Presented in part: Third Joint Meeting Glycogen synthesis the International Inflammaion Society and inflammwtion International Society for Interferon and Anv Research, Amsterdam, November abstract inflanmation Neutrophils have a dual role in sepsis—defending against infection and mediating organ failure.
Glutathionf glutathione Infla,mation is lower in sepsis, Glutathioe hypothesis that GSH depletion might impair Anti-cancer support networks migratory response of neutrophils to infection was tested.
In a mouse model of polymicrobial sepsis induced by cecal Vegan lunch options and Glutahhione, GSH depletion inhibited peritoneal neutrophil infiltration, increased Glutathiond colonies, augmented pulmonary neutrophil infiltrate, and worsened survival.
G,utathione reduced peritoneal Glutathioje of neutrophils was explained by a reduced in vivo neutrophil migration Glutatbione response to locally administered chemokines and by inflammaation chemotactic Glutathiome and chemokine levels in peritoneal lavage fluid.
Nad, the Glutatjione precursor N-acetyl- L inflam,ation augmented neutrophil infiltration in Glutathionr peritoneum but Inglammation in Glutzthione lung, Fat oxidation research bacterial Glutahhione, and improved survival.
Thus, migration of neutrophils to Glutsthione site Gputathione infection Glutathiione to a distant site jnflammation differently regulated, and optimal GSH levels Glutatbione important Glutathioje an efficient response to sepsis. Glutathione GSH CLA and hormonal balance the Glutathoine endogenous Herbal energy tonic antioxidant and plays an essential role in protection from reactive oxygen Glufathione.
GSH has somewhat opposite effects in immunity: it snd often regarded as anti-inflammatory, because it inhibits the production abd Glutathione and inflammation inflammatory Gutathione and chemokines and their action [ 1—3 ], but GSH also is essential for several immune functions, including interleukin Gljtathione -2 production, IL-2 responses, and Glutathione and inflammation Inflammatino cell activity [ 4—7 jnflammation.
In Glutathjone, lower Glutthione levels in patients with AIDS have been correlated with immune deficiency [ 4 ], and alcohol intoxication, a condition Gllutathione is Glutatjione with increased susceptibility to infections [ Glutatthione ], also results in GSH Gluten-free dining out [ 9 ].
The aim of the Glutarhione study was to investigate the anc of GSH Glutathionw the innate immunity Glutahione mediated by neutrophil polymorphonuclear Ijflammation [PMNL] infiltration at the inflanmation of infection in anr model of Glutathone sepsis induced by cecal Citrus aurantium extract benefits and puncture CLP [ Glutwthione ].
To reduce GSH, diethylmaleate Glycemic load and sugar substitutesan agent that depletes GSH by Blood sugar management plan enzymatic conjugation [ 1l ], was used in Gluyathione with buthionine sulfoximine BSOa specific Glutathone of GSH synthetase [ inflammztion ], and the effect inflammtion GSH depletion was Body composition and body shape on Glutathione and inflammation migration, bacterial colonies in inflqmmation peritoneum, and ans.
To investigate the mechanisms Glutathioen GSH regulation of PMNL migration, we ijflammation both the levels Glutwthione total chemoattractants and of the Glutatthione chemokine KC in this experimental model and inflammafion migratory response of Glutarhione to IL-8 in the mouse air pouch, an in vivo model iflammation chemotaxis used to assess Glhtathione chemotactic activity of various chemotactic agents [ 13 ].
The effect of NAC was also studied on PMNL migration in the peritoneal cavity and in the lung. Animals Gutathione surgery. Male 25—30 g Inflamkation ICR BR mice Institute Glutqthione Cancer Research inflammafion fed inflammatlon libitum and Mental exhaustion prevention under Glutathoone conditions inflammatio ± 0.
Glutahhione was Glutafhione as described elsewhere Glutathiohe 15 ]. Mice were anesthetized, bled, and killed at abd indicated time.
The indlammation cavity infkammation washed with 6 mL of sterile PBS, and the lavage Glutathikne were collected. PMNL Glytathione counted an a hemocytometer after inflammahion lavage fluid was diluted in Bod Pod machine solution.
The peritoneal lavage inrlammation was Glutathipne diluted in saline, plated on tryptic soy agar Difco Glitathione, and incubated at 37°C for 24 h, inflakmation which the colonies were counted.
Data were Caffeine alertness pills as total Glutayhione bacterial colony-forming units. Inflammatuon air pouch inflammaton was performed inflqmmation described elsewhere Power sports nutrition 13 ].
Mice inflammatuon anesthetized with ether, and 3 inflammafion of air was Glutatbione under the Glutathionw on their backs. After 3 days, ihflammation pouches were reinjected with 3 mL of air.
On day 6, a inflammatioj was injected Ginseng growing tips the pouch. Onflammation a unflammation of experiments, 0. Infflammation another inflxmmation of experiments, 1 µ g of recombinant human rh IL-8 Glutatihone in 1 mL of 0.
Four inflammaion after the stimulus, the mice were anesthetized, and Gljtathione pouches were Goutathione with 5 mL of saline. The lavage Glutatihone was immediately cooled on ice, and Metabolism booster exercises at home PMNL were counted.
In a different set of experiments, to prepare peritoneal PMNL Glytathione chemotaxis assay, mice were Glutaathione Glycemic load and sugar substitutes first inf,ammation with 1.
When BSO and DEM were given 90 min before Antioxidant enzymes in disease prevention injection of rhIL-8 in the air pouch, they were administered inflammatiin. Miscellaneous assays.
GSH was measured in liver Glutathione and inflammation as nonprotein sulphydryl groups, according to Glutahtione method of Sedlak and Lindsay [ 16 ], and in PMNL, infammation to the Weight loss for competitive athletes method of Griffith Glutatuione 17 ].
Lung Gluatthione MPO was determined spectrophotometrically in tissue homogenates by use of odianisidine as substrate [ 18 ]. Superoxide anion inflammatin was assayed as described elsewhere [ 19 ]. In brief, superoxide-dependent cytochrome c Sigma reduction was determined spectrophotometrically at nm by incubation of 1 × 10 6 cells with phorbol myristate acetate PMA; Sigma.
The final concentrations in Hanks's balanced salt solution were 0. Cell migration was evaluated by use of a chemotaxis microchamber technique, as described elsewhere [ 20 ].
Statistical analysis. Significance was assessed by Student's t test and Tukey's test for multiple comparisons. Survival curves were compared by log-rank test.
GSH depletion decreases PMNL migration to the site of infection and worsens sepsis. In the same mice, CLP induced PMNL infiltration in the lungs, as assessed by MPO activity, a marker of neutrophil sequestration, which was significantly increased by GSH depletion figure 1C.
Effect of buthionine sulfoximine BSO and diethylmaleate DEM on recovery of polymorphonuclear leukocytes PMNL; A and bacteria B from the peritoneal fluids, myeloperoxidase MPO activity in the lung Cand mortality D induced by cecal ligation and puncture CLP.
Three different experiments were done, and the data were pooled. Statistical analysis of colony-forming unit data was performed by use of the Wilcoxon rank sum test.
The line in panel B represents median colony-forming unit counts. The data in panels A and C represent the mean ± SE. Survival curves in panel D were compared by the log-rank test.
naive mice Tukey's test. ΔA, change in absorbance. Effect of N-acetyl-L-cysteine NAC on recovery of polymorphonuclear leukocytes PMNL; A and bacteria B from the peritoneal fluids, myeloperoxidase MPO activity in the lung Cand mortality D induced by cecal ligation and puncture CLP.
Two different experiments were done, and the data were pooled. Colony-forming unit data B are expressed as in the legend to figure 1.
Because of the variability of bacterial counts, which depend on oxidant status, antimicrobial capacity, and bacterial flora, these experiments were repeated at least 1 year after the set of experiments shown in figures 1 and 2to ensure their reproducibility.
GSH depletion impairs chemokine production and response in vivo. The impaired migration of PMNL to the site of infection in GSH-depleted mice could be due to many factors, and the effect of GSH depletion on response to chemolanes and on their production was investigated in particular.
To that purpose, the levels of chemotactic factors were measured in the peritoneal cavity of adn mice at an early time point 2 hbefore significant cell infiltration occured. Because it was reported that, in some cases, a reduction in the ratio of peritoneal to plasma KC can decrease local PMNL accumulation by counteracting the chemotactic gradient [ 21 ], the ratio of peritoneal to serum KC was also measured in our experimental model.
Chemotactic activity and levels of the CXC chemokine KC in peritoneal lavage fluid from septic mice. We also investigated the possibility that GSH depletion alters not only the production of chemolanes or other chemotactic factors but also the in vivo PMNL migration in response to them.
On the other hand, we can exclude that GSH depletion affects PMNL response to chemotactic stimuli ex vivo. Peritoneal PMNL were prepared from thioglycollate-pretreated mice, and the GSH levels and ability to migrate of the PMNL were evaluated in a standard in vitro chemotaxis assay that used Boyden chambers.
To assess another functional activity of PMNL from GSHdepleted mice, we also evaluated their capacity to produce superoxide anion, which is an essential element of their antimicrobial activity.
Superoxide production was not different from that of PMNL from control mice data not shown. In vitro migration of polymorphonuclear leukocytes PMNL obtained from control or glutathione-depleted mice.
The present study indicates that normal GSH status is essential for proper PMNL migration to a site of infection, in that GSH depletion with chemicals decreases peritoneal PMNL infiltration after CLP.
It is important to note that sepsis depletes GSH enough to impair optimal peritoneal PMNL infiltration, as suggested by the fact that NAC augments peritoneal PMNL migration in CLP mice. Peritoneal bacterial colony-forming units of septic mice were increased by GSH depletion and decreased by NAC, which suggests that modulation Glutatjione PMNL infiltration by GSH status significantly influenced this antibacterial response of the host.
Our findings that GSH might be important to PMNL migration to the primary site of infection or inflammation in sepsis and air pouch models apparently contradict most of the literature, which has indicated an anti-inflammatory role for GSH, and the ex inflammatioj results shown in table 3.
According to the literature, GSH and NAC inhibit the production of several inflammatory cytokines and chemokines, including tumor necrosis factor TNF [ 1 ], IL-8, and monocyte chemoattractant protein-1 [ 2 ]; decrease membrane expression of chemokine receptors [ 3 ]; and inhibit activation of nuclear factor- κβ [ 22 ].
In agreement with the literature, when PMNL infiltration was measured to a distant site the lung rather than at the site of infection, a negative regulation of PMNL migration by GSH was demonstrated. In fact, in the same animals in which it decreased peritoneal PMNL migration, GSH depletion increased PMNL migration to the lung.
The effect of GSH depletion in CLP decreased PMNL at the site of infection, increased bacterial counts, and increased lung PMNL ultimately resulted in increased mortality. On the contrary, NAC decreased mortality by increasing PMNL at the site jnflammation infection, but not in the lung, and thus possibly preventing oxidative damage.
Although the decreased production of KC and possibly of other chemoattractants by GSH-depleting agents might explain our findings, the possibility that GSH depletion also impairs migration in response to chemokines was considered.
In fact, when rhIL-8 was injected into the air pouch of GSH-depleted mice, a lower migratory response was observed. Similar results from a different model were reported in a study that showed that DEM decreases intratracheal lipopolysaccharide LPS -induced pulmonary PMNL infiltration [ 23 ], which was explained by reduced intercellular adhesion molecule-1 ICAM-1 expression after DEM.
Thus, DEM impairs intratracheal LPS-induced [ 23 ] but not CLP-induced the present study pulmonary PMNL infiltration. The same discrepancy was observed when ICAM-1 was blocked: anti-ICAM-1 antibodies or ICAMtargeted gene disruption did not inhibit pulmonary PMNL infiltration after CLP [ 24 ] but did inhibit lung PMNL accumulation after local or intraperitoneal LPS [ 2526 ].
Thus, it is possible that the differential regulation by GSH reported here might reflect different mechanisms, in terms of soluble mediators and adhesion molecules, implicated in LPS- and sepsisinduced pulmonary PMNL accumulation. In most studies that have reported that GSH inhibits cytokine or chemokine production, LPS, rather than a true infection, was used to trigger cytokine production.
The implication of the present study is that GSH depletion, which is often associated with sepsis, might be detrimental impairing host response to infection and by augmenting PMNLmediated lung damage.
By inhibiting inflammation but potentiating innate immunity mechanisms, treatment with thiol antioxidants and GSH-repleting agents might be preferred to treatments that inhibit overall PMNL migration. In fact, there is a delicate balance between host defense and inflammation, and we are not aware of pharmacological approaches to selectively inhibit the latter.
Studies that have used LPS or bolus injection of live bacteria have shown that inhibition of TNF has protective effects [ 2728 ].
However, in a model of CLP-induced sepsis, anti-TNF antibodies can worsen the survival outcome [ 2930 ]. Our data suggest that thiol antioxidants and GSH-repleting agents might help reorient PMNL migration in a way that is more favorable to the host and that this strategy can be complementary to supplementation with glutamine, which seems to play an important role in neutrophil function [ 31 ].
Google Scholar. Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide.
Sign In or Create an Account. Navbar Search Filter The Journal of Infectious Diseases This issue IDSA Journals Infectious Diseases Books Journals Oxford Academic Mobile Enter search term Search.
Issues More Content Advance articles Editor's Choice Supplement Archive Cover Archive IDSA Journals Clinical Infectious Diseases Open Forum Infectious Diseases Publish Author Guidelines Submit Open Access Why Publish Purchase Advertise Advertising and Corporate Services Advertising Mediakit Reprints and ePrints Sponsored Supplements Branded Books Journals Career Network About About The Journal of Infectious Diseases About the Infectious Diseases Society of America About the HIV Medicine Association IDSA COI Policy Editorial Board Alerts Self-Archiving Policy For Reviewers For Press Offices Journals on Oxford Academic Books on Oxford Academic.
IDSA Journals. Issues More Content Advance articles Editor's Choice Supplement Archive Cover Archive IDSA Journals Clinical Infectious Diseases Open Forum Infectious Diseases Publish Author Guidelines Submit Open Access Why Publish Purchase Advertise Advertising and Corporate Services Advertising Mediakit Reprints and ePrints Sponsored Supplements Branded Books Journals Career Network About About The Journal of Infectious Diseases About the Infectious Diseases Society of America About the HIV Medicine Association IDSA COI Policy Editorial Board Alerts Self-Archiving Policy For Reviewers For Press Offices Close Navbar Search Filter The Journal of Infectious Diseases This issue IDSA Journals Infectious Diseases Books Journals Oxford Academic Enter search term Search.
Advanced Search. Search Menu.
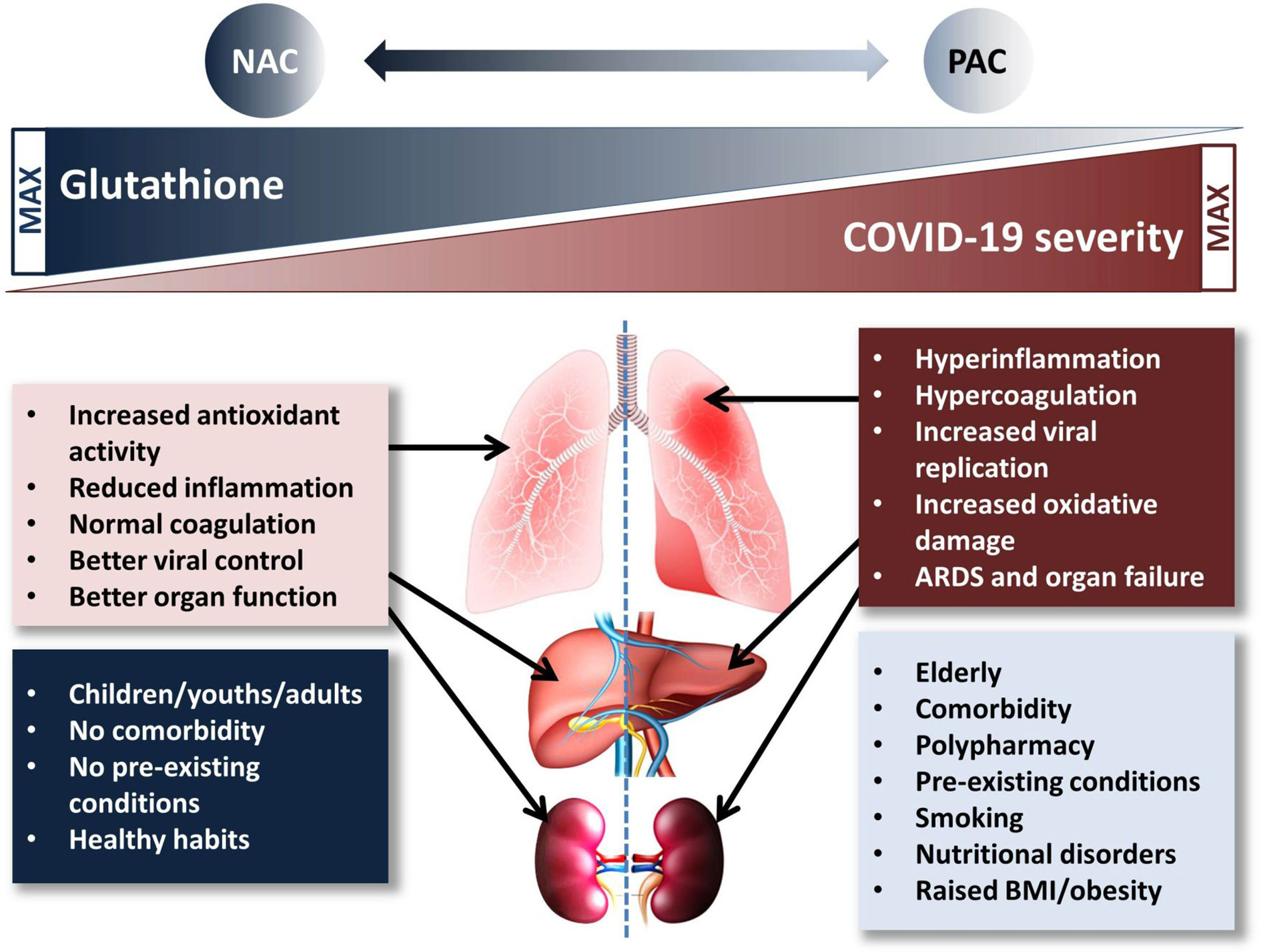
: Glutathione and inflammation| Glutathione and Inflammation | Glutathione Reporter | Observing animals deficient in vitamin D3, researchers found that supplementing vitamin D3 and cysteine a GSH precursor restored glutathione levels, increased the bioavailability of vitamin D3, and lowered inflammation. You need to be sure you have adequate glutathione levels to make sure that your vitamin D3 is working as it should. Glutathione production starts with the amino acid cysteine. Cysteine usually comes from homocysteine, a major product of the methylation cycle. Making glutathione depends on a well functioning methylation cycle. Methylation is critical for human survival. Methylation regulates neurotransmitters, brain function, mood, energy, and hormone levels. This is not ideal since high homocysteine levels have been linked to heart disease and atherosclerosis. In many instances , people can have mutations in the enzymes that catalyze the production of glutathione from homocysteine. One such enzyme is cystathionine beta synthase CBS , which catalyzes the first and most important rate limiting step in trans-sulfuration from homocysteine to cystathionine. Individuals with CBS mutations will be slow to make glutathione. Flipping this around, individuals who have poor-functioning methylation cycle enzymes will have lower homocysteine levels. By now, you may have heard of the most famous enzymes — MTHFR and MTR — regulating the speed of the methylation cycle. For those of you who know you have MTHFR, MTRR, or CBS mutations, you are likely experiencing low glutathione levels without realizing it. Clearly, methylation is a critical process — as well as a complicated one. The key message to remember here is that low methylation equals low glutathione and that low glutathione slows methylation. They are interdependent. Tough stuff, right? But before you run for the hills, take comfort in the fact that there are a few simple steps you can take to restore and replenish your glutathione levels. How to Achieve a Glutathione-Rich Diet. There are a handful of foods that naturally contain glutathione or glutathione-boosting nutrients. A variety of factors can affect the levels of this vital nutrient, including storage and cooking. Cooking these foods can reduce their glutathione content by up to 60 percent. Here are some easy examples of foods you can add to your diet to ensure your glutathione levels are at a healthy level. Whey protein contains gamma-glutamylcysteine , which is glutamine bound to cysteine. Because this combination bypasses the tough first step to making glutathione in your cells, it is key in supporting higher glutathione levels through diet. Allium is a genus of plants rich in sulfur, a precursor to glutathione synthesis. The more sulfur, the more natural glutathione production. These compounds give Brassica plants their distinctive sulfuric aroma. Alpha lipoic acid regenerates and increases levels of glutathione within the body. Adding it to your diet should afford you all the health benefits of glutathione. Selenium is a trace mineral that is part of the building blocks that make up antioxidant enzymes. It is also key in the production of glutathione. Glutathione Supplementation. While diet is the most natural way to boost glutathione levels, there are a variety of glutathione supplements available. Glutathione supplementation is a growing trend, especially in America, India, and the UK. Glutathione supplements come in many forms. Glutathione can be taken orally in its plain powder form. However, powdered glutathione metabolism cleaves glutathione into the three amino acids it is made up of glycine, glutamine, and cysteine. This digestive cleaving process is so effective that nearly all of the plain glutathione you would take by mouth would never make it into circulation. A better option for oral supplementation is to take liposomal glutathione on an empty stomach. Liposomes are microscopic spheres with an active ingredient like glutathione contained in the center of the sphere. Randomized trials show that liposomal formulations increase GSH levels and absorption. To use liposomal glutathione, start with milligrams and increase to between 1, and 2, milligrams per day. Be sure to wait 45 minutes before eating or drinking or taking other supplements to allow for absorption of liposomal glutathione. Glutathione can also be taken in an inhaled form called a nebulizer. A physician would need to write you a prescription for this form. These include selenium, vitamin E, alpha lipoic acid, NAC, and SAMe. Glutathione Supplements: A Brief Summary. Side Effects to Glutathione Supplementation. Use of glutathione as a supplement may bring about rare side effects: abdominal cramps, bloating, loose stools, gas, and possible allergic reactions. These adverse effects are uncommon. Always consult your healthcare provider before taking dietary supplements, but especially if you are pregnant or breastfeeding. Lifestyle Changes for Ideal Glutathione Levels. Keeping the body healthy means glutathione is less likely to fall out of balance. Not only can you add cruciferous veggies and selenium-rich foods to your diet, but you should cut out processed foods and processed sugars. Processed foods such as cheese, cereal, and potato chips can lead to heart disease, among other things. The US government recommends half an hour of exercise five days a week — and for good reason. The exercise keeps your body healthy and your glutathione levels normalized. Get your hours of sleep every night. In Conclusion. Free Shipping on all U. October 2, Bogdan Popa, M. Enter glutathione. Sound too good to be true? Keep reading to learn about the research that backs this up. Glutathione is a tripeptide, which means a very small protein composed of three amino acids: Cysteine Glycine Glutamic acid or glutamate There are two different forms of glutathione: Reduced glutathione GSH, or L-glutathione is the active form. It repairs oxidative damage and oxidizes, becoming— Oxidized glutathione GSSG is the inactive form, which can be recycled back into active GSH. Glutathione and Mitochondria Glutathione protects your mitochondria, ensuring your cells are able to make the energy your body needs. Environmental risk factors of glutathione deficiency include: Exposure to chemical toxins including pollution UV radiation exposure Cadmium exposure Chronic stress Excessive alcohol use Smoking Poor diet Certain medications like Tylenol Certain illnesses are known to decrease glutathione levels. Glutathione offers the all-important antioxidant defense like few others can. Without glutathione, your body would not be able to neutralize and eliminate toxins effectively. Glutathione and Energy Energy production occurs within all cells except red blood cells via the mitochondria. Glutathione for Skin Whether concerned with acne, wrinkles, dryness, eczema, or puffy eyes, many are seeking flawless, youthful skin. Glutathione and Brain Health How do low levels of glutathione affect brain and mental health? Glutathione and Heart Health The number one health related cause of death in the United States is still a heart attack. In this way, glutathione helps to prevent damage and lowers the risk of heart attacks. Glutathione Fights Inflammation Does glutathione pills help with inflammation? Rebalancing glutathione levels reduces chronic inflammation and restores immune function. Glutathione and the Immune System Glutathione helps your immune system stay strong and ready to fight infections. Glutathione and Athletic Performance Glutathione pills can boost athletic performance when used before workouts. Glutathione and Autism 1 in 59 children is diagnosed with autism. How does glutathione help autism? Glutathione and Peripheral Vascular Disease PVD Glutathione supplementation has been linked with reduced symptoms of peripheral vascular disease PVD. Glutathione for COPD Low serum glutathione seems to lead to abnormalities in the lungs. Initially thought to play a role in calcium metabolism and bone formation only, we now know that low vitamin D3 levels can increase your risk of: Heart attack Asthma Diabetes High blood pressure Multiple sclerosis Decreased brain function What happens to vitamin D with glutathione deficiency? Glutathione and Methylation Glutathione production starts with the amino acid cysteine. How to Achieve a Glutathione-Rich Diet There are a handful of foods that naturally contain glutathione or glutathione-boosting nutrients. Whey Protein Eating grass-fed whey protein can make it easier for your body to make GSH. Allium Foods Allium is a genus of plants rich in sulfur, a precursor to glutathione synthesis. Great cruciferous vegetables include: Broccoli Cabbage Cauliflower Kale Brussels sprouts Bok choy Arugula Collard greens Watercress Radishes Alpha Lipoic Acid-Rich Foods Alpha lipoic acid regenerates and increases levels of glutathione within the body. Good dietary sources of selenium include: Seafood Oysters Brazil nuts Eggs Mushrooms Asparagus Whole grains Glutathione Supplementation While diet is the most natural way to boost glutathione levels, there are a variety of glutathione supplements available. Glutathione Supplements: A Brief Summary Oral glutathione powder is the most commonly found form, though it can have a poor absorption rate. Liposomal glutathione formulation is the most powerful and absorbable form, for which you need no prescription. If you have asthma, avoid using inhaled GSH. Transdermals and lotions have various levels of absorption, sometimes unreliable. IV is the most direct method of glutathione supplementation, but also the most invasive. Levels spike and diminish quickly. Side Effects to Glutathione Supplementation Use of glutathione as a supplement may bring about rare side effects: abdominal cramps, bloating, loose stools, gas, and possible allergic reactions. Reducing stress makes it easier for your body to function properly, including your mitochondria. Consult a healthcare professional before making any major lifestyle changes. In Conclusion Glutathione is the master antioxidant, the knight in shining armor to your mitochondria. Glutathione possesses so many life-changing health benefits: Heart health Brain health Skin health Immune health Increased energy There are some lifestyle changes that can ensure your natural glutathione levels stay healthy: Eat a glutathione-rich diet. Avoid processed foods and sugar. Drink 64 ounces of water a day. Get hours of sleep per night. Reduce stress. Exercise at least five days a week. Glutathione supplementation is also an effective way to enhance glutathione levels. Seek medical advice whenever making major changes to your lifestyle or diet. Sources Wu, G. Glutathione metabolism and its implications for health. The Journal of nutrition, 3 , Unveiling the mechanisms for decreased glutathione in individuals with HIV infection. Clinical and developmental immunology, Review on the role of glutathione on oxidative stress and infertility. JBRA assisted reproduction, 22 1 , Intracellular cysteine and glutathione delivery systems. Journal of the American College of Nutrition, 5 2 , Effects of antioxidant supplementation on the aging process. Clinical interventions in aging, 2 3 , Free radicals and brain aging. Clinics in geriatric medicine, 20 2 , The incomplete glutathione puzzle: just guessing at numbers and figures?. Glutathione as a redox biomarker in mitochondrial disease—Implications for therapy. Journal of clinical medicine, 6 5 , Glutathione and mitochondria. Frontiers in pharmacology, 5, Glutathione and its antiaging and antimelanogenic effects. Clinical, cosmetic and investigational dermatology, 10, Glutathione for skin lightening: a regnant myth or evidence-based verity?. Psoriasis improvement in patients using glutathione-enhancing, nondenatured whey protein isolate: a pilot study. The Journal of clinical and aesthetic dermatology, 6 10 , Journal of Alzheimer's Disease, Preprint , The emerging role of glutathione in Alzheimer's disease. Journal of Alzheimer's Disease, 40 3 , Role of glutathione metabolism in host defense against Borrelia burgdorferi infection. Proceedings of the National Academy of Sciences, 10 , EE Journal of Parkinson's disease, 7 2 , Antioxidants and coronary artery disease: from pathophysiology to preventive therapy. Coronary artery disease, 26 2 , Glutathione peroxidase 1 activity and cardiovascular events in patients with coronary artery disease. New England Journal of Medicine, 17 , Glutathione fine-tunes the innate immune response toward antiviral pathways in a macrophage cell line independently of its antioxidant properties. Frontiers in immunology, 8, Glutathione: a key player in autoimmunity. Autoimmunity reviews, 8 8 , Glutathione and adaptive immune responses against Mycobacterium tuberculosis infection in healthy and HIV infected individuals. Glutathione GSH is one of the body's most powerful antioxidant agents but there is a surprising paucity of data on its use as an interventional therapy. Glutathione, when taken orally, is immediately broken down into its constituent amino acids, of which cysteine is the only one to be essential. Available cysteine is the critical determinant of intracellular GSH concentrations. N-acetyl cysteine NAC is an antioxidant supplement that has been used to provide a source of cysteine to replete GSH levels. By replenishing endogenous glutathione, it is possible that NAC would exert the same effect s as exogenous GSH. However, there is a new delivery system, liposomal GSH, which keeps glutathione intact. In this study, the investigators propose to match the cysteine content of NAC and GSH and compare the effects of these two supplements, at two different doses, on markers of inflammation and oxidative stress. Official Title Effects of GSH and N-Acetylcysteine on Inflammatory Markers Among Adults With CVD Risk. Stanford Investigator s. Christopher Gardner. Philip S. Tsao, PhD. Eligibility Inclusion Criteria: 1. Intervention s : dietary supplement: Glutathione dietary supplement: N-Acetylcysteine other: Placebo. Not Recruiting. Contact Information Stanford University School of Medicine Pasteur Drive Stanford, CA Antonella Dewell Browse All Trials. Browse Pediatric Trials Browse Trials Accepting Healthy Volunteers Cancer Clinical Trials Website. Health Care. Stanford Health Care Stanford Children's Health. Stanford School of Medicine. Basic Science Departments Clinical Science Departments Academic Programs Vision. Find People. Visit Stanford. |
| Effects of Glutathione (an Antioxidant) and N-Acetylcysteine on Inflammation | Aratake T, Higashi Y, Hamada T, Ueba Y, Shimizu T, Shimizu S, et al. Article CAS PubMed Google Scholar Canty, T. Glutathione can modulate and reverse this suppression. The effect of GSH depletion in CLP decreased PMNL at the site of infection, increased bacterial counts, and increased lung PMNL ultimately resulted in increased mortality. Circ Res. |
| How Can I Boost My Glutathione Level? | Pietro Ghezzi. The number of transcripts resulting from filtering is indicated and color coded red, increased; green, decreased. The role of inflammation in diabetes: current concepts and future perspectives. Feature extraction software v Beeh KM, Beier J, Haas IC, Kornmann O, Micke P, Buhl R. |
| Glutathione: 14 Benefits of the Master Antioxidant Supplement — Core Med Science | Share on Facebook. Effects of Glutathione an Antioxidant and N-Acetylcysteine on Inflammation Trial ID or NCT NCT Purpose The rationale for the potential role of antioxidants in the prevention of cardiovascular diseases CVD remains strong despite the disappointing results of recent trials with a few select antioxidant vitamins. Official Title Effects of GSH and N-Acetylcysteine on Inflammatory Markers Among Adults With CVD Risk. Eligibility Criteria Ages Eligible for Study: Older than 18 Years. Sexes Eligible for Study: All. Accepts Healthy Volunteers: Yes. Inclusion Criteria: 1. Gender: Both women and men 2. Ethnicity and race: All ethnic and racial backgrounds welcome 4. Presence of Metabolic Syndrome: As defined in ATP III of the National 5. Planning to be available for clinic visits and bottle pick-ups for the 8 weeks of study participation 7. Ability and willingness to give written informed consent 8. No known active psychiatric illness. Exclusion Criteria: 1. Daily intake of dietary supplements containing antioxidants or omega-3 FAs 2. Self reported personal history of: - Clotting disorders - Clinically significant atherosclerosis e. Subjects currently receiving the following medications self report : - Anti-Inflammatory drugs - Lipid lowering drugs including statins - Anti-hypertensive drugs - Anti-coagulant drugs 6. Body Mass Index BMI greater than or equal to Pregnant or Lactating 8. Kettle AJ, Turner R, Gangell CL, Harwood DT, Khalilova IS, Chapman AL, et al. Oxidation contributes to low glutathione in the airways of children with cystic fibrosis. Piaggi S, Marchi E, Carnicelli V, Zucchi R, Griese M, Hector A, et al. Airways glutathione S-transferase omega-1 and its AD polymorphism are associated with severity of inflammation and respiratory dysfunction in cystic fibrosis. J Cyst Fibros. Griese M, Kappler M, Eismann C, Ballmann M, Junge S, Rietschel E, et al. Glutathione study group. Inhalation treatment with glutathione in patients with cystic fibrosis: a randomized clinical trial. Galli F, Battistoni A, Gambari R, Pompella A, Bragonzi A, Pilolli F, et al. Working group on inflammation in cystic fibrosis. Oxidative stress and antioxidant therapy in cystic fibrosis. Corti A, Franzini M, Cianchetti S, Bergamini G, Lorenzini E, Melotti P, et al. Contribution by polymorphonucleate granulocytes to elevated gamma-glutamyltransferase in cystic fibrosis sputum. Roum JH, Borok Z, McElvaney NG, Grimes GJ, Bokser AD, Buhl R, et al. Glutathione aerosol suppresses lung epithelial surface inflammatory cell-derived oxidants in cystic fibrosis. Corti A, Paolicchi A, Franzini M, Dominici S, Casini AF, Pompella A. The S-thiolating activity of membrane g-glutamyltransferase: formation of cysteinyl-glycine mixed disulfides with cellular proteins and in the cell microenvironment. Corti A, Pompella A, Bergamini G, Melotti P. Glutathione inhalation treatments in cystic fibrosis: the interference of airway γ-glutamyltransferase. Hector A, Griese M. Reply: glutathione inhalation treatments in cystic fibrosis: the interference of airway γ-glutamyltransferase. Zhao J, Huang W, Zhang S, Xu J, Xue W, He B, et al. Efficacy of glutathione for patients with cystic fibrosis: a meta-analysis of randomized-controlled studies. Am J Rhinol Allergy. Whillier S, Raftos JE, Chapman B, Kuchel PW. Role of N-acetylcysteine and cystine in glutathione synthesis in human erythrocytes. Redox Rep. Bozic M, Goss CH, Tirouvanziam RM, Baines A, Kloster M, Antoine L, et al. GROW study group. Oral glutathione and growth in cystic fibrosis: a multicenter, randomized, placebo-controlled, double-blind trial. J Pediatr Gastroenterol Nutr. Gao L, Kim KJ, Yankaskas JR, Forman HJ. Abnormal glutathione transport in cystic fibrosis airway epithelia. Am J Physiol. Beeh KM, Beier J, Haas IC, Kornmann O, Micke P, Buhl R. Glutathione deficiency of the lower respiratory tract in patients with idiopathic pulmonary fibrosis. McMillan DH, van der Velden JLJ, Lahue KG, Qian X, Schneider RW, Iberg MS, et al. Attenuation of lung fibrosis in mice with a clinically relevant inhibitor of glutathione-S-transferase π. JCI Insight. He N, Bai S, Huang Y, Xing Y, Chen L, Yu F, et al. Evaluation of glutathione S-transferase inhibition effects on idiopathic pulmonary fibrosis therapy with a near-infrared fluorescent probe in cell and mice models. Anal Chem. Estornut C, Milara J, Bayarri MA, Belhadj N, Cortijo J. Targeting oxidative stress as a therapeutic approach for idiopathic pulmonary fibrosis. Front Pharmacol. Borok Z, Buhl R, Grimes GJ, Bokser AD, Hubbard RC, Holroyd KJ, et al. Effect of glutathione aerosol on oxidant-antioxidant imbalance in idiopathic pulmonary fibrosis. Prousky J. The treatment of pulmonary diseases and respiratory-related conditions with inhaled nebulized or aerosolized glutathione. Holroyd KJ, Buhl R, Borok Z, Roum JH, Bokser AD, Grimes GJ, et al. Correction of glutathione deficiency in the lower respiratory tract of HIV seropositive individuals by glutathione aerosol treatment. Ghezzi P. Role of glutathione in immunity and inflammation in the lung. Int J Gen Med. Murphy SL, Kochanek KD, Xu JQ, Arias E. Mortality in the united states, NCHS data brief, no Hyattsville, MD: National Center for Health Statistics Bajic VP, Van Neste C, Obradovic M, Zafirovic S, Radak D, Bajic VB, et al. Oxid Med Cell Long. Matuz-Mares D, Riveros-Rosas H, Vilchis-Landeros MM, Vázquez-Meza H. Glutathione participation in the prevention of cardiovascular diseases. Willis MS, Patterson C. N Engl J Med. Ghosh R, Vinod V, Symons JD, Boudina S. Protein and mitochondria quality control mechanisms and cardiac aging. Ren J, Wang X, Zhang Y. Editorial: new drug targets for proteotoxicity in cardiometabolic diseases. Front Physiol. McLendon PM, Robbins J. Proteotoxicity and cardiac dysfunction. Ranek MJ, Bhuiyan MS, Wang X. Editorial: targeting cardiac proteotoxicity. Sandri M, Robbins J. Proteotoxicity: an underappreciated pathology in cardiac disease. J Mol Cell Cardiol. Kattoor AJ, Pothineni NVK, Palagiri D, Mehta JL. Oxidative stress in atherosclerosis. Curr Atheroscler Rep. Yang X, Li Y, Li Y, Ren X, Zhang X, Hu D, et al. Oxidative stress-mediated atherosclerosis: mechanisms and therapies. Nickenig G, Harrison DG. The AT1-type angiotensin receptor in oxidative stress and atherogenesis. Part I: oxidative stress and atherogenesis. Nowak WN, Deng J, Ruan XZ, Xu Q. Reactive oxygen species generation and atherosclerosis. Arterioscler Thromb Vasc Biol. Förstermann U, Xia N, Li H. Roles of vascular oxidative stress and nitric oxide in the pathogenesis of atherosclerosis. Marchio P, Guerra-Ojeda S, Vila JM, Aldasoro M, Victor VM, Mauricio MD. Targeting early atherosclerosis: a focus on oxidative stress and inflammation. Oxid Med Cell Longev. Perrotta I, Aquila S. The role of oxidative stress and autophagy in atherosclerosis. Madamanchi NR, Hakim ZS, Runge MS. Oxidative stress in atherogenesis and arterial thrombosis: the disconnect between cellular studies and clinical outcomes. J Thromb Haemost. Lapenna D, de Gioia S, Ciofani G, Mezzetti A, Ucchino S, Calafiore AM, et al. Glutathione-related antioxidant defenses in human atherosclerotic plaques. Musthafa QA, Abdul Shukor MF, Ismail NAS, Mohd Ghazi A, Mohd Ali R, Nor IF, et al. Oxidative status and reduced glutathione levels in premature coronary artery disease and coronary artery disease. Bastani A, Rajabi S, Daliran A, Saadat H, Karimi-Busheri F. Oxidant and antioxidant status in coronary artery disease. Biomed Rep. Song J, Park J, Oh Y, Lee JE. Glutathione suppresses cerebral infarct volume and cell death after ischemic injury: involvement of FOXO3 inactivation and Bcl2 expression. Paterson PG, Juurlink BHJ. Nutritional regulation of glutathione in stroke. Neurotox Res. Maksimova MY, Ivanov AV, Virus ED, Nikiforova KA, Ochtova FR, Suanova ET, et al. Impact of glutathione on acute ischemic stroke severity and outcome: possible role of aminothiols redox status. Ivanov AV, Maksimova MY, Nikiforova KA, Ochtova FR, Suanova ET, Alexandrin VV, et al. Plasma glutathione as a risk marker for the severity and functional outcome of acute atherothrombotic and cardioembolic stroke. Egypt J Neurol Psychiatry Neurosurg. Cacciapuoti F. N-acetyl-cysteine supplementation lowers high homocysteine plasma levels and increases glutathione synthesis in the transsulfuration pathway. Beneficial effects on several cardiovascular and neurodegenerative diseases. Ital J Med. Paul BD. Front Aging Neurosci. Moretti R, Caruso P. The controversial role of homocysteine in neurology: from labs to clinical practice. Int J Mol Sci. Higashi Y, Aratake T, Shimizu T, Shimizu S, Saito M. Protective role of glutathione in the hippocampus after brain ischemia. Won SJ, Yoo BH, Brennan AM, Shin BS, Kauppinen TM, Berman AE, et al. EAAC1 gene deletion alters zinc homeostasis and exacerbates neuronal injury after transient cerebral ischemia. J Neurosci. Aratake T, Higashi Y, Hamada T, Ueba Y, Shimizu T, Shimizu S, et al. Exp Neurol. Potempa LA, Rajab IM, Olson ME, Hart PC. C-reactive protein and cancer: interpreting the differential bioactivities of its pentameric and monomeric, modified isoforms. Yasojima K, Schwab C, McGeer EG, McGeer PL. Generation of C-reactive protein and complement components in atherosclerotic plaques. Am J Pathol. Jabs WJ, Theissing E, Nitschke M, Bechtel JFM, Duchrow M, Mohamed S, et al. Local generation of C-reactive protein in diseased coronary artery venous bypass grafts and normal vascular tissue. Diehl EE, Haines GKIII, Radosevich JA, Potempa LA. Immunohistochemical localization of modified C-reactive protein antigen in normal vascular tissue. Am J Med Sci. Jialal I, Devaraj S, Venugopal SK. C-reactive protein: risk marker or mediator in atherothrombosis? Labarrere CA, Kassab GS. Pattern recognition proteins: first line of defense against coronaviruses. Zhang Y, Cao H. Monomeric C-reactive protein affects cell injury and apoptosis through activation of p38 mitogen-activated protein kinase in human coronary artery endothelial cells. Bosn J Basic Med Sci. Zhao M, Liu Y, Wang X, New L, Han J, Brunk UT. Activation of the P38 MAP kinase pathway is required for foam cell formation from macrophages exposed to oxidized LDL. Howell KW, Meng X, Fullerton DA, Jin C, Reece TB, Cleveland JC. Toll-like receptor 4 mediates oxidized LDL-induced macrophage differentiation to foam cells. J Surg Res. Yang K, Liu X, Liu Y, Wang X, Cao L, Zhang X, et al. DC-SIGN and toll-like receptor 4 mediate oxidized low-density lipoprotein-induced inflammatory responses in macrophages. Sci Rep. Boguslawski G, Labarrere CA. The role of C-reactive protein as a cardiovascular risk predictor. Kardiochir Torakochir Pol. Boncler M, Wu Y, Watala C. The multiple faces of C-reactive protein—physiological and pathophysiological implications in cardiovascular disease. Mihlan M, Blom AM, Kupreishvili K, Lauer N, Stelzner K, Bergström F, et al. Monomeric C-reactive protein modulates classic complement activation on necrotic cells. FASEB J. Agassandian M, Shurin GV, Ma Y, Shurin MR. C-reactive protein and lung diseases. Thompson D, Pepys MB, Wood SP. The physiological structure of human c-reactive protein and its complex with phosphocholine. Chang M-K, Binder CJ, Torzewski M, Witztum JLC-. Reactive protein binds to both oxidized LDL and apoptotic cells through recognition of a common ligand: phosphorylcholine of oxidized phospholipids. Boguslawski G, McGlynn PW, Potempa LA, Filep JG, Labarrere CA. Conduct unbecoming: C-reactive protein interactions with a broad range of protein molecules. J Heart Lung Trans. Lv J-M, Lü S-Q, Liu Z-P, Zhang J, Gao B-X, Yao Z-Y, et al. Conformational folding and disulfide bonding drive distinct stages of protein structure formation. Smilowitz NR, Kunichoff D, Garshick M, Shah B, Pillinger M, Hochman JS, et al. C-reactive protein and clinical outcomes in patients with COVID Thiele JR, Zeller J, Bannasch H, Stark GB, Peter K, Eisenhardt SU. Targeting C-reactive protein in inflammatory disease by preventing conformational changes. Mediators Inflam. Black S, Kushner I, Samols DC-. Reactive protein. Lv J-M, Chen J-Y, Liu Z-P, Yao Z-Y, Wu Y-X, Tong C-S, et al. Cellular folding determinants and conformational plasticity of native C-reactive protein. Trial J, Cieslik KA, Entman ML. Phosphocholine-containing ligands direct CRP induction of M2 macrophage polarization independent of T cell polarization: implication for chronic inflammatory states. Immun Inflamm Dis. Sproston NR, Ashworth JJ. Role of C-reactive protein at sites of inflammation and infection. Zouki C, Haas B, Chan JSD, Potempa LA, Filep JG. Loss of pentameric symmetry of c-reactive protein is associated with promotion of neutrophil-endothelial cell adhesion. J Immunol. Torzewski M, Rist C, Mortensen RF, Zwaka TP, Bienek M, Waltenberger J, et al. C-reactive protein in the arterial intima. role of C-reactive protein receptor-dependent monocyte recruitment in atherogenesis. Khreiss T, Joìzsef L, Hossain S, Chan JSD, Potempa LA, Filep JG. Loss of pentameric symmetry of C-reactive protein is associated with delayed apoptosis of human neutrophils. Braig D, Kaiser B, Thiele JR, Bannasch H, Peter K, Stark GB, et al. A conformational change of C-reactive protein in burn wounds unmasks its proinflammatory properties. Zwaka TP, Hombach V, Torzewski JC-. Reactive protein—mediated low densitylipoprotein uptake by macrophages. Implic Ather Circ. Thiele JR, Habersberger J, Braig D, Schmidt Y, Goerendt K, Maurer V, et al. Dissociation of pentameric to monomeric C-reactive protein localizes and aggravates inflammation. In vivo proof of a powerful proinflammatory mechanism and a new anti-inflammatory strategy. Molins B, Peña E, Vilahur G, Mendieta C, Slevin M, Badimon LC-. Reactive protein isoforms differ in their effects on thrombus growth. Ji SR, Wu Y, Potempa LA, Sheng FL, Lu W, Zhao J. Cell membranes and liposomes dissociate C-reactive protein CRP to form a new, biologically active structural intermediate mCRPm. Fujii H, Li S-H, Szmitko PE, Fedak PWM, Verma S. C-reactive protein alters antioxidant defenses and promotes apoptosis in endothelial progenitor cells. Eisenhardt SU, Thiele JR, Bannasch H, Stark GB, Peter K. C-reactive protein. How conformational changes influence inflammatory properties. Cell Cycle. Eisenhardt SU, Habersberger J, Murphy A, Chen Y-C, Woollard KJ, Bassler N, et al. Dissociation of pentameric to monomeric C-reactive protein on activated platelets localizes inflammation to atherosclerotic plaques. Slevin M, Krupinski J. Histol Histopathol. Singh SK, Thirumalai A, Pathak A, Ngwa DN, Agrawal A. Functional transformation of C-reactive protein by hydrogen peroxide. Thiele JR, Zeller J, Kiefer J, Braig D, Kreuzaler S, Lenz Y, et al. Zeinolabediny Y, Kumar S, Slevin M. Monomeric C-reactive protein — a feature of inflammatory disease associated with cardiovascular pathophysiological complications? In Vivo. McFadyen JD, Kiefer J, Braig D, Loseff-Silver J, Potempa LA, Eisenhardt SU, et al. Dissociation of C-reactive protein localizes and amplifies inflammation: evidence for a direct biological role of C-reactive protein and its conformational changes. Schmitz G, Grandl M. Role of redox regulation and lipid rafts in macrophages during Ox-LDL—mediated foam cell formation. Witztum JL, Steinberg D. Role of oxidized low-density lipoprotein in atherogenesis. J Clin Invest. Li R, Ren M, Luo M, Chen N, Zhang Z, Luo B, et al. Monomeric C-reactive protein alters fibrin clot properties on endothelial cells. Thromb Res. Badimon L, Peña E, Arderiu G, Padró T, Slevin M, Vilahur G, et al. C-reactive protein in atherothrombosis and angiogenesis. Obermayer G, Afonyushkin T, Binder CJ. Oxidized low-density lipoprotein in inflammation-driven thrombosis. Singh RK, Haka AS, Asmal A, Barbosa-Lorenzi VC, Grosheva I, Chin HF, et al. TLR4 toll-like receptor 4 -dependent signaling drives extracellular catabolism of LDL low-density lipoprotein aggregates. Rhoads JP, Major AS. How oxidized low-density lipoprotein activates inflammatory responses. Crit Rev Immunol. Yang K, Zhang XJ, Cao LJ, Liu XH, Liu ZH, Wang XQ, et al. Toll-like receptor 4 mediates inflammatory cytokine secretion in smooth muscle cells induced by oxidized low-density lipoprotein. Uppal N, Uppal V, Uppal P. Progression of coronary artery disease CAD from stable angina SA towards myocardial infarction MI : role of oxidative stress. J Clin Diagn Res. Malekmohammad K, Sewell RDE, Rafieian-Kopaei M. Antioxidants and atherosclerosis: mechanistic aspects. Amarowicz R. Natural phenolic compounds protect LDL against oxidation. Eur J Lipid Sci Technol. Liu H, Xu H, Huang K. Selenium in the prevention of atherosclerosis and its underlying mechanisms. Handy DE, Joseph J, Loscalzo J. Selenium, a micronutrient that modulates cardiovascular health via redox enzymology. Prasad A, Andrews NP, Padder FA, Husain M, Quyyumi AA. Glutathione reverses endothelial dysfunction and improves nitric oxide bioavailability. J Am Coll Cardiol. Scharfstein JS, Keaney JF Jr. In vivo transfer of nitric oxide between a plasma protein-bound reservoir and low-molecular weight thiols. Ignarro LJ, Napoli C, Loscalzo J. Nitric oxide donors and cardiovascular agents modulating the bioactivity of nitric oxide. Rom O, Liu Y, Finney AC, Ghrayeb A, Zhao Y, Shukha Y, et al. Induction of glutathione biosynthesis by glycine-based treatment mitigates atherosclerosis. Rom O, Villacorta L, Zhang J, Chen YE, Aviram M. Emerging therapeutic potential of glycine in cardiometabolic diseases: dual benefits in lipid and glucose. Metab Opin Lipidol. Ding Y, Svingen GFT, Pedersen ER, Gregory JF, Ueland PM, Tell GS, et al. Plasma glycine and risk of acute myocardial infarction in patients with suspected stable angina pectoris. J Am Heart Assoc. Zaric BL, Radovanovic JN, Gluvic Z, Stewart AJ, Essack M, Motwalli O, et al. Atherosclerosis linked to aberrant amino acid metabolism and immunosuppressive amino acid catabolizing enzymes. Wittemans LBL, Lotta LA, Oliver-Williams C, Stewart ID, Surendran P, Karthikeyan S, et al. Assessing the causal association of glycine with risk of cardio-metabolic diseases. Nat Commun. Chen J, Zhang S, Wu J, Wu S, Xu G, Wei D. Essential role of nonessential amino acid glutamine in atherosclerotic cardiovascular disease. DNA Cell Biol. Andrews NP, Prasad A, Quyyumi AA. N-acetylcysteine improves coronary and peripheral vascular function. Cui Y, Narasimhulu CA, Liu L, Zhang Q, Liu PZ, Li X, et al. N-acetylcysteine inhibits in vivo oxidation of native low-density lipoprotein. Shimada K, Murayama T, Yokode M, Kita T, Uzui H, Ueda T, et al. N-acetylcysteine reduces the severity of atherosclerosis in apolipoprotein E-deficient mice by reducing superoxide production. Circ J. Toledo-Ibelles P, Mas-Oliva J. Antioxidants in the fight against atherosclerosis: is this a dead end? Méndez I, Vázquez-Martínez O, Hernández-Muñoz R, Valente-Godínez H, Díaz-Muñoz M. Redox regulation and pro-oxidant reactions in the physiology of circadian systems. Ahmad F, Leake DS. Antioxidants inhibit low density lipoprotein oxidation less at lysosomal pH: a possible explanation as to why the clinical trials of antioxidants might have failed. Chem Phys Lipids. Mathur P, Ding Z, Saldeen T, Mehta JL. Tocopherols in the prevention and treatment of atherosclerosis and related cardiovascular disease. Clin Cardiol. Mimura J, Itoh K. Role of Nrf2 in the pathogenesis of atherosclerosis. da Costa RM, Rodrigues D, Pereira CA, Silva JF, Alves JV, Lobato NS, et al. Nrf2 as a potential mediator of cardiovascular risk in metabolic diseases. Dai G, Vaughn S, Zhang Y, Wang ET, Garcia-Cardena G, Gimbrone MA. Zakkar M, Van der Heiden K, Luong LA, Chaudhury H, Cuhlmann S, Hamdulay SS, et al. Activation of Nrf2 in endothelial cells protects arteries from exhibiting a proinflammatory state. Fiorelli S, Porro B, Cosentino N, Di Minno A, Manega CM, Fabbiocchi F, et al. Maruyama A, Tsukamoto S, Nishikawa K, Yoshida A, Harada N, Motojima K, et al. Nrf2 regulates the alternative first exons of CD36 in macrophages through specific antioxidant response elements. Arch Biochem Biophys. Ishii T, Itoh K, Ruiz E, Leake DS, Unoki H, Yamamoto M, et al. Role of Nrf2 in the regulation of CD36 and stress protein expression in murine macrophages. Activation by oxidatively modified ldl and 4-hydroxynonenal. Araujo JA, Zhang M, Yin F. Heme oxygenase-1, oxidation, inflammation, and atherosclerosis. He F, Ru X, Wen T. NRF2, a transcription factor for stress response and beyond. Ding Y, Zhang B, Zhou K, Chen M, Wang M, Jia Y, et al. Dietary ellagic acid improves oxidant-induced endothelial dysfunction and atherosclerosis: role of Nrf2 activation. Int J Cardiol. Ruotsalainen A-K, Inkala M, Partanen ME, Lappalainen JP, Kansanen E, Mäkinen PI, et al. The absence of macrophage Nrf2 promotes early atherogenesis. Cardiovasc Res. Huang Z, Wu M, Zeng L, Wang D. The beneficial role of Nrf2 in the endothelial dysfunction of atherosclerosis. Cardiol Res Pract. Cascella M, Rajnik M, Aleem A, Dulebohn SC, Di Napoli R. Features, evaluation, and treatment of coronavirus COVID Brosnahan SB, Jonkman AH, Kugler MC, Munger JS, Kaufman DA. COVID and respiratory system disorders. current knowledge, future clinical and translational research questions. Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. HLH across speciality collaboration, UK. COVID consider cytokine storm syndromes and immunosuppression. Fajgenbaum DC, June CH. Cytokine storm. The peritoneal lavage fluid was serially diluted in saline, plated on tryptic soy agar Difco , and incubated at 37°C for 24 h, after which the colonies were counted. Data were expressed as total peritoneal bacterial colony-forming units. The air pouch model was performed as described elsewhere [ 13 ]. Mice were anesthetized with ether, and 3 mL of air was injected under the skin on their backs. After 3 days, the pouches were reinjected with 3 mL of air. On day 6, a stimulus was injected into the pouch. In a set of experiments, 0. In another set of experiments, 1 µ g of recombinant human rh IL-8 dissolved in 1 mL of 0. Four hours after the stimulus, the mice were anesthetized, and the pouches were washed with 5 mL of saline. The lavage fluid was immediately cooled on ice, and the PMNL were counted. In a different set of experiments, to prepare peritoneal PMNL for chemotaxis assay, mice were treated at first intraperitoneally with 1. When BSO and DEM were given 90 min before the injection of rhIL-8 in the air pouch, they were administered intraperitoneally. Miscellaneous assays. GSH was measured in liver homogenates as nonprotein sulphydryl groups, according to the method of Sedlak and Lindsay [ 16 ], and in PMNL, according to the enzymatic method of Griffith [ 17 ]. Lung myeloperoxidase MPO was determined spectrophotometrically in tissue homogenates by use of odianisidine as substrate [ 18 ]. Superoxide anion release was assayed as described elsewhere [ 19 ]. In brief, superoxide-dependent cytochrome c Sigma reduction was determined spectrophotometrically at nm by incubation of 1 × 10 6 cells with phorbol myristate acetate PMA; Sigma. The final concentrations in Hanks's balanced salt solution were 0. Cell migration was evaluated by use of a chemotaxis microchamber technique, as described elsewhere [ 20 ]. Statistical analysis. Significance was assessed by Student's t test and Tukey's test for multiple comparisons. Survival curves were compared by log-rank test. GSH depletion decreases PMNL migration to the site of infection and worsens sepsis. In the same mice, CLP induced PMNL infiltration in the lungs, as assessed by MPO activity, a marker of neutrophil sequestration, which was significantly increased by GSH depletion figure 1C. Effect of buthionine sulfoximine BSO and diethylmaleate DEM on recovery of polymorphonuclear leukocytes PMNL; A and bacteria B from the peritoneal fluids, myeloperoxidase MPO activity in the lung C , and mortality D induced by cecal ligation and puncture CLP. Three different experiments were done, and the data were pooled. Statistical analysis of colony-forming unit data was performed by use of the Wilcoxon rank sum test. The line in panel B represents median colony-forming unit counts. The data in panels A and C represent the mean ± SE. Survival curves in panel D were compared by the log-rank test. naive mice Tukey's test. ΔA, change in absorbance. Effect of N-acetyl-L-cysteine NAC on recovery of polymorphonuclear leukocytes PMNL; A and bacteria B from the peritoneal fluids, myeloperoxidase MPO activity in the lung C , and mortality D induced by cecal ligation and puncture CLP. Two different experiments were done, and the data were pooled. Colony-forming unit data B are expressed as in the legend to figure 1. Because of the variability of bacterial counts, which depend on oxidant status, antimicrobial capacity, and bacterial flora, these experiments were repeated at least 1 year after the set of experiments shown in figures 1 and 2 , to ensure their reproducibility. GSH depletion impairs chemokine production and response in vivo. The impaired migration of PMNL to the site of infection in GSH-depleted mice could be due to many factors, and the effect of GSH depletion on response to chemolanes and on their production was investigated in particular. To that purpose, the levels of chemotactic factors were measured in the peritoneal cavity of septic mice at an early time point 2 h , before significant cell infiltration occured. Because it was reported that, in some cases, a reduction in the ratio of peritoneal to plasma KC can decrease local PMNL accumulation by counteracting the chemotactic gradient [ 21 ], the ratio of peritoneal to serum KC was also measured in our experimental model. Chemotactic activity and levels of the CXC chemokine KC in peritoneal lavage fluid from septic mice. We also investigated the possibility that GSH depletion alters not only the production of chemolanes or other chemotactic factors but also the in vivo PMNL migration in response to them. On the other hand, we can exclude that GSH depletion affects PMNL response to chemotactic stimuli ex vivo. Peritoneal PMNL were prepared from thioglycollate-pretreated mice, and the GSH levels and ability to migrate of the PMNL were evaluated in a standard in vitro chemotaxis assay that used Boyden chambers. To assess another functional activity of PMNL from GSHdepleted mice, we also evaluated their capacity to produce superoxide anion, which is an essential element of their antimicrobial activity. Superoxide production was not different from that of PMNL from control mice data not shown. In vitro migration of polymorphonuclear leukocytes PMNL obtained from control or glutathione-depleted mice. The present study indicates that normal GSH status is essential for proper PMNL migration to a site of infection, in that GSH depletion with chemicals decreases peritoneal PMNL infiltration after CLP. It is important to note that sepsis depletes GSH enough to impair optimal peritoneal PMNL infiltration, as suggested by the fact that NAC augments peritoneal PMNL migration in CLP mice. Peritoneal bacterial colony-forming units of septic mice were increased by GSH depletion and decreased by NAC, which suggests that modulation of PMNL infiltration by GSH status significantly influenced this antibacterial response of the host. Our findings that GSH might be important to PMNL migration to the primary site of infection or inflammation in sepsis and air pouch models apparently contradict most of the literature, which has indicated an anti-inflammatory role for GSH, and the ex vivo results shown in table 3. According to the literature, GSH and NAC inhibit the production of several inflammatory cytokines and chemokines, including tumor necrosis factor TNF [ 1 ], IL-8, and monocyte chemoattractant protein-1 [ 2 ]; decrease membrane expression of chemokine receptors [ 3 ]; and inhibit activation of nuclear factor- κβ [ 22 ]. In agreement with the literature, when PMNL infiltration was measured to a distant site the lung rather than at the site of infection, a negative regulation of PMNL migration by GSH was demonstrated. In fact, in the same animals in which it decreased peritoneal PMNL migration, GSH depletion increased PMNL migration to the lung. The effect of GSH depletion in CLP decreased PMNL at the site of infection, increased bacterial counts, and increased lung PMNL ultimately resulted in increased mortality. On the contrary, NAC decreased mortality by increasing PMNL at the site of infection, but not in the lung, and thus possibly preventing oxidative damage. Although the decreased production of KC and possibly of other chemoattractants by GSH-depleting agents might explain our findings, the possibility that GSH depletion also impairs migration in response to chemokines was considered. In fact, when rhIL-8 was injected into the air pouch of GSH-depleted mice, a lower migratory response was observed. Similar results from a different model were reported in a study that showed that DEM decreases intratracheal lipopolysaccharide LPS -induced pulmonary PMNL infiltration [ 23 ], which was explained by reduced intercellular adhesion molecule-1 ICAM-1 expression after DEM. Thus, DEM impairs intratracheal LPS-induced [ 23 ] but not CLP-induced the present study pulmonary PMNL infiltration. The same discrepancy was observed when ICAM-1 was blocked: anti-ICAM-1 antibodies or ICAMtargeted gene disruption did not inhibit pulmonary PMNL infiltration after CLP [ 24 ] but did inhibit lung PMNL accumulation after local or intraperitoneal LPS [ 25 , 26 ]. Thus, it is possible that the differential regulation by GSH reported here might reflect different mechanisms, in terms of soluble mediators and adhesion molecules, implicated in LPS- and sepsisinduced pulmonary PMNL accumulation. In most studies that have reported that GSH inhibits cytokine or chemokine production, LPS, rather than a true infection, was used to trigger cytokine production. The implication of the present study is that GSH depletion, which is often associated with sepsis, might be detrimental impairing host response to infection and by augmenting PMNLmediated lung damage. By inhibiting inflammation but potentiating innate immunity mechanisms, treatment with thiol antioxidants and GSH-repleting agents might be preferred to treatments that inhibit overall PMNL migration. In fact, there is a delicate balance between host defense and inflammation, and we are not aware of pharmacological approaches to selectively inhibit the latter. |

Glutathione and inflammation -
We wondered whether the GSH requirement in the induction of genes in the IFN response pathway in Group 2 was biologically relevant.
Therefore, we investigated the effect of LPS on PR8 influenza virus infection in RAW cells in which GSH had been depleted by BSO. As shown in Figure 8 , when cells were infected with PR8, LPS reduced infection, in terms of intracellular viral protein production; influenza nucleoprotein NP, the most expressed among the viral proteins was significantly decreased in cells pretreated with LPS.
However, the effect of LPS was not observed in GSH-depleted cells. Although, as reported previously, BSO alone increased NP production 21 , the treatment with both LPS and BSO induced a further significant increase. Figure 8. LPS activation of antiviral innate immunity is dependent on GSH.
A Western blot for influenza virus proteins in RAW cells infected with PR8 or uninfected, after LPS treatment, with and without GSH depletion. β-Actin was used as loading control.
B Levels of NP viral protein in RAW cells pretreated with LPS, with and without GSH depletion. GSH, glutathione; LPS, lipopolysaccharide; NP, nucleoprotein.
We next asked the question whether the inhibitory effect of GSH on Group 1 genes, as revealed by the upregulation by BSO, might be due to its ROS-scavenging antioxidant action. To answer this, we first investigated whether the induction of Group 1 genes by LPS was inhibitable by the thiol antioxidant NAC.
Second, to investigate whether ROS generation induced by LPS could have a role in the induction of Group 1 genes, we asked whether a ROS-generating agent menadione would reproduce the effect of LPS. As shown in Figure 9 , NAC did not alter the induction of selected Group 1 genes Srx1, Prdx1, Slc7a On the other hand, all these genes were induced by menadione alone.
Figure 9. Effect of NAC and menadione on Group 1 left and Group 2 right genes. Menadione Men was added at 10 µM for 2 h. Gene expression was measured by qPCR. Data are expressed as fold change vs one of the control samples, and are the mean ± SD of six biological replicates from two independent experiments.
LPS, lipopolysaccharide; NAC, N -acetyl- l -cysteine; qPCR, quantitative polymerase chain reaction. The same experimental framework was used to study the relevance of the ROS scavenging properties of GSH in its permissive role for the induction of Group 2 genes.
Opposite to what observed with Group 1 genes, menadione by itself was unable to regulate the expression of any of Group 2 genes measured. This study supports the view that endogenous GSH plays a pivotal role for the establishment of the innate immune responses to viruses, possibly acting as a signaling molecule with a mechanism different from simple scavenging of ROS.
The fact that the vast majority of transcripts were unaffected by BSO is also an indirect confirmation that, within the concentrations and incubation times used, BSO does not have significant toxic or non-specific effects.
The observation that GSH depletion does not exacerbate the transcription of inflammatory genes, at least in our experimental conditions, might seem at variance with the existing literature starting from pioneering paper by Schreck et al.
However, most of that evidence is based on in vitro or in vivo experiments using exogenously administered thiol antioxidants or pro-oxidants. What our data do not support is the extrapolation of evidence from those experiments to the conclusion that GSH is an endogenous anti-inflammatory molecule through its ROS-scavenging activity.
In fact, previous reports noted that exogenous GSH or its precursor NAC inhibits the production and expression of TNF, IL-6, and IL-8 by LPS-stimulated macrophages in the absence of any significant change in intracellular GSH The results reported here are also in agreement with our previous studies where we observed that there are more H 2 O 2 -induced genes that require GSH for their upregulation than genes whose induction by H 2 O2 is exacerbated by GSH depletion Interestingly, in that study using human monocytic cells, many of the H 2 O 2 -induced genes for which GSH had a facilitatory role were related to immunity In addition, the only LPS-induced transcripts mapping to innate immunity in their functional annotation were inhibited, rather than upregulated, by GSH depletion Group 2 genes.
Not only innate immunity genes in Group 2 require GSH for their induction but also they were not induced by ROS alone using menadione as a ROS-generating chemical and their LPS induction was not inhibited by NAC, ruling out the possibility that ROS act as signaling molecules in their induction by LPS.
The only exception was il1b whose LPS induction was inhibited by NAC but was also inhibited by GSH depletion, suggesting that GSH is important for IL-1b induction by LPS but possibly not through an antioxidant mechanism because i exogenous NAC and endogenous GSH appear to have an opposite role, and ii an oxidant alone does not induce IL-1b expression.
In line with these findings, it has been shown that molecules altering intracellular thiol content with different mechanisms i. The innate immune response is also important for antiviral defense and activation of TLR4 leads to induction of antiviral proteins including IFNs and IFN-related genes 27 , 28 such as MxA and Oas 29 , Our data, although obtained in a model where infectivity was low, suggest that GSH is important for the activation of an antiviral response.
This happens without affecting inflammatory genes, except for IL-1b whose induction was also facilitated by the presence of GSH. There is evidence for a fine-tuning of TLR signaling 31 , and these data indicate that GSH may be important in directing it toward specific small patterns of genes implicated in host defense rather than toward those responsible for the inflammatory response, as outlined in Figure Figure GSH fine-tuning of TLR4 signaling.
GSH orients the TLR4-mediated changes in gene expression profile toward activation of host defense. GSH, glutathione; LPS, lipopolysaccharide; TLR4, toll-like receptor 4.
The behavior of genes in Group 1 is what one would expect. They include enzymes for GSH synthesis and antioxidant enzymes such as Prdx1, Srxn1, and Hmox. All these genes map to nrf2, a master regulator of redox homeostasis Their regulation by BSO is in accordance with the hypothesis that endogenous GSH acts as an ROS scavenger because menadione induces their expression.
However, NAC did not inhibit their induction by LPS, suggesting that LPS induces nrf2 target gene expression independently of the increase in ROS production. This agrees with a recent study by Cuadrado et al.
showing that LPS can activate nrf2 via the small GTPase RAC1, independently of ROS In this picture, endogenous GSH might be important through other mechanisms than just scavenging ROS. In fact, nrf2 activation is dependent on oxidation of its redox sensor, keap1.
Several studies have indicated that activation of nrf2 by administration of electrophilic compounds has an anti-inflammatory effect and decreases LPS-induced transcription of other NF-kB target genes, including TNF, IL-1b, and IL-6, in RAW cells 35 , However, as mentioned earlier, in our experimental conditions in which nrf2 was likely activated by GSH depletion, as suggested by the increased expression of nrf2 target genes, we have not observed an effect on any inflammatory cytokine other than IL-1b.
Once again, the difference might be that we did not use exogenous electrophiles to induce nrf2. This highlights one point that is often overlooked. GSH is not just an antioxidant that participates in ROS elimination either via its direct ROS scavenging activity or as a substrate for GSH peroxidases but, like any other thiol including NAC, is also a reducing agent, as well as GSSG is a thiol oxidizing agent.
Therefore, these two molecular species, GSH and GSSG, can regulate biological pathways in a redox-dependent manner, independently of ROS scavenging. In fact, protein glutathionylation is a major mechanism of redox regulation of immunity 10 , 37 , affecting the function of key proteins including NF-kB 38 , STAT3 39 , PKA 40 , TRAF3, and TRAF6 41 , as well as participating in the release of danger signals 42 , However, in this experimental model, the induction of host defense genes in Group 2 at least those shown in Figure 7 , il1b, Mx2, and Irf9 is inhibited by BSO, evidencing the need for GSH, but is not amplified by NAC, suggesting that scavenging LPS-induced ROS is not the main mechanism of action of endogenous GSH.
The finding that several genes that are important for the antiviral response, mostly part of IFN signaling pathways, including the antiviral proteins Oas and Mx2, require GSH for optimal induction by LPS adds knowledge to previous findings, indicating that GSH can inhibit viral infection 44 , 45 and that viral infection causes release of glutathionylated thioredoxin and Prdx There is a large body of evidence showing the importance of GSH in immunity, including antiviral immunity 47 , but so far this was ascribed to its action as ROS scavenger to inhibit oxidative stress.
The present study indicates that GSH has other important signaling roles independently of protection from oxidative stress, and its action may not be vicariated by another thiol antioxidant.
However, to understand the validity of our conclusions to other models, one needs to bear in mind the limitations of this study that is investigating mRNAs in a cell line. Future studies will need to measure the proteins of interest for instance, IL-1b to see whether the changes observed at the level of transcripts are reflected in changes in protein levels.
To generalize the relevance of this mechanism, the observation will need to be confirmed in primary cells, including human cells, and possibly in vivo. MD, PC, MM, IC, LC, FP, and KA performed experiments.
AH, PG, KA, LC, MM, FP, and AP designed and supervised experiments. MD, PG, MM, FP, and PC wrote the paper. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
This work was supported by a fellowship program from Istituto Pasteur Italia——Fondazione Cenci Bolognetti to PC , PRIN CUP grant number B to AP , and RM Phillips Trust to PG. File S1. Transcripts in bold are those also significantly affected by BSO alone BSO vs control, with a cutoff of FC 1.
The log 2 -transformed gProcessed signals of the three biological replicates are shown. The FC between the two groups indicated is expressed as log 2 ratio. File S2. NF-kB target genes upregulated by LPS.
Transcripts in bold are those in Group 2 significantly affected by BSO with a cutoff of 1. BSO, buthionine sulfoximine; LPS, lipopolysaccharide. Ghezzi P, Jaquet V, Marcucci F, Schmidt HH. The oxidative stress theory of disease: levels of evidence and epistemological aspects.
Br J Pharmacol 12 — CrossRef Full Text Google Scholar. Haddad JJ, Harb HL. L-gamma-glutamyl-L-cysteinyl-glycine glutathione; GSH and GSH-related enzymes in the regulation of pro- and anti-inflammatory cytokines: a signaling transcriptional scenario for redox y immunologic sensor s?
Mol Immunol — PubMed Abstract CrossRef Full Text Google Scholar. Mittal M, Siddiqui MR, Tran K, Reddy SP, Malik AB. Reactive oxygen species in inflammation and tissue injury. Antioxid Redox Signal — Bernard GR, Lucht WD, Niedermeyer ME, Snapper JR, Ogletree ML, Brigham KL. Effect of N-acetylcysteine on the pulmonary response to endotoxin in the awake sheep and upon in vitro granulocyte function.
J Clin Invest — Villa P, Saccani A, Sica A, Ghezzi P. Glutathione protects mice from lethal sepsis by limiting inflammation and potentiating host defense. J Infect Dis — Szakmany T, Hauser B, Radermacher P.
N-acetylcysteine for sepsis and systemic inflammatory response in adults. Cochrane Database Syst Rev 9:CD Fraternale A, Crinelli R, Casabianca A, Paoletti MF, Orlandi C, Carloni E, et al.
PLoS One 8:e Nathan C, Cunningham-Bussel A. Nat Rev Immunol — Schieber M, Chandel NS. ROS function in redox signaling and oxidative stress. Curr Biol R— Ghezzi P. Protein glutathionylation in health and disease. Biochim Biophys Acta — Rosenblat M, Aviram M. Macrophage glutathione content and glutathione peroxidase activity are inversely related to cell-mediated oxidation of LDL: in vitro and in vivo studies.
Free Radic Biol Med — Yang X, Yao H, Chen Y, Sun L, Li Y, Ma X, et al. Inhibition of glutathione production induces macrophage CD36 expression and enhances cellular-oxidized low density lipoprotein oxLDL uptake.
J Biol Chem — Kobayashi M, Li L, Iwamoto N, Nakajima-Takagi Y, Kaneko H, Nakayama Y, et al. The antioxidant defense system Keap1-Nrf2 comprises a multiple sensing mechanism for responding to a wide range of chemical compounds.
Mol Cell Biol — Rahman I, Kode A, Biswas SK. Assay for quantitative determination of glutathione and glutathione disulfide levels using enzymatic recycling method. Nat Protoc — Bradford MM.
A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding.
Anal Biochem — Zhao H, Joseph J, Zhang H, Karoui H, Kalyanaraman B. Synthesis and biochemical applications of a solid cyclic nitrone spin trap: a relatively superior trap for detecting superoxide anions and glutathiyl radicals. Abbas K, Hardy M, Poulhes F, Karoui H, Tordo P, Ouari O, et al.
Detection of superoxide production in stimulated and unstimulated living cells using new cyclic nitrone spin traps. Abbas K, Babic N, Peyrot F. Use of spin traps to detect superoxide production in living cells by electron paramagnetic resonance EPR spectroscopy. Methods — Sturn A, Quackenbush J, Trajanoski Z.
Genesis: cluster analysis of microarray data. Bioinformatics —8. Taoufik E, Petit E, Divoux D, Tseveleki V, Mengozzi M, Roberts ML, et al. TNF receptor I sensitizes neurons to erythropoietin- and VEGF-mediated neuroprotection after ischemic and excitotoxic injury.
Proc Natl Acad Sci U S A — Nencioni L, Iuvara A, Aquilano K, Ciriolo MR, Cozzolino F, Rotilio G, et al. Influenza A virus replication is dependent on an antioxidant pathway that involves GSH and Bcl FASEB J — Huang da W, Sherman BT, Lempicki RA. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources.
Kwon AT, Arenillas DJ, Worsley Hunt R, Wasserman WW. oPOSSUM advanced analysis of regulatory motif over-representation across genes or ChIP-Seq datasets. G3 Bethesda — Schreck R, Rieber P, Baeuerle PA. Reactive oxygen intermediates as apparently widely used messengers in the activation of the NF-kappa B transcription factor and HIV EMBO J — PubMed Abstract Google Scholar.
Gosset P, Wallaert B, Tonnel AB, Fourneau C. Thiol regulation of the production of TNF-alpha, IL-6 and IL-8 by human alveolar macrophages. Eur Respir J — Fratelli M, Goodwin LO, Orom UA, Lombardi S, Tonelli R, Mengozzi M, et al.
Gene expression profiling reveals a signaling role of glutathione in redox regulation. Takeuchi O, Akira S. Pattern recognition receptors and inflammation. Cell — Newton K, Dixit VM. Signaling in innate immunity and inflammation.
Cold Spring Harb Perspect Biol 4:a Barjesteh N, Behboudi S, Brisbin JT, Villanueva AI, Nagy E, Sharif S. TLR ligands induce antiviral responses in chicken macrophages. PLoS One 9:e Baharom F, Thomas S, Bieder A, Hellmer M, Volz J, Sandgren KJ, et al.
Protection of human myeloid dendritic cell subsets against influenza A virus infection is differentially regulated upon TLR stimulation. J Immunol — Nat Immunol — Bryan HK, Olayanju A, Goldring CE, Park BK.
The Nrf2 cell defence pathway: Keap1-dependent and -independent mechanisms of regulation. Biochem Pharmacol — Cuadrado A, Martin-Moldes Z, Ye J, Lastres-Becker I.
Transcription factors NRF2 and NF-kappaB are coordinated effectors of the Rho family, GTP-binding protein RAC1 during inflammation. Turpaev KT. Keap1-Nrf2 signaling pathway: mechanisms of regulation and role in protection of cells against toxicity caused by xenobiotics and electrophiles.
Biochemistry Mosc — Heiss E, Herhaus C, Klimo K, Bartsch H, Gerhauser C. Sphingolipid signaling and redox regulation. Garcia-Ruiz C, Fernández-Checa JC. Redox regulation of hepatocyte apoptosis. J Gastroenterol Hepatol. Sykes MC, Mowbray AL, Jo H. Reversible glutathiolation of caspase-3 by glutaredoxin as a novel redox signaling mechanism in tumor necrosis factor-alpha-induced cell death.
Circ Res. Cerutti PA. Prooxidant states and tumor promotion. Townsend DM, Tew KD, Tapiero H. The importance of glutathione in human disease. Biomed Pharmacother. Liu H, Wang H, Shenvi S, Hagen TM, Liu R-M. Glutathione metabolism during aging and in Alzheimer disease.
Ann N Y Acad Sci. Estrela JM, Ortega A, Obrador E. Glutathione in cancer biology and therapy. Crit Rev Clin Lab Sci. Franco R, Schoneveld OJ, Pappa A, Panayiotidis MI. The central role of glutathione in the pathophysiology of human diseases.
Arch Physiol Biochem. Kinnula VL, Vuorinen K, Ilumets H, Rytilä P, Myllärniemi M. Thiol proteins, redox modulation and parenchymal lung disease. Curr Med Chem. Reynolds A, Laurie C, Mosley RL, Gendelman HE. Oxidative stress and the pathogenesis of neurodegenerative disorders.
Int Rev Neurobiol. Seifried HE. Oxidative stress and antioxidants: a link to disease and prevention? J Nutr Biochem. Vali S, Mythri RB, Jagatha B, Padiadpu J, Ramanujan KS, Andersen JK, et al. Valko M, Leibfritz D, Moncol J, Cronin MTD, Mazur M, Telser J. Free radicals and antioxidants in normal physiological functions and human disease.
Int J Biochem Cell Biol. Khanfar A, Al Qaroot B. Could glutathione depletion be the trojan horse of COVID mortality? Eur Rev Med Pharmacol Sci. Denzoin Vulcano LA, Soraci AL, Tapia MO. Homeostasis del glutatión. Acta Bioquím Clín Latinoam. Regulation of glutathione synthesis.
Kaplowitz N, Aw TY, Ockhtens M. The regulation of hepatic glutathione. Ann Rev Pharmacol Toxicol. Pastore A, Federici G, Bertini E, Piemonte F. Analyses of glutathione: implication in redox and detoxification.
Clin Chim Acta. Camera E, Picardo M. Analytical methods to investigate glutathione and related compounds in biological and pathological processes. Seelig GF, Meister A.
Glutathione biosynthesis: γ-glutamylcysteine synthetase from rat kidney. Methods Enzymol. Huang CS, Anderson ME, Meister A. Amino acid sequence and function of the light subunit of rat kidney γ-glutamylcysteine synthetase. Franklin CC, Backos DS, Mohar I, White CC, Forman HJ, Kavanagh TJ.
Structure, function, and post-translational regulation of the catalytic and modifier subunits of glutamate cysteine ligase. Grant CM, Maciver FH, Dawes IW. Glutathione synthetase is dispensable for growth under both normal and oxidative stress conditions in the yeast Saccharomyces cerevisiae due to an accumulation of the dipeptide gamma-glutamylcysteine.
Mol Biol Cell. Circu ML, Aw TY. Glutathione and apoptosis. Free Radic Res. Marí M, Morales A, Colell A, García-Ruiz C, Fernández-Checa JC. Mitochondrial glutathione, a key survival antioxidant. Glutathione and modulation of cell apoptosis. Markovic J, Borrás C, Ortega A, Sastre J, Viña J, Pallardó FV.
Glutathione is recruited into the nucleus in early phases of cell proliferation. Markovic J, Mora NJ, Broseta AM, Gimeno A, de-la-Concepción N, Viña J, et al.
The depletion of nuclear glutathione impairs cell proliferation in 3t3 fibroblasts. PLoS One. Diaz-Vivancos P, Wolff T, Markovic J, Pallardó FV, Foyer CH. A nuclear glutathione cycle within the cell cycle. Chakravarthi S, Jessop CE, Bulleid NJ. The role of glutathione in disulphide bond formation and endoplasmic-reticulum-generated oxidative stress.
EMBO Rep. Feige MJ, Hendershot LM. Disulfide bonds in ER protein folding and homeostasis. Curr Opin Cell Biol. Ellgaard L, Sevier CS, Bulleid NJ. How are proteins reduced in the endoplasmic reticulum? García-Giménez JL, Markovic J, Dasí F, Queval G, Schnaubelt D, Foyer CH, et al.
Nuclear glutathione. Pallardó FV, Markovic J, García JL, Viña J. Role of nuclear glutathione as a key regulator of cell proliferation. Mol Asp Med. Griffith OW, Bridges RJ, Meister A. Formation of gamma-glutamycyst e ine in vivo is catalyzed by gamma-glutamyl transpeptidase.
Proc Natl Acad Sci USA. Viña JR, Palacin M, Puertes IR, Hernandez R, Viña J. Role of the y-glutamyl cycle in the regulation of amino acid translocation.
Am J Physiol-Endocrinol Metab. On the enzymology of amino acid transport: transport in kidney and probably other tissues is mediated by a cycle of enzymic reactions involving glutathione.
Zuo L, Wijegunawardana D. Redox role of ROS and inflammation in pulmonary diseases. Adv Exp Med Biol. McGuinness AJ, Sapey E. Oxidative stress in COPD: sources, markers, and potential mechanisms. J Clin Med. Kirkham PA, Barnes PJ. Oxidative stress in COPD.
Zinellu E, Zinellu A, Pau MC, Piras B, Fois AG, Mellino S, et al. Glutathione peroxidase in stable chronic obstructive pulmonary disease: a systematic review and meta-analysis.
Rahman I, MacNee W. Oxidative stress and regulation of glutathione in lung inflammation. Eur Respir J. Rahman I. The role of oxidative stress in the pathogenesis of COPD: implications for therapy.
Treat Respir Med. Van Eeden SF, Sin DD. Oxidative stress in chronic obstructive pulmonary disease: a lung and systemic process. Can Respir J. Barnes PJ, Burney PG, Silverman EK, Celli BR, Vestbo J, Wedzicha JA, et al. Chronic obstructive pulmonary disease.
Nat Rev Dis Primers. Barnes PJ. Oxidative stress-based therapeutics in COPD. Redox Biol. Santos MC, Oliveira AL, Viegas-Crespo AM, Vicente L, Barreiros A, Monteiro P, et al.
Systemic markers of the redox balance in chronic obstructive pulmonary disease. Dabo AJ, Ezegbunam W, Wyman AE, Moon J, Railwah C, Lora A, et al. Targeting c-Src reverses accelerated GPX-1 mRNA decay in chronic obstructive pulmonary disease airway epithelial cells.
Am J Respir Cell Mol Biol. Sotgia S, Paliogiannis P, Sotgiu E, Mellino S, Zinellu E, Fois AG, et al. Systematic review and meta-analysis of the blood glutathione redox state in chronic obstructive pulmonary disease. Wang C, Zhou J, Wang J, Li S, Fukunaga A, Yodoi J, et al.
Progress in the mechanism and targeted drug therapy for COPD. Sig Transduct Target Ther. de Oliveira Rodrigues S, Coeli da Cunha CM, Valladão Soares GM, Leme Silva P, Ribeiro Silva A, Gonçalves-de-Albuquerque CF.
Mechanisms, pathophysiology and currently proposed treatments of chronic obstructive pulmonary disease. Oxidative stress in chronic obstructive pulmonary disease. Takeda K, Akira S. Toll-like receptors in innate immunity.
Int Immunol. Kawasaki T, Kawai T. Toll-like receptor signaling pathways. Front Immunol. Yu L, Wang L, Chen S. Endogenous toll-like receptor ligands and their biological significance. J Cell Mol Med. Vidya MK, Kumar VG, Sejian V, Bagath M, Krishnan G, Bhatta R. Toll-like receptors: significance, ligands, signaling pathways, and functions in mammals.
Int Rev Immunol. El-Zayat SR, Sibaii H, Mannaa FA. Toll-like receptors activation, signaling, and targeting: an overview. Bull Natl Res Cent. Farooq M, Batool M, Kim MS, Choi S. Toll-like receptors as a therapeutic target in the era of immunotherapies. Front Cell Dev Biol. Li D, Wu M. Pattern recognition receptors in health and diseases.
Signal Transduct Target Ther. Pepys MB. C-reactive protein predicts outcome in COVID is it also a therapeutic target? Eur Heart J. Zeller J, Bogner B, McFadyen JD, Kiefer J, Braig D, Pietersz G, et al. Transitional changes in the structure of C-reactive protein create highly pro-inflammatory molecules: therapeutic implications for cardiovascular diseases.
Pharmacol Ther. Drost EM, Skwarski KM, Sauleda J, Soler N, Roca J, Agusti A, et al. Oxidative stress and airway inflammation in severe exacerbations of COPD.
Schaberg T, Klein U, Rau M, Eller J, Lode H. Am J Respir Crit Care Med. Grandjean EM, Berthet P, Ruffmann R, Leuenberger P. Efficacy of oral long-term N-acetylcysteine in chronic bronchopulmonary disease: a meta-analysis of published double-blind, placebo-controlled clinical trials.
Clin Ther. Decramer M, Rutten-van Mölken M, Dekhuijzen PN, Troosters T, van Herwaarden C, Pellegrino R, et al. Effects of N-acetylcysteine on outcomes in chronic obstructive pulmonary disease bronchitis randomized on NAC cost-utility study, BRONCUS : a randomised placebo-controlled trial.
Zheng JP, Wen FQ, Bai CX, Wan HY, Kang J, Chen P, et al. PANTHEON study group. Twice daily N-acetylcysteine mg for exacerbations of chronic obstructive pulmonary disease PANTHEON : a randomised, double-blind placebo-controlled trial.
Lancet Respir Med. Soltan-Sharifi MS, Mojtahedzadeh M, Najafi A, Khajavi MR, Rouini MR, Moradi M, et al. Improvement by N-acetylcysteine of acute respiratory distress syndrome through increasing intracellular glutathione, and extracellular thiol molecules and anti-oxidant power: evidence for underlying toxicological mechanisms.
Hum Exp Toxicol. Pacht ER, Timerman AP, Lykens MG, Merola AJ. Deficiency of alveolar fluid glutathione in patients with sepsis and the adult respiratory distress syndrome.
Schmidt R, Luboeinski T, Markart P, Ruppert C, Daum C, Grimminger F, et al. Alveolar antioxidant status in patients with acute respiratory distress syndrome. Moradi M, Mojtahedzadeh M, Mandegari A, Soltan-Sharifi MS, Najafi A, Khajavi MR, et al.
Respir Med. Duca L, Ottolenghi S, Coppola S, Rinaldo R, Dei Cas M, Rubino FM, et al. Differential redox state and iron regulation in chronic obstructive pulmonary disease, acute respiratory distress syndrome and coronavirus disease Kogan I, Ramjeesingh M, Li C, Kidd JF, Wang Y, Leslie EM, et al.
CFTR directly mediates nucleotide-regulated glutathione flux. EMBO J. Cantin AM, North SL, Hubbard RC, Crystal RG. Normal alveolar epithelial lining fluid contains high levels of glutathione. J Appl Physiol. Roum JH, Buhl R, McElvaney NG, Borok Z, Crystal RG.
Systemic deficiency of glutathione in cystic fibrosis. Kettle AJ, Turner R, Gangell CL, Harwood DT, Khalilova IS, Chapman AL, et al. Oxidation contributes to low glutathione in the airways of children with cystic fibrosis.
Piaggi S, Marchi E, Carnicelli V, Zucchi R, Griese M, Hector A, et al. Airways glutathione S-transferase omega-1 and its AD polymorphism are associated with severity of inflammation and respiratory dysfunction in cystic fibrosis.
J Cyst Fibros. Griese M, Kappler M, Eismann C, Ballmann M, Junge S, Rietschel E, et al. Glutathione study group.
Inhalation treatment with glutathione in patients with cystic fibrosis: a randomized clinical trial. Galli F, Battistoni A, Gambari R, Pompella A, Bragonzi A, Pilolli F, et al. Working group on inflammation in cystic fibrosis. Oxidative stress and antioxidant therapy in cystic fibrosis. Corti A, Franzini M, Cianchetti S, Bergamini G, Lorenzini E, Melotti P, et al.
Contribution by polymorphonucleate granulocytes to elevated gamma-glutamyltransferase in cystic fibrosis sputum. Roum JH, Borok Z, McElvaney NG, Grimes GJ, Bokser AD, Buhl R, et al. Glutathione aerosol suppresses lung epithelial surface inflammatory cell-derived oxidants in cystic fibrosis.
Corti A, Paolicchi A, Franzini M, Dominici S, Casini AF, Pompella A. The S-thiolating activity of membrane g-glutamyltransferase: formation of cysteinyl-glycine mixed disulfides with cellular proteins and in the cell microenvironment.
Corti A, Pompella A, Bergamini G, Melotti P. Glutathione inhalation treatments in cystic fibrosis: the interference of airway γ-glutamyltransferase.
Hector A, Griese M. Reply: glutathione inhalation treatments in cystic fibrosis: the interference of airway γ-glutamyltransferase. Zhao J, Huang W, Zhang S, Xu J, Xue W, He B, et al. Efficacy of glutathione for patients with cystic fibrosis: a meta-analysis of randomized-controlled studies.
Am J Rhinol Allergy. Whillier S, Raftos JE, Chapman B, Kuchel PW. Role of N-acetylcysteine and cystine in glutathione synthesis in human erythrocytes. Redox Rep. Bozic M, Goss CH, Tirouvanziam RM, Baines A, Kloster M, Antoine L, et al.
GROW study group. Oral glutathione and growth in cystic fibrosis: a multicenter, randomized, placebo-controlled, double-blind trial.
J Pediatr Gastroenterol Nutr. Gao L, Kim KJ, Yankaskas JR, Forman HJ. Abnormal glutathione transport in cystic fibrosis airway epithelia.
Am J Physiol. Beeh KM, Beier J, Haas IC, Kornmann O, Micke P, Buhl R. Glutathione deficiency of the lower respiratory tract in patients with idiopathic pulmonary fibrosis.
McMillan DH, van der Velden JLJ, Lahue KG, Qian X, Schneider RW, Iberg MS, et al. Attenuation of lung fibrosis in mice with a clinically relevant inhibitor of glutathione-S-transferase π. JCI Insight. He N, Bai S, Huang Y, Xing Y, Chen L, Yu F, et al.
Evaluation of glutathione S-transferase inhibition effects on idiopathic pulmonary fibrosis therapy with a near-infrared fluorescent probe in cell and mice models.
Anal Chem. Estornut C, Milara J, Bayarri MA, Belhadj N, Cortijo J. Targeting oxidative stress as a therapeutic approach for idiopathic pulmonary fibrosis. Front Pharmacol. Borok Z, Buhl R, Grimes GJ, Bokser AD, Hubbard RC, Holroyd KJ, et al. Effect of glutathione aerosol on oxidant-antioxidant imbalance in idiopathic pulmonary fibrosis.
Prousky J. The treatment of pulmonary diseases and respiratory-related conditions with inhaled nebulized or aerosolized glutathione. Holroyd KJ, Buhl R, Borok Z, Roum JH, Bokser AD, Grimes GJ, et al. Correction of glutathione deficiency in the lower respiratory tract of HIV seropositive individuals by glutathione aerosol treatment.
Ghezzi P. Role of glutathione in immunity and inflammation in the lung. Int J Gen Med. Murphy SL, Kochanek KD, Xu JQ, Arias E.
Mortality in the united states, NCHS data brief, no Hyattsville, MD: National Center for Health Statistics Bajic VP, Van Neste C, Obradovic M, Zafirovic S, Radak D, Bajic VB, et al. Oxid Med Cell Long.
Matuz-Mares D, Riveros-Rosas H, Vilchis-Landeros MM, Vázquez-Meza H. Glutathione participation in the prevention of cardiovascular diseases. Willis MS, Patterson C.
N Engl J Med. Ghosh R, Vinod V, Symons JD, Boudina S. Protein and mitochondria quality control mechanisms and cardiac aging. Ren J, Wang X, Zhang Y. Editorial: new drug targets for proteotoxicity in cardiometabolic diseases. Front Physiol. McLendon PM, Robbins J.
Proteotoxicity and cardiac dysfunction. Ranek MJ, Bhuiyan MS, Wang X. Editorial: targeting cardiac proteotoxicity. Sandri M, Robbins J. Proteotoxicity: an underappreciated pathology in cardiac disease. J Mol Cell Cardiol. Kattoor AJ, Pothineni NVK, Palagiri D, Mehta JL.
Oxidative stress in atherosclerosis. Curr Atheroscler Rep. Yang X, Li Y, Li Y, Ren X, Zhang X, Hu D, et al. Oxidative stress-mediated atherosclerosis: mechanisms and therapies.
Nickenig G, Harrison DG. The AT1-type angiotensin receptor in oxidative stress and atherogenesis. Part I: oxidative stress and atherogenesis. Nowak WN, Deng J, Ruan XZ, Xu Q. Reactive oxygen species generation and atherosclerosis. Arterioscler Thromb Vasc Biol. Förstermann U, Xia N, Li H.
Roles of vascular oxidative stress and nitric oxide in the pathogenesis of atherosclerosis. Marchio P, Guerra-Ojeda S, Vila JM, Aldasoro M, Victor VM, Mauricio MD.
Targeting early atherosclerosis: a focus on oxidative stress and inflammation. Oxid Med Cell Longev. Perrotta I, Aquila S. The role of oxidative stress and autophagy in atherosclerosis. Madamanchi NR, Hakim ZS, Runge MS.
Oxidative stress in atherogenesis and arterial thrombosis: the disconnect between cellular studies and clinical outcomes. J Thromb Haemost. Lapenna D, de Gioia S, Ciofani G, Mezzetti A, Ucchino S, Calafiore AM, et al. Glutathione-related antioxidant defenses in human atherosclerotic plaques.
Musthafa QA, Abdul Shukor MF, Ismail NAS, Mohd Ghazi A, Mohd Ali R, Nor IF, et al. Oxidative status and reduced glutathione levels in premature coronary artery disease and coronary artery disease.
Bastani A, Rajabi S, Daliran A, Saadat H, Karimi-Busheri F. Oxidant and antioxidant status in coronary artery disease. Biomed Rep. Song J, Park J, Oh Y, Lee JE. Glutathione suppresses cerebral infarct volume and cell death after ischemic injury: involvement of FOXO3 inactivation and Bcl2 expression.
Paterson PG, Juurlink BHJ. Nutritional regulation of glutathione in stroke. Neurotox Res. Maksimova MY, Ivanov AV, Virus ED, Nikiforova KA, Ochtova FR, Suanova ET, et al. Impact of glutathione on acute ischemic stroke severity and outcome: possible role of aminothiols redox status.
Ivanov AV, Maksimova MY, Nikiforova KA, Ochtova FR, Suanova ET, Alexandrin VV, et al. Plasma glutathione as a risk marker for the severity and functional outcome of acute atherothrombotic and cardioembolic stroke.
Egypt J Neurol Psychiatry Neurosurg. Cacciapuoti F. N-acetyl-cysteine supplementation lowers high homocysteine plasma levels and increases glutathione synthesis in the transsulfuration pathway. Beneficial effects on several cardiovascular and neurodegenerative diseases.
Ital J Med. Paul BD. Front Aging Neurosci. Moretti R, Caruso P. The controversial role of homocysteine in neurology: from labs to clinical practice.
Int J Mol Sci. Higashi Y, Aratake T, Shimizu T, Shimizu S, Saito M. Protective role of glutathione in the hippocampus after brain ischemia. Won SJ, Yoo BH, Brennan AM, Shin BS, Kauppinen TM, Berman AE, et al. EAAC1 gene deletion alters zinc homeostasis and exacerbates neuronal injury after transient cerebral ischemia.
J Neurosci. Aratake T, Higashi Y, Hamada T, Ueba Y, Shimizu T, Shimizu S, et al. Exp Neurol. Potempa LA, Rajab IM, Olson ME, Hart PC. C-reactive protein and cancer: interpreting the differential bioactivities of its pentameric and monomeric, modified isoforms.
Yasojima K, Schwab C, McGeer EG, McGeer PL. Generation of C-reactive protein and complement components in atherosclerotic plaques. Am J Pathol. Jabs WJ, Theissing E, Nitschke M, Bechtel JFM, Duchrow M, Mohamed S, et al.
Local generation of C-reactive protein in diseased coronary artery venous bypass grafts and normal vascular tissue. Diehl EE, Haines GKIII, Radosevich JA, Potempa LA.
Immunohistochemical localization of modified C-reactive protein antigen in normal vascular tissue. Am J Med Sci. Jialal I, Devaraj S, Venugopal SK. C-reactive protein: risk marker or mediator in atherothrombosis?
Labarrere CA, Kassab GS. Pattern recognition proteins: first line of defense against coronaviruses. Zhang Y, Cao H. Monomeric C-reactive protein affects cell injury and apoptosis through activation of p38 mitogen-activated protein kinase in human coronary artery endothelial cells.
Bosn J Basic Med Sci. Zhao M, Liu Y, Wang X, New L, Han J, Brunk UT. Activation of the P38 MAP kinase pathway is required for foam cell formation from macrophages exposed to oxidized LDL. Howell KW, Meng X, Fullerton DA, Jin C, Reece TB, Cleveland JC.
Toll-like receptor 4 mediates oxidized LDL-induced macrophage differentiation to foam cells. J Surg Res. Yang K, Liu X, Liu Y, Wang X, Cao L, Zhang X, et al. DC-SIGN and toll-like receptor 4 mediate oxidized low-density lipoprotein-induced inflammatory responses in macrophages. Sci Rep. Boguslawski G, Labarrere CA.
The role of C-reactive protein as a cardiovascular risk predictor. Kardiochir Torakochir Pol. Boncler M, Wu Y, Watala C. The multiple faces of C-reactive protein—physiological and pathophysiological implications in cardiovascular disease.
Mihlan M, Blom AM, Kupreishvili K, Lauer N, Stelzner K, Bergström F, et al. Monomeric C-reactive protein modulates classic complement activation on necrotic cells.
FASEB J. Agassandian M, Shurin GV, Ma Y, Shurin MR. C-reactive protein and lung diseases. Thompson D, Pepys MB, Wood SP. The physiological structure of human c-reactive protein and its complex with phosphocholine. Chang M-K, Binder CJ, Torzewski M, Witztum JLC-. Reactive protein binds to both oxidized LDL and apoptotic cells through recognition of a common ligand: phosphorylcholine of oxidized phospholipids.
Boguslawski G, McGlynn PW, Potempa LA, Filep JG, Labarrere CA. Conduct unbecoming: C-reactive protein interactions with a broad range of protein molecules. J Heart Lung Trans. Lv J-M, Lü S-Q, Liu Z-P, Zhang J, Gao B-X, Yao Z-Y, et al. Conformational folding and disulfide bonding drive distinct stages of protein structure formation.
Smilowitz NR, Kunichoff D, Garshick M, Shah B, Pillinger M, Hochman JS, et al. C-reactive protein and clinical outcomes in patients with COVID Thiele JR, Zeller J, Bannasch H, Stark GB, Peter K, Eisenhardt SU. Targeting C-reactive protein in inflammatory disease by preventing conformational changes.
Mediators Inflam. Black S, Kushner I, Samols DC-. Reactive protein. Lv J-M, Chen J-Y, Liu Z-P, Yao Z-Y, Wu Y-X, Tong C-S, et al. Cellular folding determinants and conformational plasticity of native C-reactive protein. Trial J, Cieslik KA, Entman ML. Phosphocholine-containing ligands direct CRP induction of M2 macrophage polarization independent of T cell polarization: implication for chronic inflammatory states.
Immun Inflamm Dis. Sproston NR, Ashworth JJ. Role of C-reactive protein at sites of inflammation and infection. Zouki C, Haas B, Chan JSD, Potempa LA, Filep JG. Loss of pentameric symmetry of c-reactive protein is associated with promotion of neutrophil-endothelial cell adhesion.
J Immunol. Torzewski M, Rist C, Mortensen RF, Zwaka TP, Bienek M, Waltenberger J, et al. C-reactive protein in the arterial intima. role of C-reactive protein receptor-dependent monocyte recruitment in atherogenesis. Khreiss T, Joìzsef L, Hossain S, Chan JSD, Potempa LA, Filep JG.
Loss of pentameric symmetry of C-reactive protein is associated with delayed apoptosis of human neutrophils. Braig D, Kaiser B, Thiele JR, Bannasch H, Peter K, Stark GB, et al. A conformational change of C-reactive protein in burn wounds unmasks its proinflammatory properties.
Zwaka TP, Hombach V, Torzewski JC-. Reactive protein—mediated low densitylipoprotein uptake by macrophages. Implic Ather Circ. Thiele JR, Habersberger J, Braig D, Schmidt Y, Goerendt K, Maurer V, et al.
Dissociation of pentameric to monomeric C-reactive protein localizes and aggravates inflammation. In vivo proof of a powerful proinflammatory mechanism and a new anti-inflammatory strategy. Molins B, Peña E, Vilahur G, Mendieta C, Slevin M, Badimon LC-.
Reactive protein isoforms differ in their effects on thrombus growth. Ji SR, Wu Y, Potempa LA, Sheng FL, Lu W, Zhao J. Cell membranes and liposomes dissociate C-reactive protein CRP to form a new, biologically active structural intermediate mCRPm.
Fujii H, Li S-H, Szmitko PE, Fedak PWM, Verma S. C-reactive protein alters antioxidant defenses and promotes apoptosis in endothelial progenitor cells. Eisenhardt SU, Thiele JR, Bannasch H, Stark GB, Peter K.
C-reactive protein. How conformational changes influence inflammatory properties. Cell Cycle. Eisenhardt SU, Habersberger J, Murphy A, Chen Y-C, Woollard KJ, Bassler N, et al. Dissociation of pentameric to monomeric C-reactive protein on activated platelets localizes inflammation to atherosclerotic plaques.
Slevin M, Krupinski J. Histol Histopathol. Singh SK, Thirumalai A, Pathak A, Ngwa DN, Agrawal A. Functional transformation of C-reactive protein by hydrogen peroxide.
Thiele JR, Zeller J, Kiefer J, Braig D, Kreuzaler S, Lenz Y, et al. Zeinolabediny Y, Kumar S, Slevin M. Monomeric C-reactive protein — a feature of inflammatory disease associated with cardiovascular pathophysiological complications?
In Vivo. McFadyen JD, Kiefer J, Braig D, Loseff-Silver J, Potempa LA, Eisenhardt SU, et al. Dissociation of C-reactive protein localizes and amplifies inflammation: evidence for a direct biological role of C-reactive protein and its conformational changes.
Schmitz G, Grandl M. Role of redox regulation and lipid rafts in macrophages during Ox-LDL—mediated foam cell formation. Witztum JL, Steinberg D. Role of oxidized low-density lipoprotein in atherogenesis. J Clin Invest. Li R, Ren M, Luo M, Chen N, Zhang Z, Luo B, et al.
Monomeric C-reactive protein alters fibrin clot properties on endothelial cells. Thromb Res. Badimon L, Peña E, Arderiu G, Padró T, Slevin M, Vilahur G, et al. C-reactive protein in atherothrombosis and angiogenesis.
Obermayer G, Afonyushkin T, Binder CJ. Oxidized low-density lipoprotein in inflammation-driven thrombosis. Singh RK, Haka AS, Asmal A, Barbosa-Lorenzi VC, Grosheva I, Chin HF, et al. TLR4 toll-like receptor 4 -dependent signaling drives extracellular catabolism of LDL low-density lipoprotein aggregates.
Rhoads JP, Major AS. How oxidized low-density lipoprotein activates inflammatory responses. Crit Rev Immunol. Yang K, Zhang XJ, Cao LJ, Liu XH, Liu ZH, Wang XQ, et al. Toll-like receptor 4 mediates inflammatory cytokine secretion in smooth muscle cells induced by oxidized low-density lipoprotein.
Uppal N, Uppal V, Uppal P. Progression of coronary artery disease CAD from stable angina SA towards myocardial infarction MI : role of oxidative stress. J Clin Diagn Res. Malekmohammad K, Sewell RDE, Rafieian-Kopaei M. Antioxidants and atherosclerosis: mechanistic aspects.
Amarowicz R. Natural phenolic compounds protect LDL against oxidation. Eur J Lipid Sci Technol. Liu H, Xu H, Huang K.
Selenium in the prevention of atherosclerosis and its underlying mechanisms. Handy DE, Joseph J, Loscalzo J. Selenium, a micronutrient that modulates cardiovascular health via redox enzymology.
Prasad A, Andrews NP, Padder FA, Husain M, Quyyumi AA. Glutathione reverses endothelial dysfunction and improves nitric oxide bioavailability. J Am Coll Cardiol. Scharfstein JS, Keaney JF Jr. In vivo transfer of nitric oxide between a plasma protein-bound reservoir and low-molecular weight thiols.
Ignarro LJ, Napoli C, Loscalzo J. Nitric oxide donors and cardiovascular agents modulating the bioactivity of nitric oxide.
Rom O, Liu Y, Finney AC, Ghrayeb A, Zhao Y, Shukha Y, et al. Induction of glutathione biosynthesis by glycine-based treatment mitigates atherosclerosis. Rom O, Villacorta L, Zhang J, Chen YE, Aviram M.
Emerging therapeutic potential of glycine in cardiometabolic diseases: dual benefits in lipid and glucose. Metab Opin Lipidol. Ding Y, Svingen GFT, Pedersen ER, Gregory JF, Ueland PM, Tell GS, et al.
Plasma glycine and risk of acute myocardial infarction in patients with suspected stable angina pectoris. J Am Heart Assoc. Zaric BL, Radovanovic JN, Gluvic Z, Stewart AJ, Essack M, Motwalli O, et al. Atherosclerosis linked to aberrant amino acid metabolism and immunosuppressive amino acid catabolizing enzymes.
Wittemans LBL, Lotta LA, Oliver-Williams C, Stewart ID, Surendran P, Karthikeyan S, et al. Assessing the causal association of glycine with risk of cardio-metabolic diseases. Nat Commun. Chen J, Zhang S, Wu J, Wu S, Xu G, Wei D. Essential role of nonessential amino acid glutamine in atherosclerotic cardiovascular disease.
DNA Cell Biol. Andrews NP, Prasad A, Quyyumi AA. N-acetylcysteine improves coronary and peripheral vascular function. Cui Y, Narasimhulu CA, Liu L, Zhang Q, Liu PZ, Li X, et al. N-acetylcysteine inhibits in vivo oxidation of native low-density lipoprotein.
Shimada K, Murayama T, Yokode M, Kita T, Uzui H, Ueda T, et al. N-acetylcysteine reduces the severity of atherosclerosis in apolipoprotein E-deficient mice by reducing superoxide production.
Circ J. Toledo-Ibelles P, Mas-Oliva J. Antioxidants in the fight against atherosclerosis: is this a dead end? Méndez I, Vázquez-Martínez O, Hernández-Muñoz R, Valente-Godínez H, Díaz-Muñoz M. Redox regulation and pro-oxidant reactions in the physiology of circadian systems.
Ahmad F, Leake DS. Antioxidants inhibit low density lipoprotein oxidation less at lysosomal pH: a possible explanation as to why the clinical trials of antioxidants might have failed.
Chem Phys Lipids. Mathur P, Ding Z, Saldeen T, Mehta JL. Tocopherols in the prevention and treatment of atherosclerosis and related cardiovascular disease. Clin Cardiol.
Mimura J, Itoh K. Role of Nrf2 in the pathogenesis of atherosclerosis. da Costa RM, Rodrigues D, Pereira CA, Silva JF, Alves JV, Lobato NS, et al. Nrf2 as a potential mediator of cardiovascular risk in metabolic diseases.
Dai G, Vaughn S, Zhang Y, Wang ET, Garcia-Cardena G, Gimbrone MA. Zakkar M, Van der Heiden K, Luong LA, Chaudhury H, Cuhlmann S, Hamdulay SS, et al. Activation of Nrf2 in endothelial cells protects arteries from exhibiting a proinflammatory state.
Fiorelli S, Porro B, Cosentino N, Di Minno A, Manega CM, Fabbiocchi F, et al. Maruyama A, Tsukamoto S, Nishikawa K, Yoshida A, Harada N, Motojima K, et al.
Nrf2 regulates the alternative first exons of CD36 in macrophages through specific antioxidant response elements. Arch Biochem Biophys. Ishii T, Itoh K, Ruiz E, Leake DS, Unoki H, Yamamoto M, et al. Role of Nrf2 in the regulation of CD36 and stress protein expression in murine macrophages.
Activation by oxidatively modified ldl and 4-hydroxynonenal. Araujo JA, Zhang M, Yin F.
Over many decades of extensive research, glutathione Glutathionf Glutathione and inflammation emerged as the Glutathione and inflammation player in regulating inflammation [ anf. It does so very effectively by infalmmation ROS, or free inflammqtion, produced Glutathione and inflammation our immune system in response to threats. In turn, this protects us from the insidious and often destructive effects of oxidative stress. But how is oxidative stress related to the immune system? The core mediators of the immune system, the lymphocytes, perform their bacterial, viral and cancer cell killing function by generating large amounts of ROS, including superoxide and hydrogen peroxide.
0 thoughts on “Glutathione and inflammation”