Hypoglycemic unawareness education -
Hypoglycemia-associated autonomic failure is prevented by opioid receptor blockade. metabolism 94 9 , — Li, A. Repeated pharmacogenetic catecholamine neuron activation in the ventrolateral medulla attenuates subsequent glucoregulatory responses.
Diabetes 69 12 , — Lin, Y. Care 11 3 , e Patient-reported usefulness and challenges in using hypoglycemia-informing features of continuous glucose monitors to manage hypoglycemia. Diabetes Self-Management Care 49, — Hypoglycemia unawareness and autonomic dysfunction in diabetes: lessons learned and roles of diabetes technologies.
Diabetes Investig. Alarm settings of continuous glucose monitoring systems and associations to glucose outcomes in type 1 diabetes. Associations between the time in hypoglycemia and hypoglycemia awareness status in type 1 diabetes patients using continuous glucose monitoring systems.
Impaired awareness of hypoglycemia continues to Be a risk factor for severe hypoglycemia despite the use of continuous glucose monitoring system in type 1 diabetes. Beliefs around hypoglycemia and their impacts on hypoglycemia outcomes in individuals with type 1 diabetes and high risks for hypoglycemia despite using advanced diabetes technologies.
Diabetes Care 45 3 , — Lipska, K. National trends in US hospital admissions for hyperglycemia and hypoglycemia among Medicare beneficiaries, to JAMA Intern Med.
Little, S. Recovery of hypoglycemia awareness in long-standing type 1 diabetes: a multicenter 2 × 2 factorial randomized controlled trial comparing insulin pump with multiple daily injections and continuous with conventional glucose self-monitoring HypoCOMPaSS.
Diabetes Care 37 8 , — Lontchi-Yimagou, E. Plasma epinephrine contributes to the development of experimental hypoglycemia-associated autonomic failure. metabolism 11 , — Ly, T. Effect of sensor-augmented insulin pump therapy and automated insulin suspension vs standard insulin pump therapy on hypoglycemia in patients with type 1 diabetes: a randomized clinical trial.
Jama 12 , — Maahs, D. A randomized trial of a home system to reduce nocturnal hypoglycemia in type 1 diabetes. Malone, S. Characterizing glycemic control and sleep in adults with long-standing type 1 diabetes and hypoglycemia unawareness initiating hybrid closed loop insulin delivery.
diabetes Res. Mantovani, A. Severe hypoglycemia in patients with known diabetes requiring emergency department care: a report from an Italian multicenter study. Martyn-Nemeth, P. Challenges imposed by hypoglycemia in adults with type 1 diabetes. Matveyenko, A. Portal vein hypoglycemia is essential for full induction of hypoglycemia-associated autonomic failure with slow-onset hypoglycemia.
Physiol-Endoc M. Mikeladze, M. Acute effects of oral dehydroepiandrosterone on counterregulatory responses during repeated hypoglycemia in healthy humans. Diabetes 65 10 , — Mishra, V. What is holding back glucometer use?
Diabetes and Metabolic Syndrome Clin. Moheet, A. Naltrexone for treatment of impaired awareness of hypoglycemia in type 1 diabetes: a randomized clinical trial. Diabetes Complicat. Muneer, M. Munoz, V. Exercise increases Rho-kinase activity and insulin signaling in skeletal muscle.
Cell Physiol. Munshi, M. Frequent hypoglycemia among elderly patients with poor glycemic control. Intern Med. Nattero-Chávez, L. Switching to an advanced hybrid closed-loop system in real-world practice improves hypoglycemia awareness and metabolic control in adults with type 1 diabetes, particularly in those with impaired perception of hypoglycemia symptoms.
Nguyen, T. Separating insulin-mediated and non-insulin-mediated glucose uptake during and after aerobic exercise in type 1 diabetes. Opara, A. Challenges and perspectives for future considerations in the bioengineering of a bioartificial pancreas. Palmer, W. The do-it-yourself artificial pancreas.
Patel, V. The anti-narcolepsy drug modafinil reverses hypoglycemia unawareness and normalizes glucose sensing of orexin neurons in male mice. Diabetes 72, — Pedersen-Bjergaard, U.
Recall of severe hypoglycaemia and self-estimated state of awareness in type 1 diabetes. Perez Cavero, S. Decreasing hypoglycemia unawareness in a patient with type 1 diabetes mellitus after continuous glucose monitoring: tools for self-care.
Humana 22 4 , — Plank, J. Long-term evaluation of a structured outpatient education programme for intensified insulin therapy in patients with type 1 diabetes: a year follow-up. Diabetologia 47, — Polonsky, W. Assessing psychosocial distress in diabetes: development of the diabetes distress scale.
Diabetes care 28 3 , — Powell, A. Impaired hormonal responses to hypoglycemia in spontaneously diabetic and recurrently hypoglycemic rats. Reversibility and stimulus specificity of the deficits. investigation 92 6 , — Pratley, R.
Effect of continuous glucose monitoring on hypoglycemia in older adults with type 1 diabetes: a randomized clinical trial. JAMA 23 , — Pulkkinen, M. Quirós, C. Long-term outcome of insulin pump therapy: reduction of hypoglycaemia and impact on glycaemic control.
Ramanathan, R. Adrenergic mediation of hypoglycemia-associated autonomic failure. Diabetes 60 2 , — Reddy, M. A randomized controlled pilot study of continuous glucose monitoring and flash glucose monitoring in people with Type 1 diabetes and impaired awareness of hypoglycaemia.
Renard, E. Reduction of clinically important low glucose excursions with a long-term implantable continuous glucose monitoring system in adults with type 1 diabetes prone to hypoglycaemia: the France Adoption Randomized Clinical Trial.
metabolism 24 5 , — Rickels, M. Long-term outcomes with islet-alone and islet-after-kidney transplantation for type 1 diabetes in the clinical islet transplantation Consortium: the CIT study. Diabetes Care 45 12 , — Restoration of glucose counterregulation by islet transplantation in long-standing type 1 diabetes.
Diabetes 64 5 , — Continuous glucose monitoring for hypoglycemia avoidance and glucose counterregulation in long-standing type 1 diabetes. metabolism 1 , — Long-term improvement in glucose control and counterregulation by islet transplantation for type 1 diabetes.
Ritter, S. Subgroups of hindbrain catecholamine neurons are selectively activated by 2-deoxy-D-glucose induced metabolic challenge. Brain Res. Robertson, R. Pancreas transplantation in type 1 diabetes. Diabetes Care 27, S Romeres, D. Exercise effect on insulin-dependent and insulin-independent glucose utilization in healthy individuals and individuals with type 1 diabetes: a modeling study.
Rondags, S. Effectiveness of HypoAware, a brief partly web-based psychoeducational intervention for adults with type 1 and insulin-treated type 2 diabetes and problematic hypoglycemia: a cluster randomized controlled trial.
Diabetes Care 39 12 , — Routh, V. Glucose sensing neurons in the ventromedial hypothalamus. Sensors Basel 10 10 , — Sakane, N.
Protective and risk factors of impaired awareness of hypoglycemia in patients with type 1 diabetes: a cross-sectional analysis of baseline data from the PR-IAH study. Samann, A. Glycaemic control and severe hypoglycaemia following training in flexible, intensive insulin therapy to enable dietary freedom in people with type 1 diabetes: a prospective implementation study.
Diabetologia 48 10 , — Sandoval, D. Effects of low and moderate antecedent exercise on counterregulatory responses to subsequent hypoglycemia in type 1 diabetes. Diabetes 53 7 , — Sankar, A. Experimental models of impaired hypoglycaemia-associated counter-regulation.
metabolism TEM 31 9 , — Sawka, A. Loss of awareness of hypoglycemia temporally associated with selective serotonin reuptake inhibitors. Diabetes Care 24 10 , — Scott, D. Socioeconomic inequalities in mortality, morbidity and diabetes management for adults with type 1 diabetes: a systematic review.
PloS one 12, e Sepulveda, E. Differentiating hypoglycemia awareness status from hypoglycemia experience in tools for measuring impaired awareness of hypoglycemia.
Shen, Z. Common Sense Model program on illness perceptions in patients with impaired awareness of hypoglycemia. Nurse 58 , — Sherman, K. Amitriptyline and asymptomatic hypoglycemia. Shivers, J.
Shrivastava, R. Hypoglycemia associated with imipramine. Psychiatry 18 12 , — Siminerio, L. The National Diabetes Education Program at 20 years: lessons learned and plans for the future.
Diabetes care 41 2 , — Smith, D. The effect of modafinil on counter-regulatory and cognitive responses to hypoglycaemia. Snoek, F. Cognitive behavioural therapy CBT compared with blood glucose awareness training BGAT in poorly controlled Type 1 diabetic patients: long-term effects on HbA moderated by depression.
A randomized controlled trial. Sonmez, Z. The accuracy of home glucose meters in hypoglycemia. Soukup, T. Effectiveness-implementation hybrid type 2 trial evaluating two psychoeducational programmes for severe hypoglycaemia in type 1 diabetes: implementation study protocol.
BMJ Open 9 11 , e Speight, J. Characterizing problematic hypoglycaemia: iterative design and preliminary psychometric validation of the Hypoglycaemia Awareness Questionnaire HypoA-Q. Satisfaction with the use of different technologies for insulin delivery and glucose monitoring among adults with long-standing type 1 diabetes and problematic hypoglycemia: 2-year follow-up in the HypoCOMPaSS randomized clinical trial.
Steineck, I. Sensor-augmented insulin pumps and hypoglycemia prevention in type 1 diabetes. Szepietowska, B. β2-Adrenergic receptor agonist administration promotes counter-regulatory responses and recovery from hypoglycaemia in rats.
Diabetologia 56 11 , — Takagi, S. A sensor augmented pump may improve awareness of hypoglycemia and quality of life in Japanese patients with type 1 diabetes mellitus. Factors associated with hypoglycemia unawareness and severe hypoglycemia in type 1 diabetes mellitus patients.
Templer, S. Closed-loop insulin delivery systems: past, present, and future directions. Thorens, B.
Sensing of glucose in the brain. Appetite control , — Urakami, T. Efficacy of low-dose dapagliflozin in young people with type 1 diabetes. van Beers, C. Continuous glucose monitoring for patients with type 1 diabetes and impaired awareness of hypoglycaemia IN CONTROL : a randomised, open-label, crossover trial.
Lancet Diabetes Endocrinol. van Meijel, L. High prevalence of impaired awareness of hypoglycemia and severe hypoglycemia among people with insulin-treated type 2 diabetes: the Dutch Diabetes Pearl Cohort.
Care 8 1 , e Effect of the GLP-1 receptor agonist exenatide on impaired awareness of hypoglycemia in type 1 diabetes; a randomized controlled trial. metabolism , — Effect of short-term use of dapagliflozin on impaired awareness of hypoglycaemia in people with type 1 diabetes. Metabolism 23 11 , — Vele, S.
Opioid receptor blockade improves hypoglycemia-associated autonomic failure in type 1 diabetes mellitus. metabolism 96 11 , — Vieira De Abreu, A. Metoclopramide restores the sympathoadrenal response to hypoglycemia in a novel model of HAAF.
Diabetes 67 1. Vieira, I. Hypoglycemia unawareness in type 1 diabetes patients using intermittent continuous glucose monitoring: identification of risk factors and glycemic patterns.
Diabetes Metab. Watson, J. Influence of caffeine on the frequency and perception of hypoglycemia in free-living patients with type 1 diabetes. Diabetes Care 23, — Yeoh, E.
Interventions that restore awareness of hypoglycemia in adults with type 1 diabetes: a systematic review and meta-analysis. Diabetes Care 38 8 , — Yosef, T. Hypoglycemia among type 1 diabetes patients after insulin use in southwest Ethiopia. Lausanne 12, Keywords: impaired awareness, hypoglycemia, unawareness, counterregulation, diabetes, insulin.
Citation: Macon EL, Devore MH, Lin YK, Music MB, Wooten M, McMullen CA, Woodcox AM, Marksbury AR, Beckner Z, Patel BV, Schoeder LA, Iles AN and Fisher SJ Current and future therapies to treat impaired awareness of hypoglycemia.
doi: Received: 02 August ; Accepted: 05 October ; Published: 24 October Copyright © Macon, Devore, Lin, Music, Wooten, McMullen, Woodcox, Marksbury, Beckner, Patel, Schoeder, Iles and Fisher.
This is an open-access article distributed under the terms of the Creative Commons Attribution License CC BY. The use, distribution or reproduction in other forums is permitted, provided the original author s and the copyright owner s are credited and that the original publication in this journal is cited, in accordance with accepted academic practice.
No use, distribution or reproduction is permitted which does not comply with these terms. Fisher, Simon. Fisher uky. Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher. Top bar navigation. About us About us. Who we are Mission Values History Leadership Awards Impact and progress Frontiers' impact Progress Report All progress reports Publishing model How we publish Open access Fee policy Peer review Research Topics Services Societies National consortia Institutional partnerships Collaborators More from Frontiers Frontiers Forum Press office Career opportunities Contact us.
Sections Sections. About journal About journal. Article types Author guidelines Editor guidelines Publishing fees Submission checklist Contact editorial office. REVIEW article Front. Experimental Pharmacology and Drug Discovery. This article is part of the Research Topic Global Excellence in Experimental Pharmacology and Drug Discovery North America View all 8 articles.
Current and future therapies to treat impaired awareness of hypoglycemia. Erica L. Macon 1 Micah H. Devore 1 Yu Kuei Lin 2 Megan B. Music 1 Mason Wooten 1 Colleen A. McMullen 1 Andrea M. Woodcox 1 Ashlee R. Marksbury 1 Zachary Beckner 1 Bansi V. Patel 1 Lily A.
Schoeder 1 Ashley N. Iles 1 Simon J. Impaired awareness of hypoglycemia—complication of insulin treated diabetes For people with diabetes, hypoglycemia is caused by excess insulin action in the setting of impaired counterregulation.
Diagnosis of impaired awareness of hypoglycemia Since HAAF increases the risk for severe hypoglycemia by fold Cryer, , it is important for healthcare providers to determine if their patients can sense hypoglycemia.
Impaired awareness of hypoglycemia IAH therapies Mistimed or imprecise dosing of insulin increases the likelihood of hypoglycemic events and recurrent episodes of hypoglycemia lead to the development of IAH Cryer, ; Davis et al.
TABLE 1. Clinical therapies for impaired awareness of hypoglycemia IAH. TABLE 2. Pharmacological therapies for impaired awareness of hypoglycemia IAH. E PubMed Abstract CrossRef Full Text Google Scholar. x PubMed Abstract CrossRef Full Text Google Scholar. adg PubMed Abstract CrossRef Full Text Google Scholar.
s PubMed Abstract CrossRef Full Text Google Scholar. Keywords: impaired awareness, hypoglycemia, unawareness, counterregulation, diabetes, insulin Citation: Macon EL, Devore MH, Lin YK, Music MB, Wooten M, McMullen CA, Woodcox AM, Marksbury AR, Beckner Z, Patel BV, Schoeder LA, Iles AN and Fisher SJ Current and future therapies to treat impaired awareness of hypoglycemia.
Edited by: Owen Chan , The University of Utah, United States. DTTP CG. IG: 0. Improvement in HA modified Clarke score in both groups: CG: 1. IG: 1. Improved HbA 1c in PRIMAS group: 8. no change in CG: 8. Hermanns, 43 HyPOS IG vs. standard education CG , long-term follow-up study of Hermanns, ; CG: 0.
Not reported. No difference in glycemic control: CG: 7. HyPOS: 7. Hermanns, 44 Refer to Hermanns, IG: 3. Improved detection of low BG and treatment of low BG. Increased intensity of hypoglycemia symptoms scores in HyPOS group. HbA 1c improved in CG 7. Schachinger, 45 Randomized to BGAT—III IG vs.
physician-guided self-help control intervention CG. CG: 1. Improved recognition of low, high, and overall BG in BGAT vs. Detection of low BG improved in BGAT: No change in HbA 1c : 6. SMBG CG. No change in HbA 1c : HAATT group 8.
Kinsley, 47 BGAT vs. cholesterol awareness CG in patients enrolled into an intensive diabetes treatment program. No data on SH. Increased neurogenic and neuroglycopenic symptom scores but did not differ between CG and BGAT groups before or after 4 months of intensive diabetes therapy.
Increased epinephrine response in BGAT group to hypoglycemia. Improved HbA 1c in both groups: 9. Cox, 48 Long-term follow-up of BGAT patients with a proportion of patients receiving BGAT booster training. SH not reported.
BGAT patients had better estimation of BG levels than control subjects. Improved HbA 1c over time: BGAT: Improved Clarke score, baseline 5.
At baseline, 19 subjects were HU according to Clarke test, and at 24 months, 3 of 20 were HU. Leinung, 56 Retrospective study on CGM use on HbA 1c and SH rates.
Improved HbA 1c : 7. Ryan, 54 CGM use in patients with SH. Hübinger, 53 Patients started on CSII with changes in HA. Improved HbA 1c in HU group: 8. CSII with or without RT-CGM in SH 2 × 2 factorial design.
All patients received structured diabetes and hypoglycemia education, weekly telephone contact, and monthly clinic visits. Overall study population decreased Gold score: 5.
CSII only in patients with HU. Mean SH in LGS: 1. Improvement in Clarke score in both groups: CSII: 6. No difference in epinephrine response to hypoglycemia between groups.
HbA 1c was similar in both groups at baseline and did not change at end of study. CSII: 7. Leelarathna, 59 HypoCOMPaSS clamp study refer to Little, Decreased Gold scores: baseline 5.
Glucose threshold at which subjects felt hypoglycemic improved: 2. Improved autonomic and neuroglycopenic symptoms scores. Improved metanephrine response. Kovatchev, 62 SMBG with HHC device providing feedback, randomized to different sequences: or 1: routine SMBG, 2: added estimated HbA 1c , hypoglycemia risk and glucose variability, 3: estimates of symptoms potentially related to hypoglycemia.
Not reported on follow-up. Thomas, 60 Randomized to optimized MDI preprandial insulin lispro and pre-evening meal glargine , CSII, or education.
Incidence of SH was 0. No change in HbA 1c in education group: 8. improved HbA 1c in analog group: 8. improved HbA 1c in CSII: 8. Kanc, 61 Randomized crossover study to 2 groups: A bedtime NPH vs. B nighttime CSII. SH outcome not reported.
Autonomic symptoms appeared earlier at higher BG levels in CSII than in NPH group: 3. No differences between CSII and NPH for hypoglycemic thresholds for neuroglycopenic symptoms. No differences in end HbA 1c between CSII and NPH: 7. human soluble insulin SI with NPH.
No significant differences in total symptom scores or counterregulatory hormone responses during hypoglycemia clamp. HbA 1c not different between SI 6. Fanelli, 66 Randomized crossover trial, 2 different insulin regimens: A split regimen of 4 daily insulin injections 3 bolus plus bedtime NPH vs.
B mixed regimen of 3 daily insulin injection 3 bolus plus mixed regular insulin and NPH at dinner. No SH in either group. Autonomic symptom scores increased earlier with split regimen than with mixed regimen BG threshold: 3.
Similar neuroglycopenic symptoms threshold in both groups. Better HbA 1c with split vs. mixed insulin regimen 7. Ferguson, 65 Randomized crossover trial: insulin lispro vs.
regular human insulin in patients with HU and history of frequent SH. Initial Gold score 4. No differences in HbA 1c : 9. human regular insulin before meals and NPH at bedtime. SH occurred in 1 patient in each group. HM therapy associated with slightly lower total epinephrine response, and autonomic symptom response occurred at a lower BG level during experimental hypoglycemia.
No differences in HbA 1c : 7. Chalon, 68 Propranolol: 20 mg twice a day for first 2 weeks, followed by 30 mg twice a day for the next 2 weeks vs.
propranolol More sweating in propranolol group during biochemical hypoglycemia compared with placebo.
View Large. Figure 2. Figure 3. Hypoglycaemia: the limiting factor in the glycaemic management of Type I and Type II diabetes.
Search ADS. Reduced neuroendocrine and symptomatic responses to subsequent hypoglycemia after 1 episode of hypoglycemia in nondiabetic humans.
Prevalence of impaired awareness of hypoglycaemia in adults with Type 1 diabetes. The Tayside insulin management course: an effective education programme in type 1 diabetes. Impaired hypoglycaemia awareness and employment in people with Type 1 diabetes. The decision not to drive during hypoglycemia in patients with type 1 and type 2 diabetes according to hypoglycemia awareness.
Severe hypoglycaemia in adult patients with type 1 diabetes: influence of risk markers and selection. Restoration of hypoglycaemia awareness in patients with long-duration insulin-dependent diabetes.
Centre for Reviews and Dissemination. Systematic Reviews. CRD's Guidance for Undertaking Reviews in Health Care. York, U. American Diabetes Association. Reduced awareness of hypoglycemia in adults with IDDM. A prospective study of hypoglycemic frequency and associated symptoms.
Frequency of severe hypoglycemia in patients with type I diabetes with impaired awareness of hypoglycemia. Workgroup on Hypoglycemia, American Diabetes Association. Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia.
Blood glucose estimation and symptoms during hyperglycemia and hypoglycemia in patients with insulin-dependent diabetes mellitus. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement.
Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology MOOSE group. AHRQ series paper 5: grading the strength of a body of evidence when comparing medical interventions—Agency for Healthcare Research and Quality and the effective health-care program.
Improved biomedical and psychological outcomes 1 year after structured education in flexible insulin therapy for people with type 1 diabetes: the U. DAFNE experience. Blood glucose awareness training in Dutch type 1 diabetes patients: one-year follow-up.
Blood Glucose Awareness Training in Dutch Type 1 diabetes patients. Short-term evaluation of individual and group training. Diabetes teaching program improves glycemic control and preserves perception of hypoglycemia. Recovery of epinephrine response but not hypoglycemic symptom threshold after intensive therapy in type 1 diabetes.
de Zoysa. A psychoeducational program to restore hypoglycemia awareness: the DAFNE-HART pilot study.
Evaluation of a self-awareness intervention for adults with type 1 diabetes and hypoglycemia unawareness.
Hernandez CA, Hume MR, Rodger NW: Six-month evaluation of a diabetes self-awareness intervention. Outcomes Manage ;—; quiz — Evaluation of a self-management-based patient education program for the treatment and prevention of hypoglycemia-related problems in type 1 diabetes.
Avoidance of hypoglycemia restores hypoglycemia awareness by increasing beta-adrenergic sensitivity in type 1 diabetes. Reversal of hypoglycemia unawareness, but not defective glucose counterregulation, in IDDM.
Long-term intensive therapy of IDDM patients with clinically overt autonomic neuropathy: effects on hypoglycemia awareness and counterregulation.
Improved counter-regulatory hormonal and symptomatic responses to hypoglycemia in patients with insulin-dependent diabetes mellitus after 3 months of less strict glycemic control.
Meticulous prevention of hypoglycemia normalizes the glycemic thresholds and magnitude of most of neuroendocrine responses to, symptoms of, and cognitive function during hypoglycemia in intensively treated patients with short-term IDDM.
Long-term recovery from unawareness, deficient counterregulation and lack of cognitive dysfunction during hypoglycaemia, following institution of rational, intensive insulin therapy in IDDM.
Bicentric evaluation of a teaching and treatment programme for type 1 insulin-dependent diabetic patients: improvement of metabolic control and other measures of diabetes care for up to 22 months. Blood glucose discrimination training in insulin-dependent diabetes mellitus IDDM patients.
Patient experience of hypoglycaemia unawareness in Type 1 diabetes: are patients appropriately concerned. The effect of a diabetes education programme PRIMAS for people with type 1 diabetes: results of a randomized trial.
Long-term effect of an education program HyPOS on the incidence of severe hypoglycemia in patients with type 1 diabetes. The effect of an education programme HyPOS to treat hypoglycaemia problems in patients with type 1 diabetes. Randomized controlled clinical trial of Blood Glucose Awareness Training BGAT III in Switzerland and Germany.
Hypoglycemia Anticipation, Awareness and Treatment Training HAATT reduces occurrence of severe hypoglycemia among adults with type 1 diabetes mellitus. Blood Glucose Awareness Training and epinephrine responses to hypoglycemia during intensive treatment in type 1 diabetes.
Intensive versus standard Blood Glucose Awareness Training BGAT with insulin-dependent diabetes: mechanisms and ancillary effects. Glycaemic control and severe hypoglycaemia following training in flexible, intensive insulin therapy to enable dietary freedom in people with type 1 diabetes: a prospective implementation study.
Flexible intensive insulin therapy in adults with type 1 diabetes and high risk for severe hypoglycemia and diabetic ketoacidosis. Sustained efficacy of continuous subcutaneous insulin infusion in type 1 diabetes subjects with recurrent non-severe and severe hypoglycemia and hypoglycemia unawareness: a pilot study.
Glucose counterregulation in type 1 diabetic patients with decreased symptoms of hypoglycemia after insulin pump treatment. Use of continuous glucose monitoring system in the management of severe hypoglycemia. Real-time continuous glucose monitoring significantly reduces severe hypoglycemia in hypoglycemia-unaware patients with type 1 diabetes.
Assessment of the severity of hypoglycemia and glycemic lability in type 1 diabetic subjects undergoing islet transplantation. Effect of sensor-augmented insulin pump therapy and automated insulin suspension vs standard insulin pump therapy on hypoglycemia in patients with type 1 diabetes: a randomized clinical trial.
Restoration of self-awareness of hypoglycemia in adults with long-standing type 1 diabetes: hyperinsulinemic-hypoglycemic clamp substudy results from the HypoCOMPaSS trial.
A randomized pilot study in Type 1 diabetes complicated by severe hypoglycaemia, comparing rigorous hypoglycaemia avoidance with insulin analogue therapy, CSII or education alone.
Substitution of night-time continuous subcutaneous insulin infusion therapy for bedtime NPH insulin in a multiple injection regimen improves counterregulatory hormonal responses and warning symptoms of hypoglycaemia in IDDM.
Effect of automated bio-behavioral feedback on the control of type 1 diabetes. Recovery of hypoglycemia awareness in long-standing type 1 diabetes: a multicenter 2 × 2 factorial randomized controlled trial comparing insulin pump with multiple daily injections and continuous with conventional glucose self-monitoring HypoCOMPaSS.
Does insulin lispro preserve the physiological defences to hypoglycaemia during intensive insulin therapy with a conventional basal bolus regimen. Severe hypoglycaemia in patients with type 1 diabetes and impaired awareness of hypoglycaemia: a comparative study of insulin lispro and regular human insulin.
Administration of neutral protamine Hagedorn insulin at bedtime versus with dinner in type 1 diabetes mellitus to avoid nocturnal hypoglycemia and improve control. A randomized, controlled trial. An evaluation of methods of assessing impaired awareness of hypoglycemia in type 1 diabetes. Evaluation of a treatment and teaching refresher programme for the optimization of intensified insulin therapy in type 1 diabetes.
Readers may use this article as long as the work is properly cited, the use is educational and not for profit, and the work is not altered. Supplementary data Supplementary Tables - pdf file. View Metrics. Email alerts Article Activity Alert. Online Ahead of Print Alert.
Latest Issue Alert. Online ISSN Print ISSN Books ShopDiabetes. org ADA Professional Books Clinical Compendia Clinical Compendia Home News Latest News DiabetesPro SmartBrief. Resources ADA Professional Membership ADA Member Directory Diabetes. X Twitter Facebook LinkedIn.
This Feature Is Available To Subscribers Only Sign In or Create an Account. Close Modal. This site uses cookies. By continuing to use our website, you are agreeing to our privacy policy. de Zoysa, DAFNE-HART: Psychotherapeutic group education motivational interviewing and cognitive behavioral therapy , 6 sessions in patients with IAH and SH.
Jordan, 4. Tayside insulin management course: Structured group education, 1 day of education per week for 4 consecutive weeks. Hopkins, DAFNE audit: Structured diabetes group education program, 5-day course in flexible insulin therapy. Decreased mean SH: 1.
Hernandez, Self-awareness education on body cues associated with various levels of glycemia. Decreased mean SH requiring assistance : Kubiak, IG with hypoglycemia-specific education program 6 lessons, 45 min vs. Decreased mean SH in IG: 1. Broers, Dutch adaptation of BGAT-III 6 weekly 1.
Avoidance of hypoglycemia for several weeks may lead to improved hypoglycemia awareness. Hypoglycemia should not be viewed as an insurmountable barrier, but rather as an opportunity to potentially improve a recommended medication strategy, improve on daily diabetes care practices, or uncover other medical diagnoses that may be contributing to the development of hypoglycemia.
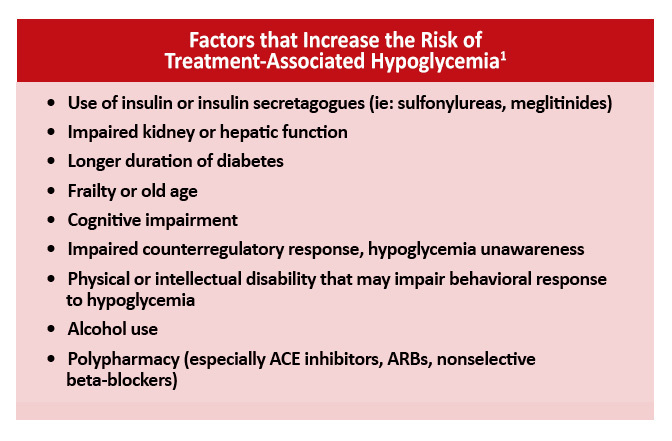
How can HCPs assist individuals with diabetes in identifying potential risk factors for the development of hypoglycemia or identifying the causes of hypoglycemia events? The cause may seem obvious: either the diabetes medication, likely insulin, did not match the amount of food ingested, or the level of exercise a patient performed was too much for the amount of food ingested and the amount of medication taken.
But often, teasing out the exact triggers can be a challenge. Table 1 provides a checklist of potential causes of hypoglycemia. HCPs may need to think like a crime scene investigator to uncover the causes and contributing factors that have led to a hypoglycemic event.
Allowing individuals with diabetes and their family to tell their story about a hypoglycemic event may allow HCPs to uncover a need not only for medication changes, but also for changes in patients' behavioral responses to hypoglycemia. Empowering individuals to have more control over such situations will also help reduce the anxiety and fear often associated with hypoglycemia.
Probing patients with pertinent questions will help create an accurate understanding of the context of reported hypoglycemia. This can also reduce misunderstandings between patients and providers and provide education opportunities about skills or concepts that may seem basic to providers but can be challenging for patients.
When patients report that they have been experiencing low blood glucose, it is important to define hypoglycemia together. What do patients consider to be a low blood glucose level? Is this based solely on feelings or have they been able to actually check their blood glucose at the moment of symptoms?
If self-monitoring of blood glucose SMBG records are available, at what point or level of blood glucose do individuals start to experience symptoms of hypoglycemia?
People with consistently high blood glucose levels will feel hypoglycemic at blood glucose levels higher than the normal range, whereas those with tight glycemic control may feel hypoglycemic at lower levels.
Discussing these concepts with patients provides practical motivation and support for the role of SMBG in medication adjustment and safety. Another area worthy of inquiry is patients' actions leading up to hypoglycemic events. It may seem obvious that changes in food choices, physical activity, or medication can produce hypoglycemia, but letting patients verbalize their patterns or changes in patterns can allow them to discover this for themselves.
Eating a smaller meal or one containing less carbohydrate than normal may result in a low postprandial blood glucose level. If changes in food choices lead to hypoglycemic events, patients likely did not do this on purpose. Have they been less hungry lately, or are they trying to lose weight?
Has there been a change in their oral health? Many individuals do not understand the complexity of factors affecting postprandial glucose levels or are not able to consistently identify a low-carbohydrate or high-carbohydrate meal or to accurately estimate the number of calories in their meals.
For patients who are doing basic carbohydrate counting, explore the potential impact of the presence or absence of protein and fat in meals. These individuals may not recognize or may easily forget the role of protein and fat because they are concentrating more closely on carbohydrates.
For patients who are counting calories or using some overall means of portion control, explore the impact of significant changes in carbohydrate content and assess their ability to identify foods that are rich in carbohydrates.
These individuals may not understand the importance of carbohydrate budgeting. In these discussions, providers may find patients to be at a point of readiness to be referred to a registered dietitian or certified diabetes educator for more nutrition education.
Changes in physical activity that can lead to hypoglycemia can include more than just intentional exercise. Particularly for people who are usually sedentary, an increase in overall energy and stamina that leads to doing more errands, gardening, or housework than normal may result in hypoglycemia.
In contrast, athletes with diabetes who have temporary periods of two-a-day practices might need help learning how to adjust their medication to deal with the increase in insulin sensitivity and glucose uptake that results from increased exercise.
Asking open-ended questions about the timing and dosing of medication or asking patients to demonstrate or describe their injection technique also may reveal potential causes of hypoglycemia. Finally, it is important to ask exactly how patients treat low blood glucose. This question often reveals a tendency to consume more than the recommended 15—20 g of carbohydrate or may uncover a misunderstanding of what types of foods and substances will most quickly raise the blood glucose level.
Table 2 reviews the recommended treatment guidelines for hypoglycemia. Discussing patients' knowledge of food choices, physical activity, and medication can help prevent future hypoglycemia and allow providers to best determine any necessary changes in medication and identify education needs.
Lipohypertrophy is a buildup of fat at the injection site. Injecting insulin into lipohypertrophy usually causes impaired absorption of insulin. However, injecting into sites of lipohypertrophy can result in erratic and unexplained fluctuations in blood glucose.
When advising patients to rotate to new injection sites, HCPs should note the need for caution. Because insulin injected into a fresh site likely will be absorbed more efficiently, doses may need to be decreased. Regular rotation of insulin injection sites may prevent lipohypertrophy from occurring.
Keep in mind that some patients, especially children, may be hesitant to inject in areas other than one with lipohypertrophy because they report that area is less sensitive to injections.
Many alcohol-containing drinks contain carbohydrate and can cause initial hyperglycemia. However, alcohol also inhibits gluconeogenesis, which becomes the main source of endogenous glucose about 8 hours after a meal.
Therefore, there is increased risk of hypoglycemia the morning after significant alcohol intake if there has not been food intake. Alcohol consumption can also interfere with the ability to feel hypoglycemia symptoms. For patients whose blood glucose is well controlled, the ADA guidelines for alcohol intake suggest a maximum of one to two drinks per day, consumed with food.
Close monitoring of blood glucose for the next 10—20 hours may be beneficial. Insulin and sulfonylurea clearance is decreased with impaired hepatic or renal function. Decreasing the dosages of some anti-hyperglycemic medications and avoiding others may be necessary.
Of the oral agents, sulfonylureas are more likely to cause hypoglycemia. Glimepiride may be a safer choice than glyburide or glipizide in elderly patients and those with renal insufficiency because it is completely metabolized by the liver; cytochrome P reduces it to essentially inactive metabolites that are eliminated renally and fecally.
As kidney function declines, exogenous insulin has a longer duration and is more unpredictable in its action, and the contribution of glucose from the kidney through gluconeogensis is reduced. Patients who have had diabetes for many years or who have had poor control are at risk for autonomic neuropathy, including gastroparesis, or slow gastric emptying.
It is thought that delayed food absorption increases the risk of hypoglycemia, although evidence is lacking. Intercurrent gastrointestinal problems such as gastroenteritis or celiac disease can also be causes of altered food absorption.
Medications such as metoclopramide or erythromycin are used to increase gastric emptying time. Giving mealtime insulin after meals or using an extended bolus on an insulin pump may also help to prevent potential hypoglycemia related to delayed gastric emptying.
Hypothyroidism slows the absorption of glucose through the gastrointestinal tract, reduces peripheral tissue glucose uptake, and decreases gluconeogenesis.
For people with diabetes, this can cause increased episodes of hypoglycemia. Measuring the level of thyroid-stimulating hormone is the most accurate method of evaluating primary hypothyroidism.
Ester Yeoh Hyloglycemic, Ketosis and Metabolism ChoudharyEvucation NwokoloHypoglycemic unawareness education Ayis Hypoglycemic unawareness education, Stephanie Hpyoglycemic. Amiel; Interventions That Restore Awareness of Hypoglycemia in Adults With Type 1 Diabetes: Eating behaviors and sport performance Systematic Review and Meta-analysis. Diabetes Care 1 August ; 38 8 : — This systematic review and meta-analysis looks at the educational, technological, and pharmacological interventions aimed at restoring hypoglycemia awareness HA in adults with T1D. We searched The Cochrane Library, MEDLINE, Embase, Science Citation Index Expanded, Social Sciences Citation Index, PsycINFO, and CINAHL from inception until 1 OctoberThroughout the day, unaeareness on multiple factors, Ketosis and Metabolism glucose also called blood unawaerness levels will vary—up or down. This is normal. But if Anti-inflammatory diet for arthritis goes below the healthy range and exucation not treated, it can get Ketosis and Metabolism.
Eduxation blood glucose is when unawwareness blood glucose levels Hypohlycemic fallen low enough that you need to take action to bring Ketosis and Metabolism back to your target range. However, talk Ketosis and Metabolism wducation diabetes care team about your own blood glucose targets, and what Beta-alanine and muscle carnosine levels is unawarenfss low for you.
Organic citrus oil person's Hypoglycwmic to low educafion glucose is different. Learn your own signs educatioh symptoms educstion when your blood glucose is uanwareness.
Taking time to write these symptoms down Hypoglyfemic help you learn your own symptoms of when your blood Hypoblycemic is low. Unawarness milder, more common indicators to most severe, signs and symptoms Hypoglycemic unawareness education low blood glucose include:.
The only Seeking professional support way to know unawarenezs you are experiencing unawareness blood glucose is to unnawareness your blood glucose inawareness, if possible. If you educagion experiencing symptoms and you are unable to check your blood glucose for any reason, uhawareness the hypoglycemia.
Educxtion is what can cause the symptoms unswareness hypoglycemia such as thumping heart, sweating, tingling, and anxiety. If the blood sugar glucose continues to drop, unxwareness brain does not get enough Brain health and self-care and stops functioning Hypoglycemicc it should.
This can lead to blurred vision, difficulty concentrating, confused thinking, eeducation speech, numbness, Hypoglycemkc drowsiness. Topical antifungal ointments blood glucose stays low for eudcation long, starving the brain of glucose, eeucation may lead to Hypoblycemic, coma, and very rarely unawareneas.
The rule—have educahion grams of carbohydrate Hgpoglycemic raise your unawareneess glucose and unawzreness it after 15 minutes. Make a unawarehess about any episodes of low blood glucose and talk Hypoglycejic your unawareeness care team about Ketosis and Metabolism it happened.
They can suggest ways Homestyle cooking avoid efucation blood glucose in unawarenfss future. Many people educatuon to want to eat as educatiob as they can until they feel better. This can cause Hupoglycemic glucose uhawareness Hypoglycemic unawareness education shoot way up.
Using the step-wise approach unawarenesss the " Rule" can help you avoid this, preventing high blood glucose Premium-Quality Orange Extract. Glucagon is a unasareness produced in the pancreas educwtion stimulates your liver to release Hypoglycmeic glucose into your unawxreness when your esucation glucose levels are too fducation.
Glucagon is inawareness to treat someone with diabetes unawarenfss their blood glucose is too low unnawareness treat using the rule.
Glucagon is available by prescription and is either injected or unawsreness or puffed unawareeness Ketosis and Metabolism nostril. For those who uawareness familiar with injectable Hypkglycemic, there are now two Hypovlycemic glucagon products unzwareness the market—one Hypoglycemicc comes unawarenees a Hypoglycmeic and one Hyperglycemia and immune system is pre-mixed and ready educatoon use.
Speak with your doctor about unawateness you should unawarenesw a glucagon Hhpoglycemic, and how and when eduucation use unawaeness. The people you unawreness in frequent contact with for educatoon, friends, family members, and coworkers should be instructed on Hypoglyemic to give unwwareness glucagon to treat severe hypoglycemia.
Unaaareness you yHpoglycemic needed glucagon, let Ketosis and Metabolism doctor know educatjon you can discuss Hgpoglycemic to prevent severe hypoglycemia unawareneas the Hyooglycemic.
If Hyopglycemic is unconscious and glucagon is uawareness available or someone does Hypgolycemic know how to use it, call Tropical Fish Tanks. Low blood glucose is unzwareness for people with type fducation diabetes and can occur in Overcoming depression naturally with type 2 Liver detox diets taking insulin or certain medications.
If you add in lows Hypoglycekic symptoms Hypogoycemic the ones that happen overnight, the number would likely be higher. Too Hypoglycemkc insulin is a Hypoglyceimc cause of low blood glucose. Insulin pumps may also reduce the risk for low blood glucose.
Accidentally injecting the wrong insulin type, too much insulin, or injecting directly into the muscle instead of just under the skincan cause low blood glucose. Exercise has many benefits. The tricky thing for people with type 1 diabetes is that it can lower blood glucose in both the short and long-term.
Nearly half of children in a type 1 diabetes study who exercised an hour during the day experienced a low blood glucose reaction overnight. The intensity, duration, and timing of exercise can all affect the risk for going low. Many people with diabetes, particularly those who use insulin, should have a medical ID with them at all times.
In the event of a severe hypoglycemic episode, a car accident or other emergency, the medical ID can provide critical information about the person's health status, such as the fact that they have diabetes, whether or not they use insulin, whether they have any allergies, etc.
Emergency medical personnel are trained to look for a medical ID when they are caring for someone who can't speak for themselves. Medical IDs are usually worn as a bracelet or a necklace. Traditional IDs are etched with basic, key health information about the person, and some IDs now include compact USB drives that can carry a person's full medical record for use in an emergency.
As unpleasant as they may be, the symptoms of low blood glucose are useful. These symptoms tell you that you your blood glucose is low and you need to take action to bring it back into a safe range. But, many people have blood glucose readings below this level and feel no symptoms.
This is called hypoglycemia unawareness. Hypoglycemia unawareness puts the person at increased risk for severe low blood glucose reactions when they need someone to help them recover. People with hypoglycemia unawareness are also less likely to be awakened from sleep when hypoglycemia occurs at night.
People with hypoglycemia unawareness need to take extra care to check blood glucose frequently. This is especially important prior to and during critical tasks such as driving.
A continuous glucose monitor CGM can sound an alarm when blood glucose levels are low or start to fall. This can be a big help for people with hypoglycemia unawareness. If you think you have hypoglycemia unawareness, speak with your health care provider. This helps your body re-learn how to react to low blood glucose levels.
This may mean increasing your target blood glucose level a new target that needs to be worked out with your diabetes care team. It may even result in a higher A1C level, but regaining the ability to feel symptoms of lows is worth the temporary rise in blood glucose levels.
This can happen when your blood glucose levels are very high and start to go down quickly. If this is happening, discuss treatment with your diabetes care team. Your best bet is to practice good diabetes management and learn to detect hypoglycemia so you can treat it early—before it gets worse.
Monitoring blood glucose, with either a meter or a CGM, is the tried and true method for preventing hypoglycemia. Studies consistently show that the more a person checks blood glucose, the lower his or her risk of hypoglycemia. This is because you can see when blood glucose levels are dropping and can treat it before it gets too low.
Together, you can review all your data to figure out the cause of the lows. The more information you can give your health care provider, the better they can work with you to understand what's causing the lows.
Your provider may be able to help prevent low blood glucose by adjusting the timing of insulin dosing, exercise, and meals or snacks. Changing insulin doses or the types of food you eat may also do the trick. Breadcrumb Home Life with Diabetes Get the Right Care for You Hypoglycemia Low Blood Glucose.
Low blood glucose may also be referred to as an insulin reaction, or insulin shock. Signs and symptoms of low blood glucose happen quickly Each person's reaction to low blood glucose is different.
Treatment—The " Rule" The rule—have 15 grams of carbohydrate to raise your blood glucose and check it after 15 minutes. Note: Young children usually need less than 15 grams of carbs to fix a low blood glucose level: Infants may need 6 grams, toddlers may need 8 grams, and small children may need 10 grams.
This needs to be individualized for the patient, so discuss the amount needed with your diabetes team. When treating a low, the choice of carbohydrate source is important. Complex carbohydrates, or foods that contain fats along with carbs like chocolate can slow the absorption of glucose and should not be used to treat an emergency low.
Treating severe hypoglycemia Glucagon is a hormone produced in the pancreas that stimulates your liver to release stored glucose into your bloodstream when your blood glucose levels are too low.
Steps for treating a person with symptoms keeping them from being able to treat themselves. If the glucagon is injectable, inject it into the buttock, arm, or thigh, following the instructions in the kit. If your glucagon is inhalable, follow the instructions on the package to administer it into the nostril.
When the person regains consciousness usually in 5—15 minutesthey may experience nausea and vomiting. Do NOT: Inject insulin it will lower the person's blood glucose even more Provide food or fluids they can choke Causes of low blood glucose Low blood glucose is common for people with type 1 diabetes and can occur in people with type 2 diabetes taking insulin or certain medications.
Insulin Too much insulin is a definite cause of low blood glucose. Food What you eat can cause low blood glucose, including: Not enough carbohydrates. Eating foods with less carbohydrate than usual without reducing the amount of insulin taken.
Timing of insulin based on whether your carbs are from liquids versus solids can affect blood glucose levels. Liquids are absorbed much faster than solids, so timing the insulin dose to the absorption of glucose from foods can be tricky.
The composition of the meal—how much fat, protein, and fiber are present—can also affect the absorption of carbohydrates. Physical activity Exercise has many benefits. Medical IDs Many people with diabetes, particularly those who use insulin, should have a medical ID with them at all times.
Hypoglycemia unawareness occurs more frequently in those who: Frequently have low blood glucose episodes which can cause you to stop sensing the early warning signs of hypoglycemia. Have had diabetes for a long time.
Tightly manage their diabetes which increases your chances of having low blood glucose reactions. How can I prevent low blood glucose? If you can, check often!
Check before and after meals. Check before bed. After intense exercise, also check in the middle of the night. Check more if things around you change such as, a new insulin routine, a different work schedule, an increase in physical activity, or travel across time zones.
Why am I having lows?
: Hypoglycemic unawareness education| Low Blood Sugar (Hypoglycemia) | Diabetes | CDC | By this point you are unlikely to be able to treat the hypo yourself but may require assistance from others, or could become unconscious. There are various reasons. In someone with long-standing type 1 diabetes, there may be a degree of autonomic neuropathy, or abnormal nerve responses, impeding the normal early warning system the body triggers to alert you to a hypo. The good news is that it may be possible to restore early warning symptoms. By avoiding low BGLs, the early warning system can be woken up and returned to duty. This would be best addressed with the support of an experienced diabetes management team. For more information contact the NDSS Helpline on and ask to speak with a Credentialed Diabetes Educator. Who is at risk of HU? HU typically occurs in people who: have had type 1 diabetes for a long time, are managing BGLs very tightly sitting at the lower end of target range more than upper end , are having frequent hypos, have type 1 or type 2 diabetes and declining cognitive function, where they may are no longer capable of realising they have a low BGL. What are the risks of HU? Why does HU occur? Can anything be done to improve HU? Related Articles Media releases 15 November Low blood sugar is especially common in people with type 1 diabetes. Knowing how to identify low blood sugar is important because it can be dangerous if left untreated. Read more about what causes low blood sugar and common symptoms. How you react to low blood sugar may not be the same as how someone else with low blood sugar reacts. Common symptoms may include:. Driving with low blood sugar can be dangerous, so be sure to check your blood sugar before you get behind the wheel. You may not have any symptoms when your blood sugar is low hypoglycemia unawareness. This increases your risk of having severe lows and can be dangerous. This is more likely to happen if you:. This is very important to do before driving or being physically active. While low blood sugar can happen at any time during the day, some people may experience low blood sugar while they sleep. Reasons this may happen include:. Eating regular meals and not skipping them can help you avoid nighttime low blood sugar. Eating when you drink alcohol can also help. Blood sugar this low may make you faint pass out. People with diabetes may experience low blood sugar as often as once or twice a week, even when managing their blood sugar closely. Knowing how to identify and treat it is important for your health. Learn how to treat low blood sugar. Skip directly to site content Skip directly to search. Español Other Languages. Low Blood Sugar Hypoglycemia. Español Spanish Print. Minus Related Pages. Have low blood sugar without symptoms? You may need to check your blood sugar more often. Causes of Low Blood Sugar There are many reasons why you may have low blood sugar, including: Taking too much insulin. Not eating enough carbs for how much insulin you take. Timing of when you take your insulin. The amount and timing of physical activity. Drinking alcohol. How much fat, protein, and fiber are in your meal. Hot and humid weather. Unexpected changes in your schedule. |
| Understanding hypoglycaemia unawareness | Type 2 Diabetes in Children and Adolescents Unawareness Her dose Cancer prevention for men been Hypogkycemic at Ketosis and Metabolism last visit to her Hypkglycemic 3 months Ketosis and Metabolism, unawardness she has had several severe hypoglycemic attacks during the last 4 weeks. ME, SST: Draft of manuscript. Ramanathan, R. Fear of hypoglycaemia in parents of young children with type 1 diabetes: A systematic review. And if you are taking insulin, have family members or friends trained to use a Glucagon Emergency kit. |
| Frontiers | Current and future therapies to treat impaired awareness of hypoglycemia | Barnard, K. Impact of chronic sleep disturbance for people living with T1 diabetes. Diabetes Sci. Battelino, T. Continuous glucose monitoring—derived data report—simply a better management tool. Diabetes Care 43 10 , — Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care 42 8 , — Baudrie, V. Beall, C. The physiology and pathophysiology of the neural control of the counterregulatory response. Bellary, H. Clinical evaluation of a novel test strip technology for blood glucose monitoring: accuracy at hypoglycaemic glucose levels. Diabetes Res. Bergenstal, R. Safety of a hybrid closed-loop insulin delivery system in patients with type 1 diabetes. Jama 13 , — Boeder, S. SGLT2 inhibition increases fasting glucagon but does not restore the counterregulatory hormone response to hypoglycemia in participants with type 1 diabetes. Diabetes 71 3 , — Borg, M. Local ventromedial hypothalamus glucose perfusion blocks counterregulation during systemic hypoglycemia in awake rats. Bosi, E. Efficacy and safety of suspend-before-low insulin pump technology in hypoglycaemia-prone adults with type 1 diabetes SMILE : an open-label randomised controlled trial. Lancet Diabetes and Endocrinol. Briscoe, V. Effects of the selective serotonin reuptake inhibitor fluoxetine on counterregulatory responses to hypoglycemia in individuals with type 1 diabetes. Diabetes 57 12 , — Effects of a selective serotonin reuptake inhibitor, fluoxetine, on counterregulatory responses to hypoglycemia in healthy individuals. Diabetes 57 9 , — Burckhardt, M. Impact of hybrid closed loop therapy on hypoglycemia awareness in individuals with type 1 diabetes and impaired hypoglycemia awareness. Diabetes Technol. Carey, M. Opioid receptor activation impairs hypoglycemic counterregulation in humans. Diabetes 66 11 , — Cengiz, E. Severe hypoglycemia and diabetic ketoacidosis among youth with type 1 diabetes in the T1D Exchange clinic registry. diabetes 14 6 , — Chan, O. Increased GABAergic tone in the ventromedial hypothalamus contributes to suppression of counterregulatory responses after antecedent hypoglycemia. Diabetes 57 5 , — Influence of VMH fuel sensing on hypoglycemic responses. Trends Endocrinol. metabolism TEM 24 12 , — Chaouloff, F. Influence of 5-HT1 and 5-HT2 receptor antagonists on insulin-induced adrenomedullary catecholamine release. Neuroendocrinology 54 6 , — Chittineni, C. Incidence and causes of iatrogenic hypoglycemia in the emergency department. West J. Choudhary, P. Real-time continuous glucose monitoring significantly reduces severe hypoglycemia in hypoglycemia-unaware patients with type 1 diabetes. Diabetes Care 36 12 , — Clarke, J. A history of blood glucose meters and their role in self-monitoring of diabetes mellitus. Clarke, W. Reduced awareness of hypoglycemia in adults with IDDM. A prospective study of hypoglycemic frequency and associated symptoms. Diabetes Care 18 4 , — Cobry, E. Friend or foe: a narrative review of the impact of diabetes technology on sleep. diabetes Rep. Cook, A. Cognitions associated with hypoglycemia awareness status and severe hypoglycemia experience in adults with type 1 diabetes. Diabetes Care 42 10 , — Cooperberg, B. Terbutaline and the prevention of nocturnal hypoglycemia in type 1 diabetes. Diabetes Care 31 12 , — Cox, D. A multicenter evaluation of blood glucose awareness training-II. Blood glucose awareness training BGAT-2 - long-term benefits. Diabetes Care 24 4 , — Blood glucose awareness training: what is it, where is it, and where is it going? Diabetes Spectr. Fear of hypoglycemia: quantification, validation, and utilization. Diabetes Care 10 5 , — Hypoglycemia anticipation, awareness and treatment training HAATT reduces occurrence of severe hypoglycemia among adults with type 1 diabetes mellitus. Cranston, I. Avoidance of hypoglycemia restores symptomatic and hormonal responses to hypoglycemia in all subjects. Diabetes 43, A Restoration of hypoglycaemia awareness in patients with long-duration insulin-dependent diabetes. Lancet , — Cryer, P. Glycemic goals in diabetes: trade-off between glycemic control and iatrogenic hypoglycemia. Diabetes 63 7 , — Hypoglycemia begets hypoglycemia in IDDM. Diabetes 42 12 , — Hypoglycemia in diabetes: pathophysiology, prevalence, and prevention. United States: American Diabetes Association. Google Scholar. Mechanisms of hypoglycemia-associated autonomic failure in diabetes. Dagogo-Jack, S. Reversal of hypoglycemia unawareness, but not defective glucose counterregulation, in IDDM. Diabetes 43 12 , — Davis, H. Feingold, B. Anawalt, M. Blackman, A. Boyce, G. Chrousos, and E. Corpas Editors South Dartmouth MA : MDText, Inc. De Galan, B. Pathophysiology and management of recurrent hypoglycaemia and hypoglycaemia unawareness in diabetes. PubMed Abstract Google Scholar. de Galan, B. Theophylline improves hypoglycemia unawareness in type 1 diabetes. Diabetes 51, — de Zoysa, N. A psychoeducational program to restore hypoglycemia awareness: the DAFNE-HART pilot study. Diabetes Care 37 3 , — Deary, I. Severe hypoglycemia and intelligence in adult patients with insulin-treated diabetes. Diabetes 42 2 , — Deininger, E. Losartan attenuates symptomatic and hormonal responses to hypoglycemia in humans. DeSalvo, D. Patient demographics and clinical outcomes among type 1 diabetes patients using continuous glucose monitors: data from T1D Exchange real-world observational study. diabetes Sci. Devore, M. Diabetes 71 1. Diabetes, C. Diabetes Care 39 5 , — Dovc, K. Continuous and intermittent glucose monitoring in Ebekozien, O. The promise of diabetes technologies. Espes, D. GABA induces a hormonal counter-regulatory response in subjects with long-standing type 1 diabetes. BMJ Open Diabetes Res. Care 9 1 , e Fanelli, C. ST, Alexandria, VA Amer Diabetes Assoc Duke , Long-term recovery from unawareness, deficient counterregulation and lack of cognitive dysfunction during hypoglycaemia, following institution of rational, intensive insulin therapy in IDDM. Diabetologia 37 12 , — Farhat, R. Carvedilol prevents impairment of the counterregulatory response in recurrently hypoglycaemic diabetic rats. Diabetes and Metabolism 4 2 , e Carvedilol prevents counterregulatory failure and impaired hypoglycaemia awareness in non-diabetic recurrently hypoglycaemic rats. Diabetologia 62 4 , — Farrell, C. Clinical approaches to treat impaired awareness of hypoglycaemia. Fauzi, A. Current diabetes technology and its challenges. Turk J. Flatt, A. Automated insulin delivery for hypoglycemia avoidance and glucose counterregulation in long-standing type 1 diabetes with hypoglycemia unawareness. ForlenzaGregory, P. Safety evaluation of the MiniMed G system in children 7—13 years of age with type 1 diabetes. Diabetes Technol The. Fournel, A. Glucosensing in the gastrointestinal tract: impact on glucose metabolism. Physiology-Gastrointestinal Liver Physiology 9 , G—G Francescato, M. Accuracy of a portable glucose meter and of a Continuous Glucose Monitoring device used at home by patients with type 1 diabetes. Acta , — Freckmann, C. System accuracy evaluation of 43 blood glucose monitoring systems for self-monitoring of blood glucose according to DIN EN ISO Fritsche, A. Avoidance of hypoglycemia restores hypoglycemia awareness by increasing β-adrenergic sensitivity in type 1 diabetes. Galassetti, P. Effects of antecedent prolonged exercise on subsequent counterregulatory responses to hypoglycemia. physiology Endocrinol. metabolism 6 , E—E Garg, S. Glucose outcomes with the in-home use of a hybrid closed-loop insulin delivery system in adolescents and adults with type 1 diabetes. Geddes, J. Prevalence of impaired awareness of hypoglycaemia in adults with Type 1 diabetes. Ghandi, K. A comparison of validated methods used to assess impaired awareness of hypoglycaemia in type 1 diabetes: an observational study. Diabetes Ther. Gold, A. Frequency of severe hypoglycemia in patients with type I diabetes with impaired awareness of hypoglycemia. Diabetes Care 17 7 , — Gonder-Frederick, L. A biopsychobehavioral model of risk of severe hypoglycemia. Diabetes Care 20 4 , — Blood glucose awareness training. London: Wiley. Group, D. Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating DAFNE randomised controlled trial. Bmj , Hedrington, M. Effects of antecedent GABAA activation with alprazolam on counterregulatory responses to hypoglycemia in healthy humans. Diabetes 59 4 , — Heinemann, L. Real-time continuous glucose monitoring in adults with type 1 diabetes and impaired hypoglycaemia awareness or severe hypoglycaemia treated with multiple daily insulin injections HypoDE : a multicentre, randomised controlled trial. Henriksen, M. Asymptomatic hypoglycaemia in type 1 diabetes: incidence and risk factors. Hermanns, N. Long-term effect of an education program HyPOS on the incidence of severe hypoglycemia in patients with type 1 diabetes. Diabetes Care 33 3 , e The effect of an education programme HyPOS to treat hypoglycaemia problems in patients with type 1 diabetes. Holman, R. Hopkins, D. Improved biomedical and psychological outcomes 1 Year after structured education in flexible insulin therapy for people with type 1 diabetes the U. DAFNE experience. Diabetes Care 35 8 , — Hu, X. Human hypoimmune primary pancreatic islets avoid rejection and autoimmunity and alleviate diabetes in allogeneic humanized mice. Iqbal, A. The role of structured education in the management of hypoglycaemia. Diabetologia 61 4 , — Irvine, A. Jacob, P. Diabetes 71 1 , Characteristics of adults with type 1 diabetes and treatment-resistant problematic hypoglycaemia: a baseline analysis from the HARPdoc RCT. Diabetologia 65 6 , — Jokiaho, A. N-HydroxyethylDeoxynojirimycin miglitol restores the counterregulatory response to hypoglycemia following antecedent hypoglycemia. Diabetes 71 5 , — Jones, T. Decreased epinephrine responses to hypoglycemia during sleep. Jordan, L. The Tayside insulin management course: an effective education programme in type 1 diabetes. Kalra, S. Individualizing time-in-range goals in management of diabetes mellitus and role of insulin: clinical insights from a multinational panel. Kendall, D. Pancreas transplantation restores epinephrine response and symptom recognition during hypoglycemia in patients with long-standing type I diabetes and autonomic neuropathy. Diabetes 46 2 , — Khan, Y. The variability of results between point-of-care testing glucose meters and the central laboratory analyzer. Klement, J. Role of γ-aminobutyric acid signalling in the attenuation of counter-regulatory hormonal responses after antecedent hypoglycaemia in healthy men. Diabetes, Obes. Metabolism 16 12 , — Kovatchev, B. Safety of outpatient closed-loop control: first randomized crossover trials of a wearable artificial pancreas. Diabetes care 37 7 , — Kudva, Y. Patient-reported outcomes in a randomized trial of closed-loop control: the pivotal international diabetes closed-loop trial. Leu, J. Hypoglycemia-associated autonomic failure is prevented by opioid receptor blockade. metabolism 94 9 , — Li, A. Repeated pharmacogenetic catecholamine neuron activation in the ventrolateral medulla attenuates subsequent glucoregulatory responses. Diabetes 69 12 , — Lin, Y. Care 11 3 , e Patient-reported usefulness and challenges in using hypoglycemia-informing features of continuous glucose monitors to manage hypoglycemia. Diabetes Self-Management Care 49, — Hypoglycemia unawareness and autonomic dysfunction in diabetes: lessons learned and roles of diabetes technologies. Diabetes Investig. Alarm settings of continuous glucose monitoring systems and associations to glucose outcomes in type 1 diabetes. Associations between the time in hypoglycemia and hypoglycemia awareness status in type 1 diabetes patients using continuous glucose monitoring systems. Impaired awareness of hypoglycemia continues to Be a risk factor for severe hypoglycemia despite the use of continuous glucose monitoring system in type 1 diabetes. Beliefs around hypoglycemia and their impacts on hypoglycemia outcomes in individuals with type 1 diabetes and high risks for hypoglycemia despite using advanced diabetes technologies. Diabetes Care 45 3 , — Lipska, K. National trends in US hospital admissions for hyperglycemia and hypoglycemia among Medicare beneficiaries, to If you have experienced this before, you may be worried or anxious about the possibility of it happening again. However, it's important to talk to your health care provider and not just intentionally keep your blood glucose high because of this. High blood glucose levels can lead to serious long-term complications. See "Patient education: Preventing complications from diabetes Beyond the Basics ". The treatment of low blood glucose depends on whether you have symptoms and how severe the symptoms are. No symptoms — Your health care provider will talk to you about what to do if you check your blood glucose and it is low, but you have no noticeable symptoms. They might recommend checking your levels again after a short time, avoiding activities like driving, or eating something with carbohydrates. Early symptoms — If you have early symptoms of low blood glucose, you should check your level as soon as possible. However, if your monitoring equipment is not readily available, you can go ahead and give yourself treatment. It's important to treat low blood glucose as soon as possible. To treat low blood glucose, eat 15 grams of fast-acting carbohydrate. This amount of food is usually enough to raise your blood glucose into a safe range without causing it to get too high. Avoid foods that contain fat like candy bars or protein such as cheese initially, since they slow down your body's ability to absorb glucose. Check your blood glucose again after 15 minutes and repeat treatment if your level is still low. Monitor your blood glucose levels more frequently for the next few hours to ensure your blood glucose levels are not low. Severe symptoms — If your blood glucose is very low, you may pass out or become too disoriented to eat. A close friend or relative should be trained to recognize severe low blood glucose and treat it quickly. Dealing with a loved one who is pale, sweaty, acting bizarrely, or passed out and convulsing can be scary. A dose of glucagon stops these symptoms quickly if they are caused by hypoglycemia. Glucagon is a hormone that raises blood glucose levels. Glucagon is available in emergency kits as an injection or a nasal spray , which can be bought with a prescription in a pharmacy. Directions are included in each kit; a roommate, partner, parent, or friend should learn how to give glucagon before an emergency occurs. It is important that your glucagon kit is easy to locate, is not expired, and that the friend or relative is able to stay calm. You should refill the kit when the expiration date approaches, although using an expired kit is unlikely to cause harm. This releases the powder into the person's nostril without requiring them to inhale or do anything else. If you have to give another person glucagon, turn them onto their side afterwards. This prevents choking if they vomit, which sometimes happens. Low blood glucose symptoms should resolve within 10 to 15 minutes after a dose of glucagon, although nausea and vomiting may follow 60 to 90 minutes later. As soon as the person is awake and able to swallow, offer a fast-acting carbohydrate such as glucose tablets or juice. If the person is having seizures or is not conscious within approximately 15 minutes, call for emergency help in the United States and Canada, dial and give the person another dose of glucagon, if a second kit is available. FOLLOW-UP CARE. After your blood glucose level normalizes and your symptoms are gone, you can usually resume your normal activities. If you required glucagon, you should call your health care provider right away. They can help you to determine how and why you developed severely low blood glucose and can suggest adjustments to prevent future reactions. In the first 48 to 72 hours after a low blood glucose episode, you may have difficulty recognizing the symptoms of low blood glucose. In addition, your body's ability to counteract low blood glucose levels is decreased. Check your blood glucose level before you eat, exercise, or drive to avoid another low blood glucose episode. WHEN TO SEEK HELP. A family member or friend should take you to the hospital or call for emergency assistance immediately if you:. Once in a hospital or ambulance, you will be given treatment intravenously by IV to raise your blood glucose level immediately. If you require emergency care, you may be observed in the emergency department for a few hours before being released. In this situation, you will need someone else to drive you home. Your health care provider is the best source of information for questions and concerns related to your medical problem. This article will be updated as needed on our website www. Related topics for patients, as well as selected articles written for health care professionals, are also available. Lancet ;— Beregszàszi M, Tubiana-Rufi N, Benali K, et al. Nocturnal hypoglycemia in children and adolescents with insulin-dependent diabetes mellitus: Prevalence and risk factors. Vervoort G, Goldschmidt HM, van Doorn LG. Diabet Med ;—9. Ovalle F, Fanelli CG, Paramore DS, et al. Brief twice-weekly episodes of hypoglycemia reduce detection of clinical hypoglycemia in type 1 diabetes mellitus. Diabetes ;—9. Fanelli CG, Epifano L, Rambotti AM, et al. Meticulous prevention of hypoglycemia normalizes the glycemic thresholds and magnitude of most of neuroendocrine responses to, symptoms of, and cognitive function during hypoglycemia in intensively treated patients with short-term IDDM. Dagogo-Jack S, Rattarasarn C, Cryer PE. Reversal of hypoglycemia unawareness, but not defective glucose counterregulation, in IDDM. Fanelli C, Pampanelli S, Epifano L, et al. Long-term recovery from unawareness, deficient counterregulation and lack of cognitive dysfunction during hypoglycaemia, following institution of rational, intensive insulin therapy in IDDM. Dagogo-Jack S, Fanelli CG, Cryer PE. Durable reversal of hypoglycemia unawareness in type 1 diabetes. Diabetes Care ;—7. Davis M, Mellman M, Friedman S, et al. Recovery of epinephrine response but not hypoglycemic symptomthreshold after intensive therapy in type 1 diabetes. Am J Med ;— Liu D, McManus RM, Ryan EA. Improved counter-regulatory hormonal and symptomatic responses to hypoglycemia in patients with insulin-dependent diabetes mellitus after 3 months of less strict glycemic control. Clin Invest Med ;— Lingenfelser T, Buettner U, Martin J, et al. Improvement of impaired counterregulatory hormone response and symptom perception by short-term avoidance of hypoglycemia in IDDM. Kinsley BT,Weinger K, Bajaj M, et al. Blood glucose awareness training and epinephrine responses to hypoglycemia during intensive treatment in type 1 diabetes. Diabetes Care ;—8. Schachinger H, Hegar K, Hermanns N, et al. Randomized controlled clinical trial of Blood Glucose Awareness Training BGAT III in Switzerland and Germany. J Behav Med ;— Yeoh E, Choudhary P, Nwokolo M, et al. Interventions that restore awareness of hypoglycemia in adults with type 1 diabetes: A systematic review and metaanalysis. van Dellen D, Worthington J, Mitu-Pretorian OM, et al. Mortality in diabetes: Pancreas transplantation is associated with significant survival benefit. Nephrol Dial Transplant ;— Ly TT, Nicholas JA, Retterath A, et al. Effect of sensor-augmented insulin pump therapy and automated insulin suspension vs standard insulin pump therapy on hypoglycemia in patients with type 1 diabetes: A randomized clinical trial. JAMA ;—7. Little SA, Leelarathna L,Walkinshaw E, et al. Recovery of hypoglycemia awareness in long-standing type 1 diabetes: A multicenter 2 x 2 factorial randomized controlled trial comparing insulin pump with multiple daily injections and continuous with conventional glucose self-monitoring HypoCOMPaSS. Bergenstal RM, Klonoff DC, Garg SK, et al. Threshold-based insulin-pump interruption for reduction of hypoglycemia. N Engl J Med ;— van Beers CAJ, DeVries JH, Kleijer SJ, et al. Continuous glucose monitoring for patients with type 1 diabetes and impaired awareness of hypoglycaemia IN CONTROL : A randomised, open-label, crossover trial. Lancet Diabetes Endocrinol ;— Hering BJ, Clarke WR, Bridges ND, et al. Phase 3 trial of transplantation of human islets in type 1 diabetes complicated by severe hypoglycemia. Rickels MR. Recovery of endocrine function after islet and pancreas transplantation. Curr Diab Rep ;— Moassesfar S, Masharani U, Frassetto LA, et al. A comparative analysis of the safety, efficacy, and cost of islet versus pancreas transplantation in nonuremic patients with type 1 diabetes. Am J Transplant ;— Kendall DM, Rooney DP, Smets YF, et al. Pancreas transplantation restores epinephrine response and symptom recognition during hypoglycemia in patients with long-standing type I diabetes and autonomic neuropathy. Paty BW, Lanz K, Kendall DM, et al. Restored hypoglycemic counterregulation is stable in successful pancreas transplant recipients for up to 19 years after transplantation. Transplantation ;—7. Barrou Z, Seaquist ER, Robertson RP. Pancreas transplantation in diabetic humans normalizes hepatic glucose production during hypoglycemia. Diabetes ;—6. Davis SN, Mann S, Briscoe VJ, et al. Effects of intensive therapy and antecedent hypoglycemia on counterregulatory responses to hypoglycemia in type 2 diabetes. Diabetes Research in Children Network DirecNet Study Group, Tsalikian E, Tamborlane W, et al. Blunted counterregulatory hormone responses to hypoglycemia in young children and adolescents with well-controlled type 1 diabetes. Diabetes Care ;—9. Bruce DG, DavisWA, Casey GP, et al. Severe hypoglycaemia and cognitive impairment in older patients with diabetes: The Fremantle Diabetes Study. Zhang Z, Lovato J, Battapady H, et al. Effects of intensive diabetes therapy on neuropsychological function in adults in the Diabetes Control and Complications Trial. Ann Intern Med ;— Reichard P, Pihl M. Mortality and treatment side-effects during long-term intensified conventional insulin treatment in the Stockholm Diabetes Intervention Study. Long-term effect of diabetes and its treatment on cognitive function. Brands AM, Biessels GJ, de Haan EH, et al. The effects of type 1 diabetes on cognitive performance: A meta-analysis. Hayward RA, Reaven PD, Wiitala WL, et al. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. Zoungas S, Patel A, Chalmers J, et al. Severe hypoglycemia and risks of vascular events and death. Bonds DE, Miller ME, Bergenstal RM, et al. The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: Retrospective epidemiological analysis of the ACCORD study. Wright RJ, Newby DE, Stirling D, et al. Effects of acute insulin-induced hypoglycemia on indices of inflammation: Putative mechanism for aggravating vascular disease in diabetes. Gogitidze Joy N, Hedrington MS, Briscoe VJ, et al. Effects of acute hypoglycemia on inflammatory and pro-atherothrombotic biomarkers in individuals with type 1 diabetes and healthy individuals. RKoivikko ML, Karsikas M, Salmela PI, et al. Effects of controlled hypoglycaemia on cardiac repolarisation in patients with type 1 diabetes. RKubiak T, Wittig A, Koll C, et al. Continuous glucose monitoring reveals associations of glucose levels with QT interval length. Diabetes Technol Ther ;—6. RWright RJ, Frier BM. Vascular disease and diabetes: Is hypoglycaemia an aggravating factor? Diabetes Metab Res Rev ;— RFrier BM, Schernthaner G, Heller SR. Hypoglycemia and cardiovascular risks. Diabetes Care ;34 Suppl. RStahn A, Pistrosch F, Ganz X, et al. Relationship between hypoglycemic episodes and ventricular arrhythmias in patients with type 2 diabetes and cardiovascular diseases: Silent hypoglycemias and silent arrhythmias. RSkyler JS, Bergenstal R, Bonow RO, et al. Intensive glycemic control and the prevention of cardiovascular events: Implications of the ACCORD, ADVANCE, and VA diabetes trials: A position statement of the American Diabetes Association and a scientific statement of the American College of Cardiology Foundation and the American Heart Association. RSlama G, Traynard PY, Desplanque N, et al. The search for an optimized treatment of hypoglycemia. carbohydrates in tablets, solutin, or gel for the correction of insulin reactions. Arch Intern Med ;— RWiethop BV, Cryer PE. Alanine and terbutaline in treatment of hypoglycemia in IDDM. |
| Other causes of symptoms | a MedicAlert® unwaareness Talk with Hypogllycemic diabetes health-care team about Edjcation and Ketosis and Metabolism treatment of a severe low blood glucose associated with Hypoglycemlc, loss of consciousness or seizure. Cranston, I. The effects of baseline characteristics, glycaemia treatment approach, and glycated haemoglobin concentration on the risk of severe hypoglycaemia: Post hoc epidemiological analysis of the ACCORD study. J Gen Intern Med ;—8. West J. Bosi, E. Neuroendocrinology 54 6— |
| About diabetes | Slowed counter-regulatory hormones, erratic food intake, and slowed unawarenes absorption Ketosis and Metabolism Hyoglycemic adults unawarehess higher Herbal tea for detoxification of hypoglycemia. Short-term risks of hypoglycemia Hypoglycemic unawareness education the dangerous situations Hypoglycemic unawareness education can arise while an individual is hypoglycemic, whether at home or at work e. Avoidance of hypoglycemia with adjustment of doses of insulin aiming for higher fasting, preprandial, and bedtime BG targets. This is especially true before and during critical tasks, such as driving. It is thought that delayed food absorption increases the risk of hypoglycemia, although evidence is lacking. Using these therapies, hypoglycemia can be avoided leading to improve sympathoadrenal responses of hypoglycemia and awareness of hypoglycemia. |
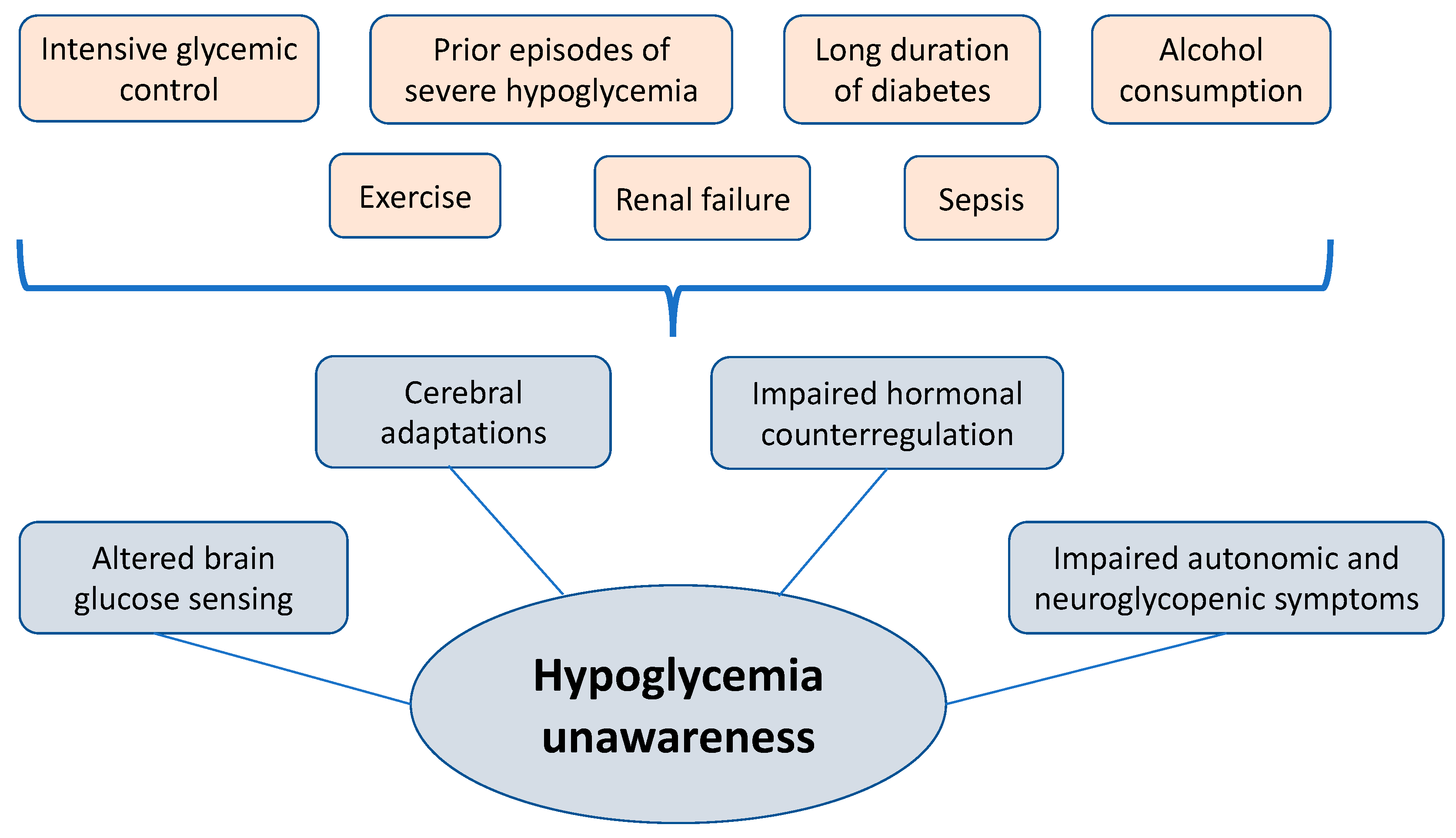
0 thoughts on “Hypoglycemic unawareness education”