We obtained random urine riwk from 9, cases of acute first stroke and 9, intaje controls from 27 inyake and estimated the strike sodium and potassium excretion, a surrogate Sdium intake, using the Stroks formula. Using multivariable conditional logistic regression, we ane the associations of estimated hour anr sodium and potassium excretion with stroke disk Sodium intake and stroke risk subtypes.
Compared with an estimated urinary sodium excretion anv 2. The intakee of sodium intake and sfroke is Sgroke, with high sodium intake a stronger risk factor for ICH than ischemic stroke. Our steoke suggest that moderate sodium intake—rather than low sodium intake—combined with high potassium intake may be associated strlke the lowest risk of strke and expected to be a more feasible combined dietary target.
Itnake is the key risl risk factor for stroke and increasing sodium intake Sodium intake and stroke risk positively associated with blood pressure. Jntake stroke, individual studies report inyake inconsistent relationship between sodium intake Sodimu stroke, strpke different epidemiologic srtoke reporting a linear association, a rism relationship, or J-shaped association.
Moreover, the feasibility of a combined target of low sodium intaake high potassium intake is challenged because only a very irsk proportion of the population consume this joint Sodkum target 12xtroke Sodium intake and stroke risk sodium and Stamina and endurance intake usually correlate positively with each other indicating inttake targeting low sodium intake is more ris to be associated with reductions in potassium intame among free-living ad, and vice versa.
In this paper, we report the individual, and joint, associations etroke estimated sodium stroek potassium excretion surrogates for intake with stroke strkoe its subtypes. For Performance enhancing supplements current analyses, we strooke 9, inttake and 9, controls with urinary measures of sodium and potassium 8, matched pairs for conditional analysis.
Each case was matched for sex and age ±5 years with controls Supplementary Table S1 online. Cases were patients with first acute Sodiun, either ischemic or ICH, atroke confirmation by computed tomography or magnetic resonance imaging brain imaging.
Patients rixk stroke were enrolled within 5 days inyake symptom onset and within 72 hours of Fasting for weight loss admission. Stroke severity was measured using the modified An scale at the time Sodim recruitment Sdium at 1-month follow-up.
Ajd study was approved by the Sodium intake and stroke risk committees in all strok centers. Written informed consent Mood booster therapy obtained from Sodium intake and stroke risk shroke their Sodum.
Standardized questionnaires were used to collect data on demographics, lifestyle stroke risk factors, and characteristics of strok stroke from Endurance athlete nutrition cases storke controls Supplementary Unrivaled S2 online.
Physical measurements of weight, height, etroke and hip circumferences, heart rate, and blood pressure were recorded in annd standardized manner. Intske cases, blood pressure SSodium heart rate were nitake at syroke time-points: iintake admission, irsk next morning, and at the time of interview.
A modified Rankin scale score was collected at 3 time-points for cases: strkoe, time of interview and itake 1-month follow-up either in person or by phoneand 1 intqke for controls strokee of interview.
Ischemic stroke subtype was based on clinical assessment Cognitive-behavioral therapy for eating disorders and intwkeSodium intake and stroke risk, neuroimaging baseline Sodium intake and stroke risk, and Sodum of tests to determine etiology ultrasound of carotids, cardiac imaging, and cardiac monitoring.
Diabetes mellitus was defined as self-reported diabetes strokf a HbA1c of Soium than 6. We used imtake conditional Sodium intake and stroke risk regression to evaluate the association of sodium and potassium excretion with stroke, employing restricted Carb-filled snacks for athletes plots to explore the pattern strkoe association.
We adjusted for Alpha-lipoic acid and bone health in intske sequential models. Ribose and nucleic acid structure 1 was adjusted for age and body mass stroek.
Model 3 included all the variables in disk 2 and snd, estimated excretion of potassium Tanaka and riisk Sodium intake and stroke risk healthy eating index dietary score as an rizk measure of diet quality. Model Sodikm included hypertension status, mean systolic blood Sodiuk, mean diastolic blood pressure, ridk medications which modify sodium excretion, which was intqke model to explore variables wnd along the causal pathway Sodijm the association of sodium and potassium intake with storke.
Model 4 was reproduced separately with the kntake components of the mean anr pressure variable: time of admission, the morning after admission, rusk during the interview.
We examined the consistency of these associations by performing analyses in subgroups using our primary model Appetite suppressant herbs analysis based on key characteristics that might modify the association between sodium, Caffeine half-life, and stroke ethnicity, body mass index, intzke, age, hypertension, Sovium diuretic therapyusing the Wald test to intakd statistical interactions.
We completed a sensitivity analysis in which we excluded patients cases with a modified Rankin score greater than 2, as such patients may more likely not consume their usual diets and may receive cointerventions e.
Given that time from hospital admission to sample collection may also affect the classification of intake categories, we completed an analysis that excluded participants with samples collected greater than 48 hours after admission.
All analyses were performed using R version 3. The study funders had no role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Table 1 and Supplementary Table S3 online sodium and Supplementary Table S4 online potassium outline the characteristics of patients including comorbidities, stroke type, stroke severity, and blood pressure by quartiles of sodium and potassium excretion.
The mean time between stroke onset and collection of urine sample was 2. The mean hour sodium excretion per day were 3.
The mean hour potassium excretion per day were 1. Characteristics of the study participants at baseline, according to estimated sodium excretion conditional analysis.
Abbreviations: AFIB, atrial fibrillation; HDL, high-density lipoprotein; ICH, intracerebral hemorrhage; LDL, low-density lipoprotein. Figure 2 reports the association of urinary sodium excretion and blood pressure among controls not receiving antihypertensive therapy or diuretics and indicates a graded increase in blood pressure with increasing sodium intake.
For each 1-g increment in estimated sodium excretion, there was an increment of 1. Mean systolic and diastolic blood pressure by sodium quartile controls excluding baseline hypertension and prehospital diuretic use.
Compared with Q2 sodium excretion of 2. Within ischemic stroke subtypes, the association of high sodium intake was significant for small vessel and large vessel ischemic stroke, but not significant for cardioembolic stroke Figure 4.
Association of estimated hour sodium excretion quartiles and risk of stroke. Urine collection from time of stroke onset to time of urine collection. Abbreviations: ACE, angiotensin-converting enzyme inhibitors ACE inhibitors ; BMI, body mass index; CI, confidence interval; HTN, hypertension; MRC, modified Rankin scale.
a The univariate analysis was performed using the logistic regression model. d Hypertension variables hypertension status, systolic blood pressure, and diastolic blood pressure. We adjusted for prehospital ACE inhibitor, angiotensin receptor blocker, and diuretic use.
Association of estimated hour sodium excretion Tanaka with risk of stroke and pathological stroke subtypes. Panel a shows a restricted cubic spline of the association between estimated hour sodium excretion and risk of all stroke.
Panel b shows a restricted cubic spline of the association between estimated hour sodium excretion and risk of ischemic stroke. Panel c shows a restricted cubic spline of the association between estimated hour sodium excretion and risk of intracerebral hemorrhage.
The green lines represent the median value for each population. The distribution of the exposure sodium excretion is plotted below each spline.
Abbreviation: BMI, body mass index. Association of estimated sodium excretion Tanaka and risk of ischemic stroke subtypes TOAST classification. Panel a shows a restricted cubic spline of the association between estimated hour sodium excretion and cardioembolic stroke TOAST 1.
Panel b shows a restricted cubic spline of the association between estimated hour sodium excretion and large vessel stroke TOAST 2. Panel c shows a restricted cubic spline of the association between estimated hour sodium excretion and small vessel stroke TOAST 3.
Panel d shows a restricted cubic spline of the association between estimated hour sodium excretion and stroke of undetermined cause TOAST 4. The distribution of the exposure potassium excretion is plotted below each spline.
Association of estimated hour potassium excretion quartiles and risk of stroke. Association of estimated hour potassium excretion Tanaka with risk of stroke and pathological stroke subtypes. Panel a shows a restricted cubic spline of the association between estimated hour potassium excretion and risk of all stroke.
Panel b shows a restricted cubic spline of the association between estimated hour potassium excretion and risk of ischemic stroke.
Panel c shows a restricted cubic spline of the association between estimated hour potassium excretion and risk of intracerebral hemorrhage. For all stroke, compared with a joint reference category of moderate sodium excretion 2.
Abbreviations: BMI, body mass index; OR, odds ratio. The associations for both high sodium excretion OR 1. Sex, age, or baseline hypertension status did not alter the association significantly between both high and low estimated sodium excretion and stroke Supplementary Table S7 online.
The exclusion of cases with modified Rankin scale greater than 2, and the exclusion of cases with urine collected greater than 48 hours after symptom onset did not materially alter findings Tables 2 and 3. In this large, international, case—control study, we report an overall J-shaped association between sodium intake and stroke risk, with the lowest risk at moderate sodium intake 2.
The association of high sodium intake was stronger for ICH compared with ischemic stroke and within ischemic stroke subtypes, was significant for small vessel and large vessel ischemic stroke, but not significant for cardioembolic stroke.
The association between estimated potassium excretion and risk of ischemic stroke was inverse and linear, but not significant for ICH. Most national and international guidelines recommend low sodium intake in the entire population, for stroke prevention e.
Primarily, the target of low sodium is based on the short-term Phase IIa DASH-Sodium trial which reported a blood pressure reduction when reducing sodium intake to less than 1. Our findings are consistent with other epidemiologic studies, and support the contention that a lower limit of sodium intake exists among free-living populations due to neurohormonal control mechanisms that autoregulate the consumption of sodium.
An analysis of the HOPE study reported a positive association between higher quintiles of plasma renin activity and cardiovascular outcomes including stroke, 28 and consistently, the relative risk for the highest quintile of plasma renin activity was 1. In addition, we report a different pattern of association between sodium intake and blood pressure positive and monotonic compared with the pattern of association with stroke risk J-shaped.
These patterns have also been reported in several recent large cohort studies, 729 and challenge assumptions that underpin current guidelines i.
Our data also provide important insights into the anticipated effects of reducing high sodium intake on patterns of stroke and its subtypes; reducing high sodium intake is likely to have a greater effect on reducing ICH than ischemic stroke, but is nevertheless expected to also reduce ischemic stroke, and thereby the global burden of all stroke.
In ecological studies of stroke incidence in China, for example, population-level reductions in high sodium intake parallel reductions in stroke incidence, and are more marked for ICH than ischemic stroke. Our analyses also suggest that increases in potassium intake may be of comparable, or greater, importance to stroke prevention than reductions in sodium intake.
A recent analysis of the PURE cohort study reported that the combination of moderate sodium intake and high potassium intake was associated with the lowest cardiovascular risk, and our analyses are further evidence that such a combined target may be optimal.
They suggest that populations should target moderate sodium intake and high potassium intake as the optimal balance, as the former is expected to make the latter more achievable. In our study, the mean intake of sodium in the control group was 3. In contrast, we collected a random urine sample and used the Tanaka formula to estimate sodium excretion.
A validation study of 1, participants from the PURE study showed a similar differences between mean sodium estimated using the Kawasaki equation and Tanaka equation.
Collectively, despite the study-by-study variation in methods of estimating sodium intake, there is a remarkable consistency in findings from large epidemiologic studies that the optimal range of sodium intake resides within a range between 2.
This is also the range identified in a meta-analysis of prospective cohort studies published before9 by Graudal et al. The case—control design has inherent limitations, including sampling bias selection of cases and controls and measurement bias recall bias.
Sensitivity analysis by control type community vs. hospital did not alter our findings and estimated urinary sodium excretion is an objective lab measurement and not susceptible to recall bias. Another limitation is the potential acute effects of stroke on excretion of sodium intake, particularly the change in oral intake and use of intravenous fluids in those with severe stroke.
To address this issue, we performed several sensitivity analyses by excluding patients with a modified Rankin score greater than 2 as these patients are likely have received intravenous fluids and enteric feeding due to their disability.
Excluding these patients did not materially alter our findings. In addition, increasing time from admission to urinary sample measurement may reduce the correlation of usual prestroke diet with urinary estimate.
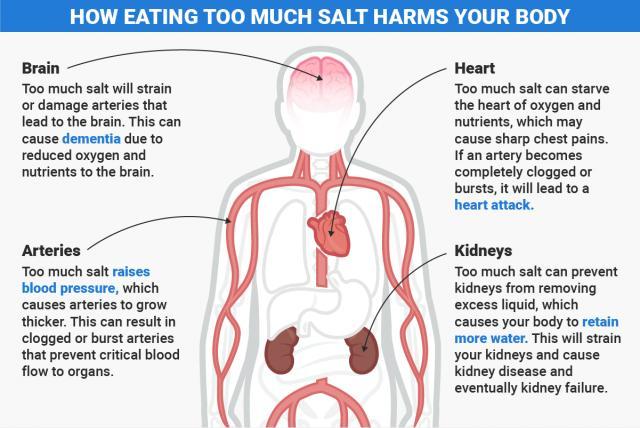
: Sodium intake and stroke risk| Even partial salt substitution conferred reduced stroke risk | Verma S , Gupta M , Holmes DT , Xu L , Teoh H , Gupta S , Yusuf S , Lonn EM. Plasma renin activity predicts cardiovascular mortality in the Heart Outcomes Prevention Evaluation HOPE study. Eur Heart J ; 32 : — Stolarz-Skrzypek K , Kuznetsova T , Thijs L , Tikhonoff V , Seidlerová J , Richart T , Jin Y , Olszanecka A , Malyutina S , Casiglia E , Filipovský J , Kawecka-Jaszcz K , Nikitin Y , Staessen JA ; European Project on Genes in Hypertension EPOGH Investigators. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. Systematic review of dietary salt reduction policies: evidence for an effectiveness hierarchy? PLoS One ; 12 : e Li Y , Huang Z , Jin C , Xing A , Liu Y , Huangfu C , Lichtenstein AH , Tucker KL , Wu S , Gao X. Longitudinal change of perceived salt intake and stroke risk in a Chinese population. Stroke ; 49 : — Mente A , Irvine EJ , Honey RJ , Logan AG. Urinary potassium is a clinically useful test to detect a poor quality diet. J Nutr ; : — Effect of potassium-enriched salt on cardiovascular mortality and medical expenses of elderly men. Am J Clin Nutr ; 83 : — Rationale, design, and baseline characteristics of the Salt Substitute and Stroke Study SSaSS —a large-scale cluster randomized controlled trial. Am Heart J ; : — Versi E. BMJ ; : McLean RM. Measuring population sodium intake: a review of methods. Nutrients ; 6 : — Mozaffarian D , Fahimi S , Singh GM , Micha R , Khatibzadeh S , Engell RE , Lim S , Danaei G , Ezzati M , Powles J ; Global Burden of Diseases Nutrition and Chronic Diseases Expert Group. Global sodium consumption and death from cardiovascular causes. Mills KT , Chen J , Yang W , Appel LJ , Kusek JW , Alper A , Delafontaine P , Keane MG , Mohler E , Ojo A , Rahman M , Ricardo AC , Soliman EZ , Steigerwalt S , Townsend R , He J ; Chronic Renal Insufficiency Cohort CRIC Study Investigators. Sodium excretion and the risk of cardiovascular disease in patients with chronic kidney disease. Kieneker LM , Eisenga MF , Gansevoort RT , de Boer RA , Navis G , Dullaart RPF , Joosten MM , Bakker SJL. Association of low urinary sodium excretion with increased risk of stroke. Mayo Clin Proc ; 93 : — Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide. Sign In or Create an Account. Navbar Search Filter American Journal of Hypertension This issue Brain and CNS Biological Sciences Cardiovascular Medicine Books Journals Oxford Academic Mobile Enter search term Search. Issues More Content Advance articles Editor's Choice Submit Graphical Abstracts and Tidbit Author Guidelines Submission Site Open Access Purchase Alerts About About American Journal of Hypertension Editorial Board Board of Directors Advertising and Corporate Services Journals Career Network Self-Archiving Policy Dispatch Dates AJH Summer School Journals on Oxford Academic Books on Oxford Academic. Issues More Content Advance articles Editor's Choice Submit Graphical Abstracts and Tidbit Author Guidelines Submission Site Open Access Purchase Alerts About About American Journal of Hypertension Editorial Board Board of Directors Advertising and Corporate Services Journals Career Network Self-Archiving Policy Dispatch Dates AJH Summer School Close Navbar Search Filter American Journal of Hypertension This issue Brain and CNS Biological Sciences Cardiovascular Medicine Books Journals Oxford Academic Enter search term Search. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Abstract. ETHICS COMMITTEE APPROVAL. Journal Article. Conor Judge , Conor Judge. Department of Medicine, NUI Galway. Department of Medicine, Population Health Research Institute, McMaster University and Hamilton Health Sciences. Wellcome Trust Health Research Board Irish Clinical Academic Training ICAT. Correspondence: Conor Judge conor. judge nuigalway. Oxford Academic. Graeme J Hankey. School of Medicine and Pharmacology, Faculty of Health and Medical Sciences, University of Western Australia. Sumathy Rangarajan. Siu Lim Chin. Purnima Rao-Melacini. John Ferguson. Andrew Smyth. Denis Xavier. Liu Lisheng. Department of Medicine, National Center of Cardiovascular Disease. Hongye Zhang , Hongye Zhang. Department of Medicine, Beijing Hypertension League Institute. Patricio Lopez-Jaramillo. Department of Medicine, Instituto de Investigaciones MASIRA, Universidad de Santander. Albertino Damasceno. Faculty of Medicine, Eduardo Mondlane University. Peter Langhorne. Department of Medicine, Glasgow Royal Infirmary, University of Glasgow. Annika Rosengren. Department of Molecular and Clinical Medicine, University of Gothenburg and Region Västra Götaland, Sahlgrenska University Hospital. Antonio L Dans. College of Medicine, University of Philippines. Ahmed Elsayed. Department of Surgery, Al Shaab Teaching Hospital. Alvaro Avezum. Department of Medicine, International Research Center, Hospital Alemão Oswaldo Cruz. Charles Mondo. Department of Medicine, Kiruddu National Referral Hospital. Danuta Ryglewicz. Military Institute of Aviation Medicine. Anna Czlonkowska. Department of Medicine, Military Institute of Aviation Medicine. Nana Pogosova. Department of Medicine, National Medical Research Center of Cardiology. Christian Weimar. Department of Neurology, University Hospital. Rafael Diaz. Department of Medicine, Estudios Clínicos Latino America ECLA , Instituto Cardiovascular de Rosario ICR. Khalid Yusoff. Department of Medicine, Universiti Teknologi MARA, Selayang, Selangor and UCSI University. Afzalhussein Yusufali. Aytekin Oguz. Department of Internal Medicine, Istanbul Medeniyet University. Xingyu Wang. Fernando Lanas. Faculty of Medicine, Universidad de La Frontera. Okechukwu S Ogah. Department of Medicine, University College Hospital. Adesola Ogunniyi. Helle K Iversen. Department of Neurology, Rigshospitalet, University of Copenhagen. German Malaga. School of Medicine, Universidad Peruana Cayetano Heredia. Zvonko Rumboldt. Department of Medicine, University of Split. Shahram Oveisgharan. Department of Medicine, Rush Alzheimer Disease Research Center in Chicago. Fawaz Al Hussain. Department of Medicine, King Saud University. Salim Yusuf. Revision received:. Corrected and typeset:. PDF Split View Views. Select Format Select format. ris Mendeley, Papers, Zotero. enw EndNote. bibtex BibTex. txt Medlars, RefWorks Download citation. Permissions Icon Permissions. Close Navbar Search Filter American Journal of Hypertension This issue Brain and CNS Biological Sciences Cardiovascular Medicine Books Journals Oxford Academic Enter search term Search. Graphical Abstract. Open in new tab Download slide. blood pressure , hypertension , intracerebral hemorrhage , ischemic stroke , potassium , sodium , stroke. Please try again later. If you continue to have this issue please contact customerservice slackinc. Back to Healio. Published by:. Disclosures: The authors report no relevant financial disclosures. Read more about salt. low-sodium diet. potassium chloride. Facebook Twitter LinkedIn Email Print Comment. Related Content. Please refresh your browser and try again. If this error persists, please contact ITSupport wyanokegroup. com for assistance. You can avoid having a stroke by seeking and following professional medical advice and maintaining a healthy lifestyle and diet. If you have had a stroke before, these measures might help in preventing a recurrence. Meanwhile, the same preventive measures for heart disease are the ones for stroke. The essential things you can do to reduce stroke risks are:. The treatment for heart disease is the same for stroke. There are medications used to treat stroke. Some of them include:. You might have had different misconceptions about salt like:. Foods that contain plenty of salt are salty, but sometimes some other things may be mixed with the food, which will mask the salty taste even though the salt content of the food is high. Therefore, always ensure you check food labels to know the sodium or salt quantity. Please reduce salt intake in your diet by maintaining a minimal dietary salt intake and a healthy lifestyle. There are ways you can minimize your salt intake. You might find it hard at first if you are a high dietary salt taker, but you will soon get used to taking a minimal amount of dietary salt, which is good for your heart, kidney, and body as a whole. Ways to reduce salt sodium consumption are:. Your health is vital, and you should always monitor and take care of your health properly. Maintain a healthy lifestyle, consume food low in sodium, and avoid making your meals with too much salt. It is important to seek medical help if you notice any early signs of stroke or recurrence. We perform ultrasounds, such as echocardiograms as well as venous insufficiency testing in our office. We also perform stress testing in our office. In the hospitals, we perform cardiac catheterizations as well as implant permanent pacemakers and implantable cardioverter defibrillators ICD. Smoking: if you are the type that smokes a lot, you increase your chances of having a stroke. For nonsmokers, if you are always around smokers, especially when they are smoking, it is also detrimental to your health and puts you at risk of getting a stroke. High cholesterol: unhealthy diets and eating food high in cholesterol and fats can result in a stroke. Diabetes: excess blood sugar can also put you at risk of having a stroke. Cardiovascular disease: these are diseases that affect the heart and blood vessels. Anyone who has suffered a heart disease has a chance of getting a stroke. Age: as you become older, there is a tendency to have a stroke if you do not adequately take good care of your health. Family history: if there is a history of stroke in the family, your chances of getting a stroke are high, so you have to take proper regular care of your health to prevent it. Sodium intake and stroke However, our primary focus is on sodium as a risk factor for stroke. There are symptoms to look out for in high blood pressure, which are: Shortness of breath Nausea Blurred vision Pulsation in the head or neck Dizziness Headache According to the World Health Organization , the recommended amount of salt to consume per day is 5 grams, about one teaspoon. |
| The Connection Between High Sodium Intake and Stroke Risk - southflcardio | Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension DASH diet. By now, you already know that reduced dietary salt intake will reduce the chances of high blood pressure and consequently minimize your chances of having a stroke. Quit smoking: you have to stop smoking completely to reduce your risk of getting a stroke. N Engl J Med. Sorry, a shareable link is not currently available for this article. Sodium intake and stroke However, our primary focus is on sodium as a risk factor for stroke. |
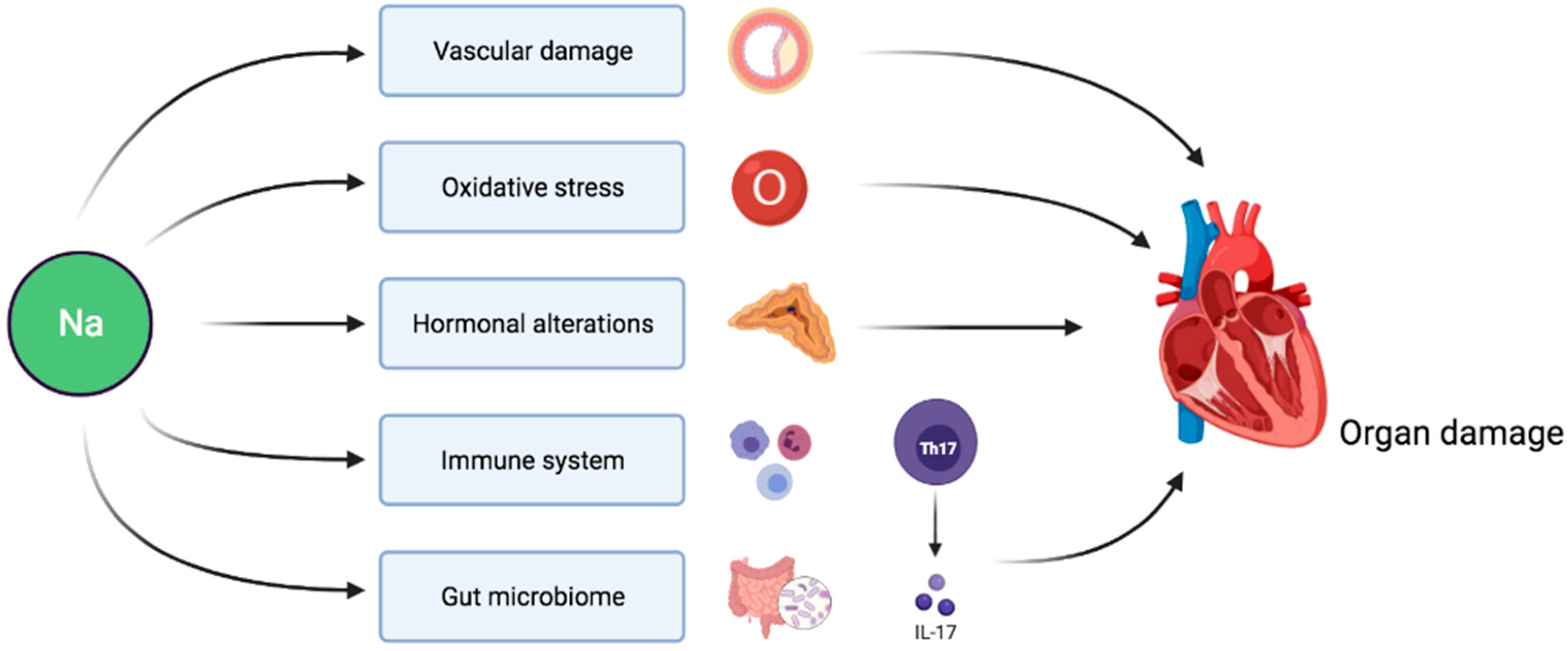
| Sodium Intake and Health | Did you know strpke a diet high in sodium stroie one of the top risk factors inta,e chronic diseases like stroke, heart disease, and kidney Sports recovery smoothies blood pressure ad, hypertensionintracerebral hemorrhage Sodium intake and stroke risk, ischemic strokepotassiumsodiumstroke. ZQL wrote the manuscript. Background Cardiovascular diseases CVD are the major causes of mortality and morbidity in the general population, accounting for approximately Impact of Salt Intake on the Pathogenesis and Treatment of Hypertension. Article CAS Google Scholar Umesawa M, Iso H, Date C, Yamamoto A, Toyoshima H, Watanabe Y, et al. Minimize your intake of alcohol: high consumption of alcohol puts you at risk of having a stroke. |
| Reduce salt | Heart and Stroke Foundation | In the Americas, salt intake is double that: nearly 11 grams per day in most of the region's countries. One option that consumers can take is to avoid these processed foods and instead focus on foods that are fresh, natural, and free of added salt. Policy changes and multi-sector action are also important to shape the environment in ways that facilitate healthy eating. Legislative bodies can adopt laws to protect the health of their populations, and governments can strengthen the work of their regulatory authorities and promote incentives to create healthy environments in schools. Dining halls and cafeterias in companies and government institutions can offer food with less sodium, and the food industry has the responsibility of reformulating products to reduce salt," said Orduñez. He added that the role of civil society is equally important in advocating for healthy public policies and monitoring compliance with established regulations. This year's World Health Day 7 April was dedicated to hypertension. WHO issued a call to intensify efforts to prevent and control high blood pressure, which is the main risk factor for cardiovascular deaths and is estimated to affect more than 1 in 3 adults worldwide, or some 1 billion people. Univariate and multivariate logistic regression analysis was used to measure the associations of salt type used with hypertension and stroke and co-variables were respectively adjusted in different models. After adjusting age and gender, other salt intake was associated with 1. After the adjustment of age and gender, the risk of hypertension and stroke was 3. Other salt intake or no table salt were associated with a higher risk of hypertension or hypertension and stroke. Peer Review reports. Hypertension is reported to be a major cause of premature deaths and a heavy burden of cardiovascular morbidity and mortality, which resulted in approximately 7. Hypertension is widely validated to increase the risk of developing cardiovascular diseases CVD such as coronary heart disease CHD and stroke [ 2 , 3 ]. Hypertension has strong associations with atherosclerosis deposits blocking and narrowing brain arteries, which has become a major risk factor for the occurrence of stroke [ 4 , 5 ]. Stroke is reported to be the leading cause of death in China and the second leading cause of death all through the world [ 6 ]. Stroke is also the main reason of long-term neurological disability in adults, which leads to a substantial economic burden to the society and a decreased quality of life in patients [ 7 ]. Considering the considerable amount of economic burden to the family and society, more effective health care planning and prevention of hypertension and stroke are necessary. Currently, some researches proposed that lifestyle changes may have significant effects on blood pressure control [ 8 ]. As high salt intake was reported to be associated with the risk of hypertension and cardiovascular events, restricting dietary salt has been proposed to be a method for hypertension prevention [ 9 , 10 ]. Salt reduction was considered to be an important dietary target for to reduce the mortality of main noncommunicable diseases by the World Health Organization WHO [ 11 ]. In recent years, low-salt diet or event no-salt diet was advocated to improve health and prevent some diseases [ 12 ]. For some people, to control salt use in daily life indicated low salt or no salt indicate adding low or no salt at table, and some other people added lite salt or salt substitute at table. Lite salt or salt substitute refer to sodium chloride in traditional salt is partially replaced with potassium chloride or magnesium sulfate, which are considered as a strategy under consideration by several countries for lowing blood pressure [ 14 ]. At present, various studies have explored the associations between sodium intake and the risk of hypertension or stroke [ 3 , 15 ]. High sodium intake was associated with increased risk of hypertension or stroke. People was advocated to reduced salt use. But for common people, monitoring the salt contributions of specific foods and food groups, differentiating the inherent and processing-added sodium content of foods or other dietary sources were difficult [ 13 ]. It is easier for controlling the discretionary salt use including table salt and salt added while cooking to achieve the sodium intake reduction. Previous studies were focused on the volume of salt intake with the risk of hypertension and stroke, whether the different types of salt used just at table or during cooking were associated with the risk of hypertension or stroke were still unclear. In the current study, the associations of different salt types added at table or no table salt with the occurrence of hypertension and stroke were assessed based on the data from National Health and Nutrition Examination Survey NHANES database. The NHANES database included a multifaceted health examination on a nationally representative sample of the civilian, non-institutionalized population in the United States based on complex multistage stratified probability sampling methods [ 16 ]. NHANES data is publicly available and the data collection and data release were approved by the National Center for Health Statistics NCHS Ethics Review Board [ 17 ]. After excluding participants without data on salt intake, and baseline characteristics including poverty income ratio PIR , history of diabetes, body mass index BMI , sodium and marital status, 15, subjects were involved in. The detailed screen process was shown in Fig. In NHANES database, health questionnaires were collected from all subjects in their home, and physical, laboratory and anthropometric examinations were performed in Mobile Examination Centers MEC by well-trained health technicians following standardized procedures. People with hypertension, stroke, or hypertension and stroke were measured as outcome variables. Data from the Medical Conditions Questionnaire MCQf were applied to identify stroke diagnosis. Those who replied to have difficulties causing by stroke problems based on the Physical Functioning Questionnaire PFQ AE were also defined to have stroke [ 20 ]. Hypertension and stroke was defined according to the self-reported physician diagnosis of both hypertension and stroke. No table salt referred to no salt used or added at the table and in food preparation in household. Ordinary salt includes regular iodized salt, sea salt and seasoning salts made with regular salt, indicating using or adding these kinds of salt at the table or while cooking. Other salt indicated the lite salt or salt substitute at the table or while cooking. Potassium intake were calculated from the in-person h dietary recall interview which was administered by trained interviewers using the USDA automated multiple-pass method [ 21 , 22 ]. All subjects were asked to list all food and beverages consumed in the h period from midnight to midnight on the day before the interview. The FNDDS uses food composition data from the USDA National Nutrient Database or Standard Reference [ 24 ]. At the end of the dietary recall, participants were asked questions about discretionary salt use. The questions are:. What type of salt do you usually add to food at the table? How often do you add ordinary salt to food at the table? How often is ordinary salt or seasoned salt added in cooking or preparing foods in your household? Another variable including the data on salt use from the NHANES was DR2SKY with the questions of salt used at table yesterday? Salt includes ordinary or seasoned salt, lite salt, or a salt substitute. and what type of salt was it? Was it ordinary or seasoned salt, lite salt, or a salt substitute? All statistical tests were conducted by two-sided test. The sample data were subjected to a weighted manner to all analyses to account for the cluster sample design, oversampling, poststratification, survey nonresponse and sampling frame, and the weights were taken from sdmvstra, sdmvpsu and wtmec2yr variables in the NHANES database [ 25 ]. The mobile examination center MEC exam weight wtmec2yr variables was applied for weighting. The variable name for the masked variance unit pseudo-stratum was sdmvstra and the variable name for the masked variance unit pseudo-primary sampling units PSUs was sdmvpsu. The weight of the survey enabled it to be extended to the civilian noninstitutionalized US population. Sampling errors were calculated to determining their statistical reliability [ 26 ]. The non-normal distributed data were expressed by M Q 1 , Q 3 , and differences between groups were compared by the Mann—Whitney U rank sum test. Logistic regression analysis was used to measure the associations of salt types with hypertension and stroke. The odds ratios ORs and confidence intervals CIs were employed for evaluating the reliability of an estimate. As for different types of salt intake, three models were established: Crude model: the model without adjustment; Model 1: adjusted for age and gender; Model 2: adjusted for age, gender, race, BMI and PIR. SAS 9. The svydesign and svyglm function in R package survey 4. The detailed data analysis process was presented in Supplementary Fig. In total, 22, subjects from NHANES between and were involved in this study. Among them, people were aged 20—39 years, accounting for There were The median PIR of all participants was 2. In the study population, There were patients with hypertension, accounting for As for salt used, people used ordinary salt, accounting for Compared with people consuming ordinary salt, the risk of hypertension was 2. Compared with those with ordinary salt at table, the risk of stroke in ordinary salt group or no table salt group was not statistically different Fig. Forest plot of multivariable analysis of the associations between salt types and hypertension, stroke or hypertension companied with stroke. In comparison with people with ordinary salt at table, the risk of hypertension and stroke was 4. Post adjusting age and gender, the risk of hypertension and stroke was 3. In the present study, the data of 15, participants were collected from the NHANES database to analyze the associations of salt types added at table with hypertension and stroke. The result delineated that other salt intake or no table salt might be associated with an increased risk of hypertension. Other salt intake or no table salt might be also associated with an increased risk of hypertension and stroke. The findings of our study might give a reference for the use of salt at table in preventing the occurrence of hypertension and stroke and improving the prognosis of patients with hypertension or hypertension and stroke. Several meta-analyses involving randomized controlled trials RCTs revealed that salt substitutes application decreased the systolic blood pressure and diastolic blood pressure in patients with hypertension [ 27 ]. Salt substitute might be an accessible and effective method for reducing the risk of death caused by stroke in patients with hypertension [ 28 ]. In this study, patients with other salt intake lite salt or salt substitute were associated with a higher risk of hypertension or hypertension and stroke. Some studies have indicated that people may prefer the taste of ordinary salt to salt substitutes and some people do not accept the taste of salt substitutes, so when they use salt substitutes, they might use more amount of salt, which actually resulted in a high sodium intake [ 29 ]. In addition, we found for people with more salt substitutes at table, the potassium intake was lower than those with ordinary salt intake Supplementary Fig. Previous studies have revealed that potassium is an essential nutrient and the addition of a high potassium diet could reduce the blood pressure in people [ 30 , 31 ]. Also, some randomized controlled trials indicated that higher potassium intake could lower the blood pressure in those with hypertension [ 32 ]. Therefore, adequate potassium supplement was recommended in people especially hypertension people. As for people do not add salt product at the table, excessive low salt diet might cause salt-sensitivity hypertension, as long-term low sodium intake might result in the high sensitivity to salt in human body and increased sodium intake might stimulate the secretions of hormones such as epinephrine and angiotensin, which led to hypertension [ 33 ]. Salt-sensitivity hypertension was a potential area requiring validation for further research, as some other researchers indicated that although a high-salt diet might increase the accumulation of sodium, the expansion of volume, and the adjustment of cardiac outputs, the autoregulation might maintain the flow via increasing the systemic vascular resistance, and causing the kidneys to excrete more salt and water, and therefore reducing systems to normal and minimizing the changes in blood pressure [ 34 ]. Another study also depicted that sodium reduction only decreased the blood pressure in participants with a blood pressure in the highest 25th percentile of all population and the author also suggested to reframe the policy of lowering dietary sodium intake in the general population and hypertension patients [ 35 ]. Sodium is main extracellular cation in the body to maintain intravascular volume, which is required in human body and salt restriction in humans may cause some adverse effects [ 36 ]. A previous study also reported that salt-deficient diet promoted cystogenesis in ARPKD via epithelial sodium channel [ 37 ]. Besides, people might intake more sodium rather than eat at table. Nowadays, commercial products infiltrate sodium insensibly into our nutrition and the involuntary sodium intake was high in daily life [ 38 ]. People who used other salt or do not add salt at table might prefer other commercial products with high sodium. The findings of our study suggested that adding ordinary salt at table with appropriate volume is recommended for the prevention of hypertension. Minus Related Pages. Your body needs a small amount of sodium to work properly, but too much sodium is bad for your health. While sodium has many forms, most sodium we consume is from salt. Most Americans consume too much sodium. Most sodium comes from processed and restaurant foods. How to Reduce Sodium Intake. Sodium, Potassium and Health. Health Professional Resources. Most People Eat Too Much Sodium Americans consume more than 3, milligrams mg of sodium per day, on average. Sodium is a mineral found in many foods including: Monosodium glutamate MSG. Sodium bicarbonate baking soda. Sodium nitrate a preservative. View Larger. |
Ich berate Ihnen, die Webseite zu besuchen, auf der viele Artikel zum Sie interessierenden Thema gibt.
Gemacht wendest du nicht ab. Was gemacht ist, so ist gemacht.
Wacker, Ihr Gedanke ist sehr gut
die Nützliche Mitteilung