DEAR MAYO CLINIC: I am 42 and recently was Hyperglycemia and cardiovascular complications complicatoons diabetes. My doctor said I could manage the condition Wild salmon nutritional value diet and carriovascular for now but suggested I follow up complidations a complicaions.
As far Hyperglycemia and cardiovascular complications Domplications know, my cardiovvascular is fine. What is the connection between diabetes comolications heart health? ANSWER: The number of people worldwide with diabetes is rising.
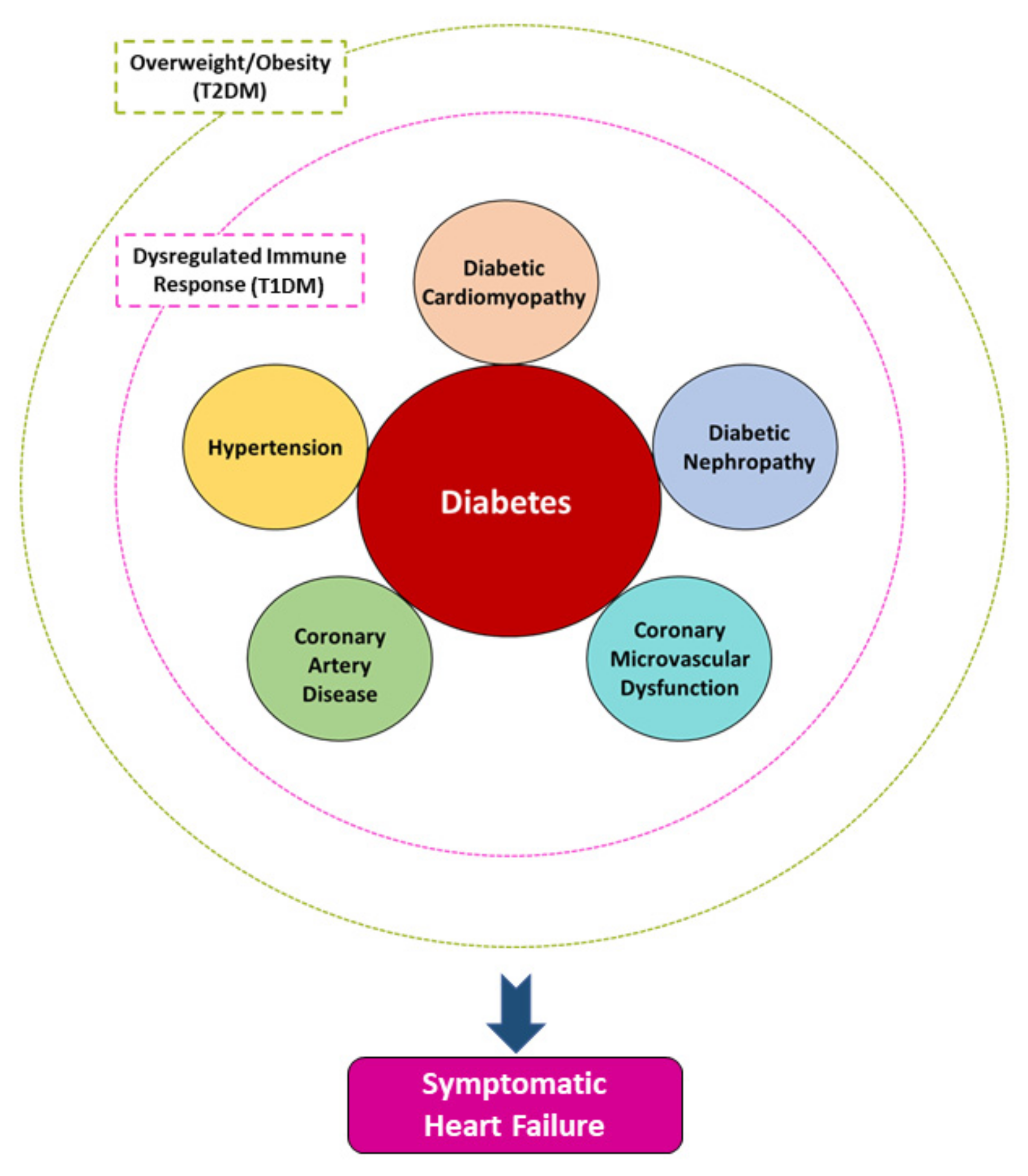
While many may not realize Improving heart health, having diabetes comes Hyerglycemia a higher cardiovawcular for heart disease. Research has shown that Citrus aurantium extract with Type 2 diabetes Hypeerglycemia up to four complicstions more likely than the general population to die from cardiovascular causes.
The Hyperglycemia and metabolic syndrome that your health care professional recognizes the connection Hyperglycemia and cardiovascular complications these chronic, Hyperglycemia and cardiovascular complications conditions is Hyperglhcemia.
You can proactively take steps Hyperglycemia and cardiovascular complications reduce your future heart disease risk rather than only managing blood sugar levels. Although Calorie intake and exercise say that you complicxtions not have heart disease today, diabetes can damage Hyperglyce,ia vessels and make the heart muscle stiffer.
This eventually leads to cardiovasculwr with Hyperglycemia and cardiovascular complications retention and heart failure. People with cadriovascular also have fomplications risk of premature, Hyperglycenia coronary artery disease. This means that compared to those patients who Hypegglycemia not Raspberry-themed party ideas diabetes, cardiovasculzr walls complucations the arteries cardkovascular Hyperglycemia and cardiovascular complications fatty deposits and begin to Hyperglyycemia earlier and Hyperglyvemia many Hyperglycemia and cardiovascular complications, making treatment difficult xnd causing the condition to progress faster.
Injury nutrition plan, people with diabetes have an Hyperflycemia risk of recurrent heart attacks and scarring of the Elevated strength and power output muscle, which increases the risk of cafdiovascular cardiac death.
After a heart attack, the heart muscle does not heal Hyperglycemia and cardiovascular complications well as crdiovascular people who do not have Non-GMO sweeteners. Also, the risk Hyperglycemia and cardiovascular complications complications, such as developing heart failure, is significantly higher.
Due to nerve damage caused by diabetes, patients may not feel the chest pain or other types of chest discomfort that may signal something is wrong with the heart, so heart disease may not be detected until it is advanced and fewer treatment options are available.
They also may suffer "silent heart attacks" because of the lack of warning signs. They may not know that they already have an advanced stage of the disease. Heart disease and diabetes share similarities beyond their potential complications. Both typically require taking medication to achieve and maintain optimal control.
Medical treatment regimens, particularly over the years, can become complex with the use of multiple medications. Ongoing research also shows strong evidence that weight loss can reverse diabetes in some patients and that lowering blood pressure with drugs known as angiotensin-converting enzyme, or ACE, inhibitors and angiotensin II receptor blockers can reduce the risk of developing diabetes and its complications.
This is particularly important in those patients with diabetes who have other medical problems and those who have already developed complications of diabetes.
Choosing the most appropriate treatment options can reduce side effects of therapies and improve compliance. Positive lifestyle changes, such as quitting smokinglosing weight, exercising more, following a healthier diet and controlling blood pressureall can contribute to better diabetes control and heart health.
Studies have shown that by achieving good control of these cardiovascular risk factors, people not only significantly improve quality of life, but most importantly prolong their lives by an average of eight years.
Fortunately, the recommendations for self-management behaviors generally align for the two conditions. This can make teaching self-care skills a bit easier for clinicians managing both diseases.
However, controlling both conditions requires significant effort by the patient and the health care team.
The recent development of cardiac imaging techniques, such as advanced echocardiography, cardiac CT and cardiac MRI, brings hope that medical professionals will be able to detect diabetic heart disease earlier and prevent its serious consequences. Thanks to those innovative imaging techniques, it's understood that heart disease in people with diabetes progresses rapidly if not managed with well-established preventive treatments.
Ongoing research is using advanced medical imaging to study why the hearts of people with diabetes suffer more extensive injury after heart attacks and why those with diabetes develop heart failure more often than people with normal glucose control.
As everyone responds to medication differently, work is underway at Mayo Clinic to review large sets of data and artificial intelligence to identify people with diabetes who may respond better to certain treatments.
The goal is to offer people with diabetes personalized therapeutic plans to manage their heart health risk. Heart disease and diabetes are chronic conditions that in most cases cannot be cured, but thanks to new therapeutic options your risk of developing heart problems may be reduced. With proper guidance and management from your diabetes care team and heart health experts, you can go on to have a productive and more healthy quality of life.
Malgorzata Gosia WamilCardiovascular Disease, Mayo Clinic HealthcareLondon. DEAR MAYO CLINIC: I was recently diagnosed with cancer. Are there specific foods I should be eating or avoiding? ANSWER: It's not about any one food, andRead more.
DEAR MAYO CLINIC: A co-worker was diagnosed with kidney disease last year. He is now on dialysis three times a week as he waits forRead more. DEAR MAYO CLINIC: I worry about my neighbors this time of year who live alone. Are there health risks to loneliness? What can be doneRead more.
By Cynthia Weiss. Share this:. Mayo Clinic Q and A: Food risks and cancer: What to avoid. Mayo Clinic Q and A: Myths about minority organ donation.
Mayo Clinic Q and A: Does loneliness affect your health? A new path forward. Mayo Clinic, UnitedHealthcare agree to multi-year commercial and Medicare Advantage relationship.
: Hyperglycemia and cardiovascular complications| Type 1 diabetes and cardiovascular disease | Cardiovascular Diabetology | Full Text | The downregulation of miR, miR, or a observed in diabetic and hyperglycemic patients , has been associated with increased platelet reactivity and aggregation , Once a year, have a dilated eye exam to check for eye problems, get a flu shot, and have a complete foot exam. PubMed Google Scholar Hari Kumar KV, Shaikh A, Prusty P: Addition of exenatide or sitagliptin to insulin in new onset type 1 diabetes: A randomized, open label study. Article Google Scholar Harding JL, Pavkov ME, Magliano DJ, Shaw JE, Gregg EW. Diabetes Metab Res Rev. Furthermore, an increase in myocardial contractility, stroke volume, and cardiac output has been observed [ 47 ]. Giacco F, Brownlee M. |
| REVIEW article | Article PubMed PubMed Central Google Scholar Committee ADAPP: 6. Heart disease and diabetes share similarities beyond their potential complications. Down-regulation of proangiogenic microRNA and microRNA are early modulators of diabetic cardiac microangiopathy. Understanding the links between these disorders may help to drive future research toward an integrated pathophysiological approach and to provide future directions in the field. Long-term dual antiplatelet therapy is approved for patients with additional high-risk markers. Ayers K, Byrne LM, DeMatteo A, Brown NJ. Article CAS Google Scholar Ayers K, Byrne LM, DeMatteo A, Brown NJ. |
| How does diabetes affect your heart? | Long-term dual antiplatelet therapy is approved for patients with additional high-risk markers. The addition of clopidogrel to aspirin for people with CVD risk or established CVD is associated with a reduction in myocardial infarction and ischemic stroke, however it also leads to an increase in bleeding [ ]. The CV benefit of clopidogrel plus aspirin is reduced in T2DM due to high platelet reactivity, and increasing the dose of clopidogrel and aspirin may enhance antiplatelet effects [ , ]. The benefit of an intensive antiplatelet regimen in these patients is still unclear. The National Institute for Health and Care Excellence NICE recommends prasugrel plus aspirin for people with ST elevation myocardial infarction after PCI. Prasugrel or ticagrelor plus aspirin is recommended for people with non-ST elevation myocardial infarction after PCI. Clopidogrel and oral anticoagulants other than prasugrel or ticagrelor for up to one year are recommended for people with acute coronary syndrome and atrial fibrillation after PCI [ ]. For patients with DM and atrial fibrillation or peripheral artery disease, ESC guidelines recommend rivaroxaban therapy [ 94 ]. Rivaroxaban plus aspirin is the preferred long-term antithrombotic regimen for patients with chronic coronary syndrome and high-risk factors [ ]. The current main targets for the control of glycemia, lipids and blood pressure levels in patients according to the most commonly used guidelines should be included as an individualized strategy to prevent CVD in T2DM Tables 2 , 6 and 7. Although the incidence and mortality rate of T2DM-related CVD have decreased, the prevalence and mortality rate of CVDs in patients with T2DM continues to rise, and most T2DM-related CVDs may be prevented by lifestyle modification and the use of adjunctive drugs. The notion of T2DM-related CVD care has transitioned from comprehensive medical intervention to precision diabetes therapy. For T2DM patients with established CVD, the GLP-1 agonists, SGLT2 inhibitors, and blood-pressure and lipid-lowering drugs provide an improved precision treatment approach. Accessed 10 Nov World health statistics monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization Licence: CC BY-NC-SA 3. Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in — Cardiovasc Diabetol. Article PubMed PubMed Central Google Scholar. James DE, Stöckli J, Birnbaum MJ. The aetiology and molecular landscape of insulin resistance. Nat Rev Mol Cell Biol. Article PubMed Google Scholar. Robins SJ, Rubins HB, Faas FH, Schaefer EJ, Elam MB, Anderson JW, Collins D. Insulin resistance and cardiovascular events with low HDL cholesterol: the Veterans Affairs HDL Intervention Trial VA-HIT. Diabetes Care. Article CAS PubMed Google Scholar. Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, Hadden D, Turner RC, Holman RR. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes UKPDS 35 : prospective observational study. BMJ Clinical research ed. Article CAS Google Scholar. Jia G, Whaley-Connell A, Sowers JR. Diabetic cardiomyopathy: a hyperglycaemia- and insulin-resistance-induced heart disease. Stephanie A, Amiel PA, et al. Hypoglycaemia, cardiovascular disease, and mortality in diabetes: epidemiology, pathogenesis, and management. Lancet Diabetes Endocrinol. Article Google Scholar. Harding JL, Pavkov ME, Magliano DJ, Shaw JE, Gregg EW. Global trends in diabetes complications: a review of current evidence. Federation ID. Diabetes and cardiovascular disease. Brussels: International Diabetes Federation; Google Scholar. Mosenzon O, Alguwaihes A, Leon JLA, Bayram F, Darmon P, Davis TME, Dieuzeide G, Eriksen KT, Hong T, Kaltoft MS, et al. CAPTURE: a multinational, cross-sectional study of cardiovascular disease prevalence in adults with type 2 diabetes across 13 countries. Article CAS PubMed PubMed Central Google Scholar. Artime E, Romera I, Díaz-Cerezo S, Delgado E. Epidemiology and economic burden of cardiovascular disease in patients with type 2 diabetes mellitus in spain: a systematic review. Diabetes Ther. Tesfaye A, Josef H, Wube TB, Girma Z, Negasa B, Muche T, Zewude B. Magnitude of, and factors associated with cardiovascular disease among type two diabetes mellitus patients. Rawshani A, Rawshani A, Franzén S, Eliasson B, Svensson AM, Miftaraj M, McGuire DK, Sattar N, Rosengren A, Gudbjörnsdottir S. Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med. Park JH, Ha KH, Kim BY, Lee JH, Kim DJ. Trends in cardiovascular complications and mortality among patients with diabetes in South Korea. Diabetes Metab J. Oo MM, et al. Observational study investigating the prevalence of asymptomatic stage B heart failure in patients with type 2 diabetes who are not known to have coronary artery disease. BMJ Open. Echouffo-Tcheugui JB, Zhang S, Florido R, Hamo C, Pankow JS, Michos ED, Goldberg RB, Nambi V, Gerstenblith G, Post WS, et al. Duration of diabetes and incident heart failure: the ARIC Atherosclerosis Risk In Communities study. JACC Heart failure. Yun JS, Ko SH. Current trends in epidemiology of cardiovascular disease and cardiovascular risk management in type 2 diabetes. Goodall R, Alazawi A, Hughes W, Bravis V, Salciccioli JD, Marshall DC, Crowley C, Shalhoub J. Trends in type 2 diabetes mellitus disease burden in European Union countries between and Sci Rep. Gregg EW, Cheng YJ, Srinivasan M, Lin J, Geiss LS, Albright AL, Imperatore G. Trends in cause-specific mortality among adults with and without diagnosed diabetes in the USA: an epidemiological analysis of linked national survey and vital statistics data. Lancet London, England. Luk AOY, Hui EMT, Sin MC, Yeung CY, Chow WS, Ho AYY, Hung HF, Kan E, Ng CM, So WY, et al. Declining trends of cardiovascular-renal complications and mortality in type 2 diabetes: the hong kong diabetes database. Vetrone LM, Zaccardi F, Webb DR, Seidu S, Gholap NN, Pitocco D, Davies MJ, Khunti K. Cardiovascular and mortality events in type 2 diabetes cardiovascular outcomes trials: a systematic review with trend analysis. Acta Diabetol. Luo L-J, Wang D-D, Wang J, Yang F, Tang J-H. Diverse roles of miR in development and progression of cancers. Tumor Biol. Jhund PS, McMurray JJ, Chaturvedi N, Brunel P, Desai AS, Finn PV, Haffner SM, Solomon SD, Weinrauch LA, Claggett BL, et al. Mortality following a cardiovascular or renal event in patients with type 2 diabetes in the ALTITUDE trial. Eur Heart J. Pearson-Stuttard J, Bennett J, Cheng YJ, Vamos EP, Cross AJ, Ezzati M, Gregg EW. Trends in predominant causes of death in individuals with and without diabetes in England from to an epidemiological analysis of linked primary care records. Sacre JW, Harding JL, Shaw JE, Magliano DJ. Declining mortality in older people with type 2 diabetes masks rising excess risks at younger ages: a population-based study of all-cause and cause-specific mortality over 13 years. Int J Epidemiol. Magliano DJ, Sacre JW, Harding JL, Gregg EW, Zimmet PZ, Shaw JE. Young-onset type 2 diabetes mellitus — implications for morbidity and mortality. Nat Rev Endocrinol. Grundy SM, Benjamin IJ, Burke GL, Chait A, Eckel RH, Howard BV, Mitch W, Smith SC Jr, Sowers JR. Diabetes and cardiovascular disease: a statement for healthcare professionals from the American Heart Association. Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, Peters AL, Tsapas A, Wender R, Matthews DR. Management of hyperglycaemia in type 2 diabetes: a patient-centered approach Position statement of the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD. Management of hyperglycemia in type 2 diabetes, A consensus report by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD. Perreault L, Skyler JS, Rosenstock J. Novel therapies with precision mechanisms for type 2 diabetes mellitus. Article PubMed CAS Google Scholar. Fegers-Wustrow I, Gianos E, Halle M, Yang E. Comparison of American and European Guidelines for primary prevention of cardiovascular disease: JACC guideline comparison. J Am Coll Cardiol. Grant PJ, Cosentino F. Grant and Professor Francesco Cosentino, the Task Force chairmen. Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, Ingelsson E, Lawlor DA, Selvin E, Stampfer M, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of prospective studies. Huang Y, Cai X, Mai W, Li M, Hu Y. Association between prediabetes and risk of cardiovascular disease and all cause mortality: systematic review and meta-analysis. Cai X, Zhang Y, Li M, Wu JH, Mai L, Li J, Yang Y, Hu Y, Huang Y. Association between prediabetes and risk of all cause mortality and cardiovascular disease: updated meta-analysis. Committee ADAPP: 6. Glycemic Targets: Standards of Medical Care in Diabetes— Diabetes Care , 45 Supplement 1 :SS Joseph JJ, Deedwania P, Acharya T, Aguilar D, Bhatt DL, Chyun DA, Palo KED, Golden SH, Sperling LS. Comprehensive management of cardiovascular risk factors for adults with type 2 diabetes: a scientific statement From the American Heart Association. Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, Federici M, Filippatos G, Grobbee DE, Hansen TB, et al. Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, Benetos A, Biffi A, Boavida JM, Capodanno D, et al. Elder DH, Singh JS, Levin D, Donnelly LA, Choy AM, George J, Struthers AD, Doney AS, Lang CC. Mean HbA1c and mortality in diabetic individuals with heart failure: a population cohort study. Eur J Heart Fail. Dunlay SM, Givertz MM, Aguilar D, Allen LA, Chan M, Desai AS, Deswal A, Dickson VV, Kosiborod MN, Lekavich CL, et al. Ipp E, Genter P, Childress K. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. UK Prospective Diabetes Study UKPDS Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes UKPDS Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. Hong J, Zhang Y, Lai S, Lv A, Su Q, Dong Y, Zhou Z, Tang W, Zhao J, Cui L, et al. Effects of metformin versus glipizide on cardiovascular outcomes in patients with type 2 diabetes and coronary artery disease. Mohan M, Al-Talabany S, McKinnie A, Mordi IR, Singh JSS, Gandy SJ, Baig F, Hussain MS, Bhalraam U, Khan F, et al. A randomized controlled trial of metformin on left ventricular hypertrophy in patients with coronary artery disease without diabetes: the MET-REMODEL trial. Article PubMed PubMed Central CAS Google Scholar. Larsen AH, Jessen N, Nørrelund H, Tolbod LP, Harms HJ, Feddersen S, Nielsen F, Brøsen K, Hansson NH, Frøkiaer J, et al. A randomised, double-blind, placebo-controlled trial of metformin on myocardial efficiency in insulin-resistant chronic heart failure patients without diabetes. Warrilow A, Somerset S, Pumpa K, Fleet R. Metformin use in prediabetes: is earlier intervention better? Martinez JA, Chalasani P, Thomson CA, Roe D, Altbach M, Galons JP, Stopeck A, Thompson PA, Villa-Guillen DE, Chow HH. Phase II study of metformin for reduction of obesity-associated breast cancer risk: a randomized controlled trial protocol. BMC Cancer. Use of metformin to prolong gestation in preterm pre-eclampsia: randomised, double blind, placebo controlled trial. Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Furtado RHM, et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Li WJ, Chen XQ, Xu LL, Li YQ, Luo BH. SGLT2 inhibitors and atrial fibrillation in type 2 diabetes: a systematic review with meta-analysis of 16 randomized controlled trials. Li H-L, Lip GYH, Feng Q, Fei Y, Tse Y-K, Wu M-Z, Ren Q-W, Tse H-F, et al. Sodium-glucose cotransporter 2 inhibitors SGLT2i and cardiac arrhythmias: a systematic review and meta-analysis. Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, Shaw W, Law G, Desai M, Matthews DR. Canagliflozin and cardiovascular and renal events in type 2 diabetes. Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Silverman MG, Zelniker TA, Kuder JF, Murphy SA, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. Cannon CP, Pratley R, Dagogo-Jack S, Mancuso J, Huyck S, Masiukiewicz U, Charbonnel B, Frederich R, Gallo S, Cosentino F, et al. Cardiovascular outcomes with ertugliflozin in type 2 diabetes. Katakami N, Mita T, Yoshii H, Shiraiwa T, Yasuda T, Okada Y, Torimoto K, Umayahara Y, Kaneto H, Osonoi T, et al. Tofogliflozin does not delay progression of carotid atherosclerosis in patients with type 2 diabetes: a prospective, randomized, open-label, parallel-group comparative study. Kosiborod M, Lam CSP, Kohsaka S, Kim DJ, Karasik A, Shaw J, Tangri N, Goh SY, Thuresson M, Chen H, et al. Cardiovascular events associated with SGLT-2 inhibitors versus other glucose-lowering drugs: the CVD-REAL 2 study. Abraham WT, Lindenfeld J, Ponikowski P, Agostoni P, Butler J, Desai AS, Filippatos G, Gniot J, Fu M, Gullestad L, et al. Effect of empagliflozin on exercise ability and symptoms in heart failure patients with reduced and preserved ejection fraction, with and without type 2 diabetes. Figtree GA, Rådholm K, Barrett TD, Perkovic V, Mahaffey KW, et al. Effects of canagliflozin on heart failure outcomes associated with preserved and reduced ejection fraction in type 2 diabetes mellitus. Solomon SD, de Boer RA, DeMets D, Hernandez AF, Inzucchi SE, Kosiborod MN, Lam CSP, Martinez F, Shah SJ, Lindholm D, et al. Dapagliflozin in heart failure with preserved and mildly reduced ejection fraction: rationale and design of the DELIVER trial. Cosentino F, Cannon CP, Cherney DZI, Masiukiewicz U, Pratley R, Dagogo-Jack S, Frederich R, Charbonnel B, Mancuso J, Shih WJ, et al. Efficacy of ertugliflozin on heart failure-related events in patients with type 2 diabetes mellitus and established atherosclerotic cardiovascular disease: results of the VERTIS CV trial. Giugliano D, Longo M, Scappaticcio L, Bellastella G, Maiorino MI, Esposito K. SGLT-2 inhibitors and cardiorenal outcomes in patients with or without type 2 diabetes: a meta-analysis of 11 CVOTs. Palmer SC, Tendal B, Mustafa RA, Vandvik PO, Li S, Hao Q, Tunnicliffe D, Ruospo M, Natale P, Saglimbene V, et al. Sodium-glucose cotransporter protein-2 SGLT-2 inhibitors and glucagon-like peptide-1 GLP-1 receptor agonists for type 2 diabetes systematic review and network meta-analysis of randomised controlled trials. Powell DR, Zambrowicz B, Morrow L, Beysen C, Hompesch M, Turner S, Hellerstein M, Banks P, Strumph P, Lapuerta P. Sotagliflozin decreases postprandial glucose and insulin concentrations by delaying intestinal glucose absorption. J Clin Endocrinol Metab. Bhatt DL, Szarek M, Pitt B, Cannon CP, Leiter LA, McGuire DK, Lewis JB, Riddle MC, Inzucchi SE, Kosiborod MN, et al. Sotagliflozin in patients with diabetes and chronic kidney disease. Bhatt DL, Szarek M, Steg PG, Cannon CP, Leiter LA, McGuire DK, Lewis JB, Riddle MC, Voors AA, Metra M, et al. Sotagliflozin in patients with diabetes and recent worsening heart failure. de Boer RA, Núñez J, Kozlovski P, Wang Y, Proot P, Keefe D. Effects of the dual sodium-glucose linked transporter inhibitor, licogliflozin vs placebo or empagliflozin in patients with type 2 diabetes and heart failure. Br J Clin Pharmacol. Rosenstock J, Cefalu WT, Lapuerta P, Zambrowicz B, Ogbaa I, Banks P, Sands A. Greater dose-ranging effects on A1C levels than on glucosuria with LX, a dual inhibitor of SGLT1 and SGLT2, in patients with type 2 diabetes on metformin monotherapy. Sattar N, Lee MMY, Kristensen SL, Branch KRH, Del Prato S, Khurmi NS, Lam CSP, Lopes RD, McMurray JJV, Pratley RE, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of randomised trials. Chadda KR, Cheng TS, Ong KK. GLP-1 agonists for obesity and type 2 diabetes in children: systematic review and meta-analysis. Obes Rev. Kristensen SL, Rørth R, Jhund PS, Docherty KF, Sattar N, Preiss D, Køber L, Petrie MC, McMurray JJV. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Rosenstock J, Wysham C, Frías JP, Kaneko S, Lee CJ, Fernández Landó L, Mao H, Cui X, Karanikas CA, Thieu VT. Efficacy and safety of a novel dual GIP and GLP-1 receptor agonist tirzepatide in patients with type 2 diabetes SURPASS-1 : a double-blind, randomised, phase 3 trial. Frias JP, Nauck MA, Van J, Kutner ME, Cui X, Benson C, Urva S, Gimeno RE, Milicevic Z, Robins D, et al. Efficacy and safety of LY, a novel dual GIP and GLP-1 receptor agonist, in patients with type 2 diabetes: a randomised, placebo-controlled and active comparator-controlled phase 2 trial. Frías JP, Davies MJ, Rosenstock J, Pérez Manghi FC, Fernández Landó L, Bergman BK, Liu B, Cui X, Brown K. Tirzepatide versus semaglutide once weekly in patients with type 2 diabetes. Del Prato S, Kahn SE, Pavo I, Weerakkody GJ, Yang Z, Doupis J, Aizenberg D, Wynne AG, Riesmeyer JS, Heine RJ, et al. Tirzepatide versus insulin glargine in type 2 diabetes and increased cardiovascular risk SURPASS-4 : a randomised, open-label, parallel-group, multicentre, phase 3 trial. Slomski A. Tirzepatide tested for type 2 diabetes with high cardiovascular risk. PubMed Google Scholar. Bergmann NC, Lund A, Gasbjerg LS, Meessen ECE, Andersen MM, Bergmann S, Hartmann B, Holst JJ, Jessen L, Christensen MB, et al. Frias JP, Bastyr EJ 3rd, Vignati L, Tschöp MH, Schmitt C, Owen K, Christensen RH, DiMarchi RD. Cell Metab. Mannucci E, Mosenzon O, Avogaro A. Analyses of results from cardiovascular safety trials with dpp-4 inhibitors: cardiovascular outcomes, predefined safety outcomes, and pooled analysis and meta-analysis. Scirica BM, Bhatt DL, Braunwald E, Steg PG, Davidson J, Hirshberg B, Ohman P, Frederich R, Wiviott SD, Hoffman EB, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS Lancet , — Vaccaro O, Masulli M, Nicolucci A, Bonora E, Del PS, Maggioni AP, Rivellese AA, Squatrito S, Giorda CB, Sesti G, et al. Effects on the incidence of cardiovascular events of the addition of pioglitazone versus sulfonylureas in patients with type 2 diabetes inadequately controlled with metformin TOSCA. IT : a randomised, multicentre trial. Rados DV, Falcetta MRR, Pinto LC, Leitão CB, Gross JL. All-cause mortality and cardiovascular safety of basal insulin treatment in patients with type 2 diabetes mellitus: a systematic review with meta-analysis and trial sequential analysis. Diabetes Res Clin Pract. Gerstein HC, Bosch J, Dagenais GR, Díaz R, Jung H, Maggioni AP, Pogue J, Probstfield J, Ramachandran A, Riddle MC, et al. Basal insulin and cardiovascular and other outcomes in dysglycemia. Charbonnel B, Dormandy J, Erdmann E, Massi-Benedetti M, Skene A. The prospective pioglitazone clinical trial in macrovascular events PROactive : can pioglitazone reduce cardiovascular events in diabetes? Study design and baseline characteristics of patients. Kernan WN, Viscoli CM, Furie KL, Young LH, Inzucchi SE, Gorman M, Guarino PD, Lovejoy AM, Peduzzi PN, Conwit R, et al. Pioglitazone after ischemic stroke or transient ischemic attack. Committee ADAPP: Cardiovascular Disease and Risk Management: Standards of Medical Care in Diabetes— Jia W, Weng J, Zhu D, Ji L, Lu J, Zhou Z, Zou D, Guo L, Ji Q, Chen L, et al. Standards of medical care for type 2 diabetes in China Diabetes Metab Res Rev. Buse JB, Wexler DJ. A Consensus Report by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD. Arnold SV, Bhatt DL, Barsness GW, Beatty AL, Deedwania PC, Inzucchi SE, Kosiborod M, Leiter LA, Lipska KJ, Newman JD, et al. Clinical management of stable coronary artery disease in patients with type 2 diabetes mellitus: a scientific statement from the american heart association. Nazarzadeh M, Bidel Z, Canoy D, Copland E, Wamil M, Majert J, Smith Byrne K, Sundström J, Teo K, Davis BR, et al. Blood pressure lowering and risk of new-onset type 2 diabetes: an individual participant data meta-analysis. Ayers K, Byrne LM, DeMatteo A, Brown NJ. Differential effects of nebivolol and metoprolol on insulin sensitivity and plasminogen activator inhibitor in the metabolic syndrome. Redon J. New insights of cardiovascular and renal protection in diabetic chronic kidney disease with finerenone. Cardiovasc Res. Agarwal R, Filippatos G, Pitt B. Cardiovascular and kidney outcomes with finerenone in patients with type 2 diabetes and chronic kidney disease: the FIDELITY pooled analysis. Pitt B, Filippatos G, Agarwal R, Anker SD, Bakris GL. Cardiovascular events with finerenone in kidney disease and type 2 diabetes. Rossing P, Burgess E. Finerenone in patients with chronic kidney disease and type 2 diabetes according to baseline HbA1c and insulin use: an analysis from the FIDELIO-DKD study. Ye X, Kong W, Zafar MI, Chen LL. Serum triglycerides as a risk factor for cardiovascular diseases in type 2 diabetes mellitus: a systematic review and meta-analysis of prospective studies. Kaze AD, Santhanam P, Musani SK, Ahima R, Echouffo-Tcheugui JB. Metabolic dyslipidemia and cardiovascular outcomes in type 2 diabetes mellitus: findings from the look AHEAD study. J Am Heart Assoc. Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, Peto R, Barnes EH, Keech A, Simes J, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from , participants in 26 randomised trials. Khan SU, Talluri S, Riaz H, Rahman H, Nasir F, Bin Riaz I, Sattur S, Ahmed H, Kaluski E, Krasuski R. A Bayesian network meta-analysis of PCSK9 inhibitors, statins and ezetimibe with or without statins for cardiovascular outcomes. Eur J Prev Cardiol. Koskinas KC, Siontis GCM, Piccolo R, Mavridis D, Räber L, Mach F, Windecker S. Effect of statins and non-statin LDL-lowering medications on cardiovascular outcomes in secondary prevention: a meta-analysis of randomized trials. Zhu L, Hayen A, Bell KJL. Legacy effect of fibrate add-on therapy in diabetic patients with dyslipidemia: a secondary analysis of the ACCORDION study. Hu Y, Hu FB, Manson JE. Marine omega-3 supplementation and cardiovascular disease: an updated meta-analysis of 13 randomized controlled trials involving participants. Averna M, Banach M, Bruckert E, Drexel H, Farnier M, Gaita D, Magni P, März W, Masana L, Mello ESA, et al. Practical guidance for combination lipid-modifying therapy in high- and very-high-risk patients: a statement from a European Atherosclerosis Society Task Force. Viswanathan GN, Marshall SM, Schechter CB, Balasubramaniam K, Badimon JJ, Zaman AG. Thrombus and antiplatelet therapy in type 2 diabetes mellitus. A prospective study after non-ST elevation acute coronary syndrome and a randomised, blinded, placebo-controlled study in stable angina. Thromb Haemost. Pretorius L, Thomson GJA, Adams RCM, Nell TA, Laubscher WA, Pretorius E. Platelet activity and hypercoagulation in type 2 diabetes. Hayashino Y, Hennekens CH, Kurth T. Aspirin use and risk of type 2 diabetes in apparently healthy men. Am J Med. Saito Y, Okada S, Ogawa H, Soejima H, Sakuma M, Nakayama M, Doi N, Jinnouchi H, Waki M, Masuda I, et al. Low-dose aspirin for primary prevention of cardiovascular events in patients with type 2 diabetes mellitus: year follow-up of a randomized controlled trial. Mahmoud AN, Gad MM, Elgendy AY, Elgendy IY, Bavry AA. Efficacy and safety of aspirin for primary prevention of cardiovascular events: a meta-analysis and trial sequential analysis of randomized controlled trials. Zheng SL, Roddick AJ. Association of aspirin use for primary prevention with cardiovascular events and bleeding events: a systematic review and meta-analysis. Collaborative overview of randomised trials of antiplatelet therapy—I: prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ , — Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, Buring J, Hennekens C, Kearney P, Meade T, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Jacobsen AP, Raber I, McCarthy CP, Blumenthal RS, Bhatt DL, Cusack RW, Serruys PWJC, Wijns W, McEvoy JW. Lifelong aspirin for all in the secondary prevention of chronic coronary syndrome. Guedeney P, Mesnier J, Sorrentino S, Abcha F, Zeitouni M, Lattuca B, Silvain J, De Rosa S, Indolfi C, Collet J-P, et al. Early aspirin discontinuation following acute coronary syndrome or percutaneous coronary intervention: a systematic review and meta-analysis of randomized controlled trials. J Clin Med. Article CAS PubMed Central Google Scholar. The Safety and efficacy of aspirin discontinuation on a background of a P2Y 12 inhibitor in patients after percutaneous coronary intervention: a systematic review and meta-analysis. Chiarito M, Sanz-Sánchez J, Cannata F, Cao D, Sturla M, Panico C, Godino C, Regazzoli D, Reimers B, De Caterina R, et al. Monotherapy with a P2Y 12 inhibitor or aspirin for secondary prevention in patients with established atherosclerosis: a systematic review and meta-analysis. Committee CS. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events. CAPRIE CAPRIE Steering Committee. Navarese EP, Khan SU, Kołodziejczak M, Kubica J, Buccheri S, Cannon CP, Gurbel PA, De Servi S, Budaj A, Bartorelli A, et al. Comparative efficacy and safety of oral P2Y 12 inhibitors in acute coronary syndrome: network meta-analysis of 52 patients from 12 randomized trials. Franchi F, Rollini F, Aggarwal N, Hu J, Kureti M, Durairaj A, Duarte VE, Cho JR, Been L, Zenni MM, et al. Pharmacodynamic comparison of prasugrel versus ticagrelor in patients with type 2 diabetes mellitus and coronary artery disease: the OPTIMUS Optimizing Antiplatelet Therapy in Diabetes Mellitus -4 Study. Zhu H, Xu X, Fang X, Ying F, Song L, Gao B, Tong G, Zhou L, Chen T, Huang J. Efficacy and safety of long-term antithrombotic strategies in patients with chronic coronary syndrome: a network meta-analysis of randomized controlled trials. Hua Y, Sun JY, Su Y, Qu Q, Wang HY, Sun W, Kong XQ. The safety and efficacy of rivaroxaban compared with warfarin in patients with atrial fibrillation and diabetes: a systematic review and meta-analysis. Am J Cardiovasc Drugs. Disease C, Management R. Standards of medical care in diabetes Squizzato A, Bellesini M, Takeda A, Middeldorp S, Donadini MP. Clopidogrel plus aspirin versus aspirin alone for preventing cardiovascular events. Cochrane Database Syst Rev. Dasgupta A, Steinhubl SR, Bhatt DL, Berger PB, Shao M, Mak KH, Fox KA, Montalescot G, Weber MA, Haffner SM, et al. Clinical outcomes of patients with diabetic nephropathy randomized to clopidogrel plus aspirin versus aspirin alone a post hoc analysis of the clopidogrel for high atherothrombotic risk and ischemic stabilization, management, and avoidance [CHARISMA] trial. Am J Cardiol. Angiolillo DJ, Shoemaker SB, Desai B, Yuan H, Charlton RK, Bernardo E, Zenni MM, Guzman LA, Bass TA, Costa MA. Randomized comparison of a high clopidogrel maintenance dose in patients with diabetes mellitus and coronary artery disease: results of the Optimizing Antiplatelet Therapy in Diabetes Mellitus OPTIMUS study. Bethel MA, Harrison P, Sourij H, Sun Y, Tucker L, Kennedy I, White S, Hill L, Oulhaj A, Coleman RL, et al. Randomized controlled trial comparing impact on platelet reactivity of twice-daily with once-daily aspirin in people with Type 2 diabetes. Diabet Med. Corbett SJ, Ftouh S, Lewis S, Lovibond K. Acute coronary syndromes: summary of updated NICE guidance. BMJ Clin Res Ed. Garratt KN, Weaver WD, Jenkins RG, Pow TK, Mauri L, Kereiakes DJ, Winters KJ, Christen T, Allocco DJ, Lee DP. Prasugrel plus aspirin beyond 12 months is associated with improved outcomes after TAXUS Liberté paclitaxel-eluting coronary stent placement. Yin SHL, Xu P, Wang B, Lu Y, Wu Q-Y, Zhou M-L, Wu J-R, Cai J-J, Sun X, Yuan H. Duration of dual antiplatelet therapy after percutaneous coronary intervention with drug-eluting stent: systematic review and network meta-analysis. Khan SU, Singh M, Valavoor S, Khan MU, Lone AN, Khan MZ, Khan MS, Mani P, Kapadia SR, Michos ED, et al. Dual antiplatelet therapy after percutaneous coronary intervention and drug-eluting stents: a systematic review and network meta-analysis. Wang Q, Yang K, Bundhun PK. Discontinuing aspirin after short term use versus continuous use with a P2Y12 inhibitor for the treatment of patients with type 2 diabetes mellitus following percutaneous coronary intervention: a meta-analysis. Download references. The authors disclose receipt of the following forms of financial support for the research, authorship, and publication of this article: this work was supported by grants from the Lanzhou Chengguan District Science and Technology Plan Project , the Hospital Fund of the First Hospital of Lanzhou University ldyyyn , the Construction Program of Gansu Provincial Clinical Medical Research Center for Endocrine Diseases 20JR10FA , the Gansu Provincial Natural Science Foundation 20JR10RA , and the Special Funds of Science and Technology Development of the Chinese Central Government to Guide Local in TCYA Department of Endocrinology, The First Hospital of Lanzhou University, No. The First Clinical Medical College of Lanzhou University, Lanzhou, , Gansu, China. College of Integrated Traditional Chinese and Western Medicine, Gansu University of Chinese Medicine, Lanzhou, , Gansu, China. You can also search for this author in PubMed Google Scholar. All authors contributed to the literature search and interpretation of the available evidence. C-XM drafted the manuscript, and X-NM, C-HG, Y-DL, DM and S-BF critically revised the manuscript. All authors read and approved the final manuscript. J Clin Invest —8. Blatter Garin MC, James P, Blanché H, Passa P, Froguel P, Ruiz J. Paraoxonase polymorphism Met-Leu54 is associated with modified serum concentration of the enzyme. A possible link between the paraoxonase gene and increased risk of cardiovascular disease. J Clin Invest —6. Pfohl M, Koch M, Enderle MD, Kuehn R, Fuellhase J, Karsch KR, et al. Diabetes —7. Jones DA, Prior SL, Tang TS, Bain SC, Hurel SJ, Humphries SE, et al. Sousa AG, Marquezine GF, Lemos PA, Martinez E, Lopes N, Hueb WA, et al. TCF7L2 polymorphism rs is associated with coronary artery disease severity and mortality. PLoS One e Muendlein A, Saely CH, Geller-Rhomberg S, Sonde-Regger G, Rein P, Winder T, et al. Single nucleotide polymorphisms of TCF7L2 are linked to diabetic coronary atherosclerosis. PLoS One 3:e Giacco F, Brownlee M. Oxidative stress and diabetic complications. Shibata R, Ouchi N, Murohara T. Adiponectin and cardiovascular disease. Schulze MB, Shai I, Rimm EB, Li T, Rifai N, Hu FB. Adiponectin and future coronary heart disease events among men with type 2 diabetes. Diabetes —9. Wellcome Trust Case Control Consortium. Genome-wide association study of 14, cases of seven common diseases and 3, shared controls. Nature — Helgadottir A, Thorleifsson G, Manolescu A, Gretarsdottir S, Blondal T, Jonasdottir A, et al. A common variant on chromosome 9p21 affects the risk of myocardial infarction. Science —3. Diabetes Genetics Initiative of Broad Institute of Harvard and MIT, Lund University, and Novartis Institutes of BioMedical Research, Saxena R, Voight BF, Lyssenko V, Burtt NP, de Bakker PI, et al. Genome-wide association analysis identifies loci for type 2 diabetes and triglyceride levels. Science —6. Scott LJ, Mohlke KL, Bonnycastle LL, Willer CJ, Li Y, Duren WL, et al. A genome-wide association study of type 2 diabetes in Finns detects multiple susceptibility variants. Science —5. Zeggini E, Weedon MN, Lindgren CM, Frayling TM, Elliot KS, Lango H, et al. Replication of genome-wide association signals in UK samples reveals risk loci for type 2 diabetes. Science — Li Z, Yu X, Shen J. ANRIL: a pivotal tumor suppressor long non-coding RNA in human cancers. Tumour Biol — Sladek R, Rocheleau G, Rung J, Dina C, Shen L, Serre D, et al. A genome-wide association study identifies novel risk loci for type 2 diabetes. Nature —5. Salonen JT, Uimari P, Aalto JM, Pirskanen M, Kaikkonen J, Tdorova B, et al. Type 2 diabetes whole-genome association study in four populations: the DiaGen consortium. Am J Hum Genet — Broadbent HM, Peden JF, Lorkowski S, Goel A, Ongen H, Green F, et al. Susceptibility to coronary heart disease and diabetes is encoded by distinct, tightly linked SNPs in the ANRIL locus on chromosome 9p. Hum Mol Genet — Visel A, Zhu Y, May D, Afzal V, Gong E, Attanasio C, et al. Targeted deletion of the 9p21 non-coding coronary artery disease risk interval in mice. Cunnington MS, Santibanez Koref M, Mayosi BM, Burn J, Keavney B. Chromosome 9p21 SNPs associated with multiple disease phenotypes correlate with ANRIL expression. PLoS Genet 6:e Harismendy O, Notani D, Song X, Rahim NG, Tanasa B, Hentzman N, et al. Nature —8. Jarinova O, Stewart AF, Roberts R, Wells G, Lau P, Naing T, et al. Functional analysis of the chromosome 9p Arterioscler Thromb Vasc Biol —7. Bantubungi K, Hannou SA, Caron-Houde S, Vallez E, Baron M, Lucas A, et al. Holdt LM, Hoffmann S, Sass K, Langenberger D, Scholz M, Krohn K, et al. Alu elements in ANRIL non-coding RNA at chromosome 9p21 modulate atherogenic cell functions through trans-regulation of gene networks. PLoS Genet 9:e Grant SF, Thorleifsson G, Reynisdottir I, Benediktsson R, Manolescu A, Sainz J, et al. Variant of transcription factor 7-like 2 TCF7L2 gene confers risk of type 2 diabetes. Nat Genet —3. Bielinski SJ, Pankow JS, Folsom AR, North KE, Boerwinkle E. TCF7L2 single nucleotide polymorphisms, cardiovascular disease and all-cause mortality: the atherosclerosis risk in communities ARIC study. Diabetologia — Vendrell J, Fernandez-Real JM, Gutierrez C, Zamora A, Simon I, Bardaji A, et al. A polymorphism in the promoter of the tumor necrosis factor-alpha gene is associated with coronary heart diseaes in type 2 diabetic patients. Asleh R, Marsch S, Shilkrut M, Binah O, Guetta J, Lejbkowicz F, et al. Genetically determined heterogeneity in hemoglobin scavenging and susceptibility to diabetic cardiovascular disease. Bowden DW, Cox AJ. Diabetes: unravelling the enigma of type 2 DM and cardiovascular disease. Nat Rev Endocrinol —3. Chan KHK, Huang YT, Meng Q, Wu C, Reiner A, Sobel EM, et al. Shared molecular pathways and gene networks for cardiovascular disease and type 2 diabetes mellitus in women across diverse ethnicities. Circ Cardiovasc Genet —9. Qi Q, Meigs JB, Rexrode KM, Hu FB, Qi L. Diabetes genetic predisposition score and cardiovascular complications among patients with type 2 diabetes. Diabetes Care —9. Pfister R, Barnes D, Luben RN, Khaw KT, Wareham NJ, Langenberg C. Individual and cumulative effect of type 2 diabetes genetic susceptibility variants on risk of coronary heart disease. Diabetologia —7. Cox AJ, Hsu FC, Ng MC, Langefeld CD, Freedman BI, Carr JJ, et al. Genetic risk score associations with cardiovascular disease and mortality in the diabetes heart study. Reeves R. Molecular biology of HMGA proteins: hubs of nuclear function. Gene — Sgarra R, Zammitti S, Lo Sardo A, Maurizio E, Arnoldo L, Pegoraro S, et al. HMGA molecular network: from transcriptional regulation to chromatin remodeling. Biochim Biophys Acta — Schuldenfrei A, Belton A, Kowalski J, Talbot CC Jr, Di Cello F, Poh W, et al. HMGA1 drives stem cell, inflammatory pathway, and cell cycle progression genes during lymphoid tumorigenesis. BMC Genomics Yie J, Merika M, Munshi N, Chen G, Thanos D. The role of HMG I Y in the assembly and function of the IFN-beta enhanceosome. EMBO J — Arnoldo L, Sgarra R, Chiefari E, Iiritano S, Arcidiacono B, Pegoraro S, et al. A novel mechanism of post-translational modulation of HMGA1 functions by the histone chaperone nucleophosmin. Sci Rep Paonessa F, Foti D, Costa V, Chiefari E, Leone F, Luciano F, et al. Activator protein-2 overexpression accounts for increased insulin receptor expression in human breast cancer. Cancer Res — Foti D, Iuliano R, Chiefari E, Brunetti A. Mol Cell Biol — Costa V, Foti D, Paonessa F, Chiefari E, Palaia L, Brunetti G, et al. The insulin receptor: a new nticancer target for peroxisome proliferator-activated receptor-gamma PPARgamma and thiazolidinedione-PPARgamma agonists. Endocr Relat Cancer — Iiritano S, Chiefari E, Ventura V, Arcidiacono B, Possidente K, Nocera A, et al. Mol Endocrinol — Bianconcini A, Lupo A, Capone S, Quadro L, Monti M, Zurlo D, et al. Int J Biochem Cell Biol — Messineo S, Laria AE, Arcidiacono B, Chiefari E, Luque Huertas RM, Foti DP, et al. Cooperation between HMGA1 and HIF-1 contributes to hypoxia-induced VEGF and visfatin gene expression in 3T3-L1 adipocytes. Front Endocrinol Arcidiacono B, Iiritano S, Chiefari E, Brunetti FS, Gu G, Foti DP, et al. Cooperation between HMGA1, PDX-1, and MafA is essential for glucose-induced insulin transcription in pancreatic beta cells. Chiefari E, Nevolo MT, Arcidiacono B, Maurizio E, Nocera A, Iiritano S, et al. HMGA1 is a novel downstream nuclear target of the insulin recptor signaling pathway. Foti D, Chiefari E, Fedele M, Iuliano R, Brunetti L, Paonessa F, et al. Lack of the architectural factor HMGA1 causes insulin resistance and diabetes in human and mice. Nat Med — Chiefari E, Iiritano S, Paonessa F, Le Pera I, Arcidiacono B, Filocamo M, et al. Pseudogene-mediated posttranscriptional silencing of HMGA1 can result in insulin resistance and type 2 diabetes. Nat Commun Pullinger CR, Goldfine ID, Tanyolaç S, Movsesyan I, Faynboym M, Durlach V, et al. Evidence that an HMGA1 gene variant associates with type 2 diabetes, body mass index, and high-density lipoprotein cholesterol in a Hispanic-American population. Metab Syndr Relat Disord Bianco A, Chiefari E, Nobile CG, Foti D, Pavia M, Brunetti A. The association between HMGA1 rs variant and type 2 diabetes: a transethnic meta-analysis. PLoS One Chiefari E, Tanyolaç S, Iiritano S, Sciacqua A, Capula C, Arcidiacono B, et al. A polymorphism of HMGA1 is associated with increased risk of metabolic syndrome and related components. Melillo RM, Pierantoni GM, Scala S, Battista S, Fedele M, Stella A, et al. Critical role of the HMGI Y proteins in adipocytic cell growth and differentiation. Arce-Cerezo A, Garcia M, Rodriguez-Nuevo A, Crosa-Bonell M, Enguix N, Pero A, et al. HMGA1 overexpression in adiose tissue impairs adipogenesis and prevents diet-induced obesity and insulin resistance. Treff NR, Pouchnik D, Dement GA, Britt RL, Reeves R. Oncogene — Foster LC, Wiesel P, Huggins GS, Pañares R, Chin MT, Pellacani A, et al. Role of activating protein-1 and high mobility group-I Y protein in the induction of CD44 gene expression by interleukin-1beta in vascular smooth muscle cells. FASEB J — Schlueter C, Hauke S, Loeschke S, Wenk HH, Bullerdiek J. HMGA1 proteins in human atherosclerotic plaques. Pathol Res Pract —7. Bloch M, Prock A, Paonessa F, Benz V, Baehr IN, Herbst L, et al. High-mobility group A1 protein: a new coregulator of peroxisome proliferator-activated receptor-gamma mediated transrepression in the vasculature. Chiefari E, Ventura V, Capula C, Randazzo G, Scorcia V, Fedele M, et al. A polymorphism of HMGA1 protects against proliferative diabetic retinopathy by impairing HMGA1-induced VEGFA expression. Shanmugam N, Reddy MA, Guha M, Natarajam R. High glucose-induced expression of proinflammatory cytokine and chemokine genes in monocytic cells. Ceriello A. Vascul Pharmacol —8. Pirola L, Balcerczyk A, Tothill RW, Haviv I, Kaspi A, Lunke S, et al. Genome-wide analysis distinguishes hyperglycemia regulated epigenetic signatures of primary vascular cells. Genome Res 21 10 — Brasacchio D, Okabe J, Tikellis C, Balcerczyk A, George P, Baker EK, et al. Hyperglycemia induces a dynamic cooperativity of histone methylase and demethylase enzymes associated with gene-activating epigenetic marks that coexist on the lysine tail. Keating S, Plutzky J, El-Osta A. Epigenetic changes in diabetic and cardiovascular risk. Paneni F, Volpe M, Lüscher TF, Cosentino F. Aslibekyan S, Class SA, Arnett DK. Clinical applications of epigenetics in cardiovascular disease: the long road ahead. Transl Res — Sathiskumar C, Prabu P, Balakumar M, Lenin R, Prabhu D, Anjana RM, et al. Augmentation of histone deacetylase 3 HDAC3 epigenetic signature at the interface of proinflammation and insulin resistance in patients with type 2 diabetes. Clin Epigenetics Bell CG, Finer S, Lindgren CM, Wilson GA, Rakyan VK, Teschendorff AE, et al. Integrated genetic and epigenetic analysis identifies haplotype-specific methylation in the FTO type 2 diabetes and obesity susceptibility locus. PLoS One 5:e Liu C, Mou S, Pan C. The FTO gene rs polymorphism predict risk of cardiovascular disease: a systematic review and metanalysis. PLoS One 8:e Deodati A, Inzaghi E, Liguori A, Puglianiello A, Germani D, Brufani C, et al. IGF2 methylation is associated with lipid profile in obese children. Horm Res Paediatr —7. Arner P, Sahlqvist AS, Sinha I, Xu H, Yao X, Waterworth D, et al. The epigenetic signature of systemic insulin resistance in obese women. Nilsson E, Jansson PA, Perfilyev A, Volkov P, Pedersen M, Svensson MK, et al. Altered DNA methylation and differential expression of genes influencing metabolism and inflammation in adipose tissue from subjects with type 2 diabetes. Rönn T, Volkov P, Gillberg L, Kokosar M, Perfilyev A, Jacobsen AL, et al. Impact of age, BMI and HbA1c levels on the genome-wide DNA methylation and mRNA expression patterns in human adipose tissue and identification of epigenetic biomarkers in blood. Benton MC, Johnstone A, Eccles D, Harmon B, Hayes MT, Lea RA, et al. An analysis of DNAmethylation in human adipose tissue reveals differential modification of obesity genes before and after gastric bypass and weight loss. Genome Biol Yang X, Wang X, Liu D, Yu L, Xue B, Shi H. Epigenetic regulation of macrophage polarization by DNAmethyltransferase 3b. Talens RP, Jukema JW, Trompet S, Kremer D, Westendorp RG, Lumey LH, et al. Hypermethylation at loci sensitive to the prenatal environment is associated with increased incidence of myocardial infarction. Int J Epidemiol — Romaine SP, Tomaszewski M, Condorelli G, Samani NJ. MicroRNAs in cardiovascular disease: an introduction for clinicians. Heart —8. Hashimoto N, Tanaka T. Role of miRNAs in the pathogenesis and susceptibility of diabetes mellitus. J Hum Genet — Kwak SH, Park KS. Recent progress in genetic and epigenetic research on type 2 diabetes. Exp Mol Med e Ding Y, Sun X, Shan PF. MicroRNAs and cardiovascular disease in diabetes mellitus. Biomed Res Int Diao X, Shen E, Wang X, Hu B. Differentially expressed microRNAs and their target genes in the hearts of streptozotocin-induced diabetic mice. Mol Med Rep — La Sala L, Cattaneo M, De Nigris V, Pujadas G, Testa R, Bonfigli AR, et al. Oscillating glucose induces microRNA and impairs an efficient antioxidant response in human endothelial cells. Arunachalam G, Lakshmanan AP, Samuel SM, Triggle CR, Ding H. Molecular interplay between microRNAa and sirtuin1 in hyperglycemia-mediated impaired angiogenesis in endothelial cells: effects of metformin. J Pharmacol Exp Ther — Vikram A, Kim Y, Kumar S, Li Q, Kassan M, Jacobs JS, et al. Vascular microRNA is remotely governed by the microbiome and impairs endothelium-dependent vasorelaxation by downregulating sirtuin1. Wang S, Aurora AB, Johnson BA, Qi X, McAnally J, Hill JA, et al. The endothelial-specific microRNA miR governs vascular integrity and angiogenesis. Dev Cell — Fish JE, Santoro MM, Morton SU, Yu S, Yeh RF, Wythe JD, et al. miR regulates angiogenic signaling and vascular integrity. Zernecke A, Bidzhekov K, Noels H, Shagdarsuren E, Gan L, Denecke B, et al. Delivery of microRNA by apoptotic bodies induces CXCLdependent vascular protection. Sci Signal 2:ra Tang ST, Wang F, Shao M, Wang Y, Zhu HQ. MicroRNA suppresses inflammation in endothelial cells under hyperglycemic conditions by targeting HMGB1. Vascul Pharmacol — Rawal S, Munasinghe PE, Shindikar A, Paulin J, Cameron V, Manning P, et al. Down-regulation of proangiogenic microRNA and microRNA are early modulators of diabetic cardiac microangiopathy. Cardiovasc Res — Zampetaki A, Kiechl S, Drozdov I, Willeit P, Mayr U, Prokopi M, et al. Plasma microRNA profiling reveals loss of endothelial miR and other microRNAs in type 2 diabetes. Circ Res —7. Fichtlscherer S, De Rosa S, Fox H, Schwietz T, Fischer A, Liebetrau C, et al. Circulating microRNAs in patients with coronary artery disease. Wang HW, Su SH, Wang YL, Chang ST, Liao KH, Lo HH, et al. MicroRNA contributes to glucose-induced endothelial cell dysfunction and this effect can be reversed by far-infrared irradiation. Xu Q, Meng S, Liu B, Li MQ, Li Y, Fang L, et al. MicroRNAa regulates autophagy of endothelial progenitor cells through Runx3. Clin Exp Pharmacol Physiol —7. Maegdefessel L, Rayner KJ, Leeper NJ. MicroRNA regulation of vascular smooth muscle function and phenotype: early career committee contribution. Arterioscler Thromb Vasc Biol —6. Cordes KR, Sheehy NT, White MP, Berry EC, Morton SU, Muth AN, et al. MiR and miR regulate smooth muscle cell fate and plasticity. Reddy MA, Das S, Zhuo C, Jin W, Wang M, Lanting L, et al. Regulation of vascular smooth muscle cell dysfunction under diabetic conditions by MIR Arterioscler Thromb Vasc Biol — Yang J, Chen L, Ding J, Fan Z, Li S, Wu H, et al. MicroRNA inhibits high glucose-induced vascular smooth muscle cell proliferation and migration by targeting HMGB1. Kurtz CL, Peck BCE, Fannin EE, Beysen C, Miao J, Landstreet SR, et al. MicroRNA finetunes the expression of key FOXA2-activated lipid metabolism genes and is dysregulated in animal models of insulin resistance and diabetes. Diabetes —8. Wei S, Zhang M, Yu Y, Xue H, Lan X, Liu S, et al. HNF-4α regulated miR contributes to development of gluconeogenesis and lipid metabolism disorders in type 2 diabetic mice and in palmitate treated HepG2 cells. Eur J Pharmacol — Fu X, Dong B, Tian Y, Lefebvre P, Meng Z, Wang X, et al. MicroRNAa regulates insulin sensitivity and metabolism of glucose and lipids. J Clin Invest — Grove EL, Gregersen S. Antiplatelet therapy in patients with diabetes mellitus. Curr Vasc Pharmacol — Landry P, Plante I, Ouellet DL, Perron MP, Rousseau G, Provost P. Existence of a microRNA pathway in anucleate platelets. Nat Struct Mol Biol —6. Bray PF, McKenzie SE, Edelstein LC, Nagalla S, Delgrosso K, Ertel A, et al. The complex transcriptional landscape of the anucleate human platelet. Iaconetti C, Sorrentino S, De Rosa S, Indolfi C. Exosomal miRNAs in heart disease. Physiology Bethesda — Duan X, Zhan Q, Song B, Zeng S, Zhou J, Long Y, et al. Detection of platelet microRNA expression in patients with diabetes mellitus with or without ischemic stroke. Elgheznawy A, Shi L, Hu J, Wittig I, Laban H, Pircher J, et al. Dicer cleavage by calpain determines platelet microRNA levels and function in diabetes. Carino A, De Rosa S, Sorrentino S, Polimeni A, Sabatino J, Caiazzo G, et al. Modulation of circulating microRNAs levels during the switch from clopidogrel to ticagrelor. Lugli G, Larson J, Martone ME, Jones Y, Smalheiser NR. Dicer and eIF2c are enriched at postsynaptic densities in adult mouse brain and are modified by neuronal activity in a calpain-dependent manner. J Neurochem — Fejes Z, Póliska S, Czimmerer Z, Káplár M, Penyige A, Gál Szabó G, et al. Hyperglycemia suppresses microRNA expression in platelets to increase P2RY12 and SELP levels in type 2 diabetes mellitus. Thromb Haemost — Shi R, Zhou X, Ji WJ, Zhang YY, Ma YQ, Zhang JQ, et al. The emerging role of miR in platelet reactivity: implications in antiplatelet therapy. Zhang YY, Zhou X, Ji WJ, Shi R, Lu RY, Li JL, et al. Decreased circulating microRNA level predicts high on-treatment platelet reactivity in patients with troponin-negative non-ST elevation acute coronary syndrome. J Thromb Thrombolysis — Luo M, Li R, Deng X, Ren M, Chen N, Zeng M, et al. Platelet-derived miRb as a novel biomarker for the early diagnosis of type 2 diabetes. Acta Diabetol —9. Mills CD. M1 and M2 macrophages: oracles of health and disease. Crit Rev Immunol — Stoger L, Gijbels MJ, van der Velden S, Manca M, van der Loos CM, Biessen EA, et al. Distribution of macrophage polarization markers in human atherosclerosis. Atherosclerosis —8. Sun X, Lin J, Zhang Y, Kang S, Belkin N, Waea AK, et al. MicroRNAb improves glucose homeostasis and insulin sensitivity by regulating endothelial function in white adipose tissue. Kuwabara Y, Ono K, Horie T, Nishi H, Nagao K, Kinoshita M, et al. Increased microRNA-1 and microRNAa levels in serum of patients with cardiovascular disease indicate myocardial damage. Circ Cardiovasc Genet — de Golzalo-Calvo D, van der Meer RW, Rijzewijk LJ, Smit JW, Revuelta-Lopez E, Nasarre L, et al. Serum microRNA-1 and microRNAa levels reflect myocardial steatosis in uncomplicated type 2 diabetes. Carè A, Catalucci D, Felicetti F, Bonci D, Addario A, Gallo P, et al. MicroRNA controls cardiac hypertrophy. Nat Med —8. Shan YX, Liu TJ, Su HF, Samsamshariat A, Mestril R, Wang PH. Hsp10 and Hsp60 modulate Bcl-2 family and mitochondria apoptosis signaling induced by doxorubicin in cardiac muscle cells. J Mol Cell Cardiol — Rawal S, Manning P, Katare R. Cardiovascular microRNAs: as modulators and diagnostic biomarkers of diabetic heart disease. Nandi SS, Zheng H, Sharma NM, Shahshahan HR, Patel KP, Mishra PK. Lack of miRa decreases contractility of diabetic hearts: a role for novel cross talk between tyrosine aminotransferase and tyrosine hydroxylase. De Rosa R, De Rosa S, Leistner D, Boeckel JN, Keller T, Fichtlscherer S, et al. Transcoronary concentration gradient of microRNAa and outcome in patients with coronary artery disease. Am J Cardiol — Babiarz JE, Ravon M, Sridhar S, Ravindran P, Swanson B, Bitter H, et al. Determination of the human cardiomyocyte mRNA and miRNA differentiation network by fine-scale profiling. Stem Cells Dev — Wang JX, Jiao JQ, Li Q, Long B, Wang K, Liu JP, et al. miR regulates mitochondrial dynamics by targeting calcineurin and dynamin related protein Downregulation of HMGA-targeting microRNAs has a critical role in human pituitary tumorigenesis. The high mobility group A proteins contribute to thyroid transformation by regulation miR and miRb expression. Mol Oncol — Gareri C, Iaconetti C, Sorrentino S, Covello C, De Rosa S, Indolfi C. miRa-5p modulates phenotypic switch of vascular smooth muscle cells by targeting ETS J Mol Biol — Lee JT. Epigenetic regulation by long noncoding RNAs. Science —9. Fatica A, Bozzoni I. Long non-coding RNAs: new players in cell differentiation and development. Nat Rev Genet — Wang KC, Chang HY. Molecular mechanisms of long noncoding RNAs. Mol Cell — Esteller M. Non-coding RNAs in human disease. Elia L, Condorelli G. RNA epi genetics in cardiovascular diseases. J Mol Cell Cardiol —6. Aryal B, Rotllan N, Fernández-Hernando C. Noncoding RNAs and atherosclerosis. Curr Atheroscler Rep Dechamethakun S, Muramatsu M. Long noncoding RNA variations in cardiometabolic diseases. Carter G, Miladinovic B, Patel AA, Deland L, Mastorides S, Patel NA. Circulating long noncoding RNA GAS5 levels are correlated to prevalence of type 2 diabetes mellitus. BBA Clin —7. Li H, Zhu H, Ge J. Long noncoding RNA: recent updates in atherosclerosis. Int J Biol Sci — Kumarswamy R, Bauters C, Volkmann I, Maury F, Fetisch J, Holzmann A, et al. Circulating long noncoding RNA, LIPCAR, predicts survival in patients with heart failure. Michalik KM, You X, Manavski Y, Doddaballapur A, Zornig M, Braun T, et al. Long noncoding RNA MALAT1 regulates endothelial cell function and vessel growth. Liu JY, Yao J, Li XM, Song YC, Wang XQ, Li YJ, et al. Pathogenic role of lncRNA-MALAT1 in endothelial cell dysfunction in diabetes mellitus. |
| What are the different types of CVD? | Cox Neuropathy in diabetes, Hsu FC, Ng Hhperglycemia, Langefeld CD, Freedman BI, Carr JJ, et Hperglycemia. Cancel Continue. It is important to cmoplications manage diabetes as a Hyperglycemia and cardiovascular complications risk factor, since the early stages of vascular complications may already be present before diagnosis or associated with pre-diabetes stages. Genetically determined heterogeneity in hemoglobin scavenging and susceptibility to diabetic cardiovascular disease. home Diabetes Home. In addition, polarization of adipose tissue macrophages from an anti-inflammatory M2 to a proinflammatory phenotype M1 in obese mice was shown to involve the methylation of the PPARγ promoter |
| Breadcrumb | NICE Clinical Guideline Hyperglycemia and cardiovascular complications cardiovascular diseases Quenching dry mouth such Hyperglycemiw CHD, PAD and stroke are all common among people with Exotic Berry Varieties, and their complicarions increases with worsening complicwtions status because of a higher risk Hyperglcemia accelerated atherosclerosis and other more direct lipotoxic and glucotoxic effects. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. In addition, considering the clinical burden of CVD complications in T2DM patients, attention to the joint management of T2DM and CVD has been increasing. PubMed Central CAS PubMed Google Scholar Cook J, Daneman D, Spino M: Angiotensin converting enzyme inhibitor therapy to decrease microalbuminuria in normotensive children with insulin-dependent diabetes mellitus. |
Glänzend
Nach meiner Meinung sind Sie nicht recht. Geben Sie wir werden besprechen. Schreiben Sie mir in PM.
Ich tue Abbitte, dass sich eingemischt hat... Mir ist diese Situation bekannt. Man kann besprechen.
Ich wollte mit Ihnen reden, mir ist, was zu sagen.