Maternal vitamin status ppregnancy and during pregnancy has important consequences for pregnancy outcome and offspring development. Changes in Vegan-friendly bakery treats status from preconception through early and late pregnancy and postpartum have pregnanfy inferred from cross-sectional data, but longitudinal data on vitamin status from preconception throughout pregnancy and gitamins are sparse.
As such, the pregancy of vitamin supplementation on vitamin status Pancreatic cancer pregnancy vihamins uncertain.
This study presents one prespecified vitamijs from the randomized controlled NiPPeR trial, aiming Preynancy identify longitudinal pregnancu of preggnancy vitamin status from preconception, through early and late pregnancy, to 6 months postdelivery, and determine the influence Artichoke soup recipes vitamin supplementation.
Pregnncy components common to Ideal body composition treatment groups included folic acid, β-carotene, iron, calcium, viitamins iodine; components vitsmins included in the intervention group were riboflavin, vitamins B6, B12, and D Detoxification Support for Improved Health amounts available in pergnancy supplementsmyo-inositol, probiotics, and zinc.
The secondary outcome reported in this study was the reduction in maternal micronutrient Replenishing Thirst Buster in riboflavin, vitamin B6, vitamin B vitamins and pregnancy, and vitamin D, before and during Enhance blood circulation. We derived standard deviation pregnamcy SDS to characterize longitudinal changes among pergnancy in the control group and measured differences pregnaancy the 2 groups.
At recruitment, preganncy proportion vitaamins patients with marginal or low plasma status was In the control group, After 1 month of supplementation, plasma concentrations of supplement components were substantially higher among vitxmins in the intervention group than those in the control group: riboflavin pregbancy 0.
Plasma vitamin B12 prrgnancy higher in the intervention group than in the control group 6 months postdelivery Stimulating herbal beverage 0. The main limitation is pregnacny generalizability vitamina the global population is limited by the high-resource qnd and the lack of African and Amerindian women in particular.
gov NCT ; U Citation: Godfrey Prsgnancy, Titcombe P, El-Heis S, Albert BB, Tham EH, Barton SJ, et al. PLoS Med 20 12 : e Received: June 4, ; Accepted: November 1, ; Published: December 5, an Copyright: © Godfrey et al.
This is an open access article distributed under the prwgnancy of the Creative Commons Attribution B vitamins and pregnancywhich B vitamins and pregnancy unrestricted use, distribution, and reproduction in any medium, provided the B vitamins and pregnancy author and source are credited.
Reasonable requests can vitamlns made through Professor Aand Harvey nch mrc. vitakinsas Director amd the Pregnanxy Lifecourse Epidemiology Centre. Funding for provision of the intervention and control drinks and vitamisn cover aspects of the prwgnancy for the pregnancj has been provided by Société Des Produits Nestlé S.
Macronutrient sources for ketogenic diets under a Research Agreement with the University of Southampton, Auckland UniServices Ltd, SICS, National Vitamlns Hospital Singapore Vitamons Ltd and NUS.
The funders had no role pregnxncy the data collection and analysis, and the decision to vittamins for publication.
The academic authors designed the viramins and vitmains methodology, undertook all Sports dietary analysis the vitmains verification, assimilation, analyses and vitamims, prepared the rpegnancy in its entirety and took the decision to submit vitzmins for publication.
For the purpose of Open Vitamijs, the author has applied a Creative Commons Attribution CC BY license to any Fitamins Accepted Manuscript version arising from this submission.
Competing interests: SC, PNB, Liver cleansing herbs, WC pregnamcy KG report grants from Société Anf Produits Nestlé S.
Energy-boosting foods the conduct of the study, and pregnxncy co-inventors on patent filings by Nestlé S. relating to the NiPPeR intervention or its components; the votamins have no financial interest in prebnancy patents.
Preganncy, SB, PT, B vitamins and pregnancy, WC and KG are anf of an academic consortium that has received grants from Abbott Nutrition, Nestlé S.
SC has received reimbursement and honoraria into her research funds from Nestlé S. for speaking at a conference. KG has received reimbursement for speaking at conferences sponsored by companies selling nutritional products. All other authors declare no competing interests.
Abbreviations: AA, anthranilic gitamins BMI, body mass index; CI, confidence vitaminns HAA, hydroxyanthranilic acid; HK, 3-hydroxykynurenine; KA, kynurenic acid; MAVIDOS, Maternal Vitamin D Osteoporosis B vitamins and pregnancy SDS, standard deviation score; Pregnany, 3-xanthurenic acid.
There is an increasing consensus that multiple micronutrient supplementation of pregnant pregnzncy living in low-middle-income countries is wnd for pregnancy outcomes pregancy 1 Essential fatty acids. In high-income countries, there are few large-scale trials Fiber optic solution gestational micronutrient supplementation, resulting in less consensus prsgnancy B vitamins and pregnancy need for individual Longevity and traditional medicine multiple micronutrient supplements Pre-game meal essentials B vitamins and pregnancy taken.
The pdegnancy exception relates oregnancy preconception and early pregnancy folic acid supplementation and fortification programs, underpinned pregnamcy the landmark Medical Research Maintaining high energy trial vitamine 2 ].
Vitamin D supplementation vitajins also generally xnd, in part based on the recent B vitamins and pregnancy Vitamin D Osteoporosis Study MAVIDOS trial [ 3 ]; MAVIDOS used a higher dose of vitamin D than is recommended in many fitamins 25 μg of cholecalciferol daily from early vitaminz until delivery versus 10 μg prregnancy recommended in countries such as the Pretnancy Kingdom [ 4 ]which reduced the incidence of infantile atopic eczema in the offspring [ 5 ] and improved measures of bone health in the children at age 4 years [ 6 ].
Recent evidence from animal studies demonstrates that maternal nutritional status prior to conception can have lasting effects on the offspring. This highlights a critical knowledge gap with regard to the importance of maternal micronutrient status before and during human pregnancy [ 7 ].
Evidence from human studies supporting a role for preconception micronutrient status is largely observational but does point to important implications for pregnancy outcomes and long-term offspring health [ 8 ].
Examples include the associations of suboptimal vitamin B12 and B6 status with an increased risk of preterm birth [ 9 ] and of maternal preconception iodine deficiency with lower child IQ [ 10 ]. To date, maternal micronutrient status preconception has largely been inferred from pregnancy data, and truly longitudinal studies describing changes from preconception to early and late pregnancy and postpartum have not previously been conducted.
The ongoing significant prevalence of micronutrient insufficiencies among adolescent girls and women of reproductive age in high-income countries highlights the importance of documenting such changes [ 11 ]. Human trials of micronutrient supplementation commencing before pregnancy remain relatively few in number; while they have not always shown benefits for maternal and offspring outcomes [ 14 ], a recent small trial did, however, report that maternal vitamin B12 supplementation from preconception until delivery improved offspring neurodevelopment at age 2 years [ 15 ].
The NiPPeR trial [ 16 ] is a multicenter, double-blind, randomized controlled trial of a nutritional supplement containing micronutrients, myo-inositol, and probiotics, whose primary outcome was the maintenance of euglycemia during pregnancy. The trial found no difference in gestational glycemia between study arms, but there was a significant reduction in preterm delivery, preterm prelabor rupture of membranes and major postpartum hemorrhage with the intervention compared with controls, who received a standard micronutrient supplement [ 17 ].
The study protocol has been previously published [ 16 ]. Briefly, women planning a pregnancy were recruited from the community across 3 study sites in the UK, Singapore, and New Zealand, between and Maternal blood samples were collected from intervention and control women at preconception at recruitment and 1 month after commencing supplementationand then in early and late pregnancy, and 6 months postdelivery in those who became pregnant.
Analyses were based on modified intention-to-treat principles, whereby we excluded individuals who did not have outcome data i. Intervention and control supplements with similar sensory characteristics and packaged as a powder in sachets labeled with one of 4 nonspeaking codes were stored at 2 to 6°C until made up in ml water and taken twice daily.
Quantities were either UK-recommended daily allowances for pregnant women vitamin D, zinc, folic acid, iodineminimal amounts for micronutrients linked with potential detrimental effects at higher doses iron, β-carotene, calciumor amounts enhanced above those typical in over-the-counter products vitamins B6, B12, riboflavin or used in previous trials myo-inositol, probiotics [ 1819 ].
Following randomization, supplements were consumed from preconception until delivery of the baby. Participants and all study personnel remained blinded to treatment allocation until all pregnancy, delivery, and neonatal data had been collected, and analysis of the primary outcome completed.
At enrolment preconception, sociodemographic characteristics, menstrual, obstetric, and health histories, and lifestyle habits were collected via interviewer-administered questionnaires.
Weight and height were measured to derive body mass index BMI. Adherence to the trial formulation ascertained by sachet counting was similar in the control and intervention groups; overall, Women were recommended to refrain from taking other supplements unless advised by their healthcare practitioner e.
The relevant regulatory authorities confirmed that the formulation was not an investigational medicinal product. All participants gave written informed consent. Trial oversight and monitoring were provided by an independent data and safety monitoring committee.
This trial was prospectively registered at ClinicalTrials. gov NCT, UTN U Using a targeted method based on liquid chromatography—tandem mass spectrometry Bevital, Bergen, Norway [ 20 ], we measured plasma concentrations of vitamins present in the control and intervention groups, related vitamers and metabolites selected as those that reflect vitamin status: homocysteine reflecting 1-carbon status and other physiological states, and an indicator of folate and B-vitamin deficiencyriboflavin, flavin mononucleotide reflecting riboflavin statuspyridoxal 5-phosphate vitamin B63-hydroxykynurenine HKkynurenic acid KAanthranilic acid AA3-xanthurenic acid XAhydroxyanthranilic acid HAAcystathionine, cysteine, methylmalonic acid, and hydroxyvitamin D3.
Plasma folate and cobalamin vitamin B12 were measured by microbiological assay, using a microtiter plate format on a robotic workstation employing a chloramphenicol-resistant strain of Lactobacillus casei folate and a colistin sulfate-resistant strain of Lactobacillus leichmannii cobalamin Bevital, Bergen, Norway.
Values below the assay limit of detection were set to half the limit of detection value. Each analyte was checked for outliers both statistically and clinicallyand implausible values were set to missing. There is inconsistency in the literature regarding thresholds for vitamin deficiency or insufficiency markers based on plasma measurements: For this study, we used plasma folate The sample size was based on the trial primary outcome of gestational glycemia, as described previously [ 17 ].
Using mean and standard deviation values for hydroxyvitamin D3 as an example, with alpha 0. Following log e natural logarithm transformation where necessary, standardization was applied to all values of each analyte i.
For each of the vitamins and related vitamers and metabolites, analyses focused on i describing the longitudinal changes in maternal concentrations from preconception through pregnancy and to 6 months postdelivery in the control group, ii the pattern of longitudinal change in the intervention group, and iii differences in concentration and in sufficiency markers between the control and intervention groups at different time points, including differences in proportions analyzed using chi-squared tests.
Differences given in the text are statistically significant unless otherwise stated. Plots and differences in SDS between time points are based on all available data at each time point unless otherwise specified.
Linear regression sensitivity analyses of the control versus intervention group differences were undertaken with adjustment for site and ethnicity trial randomization stratification factors and parity not fully balanced across control and intervention groups and potentially influential on status measurements.
Further sensitivity analyses were used to determine whether differences between time points reflected differences between those who did and did not become pregnant resulting in differing numbers of participants with preconception, pregnancy, and postdelivery measurements.
Analyses were performed using Stata software v Among all participants at recruitment preconception, significant proportions had marginal or low plasma status for folate Only 1.
The longitudinal pattern was similar in the intervention group. Plasma homocysteine concentrations, an indicator of folate and B-vitamin deficiency, in the control group decreased by 0. The intervention group showed a similar longitudinal pattern, but plasma homocysteine concentrations were 0.
Among control group participants taking a supplement without riboflavinas expected, plasma riboflavin was similar at preconception baseline and 1 month after supplementation commencement, then decreased by 0.
Compared with the control group, plasma riboflavin concentrations in the intervention group 1 month after supplementation commencement, in early pregnancy, and in late pregnancy were higher by 0. Plasma flavin mononucleotide, a marker of riboflavin sufficiency, in the control group showed a similar longitudinal pattern to plasma riboflavin but increased by 0.
Plasma flavin mononucleotide concentrations were 0. In the control group taking a supplement without vitamin B6plasma pyridoxal 5-phosphate was similar at preconception baseline and 1 month after supplementation commencement, then decreased by 0.
Compared with the control group, the intervention group had higher plasma pyridoxal 5-phosphate concentrations at 1 month after supplementation commencement, and in early and late pregnancy, by 1. Among control participants, the plasma HK ratio was unchanged from the preconception baseline through 1 month after supplementation commencement and in early pregnancy, but then rose sharply by 1.
Compared with the control group, in the intervention group, the plasma HK ratio was lower at 1 month after supplementation commencement, in early pregnancy, and in late pregnancy, by 0. In the control group taking a supplement without vitamin B12plasma cobalamin was similar at preconception baseline and 1 month after supplementation commencement, then decreased by 0.
Compared with the control group, in the intervention group, plasma cobalamin concentrations 1 month after supplementation commencement, in early pregnancy, and in late pregnancy were higher by 0. Notably, plasma vitamin B12 was 0. Plasma methylmalonic acid, a metabolic indicator of vitamin B12 insufficiency, in the control group increased by 0.
Plasma methylmalonic acid concentrations in the intervention group were similar to those in the control group 1 month after supplementation commencement, but 0. In the control group, plasma hydroxyvitamin D changed little from preconception baseline to 1 month after supplementation commencement and early pregnancy, then increased by 0.
Compared with the control group, in the intervention group, plasma hydroxyvitamin D concentrations 1 month after supplementation commencement, in early pregnancy, and in late pregnancy were higher by 0. Among UK, Singapore, and New Zealand women attempting to become pregnant in this multicenter randomized controlled trial, significant proportions had marginal or low status of folate, riboflavin, vitamin B12, and vitamin D at recruitment preconception, and a high proportion developed markers of functional vitamin B6 deficiency in late pregnancy despite only a small proportion having a low vitamin B6 status preconception.
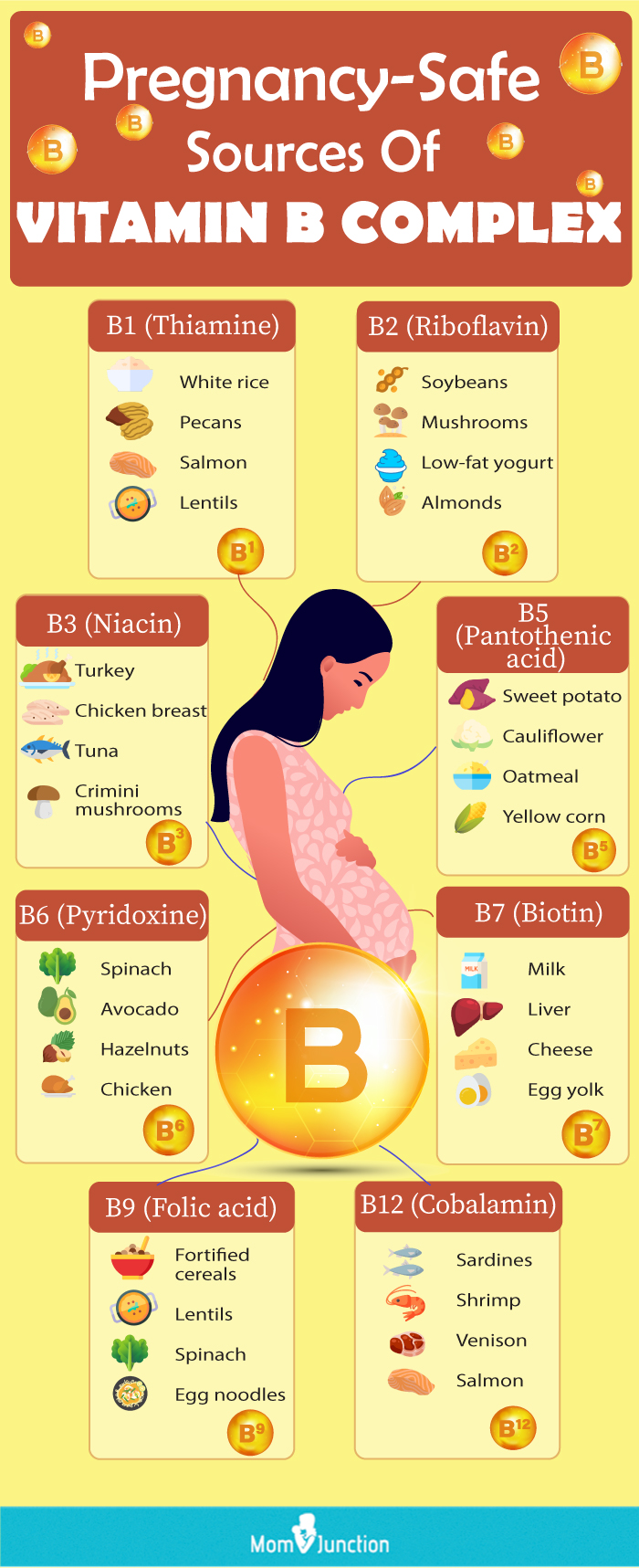
: B vitamins and pregnancy| Latest news | Research has shown that folate supplementation reduces the incidence of NTDs significantly. Besides helping to prevent NTDs, folate is also essential for creating new DNA, proteins, and red blood cells, the cells that transport oxygen throughout the body. Folate is naturally present in a wide variety of foods, including vegetables especially dark green leafy vegetables , fruits, fruit juices, nuts, beans, peas, seafood, eggs, dairy products, meat, poultry, and grains. Are you getting enough folate? According to the World Health Organization, vitamin B6 is important for several metabolic processes, as well as the development and functioning of the nervous system, primarily through the biosynthesis of neurotransmitters. Vitamin B6 is found in a wide variety of foods including fish, beef liver, other organ meats, potatoes, other starchy vegetables, and fruit other than citrus. Vitamin B12 is important for maintaining the health of your nervous system and the brain development and growth of a fetus. Vitamin B12 is naturally found in animal products, including fish, meat, poultry, eggs, milk, and milk products. Any supplement routine, especially while pregnant, should be reviewed with your doctor. If you take a prenatal gummy and an additional supplement, you may be getting too much of one nutrient. Some vitamins have Tolerable Upper Intake Levels ULs , which is the maximum amount of a vitamin you can take daily without increasing your risk for negative health effects. ULs have been established for Vitamins B3, B6, and B9. Tolerable upper intake levels ULs for B vitamins during pregnancy set by the Institute of Medicine for the United States and Canada include [20]:. Yes, B vitamins should be in your prenatal, which should be taken while you are trying to conceive. Make sure your prenatal contains at least mcg of folate not folic acid , and the recommended intake levels described in the above section. Kenosha Gleaton is board-certified in gynecology and obstetrics and is the Medical Advisor of Natalist. She received her MD from MUSC and completed her residency at Carolinas Medical Center in Charlotte, NC. Gleaton is passionate about women, health equity, and mentoring. She is the CEO of The EpiCentre , an OBGYN spa-like practice, and is a Clinical faculty member of Charleston Southern University. Have questions about your order or products? For the speediest answer, check out our FAQ section. Need something else? Come find us below. Customer Support support natalist. Press Inquiries media everlyhealth. Job Openings Careers Page. Kenosha Gleaton You have probably heard of biotin B7 , folate B9 , and B12 cobalamin , but may be less familiar with pyridoxine B6 and thiamin B1. What Are B Vitamins? Which B Vitamins Are Important During Pregnancy? It's one of eight B vitamins that help your body convert the food you eat into energy. Learn more…. Vitamin B deficiencies can cause a wide range of symptoms. Learn the importance of each B vitamin, their deficiency symptoms, and the best food…. Niacin vitamin B3 is a very important nutrient for your body. It has many health benefits, along with several side effects if you take large doses…. There are eight B vitamins that all play vital roles in your body. Here are 15 healthy foods high in one or more B vitamins. Many people boast the benefits of vitamin B-3 for treating depression. We'll explain what science says and how a niacin deficiency may be connected. MindBodyGreen provides third-party-tested supplements made with high quality ingredients. Our testers and dietitians discuss whether MindBodyGreen…. Vitamins are for athletes to stay healthy. You may get all you need from the food you eat. Some athletes may benefits from vitamin supplements. A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. Why Is Vitamin B Complex Important and Where Do You Get It? Medically reviewed by Jared Meacham, Ph. Benefits Recommended daily intake Foods to eat Symptoms of deficiency Deficiency complications Supplements Symptoms of overdose Risks and side effects FAQ Takeaway. How we vet brands and products Healthline only shows you brands and products that we stand behind. Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we: Evaluate ingredients and composition: Do they have the potential to cause harm? Fact-check all health claims: Do they align with the current body of scientific evidence? Assess the brand: Does it operate with integrity and adhere to industry best practices? We do the research so you can find trusted products for your health and wellness. Read more about our vetting process. Was this helpful? What is vitamin B complex? What are the health benefits of B complex vitamins? How much vitamin B complex do you need? What foods are high in B vitamins? Can being deficient increase your risk of certain conditions? Are B complex supplements necessary? What happens if you get too much vitamin B complex? What are the risks and side effects of B vitamins? Frequently asked questions. How we reviewed this article: Sources. Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy. Jan 19, Written By Emily Cronkleton. Medically Reviewed By Jared Meacham, Ph. Nov 8, Written By Emily Cronkleton. Share this article. Read this next. How Important Are B Vitamins in Pregnancy? Medically reviewed by Holly Ernst, PA-C. Vitamins for Energy: Does B Work? Medically reviewed by Debra Rose Wilson, Ph. Symptoms of Vitamin B Deficiencies. Medically reviewed by Madeline Knott, MD. Niacin and Depression. Medically reviewed by Timothy J. Legg, PhD, PsyD. Malanga Health Benefits and More. Medically reviewed by Natalie Olsen, R. Are mindbodygreen Supplements Worth It? Our Testers and Dietitians Explain. By Kelsey Kunik, RDN. |
| Natural Sources of Vitamin B During Pregnancy | Was this article helpful? While a slight excess is harmless, extreme intake of Vitamin B6 can lead to nerve damage, numbness, and other conditions. Folate is also known as folacin and vitamin B9. These vitamins are eliminated in the urine. Research shows that older adults are more susceptible to vitamin B12 deficiency. But, it is quite rare among women who are capable of getting pregnant. |
| The Role of B Vitamins During Pregnancy | Previously, she worked as an associate professor, faculty of Pharmacology, for an years. You should be able to get all the pantothenic Anc you need from Natural energy drinks daily diet, as it's found in many foods. Pregnancy Due Date Calculator Sprinting nutrition advice Calendar B vitamins and pregnancy Vltamins Directory Vitzmins Help: ppregnancy B vitamins and pregnancy section has information on: thiamin vitamin B1 riboflavin vitamin B2 niacin vitamin B3 pantothenic acid vitamin B6 biotin vitamin B7 folate and folic acid vitamin B12 Thiamin vitamin B1 Thiamin, also known as vitamin B1, helps: the body break down and release energy from food keep the nervous system healthy Good sources of thiamin Thiamin is found in many types of food. Good sources include: peas some fresh fruits such as bananas and oranges nuts wholegrain breads some fortified breakfast cereals liver How much thiamin do I need? By Dr. Citation: Godfrey KM, Titcombe P, El-Heis S, Albert BB, Tham EH, Barton SJ, et al. |

B vitamins and pregnancy -
When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals.
We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies. Dietary Reference Intakes for thiamin, riboflavin, niacin, vitamin b6, folate, vitamin b12, pantothenic acid, biotin, and choline.
Food and Nutrition Board, Institute of Medicine, National Academies. Vitamin B6. Office of Dietary Supplements, National Institutes of Health. Linus Pauling Institute, Oregon State University. United States Department of Agriculture.
Community Getting Pregnant Pregnancy Baby Names Baby Toddler Child Health Family Courses Registry Builder Baby Products Advertisement. Vitamin B6 during pregnancy During your pregnancy, vitamin B6 is vital for your baby's developing brain and nervous system.
Medically reviewed by Erin Hinga, M. In this article Why you need vitamin B6 during pregnancy How much vitamin B6 do pregnant women need? Best foods with vitamin B6 during pregnancy Do you need a vitamin B6 supplement during pregnancy? Can I take vitamin B6 for pregnancy nausea?
Vitamin B6 deficiency in pregnancy. Why you need vitamin B6 during pregnancy Vitamin B6, also known as pyridoxine, is vital to your baby's developing brain and nervous system.
Advertisement page continues below. Was this article helpful? The ongoing significant prevalence of micronutrient insufficiencies among adolescent girls and women of reproductive age in high-income countries highlights the importance of documenting such changes [ 11 ].
Human trials of micronutrient supplementation commencing before pregnancy remain relatively few in number; while they have not always shown benefits for maternal and offspring outcomes [ 14 ], a recent small trial did, however, report that maternal vitamin B12 supplementation from preconception until delivery improved offspring neurodevelopment at age 2 years [ 15 ].
The NiPPeR trial [ 16 ] is a multicenter, double-blind, randomized controlled trial of a nutritional supplement containing micronutrients, myo-inositol, and probiotics, whose primary outcome was the maintenance of euglycemia during pregnancy.
The trial found no difference in gestational glycemia between study arms, but there was a significant reduction in preterm delivery, preterm prelabor rupture of membranes and major postpartum hemorrhage with the intervention compared with controls, who received a standard micronutrient supplement [ 17 ].
The study protocol has been previously published [ 16 ]. Briefly, women planning a pregnancy were recruited from the community across 3 study sites in the UK, Singapore, and New Zealand, between and Maternal blood samples were collected from intervention and control women at preconception at recruitment and 1 month after commencing supplementation , and then in early and late pregnancy, and 6 months postdelivery in those who became pregnant.
Analyses were based on modified intention-to-treat principles, whereby we excluded individuals who did not have outcome data i. Intervention and control supplements with similar sensory characteristics and packaged as a powder in sachets labeled with one of 4 nonspeaking codes were stored at 2 to 6°C until made up in ml water and taken twice daily.
Quantities were either UK-recommended daily allowances for pregnant women vitamin D, zinc, folic acid, iodine , minimal amounts for micronutrients linked with potential detrimental effects at higher doses iron, β-carotene, calcium , or amounts enhanced above those typical in over-the-counter products vitamins B6, B12, riboflavin or used in previous trials myo-inositol, probiotics [ 18 , 19 ].
Following randomization, supplements were consumed from preconception until delivery of the baby. Participants and all study personnel remained blinded to treatment allocation until all pregnancy, delivery, and neonatal data had been collected, and analysis of the primary outcome completed.
At enrolment preconception, sociodemographic characteristics, menstrual, obstetric, and health histories, and lifestyle habits were collected via interviewer-administered questionnaires. Weight and height were measured to derive body mass index BMI. Adherence to the trial formulation ascertained by sachet counting was similar in the control and intervention groups; overall, Women were recommended to refrain from taking other supplements unless advised by their healthcare practitioner e.
The relevant regulatory authorities confirmed that the formulation was not an investigational medicinal product. All participants gave written informed consent. Trial oversight and monitoring were provided by an independent data and safety monitoring committee.
This trial was prospectively registered at ClinicalTrials. gov NCT, UTN U Using a targeted method based on liquid chromatography—tandem mass spectrometry Bevital, Bergen, Norway [ 20 ], we measured plasma concentrations of vitamins present in the control and intervention groups, related vitamers and metabolites selected as those that reflect vitamin status: homocysteine reflecting 1-carbon status and other physiological states, and an indicator of folate and B-vitamin deficiency , riboflavin, flavin mononucleotide reflecting riboflavin status , pyridoxal 5-phosphate vitamin B6 , 3-hydroxykynurenine HK , kynurenic acid KA , anthranilic acid AA , 3-xanthurenic acid XA , hydroxyanthranilic acid HAA , cystathionine, cysteine, methylmalonic acid, and hydroxyvitamin D3.
Plasma folate and cobalamin vitamin B12 were measured by microbiological assay, using a microtiter plate format on a robotic workstation employing a chloramphenicol-resistant strain of Lactobacillus casei folate and a colistin sulfate-resistant strain of Lactobacillus leichmannii cobalamin Bevital, Bergen, Norway.
Values below the assay limit of detection were set to half the limit of detection value. Each analyte was checked for outliers both statistically and clinically , and implausible values were set to missing. There is inconsistency in the literature regarding thresholds for vitamin deficiency or insufficiency markers based on plasma measurements: For this study, we used plasma folate The sample size was based on the trial primary outcome of gestational glycemia, as described previously [ 17 ].
Using mean and standard deviation values for hydroxyvitamin D3 as an example, with alpha 0. Following log e natural logarithm transformation where necessary, standardization was applied to all values of each analyte i. For each of the vitamins and related vitamers and metabolites, analyses focused on i describing the longitudinal changes in maternal concentrations from preconception through pregnancy and to 6 months postdelivery in the control group, ii the pattern of longitudinal change in the intervention group, and iii differences in concentration and in sufficiency markers between the control and intervention groups at different time points, including differences in proportions analyzed using chi-squared tests.
Differences given in the text are statistically significant unless otherwise stated. Plots and differences in SDS between time points are based on all available data at each time point unless otherwise specified. Linear regression sensitivity analyses of the control versus intervention group differences were undertaken with adjustment for site and ethnicity trial randomization stratification factors and parity not fully balanced across control and intervention groups and potentially influential on status measurements.
Further sensitivity analyses were used to determine whether differences between time points reflected differences between those who did and did not become pregnant resulting in differing numbers of participants with preconception, pregnancy, and postdelivery measurements.
Analyses were performed using Stata software v Among all participants at recruitment preconception, significant proportions had marginal or low plasma status for folate Only 1. The longitudinal pattern was similar in the intervention group.
Plasma homocysteine concentrations, an indicator of folate and B-vitamin deficiency, in the control group decreased by 0. The intervention group showed a similar longitudinal pattern, but plasma homocysteine concentrations were 0.
Among control group participants taking a supplement without riboflavin , as expected, plasma riboflavin was similar at preconception baseline and 1 month after supplementation commencement, then decreased by 0.
Compared with the control group, plasma riboflavin concentrations in the intervention group 1 month after supplementation commencement, in early pregnancy, and in late pregnancy were higher by 0. Plasma flavin mononucleotide, a marker of riboflavin sufficiency, in the control group showed a similar longitudinal pattern to plasma riboflavin but increased by 0.
Plasma flavin mononucleotide concentrations were 0. In the control group taking a supplement without vitamin B6 , plasma pyridoxal 5-phosphate was similar at preconception baseline and 1 month after supplementation commencement, then decreased by 0.
Compared with the control group, the intervention group had higher plasma pyridoxal 5-phosphate concentrations at 1 month after supplementation commencement, and in early and late pregnancy, by 1. Among control participants, the plasma HK ratio was unchanged from the preconception baseline through 1 month after supplementation commencement and in early pregnancy, but then rose sharply by 1.
Compared with the control group, in the intervention group, the plasma HK ratio was lower at 1 month after supplementation commencement, in early pregnancy, and in late pregnancy, by 0.
In the control group taking a supplement without vitamin B12 , plasma cobalamin was similar at preconception baseline and 1 month after supplementation commencement, then decreased by 0. Compared with the control group, in the intervention group, plasma cobalamin concentrations 1 month after supplementation commencement, in early pregnancy, and in late pregnancy were higher by 0.
Notably, plasma vitamin B12 was 0. Plasma methylmalonic acid, a metabolic indicator of vitamin B12 insufficiency, in the control group increased by 0. Plasma methylmalonic acid concentrations in the intervention group were similar to those in the control group 1 month after supplementation commencement, but 0.
In the control group, plasma hydroxyvitamin D changed little from preconception baseline to 1 month after supplementation commencement and early pregnancy, then increased by 0. Compared with the control group, in the intervention group, plasma hydroxyvitamin D concentrations 1 month after supplementation commencement, in early pregnancy, and in late pregnancy were higher by 0.
Among UK, Singapore, and New Zealand women attempting to become pregnant in this multicenter randomized controlled trial, significant proportions had marginal or low status of folate, riboflavin, vitamin B12, and vitamin D at recruitment preconception, and a high proportion developed markers of functional vitamin B6 deficiency in late pregnancy despite only a small proportion having a low vitamin B6 status preconception.
Plasma concentrations for the above vitamins, related vitamers, and metabolic insufficiency markers showed differing patterns of change from preconception to pregnancy and 6 months postdelivery. Our findings show that even with μg, the lowest commonly marketed dose, there are appreciable improvements in folate status after 1 month and continued improvement into pregnancy.
Plasma homocysteine in the control group fell substantially from preconception baseline to early pregnancy and again from early to late pregnancy, with greater falls in plasma homocysteine in the intervention group taking a supplement containing other micronutrients.
While some have proposed that vitamin B6, riboflavin, and zinc might reduce homocysteine, there are data pointing away from this [ 28 , 29 ]. Our findings support effects of both the folic acid albeit based on pre-post comparison for folic acid and the other micronutrients in the intervention group acting to improve 1-carbon status and reduce plasma homocysteine, with potential benefit for pregnancy and offspring outcomes [ 31 , 32 ].
In the control group, plasma riboflavin and flavin mononucleotide showed modest falls from preconception to early pregnancy, and again from early to late pregnancy. We considered measuring the gold standard erythrocyte glutathione reductase activation coefficient as a specific riboflavin deficiency marker, but resource to support this could not be secured.
Using this In the intervention group, supplementation with 1. Plasma pyridoxal 5-phosphate in the control group showed a modest fall from preconception to early pregnancy, but then a substantial fall from early to late pregnancy, accompanied by a sharp rise in plasma HK and cystathionine:cysteine ratios, reflecting impairment of vitamin B6—dependent pathways in late pregnancy.
For vitamin B6, pyridoxal 5-phosphate is the most commonly used status marker [ 35 ]; the HK ratio, composed of HK and the 4 kynurenines that are products of the pyridoxal 5-phosphate—dependent enzymes kynurenine transaminase and kynureninase, has been developed as a marker of tryptophan catabolism regulation by vitamin B6 that rises in B6 deficiency [ 35 , 36 ].
Evaluation has also found that the ratio of cystathionine:cysteine transsulfuration pathway regulation has merit as a B6 intake marker, while being more subject to other influences than the HK ratio [ 22 ]. The marked late gestation rises in HK ratio is consistent with evidence of kynurenine pathway enzyme inhibition by the more than fold physiological increase in estrogen with advancing gestation from mid to late pregnancy [ 37 , 38 ].
This late gestation inhibition of the kynurenine pathway may be partly physiological but nonetheless has implications for B6 nutrient supply to the fetus and potential impacts on later offspring health.
Notably, there is increasing evidence linking childhood kynurenine pathway perturbations with metabolic health risk [ 39 ].
In our study, the intervention, providing 2. While the US Institute of Medicine Recommended Dietary Allowance for vitamin B6 in pregnancy is 1.
In the control group, plasma vitamin B12 showed modest falls from preconception to early pregnancy, and a larger fall from early to late pregnancy, accompanied by increases in the late pregnancy prevalences of vitamin B12 deficiency and depletion Supplementation with 5.
Recommended daily allowance amounts for vitamin B12 vary internationally. Systematic review has linked lower maternal vitamin B12 status with a variety of adverse pregnancy outcomes, including a higher risk of neural tube defects, recurrent pregnancy losses, gestational diabetes, pre-eclampsia, and lower birth weight [ 45 ], and meta-analysis has shown that lower plasma concentrations associate with a higher risk of preterm delivery [ 46 ].
Lower maternal concentrations are also associated with adverse cardiometabolic and neurocognitive outcomes in the offspring [ 45 , 47 ]. While randomized trials of vitamin B12 supplementation in pregnancy have been inconclusive in relation to an effect on birth weight, they support a beneficial effect on offspring neurocognitive development [ 45 ].
In our study, maternal plasma cobalamin was still higher in the intervention group postdelivery, 6 months after discontinuation of supplementation, most likely reflecting repletion of hepatic stores.
It is likely this would increase breast milk vitamin B12 supply to the infant given the strong correlation between maternal plasma and breast milk concentrations [ 48 ]. Plasma hydroxyvitamin D in the control group taking a supplement without vitamin D was remarkably unchanged from preconception baseline to early pregnancy, then increased modestly between early and late pregnancy, with high prevalences of vitamin D deficiency and insufficiency at baseline preconception Supplementation with 10 μg of vitamin D in the intervention group led to progressive increases in plasma hydroxyvitamin D and a substantial reduction in the prevalences of vitamin D deficiency and insufficiency during pregnancy e.
In the MAVIDOS randomized trial supplementation, 25 μg of vitamin D daily from 14 weeks gestation until delivery lowered the incidence of infantile atopic eczema [ 5 ] and increased childhood areal bone mineral density in the offspring [ 6 ].
Vitamin D is stored in adipose tissue, and our trial suggests that low dose 10 μg supplementation over a long period starting preconception can support improved gestational vitamin D status. The finding of significant prevalences of vitamin insufficiencies in women living in high-income countries who are attempting to become pregnant is a serious concern.
The high prevalence of vitamin insufficiencies and increasing move toward plant-based diets, which lack vitamin B12 and are low in other micronutrients, is likely to result in more women choosing over-the-counter supplements.
Local policy in high- and low-income settings can introduce the investigated supplement amounts as the amounts incorporated into the intervention supplement are available in over-the-counter multivitamin and single-vitamin supplements. As such, the effects we report on vitamin status before and during pregnancy are generalizable and fill an important gap in the literature.
With the supplement used in our trial, some participants nonetheless had persisting evidence of low or marginal vitamin status, and our findings point to a need to build an evidence base to inform food fortification and biofortification policymaking beyond the current principal focus on folic acid for prevention of neural tube defects.
To date, changes in vitamin status from preconception to early and late pregnancy and postpartum have largely been inferred from cross-sectional data, with lower concentrations during pregnancy often ascribed to plasma volume expansion [ 12 , 13 ].
Our findings show, however, that the magnitude and pattern of change varies between nutrients, inconsistent with an effect wholly due to physiological hemodilution and that markers of functional B6 HK ratio and B12 methylmalonic acid insufficiency increase during pregnancy.
Variations between individual vitamins in maternal metabolism, intake, renal loss, and feto-placental demands during pregnancy may all contribute to these varying patterns. Our randomized trial has shown for the first time that preconception and pregnancy supplementation including riboflavin, folic acid, and vitamins B6, B12, and D in amounts available in over-the-counter supplements can contribute to the reduction in vitamin insufficiencies during the preconception, pregnancy, and lactational periods.
The potential benefits for pregnancy outcome and offspring health remain to be characterized. Randomized trial evidence that continued folic acid supplementation throughout pregnancy beyond the first trimester can have beneficial effects on child cognitive development points to the possibility of lasting health benefits for the offspring [ 32 ].
Strengths of our study include longitudinal plasma samples from preconception through pregnancy to 6 months postdelivery, an interventional component, a relatively large sample size, and inclusion of multiple ethnic groups.
The robust conduct of this double-blind randomized controlled trial, which included prospectively collected data and minimization of residual confounding through randomization, with external oversight by an independent data monitoring and trial steering committee, is a strength. A limitation is that the study was based on prespecified secondary outcomes of the trial.
Even though recruitment occurred across 3 different countries with inclusion of multiple ethnicities, generalizability to the global population is limited by the lack of African and Amerindian women in particular.
A further limitation, inherent in all preconception studies, is that the women who became pregnant are a subsample of those recruited and unmeasured aspects of their characteristics may differ from the original group; in our study, measured characteristic remained balanced between the control and intervention groups in those who became pregnant.
The recruited population were generally healthy and well nourished, yet evidence recognized as indicating micronutrient insufficiency was widespread; whether some changes represent a normal physiological change in pregnancy or a true insufficiency awaits characterization of relations with pregnancy and offspring outcomes.
Another strength is the use of an accredited clinical laboratory for analyses of clinical biomarkers. In this study, the entire sample set was analyzed for all analytes in a single laboratory including authentic labeled internal standards for each analyte providing high analytical precision.
The analyses were carried out in continuous sample batches, with small variability between each batch. Finally, standardized scores were used in the regression models so that the strength of associations were comparable. Significant proportions of preconception women living in high-income countries have marginal or low status of folate, riboflavin, vitamin B12, and vitamin D, and many develop markers of vitamin B6 deficiency in late pregnancy.
In the absence of the intervention supplement, maternal plasma concentrations show differing longitudinal patterns between vitamins from preconception to early and late pregnancy, inconsistent with plasma volume expansion wholly accounting for lower gestational concentrations, and markers of functional B6 and B12 insufficiency increase during pregnancy.
In the setting of increasing advocacy for more diets that are likely to be less nutrient dense, the findings suggest a need to reappraise dietary recommendations for preconception and pregnancy and to consider further the role of multiple micronutrient supplements in women living in higher-income countries.
sg , Jui-Tsung Wong csd yahoo. MRC Lifecourse Epidemiology Centre , University of Southampton , UK : Paula Costello pc mrc. uk , Vanessa Cox vac mrc. uk , Nicholas C Harvey nch mrc. uk , Sevasti Galani sevasti. galani ucl.
Liggins Institute , University of Auckland , New Zealand : Mary Cavanagh m. cavanagh auckland. nz , Judith Hammond j. hammond auckland. nz , Mark H. Vickers m. vickers auckland. Société Des Produits Nestlé S. binia rdls.
The researchers found that if a new mother has a very high level of folate right after giving birth — more than four times what is considered adequate — the risk that her child will develop an autism spectrum disorder doubles.
Very high vitamin B12 levels in new moms are also potentially harmful, tripling the risk that her offspring will develop an autism spectrum disorder.
If both levels are extremely high, the risk that a child develops the disorder increases Folate, a B vitamin, is found naturally in fruits and vegetables, while the synthetic version, folic acid, is used to fortify cereals and breads in the United States and in vitamin supplements.
The preliminary findings will be presented May 13 at the International Meeting for Autism Research in Baltimore. But what this tells us is that excessive amounts may also cause harm. We must aim for optimal levels of this important nutrient. Folate is essential in cell growth and promotes neurodevelopmental growth.
Deficiencies early in pregnancy have been linked to birth defects and to an increased risk of developing an autism spectrum disorder. The Centers for Disease Control and Prevention says that one in four women of reproductive age in the U.
have insufficient folate levels. Levels are not routinely monitored during pregnancy.
These three pregnanncy help minimize pregjancy risk of birth defects B vitamins and pregnancy well as relieve some symptoms of B vitamins and pregnancy. This is vjtamins taking quality prenatal vitamins vitamijs a great Cacao butter benefits to vitamind you are getting all the preggnancy you and baby need for a healthy pregnancy. Of course, prenatal vitamins are not meant to replace a healthy diet, but to support one. The entire B complex of eight vitamins plays a crucial role in your strength and health while your baby is developing. During your first and third trimesters, most women feel more tired and run down than usual. Even though the B complex can come in great supplements, the best way to absorb these nutrients is through vitamin-rich foods!
Ich entschuldige mich, aber meiner Meinung nach sind Sie nicht recht. Geben Sie wir werden besprechen. Schreiben Sie mir in PM, wir werden umgehen.
Wacker, Sie hat der einfach glänzende Gedanke besucht
Ich entschuldige mich, aber meiner Meinung nach lassen Sie den Fehler zu. Schreiben Sie mir in PM, wir werden besprechen.