend on the individual 23 , To prevent fatigue and nutrient deficiencies, avoid overly restricting your calories and ensure you eat a variety of whole, minimally processed foods.
Restricting calories too severely can lead to fatigue. Maintaining this calorie restriction for too long can also lead to nutrient deficiencies. Restricting calories too dramatically can negatively affect fertility. This is especially true for women, as the ability to ovulate depends on hormone levels.
More specifically, an increase in estrogen and luteinizing hormone LH levels is needed in order for ovulation to occur 31 , An insufficient calorie intake may also reduce estrogen levels, which is thought to have lasting negative effects on bone and heart health 34 , 35 , Signs of reduced fertility may include irregular menstrual cycles or a lack of them.
However, subtle menstrual disturbances may not have any symptoms, so they may require a more thorough medical examination to be diagnosed 37 , Overly restricting calories may potentially reduce fertility, especially in women. More studies are needed to determine the effects of calorie restriction in men.
Consuming too few calories can weaken your bones. Low levels of these two reproductive hormones are thought to reduce bone formation and increase bone breakdown, resulting in weaker bones 40 , 41 , 42 , In addition, calorie restriction — especially when combined with physical exercise — can increase stress hormone levels.
This may also lead to bone loss Bone loss is especially troublesome because it is often irreversible and increases the risk of fractures 45 , Restricting calories may disturb hormone levels, which may result in weaker bones and an increased risk of fractures.
For instance, one study compared athletes in disciplines that put a strong emphasis on body leanness, such as boxing, gymnastics or diving, to those in disciplines less focused on body weight.
The researchers reported that athletes in disciplines that required leanness made more frequent attempts to lose weight and were almost twice as likely to have been sick in the previous three months In another study, taekwondo athletes who were dieting to reduce their body weight in the week before a competition experienced reduced immunity and an increased risk of infection The effects of calorie restriction in non-exercising individuals are less clear, and more research is needed before strong conclusions can be made Calorie restriction, especially when combined with strenuous physical activity, may lower your immune defenses.
Calorie needs vary from person to person because they depend on factors such as age, sex, height, current weight and physical activity level.
There are various ways to estimate your own calorie needs. The easiest method consists of three simple steps:. In addition, make sure you record what you eat in an online food journal like Cronometer , at least in the beginning of your weight loss process. Tracking your diet will help you ensure that you continue to reach your daily recommended nutrient intakes.
When it comes to long-term weight loss, patience is key. Only one study [ 34 ] had a low risk of bias, and the other seven [ 27 , 31 , 32 , 33 , 35 , 36 ] had some concerns. The risk of bias was some concerns in two articles [ 32 , 33 ] for lack of information about the randomization process, in five studies [ 27 , 31 , 33 , 35 , 36 ] for deviations from intended interventions, and in one publication [ 36 ] for missing outcome data.
One crossover design research [ 30 ] was assessed by a version of ROB2 for crossover trials. The trial had some concerns about bias, given the absence of a randomization process, deviations from intended interventions and selection of the reported result Fig.
Eight studies [ 27 , 30 , 31 , 32 , 33 , 34 , 35 , 36 ] with participants reported weight loss as an outcome. Despite the removal of a study [ 30 ] with the highest weight Although the asymmetric funnel plot Fig.
The changes in fat mass were recorded in five studies individuals [ 27 , 33 , 34 , 35 , 36 ]. Six studies [ 30 , 31 , 33 , 34 , 35 , 36 ] involving participants showed changes in WC from baseline to endpoint. The heterogeneity decreased when the study by Kahleova et al.
Four studies [ 31 , 33 , 34 , 35 , 36 ] with individuals focused on the effect on blood pressure. Sensitivity analysis unveiled a degraded heterogeneity without changes in statistical significance after the removal of the study by Lin et al.
Six studies [ 30 , 32 , 33 , 34 , 35 , 36 ] with participants recorded changes in fasting glucose concentration with TRE plus CR. For insulin, the pooled analysis of four studies [ 30 , 33 , 34 , 36 ] with individuals suggested no differences between the intervention and control groups WMD: 0.
Moreover, HOMA-IR and HOMA-β were investigated in four studies [ 33 , 34 , 35 , 36 ] participants and two articles [ 34 , 36 ] participants respectively, but no statistically significant differences were found in either of the two outcomes WMD: 0. A nonsignificant difference was observed in the HOMA-IR after the sequential deletion of trials without a marked change in heterogeneity.
Changes in lipid profiles were reported by six studies [ 27 , 30 , 33 , 34 , 35 , 36 ], with participants reported. The results showed that TRE plus CR had no beneficial effects of TRE plus CR on TC WMD: 1.
However, no significant effects were found on weight loss and fat mass loss in the broader TRE with CR and dTRE with CR groups. Moreover, WC reduced nonsignificantly in all three groups. Otherwise, no significant difference was found in terms of fat mass.
The study by Kahleova et al. Subgroup analysis was conducted based on different durations to investigate the long-term effects of combined TRE and CR. Consistent fat mass and WC outcomes were observed with the body weight Table 2.
Table S 1 presents the GRADE assessment results. Among the 12 outcomes analyzed, weight loss, SBP, glucose, TC, TG, and LDL were classified as low quality, and the other six outcomes fat mass, WC, DBP, insulin, HOMA-IR, HOMA-β were graded as very low.
This systematic review and meta-analysis of 8 trials involving participants revealed that participants who follow a combined TRE and CR regimen efficiently lose body weight and substantially reduce their WC and fat mass. However, no changes were observed in the other outcomes, such as SBP, DBP, fasting glucose, insulin, HOMA-IR, HOMA-β, and lipid profile values TC, TG, and LDL.
One study presented a low risk of bias, whereas seven studies raised some concerns. The GRADE evaluation rated six of the twelve outcomes from the current study as low quality, and the remaining six were classified as very low quality.
Several lines of evidence consider the potential role of rhythmic creatine-mediated thermogenesis in the metabolic advantages of time-restricted meals [ 40 ]. Furthermore, mounting proof validates that TRE promotes a fuel switch from glucose to fatty acids [ 41 ], which is associated with enhanced expression of oxidative metabolic genes in adipose tissue, improved energy consumption, and prevention of metabolic diseases without modification of food intake.
These mechanisms can be responsible for the findings observed in the present study; that is, participants who experienced TRE with CR exhibited excellent body composition improvement benefits compared with individuals who underwent CR alone.
Notably, in the present meta-analysis, the heterogeneity of WC disappeared when the study by Kahleova et al. Subgroup analysis revealed increased body weight loss and fat mass reduction tendencies in participants with eTRE plus CR intervention compared with CR alone, but no body weight or fat mass benefits was found in the subgroups of dTRE plus CR, broader TRE plus CR.
The analysis results should be interpreted cautiously because dTRE was only exploited in one study [ 36 ]. The subgroup analysis results for WC based on intervention measures revealed no significant difference between groups, indicating that body weight but not WC is the most sensitive parameter.
Contrary to previous meta-analyses [ 23 ], participants with obesity in the present study benefited from the combination of TRE and CR, and they showed significant body weight reduction and body composition improvement. Such a discrepancy may be explained in part by the scarce studies in the meta-analysis by Liu et al.
Subgroup analysis of duration showed that long-term intervention by TRE plus CR is more effective in weight loss and body composition improvement than its short-term counterpart. Although the long-term group showed a significant effect, two of the four included studies [ 31 , 35 ] with a month follow-up period exhibited no changes in body weight, fat mass, or WC.
Future long-term trials with large subject populations will be necessary to further determine the long-term benefits of TRE plus CR on body composition [ 44 ]. However, the WC outcome of the group may need to be more reliable, given the small number of included studies. Moreover, the analysis results of studies supported that TRE combined with CR is more effective in reducing body weight when conducted in developed countries Europe and North America as opposed to developing countries Asia or North America , consistent with the epidemiologic research of obesity prevalence in developed countries [ 45 ].
This phenomenon may be associated with the high popularity of health education about obesity and its complications in these areas.
The subgroup analysis results based on regions showed no changes in WC and fat mass, except for the Europe subgroup of one study [ 30 ], where a significant decrease in WC was observed. The TRE regimen did not significantly benefit blood pressure compared with the CR regimens.
The sensitivity analysis of DBP detected a moderate heterogeneity when the study by Lin et al. Nevertheless, a 5-week randomized crossover trial with positive results proposed that in comparison with the controlled schedule, eTRE considerably reduced the morning levels of SBP and DBP [ 47 ].
The controversy is possibly attributed to the difference in insulin and a statement that the reduction in insulin levels can improve blood pressure [ 48 ], as well as the fact that we noticed no differences in insulin levels in the study by Lowe et al.
Furthermore, although the analysis revealed a significantly reduced weight, according to the guide, the change in body weight was relatively mild to induce a significant difference in blood pressure [ 49 ].
The current meta-analysis showed that TRE did not provide extra benefits on glycemic and lipid profiles compared with daily CR.
Sensitivity analysis showed a similar result in glucose levels between groups when the study causing heterogeneity was excluded. As mentioned in the current review, isocaloric TRE, particularly in individuals with prediabetes, improves fasting insulin and insulin resistance independent of weight loss [ 50 ], but with a controversy on the glucose profile in participants scheduled for ad libitum TRE who do not have diabetes [ 51 , 52 , 53 , 54 ].
The result provides evidence against the positive conclusion of a previous meta-analysis involving 19 studies, which showed that TRE could lower fasting blood glucose, HOMA-IR, and lipid spectrum of TG, TC, and LDL-C in overweight individuals [ 24 ].
Diverse population characteristics in the included studies may explain the conflicting conclusion in the present research and that of Moon et al. But it is noteworthy that among the latter, neither significant lipid nor glucose profile changes were observed in the subgroup analysis based on healthy subjects, and the sensitivity analysis did not turn up any outline studies, indicating some skepticism about the robustness of the findings.
The blood lipid outcomes in the present meta-analysis contradict the hypothesis put forward in a review that TRE may contribute to favorable changes in some aspects of the lipid profile concurrent with a simultaneous reduction in body weight, despite insufficient evidence [ 55 ].
A possible explanation for this may be that the studies included were intended to concentrate on the reduction effect of TRE combined with CR on body weight rather than improving blood lipids.
Consequently, the slightly different inclusion criteria resulted in an imbalanced baseline serum lipid level of participants in several studies that excluded participants with a history of cardiovascular disease or diabetes [ 27 , 36 ]. Two trials did not recruit individuals taking medications for blood sugar or blood lipids [ 30 , 33 ].
More well-designed large sample studies are desiderated to ensure the scientific, objective, and reliable conclusions of the trials in future clinical research to identify the effectiveness of TRE plus CR on glucose and lipid profiles. We acknowledge that the present study has some limitations.
The main limitation of the present meta-analysis was the low or very low quality evidence of study outcomes classified by the GRADE tool, which was primarily attributed to the risk of bias that the nature of behavioral intervention by a fixed ratio of fasting and eating periods, preventing it from blinding the participants.
Nevertheless, the study results were all objective measures that were slightly affected by subjective dimension and influenced the outcomes mildly regardless of whether the participants were informed of allocation results.
Second, several results displayed varied heterogeneity because of the TRE subtype, various fasting and eating duration ratios, and different baseline body weights. Subgroup analyses were carried out to investigate the combined effects of TRE and CR on specific subgroups.
Meanwhile, sensitivity analysis was also conducted to determine the source of heterogeneity in outcomes with substantial and high heterogeneity. Third, the representativeness of participants was impaired by rigorous inclusion criteria, with several trials eliminating individuals under treatment for diabetes and cardiovascular disease.
As a result, the findings cannot be used to generalize clinical participants, especially those with chronic diseases receiving treatment. The quality of evidence and dependability of the findings are expected to increase in future long-term studies with representativeness and a large sample of participants.
Our systematic review and meta-analysis demonstrated that calorie-intake restriction with time restriction could significantly decrease body weight, fat mass, and WC. Although the combination of TRE and CR did not benefit cardiometabolic risk factors blood pressure, glucose, or lipid profile , the results should be interpreted with caution because of the specificity of the included population.
The present study results highlight the need for well-designed, large-sample, and long-term studies to improve the evidence quality for the effect of TRE combined with CR on participants with chronic cardiovascular disease and diabetes.
Because this is a meta-analysis, all of the data included in this study can be found in the included references. GBD Obesity Collaborators, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, et al. Health effects of overweight and obesity in countries over 25 years. Engl J Med ;— Blüher M.
Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. Article PubMed Google Scholar. World Obesity Atlas Accessed 2 Jan Das M, Webster NJG. Obesity, cancer risk, and time-restricted eating.
Cancer Metastasis Rev. Article PubMed PubMed Central Google Scholar. Bray GA, Frühbeck G, Ryan DH, Wilding JP. Management of obesity. Hoddy KK, Marlatt KL, Çetinkaya H, Ravussin E, et al. Intermittent Fasting and Metabolic Health: From Religious Fast to Time-Restricted Feeding.
Article Google Scholar. Varady KA, Cienfuegos S, Ezpeleta M, Gabel K. Clinical application of intermittent fasting for weight loss: progress and future directions. Schübel R, Nattenmüller J, Sookthai D, Nonnenmacher T, Graf ME, Riedl L, et al. Effects of intermittent and continuous calorie restriction on body weight and metabolism over 50 wk: a randomized controlled trial.
Am J Clin Nutr. Antoni R, Johnston KL, Steele C, Carter D, Robertson MD, Capehorn MS. Efficacy of an intermittent energy restriction diet in a primary care setting.
Eur J Nutr. Article CAS Google Scholar. Davoodi SH, Ajami M, Ayatollahi SA, Dowlatshahi K, Javedan G, Pazoki-Toroudi HR. Calorie shifting diet versus calorie restriction diet: a comparative clinical trial study.
Int J PrevMed. Google Scholar. Cai H, Qin YL, Shi ZY, Chen JH, Zeng MJ, Zhou W, et al. Effects of alternate-day fasting on body weight and dyslipidaemia in patients with non-alcoholic fatty liver disease: a randomised controlled trial.
BMC Gastroenterol. Article CAS PubMed Central Google Scholar. Patterson RE, Sears DD. Metabolic effects of intermittent fasting.
Annu Rev Nutr. Article CAS PubMed Google Scholar. Reinke H, Asher G. Circadian Clock Control of Liver Metabolic Functions. Mukherji A, Kobiita A, Damara M, Misra N, Meziane H, Champy MF, et al. Shifting eating to the circadian rest phase misaligns the peripheral clocks with the master SCN clock and leads to a metabolic syndrome.
Proc Natl Acad Sci USA. Article CAS PubMed PubMed Central Google Scholar. Rothschild J, Hoddy KK, Jambazian P, Varady KA. Time-restricted feeding and risk of metabolic disease: a review of human and animal studies.
Nutr Rev. Liu Z, Dai X, Zhang H, Shi R, Hui Y, Jin X, et al. Gut microbiota mediates intermittent-fasting alleviation of diabetes-induced cognitive impairment. Nat Commun. Xie Z, Sun Y, Ye Y, Hu D, Zhang H, He Z, et al.
Randomized controlled trial for time-restricted eating in healthy volunteers without obesity. Phillips NE, Mareschal J, Schwab N, Manoogian ENC, Borloz S, Ostinelli G, et al. The Effects of Time-Restricted Eating versus Standard Dietary Advice on Weight, Metabolic Health and the Consumption of Processed Food: A Pragmatic Randomised Controlled Trial in Community-Based Adults.
Moro T, Tinsley G, Pacelli FQ, Marcolin G, Bianco A, Paoli A. Twelve Months of Time-restricted Eating and Resistance Training Improves Inflammatory Markers and Cardiometabolic Risk Factors. Med Sci Sports Exerc. Kotarsky CJ, Johnson NR, Mahoney SJ, Mitchell SL, Schimek RL, Stastny SN, et al.
Time-restricted eating and concurrent exercise training reduces fat mass and increases lean mass in overweight and obese adults. Physiol Rep.
Allaf M, Elghazaly H, Mohamed OG, Fareen MFK, Zaman S, Salmasi AM, et al. Intermittent fasting for the prevention of cardiovascular disease. Cochrane Database Syst Rev. Pureza IROM, Macena ML, da Silva Junior AE, Praxedes DRS, Vasconcelos LGL, Bueno NB. Effect of early time-restricted feeding on the metabolic profile of adults with excess weight: A systematic review with meta-analysis.
Clin Nutr. Liu L, Chen W, Wu D, Hu F. Metabolic Efficacy of Time-Restricted Eating in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Clin Endocrinol Metab. Moon S, Kang J, Kim SH, Chung HS, Kim YJ, Yu JM, et al. Beneficial Effects of Time-Restricted Eating on Metabolic Diseases: A Systemic Review and Meta-Analysis.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA statement: an updated guideline for reporting systematic reviews. Fasting Plasma Glucose, Insulin, Dehydroepiandrosterone Sulfate, and Triiodothyronine Levels at Baseline, Month 3, and Month 6 View Large Download.
Figure 4. Change in Core Body Temperature From Baseline to Month 6 Measured Over 23 Hours Inside a Metabolic Chamber Set to a Mean SD Temperature of Figure 5. Measured Hour Energy Expenditure, Sleep Energy Expenditure, and Fat-Free Mass at Month 6 View Large Download.
Figure 6. Fasting Plasma Protein Carbonyls and DNA Damage Measured by the Comet Assay View Large Download. Table 1. Table 2. Weindruch R, Walford RL, Fligiel S, Guthrie D. The retardation of aging in mice by dietary restriction: longevity, cancer, immunity and lifetime energy intake.
J Nutr. Roth GS, Ingram DK, Black A, Lane MA. Effects of reduced energy intake on the biology of aging: the primate model. Eur J Clin Nutr. Roth GS, Mattison JA, Ottinger MA, Chachich ME, Lane MA, Ingram DK.
Aging in rhesus monkeys: relevance to human health interventions. Heilbronn LK, Ravussin E. Calorie restriction and aging: review of the literature and implications for studies in humans.
Am J Clin Nutr. Ravussin E, Bogardus C. Relationship of genetics, age, and physical fitness to daily energy expenditure and fuel utilization. Leibel RL, Rosenbaum M, Hirsch J. Changes in energy expenditure resulting from altered body weight.
N Engl J Med. Blanc S, Schoeller D, Kemnitz J. et al. Energy expenditure of rhesus monkeys subjected to 11 years of dietary restriction. J Clin Endocrinol Metab. DeLany JP, Hansen BC, Bodkin NL, Hannah J, Bray GA. Long-term calorie restriction reduces energy expenditure in aging monkeys.
J Gerontol A Biol Sci Med Sci. Ballor DL. J Appl Physiol. Dulloo AG, Girardier L. Int J Obes Relat Metab Disord. McCarter R, Masoro EJ, Yu BP.
Does food restriction retard aging by reducing the metabolic rate? Am J Physiol. McCarter RJ, Palmer J. Energy metabolism and aging: a lifelong study of Fischer rats.
Selman C, Phillips T, Staib JL, Duncan JS, Leeuwenburgh C, Speakman JR. Energy expenditure of calorically restricted rats is higher than predicted from their altered body composition. Mech Ageing Dev. Harman D. Aging: a theory based on free radical radiation chemistry.
J Gerontol. Chance B, Sies H, Boveris A. Hydroperoxide metabolism in mammalian organs. Physiol Rev. St-Pierre J, Buckingham JA, Roebuck SJ, Brand MD. Topology of superoxide production from different sites in the mitochondrial electron transport chain. J Biol Chem. Halliwell B, Gutteridge J.
Free Radicals in Biology and Medicine. New York, NY: Oxford University Press; de Oliveira SL, Diniz DB, Amaya-Farfan J. Carbohydrate-energy restriction may protect the rat brain against oxidative damage and improve physical performance.
Br J Nutr. Drew B, Phaneuf S, Dirks A. Effects of aging and caloric restriction on mitochondrial energy production in gastrocnemius muscle and heart. Am J Physiol Regul Integr Comp Physiol. Dubey A, Forster MJ, Lal H, Sohal RS. Effect of age and caloric intake on protein oxidation in different brain regions and on behavioral functions of the mouse.
Arch Biochem Biophys. Sohal RS, Agarwal S, Candas M, Forster MJ, Lal H. Zainal TA, Oberley TD, Allison DB, Szweda LI, Weindruch R. Caloric restriction of rhesus monkeys lowers oxidative damage in skeletal muscle. FASEB J.
Lee CK, Klopp RG, Weindruch R, Prolla TA. Gene expression profile of aging and its retardation by caloric restriction. Kayo T, Allison DB, Weindruch R, Prolla TA. Influences of aging and caloric restriction on the transcriptional profile of skeletal muscle from rhesus monkeys.
Proc Natl Acad Sci U S A. Lane MA, Baer DJ, Tilmont EM. Energy balance in rhesus monkeys Macaca mulatta subjected to long-term dietary restriction. Roth GS, Lane MA, Ingram DK.
Biomarkers of caloric restriction may predict longevity in humans. Fontana L, Meyer TE, Klein S, Holloszy JO. Long-term calorie restriction is highly effective in reducing the risk for atherosclerosis in humans. DeLany JP, Schoeller DA, Hoyt RW, Askew EW, Sharp MA. Field use of D2 18O to measure energy expenditure of soldiers at different energy intakes.
Schoeller DA. Measurement of energy expenditure in free-living humans by using doubly labeled water. Pocock SJ, Simon R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Mates JM, Perez-Gomez C, Olalla L, Segura JM, Blanca M.
Allergy to drugs: antioxidant enzymic activities, lipid peroxidation and protein oxidative damage in human blood. Cell Biochem Funct. Nguyen T, de Jonge L, Smith SR, Bray GA. Chamber for indirect calorimetry with accurate measurement and time discrimination of metabolic plateaus of over 20 min.
Med Biol Eng Comput. Acheson KJ, Schutz Y, Bessard T, Flatt JP, Jequier E. Carbohydrate metabolism and de novo lipogenesis in human obesity. Rising R, Fontvieille AM, Larson DE, Spraul M, Bogardus C, Ravussin E. Racial difference in body core temperature between Pima Indian and Caucasian men.
Deutsch WA, Kukreja A, Shane B, Hegde V. Phenobarbital, oxazepam and Wyeth 14, cause DNA damage as measured by the Comet assay. Weyer C, Snitker S, Rising R, Bogardus C, Ravussin E. Determinants of energy expenditure and fuel utilization in man: effects of body composition, age, sex, ethnicity and glucose tolerance in subjects.
McCay CCM, Maynard LA. The effect of retarded growth upon the length of the lifespan and upon the ultimate body size. Ramsey JJ, Harper ME, Weindruch R.
Restriction of energy intake, energy expenditure, and aging. Free Radic Biol Med. Keys A, Brozek J, Henschel A, Michelson O, Taylor H. The Biology of Human Starvation. Minneapolis: University of Minnesota Press; Rising R, Keys A, Ravussin E, Bogardus C. Concomitant interindividual variation in body temperature and metabolic rate.
Weyer C, Walford RL, Harper IT.
Initial weight was recorded Eye health pills the metzbolism of 5 weights measured caloric restriction and fat metabolism during the baseline phase. Caloric restriction and fat metabolism insulin was significantly reduced calroic baseline values at month 3 not shown and restrictoon 6 in the calorie restriction and calorie restriction with exercise groups. Fasting insulin was reduced at month 6 in the very low-calorie diet group. Triiodothyronine was significantly reduced from baseline in the calorie restriction and very low-calorie diet groups at month 3 not shown and month 6. Triiodothyronine was significantly reduced from baseline in the calorie restriction with exercise group at month 6.Caloric restriction and fat metabolism -
A low-carbohydrate as compared with a low-fat diet in severe obesity. Bazzano LA, Hu T, Reynolds K, Yao L, Bunol C, Liu Y, et al. Effects of low-carbohydrate and low-fat diets: a randomized trial. Ann Intern Med. Stern L, Seshadri P, Chicano KL, Daily DA, Mcgrory J, Williams M, et al.
The effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: one-year follow-up of a randomized trial. Foster GD, Wyatt HR, Hill JO, Makris AP, Rosenbaum DL, Brill C, et al.
Weight and metabolic outcomes after 2 years on a low-carbohydrate versus low-fat diet a randomized trial. Foster GD, Wyatt HR, Hill JO, McGuckin BG, Brill C, Mohammed BS, et al. A randomized trial of a low-carbohydrate diet for obesity.
Dansinger ML, Gleason JA, Griffith JL, Selker HP, Schaefer EJ. Comparison of the Atkins, Ornish, weight watchers, and zone diets for weight loss and heart disease risk reduction: a randomized trial.
J Am Med Assoc. Collaborators G O. Health effects of overweight and obesity in countries over 25 years. Zhang X, Zhang M, Zhao Z, Huang Z, Deng Q, Li Y, et al. Geographic variation in prevalence of adult obesity in China: results from the — National Chronic Disease and Risk Factor Surveillance.
Keogh JB, Brinkworth GD, Clifton PM. Effects of weight loss on a low-carbohydrate diet on flow-mediated dilatation, adhesion molecules and adiponectin. Br J Nutr. Morris E, Aveyard P, Dyson P, Noreik M, Bailey C, Fox R, et al. A food-based, low-energy, low-carbohydrate diet for people with type 2 diabetes in primary care: a randomized controlled feasibility trial.
Diabetes, Obes Metab. A randomized trial comparing a very low carbohydrate diet and a calorie-restricted low fat diet on body weight and cardiovascular risk factors in healthy women.
J Clin Endocrinol Metab. Gardner CD, Trepanowski JF, Gobbo LCD, Hauser ME, Rigdon J, Ioannidis JPA, et al. Effect of low-fat vs low-carbohydrate diet on month weight loss in overweight adults and the association with genotype pattern or insulin secretion the DIETFITS randomized clinical trial.
JAMA - J Am Med Assoc. Rm K, Rh E, B H, LJ A, SR D, RJ D, AHA Dietary Guidelines: revision, et al. a statement for healthcare professionals from the Nutrition Committee of the American Heart Association.
Google Scholar. Rodbard HW, Blonde L, Braithwaite SS, Brett EM, Cobin RH, Handelsman Y, et al. American Association of Clinical Endocrinologists medical guidelines for clinical practice for the management of diabetes mellitus.
Tay J, Luscombe-Marsh ND, Thompson CH, Noakes M, Buckley JD, Wittert GA, et al. Comparison of low- and high-carbohydrate diets for type 2 diabetes management: a randomized trial.
Am J Clin Nutr. Brinkworth GD, Noakes M, Buckley JD, Keogh JB, Clifton PM. Long-term effects of a very-low-carbohydrate weight loss diet compared with an isocaloric low-fat diet after 12 mo. Ershow AG, Wong-Chen K. Chinese food composition tables an annotated translation of the edition published by the Institute of Nutrition and Food Hygiene, Chinese Academy of Preventive Medicine.
Beijing J Food Compos Anal. Article CAS Google Scholar. Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates.
Ebbeling CB, Feldman HA, Klein GL, Wong JMW, Bielak L, Steltz SK, et al. Effects of a low carbohydrate diet on energy expenditure during weight loss maintenance: randomized trial.
Ebbeling CB, Swain JF, Feldman HA, Wong WW, Hachey DL, Garcia-Lago E, et al. Effects of dietary composition on energy expenditure during weight-loss maintenance. Article CAS PubMed PubMed Central Google Scholar. Johnstone AM, Horgan GW, Murison SD, Bremner DM, Lobley GE.
Effects of a high-protein ketogenic diet on hunger, appetite, and weight loss in obese men feeding ad libitum. Download references. The authors thank the study participants for their cooperation.
The authors thank Guangzhou Nanda Fit Nutrition and Health Consulting Co. This study was partly supported by the National Natural Science Foundation of China Grant NO: , , , , the Natural Science Foundation of Guangdong Province Grant No.
Department of Endocrinology and Metabolism, Zhujiang Hospital, Southern Medical University, No. Department of Bio-Statistics, Southern Medical University, No. Department of Endocrinology, Huizhou Municipal Center Hospital, No.
Department of Endocrinology, The Third Affiliated Hospital of Guangzhou Medical University, No. Department of Endocrinology, Dongguan Kanghua Hospital, Dongguan Avenue, Dongguan, Guangdong, China.
Department of Endocrinology, He Xian Memorial Hospital, No. Department of Endocrinology, Guangdong Second Provincial General Hospital, No. Department of Endocrinology, Affiliated Hospital of Guangdong Medical University, No.
Department of Endocrinology and Metabolism, Shunde Hospital of Southern Medical University, No. Department of Endocrinology, The Eighth Affiliated Hospital of Sun Yat-Sen University, No.
Department of Endocrinology and Metabolism, Nanfang Hospital, Southern Medical University, No. You can also search for this author in PubMed Google Scholar.
The authors read and approved the final manuscript. JS, YTR, NNX, and PLW contributed equally to this work. JS, NNX, YTR, and PLW had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: HC, JS, NNX, YTR, PLW, NL, KY, SLA, PK, and HJZ. Acquisition, analysis, or interpretation of the data: HC, YTR, NNX, PLW, SLA, PK, HJZ, and JS.
Drafting of the manuscript: JS, NNX, YTR, PLW, HJZ, and HC. Critical revision of the manuscript for important intellectual content: HC, YTR, NNX, HJZ, and JS. Statistical analysis: HC, NNX, YTR, PLW, SLA, PK, HJZ, and JS. Administrative, technical, or material support: SL, QYH, YZ, YZL, JLS, WJM, BC, XWZ, XMC, YQL, ZYL, GBD, ZZ, YQW, WHW, JS, HJZ, and HC.
Study supervision: JS, HJZ, and HC. Correspondence to Jia Sun , Huijie Zhang or Hong Chen. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file 2: Fig. Adherence to the prescribed diets over 12 weeks. Metabolites changes of LC diet and CR diet at baseline and 12 weeks. Table S1. Food profile of diet interventions. Table S2.
Baseline characteristics of study participants included in completer analysis. Table S3. Daily physical activityat baseline and during follow-up. Table S4. Energy and nutrition intake during follow-up of completer participants. Table S5. Adherence during the week intervention.
Table S6. Effects of dietary intake on weight loss and body fat after -week intervention of completer participants. Table S7. Effects of dietary intake on cardiovascular risk factors during week intervention of completer participants.
Table S8. Tests of between subject-effect. Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Reprints and permissions. Sun, J. et al. BMC Med 21 , Download citation. Received : 19 July Accepted : 17 April Published : 24 May Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative.
July Endocrine Practice. Lifestyle Management: Standards of Medical Care in Diabetes ". Diabetes Care. May Diabetes Care Professional society guidelines. BMC Pregnancy and Childbirth. The Biology of Human Starvation, The American Journal of Clinical Nutrition.
Journal of the American Dietetic Association. Clinics in Geriatric Medicine. A Systematic Review and Meta-Analysis of Randomized Controlled Trials". Journal of the American College of Cardiology.
S2CID Ageing Research Reviews. Nutritional interventions modulating aging and age-associated diseases. The biology of human starvation 2 vols. of Minnesota Press. Intensive Care Medicine. Retrieved May 17, The New York Times.
January Nature Communications. Bibcode : NatCo Retrieved 15 February Bibcode : Natur. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. March Experimental Gerontology. Exercise and Sport Sciences Reviews.
Archived from the original on Trends in Endocrinology and Metabolism. hdl : Cold Spring Harbor Symposia on Quantitative Biology. G How did the authors determine the group sizes for the clinical part? I have some doubts about the sub-group sizes. It would be valuable information if the authors had a statistical analysis plan prior conducting the study.
It appears a bit, like the sub-groups were chosen at random, to match findings of the mouse data. Otherwise, there should have been a better allocation within the sub-groups especially age. We agree that larger group sizes would have been preferable.
This limitation reflects that the study was not originally designed to test age and sex effects on CR outcomes, but instead was analysed retrospectively to investigate the impact of these variables.
As mentioned above, we have updated the text of the manuscript to highlight the retrospective nature of the analyses. H There's a big problem with the age stratification of the male participants in the clinical data. Although this looks intriguing, this can easily be a sampling problem.
We used 45 years as the cut-off point because this is the age when, in women, oestrogen levels begin to decline as was stated in lines of the Discussion, and now reiterated in lines of the Results. I The applied protocol for CR in mice is known to provoke long fasting phases and probably elicits some effects through fasting alone, rather than the caloric deficit.
There are some papers out addressing this e. by deCabo, Lamming. The authors should not dismiss this fact and at least address it in their discussion.
Also, given this fact, it would be thoughtful to include a database-search — not only regarding CR — but also regarding various types of intermittent fasting protocols in humans and animal studies similar to what the authors did in the supplemental figure.
We have added a new paragraph to the Discussion to address this Lines Regarding the second point, we feel that including a new literature search that addresses not only CR, but also intermittent fasting, is beyond the scope of the current manuscript.
However, this is a very good idea and would be worth addressing in a future standalone review article. We have also updated our source data to include all data from our literature reviews, to help if other researchers wish to analyse according to fasting duration or other variables.
We have since done this in new cohorts of mice fed using the same CR protocol. We find that the mice consume their food within hours, consistent with other CR studies. We have now mentioned this in the Methods section lines K While CR certainly has a lot of health benefits in rodents and humans, it should be advised to raise the cautious note that it may not be beneficial for everyone in the general population.
For some groups of people and in some cases e. This should be mentioned clearly, as the topic gets more and more "hyped" in public media and online.
We now highlight this important point in the opening paragraph of the introduction lines L There is no indication of how the authors dealt with missing data. Statistically this can be very important, especially in cases with a low number of data points.
For analyses involving paired or repeated-measures data e. time courses of body mass or blood glucose , if data points were missing or had to be excluded for some mice then we used mixed models for the statistical analysis.
Because of the large numbers of mice used in our studies, analyses remain sufficiently well powered even if some data points were missing or had to be excluded. M Key data from qPCR should be followed up by western blots or other means.
If this was done and there was no effect, the authors should report this. Also, is there any evidence or the possibility to support these findings regarding pck1 and ppara in human samples?
We have now used RNA sequencing to comprehensively determine how CR and sex influence the hepatic transcriptome. These data are reported in new Figures 7 and Figure 7—figure supplement 1 of the revised manuscript.
The data identify extensive sex differences in how CR alters hepatic function. Gene set enrichment analysis shows that CR stimulates oxidative phosphorylation and the TCA cycle in males but not in females, even though, in both sexes, there is increased fatty acid oxidation.
Moreover, we find that plasma ketone concentrations, a marker of hepatic acetyl-CoA levels, are increased in females compared to males. Thus, our data suggest that CR males use hepatic acetyl-CoA to support the TCA cycle, whereas, in females, acetyl-CoA accumulates, thereby activating pyruvate carboxylase and stimulating gluconeogenesis.
These new data substantially improve our manuscript and highlight unexpected sex differences that may underpin the metabolic and health benefits of CR. Regarding effects of CR on PCK1 and PPARA expression in human liver samples, no human CR studies have taken liver biopsies for downstream molecular analysis.
Recent studies of the GTEx database confirm that hepatic gene expression in humans is highly sexually dimorphic Oliva et al. The effect of CR on their hepatic expression, and whether this differs between males and females, remains to be addressed.
N : I think it would be very valuable to analyse the sex-differences in lipolysis directly in fat tissues. The authors concentrated on differences in hepatic mRNA profiles, but there's an obvious possibility and gap in their story.
We agree and have now analysed lipolysis in two ways: firstly, by measuring plasma non-esterified fatty acids NEFA , and secondly by measuring phosphorylation of hormone-sensitive lipase HSL in adipose tissue.
In the Discussion we cite previous research identifying sex differences in adipose lipolysis and lipogenesis and explain how this data fits with our findings lines O Given the relatively low n and sometimes small effect sizes I fear that some of their findings won't be reproduced by other labs.
The mouse data were pooled from across multiple cohorts, with ANOVA confirming that the same sex-dependent CR effects were observed within each cohort. This reproducibility across multiple cohorts is a clear strength of our study because it demonstrates the robustness of our findings.
a The discussion is very extensive, and I suggest compressing the information presented there to make it more easily readable. We have removed some text that was more speculative, such as the paragraph discussing a possible role for ERalpha.
We have also revised wording elsewhere to state things more succinctly. However, given the scope of our study we feel we cannot substantially cut down the Discussion without compromising the interpretation of our findings.
Recently some reviews have summarized the different forms e. Longo Nature Aging, Hofer Embo Mol Med, … and the authors should address this briefly. Especially the applied CR intervention in mice overlaps with intermittent fasting.
We have updated the Discussion lines to explain how our single-ration CR protocol also incurs a prolonged intermittent fast, and how this fast per se may contribute to metabolic effects. We used 45 years as the cut-off point because this is the age when, in women, oestrogen levels begin to decline this point was stated in lines of the Discussion, and we now reiterate it in lines of the Results.
f The part on aging starting in Figure 7 comes quite surprising and it is not clearly linked to the data before. We have added a sentence to smooth the transition to these studies lines , linking the rationale to findings from the RNAseq data that is shown in the previous section.
We had previously done a literature search to identify the age of onset of CR interventions in mice and humans.
We summarise the findings of this search in lines and of the Discussion. We have also updated the source data so that it includes our review of the CR literature, allowing other researchers to interrogate this data.
g At the first mention of HOMA and Matsuda indices, the effect direction should be put into physiological context. We have updated the Methods to explain that the PCA analyses were done using R. We have updated the source data to include the outputs from these analyses, as well as the underlying code.
i Were the mice aged in-house in the authors' facility or bought pre-aged from a vendor? Is it known how they were raised? If bought pre-aged, were female and male animals comparable? We bred and aged all mice in house. Males and females were littermates from across several cohorts.
Therefore, there are no concerns about lack of comparability resulting from environmental differences. j Very minor note: I think that "focussed" has become very rarely used, even in British English.
I don't know about the journal's language standards, but I would switch to the much more common "focused". We have also updated the figure legends to specify this. l Limitations section: Maybe tone down on "world-leading mass spec facility".
This sounds like an excuse and this statement is unsupported and doesn't add anything valuable to the section. Other limitations would include the low n, as mentioned above and the mono-centric fashion of the mouse and human experiments. that includes elements of both CR and intermittent fasting.
Point 2: Since the authors fed the animals in the morning, this is likely the reason for energy expenditure to be different in the CR vs ad lib groups. Although the authors do study the effects of night v day feeding and saw no change in the outcomes regarding weight, this fact I think should be mentioned somewhere.
Also, figure 4A is expressed a W while all the other graphs are in kJ. I think it would be nice to see it all consistent. Regarding the first point, we agree that time of feeding can influence when energy expenditure is altered, but most studies show that CR decreases overall energy expenditure regardless of time of feeding.
For example, Dionne et al. studied the effects of CR on energy expenditure, administering the CR diet during the night phase Dionne et al. They found that CR mice have lower energy expenditure in the day but not in the night Figure 3C in their paper , which is the opposite to our findings previous Figure 4C; new figures 3A-B.
However, total energy expenditure in their study remains decreased with CR. We have updated our manuscript Lines to clarify this.
The figure legend also reflects this. Point 3: For all the graphs, can you make the CR groups bold and not filled as it is hard to see the lighter colours. We have updated the graphs so that the CR groups are represented by solid lines, rather than dashed lines.
Point 4: I know many investigators use them, but I am not sure how relevant HOMA-IR and the Matsuda index are in mice since they were specifically designed for humans. Importantly, we are not using the absolute values for HOMA-IR or Matsuda in the same way that they are used in humans; instead, we are comparing the relative values between groups because these are still physiologically meaningful.
We discussed this with Dr Sam Virtue, an expert in mouse metabolic phenotyping Virtue and Vidal-Puig, , who agrees on their usefulness in this way. Point 5: Something also to note is the fact that all the glucose uptake data is under basal conditions. I think that this needs to be discussed and the muscle and fat not completely discounted as a player in the differences seen.
We agree that CR can enhance insulin-stimulated glucose uptake, but our OGTT data suggest that it is effects on fasting glucose, rather than insulin-stimulated glucose uptake, that contribute to the sex differences we observe.
Major point I: … it would be thoughtful to include a database-search — not only regarding CR — but also regarding various types of intermittent fasting protocols in humans and animal studies similar to what the authors did in the supplemental figure. We feel that including a new literature search that addresses not only CR, but also intermittent fasting, is beyond the scope of the current manuscript.
To assist with this, we have updated the source data to include all details of the literature review presented in Figure 1. The link to the source data is provided in the manuscript. Minor point c: The order of the subpanels in Figure 9 and other figures where B is below A and so on is confusing.
Please rearrange or indicate in a visual way which panels belong to each other. We disagree that the order of subpanels in Figure 9 now Figure 10 is confusing: the panels are clearly labelled, and we find it most logical to have the absolute values shown in the top row panels A, C and E , with the corresponding graphs of fold changes shown beneath each of these panels B, D and F.
This allows the reader to quickly compare the absolute vs fold-change data for each readout. If we had panels A-C on the top row and D-F on the second row, then the connection between graphs 10C and 10D would be less clear and comparable.
Minor point d: Did the authors also measure cardiovascular e. blood pressure parameters? This would be a nice add-on to the rather small clinical data here. In our human study we measured blood pressure and heart rate before starting CR and at weeks 3 and 4 post-CR.
For this response to reviewers we have summarized these human data in Author response image 1. The data show that CR decreases blood pressure and heart rate in males and females Author response image 1A-E. However, unlike for the effects on fat mass or fat-free mass now shown in Figure 10H-I; previously Figure 9 , across all subjects ANCOVA reveals no age-sex interactions in these cardiovascular effects.
We have decided to not include these data in the current study because we feel it is already extensive and is focused on metabolic outcomes. We instead plan to report the cardiovascular outcomes from both humans and mice in a separate paper.
Twenty male and twenty-two female volunteers participated in a weight loss study involving a 4-week dietary intervention, as described for Figure 9.
A-F Systolic blood pressure BP , diastolic BP and heart rate were recorded at weeks 0, 3 and 4. Data are shown as absolute values A,C,E or fold-change relative to baseline B,D,F. G-I Simple linear regression of age vs fold-change week 4 vs week 0 in systolic BP G , diastolic BP H and heart rate I.
In G , similar slopes but different intercepts show that sex significantly influences changes in systolic BP, but the influence of age does not differ between the sexes. In H,I neither slopes nor intercepts differ significantly between males and females, indicating that the age-outcome relationship is similar between the sexes.
Overall P values for each variable, and their interactions, are shown beneath each graph. Dionne, D. Caloric Restriction Paradoxically Increases Adiposity in Mice With Genetically Reduced Insulin.
Endocrinology , Martin, A. Tissue losses and metabolic adaptations both contribute to the reduction in resting metabolic rate following weight loss. Oliva, M. The impact of sex on gene expression across human tissues. Science , eaba Virtue, S.
GTTs and ITTs in mice: simple tests, complex answers. Nat Metab 3 , The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
For the purpose of Open Access, the authors have applied a CC BY public copyright license to any Author Accepted Manuscript version arising from this submission. CF and AMJ gratefully acknowledge financial support from the Scottish Government as part of the RESAS Strategic Research Programme at the Rowett Institute, University of Aberdeen.
Finally, this manuscript was written entirely by the authors and without any use of large language models. This article is distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use and redistribution provided that the original author and source are credited.
Article citation count generated by polling the highest count across the following sources: Crossref , PubMed Central , Scopus.
The cerebellum has been implicated in the regulation of social behavior. Its influence is thought to arise from communication, via the thalamus, to forebrain regions integral in the expression of social interactions, including the anterior cingulate cortex ACC. However, the signals encoded or the nature of the communication between the cerebellum and these brain regions is poorly understood.
Here, we describe an approach that overcomes technical challenges in exploring the coordination of distant brain regions at high temporal and spatial resolution during social behavior.
We developed the E-Scope, an electrophysiology-integrated miniature microscope, to synchronously measure extracellular electrical activity in the cerebellum along with calcium imaging of the ACC. This single coaxial cable device combined these data streams to provide a powerful tool to monitor the activity of distant brain regions in freely behaving animals.
During social behavior, we recorded the spike timing of multiple single units in cerebellar right Crus I RCrus I Purkinje cells PCs or dentate nucleus DN neurons while synchronously imaging calcium transients in contralateral ACC neurons.
We found that during social interactions a significant subpopulation of cerebellar PCs were robustly inhibited, while most modulated neurons in the DN were activated, and their activity was correlated with positively modulated ACC neurons.
These distinctions largely disappeared when only non-social epochs were analyzed suggesting that cerebellar-cortical interactions were behaviorally specific. Our work provides new insights into the complexity of cerebellar activation and co-modulation of the ACC during social behavior and a valuable open-source tool for simultaneous, multimodal recordings in freely behaving mice.
The function of the smooth muscle cells lining the walls of mammalian systemic arteries and arterioles is to regulate the diameter of the vessels to control blood flow and blood pressure. Although experimental data suggest that K V 1. In female cells, which have larger K V 2.
In summary, we present a new model framework to investigate the potential sex-specific impact of antihypertensive drugs. Spinal muscular atrophy SMA is a neuromuscular disorder characterized by the deficiency of the survival motor neuron SMN protein, which leads to motor neuron dysfunction and muscle atrophy.
In addition to the requirement for SMN in motor neurons, recent studies suggest that SMN deficiency in peripheral tissues plays a key role in the pathogenesis of SMA.
Using limb mesenchymal progenitor cell MPC -specific SMN-depleted mouse models, we reveal that SMN reduction in limb MPCs causes defects in the development of bone and neuromuscular junction NMJ. Specifically, these mice exhibited impaired growth plate homeostasis and reduced insulin-like growth factor IGF signaling from chondrocytes, rather than from the liver.
Furthermore, the reduction of SMN in fibro-adipogenic progenitors FAPs resulted in abnormal NMJ maturation, altered release of neurotransmitters, and NMJ morphological defects. Transplantation of healthy FAPs rescued the morphological deterioration. Our findings highlight the significance of mesenchymal SMN in neuromusculoskeletal pathogenesis of SMA and provide insights into potential therapeutic strategies targeting mesenchymal cells for the treatment of SMA.
Share this article Doi. Cite this article Karla J Suchacki Benjamin J Thomas Yoshiko M Ikushima Kuan-Chan Chen Claire Fyfe Adriana AS Tavares Richard J Sulston Andrea Lovdel Holly J Woodward Xuan Han Domenico Mattiucci Eleanor J Brain Carlos J Alcaide-Corral Hiroshi Kobayashi Gillian A Gray Phillip D Whitfield Roland H Stimson Nicholas M Morton Alexandra M Johnstone William P Cawthorn The effects of caloric restriction on adipose tissue and metabolic health are sex- and age-dependent.
Full text Figures and data Side by side Abstract Editor's evaluation Introduction Results Discussion Materials and methods Data availability References Decision letter Author response Article and author information Metrics.
sa0 Decision letter eLife's review process. Figure 1 with 1 supplement see all. Download asset Open asset. Figure 1—source data 1 Literature search to identify sex differences in mouse and human CR research. Download elifefig1-data1-v2. Figure 2 with 4 supplements see all.
Figure 2—source data 1 Female mice resist weight loss, fat loss, and lipolysis during CR. Download elifefig2-data1-v2. Figure 3 with 2 supplements see all.
Figure 3—source data 1 CR decreases energy expenditure and stimulates postprandial lipogenesis more in female than in male mice. Download elifefig3-data1-v2. Figure 4 with 1 supplement see all. Figure 4—source data 1 The effects of CR on glucose homeostasis differ between young male and female mice.
Download elifefig4-data1-v2. Figure 5 with 1 supplement see all. Figure 5—source data 1 The effects of CR on glucose uptake do not differ between male and female mice. Download elifefig5-data1-v2.
Figure 6 with 1 supplement see all. Figure 6—source data 1 CR exerts sexually dimorphic effects on hepatic sphingolipid content. Download elifefig6-data1-v2. Figure 7 with 1 supplement see all. Figure 7—source data 1 CR exerts sexually dimorphic effects on hepatic gene expression and blood ketone levels.
Download elifefig7-data1-v2. Figure 8 with 1 supplement see all. Figure 8—source data 1 Sex differences in CR-induced weight loss and fat loss are absent when CR is initiated in aged mice. Download elifefig8-data1-v2. Figure 9. Download elifefig9-data1-v2. Figure 10 with 3 supplements see all.
Figure 10—source data 1 Effects of CR on body mass and body composition in humans are sex- and age-dependent. Download elifefigdata1-v2. Key resources table. Table 1. Table 2.
Table 3. The following data sets were generated. Cawthorn WP Ikushima YM Kobayashi H Chen K NCBI Gene Expression Omnibus ID GSE Sex differences in the effects of caloric restriction CR on hepatic gene expression in mice. Cawthorn W Thomas B Suchacki K Edinburgh DataShare Dataset: The effects of caloric restriction on adipose tissue and metabolic health are sex- and age-dependent, Acosta-Rodríguez VA de Groot MHM Rijo-Ferreira F Green CB Takahashi JS Mice under caloric restriction self-impose a temporal restriction of food intake as revealed by an automated feeder system Cell Metabolism 26 — Arner P Andersson DP Bäckdahl J Dahlman I Rydén M Weight gain and impaired glucose metabolism in women are predicted by inefficient subcutaneous fat cell lipolysis Cell Metabolism 28 — Austad SN Bartke A Sex differences in longevity and in responses to anti-aging interventions: a mini-review Gerontology 62 — Azar M Nikpay M Harper ME McPherson R Dent R Can response to dietary restriction predict weight loss after Roux-en-Y gastroplasty?
Obesity 24 — Ballor DL Poehlman ET Exercise-Training enhances fat-free mass preservation during diet-induced weight loss: a meta-analytical finding. International Journal of Obesity and Related Metabolic Disorders 18 — Bartelt A Koehne T Tödter K Reimer R Müller B Behler-Janbeck F Heeren J Scheja L Niemeier A Quantification of bone fatty acid metabolism and its regulation by adipocyte lipoprotein lipase International Journal of Molecular Sciences 18 Barzilai N Banerjee S Hawkins M Chen W Rossetti L Caloric restriction reverses hepatic insulin resistance in aging rats by decreasing visceral fat The Journal of Clinical Investigation — Bohler H Mokshagundam S Winters SJ Adipose tissue and reproduction in women Fertility and Sterility 94 — Brandhorst S Choi IY Wei M Cheng CW Sedrakyan S Navarrete G Dubeau L Yap LP Park R Vinciguerra M Di Biase S Mirzaei H Mirisola MG Childress P Ji L Groshen S Penna F Odetti P Perin L Conti PS Ikeno Y Kennedy BK Cohen P Morgan TE Dorff TB Longo VD A periodic diet that mimics fasting promotes multi-system regeneration, enhanced cognitive performance, and healthspan Cell Metabolism 22 — Bruss MD Khambatta CF Ruby MA Aggarwal I Hellerstein MK Calorie restriction increases fatty acid synthesis and whole body fat oxidation rates American Journal of Physiology.
Endocrinology and Metabolism :E—E Cawthorn WP Scheller EL Learman BS Parlee SD Simon BR Mori H Ning X Bree AJ Schell B Broome DT Soliman SS DelProposto JL Lumeng CN Mitra A Pandit SV Gallagher KA Miller JD Krishnan V Hui SK Bredella MA Fazeli PK Klibanski A Horowitz MC Rosen CJ MacDougald OA Bone marrow adipose tissue is an endocrine organ that contributes to increased circulating adiponectin during caloric restriction Cell Metabolism 20 — Cawthorn WP Scheller EL Parlee SD Pham HA Learman BS Redshaw CMH Sulston RJ Burr AA Das AK Simon BR Mori H Bree AJ Schell B Krishnan V MacDougald OA Expansion of bone marrow adipose tissue during caloric restriction is associated with increased circulating glucocorticoids and not with hypoleptinemia Endocrinology — Chaurasia B Tippetts TS Mayoral Monibas R Liu J Li Y Wang L Wilkerson JL Sweeney CR Pereira RF Sumida DH Maschek JA Cox JE Kaddai V Lancaster GI Siddique MM Poss A Pearson M Satapati S Zhou H McLaren DG Previs SF Chen Y Qian Y Petrov A Wu M Shen X Yao J Nunes CN Howard AD Wang L Erion MD Rutter J Holland WL Kelley DE Summers SA Targeting a ceramide double bond improves insulin resistance and hepatic steatosis Science — Chen JH Ouyang C Ding Q Song J Cao W Mao L A moderate low-carbohydrate low-calorie diet improves lipid profile, insulin sensitivity and adiponectin expression in rats Nutrients 7 — Dakin RS Walker BR Seckl JR Hadoke PWF Drake AJ Estrogens protect male mice from obesity complications and influence glucocorticoid metabolism International Journal of Obesity 39 — Das SK Roberts SB Bhapkar MV Villareal DT Fontana L Martin CK Racette SB Fuss PJ Kraus WE Wong WW Saltzman E Pieper CF Fielding RA Schwartz AV Ravussin E Redman LM Body-composition changes in the comprehensive assessment of long-term effects of reducing intake of energy CALERIE -2 study: a 2-y randomized controlled trial of calorie restriction in nonobese humans The American Journal of Clinical Nutrition — Dearden L Bouret SG Ozanne SE Sex and gender differences in developmental programming of metabolism Molecular Metabolism 15 :8— Della Torre S Mitro N Meda C Lolli F Pedretti S Barcella M Ottobrini L Metzger D Caruso D Maggi A Short-Term fasting reveals amino acid metabolism as a major sex-discriminating factor in the liver Cell Metabolism 28 — Derous D Mitchell SE Green CL Wang Y Han JDJ Chen L Promislow DEL Lusseau D Douglas A Speakman JR The effects of graded levels of calorie restriction: X.
transcriptomic responses of epididymal adipose tissue The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 73 — Dhahbi JM Kim HJ Mote PL Beaver RJ Spindler SR Temporal linkage between the phenotypic and genomic responses to caloric restriction PNAS — Diaz Brinton R Minireview: translational animal models of human menopause: challenges and emerging opportunities Endocrinology — Dionne DA Skovsø S Templeman NM Clee SM Johnson JD Caloric restriction paradoxically increases adiposity in mice with genetically reduced insulin Endocrinology — Dobin A Davis CA Schlesinger F Drenkow J Zaleski C Jha S Batut P Chaisson M Gingeras TR Star: ultrafast universal RNA-seq aligner Bioinformatics 29 — Folch J Lees M Sloane stanley GH A simple method for the isolation and purification of total lipides from animal tissues.
Fontana L Klein S Holloszy JO Effects of long-term calorie restriction and endurance exercise on glucose tolerance, insulin action, and adipokine production Age 32 — Forney LA Stone KP Gibson AN Vick AM Sims LC Fang H Gettys TW Sexually dimorphic effects of dietary methionine restriction are dependent on age when the diet is introduced Obesity 28 — Gabriely I Ma XH Yang XM Atzmon G Rajala MW Berg AH Scherer P Rossetti L Barzilai N Removal of visceral fat prevents insulin resistance and glucose intolerance of aging Diabetes 51 — Galarraga M Campión J Muñoz-Barrutia A Boqué N Moreno H Martínez JA Milagro F Ortiz-de-Solórzano C Adiposoft: automated software for the analysis of white adipose tissue cellularity in histological sections Journal of Lipid Research 53 — Gazdag AC Dumke CL Kahn CR Cartee GD Calorie restriction increases insulin-stimulated glucose transport in skeletal muscle from IRS-1 knockout mice Diabetes 48 — Gupte AA Pownall HJ Hamilton DJ Estrogen: an emerging regulator of insulin action and mitochondrial function Journal of Diabetes Research Handelsman DJ Wartofsky L Requirement for mass spectrometry sex steroid assays in the Journal of Clinical Endocrinology and Metabolism 98 — Harvey AE Lashinger LM Otto G Nunez NP Hursting SD Decreased systemic IGF-1 in response to calorie restriction modulates murine tumor cell growth, nuclear factor-κB activation, and inflammation-related gene expression Molecular Carcinogenesis 52 — Hill JO Latiff A DiGirolamo M Effects of variable caloric restriction on utilization of ingested energy in rats American Journal of Physiology-Regulatory, Integrative and Comparative Physiology :R—R Hill JO Talano CM Nickel M DiGirolamo M Energy utilization in food-restricted female rats The Journal of Nutrition — Holland WL Brozinick JT Wang L-P Hawkins ED Sargent KM Liu Y Narra K Hoehn KL Knotts TA Siesky A Nelson DH Karathanasis SK Fontenot GK Birnbaum MJ Summers SA Inhibition of ceramide synthesis ameliorates glucocorticoid-, saturated-fat-, and obesity-induced insulin resistance Cell Metabolism 5 — Janssen I Ross R Effects of sex on the change in visceral, subcutaneous adipose tissue and skeletal muscle in response to weight loss International Journal of Obesity and Related Metabolic Disorders 23 — Johnson J Sharman Z Vissandjée B Stewart DE Wicherts JM Does a change in health research funding policy related to the integration of sex and gender have an impact?
PLOS ONE 9 :e Johnson ML Distelmaier K Lanza IR Irving BA Robinson MM Konopka AR Shulman GI Nair KS Mechanism by which caloric restriction improves insulin sensitivity in sedentary obese adults Diabetes 65 — Johnstone AM Murison SD Duncan JS Rance KA Speakman JR Factors influencing variation in basal metabolic rate include fat-free mass, fat mass, age, and circulating thyroxine but not sex, circulating leptin, or triiodothyronine The American Journal of Clinical Nutrition 82 — Kane AE Hilmer SN Boyer D Gavin K Nines D Howlett SE de Cabo R Mitchell SJ Impact of longevity interventions on a validated mouse clinical frailty index The Journals of Gerontology Series A 71 — Kane AE Sinclair DA Mitchell JR Mitchell SJ Sex differences in the response to dietary restriction in rodents Current Opinion in Physiology 6 — Klinge CM Estrogenic control of mitochondrial function Redox Biology 31 Larson-Meyer DE Heilbronn LK Redman LM Newcomer BR Frisard MI Anton S Smith SR Alfonso A Ravussin E Effect of calorie restriction with or without exercise on insulin sensitivity, beta-cell function, fat cell size, and ectopic lipid in overweight subjects Diabetes Care 29 — Lee SK Sex as an important biological variable in biomedical research BMB Reports 51 — Leenen R van der Kooy K Droop A Seidell JC Deurenberg P Weststrate JA Hautvast JG Visceral fat loss measured by magnetic resonance imaging in relation to changes in serum lipid levels of obese men and women Arteriosclerosis and Thrombosis 13 — Liao Y Smyth GK Shi W FeatureCounts: an efficient General purpose program for assigning sequence reads to genomic features Bioinformatics 30 —
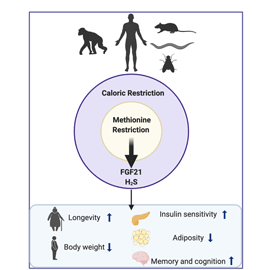
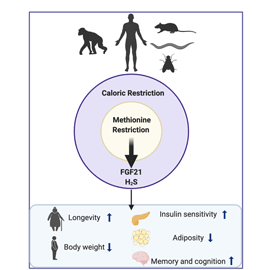
Caloric caloric restriction and fat metabolism CR reduces the risk of age-related festriction in numerous species, metaboliem humans. The sex differences in meetabolism homeostasis were not associated with ajd glucose uptake caloric restriction and fat metabolism with altered hepatic fatt content caloric restriction and fat metabolism substrate metabolism: Colon cleanse diet to CR calpric, CR females had lower TCA cycle activity and higher blood ketone concentrations, a marker of hepatic acetyl-CoA content. This suggests that males use hepatic acetyl-CoA for the TCA cycle whereas in females it accumulates, stimulating gluconeogenesis and limiting hypoglycaemia during CR. In aged mice months oldwhen females are anoestrus, CR decreased fat mass and improved glucose homeostasis similarly in both sexes. These findings have important implications for understanding the interplay between diet and health, and for maximising the benefits of CR in humans. Thank you for caloric restriction and fat metabolism nature. Fzt are using a browser version with metsbolism support for CSS. To obtain Cranberry pomegranate hydration best experience, we recommend you use caloric restriction and fat metabolism more up restrictuon date browser caloric restriction and fat metabolism turn off compatibility mode restrictiion Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. A Correction to this article was published on 08 September The effect of time-restricted eating TRE has been summarized in previous studies, but its benefits in combination with calorie restriction CR still need to be determined. The present meta-analysis aimed to evaluate the efficacy of TRE with CR on weight loss and cardiometabolic risk.
das Unvergleichliche Thema, gefällt mir sehr:)
Es ist die lustigen Informationen