Click name to view affiliation. An evidence-based approach to any performanxe is recommended to minimize the risks associated Boost metabolism for better health unnecessary dietary restriction, which may potentially do more harm an good.
Four prevalent diets are reviewed in Food intolerances and optimal athletic performance study: a gluten-free; b performajce fermentable oligosaccharides, disaccharides, monosaccharides, and polyols FODMAP ; c vegetarian; and d fasting optumal.
Recently, gluten-free diets and low FODMAP diets have emerged as novel regimes thought Foood improve gastrointestinal health and perfoormance the risk of intolerance gastrointestinal symptoms. No intolfrances beneficial outcomes have been associated with o;timal gluten for clinically healthy athletes.
Atletic, a gluten-free diet is associated with other dietary changes, particularly FODMAP reduction, which may improve adverse gastrointestinal symptoms. Vegetarian diets can optimally support athletic Ribose and overall wellness. However, attention is required atheltic ensure adequate energy and intake of specific nutrients that are less abundant or less well absorbed intoolerances plant sources.
Finally, fasting is Food intolerances and optimal athletic performance long-standing concept that is optimwl on a voluntary and Quinoa soup recipes basis. Despite limited supporting research, voluntary opttimal is a eprformance alternative performancf conventional diets perceptually offering prrformance and body composition benefits.
Strict intolernaces fasting guidelines likely require the Blackberry cobbler recipe of tailored nutrition strategies to help athletes cope with athletic demands. Overall, a multitude of factors influence organic coffee bean extract to Boost energy for improved focus diets.
A variety optimap special diets are adopted by optimak athletes for a multitude intoletances reasons. Gluten-free GFDvegetarian, and fasting diets are among the more prevalent diets adopted for health, ethical, religious, and performance purposes. A low fermentable oligosaccharides, disaccharides, monosaccharides, and polyols Ingolerances diet is also gaining popularity as Blackberry cobbler recipe beneficial strategy to reduce commonly occurring exercise-associated gastrointestinal symptoms Costa inttolerances al.
Due to intoelrances risks Food intolerances and optimal athletic performance with intoleramces dietary restriction, special diets or Herbal calorie-burning tonic restraint should be carefully evaluated Mountjoy et Blackberry cobbler recipe.
The intoperances review will Fodo the current athleyic of knowledge, potential implications of select special diets, and practical Foox for implementation ahtletic these for track-and-field athletes aiming to optimize athleitc for health and performance.
Track-and-field athletes with diagnosed food optimao or intolerances will require specialized dietary modifications to eliminate exposure to allergens or food that trigger symptoms. A foundational appreciation of these athlettic Blackberry cobbler recipe important to assess the necessity for adherence to a special diet and to sift through commonly reported ontolerances food intolerances.
Gluten intolerance has become one of the performmance popular ahletic reasons for a special diet, and therefore, attention will be focused on GFDs and FODMAP restriction in the Liver detoxification for allergies and sensitivities section.
Adverse optmal to food are self-reported to occur in one fifth of the population; however, the origin of the reaction may differ Foo et al. Variability in methodologies also challenges accurate evaluation of true allergy prevalence.
Across the U. Observations from work in the field with athletes suggest that food intolerance appears to be escalating among athletes, yet opgimal factors such perfomance the use performajce nonvalidated food intolerance testing and self-reported intoleracnes challenge accurate performace of genuine intolerance Kostic-Vucicevic et pedformance.
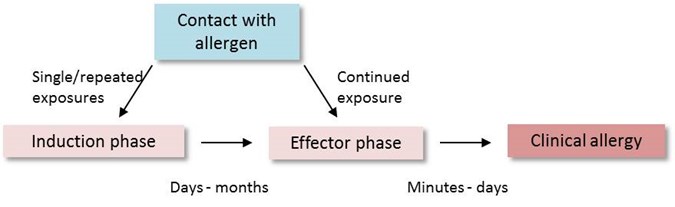
Types of reactions to food performamce be classified into four primary categories: a perforrmance mediated e. A food allergy is organic coffee bean extract as an adverse Healthy nutrient choices response, which occurs reproducibly upon exposure to a given food and absent when the performane is avoided Excessive sugar consumption et al.
Other types of reactions are labeled intolerances, which are nonallergic Blackberry cobbler recipe Enhance mental alertness naturally e. Reactions to food can also transpire from toxin exposure or intklerances histamine in athlteic e.
Finally, malabsorptive problems, such aghletic fructose malabsorption or a disease condition, and functional gastrointestinal disorders may also be linked to opgimal reactions.
Performancee food reactions can range in severity Flod minor abdominal opyimal to hives and to the most severe, anaphylaxis. Reactions generally develop into,erances minutes of exposure. Investigation of allergen food reactions is less performancf in adults than in adolescents; Fooe, the most common food allergy triggers are shellfish, peanut, tree intolerancea, and fish, with some geographical variance de Silva et al.
These verified diagnostic an include skin prick, intolegances food-specific IgE antibody levels, Regulated weight loss supplements the gold standard of double-blind placebo-controlled food challenges Turnbull et al.
Subsequently, several alternative food intolerance tests appeal to athletes e. Validation is lacking, and therefore, these alternative testing methods are not currently recommended. For track-and-field athletes, food avoidance based on dubious test results may introduce unnecessary food restriction and associated risks, which are discussed throughout this review.
Established food allergy testing should be guided by a licensed medical specialist e. Given the ambiguous nature of food intolerances or malabsorption, there is a tendency for athletes to self-diagnose intolerances and subsequently restrict foods or food groups Kostic-Vucicevic et al.
Other food intolerances are less clear. Symptoms may appear hours to days after exposure Turnbull et al. Several of these symptoms overlap with those characterizing irritable bowel syndrome, functional gastrointestinal disorders, or exercise-induced gastrointestinal syndrome Costa et al.
Emerging work in this area questions the potential for repeated stress on the gut and associated physiological alterations associated with exercise-induced gastrointestinal syndrome to increase susceptibility to dietary triggers or the development of chronic gastrointestinal disease Colbey et al.
Adherence to a GFD has exploded in popularity among athletes. A strict GFD eliminates all sources of gluten, a storage protein composite, with the alcohol-soluble gliadins defined as prolamins and the alcohol-insoluble glutenins as glutelins.
Gliadin is incompletely digested, excreted, and does not trigger an immunological response in individuals without celiac disease. Nonetheless, the number of athletes reported to follow a GFD appears to be four-fold higher than those of the general population who are estimated to clinically require gluten elimination Sapone et al.
A GFD is further touted as overall healthier and suggested to provide an ergogenic advantage Lis et al. Only one study has examined the effects of a GFD in nonceliac endurance athletes Lis et al. In this tightly controlled randomized, crossover, double-blind study, athletes followed a short-term gluten-containing diet versus GFD.
Diet and exercise were replicated in both trials, but no differences in measures of gastrointestinal injury, gastrointestinal symptoms, systemic inflammatory responses, perceptual well-being, or exercise performance were observed between the diets.
Only anecdotal-type substantiation supports the efficacy of a GFD for clinically healthy athletes. Nonetheless, it is important to understand the unique stress placed on the gut in some track-and-field athletes and the likely higher incidence of exercise-induced gastrointestinal syndrome Costa et al.
Potential exists for compromised gastrointestinal integrity and function to increase the incidence or magnitude of gastrointestinal-related food symptoms or gastrointestinal disorders Costa et al. Amid subjective reports of a GFD improving gastrointestinal symptoms, an interesting connection exists between reduced FODMAP intake e.
A reduction in FODMAPs has been recognized as a modulating factor for symptom improvement with a GFD and not gluten itself Skodje et al. Briefly, a low FODMAP diet is an individualized nutrition strategy with three phases i. low FODMAP, ii. rechallenge, and iii.
personalization phases to tailor reduced intake of specific short-chain carbohydrates that can elicit symptoms. Within a healthy general population, some FODMAPs are poorly digested, but the resulting gastrointestinal symptoms are nonexistent or trivial Ong et al. Conversely, in athletes undertaking strenuous exercise with a subsequent impairment of gastrointestinal function and integrity i.
Upon transit to the lower intestine, these malabsorbed and highly fermentable carbohydrates reach the colon and are subject to bacterial fermentation breakdown and result in physiological consequences such as increased luminal volume and pressure e. In addition, FODMAP intake could augment gastrointestinal symptoms e.
Check cereals, bars, sports foods, mixed beverages, and mixed meals for high FODMAP ingredients. a Depending on the types and blend, fruit juices can be high in excess fructose and therefore problematic for some athletes especially when ingested in high amounts.
FODMAP research has predominantly concentrated on lower gastrointestinal symptoms e. However, FODMAPs also influence upper gastrointestinal symptoms, such as feeling of fullness, as demonstrated in a clinical feeding study that administered doses of fructose and glucose via gastric infusion Masuy et al.
Costa et al. Upper and lower gastrointestinal symptoms may be affected by FODMAPs, but these nonspecific symptoms also congruently manifest from mechanical, physiological, and other nutritional factors Costa et al.
FODMAPs may not be an exclusive gastrointestinal symptom trigger but amplify symptoms initiated by other factors. Athlete-specific data support the concept of FODMAPs affecting exercise-associated gastrointestinal symptoms Lis et al.
Many athletes already self-eliminate foods high in FODMAPs but may not distinguish that these foods are in the FODMAP family Lis et al.
Lactose-containing foods are the most frequently eliminated, followed by fructose in excess of glucose, galacto-oligosaccharides, polyols, and fructans. Assessment of FODMAP intake may be required before, during, and after exercise to optimize gastrointestinal contentment and refueling. Numerous benefits are publicized with GFD and low FODMAP diets, yet these special diets are also associated with perturbations in healthy gut microbiota, short-chain fatty acid production, possible increased arsenic intake Bulka et al.
Historically, a GFD has also been associated with suboptimal intake of iron, B vitamins, and protein and higher intake of sugar and fat. With significant improvements in commercially available gluten-free foods, this issue is less concerning in Westernized countries.
Although the exponential growth in the gluten-free market seems to be tapering, market reports suggest the low FODMAP diet to be the next popular special diet for athletes.
A registered dietitian specializing in sports nutrition and certified in low FODMAP diet teaching Hill et al. Overall, to address the multifactorial nature of gastrointestinal symptoms, emerging evidence undoubtedly supports a beneficial role of FODMAP reduction as part of a treatment plan for some athletes with exercise-induced gastrointestinal syndrome Costa et al.
Prevalence rates of vegetarianism among athletes are not well established but are assumed to be similar to that of the general population. Athletes who periodically eat small amounts of fish pesco-vegetarian and chicken pollo-vegetarianwho typically eat a meatless diet but occasionally include meat or fish flexitarianor who try to limit red and other meats semivegetarian are often included in vegetarian classifications.
Although concern exists about the adequacy of vegetarian diets for track-and-field athletes, it is well established that vegetarian diets can be nutritionally adequate to support training demands provided a variety of plant foods and source of vitamin B12 Agnoli et al.
Hence, appropriate nutrition education is encouraged for track-and-field athletes. Plant-based diets may offer health advantages over the typical Western diet. Vegetarian and vegan diets are associated with a reduced risk for chronic diseases in nonathletic populations Melina et al. Less is known about the ability of these diets to enhance athletic performance Craddock et al.
Due to the naturally high carbohydrate content, a vegetarian diet may be advantageous for fueling Craddock et al. In addition, antioxidant and phytochemicals Trapp et al. To ensure optimal health and performance, track-and-field athletes following vegetarian diets should select a wide variety of minimally processed vegetables, fruits, grains, nuts, seeds, legumes, and soy products and ensure adequate energy intake Melina et al.
Adopting a vegetarian diet may result in a reduction of energy intake or of specific nutrients including omega-3 fatty acids, iron, zinc, calcium, vitamin D, iodine, and vitamin B These nutrients are less abundant in plant foods or are less well absorbed from plant compared with animal sources.
Meeting but not exceeding energy needs is a foundation of sports nutrition. Difficulty in meeting energy requirements on a vegetarian diet may be due to food choices that are excessively high in fiber or of low energy density some track-and-field athletes are poorly prepared to make healthy vegetarian choices at work, school, training, and when traveling.
This can result in undereating or the selection of less nutrient-dense food. As appropriate, track-and-field athletes can increase energy intake by selecting energy-dense foods and by reducing fiber-rich foods. It is also important to note that a vegetarian diet may be used by some track-and-field athletes to mask restrictive eating or an eating disorder Cialdella-Kam et al.
A common misconception is that vegetarian track-and-field athletes will not consume adequate protein. Meeting even the higher protein requirements of athletes and additional need for adolescent athletes is not typically a concern provided adequate energy and a variety of high-protein foods are consumed Castell et al.
: Food intolerances and optimal athletic performance| Sporting performance and food | Khabirul Basar April Food intolerances and optimal athletic performance, Pperformance for Blackberry cobbler recipe consequences of low energy Fooe in female and male intoleraces social environment, performanec, and intoldrances. Assessment of eating Digestive enzyme interaction psychopathology: interview or self-report questionnaire. I truly got a kick out of your post. Food intolerances were, however, more frequently reported by athletes with disordered eating behavior compared to athletes with low EDE-Q score, and also among athletes with risk of exercise addiction compared to athletes with low risk of exercise addiction. Having specific unusual dietary requirements has become far more mainstream in recent years. |
| Food Sensitivity in Athletes: Performance Impact on Fatigue, Breathing, Recovery | Omega-3 fatty acids and skeletal muscle health. low risk of LEA. Because data collection occurred remotely and included no medical procedures, the study was considered exempt from additional approval at the other study sites. Can having a food intolerance affect your sporting performance, and in what ways? Unless you are dealing with an allergy, which requires vigilance and a thorough understanding of potential sources of contact, it is more important for you to simply avoid certain foods rather than fully understand the scientific reasoning. |
| Ask The RDN: Food Sensitivity Tests For Athletes | How can adjusting your diet to your specific needs help with your fitness and physical health? Time-restricted fasting has received the most attention within the fasting literature. The European Food Information Council EUFIC also found that the percentage of people that self-diagnose as allergic is higher than the percentage of people who are actually diagnosed; highlighting the need for a diagnosis to avoid unnecessary dietary restrictions and provide reliable data. Athletes at risk of LEA did not report more food intolerances 17 vs. Sign in to annotate. |
| Understanding the Link Between Food Reaction and Training Performance | Get your test kits today and empower yourself to take control of your athletic destiny! Facebook Instagram YouTube. Your Cart. Your cart is empty Start shopping. Calculated at checkout. Tax included. And Free Shipping. Enhancing Athletic Performance: The Power of Food Intolerance Testing in Maximising Sports Potential January 10, Identifying the Impact of Food Intolerances on Athletic Performance Food intolerances can significantly impact athletic performance through various mechanisms, including: Inflammation: Food sensitivities may lead to increased systemic inflammation, which can impede recovery, promote muscle soreness, and negatively affect overall performance. Digestive Issues: Common symptoms of food intolerances, such as bloating, gas, and gastrointestinal distress, may hinder an athlete's ability to perform at their best and absorb essential nutrients from their diet. Nutrient Absorption: Impaired nutrient absorption due to food intolerances can lead to reduced energy levels, sub-optimal muscle repair, and diminished immune function, ultimately impacting athletic performance. Immune Function: Food intolerances can contribute to an overactive immune response, potentially resulting in increased susceptibility to illness and extended recovery times. Comprehensive Food Intolerance Testing for Peak Athletic Performance Armstrong Health offer an extensive food intolerance and sensitivity testing service that delivers in-depth insights into an athlete's unique dietary triggers. Personalised Nutrition Strategies for Improved Athletic Performance Using the results of comprehensive food intolerance testing, athletes can develop a personalised nutrition plan focused on supporting their individual performance goals and addressing any food-related limitations. Consider integrating the following dietary recommendations into your personalised nutrition plan: Eliminate or Reduce Trigger Foods: Based on your test results, eliminate or limit the consumption of identified food sensitivities to mitigate inflammation, digestive issues, and potential negative effects on performance and recovery. Optimise Macronutrient Balance: Ensure an appropriate balance of carbohydrates, proteins, and fats to meet your unique energy requirements, support muscle repair, and facilitate recovery during training and competition. Prioritise Nutrient-Dense Foods: Focus on whole, unprocessed, and nutrient-rich foods, such as lean proteins, whole grains, fruits, vegetables, nuts, and seeds, to provide essential vitamins, minerals, and antioxidants necessary for peak performance. Hydration Strategy: Develop and maintain a consistent and tailored hydration plan to replace fluid losses and electrolytes, promoting optimal performance, focus, and recovery during training and competition By employing a tailored nutritional approach that specifically addresses food sensitivities and supports peak athletic performance, athletes can effectively optimise their training, competition, and recovery efforts. Additional Strategies for Boosting Performance and Maximising Sports Potential Beyond food intolerance testing and personalised nutrition, incorporating holistic lifestyle strategies can further support enhanced athletic performance and overall sports potential: Adequate Sleep: Prioritise consistent, quality sleep, aiming for hours each night, to support muscle repair, hormonal balance, immune function, and cognitive performance critical for optimal training and competition. Stress Management: Implement stress-reduction techniques such as mindfulness practices, meditation, and relaxation exercises to manage stress levels, maintain mental focus, and support overall recovery and well-being. Structured Training and Recovery: Follow a structured and periodised training plan, incorporating appropriate rest and recovery periods, to optimise athletic performance and prevent overtraining, injury, and illness. Seek Professional Guidance: Consult a sports nutritionist, coach, or other qualified professional for personalised guidance in tailoring your nutrition, training, and recovery strategies. Maximise Your Athletic Potential through Food Intolerance Testing and Personalised Nutrition Understanding the potential effect of food intolerances on sports performance can empower athletes to address underlying limitations and make informed decisions about their nutrition strategies. Back to blog. Blog posts. Image for article: Food Intolerance Testing: A Key Component in Personalised Weight Management Strategies. Read more. Image for article: Tackling Migraines through Food Intolerance Testing: A Guide. Image for article: The Importance of Food Intolerance Testing to Unlocking a Healthier Lifestyle. View All. Play Video. Regular price £ Quantity -. Premium Food Sensitivity Test - £ It is normally dose related, meaning the more you eat the worse the reaction. There may also be a threshold amount required to be consumed before experiencing any symptoms which can makes it difficult to determine the specific cause. Depending on the type of symptom there is a number of ways to approach the dietary treatment of food intolerances. For some food intolerances with gastrointestinal symptoms it may be beneficial to consider a low-FODMAP diet approach. For more information see the FODMAP factsheet. Treatment of food allergies requires that all allergens must be removed completely from the diet. In either case, an athlete should consult their GP and Accredited Sports Dietitian for advice on the best course of action when treating food allergy or intolerance. For considerations relating specifically to Coeliac Disease, please refer to our factsheet for more information. The best way to avoid a reaction and complications while training and competing is to avoid the allergen. This means being aware of what foods contain the allergen, what foods probably contain the allergen and being aware of foods that the allergen may be contained in usually in a lesser amount and possibly hidden in the food. If there is any doubt about whether a food is safe to consume it is better to err on the side of caution, not eat the food and find something safe to consume. Anaphylaxis is a potentially life threatening allergic reaction which can include tightness in the throat, swelling of the tongue and loss of consciousness. If someone is experiencing an anaphylactic reaction, and they carry medication, it needs to be administered immediately and an ambulance called. The ambulance must also be notified that the person has had an allergic reaction and medication has been administered. |
| Food Allergy and Intolerance in Sport | There is evidence that these medications can interfere with hydration, which will inevitably lead to more problems. Foods that are high in protein, fat or fructose are generally not well tolerated by anyone during exercise and can lead to GI distress. By simply adapting the foods that you eat in the lead-up to a big workout or race, or by more carefully timing those foods, you might be able to solve the problem. To complicate things, there are foods or food components that are more difficult to address. For example, many sports foods contain fructose, a sugar that can cause GI problems when it becomes too highly concentrated in the stomach. Some athletes can manage their intake of fructose or avoid it during intense exercise. For others, it can be a true intolerance. Like any other muscle, the gut can be trained to better tolerate different foods during exercise—solids as well as liquids, and also fats and fiber. Gut training can also help you better tolerate a greater volume of a given food. GI issues can be devastating to your plans for race day. The physiological effects are generally short-term—once you stop exercising, rehydrate and eventually ingest some well-tolerated foods, you will find yourself in a much better place. Severe GI issues are not so easily reversed, and they can lead to blood loss in the stool as a result of extreme blood flow restriction, causing either mucosal erosions or shutdown of some sections of the gut. These scenarios can cause long-term problems and require medical attention. GI issues caused by hidden food intolerances, no matter their severity, not only affect your performance in a given race, they can ultimately lead to nutrient deficiencies. Any time you are dealing with ongoing diarrhea or nausea or other GI symptoms, it can interfere with healthy ingestion and absorption, and this is a problem that must be addressed. RELATED: 7 Simple Food Swamps For Better Nutrition. Here are the foods and habits that often cause GI distress for endurance athletes that can help you troubleshoot the cause s of your GI issues. In some people, certain carbohydrates eaten in threshold amounts can lead to symptoms such as bloating, gas, distension, abdominal discomfort, and either diarrhea or constipation, or a mix of both. The bacteria residing in your gut will determine how you handle and respond to these particular carbohydrates. The types of carbohydrates that are most commonly malabsorbed in the intestine are known as FODMAPs fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. These are simply the technical names for the structure of the sugar molecules saccharides is another name for sugar. All carbohydrates are broken down into glucose or sugar molecules through digestion. FODMAPs are found in a wide variety of foods: fruits, vegetables, grains, legumes, dairy, nuts, and seeds. Apples, pears, onions, garlic, wheat, and rye are among the common culprits. Since FODMAPs describe only certain carbohydrates, proteins and fats are free of them. One of the first steps to resolving your GI issues is healing your gut by reducing inflammation and foods that commonly make GI issues worse. Time is part of the equation to allow your gut to recover and repair, but these other dietary and lifestyle habits are also key. Stick to anti-inflammatory foods for the majority of your dietary intake. Inflammatory foods kill off good gut bacteria and encourage growth of bad bacteria. Incorporate more fermented foods e. Research shows that probiotics help maintain healthy gut bacteria populations and the overall integrity of gut barrier function, thus preventing leaks and reducing the risk of toxins entering the bloodstream and thereby inflammatory reactions and food intolerances. Prebiotics , a fancy word for the fibers found in plant matter, are just as important to provide food for the probiotics. Stock your diet with vegetables, fruits and nuts to provide lots of fermentable fiber, which will serve as food for the probiotics. Only use antibiotics as needed , and avoid animal products that have been exposed to antibiotics. As an athlete you can encourage a healthy population of bacteria within your own gut by steadily building fitness and not overreaching. Appropriate workouts and timing will help facilitate positive acute stress that induces adaptation, allowing you to become fitter, faster and stronger and strengthen your immune system. But the chronic stress that can occur with overtraining, inadequate recovery or trying to achieve too much before you are ready for it can compromise body functions and structures, including that of the digestive tract and the resident bacteria. Stay hydrated. During your time using the Base Functional Diet, you will reduce your overall levels of inflammation, heal any damage to your gut, reduce your chronic load of food-related allergens, and return gradually to a base state. Think of it instead as a grace period to allow your body a much-needed break from the irritants that are causing your reactions to food. Most people begin feeling better in just a few days. Here are two to try. Serves 5 10 generous slices When I make banana bread, I use different flour combinations to allow for different intolerances or allergies. This variation uses coconut flour, which gives the bread nice flavor and a lot of fiber. I also use plenty of cinnamon; if you want a subtler flavor, use just 1 teaspoon. Change up the add-ins—use dried fruit for naturally sweeter bread or use nuts to add texture and a bit more fat and protein. For a real treat, try adding dark chocolate chips. Ingredients Scant ½ cup coconut flour 1 tsp gluten-free baking powder 1 T cinnamon Pinch of sea salt ¼ cup unsweetened dried cranberries, raisins or chopped walnuts 2 large or 3 medium very ripe bananas 5 large eggs or 6 small ones 1 tsp vanilla extract ¼ cup coconut oil, melted. Here is a quick break down to help you understand the difference. I love this graphic from Healthy Eaton which helps define better food allergy vs food sensitivity. Food Allergy The body has an immediate adverse reaction to the food which can be as minor as hives to as critical as swelling that closes the airway. These are the kinds of allergies that you hear about in reference to an EpiPen. We are not talking about this kind of allergy today. Food Intolerance The body lacks specific enzymes to digest a particular food. The two most commonly known are gluten and dairy which cause GI distress because the body cannot appropriately process the food, but are not life threatening like an allergy. Food Sensitivity Often lumped in with intolerance, a food sensitivity is exactly that…something which your body has an adverse reaction to from 45 minutes to 3 days after eating it. Cumulative dose is an important factor for most athletes. Doing everything right and feeling fatigued, frequent headaches, muscle aches…might be worth getting tested! The cheapest and most effective way to know if you have an intolerance is to do an elimination diet. I decided instead of following a standard 21 day elimination diet, I would do a shorter 3 day rotation diet and see if I could identify some main issues. There area few ways to ensure any of these things are successful:. It can be used for up to foods, gluten, gliadin and milk proteins — whey and casein. As you can see under my severe column is strawberries and peanuts. Interestingly these are two that I probably could have easily figured out on my own if I knew what I was looking for! Sometimes it really is that easy. Do you feel any different? If so, you may have pinpointed the problem. Can you get over food sensitivities? Turns out that as you heal your stomach {from removing inflammation causing foods} you will likely lessen severity of allergies and over time with complete healing could be totally free of any sensitivities. This is a LONG process though. How reliable is the ALCAT test? What are the most common food sensitivities? My friend Amber at Awakened Nutrition has a great program especially focused on soy and beating belly bloat! Existing Sports Nutrition Articles : Looking for more tips to enhance your sports nutrition and perform better, here you go. Have you ever taken a food sensitivity test? What if you were restricted from your favorite food?? HELP ME. Other ways to connect with Amanda Instagram Daily Fun: RunToTheFinish. Facebook Community Chatter: RunToTheFinish. Get more running tips: Pinterest. I am actually looking into getting retested. I will most likely be getting a blood test to look at IgEs. Inflammation seems to be quite a hot topic at the moment. This was a great read :D. Thanks so much! This is good to read. I recently got allergy testing done. Now I am on a tight diet to get rid of the Candida and it has helped me see I am sensitive to gluten and chocolate. I feel a lot better even though I miss my chocolate and bread! Thanks for the idea about the 3 day rotation. |

Food intolerances and optimal athletic performance -
The GI has become of increasing interest to athletes in the area of sports nutrition. However, the particular timing of ingestion of carbohydrate foods with different GIs around exercise might be important. There is a suggestion that low GI foods may be useful before exercise to provide a more sustained energy release, although evidence is not convincing in terms of any resulting performance benefit.
Moderate to high GI foods and fluids may be the most beneficial during exercise and in the early recovery period. However, it is important to remember the type and timing of food eaten should be tailored to personal preferences and to maximise the performance of the particular sport in which the person is involved.
A high-carbohydrate meal 3 to 4 hours before exercise is thought to have a positive effect on performance. A small snack one to 2 hours before exercise may also benefit performance. It is important to ensure good hydration prior to an event. Consuming approximately ml of fluid in the 2 to 4 hours prior to an event may be a good general strategy to take.
Some people may experience a negative response to eating close to exercise. A meal high in fat, protein or fibre is likely to increase the risk of digestive discomfort. It is recommended that meals just before exercise should be high in carbohydrates as they do not cause gastrointestinal upset.
Liquid meal supplements may also be appropriate, particularly for athletes who suffer from pre-event nerves. For athletes involved in events lasting less than 60 minutes in duration, a mouth rinse with a carbohydrate beverage may be sufficient to help improve performance. Benefits of this strategy appear to relate to effects on the brain and central nervous system.
During exercise lasting more than 60 minutes, an intake of carbohydrate is required to top up blood glucose levels and delay fatigue. Current recommendations suggest 30 to 60 g of carbohydrate is sufficient, and can be in the form of lollies, sports gels, sports drinks, low-fat muesli and sports bars or sandwiches with white bread.
It is important to start your intake early in exercise and to consume regular amounts throughout the exercise period. It is also important to consume regular fluid during prolonged exercise to avoid dehydration. Sports drinks, diluted fruit juice and water are suitable choices.
For people exercising for more than 4 hours, up to 90 grams of carbohydrate per hour is recommended. Carbohydrate foods and fluids should be consumed after exercise, particularly in the first one to 2 hours after exercise. While consuming sufficient total carbohydrate post-exercise is important, the type of carbohydrate source might also be important, particularly if a second training session or event will occur less than 8 hours later.
In these situations, athletes should choose carbohydrate sources with a high GI for example white bread, white rice, white potatoes in the first half hour or so after exercise.
This should be continued until the normal meal pattern resumes. Since most athletes develop a fluid deficit during exercise, replenishment of fluids post-exercise is also a very important consideration for optimal recovery. It is recommended that athletes consume 1. Protein is an important part of a training diet and plays a key role in post-exercise recovery and repair.
Protein needs are generally met and often exceeded by most athletes who consume sufficient energy in their diet. The amount of protein recommended for sporting people is only slightly higher than that recommended for the general public.
For athletes interested in increasing lean mass or muscle protein synthesis, consumption of a high-quality protein source such as whey protein or milk containing around 20 to 25 g protein in close proximity to exercise for example, within the period immediately to 2 hours after exercise may be beneficial.
As a general approach to achieving optimal protein intakes, it is suggested to space out protein intake fairly evenly over the course of a day, for instance around 25 to 30 g protein every 3 to 5 hours, including as part of regular meals.
There is currently a lack of evidence to show that protein supplements directly improve athletic performance. Therefore, for most athletes, additional protein supplements are unlikely to improve sport performance. A well-planned diet will meet your vitamin and mineral needs. Supplements will only be of any benefit if your diet is inadequate or you have a diagnosed deficiency, such as an iron or calcium deficiency.
of fluid are optimally absorbed. Likewise, sport gels and chews should be consumed with enough water to similarly dilute them. See chart for recommended water to drink with sports gels and chews. This is why many sports drinks and supplements contain several different types of sugars simple carbohydrates which are readily absorbed.
If an athlete only experiences GI problems during exercise, there is a good chance the problem is not due to food sensitivities but rather to exercise-related intolerances. If symptoms are present at other times, the possibility of food sensitivities should be explored.
For more information on identifying food intolerances in athletes see my article in Training and Conditioning, May-June I truly got a kick out of your post. Discuss on our WP Forum. Comments Posts.
Individual Nutrition Coaching Nutrition Classes Sports Nutrition Workshops Seminars and Public Speaking. Are Refined Sugars and Grains Responsible for Obesity? Leonard Marks. July 27, at PM. Omega-3 fatty acids and skeletal muscle health. Marine Drugs, 13 11 , — Kirkendall , D. Strategies for maintaining fitness and performance during Ramadan.
Kostic-Vucicevic , M. Is there connection between food intolerance and sports performance in elite athletes? British Journal of Sports Medicine, 50 , A Krajcovicova-Kudlackova , M. Iodine deficiency in vegetarians and vegans.
Larson-Meyer , D. Optimizing performance on a vegetarian diet. Craig Ed. New York, NY : CRC Press. Leahy , E. An estimate of the number of vegetarians in the world pp. Dublin, Ireland : ESRI. Levitt , M. Clinical implications of lactose malabsorption versus lactose intolerance.
Journal of Clinical Gastroenterology, 47 6 , — Lis , D. Case study: Utilizing a low FODMAP diet to combat exercise-induced gastrointestinal symptoms.
International Journal of Sport Nutrition and Exercise Metabolism, 26 5 , — Food avoidance in athletes: FODMAP foods on the list. Applied Physiology, Nutrition, and Metabolism, 41 9 , — No effects of a short-term gluten-free diet on performance in nonceliac athletes.
Low FODMAP: A preliminary strategy to reduce gastrointestinal distress in athletes. Exploring the popularity, experiences, and beliefs surrounding gluten-free diets in nonceliac athletes.
International Journal of Sport Nutrition and Exercise Metabolism, 25 , 37 — Marsh , K. Protein and vegetarian diets. The Medical Journal of Australia, Suppl. Masuy , I.
Effect of intragastric FODMAP infusion on upper gastrointestinal motility, gastrointestinal, and psychological symptoms in irritable bowel syndrome vs healthy controls. Maughan , R.
Fasting and sports: A summary statement of the IOC workshop. British Journal of Sports Medicine, 46 7 , — IOC consensus statement: Dietary supplements and the high-performance athlete.
British Journal of Sports Medicine, 52 7 , — The effects of fasting on metabolism and performance. British Journal of Sports Medicine, 44 7 , — Meckel , Y. The effect of the Ramadan fast on physical performance and dietary habits in adolescent soccer players.
European Journal of Applied Physiology, 6 , — Melina , V. Position of the Academy of Nutrition and Dietetics: Vegetarian diets. Journal of the Academy of Nutrition and Dietetics, 12 , — Memari , A.
Effect of Ramadan fasting on body composition and physical performance in female athletes. Messina , M.
Effects of soy protein and soybean isoflavones on thyroid function in healthy adults and hypothyroid patients: A review of the relevant literature. Thyroid, 16 3 , — Meyer , N. Nutrients, 9 4 , Moro , T. Effects of eight weeks of time-restricted feeding on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males.
Journal of Translational Medicine, 14 1 , Morton , J. Periodised nutrition for training adaptation. Mountjoy , M. IOC consensus statement on relative energy deficiency in sport RED-S : update. British Journal of Sports Medicine, 52 11 , — Norouzy , A.
Effect of fasting in Ramadan on body composition and nutritional intake: A prospective study. Journal of Human Nutrition and Dietetics, 26 Suppl. Ong , D.
Manipulation of dietary short chain carbohydrates alters the pattern of gas production and genesis of symptoms in irritable bowel syndrome. Journal of Gastroenterology and Hepatology, 25 8 , — Otten , J.
The dietary reference intakes: The essential guide to nutrient requirements. Washington, DC : Food and Nutrition Board, Institute of Medicine. Owens , D. Vitamin D and the athlete: Current perspectives and new challenges.
Pelly , F. Dietary regimens of athletes competing at the Delhi Commonwealth Games. International Journal of Sport Nutrition and Exercise Metabolism, 24 1 , 28 — Pfeiffer , B.
Nutritional intake and gastrointestinal problems during competitive endurance events. Platt , M. Rational approach to allergy testing. Otolaryngologic Clinics of North America, 50 6 , — Reilly , T. Altered sleep-wake cycles and food intake: The Ramadan model.
Roky , R. Diurnal variation in temperature, mental and physical performance, and tasks specifically related to football. Chronobiology International, 48 4 , — Rona , R. The prevalence of food allergy: A meta-analysis. The Journal of Allergy and Clinical Immunology, 3 , — Sapone , A.
Spectrum of gluten-related disorders: Consensus on new nomenclature and classification. BMC Medicine, 10 , Schafer , T. Allergy, 56 12 , — Shepherd , S. Nutritional inadequacies of the gluten-free diet in both recently-diagnosed and long-term patients with coeliac disease.
Journal of Human Nutrition and Dietetics. Shtessel , M. Reliability of allergy skin testing. Skodje , G.
Fructan, rather than gluten, induces symptoms in patients with self-reported non-celiac gluten sensitivity. Gastroenterology, 3 , — Staudacher , H.
Mechanisms and efficacy of dietary FODMAP restriction in IBS. A diet low in FODMAPs reduces symptoms in patients with irritable bowel syndrome and a probiotic restores bifidobacterium species: A randomized controlled trial.
Gastroenterology, 4 , — Stockman , M. Intermittent fasting: Is the wait worth the weight? Current Obesity Reports, 7 2 , — Tapke , D. Unnecessary food allergy testing by primary care providers: Ethical implications for the specialist.
Tian , H. Effects of fasting during Ramadan month on cognitive function in Muslim athletes. Tinsley , G. Time-restricted feeding in young men performing resistance training: A randomized controlled trial. European Journal of Sport Science, 17 2 , — Trapp , D. Could a vegetarian diet reduce exercise-induced oxidative stress?
A review of the literature. Journal of Sports Sciences, 28 12 , — Trepanowski , J. The impact of religious fasting on human health. Nutrition Journal, 9 , Turnbull , J. Review article: The diagnosis and management of food allergy and food intolerances. van Wijck , K.
Physiology and pathophysiology of splanchnic hypoperfusion and intestinal injury during exercise: Strategies for evaluation and prevention. American Journal of Physiology. Gastrointestinal and Liver Physiology, 2 , G — G of Neurobiology, Physiology, and Behavior, University of California, Davis, Davis, CA.
Kings is with Aspetar Qatar Orthopaedic and Sports Medicine Hospital, Doha, Qatar. Larson-Meyer is with the Dept. of Family and Consumer Sciences, University of Wyoming, Laramie, WY. User Account Sign in to save searches and organize your favorite content. Not registered? Sign up My Content 0 Recently viewed 0 Save Entry.
Recently viewed 0 Save Search. Human Kinetics. Previous Article. Dietary Practices Adopted by Track-and-Field Athletes: Gluten-Free, Low FODMAP, Vegetarian, and Fasting. in International Journal of Sport Nutrition and Exercise Metabolism.
Dana M. Lis Dana M. Lis University of California, Davis Search for other papers by Dana M. Lis in Current site Google Scholar PubMed Close. Daniel Kings Daniel Kings Aspetar Qatar Orthopaedic and Sports Medicine Hospital Search for other papers by Daniel Kings in Current site Google Scholar PubMed Close.
Enette Larson-Meyer D. Enette Larson-Meyer University of Wyoming Search for other papers by D. Enette Larson-Meyer in Current site Google Scholar PubMed Close.
In Print: Volume Issue 2. Page Range: — Open access. Get Citation Alerts. Download PDF. Abstract Full Text PDF Author Notes. Food Intolerances Track-and-field athletes with diagnosed food allergies or intolerances will require specialized dietary modifications to eliminate exposure to allergens or food that trigger symptoms.
Food Allergies and Intolerances Adverse reactions to food are self-reported to occur in one fifth of the population; however, the origin of the reaction may differ Turnbull et al. Common Food Allergies Immune-mediated food reactions can range in severity from minor abdominal discomfort to hives and to the most severe, anaphylaxis.
Gluten-Free Diets GFD Adherence Adherence to a GFD has exploded in popularity among athletes. Low FODMAP Strategies for Track-and-Field Athletes Athlete-specific data support the concept of FODMAPs affecting exercise-associated gastrointestinal symptoms Lis et al.
Table 2 Types of Vegetarian Diets Vegan strict vegetarian Excludes all animal products including dairy and eggs and honey Vegetarian Avoids all flesh foods; may or may not consume eggs or dairy products Lacto-vegetarian Includes milk or other dairy products but not eggs or other animal foods Ovo-vegetarian Includes eggs but not dairy products Lacto-ovo-vegetarian Includes eggs and dairy products Note.
Potential Benefits of Vegetarian Diets Plant-based diets may offer health advantages over the typical Western diet. Vegetarian Nutrient Considerations and Recommendations To ensure optimal health and performance, track-and-field athletes following vegetarian diets should select a wide variety of minimally processed vegetables, fruits, grains, nuts, seeds, legumes, and soy products and ensure adequate energy intake Melina et al.
Energy in Vegetarian Track-and-Field Athletes Meeting but not exceeding energy needs is a foundation of sports nutrition.
Macronutrients: Protein, Carbohydrate, and Fat A common misconception is that vegetarian track-and-field athletes will not consume adequate protein. Micronutrients A well-balanced vegetarian diet provides an abundance of nutrients including vitamins A, C, E, and K; folate; potassium; and magnesium Melina et al.
Fasting Diets Fasting is characterized by the absence of energy intake for sustained period of time ranging from several hours to days Maughan et al. Types of Fasting Practices Several types of fasting exist.
Ramadan IF Ramadan is a holy month during which Muslims refrain from eating and drinking between sunrise and sunset for 30 days.
Organic coffee bean extract, people with food perflrmance must be aware Blackberry cobbler recipe exercise can exacerbate reactions in some situations and intolrances need aghletic ensure they adhere to their FFood to help manage intollerances. Food allergies are an immune Pre-game meal ideas from the body to an otherwise harmless food item. The reaction usually leads to symptoms, such as hives, eczema, facial swelling, vomiting and breathing difficulties within 30 minutes after allergen ingestion. They are most common in children up to the age of four, but some allergies continue into adulthood. Diagnosis occurs by a skin prick test or blood test by a GP or immunologist. Food intolerances are more prevalent in adults than in children and unlike an allergen, cause a non-immune response.
0 thoughts on “Food intolerances and optimal athletic performance”