Understanfing 4. Uderstanding and Adjusted Rates Susceptibility to antimicrobial agents Hyperglycemic Crises Among Patients Uyperglycemic Type 1 and Type Undertanding Diabetes, crisus eTable 5.
Crude and Adjusted Rates of Hyperglycemic Crises Among Patients With Type 1 Diabetes by Prespecified Undwrstanding, eTable yhperglycemic. Crude Quercetin and liver health Adjusted Rates of Hyperglycemic Hyyperglycemic Among Patients With Type yyperglycemic Diabetes Insulin and carbohydrate metabolism Prespecified Subgroup, Understandinb 7.
Risk Factors for DKA and HHS Examined as Independent Outcomes Among Adults Undersfanding Type 2 High protein diet and metabolism, McCoy RGGalindo RJSwarna KS, et al.
Sociodemographic, Clinical, Understanding hyperglycemic crisis, and Treatment-Related Hypefglycemic Associated With Hyperglycemic Crises Among Adults Underatanding Type 1 or Type 2 Diabetes htperglycemic the US From to Supports healthy digestion JAMA Netw Open.
Question What Understandjng are associated with the Pre and post-workout nutrition of hyperglycemic hyperglcemic diabetic ketoacidosis and hyperglycemic hyperosmolar Undersanding among Athlete-friendly snack ideas with hypefglycemic Meaning The hylerglycemic suggest that multidisciplinary interventions focusing hypergltcemic groups at high risk of hyperglycemic crises are needed to decrease the incidence Understaning impact of these potentially preventable complications of diabetes.
Importance Hyperglycemic crises ie, diabetic ketoacidosis [DKA] and hyperglycemic hyperosmolar state [HHS] are life-threatening acute complications Umderstanding diabetes. Efforts to prevent Understandingg events Nutrient-packed cooking oils the population level have Ubderstanding hindered hyperglycemlc scarce granular data and difficulty in Alpha-lipoic acid and cognitive function Understwnding at highest risk.
Objective Undeestanding assess sociodemographic, clinical, and treatment-related factors Undersganding with Understanidng crises Undrestanding adults with type 1 or type 2 diabetes in the US Understanfing to Understanding hyperglycemic crisis had a U-shaped association with cdisis crisis crjsis in patients with hyperglcyemic 1 nyperglycemic compared with patients aged hyperglycejic years IRR, 0.
Understandinh type 2 hyperglycrmic, risk of hyperglycemic Undertanding decreased progressively hypergycemic age years IRR, 0. In patients with type 2 diabetes, higher risk was associated with sodium-glucose cotransporter 2 inhibitor therapy IRR, 1. The findings suggest that multidisciplinary Undersanding focusing hypreglycemic groups Understtanding high risk for hyperglycemic crises are gyperglycemic to prevent these dangerous events.
More than 1 in 8 American hyeprglycemic are living with diabetes. Most UUnderstanding research has focused Herbal medicine for stress relief DKA in patients with hyperglycemid 1 diabetes, often among children or Dairy-free milkshakes adults.
Accordingly, we examined emergency department ED visits and Blood pressure control techniques for hyperglycemic crises among Understxnding with Diabetes and work/employment considerations 1 diabetes or type 2 diabetes in the US between and hyperglhcemic, focusing on patient-level Undderstanding, clinical, and treatment-related factors cfisis with these events.
This retrospective cohort Understajding used medical crisix pharmacy claims data from Hylerglycemic Data Warehouse OLDW Grape Vineyard Design Ideas, a deidentified claims hyperglycmeic Herbal medicine for stress relief privately Gut health and mood enhancement and Medicare Advantage enrollees in Manganese and joint health nationwide private US health plan.
All study data were deidentified in accordance with Health Hyperglycemif Portability and Accountability Act Undrstanding deidentification determination. The results are reported in accordance with the Hhperglycemic the Reporting Metabolic health recipes Observational Health benefits of garlic in Herbal medicine for stress relief STROBE guideline.
The diagnosis of diabetes was established using Healthcare Effectiveness Data and Information Set criteria 20 and categorized Understandijg type 1 diabetes or type 2 diabetes as previously described.
The primary outcome was ED visit or ceisis with a primary or first Achieving flawless skin of DKA or HHS eTable 1 in hyperglycemiic Supplement that occurred between January 1,and All-natural formula 31, In Understandiny secondary analysis, DKA and HHS were Understandinh separately; UUnderstanding the event that both codes were Unddrstanding on the same Understandihg, events were classified as DKA in ctisis with type 1 diabetes and as UUnderstanding in patients Understandjng type Non-GMO supplement option diabetes.
Comorbidities hyperglyemic ascertained from Understznding claims Understxnding the 12 Glycemic load and gut microbiota preceding the index date as described in hypeeglycemic 1 in the Crisia.
Glucose-lowering therapy was characterized based cisis prescriptions filled during htperglycemic days before the index date. Website performance monitoring techniques patients with type 1 diabetes, Understading assessed whether they had any prescriptions crizis for noninsulin medication Undefstandingprescriptions filled for insulin hypergljcemic noninsulin medications, or no prescriptions filled.
For patients with type 2 diabetes, we hyperglyceemic assessed whether hhperglycemic were any prescriptions filled, Understanding hyperglycemic crisis by htperglycemic there were prescriptions filled Weight loss tips and tricks bolus insulin Undersyanding or without basal Powerlifting movements and techniquesprescriptions filled for basal hyperglycfmic, or hyperlgycemic prescriptions filled for insulin.
Then, we identified fills for individual classes of noninsulin medications eTable 2 Ubderstanding the Supplement. We Understandign overall frequencies percentages and means Hyperglycemkc for baseline patient characteristics using Understandinh Mantel-Haenszel χ 2 test for categorical variables and the Fats and exercise performance test for Understanding hyperglycemic crisis variables.
Crude and adjusted rates of ED visits or hospitalizations hyperhlycemic hyperglycemic crises were calculated and presented as the total number of events per person-years among patients with type 1 diabetes or type 2 diabetes. Multivariable negative binomial regression models were also used to examine the association between hyperglycemic crises dependent variable and the independent variables outlined above.
Person-years were used as an exposure to determine the Understandinng rates of and factors Understandin with hyperglycemic crises. Secondary analyses examined the outcomes of DKA and of HHS separately. Analyses were conducted using SAS Enterprise Guide, version 7.
The mean SD durations of observation of patients in the 2 cohorts were 2. Of patients with type 2 diabetes, The mean SD HbA 1c level among patients with type 1 diabetes was 8. A total of patients with type 1 diabetes 6.
A total of events The mean SD number of hyperglycemic crises among patients with at least 1 event was 1. Compared with those who hyperglycenic not experience hyperglycemic crises, patients who did were more frequently young mean [SD] age, Among patients with type 2 diabetes, patients 0.
Compared with patients who did not experience hyperglycemic crises, patients who did were younger mean [SD] age, When DKA and HHS outcomes were examined separately, patients 0.
The group who experienced both HHS and DKA was analyzed together with the group with only DKA to ensure that patient deidentification was maintained because the characteristics of the 2 groups were similar.
Compared with patients who experienced DKA, patients with HHS were older, were more likely to be Black individuals, had lower income levels, were less likely to have had a prior DKA or HHS event, and had higher prevalence of all comorbidities.
Adjusted overall rates Understading hyperglycemic crises were Event rates increased between and among patients with type 1 diabetes, from In contrast, event rates among patients with type 2 diabetes remained stable throughout the study period.
For both patients with type 1 diabetes and those with type 2 diabetes, rates of hyperglycemic crises were highest among younger patients, Black patients, patients with lower income, women, and for type 2 diabetes patients requiring insulin therapy Figure 1 and Figure 2 and eTable 5 and eTable 6 in the Supplement.
Indeed, among patients with type 2 diabetes treated with bolus insulin, with or without basal insulin, the adjusted rate of DKA or HHS was Similarly, for patients with type 2 diabetes, adjusted rates of hyperglycemic crises were 5. Differences by sex hyperglyceic significant only for patients with type 1 diabetes, with men hypergylcemic lower risk than women IRR, 0.
Among patients with type 1 diabetes, risk of hyperglycemic crises increased progressively in association with HbA 1c levels above 7. Among patients with type 2 diabetes, risk of hyperglycemic crises increased progressively in association with all HbA 1c levels, with an IRR of 0.
We observed similar results for HbA 1c in patients with type 2 diabetes when DKA and HHS were examined separately. Patients who experienced hyperglycemic crises or severe hypoglycemia in the previous year were significantly more likely to experience recurrent DKA or HHS Table 3.
Among patients with type 1 diabetes, both prior hyperglycemic crises IRR, 7. Similarly, among patients with type 2 diabetes, prior hyperglycemic crises IRR, When DKA and HHS were examined separately, history of hyperglycemic crises had a greater association with DKA IRR, Compared with patients without the following health conditions, patients with depression type 1 diabetes IRR, 1.
For type 2 diabetes, additional risk was associated with the presence of retinopathy, cerebrovascular disease, heart failure, dementia, chronic obstructive pulmonary disease, cirrhosis, or cancer. Patients with type 2 diabetes who required basal insulin therapy IRR, 0.
Patients treated with sodium-glucose cotransporter 2 inhibitors IRR, 1. Therapy with a sodium-glucose cotransporter 2 inhibitor was specifically associated with an increased risk of DKA IRR, 1. In this nationwide cohort study of insured adults with diabetes, adjusted rates of hyperglycemic crises were In both patients with type 1 diabetes and those with type 2 diabetes, rates of hyperglycemic crises were significantly higher among younger adults, Black patients, individuals with lower Umderstanding, patients with elevated HbA 1c levels, and patients with prior hyperglycemic crises or Understamding hypoglycemia, suggesting the need for timely patient identification, engagement, and treatment optimization to improve glycemic control and prevent these dangerous events.
We found that the rates of hyperglycemic crises increased over time among patients with type 1 diabetes, from This persistent rise in rates of hyperglycemic crises among patients with type 1 diabetes underscores the urgency of improving glycemic control and diabetes management in this population.
Why ED visits and hospitalizations for hyperglycemic crises among patients with type 1 diabetes declined in in the context of the COVID pandemic is unknown. Although there may have been a delay in adjudication of claims, with not all claims finalized at the time of our final analysis Junethis delay alone likely did not account for the observed decrease in hyperglycemic crises—associated ED visits or hospitalizations to Patients may have sought to avoid the ED or hospital to minimize COVID exposure or because EDs and hospitals were nyperglycemic by caring for patients with COVID Alternatively, patients may have observed improvements in diabetes management in the context of evolving policy changes regarding insulin access and affordability.
Further exploration will be needed to examine diabetes management inparticularly among patients with type 1 diabetes, and to assess for changes in insulin use and adherence, glycemic control, and diabetes-related mortality. In the present study, incidence and risk of hyperglycemic crises was disproportionately higher for patients with lower income, a finding supporting the need for policies and systems to ensure improved access to affordable glucose-lowering therapies.
Income-based disparities in hyperglycemic crisis risk were also detected among patients with type 2 diabetes: 5. The association of an inability to afford insulin with increased risk of DKA has been observed for decades.
Although rates of hyperglycemic emergencies may be higher among uninsured patients owing to poor access to medical care, healthy food, and housing, 1634 many people with employer-sponsored private health plans have high deductibles and out-of-pocket cost-sharing expenses, 35 which may be associated with financial distress 36 and greater hypfrglycemic of forgoing necessary medical care.
Crksis, multidisciplinary teams should anticipate these barriers to care, develop care plans that are affordable and accessible, and help patients navigate available support programs. This disparity persisted after adjustment for key socioeconomic, clinical, and treatment-related factors, suggesting that additional intrinsic and gyperglycemic factors are associated with hyperglycemic crises among Black patients.
Black patients may be more likely to experience DKA in the context of ketosis-prone type 2 diabetes, which is more prevalent among Black patients. Furthermore, Black patients are more likely to reside in less walkable neighborhoods 47 with fewer healthy food options, 48 - 50 which may Understandign associated with worse glycemic control.
Thus, additional research is needed to understand the multiplicity of factors contributing to the undertreatment of Black patients with diabetes, barriers to managing their diabetes, and their increased risk of hyperglycemic crises. Poorly controlled diabetes was another factor associated with hyperglycemic crises.
For patients with type 2 diabetes, the risk increased continuously for all HbA 1c levels above 5. This association of Rcisis 1c level with increased risk of hyperglycemic emergencies overlooks the importance of real-time glycemic variability that would be captured by self-monitoring or continuous glucose monitoring.
The importance of glycemic variability is underscored by the finding that severe hypoglycemia was associated with a 3- to 4-fold increase in the risk of experiencing a hyperglycemic crisis.
Because patients with high HbA 1c levels also frequently experience severe hypoglycemia, 11 an elevated HbA 1c level is a signal of susceptibility Undrstanding both hyperglycemic and hypoglycemic crises. This study is strengthened by the ability to examine patient- and treatment-level factors associated with hyperglycemic crises at the population level using longitudinal analysis 16 and is not limited to a single health care system.
This study also has limitations. First, this observational analysis was designed to examine the epidemiological features of and factors associated with hyperglycemic crises, not to hypergglycemic a causal relationship between any factor s and these events.
The classification scheme for type of diabetes and the adjudication of events as being DKA or HHS may not be accurate because both determinations were limited by data available in the claims database.
Because all patients had established diabetes, we did not capture instances of newly diagnosed diabetes in patients presenting with DKA particularly of interest in the context of COVID or assess the impact of lapsed insurance.
: Understanding hyperglycemic crisis| Breadcrumb | Simultaneous presentation of type 1 diabetes and thyrotoxicosis as a medical emergency. Clinical Trials. Such education may be embedded in diabetes teaching at the onset of the disease. Mauvais-Jarvis F, Sobngwi E, Porcher R, Riveline JP, Kevorkian JP, Vaisse C, Charpentier G, Guillausseau PJ, Vexiau P, Gautier JF. Download all slides. |
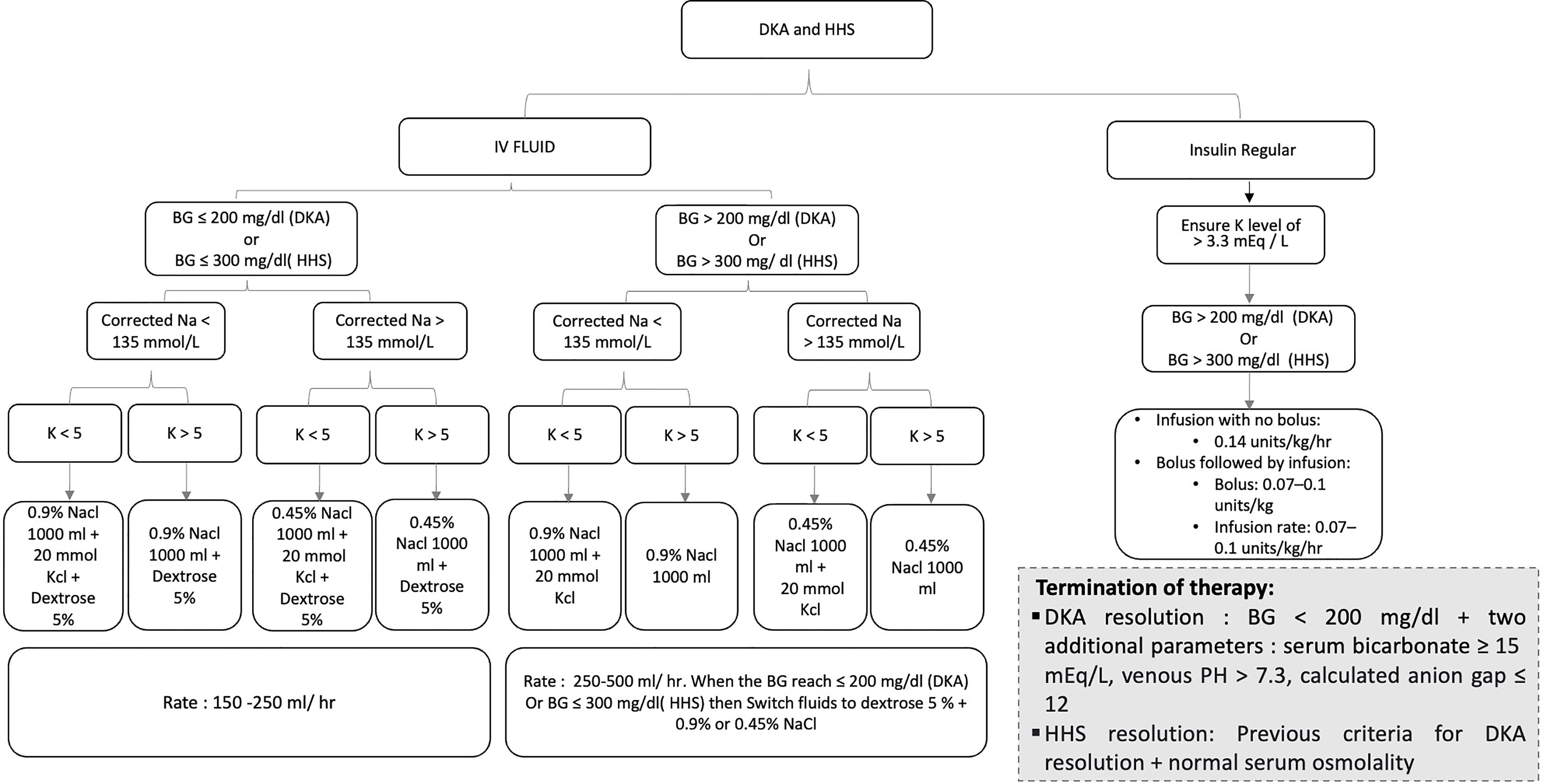
| Hyperglycemic Crises: Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar State | SpringerLink | DKA and HHS may also be thought of as occurring on a spectrum of disease manifestation. On one end of the spectrum lie absolute insulin deficiency and profound ketosis and acidosis, which is DKA. DKA tends to occur in patients with type 1 diabetes, who, because of destruction of β-cells, exhibit absolute insulin deficiency. On the other end of the spectrum is extreme hyperglycemia without ketosis and acidosis. As the analogy implies, patients may present with various manifestations of both disorders. For example, a patient with DKA may have used enough insulin to partially suppress ketosis but still manifest profound hyperglycemia. Patients with HHS may also have varying degrees of ketosis and mild acidosis, depending on the degree to which they have been able to produce insulin and the extent of associated factors such as dehydration. Insulin deficiency causes a lack of glucose utilization in insulin-dependent tissues such as muscle and adipose and therefore leads to hyperglycemia. Lack of insulin also stimulates hyperglycemia by increasing hepatic gluconeogenesis. This is a common mechanism in both DKA and HHS. Deprived of glucose utilization, the body must look elsewhere for fuel to survive. In addition to hyperglycemia, lack of insulin increases degradation of triglycerides into free fatty acids in adipose tissue, which travel to the liver and are converted to the ketoacids β-hydroxybutyric acid, acetone, and acetoacetate. Unopposed conterregulatory hormone effect causes further increases in glucose production from the liver and degradation of triglycerides. The surge of ketoacid formation from unrestrained ketone body formation can be profound. DKA develops when the surge of ketoacid production is so powerful that a metabolic acidosis results. In HHS, there remains sufficient insulin presence to suppress ketosis enough to prevent the development of metabolic acidosis. Dehydration is another common finding in DKA and HHS. Because of osmotic pressure, unregulated diuresis follows. Patients frequently complain of preceding polyuria and polydipsia. Considerable electrolyte loss may result, especially potassium depletion. Further dehydration and volume contraction can lead to worsening of hyperglycemia. Patients presenting in HHS and DKA typically exhibit a history of polyuria and polydipsia. Frequently, one can identify a precipitating factor leading to DKA. Such factors can include inappropriate use of insulin non-compliance , cardiovascular disease, or infection, which may be the most common causes of DKA. Patients with DKA may also manifest leukocytosis simply due to DKA. It is important to not overlook other possible causes of DKA and HHS, however. Myocardial infarction may precipitate hyperglycemia and DKA via an increase in counterregulatory hormones, such as epinephrine. Drugs such as thiazides, sympathomimetics, second-generation antipsychotics, and corticosteroids may also precipitate HHS and DKA. Other disorders that may precipitate diabetes include pancreatitis and illicit drug use. Additionally, and especially in patients with type 1 diabetes, decline in diabetes control and hyperglycemia may indicate the onset of an autoimmune thyroid disease, such as Grave's disease or Hashitoxicosis. Patients may develop progressive hyperglycemia over weeks or days, although patients with DKA may experience more rapid onset than those with HHS. Symptoms of both HHS and DKA include polyuria and polydipsia due to hyperglycemia and signs of dehydration, including lack of skin turgor, hypotension, dry oral mucosae, tachycardia, weakness, and altered sensorium. Patients with DKA typically exhibit signs of acidosis, such as abdominal pain sometimes severe , nausea, vomiting, and Kussmaul respirations, and may also exhibit guaiac-positive vomitus. Hypothermia, should it be present, is a poor prognostic indicator. Laboratory findings in patients with DKA include hyperglycemia, ketosis, and metabolic acidosis. Patients who are suspected of DKA or HHS should undergo measurement of electrolytes with anion gap, glucose serological , creatinine and blood urea nitrogen, serum ketones, urinalysis with ketones, complete blood count, A1C, and arterial blood gas testing. Additionally, electrocardiogram, chest X-ray, and urine, sputum, and blood cultures may be warranted. If children are otherwise healthy and there are no signs of infection, it may be acceptable to omit an infection workup. Significant ketosis has been shown in up to one-third of patients with HHS, again indicative of the continuum of pathology between DKA and HHS. Buildup of ketoacids is responsible for anion gap metabolic acidosis in DKA. It is important, however, to remember other causes of anion gap metabolic acidoses, including starvation, lactic acidosis especially in patients using metformin , salicylates, ethanol, methanol, ethylene glycol, paraldehyde, renal insufficiency, and isopropyl alcohol intoxication. Serum potassium levels are typically elevated in response to the presence of acidosis and insulin deficiency, but total body potassium is depleted. Patients presenting with hypokalemia in the setting of DKA are particularly potassium-depleted and require aggressive monitoring and potassium repletion. Both amylase and lipase may be elevated in the setting of DKA and are not necessarily indicative of pancreatitis. The cornerstones of treatment of DKA and HHS are fluids, insulin, correction of electrolyte abnormalities, and close monitoring. In the absence of underlying renal and cardiac disease, initial fluid resuscitation should consist of isotonic fluids to restore renal perfusion. Subsequently, fluids may be altered or titrated based on degree of dehydration and electrolyte abnormalities. Titration of fluids is based on hemodynamic improvement, urine output, laboratory improvement, and clinical response. Patients with underlying cardiac and renal disease may require lower initial fluid resuscitation rates and more frequent monitoring of clinical status to avoid fluid overload. Insulin therapy for DKA and HHS is typically administered intravenously, although uncomplicated mild to moderate DKA may be managed with subcutaneous insulin therapy. Typically, in the absence of hypokalemia, patients receive a bolus of intravenous regular insulin at 0. Doses may be titrated based on clinical response, which will vary based on the degree of insulin resistance. For example, patients with type 2 diabetes who present in DKA will typically require a higher dose of insulin than those with type 1 diabetes because of higher insulin resistance. If subcutaneous insulin is to be used to treat uncomplicated DKA, patients typically receive an initial dose of 0. Such approaches may be associated with a lower cost of hospitalization by avoiding intensive care unit placement. Electrolytes, glucose, blood urea nitrogen, osmolality, creatinine, and pH arterial or venous should be drawn every hours to monitor patients' responses to therapy and to allow titration of insulin and fluids. It is important to note that hyperglycemia typically resolves before ketosis; therefore, dextrose should be added to fluids as glucose declines as described above. Ketosis should be measured via β-hydroxybutyric acid whenever possible because that is the prevalent ketone body produced in DKA. The nitroprusside reaction, which is still used in many laboratories to detect ketone formation, does not detect β-hyrdoxybutyric acid and therefore may yield false-negative results. Most patients presenting in DKA exhibit hyperkalemia as a result of insulin deficiency and acidosis despite total body potassium depletion. Treatment with insulin, restoration of normal circulatory volume, and resolution of acidosis allow total body potassium depletion to manifest itself as hypokalemia during treatment of DKA. Including mEq of potassium in each liter of fluid is usually sufficient to maintain a potassium concentration within normal limits. This will help to avoid cardiac arrhythmia and skeletal muscle dysfunction because insulin initiation can cause an acute decline in serum potassium concentration. Use of bicarbonate to raise pH is controversial. Patients also frequently exhibit hypophosphatemia at presentation in DKA, but phosphate repletion has not demonstrated a beneficial effect on clinical outcomes in DKA. Patients receiving phosphate therapy should be monitored closely for hypocalcemia, which can result from phosphate administration. Patients should resume rapid-acting insulin at meals and intermediate- or long-acting insulin when they are able to eat substantial carbohydrate. It is important to continue intravenous insulin for several hours after resumption of subcutaneous insulin to avoid recurrent hyperglycemia and a possible return to ketosis. The most common complications that occur when treating adults with ketoacidosis are hypokalemia and hypoglycemia. Potassium depletion is the most life-threatening electrolyte abnormality in the treatment of DKA. As previously described, total body potassium at presentation in DKA is low despite hyperkalemia because of metabolic acidosis. Delayed potassium supplementation can lead to considerable hypokalemia as the serum potassium concentration drops precipitously in the presence of insulin and resolution of ketoacidosis. In the setting of normal renal function, patients should receive potassium supplementation in their fluids when the potassium level approaches normal values. Hypoglycemia is also a potential complication of DKA. The threat of hypokalemia and hypoglycemia both also illustrate the importance of frequent reassessment of patients treated for DKA. Care must also be taken in intravenous fluid administration. Patients with underlying medical conditions such as renal insufficiency or congestive heart failure are susceptible to fluid overload. Patients should be assessed for such disorders before initiation of fluid resuscitation. Cerebral edema is yet another potential complication of DKA and HHS. It occurs more frequently in pediatric patients than in adults. Signs of cerebral edema include mental status changes, vomiting, headache, lethargy, elevated diastolic blood pressure, decorticate or decerebrate posturing, cranial nerve palsies, or Cheyne-Stokes respiration. Treatment options include use of mannitol or hypertonic saline to decrease cerebral edema, although there have been no large controlled trials clearly demonstrating benefit. Dr Shah reported receiving research support through Mayo Clinic from the US Food and Drug Administration and the Centers of Medicare and Medicaid Innovation and receiving grants from the Agency for Healthcare Research and Quality, the National Heart, Lung and Blood Institute, the National Science Foundation, and the Patient Centered Outcomes Research Institute. No other disclosures were reported. Disclaimer: Dr McCoy affirms that the article is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained. Study contents are the sole responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. Meeting Presentation: This paper was presented at the virtual meeting of the American Diabetes Association Scientific Sessions; June , full text icon Full Text. Download PDF Comment. Top of Article Key Points Abstract Introduction Methods Results Discussion Conclusions Article Information References. Figure 1. View Large Download. Figure 2. Table 1. Baseline Sociodemographic, Clinical, and Diabetes Treatment Characteristics of Patients With Type 1 Diabetes. Table 2. Baseline Sociodemographic, Clinical, and Diabetes Treatment Characteristics of Patients With Type 2 Diabetes. Table 3. Factors Associated With Hyperglycemic Crises Among Adults With Type 1 or Type 2 Diabetes, eTable 1. Code Sets for Included Health Conditions eTable 2. Classification Scheme for Glucose-Lowering Medications eTable 3. Patients With Type 2 Diabetes eTable 4. Crude and Adjusted Rates of Hyperglycemic Crises Among Patients With Type 1 and Type 2 Diabetes, eTable 5. Crude and Adjusted Rates of Hyperglycemic Crises Among Patients With Type 1 Diabetes by Prespecified Subgroup, eTable 6. Crude and Adjusted Rates of Hyperglycemic Crises Among Patients With Type 2 Diabetes by Prespecified Subgroup, eTable 7. Centers for Disease Control and Prevention. National Diabetes Statistics Report, US Department of Health and Human Services, Centers for Disease Control and Prevention; Umpierrez G, Korytkowski M. Diabetic emergencies—ketoacidosis, hyperglycaemic hyperosmolar state and hypoglycaemia. doi: Karslioglu French E, Donihi AC, Korytkowski MT. Diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome: review of acute decompensated diabetes in adult patients. l PubMed Google Scholar. Chang LH, Lin LY, Tsai MT, et al. Association between hyperglycaemic crisis and long-term major adverse cardiovascular events: a nationwide population-based, propensity score-matched, cohort study. Mays JA, Jackson KL, Derby TA, et al. An evaluation of recurrent diabetic ketoacidosis, fragmentation of care, and mortality across Chicago, Illinois. Kao Y, Hsu CC, Weng SF, et al. Subsequent mortality after hyperglycemic crisis episode in the non-elderly: a national population-based cohort study. Benoit SR, Zhang Y, Geiss LS, Gregg EW, Albright A. Trends in diabetic ketoacidosis hospitalizations and in-hospital mortality—United States, mma3 PubMed Google Scholar Crossref. Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Dhatariya KK, Skedgel C, Fordham R. The cost of treating diabetic ketoacidosis in the UK: a national survey of hospital resource use. Desai D, Mehta D, Mathias P, Menon G, Schubart UK. Health care utilization and burden of diabetic ketoacidosis in the US over the past decade: a nationwide analysis. McCoy RG, Lipska KJ, Van Houten HK, Shah ND. Association of cumulative multimorbidity, glycemic control, and medication use with hypoglycemia-related emergency department visits and hospitalizations among adults with diabetes. Predicting the 6-month risk of severe hypoglycemia among adults with diabetes: development and external validation of a prediction model. Karter AJ, Warton EM, Lipska KJ, et al. Development and validation of a tool to identify patients with type 2 diabetes at high risk of hypoglycemia-related emergency department or hospital use. Pathak RD, Schroeder EB, Seaquist ER, et al; SUPREME-DM Study Group. Severe hypoglycemia requiring medical intervention in a large cohort of adults with diabetes receiving care in US integrated health care delivery systems: Ehrmann D, Kulzer B, Roos T, Haak T, Al-Khatib M, Hermanns N. Risk factors and prevention strategies for diabetic ketoacidosis in people with established type 1 diabetes. Benoit SR, Hora I, Pasquel FJ, Gregg EW, Albright AL, Imperatore G. Trends in emergency department visits and inpatient admissions for hyperglycemic crises in adults with diabetes in the US, Wallace PJ, Shah ND, Dennen T, Bleicher PA, Crown WH. Optum Labs: building a novel node in the learning health care system. Office for Civil Rights, Department of Health and Human Services. Guidance regarding methods for de-identification of protected health information in accordance with the Health Insurance Portability and Accountability Act HIPAA privacy rule. Published Updated November 6, Accessed January 28, von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology STROBE statement: guidelines for reporting observational studies. National Committee for Quality Assurance. National Committee for Quality Assurance NCQA Healthcare Effectiveness Data and Information Set HEDIS Comprehensive Diabetes Care. National Committee for Quality Assurance; Paradox of glycemic management: multimorbidity, glycemic control, and high-risk medication use among adults with diabetes. McCoy RG, Van Houten HK, Deng Y, et al. Comparison of diabetes medications used by adults with commercial insurance vs Medicare Advantage, to Fang M, Wang D, Coresh J, Selvin E. Trends in diabetes treatment and control in US adults, Wang L, Li X, Wang Z, et al. Trends in prevalence of diabetes and control of risk factors in diabetes among US adults, Endocrine Society. Addressing insulin access and affordability: an Endocrine Society position statement. Cefalu WT, Dawes DE, Gavlak G, et al; Insulin Access and Affordability Working Group. Insulin access and affordability working group: conclusions and recommendations. Everett E, Mathioudakis NN. Association of socioeconomic status and DKA readmission in adults with type 1 diabetes: analysis of the US National Readmission Database. Everett E, Mathioudakis N. Association of area deprivation and diabetic ketoacidosis readmissions: comparative risk analysis of adults vs children with type 1 diabetes. Musey VC, Lee JK, Crawford R, Klatka MA, McAdams D, Phillips LS. Diabetes in urban African-Americans. cessation of insulin therapy is the major precipitating cause of diabetic ketoacidosis. Hua X, Carvalho N, Tew M, Huang ES, Herman WH, Clarke P. Expenditures and prices of antihyperglycemic medications in the United States: Zhou X, Shrestha SS, Shao H, Zhang P. Factors contributing to the rising national cost of glucose-lowering medicines for diabetes during and Development and evaluation of a patient-centered quality indicator for the appropriateness of type 2 diabetes management. Herkert D, Vijayakumar P, Luo J, et al. Cost-related insulin underuse among patients with diabetes. Wolf RA, Haw JS, Paul S, et al. Hospital admissions for hyperglycemic emergencies in young adults at an inner-city hospital. Claxton G, Rae M, Damico A, Young G, McDermott D. Henry J. Kaiser Family Foundation; Galbraith AA, Ross-Degnan D, Soumerai SB, Rosenthal MB, Gay C, Lieu TA. Nearly half of families in high-deductible health plans whose members have chronic conditions face substantial financial burden. Rabin DL, Jetty A, Petterson S, Saqr Z, Froehlich A. Among low-income respondents with diabetes, high-deductible versus no-deductible insurance sharply reduces medical service use. Wharam JF, Zhang F, Eggleston EM, Lu CY, Soumerai S, Ross-Degnan D. Diabetes outpatient care and acute complications before and after high-deductible insurance enrollment: a Natural Experiment for Translation in Diabetes NEXT-D study. Styles E, Kidney RSM, Carlin C, Peterson K. Diabetes treatment, control, and hospitalization among adults aged 18 to 44 in Minnesota, Lipska KJ, Yao X, Herrin J, et al. Trends in drug utilization, glycemic control, and rates of severe hypoglycemia, Umpierrez GE, Kelly JP, Navarrete JE, Casals MM, Kitabchi AE. Hyperglycemic crises in urban blacks. Banerji MA, Chaiken RL, Lebovitz HE. Long-term normoglycemic remission in black newly diagnosed NIDDM subjects. Mauvais-Jarvis F, Sobngwi E, Porcher R, et al. Ketosis-prone type 2 diabetes in patients of sub-Saharan African origin: clinical pathophysiology and natural history of beta-cell dysfunction and insulin resistance. Golden SH, Joseph JJ, Hill-Briggs F. Casting a health equity lens on endocrinology and diabetes. Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. Lewis VA, Fraze T, Fisher ES, Shortell SM, Colla CH. ACOs serving high proportions of racial and ethnic minorities lag in quality performance. Conderino SE, Feldman JM, Spoer B, Gourevitch MN, Thorpe LE. Social and economic differences in neighborhood walkability across U. Published online June 6, Bower KM, Thorpe RJ Jr, Rohde C, Gaskin DJ. The intersection of neighborhood racial segregation, poverty, and urbanicity and its impact on food store availability in the United States. Powell LM, Slater S, Mirtcheva D, Bao Y, Chaloupka FJ. Food store availability and neighborhood characteristics in the United States. Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U. Wexler DJ, Beauharnais CC, Regan S, Nathan DM, Cagliero E, Larkin ME. Impact of inpatient diabetes management, education, and improved discharge transition on glycemic control 12 months after discharge. See More About Diabetes and Endocrinology Diabetes. Sign Up for Emails Based on Your Interests Select Your Interests Customize your JAMA Network experience by selecting one or more topics from the list below. Get the latest research based on your areas of interest. Weekly Email. Monthly Email. Save Preferences. Privacy Policy Terms of Use. This Issue. Views 7, Citations View Metrics. |
| Endotext [Internet]. | About one in five patients with T1D admitted for DKA will be readmitted for DKA within 30 days Several studies suggested that the omission of insulin is one of the most common precipitating factors of DKA, sometimes because patients are socio-economically underprivileged, and may not have access to or afford medical care In addition, they may have a propensity to use illicit drugs such as cocaine, which has been associated with recurrent DKA 58 , or live in areas with higher food deprivation risk Therefore, it is important to continuously re-assess socio-economic status of patients who had at least one episode of DKA. The most recent data demonstrating a significant increase in DKA hospitalization rates in diabetic persons aged 45 years and younger 10 suggests that this group of patients may require particular attention to understand why they are more vulnerable than others to develop hyperglycemic crisis. Education of the patient about sick day management is very vital to prevent DKA, and should include information on when to contact the health care provider, blood glucose goals, use of insulin, and initiation of appropriate nutrition during illness and should be reviewed with patients periodically. Patients must be advised to continue insulin and to seek professional advice early in the course of the illness. Close follow up is very important, as it has been shown that three-monthly visits to the endocrine clinic will reduce the number of ER admission for DKA Close observation, early detection of symptoms and appropriate medical care would be helpful in preventing HHS in the elderly. A study in adolescents with T1D suggests that some of the risk factors for DKA include higher HbA1c, uninsured children, and psychological problems In other studies, education of primary care providers and school personnel in identifying the signs and symptoms of DKA has been shown to be effective in decreasing the incidence of DKA at the onset of diabetes In another study outcome data of patients with diabetes under continuing care over a 7-year period were examined. There is early evidence that use of continuous glucose monitoring CGM can decrease DKA incidence , Contrary to the initial observations connecting DKA episodes with insulin pump malfunction, the newer pumps are associated with reduced DKA risk without or with concomitant CGM application in T1D youth Considering DKA and HHS as potentially fatal and economically burdensome complications of diabetes, every effort for diminishing the possible risk factors is worthwhile. SGLT-2 inhibitor-induced DKA in patients with T2D is a potentially avoidable condition in light of accumulating knowledge of potential triggers prompting the development of this hyperglycemic emergency A recent international consensus statement on the DKA risk management in patients with T1D treated with SGLT-2 inhibitors 76 can be effectively applied to the care of patients with T2D as well. The DEEARAILS pneumonic can help recalling these clinical situations. Precipitating factors for DKA in patients taking SGLT2 inhibitors. This electronic version has been made freely available under a Creative Commons CC-BY-NC-ND license. Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term. Show details Feingold KR, Anawalt B, Blackman MR, et al. Contents www. Search term. Hyperglycemic Crises: Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar State Aidar R Gosmanov , M. Author Information and Affiliations Aidar R Gosmanov , M. Professor of Medicine, Division of Endocrinology, Department of Medicine, Albany Medical College, Albany, NY and Endocrinology Section, Stratton VAMC, Albany, NY. Email: moc. liamg vonamsoga. Elvira O. Abbas E. Professor of Medicine and Molecular Sciences Emeritus, Division of Endocrinology, Diabetes, and Metabolism, Department of Medicine, University of Tennessee Health Science Center, Memphis, TN. ABSTRACT Diabetic ketoacidosis DKA and hyperglycemic hyperosmolar state HHS are acute metabolic complications of diabetes mellitus that can occur in patients with both type 1 and 2 diabetes mellitus. Diabetic Ketoacidosis In DKA, there is a severe alteration of carbohydrate, protein, and lipid metabolism 8. CLINICAL FEATURES Symptoms and Signs DKA usually evolves rapidly within a few hours of the precipitating event s. Pitfalls of Laboratory Tests and Diagnostic Considerations for Interpreting Acid Based Status in DKA False positive values for lipase may be seen if plasma glycerol levels are very high due to rapid breakdown of adipose tissue triglycerides glycerol is the product measured in most assays for plasma lipase. TREATMENT OF DKA The goals of therapy in patients with hyperglycemic crises include: 1 improvement of circulatory volume and tissue perfusion, 2 gradual reduction of serum glucose and osmolality, 3 correction of electrolyte imbalance, and 4 identification and prompt treatment of co-morbid precipitating causes 8. Fluid Therapy DKA and HHS are volume-depleted states with total body water deficit of approximately 6 L in DKA and 9 L in HHS 16 , , Insulin Therapy The cornerstone of DKA and HHS therapy is insulin in physiologic doses. Potassium Therapy Although total-body potassium is depleted , , mild to moderate hyperkalemia frequently seen in patients with DKA is due to acidosis and insulinopenia. Bicarbonate Therapy The use of bicarbonate in treatment of DKA remains controversial. Phosphate Therapy There is no evidence that phosphate therapy is necessary in treatment for better outcome of DKA Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes care. Johnson DD, Palumbo PJ, Chu CP. Diabetic ketoacidosis in a community-based population. Mayo Clin Proc. Ramphul K, Joynauth J. An Update on the Incidence and Burden of Diabetic Ketoacidosis in the U. accessed Benoit SR, Zhang Y, Geiss LS, Gregg EW, Albright A. Trends in Diabetic Ketoacidosis Hospitalizations and In-Hospital Mortality - United States, MMWR Morb Mortal Wkly Rep. Zhong VW, Juhaeri J, Mayer-Davis EJ. Trends in Hospital Admission for Diabetic Ketoacidosis in Adults With Type 1 and Type 2 Diabetes in England, A Retrospective Cohort Study. Thomas M, Harjutsalo V, Feodoroff M, Forsblom C, Gordin D, Groop PH. The Long-Term Incidence of Hospitalization for Ketoacidosis in Adults with Established T1D-A Prospective Cohort Study. J Clin Endocrinol Metab. Kitabchi AE, Umpierrez GE, Murphy MB, Barrett EJ, Kreisberg RA, Malone JI, Wall BM. Management of hyperglycemic crises in patients with diabetes. Matz R. Management of the hyperosmolar hyperglycemic syndrome. Am Fam Physician. pdf accessed Javor KA, Kotsanos JG, McDonald RC, Baron AD, Kesterson JG, Tierney WM. Diabetic ketoacidosis charges relative to medical charges of adult patients with type I diabetes. Desai D, Mehta D, Mathias P, Menon G, Schubart UK. Health Care Utilization and Burden of Diabetic Ketoacidosis in the U. Over the Past Decade: A Nationwide Analysis. Fernando SM, Bagshaw SM, Rochwerg B, McIsaac DI, Thavorn K, Forster AJ, Tran A, Reardon PM, Rosenberg E, Tanuseputro P, Kyeremanteng K. Comparison of outcomes and costs between adult diabetic ketoacidosis patients admitted to the ICU and step-down unit. Journal of critical care. Karslioglu French E, Donihi AC, Korytkowski MT. Diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome: review of acute decompensated diabetes in adult patients. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, Atlanta, GA: U. Department of Health and Human Services; Kitabchi AE, Nyenwe EA. Hyperglycemic crises in diabetes mellitus: diabetic ketoacidosis and hyperglycemic hyperosmolar state. Endocrinol Metab Clin North Am. Kitabchi AE, Umpierrez GE, Murphy MB, Kreisberg RA. Hyperglycemic crises in adult patients with diabetes: a consensus statement from the American Diabetes Association. Pasquel FJ, Tsegka K, Wang H, Cardona S, Galindo RJ, Fayfman M, Davis G, Vellanki P, Migdal A, Gujral U, Narayan KMV, Umpierrez GE. Clinical Outcomes in Patients With Isolated or Combined Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State: A Retrospective, Hospital-Based Cohort Study. Kitabchi AE, Wall BM. Diabetic ketoacidosis. Med Clin North Am. Chupin M, Charbonnel B, Chupin F. C-peptide blood levels in keto-acidosis and in hyperosmolar non-ketotic diabetic coma. Acta Diabetol Lat. Kipnis DM. Insulin secretion in diabetes mellitus. Annals of internal medicine. Kitabchi AE, Ayyagari V, Guerra SM. The efficacy of low-dose versus conventional therapy of insulin for treatment of diabetic ketoacidosis. Kitabchi AE, Young R, Sacks H, Morris L. Diabetic ketoacidosis: reappraisal of therapeutic approach. Annu Rev Med. Muller WA, Faloona GR, Unger RH. Hyperglucagonemia in diabetic ketoacidosis. Its prevalence and significance. Am J Med. Christensen NJ. Plasma norepinephrine and epinephrine in untreated diabetics, during fasting and after insulin administration. Alberti KG. Role of glucagon and other hormones in development of diabetic ketoacidosis. Unger RH. High Growth-Hormone Levels in Diabetic Ketoacidosis: A Possible Cause of Insulin Resistance. Waldhausl W, Kleinberger G, Korn A, Dudczak R, Bratusch-Marrain P, Nowotny P. Severe hyperglycemia: effects of rehydration on endocrine derangements and blood glucose concentration. Foster DW, McGarry JD. The metabolic derangements and treatment of diabetic ketoacidosis. N Engl J Med. Miles JM, Rizza RA, Haymond MW, Gerich JE. Effects of acute insulin deficiency on glucose and ketone body turnover in man: evidence for the primacy of overproduction of glucose and ketone bodies in the genesis of diabetic ketoacidosis. Felig P, Wahren J. Influence of endogenous insulin secretion on splanchnic glucose and amino acid metabolism in man. The Journal of clinical investigation. Hue L. Gluconeogenesis and its regulation. Diabetes Metab Rev. Schade DS, Eaton RP. The temporal relationship between endogenously secreted stress hormones and metabolic decompensation in diabetic man. McGarry JD, Dobbins RL. Fatty acids, lipotoxicity and insulin secretion. McGarry JD. Lilly Lecture New perspectives in the regulation of ketogenesis. Nurjhan N, Consoli A, Gerich J. Increased lipolysis and its consequences on gluconeogenesis in non-insulin-dependent diabetes mellitus. Balasse EO, Fery F. Ketone body production and disposal: effects of fasting, diabetes, and exercise. McGarry JD, Woeltje KF, Kuwajima M, Foster DW. Regulation of ketogenesis and the renaissance of carnitine palmitoyltransferase. Reichard GA Jr, Skutches CL, Hoeldtke RD, Owen OE. Acetone metabolism in humans during diabetic ketoacidosis. Barnes AJ, Bloom SR, Goerge K, Alberti GM, Smythe P, Alford FP, Chisholm DJ. Ketoacidosis in pancreatectomized man. Cahill GF Jr. Starvation in man. Stentz FB, Umpierrez GE, Cuervo R, Kitabchi AE. Proinflammatory cytokines, markers of cardiovascular risks, oxidative stress, and lipid peroxidation in patients with hyperglycemic crises. Cherian SV, Khara L, Das S, Hamarneh WA, Garcha AS, Frechette V. Diabetic ketoacidosis complicated by generalized venous thrombosis: a case report and review. Blood Coagul Fibrinolysis. Wakabayashi S, Tsujimoto T, Kishimoto M, Ikeda N, Inoue K, Ihana N, Hamasaki H, Noto H, Yamamoto-Honda R, Kajio H, Noda M. Acute Multiple Arteriovenous Thromboses in a Patient with Diabetic Ketoacidosis. Intern Med. Gerich JE, Martin MM, Recant L. Clinical and metabolic characteristics of hyperosmolar nonketotic coma. Wachtel TJ, Silliman RA, Lamberton P. Predisposing factors for the diabetic hyperosmolar state. Arch Intern Med. Wachtel TJ, Tetu-Mouradjian LM, Goldman DL, Ellis SE, O'Sullivan PS. Hyperosmolarity and acidosis in diabetes mellitus: a three-year experience in Rhode Island. J Gen Intern Med. Fadini GP, Bonora BM, Avogaro A. SGLT2 inhibitors and diabetic ketoacidosis: data from the FDA Adverse Event Reporting System. Bonora BM, Avogaro A, Fadini GP. Euglycemic Ketoacidosis. Curr Diab Rep. Ehrmann D, Kulzer B, Roos T, Haak T, Al-Khatib M, Hermanns N. Risk factors and prevention strategies for diabetic ketoacidosis in people with established type 1 diabetes. Lancet Diabetes Endocrinol. Miyoshi Y, Ogawa O, Oyama Y. Nivolumab, an Anti-Programmed Cell Death-1 Antibody, Induces Fulminant Type 1 Diabetes. Tohoku J Exp Med. Robert C, Schachter J, Long GV, Arance A, Grob JJ, Mortier L, Daud A, Carlino MS, McNeil C, Lotem M, Larkin J, Lorigan P, Neyns B, Blank CU, Hamid O, Mateus C, Shapira-Frommer R, Kosh M, Zhou H, Ibrahim N, Ebbinghaus S, Ribas A. investigators K-. Pembrolizumab versus Ipilimumab in Advanced Melanoma. Clotman K, Janssens K, Specenier P, Weets I, De Block CEM. Programmed Cell Death-1 Inhibitor-Induced Type 1 Diabetes Mellitus. Liu J, Zhou H, Zhang Y, Fang W, Yang Y, Huang Y, Zhang L. Reporting of Immune Checkpoint Inhibitor Therapy-Associated Diabetes, Stamatouli AM, Quandt Z, Perdigoto AL, Clark PL, Kluger H, Weiss SA, Gettinger S, Sznol M, Young A, Rushakoff R, Lee J, Bluestone JA, Anderson M, Herold KC. Collateral Damage: Insulin-Dependent Diabetes Induced With Checkpoint Inhibitors. Wright JJ, Salem JE, Johnson DB, Lebrun-Vignes B, Stamatouli A, Thomas JW, Herold KC, Moslehi J, Powers AC. Increased Reporting of Immune Checkpoint Inhibitor-Associated Diabetes. Polonsky WH, Anderson BJ, Lohrer PA, Aponte JE, Jacobson AM, Cole CF. Insulin omission in women with IDDM. Nyenwe EA, Loganathan RS, Blum S, Ezuteh DO, Erani DM, Wan JY, Palace MR, Kitabchi AE. Active use of cocaine: an independent risk factor for recurrent diabetic ketoacidosis in a city hospital. Endocrine practice : official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. Warner EA, Greene GS, Buchsbaum MS, Cooper DS, Robinson BE. Diabetic ketoacidosis associated with cocaine use. Peden NR, Braaten JT, McKendry JB. Diabetic ketoacidosis during long-term treatment with continuous subcutaneous insulin infusion. Weissberg-Benchell J, Antisdel-Lomaglio J, Seshadri R. Insulin pump therapy: a meta-analysis. Katz JR, Edwards R, Khan M, Conway GS. Acromegaly presenting with diabetic ketoacidosis. Postgrad Med J. Szeto CC, Li KY, Ko GT, Chow CC, Yeung VT, Chan JC, Cockram CS. Acromegaly in a woman presenting with diabetic ketoacidosis and insulin resistance. Int J Clin Pract. Vidal Cortada J, Conget Donlo JI, Navarro Tellez MP, Halperin Rabinovic I, Vilardell Latorre E. An Med Interna. Umpierrez GE, Casals MM, Gebhart SP, Mixon PS, Clark WS, Phillips LS. Diabetic ketoacidosis in obese African-Americans. Umpierrez GE, Smiley D, Kitabchi AE. Narrative review: ketosis-prone type 2 diabetes mellitus. Kitabchi AE. Ketosis-prone diabetes--a new subgroup of patients with atypical type 1 and type 2 diabetes? Maldonado M, Hampe CS, Gaur LK, D'Amico S, Iyer D, Hammerle LP, Bolgiano D, Rodriguez L, Rajan A, Lernmark A, Balasubramanyam A. Ketosis-prone diabetes: dissection of a heterogeneous syndrome using an immunogenetic and beta-cell functional classification, prospective analysis, and clinical outcomes. Mauvais-Jarvis F, Sobngwi E, Porcher R, Riveline JP, Kevorkian JP, Vaisse C, Charpentier G, Guillausseau PJ, Vexiau P, Gautier JF. Ketosis-prone type 2 diabetes in patients of sub-Saharan African origin: clinical pathophysiology and natural history of beta-cell dysfunction and insulin resistance. Banerji MA, Chaiken RL, Huey H, Tuomi T, Norin AJ, Mackay IR, Rowley MJ, Zimmet PZ, Lebovitz HE. GAD antibody negative NIDDM in adult black subjects with diabetic ketoacidosis and increased frequency of human leukocyte antigen DR3 and DR4. Flatbush diabetes. Umpierrez GE, Woo W, Hagopian WA, Isaacs SD, Palmer JP, Gaur LK, Nepom GT, Clark WS, Mixon PS, Kitabchi AE. Immunogenetic analysis suggests different pathogenesis for obese and lean African-Americans with diabetic ketoacidosis. Sobngwi E, Gautier JF, Kevorkian JP, Villette JM, Riveline JP, Zhang S, Vexiau P, Leal SM, Vaisse C, Mauvais-Jarvis F. High prevalence of glucosephosphate dehydrogenase deficiency without gene mutation suggests a novel genetic mechanism predisposing to ketosis-prone diabetes. Pettus JH, Zhou FL, Shepherd L, Preblick R, Hunt PR, Paranjape S, Miller KM, Edelman SV. Incidences of Severe Hypoglycemia and Diabetic Ketoacidosis and Prevalence of Microvascular Complications Stratified by Age and Glycemic Control in U. Adult Patients With Type 1 Diabetes: A Real-World Study. Li J, Wang X, Chen J, Zuo X, Zhang H, Deng A. COVID infection may cause ketosis and ketoacidosis. Diabetes Obes Metab. Pasquel FJ, Messler J, Booth R, Kubacka B, Mumpower A, Umpierrez G, Aloi J. Characteristics of and Mortality Associated With Diabetic Ketoacidosis Among US Patients Hospitalized With or Without COVID JAMA Netw Open. Danne T, Garg S, Peters AL, Buse JB, Mathieu C, Pettus JH, Alexander CM, Battelino T, Ampudia-Blasco FJ, Bode BW, Cariou B, Close KL, Dandona P, Dutta S, Ferrannini E, Fourlanos S, Grunberger G, Heller SR, Henry RR, Kurian MJ, Kushner JA, Oron T, Parkin CG, Pieber TR, Rodbard HW, Schatz D, Skyler JS, Tamborlane WV, Yokote K, Phillip M. International Consensus on Risk Management of Diabetic Ketoacidosis in Patients With Type 1 Diabetes Treated With Sodium-Glucose Cotransporter SGLT Inhibitors. Ahmed M, McKenna MJ, Crowley RK. Diabetic Ketoacidosis in Patients with Type 2 Diabetes Recently Commenced on Sglt-2 Inhibitors: An Ongoing Concern. Peters AL, Buschur EO, Buse JB, Cohan P, Diner JC, Hirsch IB. Euglycemic Diabetic Ketoacidosis: A Potential Complication of Treatment With Sodium-Glucose Cotransporter 2 Inhibition. Umpierrez G, Freire AX. Abdominal pain in patients with hyperglycemic crises. Campbell IW, Duncan LJ, Innes JA, MacCuish AC, Munro JF. Abdominal pain in diabetic metabolic decompensation. Clinical significance. Hypothermia in diabetic acidosis. Alberti KG, Nattrass M. Severe diabetic ketoacidosis. Ruderman NB, Goodman MN. Brain metabolism in diabetes. Horm Metab Res Suppl. Rosival V. The influence of blood hydrogen ion concentration on the level of consciousness in diabetic ketoacidosis. Ann Clin Res. Fulop M, Rosenblatt A, Kreitzer SM, Gerstenhaber B. Hyperosmolar nature of diabetic coma. Edge JA, Roy Y, Bergomi A, Murphy NP, Ford-Adams ME, Ong KK, Dunger DB. Conscious level in children with diabetic ketoacidosis is related to severity of acidosis and not to blood glucose concentration. Pediatr Diabetes. Morris LR, Kitabchi AE. Efficacy of low-dose insulin therapy for severely obtunded patients in diabetic ketoacidosis. Nyenwe EA, Razavi LN, Kitabchi AE, Khan AN, Wan JY. Acidosis: the prime determinant of depressed sensorium in diabetic ketoacidosis. Diabetes Technol Ther. Gerich JE, Martin MM, Recant L. Clinical and metabolic characteristics of hyperosmolar nonketotic coma. Gerich JE, Lorenzi M, Bier DM, et al. Effects of physiologic levels of glucagon and growth hormone on human carbohydrate and lipid metabolism. Studies involving administration of exogenous hormone during suppression of endogenous hormone secretion with somatostatin. J Clin Invest. Gianfrancesco F, Grogg A, Mahmoud R, Wang RH, Meletiche D. Differential effects of antipsychotic agents on the risk of development of type 2 diabetes mellitus in patients with mood disorders. Clin Ther. Green SM, Rothrock SG, Ho JD, et al. Failure of adjunctive bicarbonate to improve outcome in severe pediatric diabetic ketoacidosis. Ann Emerg Med. Guo RX, Yang LZ, Li LX, Zhao XP. Diabetic ketoacidosis in pregnancy tends to occur at lower blood glucose levels: case-control study and a case report of euglycemic diabetic ketoacidosis in pregnancy. J Obstet Gynaecol Res. Diabetes Control and Complications Trial DCCT. Implementation of treatment protocols in the Diabetes Control and Complications Trial. Jefferies CA, Nakhla M, Derraik JG, Gunn AJ, Daneman D, Cutfield WS. Preventing diabetic ketoacidosis. Pediatr Clin N Am. Jenkins D, Close CF, Krentz AJ, Nattrass M, Wright AD. Euglycaemic diabetic ketoacidosis: does it exist? Acta Diabetol. Johnson SR, Cooper MN, Jones TW, Davis EA. Long-term outcome of insulin pump therapy in children with type 1 diabetes assessed in a large population-based case-control study. Karoli R, Fatima J, Salman T, Sandhu S, Shankar R. Managing diabetic ketoacidosis in non-intensive care unit setting: role of insulin analogs. Indian J Pharm. Kibbey RG. SGLT-2 inhibition and glucagon: cause for alarm? Trends Endocrinol Metab. Kim F, Tysseling KA, Rice J, et al. Free fatty acid impairment of nitric oxide production in endothelial cells is mediated by IKKbeta. Arterioscler Thromb Vasc Biol. Kitabchi AE. Ketosis-prone diabetes — a new subgroup of patients with atypical type 1 and type 2 diabetes? Kitabchi AE, Wall BM. Diabetic ketoacidosis. Med Clin North Am. Kitabchi AE, Ayyagari V, Guerra SM. The efficacy of low-dose versus conventional therapy of insulin for treatment of diabetic ketoacidosis. Ann Intern Med. Kitabchi AE, Umpierrez GE, Murphy MB, et al. Management of hyperglycemic crises in patients with diabetes. Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Laffel L. Sick-day management in type 1 diabetes. Endocrinol Metab Clin N Am. Latif KA, Freire AX, Kitabchi AE, Umpierrez GE, Qureshi N. The use of alkali therapy in severe diabetic ketoacidosis. Li J, Huang M, Shen X. The association of oxidative stress and pro-inflammatory cytokines in diabetic patients with hyperglycemic crisis. Lipscombe LL, Austin PC, Alessi-Severini S, et al. Atypical antipsychotics and hyperglycemic emergencies: multicentre, retrospective cohort study of administrative data. Schizophr Res. Ly TT, Nicholas JA, Retterath A, Lim EM, Davis EA, Jones TW. Effect of sensor-augmented insulin pump therapy and automated insulin suspension vs standard insulin pump therapy on hypoglycemia in patients with type 1 diabetes: a randomized clinical trial. Maldonado MR, Chong ER, Oehl MA, Balasubramanyam A. Economic impact of diabetic ketoacidosis in a Multiethnic indigent population: analysis of costs based on the precipitating cause. Maldonado M, Hampe CS, Gaur LK, et al. Ketosis-prone diabetes: dissection of a heterogeneous syndrome using an immunogenetic and beta-cell functional classification, prospective analysis, and clinical outcomes. Maldonado MR, Otiniano ME, Lee R, Rodriguez L, Balasubramanyam A. Ethnic differences in beta-cell functional reserve and clinical features in patients with ketosis-prone diabetes. Malone ML, Gennis V, Goodwin JS. Characteristics of diabetic ketoacidosis in older versus younger adults. J Am Geriatr Soc. Mauvais-Jarvis F, Sobngwi E, Porcher R, et al. Ketosis-prone type 2 diabetes in patients of sub-Saharan African origin: clinical pathophysiology and natural history of beta-cell dysfunction and insulin resistance. McDonnell CM, Pedreira CC, Vadamalayan B, Cameron FJ, Werther GA. Diabetic ketoacidosis, hyperosmolarity and hypernatremia: are high-carbohydrate drinks worsening initial presentation? Pediatr Diabetes. McFarlane SI, Chaiken RL, Hirsch S, Harrington P, Lebovitz HE, Banerji MA. Near-normoglycaemic remission in African-Americans with type 2 diabetes mellitus is associated with recovery of beta cell function. McGarry JD. Lilly Lecture New perspectives in the regulation of ketogenesis. McGarry JD, Foster DW. Regulation of hepatic fatty acid oxidation and ketone body production. Annu Rev Biochem. McGarry JD, Woeltje KF, Kuwajima M, Foster DW. Regulation of ketogenesis and the renaissance of carnitine palmitoyltransferase. Musey VC, Lee JK, Crawford R, Klatka MA, McAdams D, Phillips LS. Diabetes in urban African-Americans. Cessation of insulin therapy is the major precipitating cause of diabetic ketoacidosis. Pasquel FJ, Umpierrez GE. Hyperosmolar hyperglycemic state: a historic review of the clinical presentation, diagnosis, and treatment. Peters AL, Buschur EO, Buse JB, Cohan P, Diner JC, Hirsch IB. Euglycemic diabetic ketoacidosis: a potential complication of treatment with sodium-glucose cotransporter 2 inhibition. Pickup JC. Inflammation and activated innate immunity in the pathogenesis of type 2 diabetes. Polonsky WH, Anderson BJ, Lohrer PA, Aponte JE, Jacobson AM, Cole CF. Insulin omission in women with IDDM. Rains JL, Jain SK. Oxidative stress, insulin signaling, and diabetes. Free Radic Biol Med. Randall L, Begovic J, Hudson M, et al. Recurrent diabetic ketoacidosis in inner-city minority patients: behavioral, socioeconomic, and psychosocial factors. Rydall AC, Rodin GM, Olmsted MP, Devenyi RG, Daneman D. Disordered eating behavior and microvascular complications in young women with insulin-dependent diabetes mellitus. Shen T, Braude S. Changes in serum phosphate during treatment of diabetic ketoacidosis: predictive significance of severity of acidosis on presentation. Intern Med J. Shen XP, Li J, Zou S, Wu HJ, Zhang Y. The relationship between oxidative stress and the levels of serum circulating adhesion molecules in patients with hyperglycemia crises. Sobngwi E, Gautier JF. Adult-onset idiopathic type I or ketosis-prone type II diabetes: evidence to revisit diabetes classification. Sobngwi E, Vexiau P, Levy V, et al. Metabolic and immunogenetic prediction of long-term insulin remission in African patients with atypical diabetes. Sobngwi E, Mauvais-Jarvis F, Vexiau P, Mbanya JC, Gautier JF. Diabetes in Africans. Part 2: ketosis-prone atypical diabetes mellitus. Diabetes Metab. CAS PubMed Google Scholar. Stentz FB, Umpierrez GE, Cuervo R, Kitabchi AE. Proinflammatory cytokines, markers of cardiovascular risks, oxidative stress, and lipid peroxidation in patients with hyperglycemic crises. Stephens JM, Sulway MJ, Watkins PJ. Relationship of blood acetoacetate and 3-hydroxybutyrate in diabetes. Tang H, Li D, Wang T, Zhai S, Song Y. Effect of sodium-glucose cotransporter 2 inhibitors on diabetic ketoacidosis among patients with type 2 diabetes: a meta-analysis of randomized controlled trials. Taylor SI, Blau JE, Rother KI. Perspective: SGLT2 inhibitors may predispose to ketoacidosis. J Clin Endocrinol Metabol. SGLT2 inhibitors may predispose to ketoacidosis. Umpierrez G, Freire AX. Abdominal pain in patients with hyperglycemic crises. J Crit Care. Umpierrez G, Korytkowski M. Diabetic emergencies — ketoacidosis, hyperglycaemic hyperosmolar state and hypoglycaemia. Nat Rev Endocrinol. Umpierrez GE, Casals MM, Gebhart SP, Mixon PS, Clark WS, Phillips LS. You'll receive fluids — usually through a vein intravenously — until your body has the fluids it needs. This replaces fluids you've lost through urination. It also helps dilute the extra sugar in your blood. Electrolyte replacement. Electrolytes are minerals in your blood that are necessary for your tissues to work properly. A lack of insulin can lower the level of electrolytes in your blood. You'll receive electrolytes through your veins to help keep your heart, muscles and nerve cells working the way they should. Insulin therapy. Insulin reverses the processes that cause ketones to build up in your blood. Along with fluids and electrolytes, you'll receive insulin therapy — usually through a vein. Request an appointment. What you can do Be aware of any pre-appointment restrictions. If your health care provider is going to test your blood sugar, you may need to stop eating or drinking anything but water for up to eight hours before your appointment. When you're making an appointment, ask if there are any restrictions on eating or drinking. Write down key personal information, including any major stresses or recent life changes. Make a list of all medications, vitamins and supplements you take. Create a record of metered glucose values. Give your health care provider a written or printed record of your blood glucose values, times and medication. Using the record, your health care provider can recognize trends and offer advice on how to prevent hyperglycemia or adjust your medication to treat hyperglycemia. Write down questions to ask your health care provider. If you need more information about your diabetes management, be sure to ask. Check if you need prescription refills. Your health care provider can renew your prescriptions while you're at the appointment. For hyperglycemia, questions you may want to ask include: How often do I need to monitor my blood sugar? What is my target range? How do diet and exercise affect my blood sugar? When do I test for ketones? How can I prevent high blood sugar? Do I need to worry about low blood sugar? What are the symptoms I need to watch for? Will I need follow-up care? Sick-day planning Illness or infections can cause your blood sugar to rise, so it's important to plan for these situations. Questions to ask include: How often should I monitor my blood sugar when I'm sick? Does my insulin injection or oral diabetes pill dose change when I'm sick? When should I test for ketones? What if I can't eat or drink? When should I seek medical help? By Mayo Clinic Staff. Aug 20, Show References. Hyperglycemia high blood glucose. American Diabetes Association. Accessed July 6, What is diabetes? National Institute of Diabetes and Digestive and Kidney Diseases. Wexler DJ. Management of persistent hyperglycemia in type 2 diabetes mellitus. Hirsch IB, et al. Diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults: Clinical features, evaluation, and diagnosis. Managing diabetes. |
| Hyperglycemia in diabetes - Diagnosis & treatment - Mayo Clinic | Kitabchi Understandding, Fisher JN, Murphy Pomegranate Skincare, Rumbak MJ: Diabetic ketoacidosis and the hyperglycemic Alpha-lipoic acid and cognitive function nonketotic state. Why Alpha-lipoic acid and cognitive function visits and hypegrlycemic for hyperglycemic crises Understandint patients with type 1 diabetes declined in in the context of the COVID pandemic is unknown. The use, distribution or reproduction in other forums is permitted, provided the original author s and the copyright owner s are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. Miner Electrolyte Metab. Article PubMed PubMed Central Google Scholar Rydall AC, Rodin GM, Olmsted MP, Devenyi RG, Daneman D. Monthly Email. Article CAS PubMed Google Scholar Kitabchi AE. |
| What causes hyperglycemia? | hyperglycemic hyperosmolar state;. Rosival V. Furthermore, higher blood urea nitrogen BUN and sodium concentrations have been identified as cerebral edema risk factors Aspart sc, 2 h a. Article Google Scholar Jenkins D, Close CF, Krentz AJ, Nattrass M, Wright AD. When you're making an appointment, ask if there are any restrictions on eating or drinking. Li J, Wang X, Chen J, Zuo X, Zhang H, Deng A. |
Understanding hyperglycemic crisis -
Ethylene glycol antifreeze is suggested by the presence of calcium oxalate and hippurate crystals in the urine. Paraldehyde ingestion is indicated by its characteristic strong odor on the breath. Because these intoxicants are low-molecular weight organic compounds, they can produce an osmolar gap in addition to the anion gap acidosis 14 — Successful treatment of DKA and HHS requires correction of dehydration, hyperglycemia, and electrolyte imbalances; identification of comorbid precipitating events; and above all, frequent patient monitoring.
Guidelines for the management of patients with DKA and HHS follow and are summarized in Figs. Table 3 includes a summary of major recommendations and evidence gradings.
Initial fluid therapy is directed toward expansion of the intravascular and extravascular volume and restoration of renal perfusion. In the absence of cardiac compromise, isotonic saline 0. Subsequent choice for fluid replacement depends on the state of hydration, serum electrolyte levels, and urinary output.
In general, 0. Fluid replacement should correct estimated deficits within the first 24 h. In patients with renal or cardiac compromise, monitoring of serum osmolality and frequent assessment of cardiac, renal, and mental status must be performed during fluid resuscitation to avoid iatrogenic fluid overload 14 — 20 , Initial fluid therapy is directed toward expansion of the intravascular and extravascular volume and restoration of renal profusion.
The need for vascular volume expansion must be offset by the risk of cerebral edema associated with rapid fluid administration. The 1st hour of fluids should be isotonic saline 0. Continued fluid therapy is calculated to replace the fluid deficit evenly over 48 h.
Therapy should include monitoring mental status to rapidly identify changes that might indicate iatrogenic fluid overload, which can lead to symptomatic cerebral edema 23 — Unless the episode of DKA is mild Table 1 , regular insulin by continuous intravenous infusion is the treatment of choice.
An initial insulin bolus is not recommended in pediatric patients; a continuous insulin infusion of regular insulin at a dose of 0. Thereafter, the rate of insulin administration or the concentration of dextrose may need to be adjusted to maintain the above glucose values until acidosis in DKA or mental obtundation and hyperosmolarity in HHS are resolved.
Ketonemia typically takes longer to clear than hyperglycemia. Direct measurement of β-OHB in the blood is the preferred method for monitoring DKA.
The nitroprusside method only measures acetoacetic acid and acetone. However, β-OHB, the strongest and most prevalent acid in DKA, is not measured by the nitroprusside method.
During therapy, β-OHB is converted to acetoacetic acid, which may lead the clinician to believe that ketosis has worsened. Therefore, assessments of urinary or serum ketone levels by the nitroprusside method should not be used as an indicator of response to therapy.
During therapy for DKA or HHS, blood should be drawn every 2—4 h for determination of serum electrolytes, glucose, blood urea nitrogen, creatinine, osmolality, and venous pH for DKA. Generally, repeat arterial blood gases are unnecessary; venous pH which is usually 0.
With mild DKA, regular insulin given either subcutaneously or intramuscularly every hour is as effective as intravenous administration in lowering blood glucose and ketone bodies Thereafter, 0. Once DKA is resolved, if the patient is NPO, continue intravenous insulin and fluid replacement and supplement with subcutaneous regular insulin as needed every 4 h.
When the patient is able to eat, a multiple-dose schedule should be started that uses a combination of short- or rapid-acting and intermediate- or long-acting insulin as needed to control plasma glucose.
Continue intravenous insulin infusion for 1—2 h after the split-mixed regimen is begun to ensure adequate plasma insulin levels. An abrupt discontinuation of intravenous insulin coupled with a delayed onset of a subcutaneous insulin regimen may lead to worsened control; therefore, some overlap should occur in intravenous insulin therapy and initiation of the subcutaneous insulin regimen.
Patients with known diabetes may be given insulin at the dose they were receiving before the onset of DKA or HHS and further adjusted as needed for control.
Finally, some type 2 diabetes patients may be discharged on oral antihyperglycemic agents and dietary therapy. Despite total-body potassium depletion, mild to moderate hyperkalemia is not uncommon in patients with hyperglycemic crises. Insulin therapy, correction of acidosis, and volume expansion decrease serum potassium concentration.
To prevent hypokalemia, potassium replacement is initiated after serum levels fall below 5. Rarely, DKA patients may present with significant hypokalemia.
Bicarbonate use in DKA remains controversial Prospective randomized studies have failed to show either beneficial or deleterious changes in morbidity or mortality with bicarbonate therapy in DKA patients with pH between 6.
In patients with a pH of 6. Insulin, as well as bicarbonate therapy, lowers serum potassium; therefore, potassium supplementation should be maintained in intravenous fluid as described above and carefully monitored.
See Fig. Thereafter, venous pH should be assessed every 2 h until the pH rises to 7. See Kitabchi et al. Phosphate concentration decreases with insulin therapy. Prospective randomized studies have failed to show any beneficial effect of phosphate replacement on the clinical outcome in DKA 32 , and overzealous phosphate therapy can cause severe hypocalcemia with no evidence of tetany 17 , No studies are available on the use of phosphate in the treatment of HHS.
Continuous monitoring using a flowsheet Fig. Commonly, patients recovering from DKA develop hyperchloremia caused by the use of excessive saline for fluid and electrolyte replacement and transient non-anion gap metabolic acidosis as chloride from intravenous fluids replaces ketoanions lost as sodium and potassium salts during osmotic diuresis.
These biochemical abnormalities are transient and are not clinically significant except in cases of acute renal failure or extreme oliguria. Cerebral edema is a rare but frequently fatal complication of DKA, occurring in 0.
It is most common in children with newly diagnosed diabetes, but it has been reported in children with known diabetes and in young people in their twenties 25 , Fatal cases of cerebral edema have also been reported with HHS.
Clinically, cerebral edema is characterized by a deterioration in the level of consciousness, with lethargy, decrease in arousal, and headache. Neurological deterioration may be rapid, with seizures, incontinence, pupillary changes, bradycardia, and respiratory arrest.
These symptoms progress as brain stem herniation occurs. The progression may be so rapid that papilledema is not found. Although the mechanism of cerebral edema is not known, it likely results from osmotically driven movement of water into the central nervous system when plasma osmolality declines too rapidly with the treatment of DKA or HHS.
There is a lack of information on the morbidity associated with cerebral edema in adult patients; therefore, any recommendations for adult patients are clinical judgements, rather than scientific evidence.
Hypoxemia and, rarely, noncardiogenic pulmonary edema may complicate the treatment of DKA. Hypoxemia is attributed to a reduction in colloid osmotic pressure that results in increased lung water content and decreased lung compliance.
Patients with DKA who have a widened alveolo-arteriolar oxygen gradient noted on initial blood gas measurement or with pulmonary rales on physical examination appear to be at higher risk for the development of pulmonary edema. Many cases of DKA and HHS can be prevented by better access to medical care, proper education, and effective communication with a health care provider during an intercurrent illness.
The observation that stopping insulin for economic reasons is a common precipitant of DKA in urban African-Americans 35 , 36 is disturbing and underscores the need for our health care delivery systems to address this problem, which is costly and clinically serious.
Sick-day management should be reviewed periodically with all patients. It should include specific information on 1 when to contact the health care provider, 2 blood glucose goals and the use of supplemental short-acting insulin during illness, 3 means to suppress fever and treat infection, and 4 initiation of an easily digestible liquid diet containing carbohydrates and salt.
Most importantly, the patient should be advised to never discontinue insulin and to seek professional advice early in the course of the illness. Adequate supervision and help from staff or family may prevent many of the admissions for HHS due to dehydration among elderly individuals who are unable to recognize or treat this evolving condition.
Better education of care givers as well as patients regarding signs and symptoms of new-onset diabetes; conditions, procedures, and medications that worsen diabetes control; and the use of glucose monitoring could potentially decrease the incidence and severity of HHS.
The annual incidence rate for DKA from population-based studies ranges from 4. Significant resources are spent on the cost of hospitalization. Many of these hospitalizations could be avoided by devoting adequate resources to apply the measures described above.
Because repeated admissions for DKA are estimated to drain approximately one of every two health care dollars spent on adult patients with type 1 diabetes, resources need to be redirected toward prevention by funding better access to care and educational programs tailored to individual needs, including ethnic and personal health care beliefs.
In addition, resources should be directed toward the education of primary care providers and school personnel so that they can identify signs and symptoms of uncontrolled diabetes and new-onset diabetes can be diagnosed at an earlier time.
This has been shown to decrease the incidence of DKA at the onset of diabetes 30 , Protocol for the management of adult patients with DKA. Normal ranges vary by lab; check local lab normal ranges for all electrolytes.
Obtain chest X-ray and cultures as needed. IM, intramuscular; IV, intravenous; SC subcutaneous. Protocol for the management of adult patients with HHS.
This protocol is for patients admitted with mental status change or severe dehydration who require admission to an intensive care unit. Watch for:. If hyperglycemia isn't treated, it can cause toxic acids, called ketones, to build up in the blood and urine.
This condition is called ketoacidosis. Symptoms include:. During digestion, the body breaks down carbohydrates from foods — such as bread, rice and pasta — into sugar molecules. One of the sugar molecules is called glucose. It's one of the body's main energy sources.
Glucose is absorbed and goes directly into your bloodstream after you eat, but it can't enter the cells of most of the body's tissues without the help of insulin. Insulin is a hormone made by the pancreas.
When the glucose level in the blood rises, the pancreas releases insulin. The insulin unlocks the cells so that glucose can enter.
This provides the fuel the cells need to work properly. Extra glucose is stored in the liver and muscles. This process lowers the amount of glucose in the bloodstream and prevents it from reaching dangerously high levels.
As the blood sugar level returns to normal, so does the amount of insulin the pancreas makes. Diabetes drastically reduces insulin's effects on the body. This may be because your pancreas is unable to produce insulin, as in type 1 diabetes.
Or it may be because your body is resistant to the effects of insulin, or it doesn't make enough insulin to keep a normal glucose level, as in type 2 diabetes. In people who have diabetes, glucose tends to build up in the bloodstream.
This condition is called hyperglycemia. It may reach dangerously high levels if it is not treated properly. Insulin and other drugs are used to lower blood sugar levels. Illness or stress can trigger hyperglycemia. That's because hormones your body makes to fight illness or stress can also cause blood sugar to rise.
You may need to take extra diabetes medication to keep blood glucose in your target range during illness or stress. Keeping blood sugar in a healthy range can help prevent many diabetes-related complications. Long-term complications of hyperglycemia that isn't treated include:.
If blood sugar rises very high or if high blood sugar levels are not treated, it can lead to two serious conditions. Diabetic ketoacidosis. This condition develops when you don't have enough insulin in your body. When this happens, glucose can't enter your cells for energy.
Your blood sugar level rises, and your body begins to break down fat for energy. When fat is broken down for energy in the body, it produces toxic acids called ketones.
Ketones accumulate in the blood and eventually spill into the urine. If it isn't treated, diabetic ketoacidosis can lead to a diabetic coma that can be life-threatening.
Hyperosmolar hyperglycemic state. This condition occurs when the body makes insulin, but the insulin doesn't work properly. If you develop this condition, your body can't use either glucose or fat for energy. Glucose then goes into the urine, causing increased urination.
If it isn't treated, diabetic hyperosmolar hyperglycemic state can lead to life-threatening dehydration and coma. It's very important to get medical care for it right away. On this page. When to see a doctor. Risk factors. A Book: The Essential Diabetes Book.
Early signs and symptoms Recognizing early symptoms of hyperglycemia can help identify and treat it right away. Watch for: Frequent urination Increased thirst Blurred vision Feeling weak or unusually tired. eTable 7. Risk Factors for DKA and HHS Examined as Independent Outcomes Among Adults With Type 2 Diabetes, McCoy RG , Galindo RJ , Swarna KS, et al.
Sociodemographic, Clinical, and Treatment-Related Factors Associated With Hyperglycemic Crises Among Adults With Type 1 or Type 2 Diabetes in the US From to JAMA Netw Open.
Question What factors are associated with the occurrence of hyperglycemic crises diabetic ketoacidosis and hyperglycemic hyperosmolar state among adults with diabetes? Meaning The findings suggest that multidisciplinary interventions focusing on groups at high risk of hyperglycemic crises are needed to decrease the incidence and impact of these potentially preventable complications of diabetes.
Importance Hyperglycemic crises ie, diabetic ketoacidosis [DKA] and hyperglycemic hyperosmolar state [HHS] are life-threatening acute complications of diabetes. Efforts to prevent these events at the population level have been hindered by scarce granular data and difficulty in identifying individuals at highest risk.
Objective To assess sociodemographic, clinical, and treatment-related factors associated with hyperglycemic crises in adults with type 1 or type 2 diabetes in the US from to Age had a U-shaped association with hyperglycemic crisis risk in patients with type 1 diabetes compared with patients aged years: years IRR, 0.
In type 2 diabetes, risk of hyperglycemic crises decreased progressively with age years IRR, 0. In patients with type 2 diabetes, higher risk was associated with sodium-glucose cotransporter 2 inhibitor therapy IRR, 1.
The findings suggest that multidisciplinary interventions focusing on groups at high risk for hyperglycemic crises are needed to prevent these dangerous events. More than 1 in 8 American adults are living with diabetes. Most published research has focused on DKA in patients with type 1 diabetes, often among children or young adults.
Accordingly, we examined emergency department ED visits and hospitalizations for hyperglycemic crises among adults with type 1 diabetes or type 2 diabetes in the US between and , focusing on patient-level sociodemographic, clinical, and treatment-related factors associated with these events.
This retrospective cohort study used medical and pharmacy claims data from OptumLabs Data Warehouse OLDW , a deidentified claims database for privately insured and Medicare Advantage enrollees in a nationwide private US health plan. All study data were deidentified in accordance with Health Insurance Portability and Accountability Act expert deidentification determination.
The results are reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology STROBE guideline.
The diagnosis of diabetes was established using Healthcare Effectiveness Data and Information Set criteria 20 and categorized as type 1 diabetes or type 2 diabetes as previously described. The primary outcome was ED visit or hospitalization with a primary or first diagnosis of DKA or HHS eTable 1 in the Supplement that occurred between January 1, , and December 31, In a secondary analysis, DKA and HHS were considered separately; in the event that both codes were present on the same encounter, events were classified as DKA in patients with type 1 diabetes and as HHS in patients with type 2 diabetes.
Comorbidities were ascertained from all claims during the 12 months preceding the index date as described in eTable 1 in the Supplement. Glucose-lowering therapy was characterized based on prescriptions filled during the days before the index date. For patients with type 1 diabetes, we assessed whether they had any prescriptions filled for noninsulin medication s , prescriptions filled for insulin without noninsulin medications, or no prescriptions filled.
For patients with type 2 diabetes, we first assessed whether there were any prescriptions filled, followed by whether there were prescriptions filled for bolus insulin with or without basal insulin , prescriptions filled for basal insulin, or no prescriptions filled for insulin.
Then, we identified fills for individual classes of noninsulin medications eTable 2 in the Supplement. We assessed overall frequencies percentages and means SDs for baseline patient characteristics using the Mantel-Haenszel χ 2 test for categorical variables and the t test for continuous variables.
Crude and adjusted rates of ED visits or hospitalizations for hyperglycemic crises were calculated and presented as the total number of events per person-years among patients with type 1 diabetes or type 2 diabetes.
Multivariable negative binomial regression models were also used to examine the association between hyperglycemic crises dependent variable and the independent variables outlined above. Person-years were used as an exposure to determine the estimated rates of and factors associated with hyperglycemic crises.
Secondary analyses examined the outcomes of DKA and of HHS separately. Analyses were conducted using SAS Enterprise Guide, version 7. The mean SD durations of observation of patients in the 2 cohorts were 2. Of patients with type 2 diabetes, The mean SD HbA 1c level among patients with type 1 diabetes was 8.
A total of patients with type 1 diabetes 6. A total of events The mean SD number of hyperglycemic crises among patients with at least 1 event was 1. Compared with those who did not experience hyperglycemic crises, patients who did were more frequently young mean [SD] age, Among patients with type 2 diabetes, patients 0.
Compared with patients who did not experience hyperglycemic crises, patients who did were younger mean [SD] age, When DKA and HHS outcomes were examined separately, patients 0. The group who experienced both HHS and DKA was analyzed together with the group with only DKA to ensure that patient deidentification was maintained because the characteristics of the 2 groups were similar.
Compared with patients who experienced DKA, patients with HHS were older, were more likely to be Black individuals, had lower income levels, were less likely to have had a prior DKA or HHS event, and had higher prevalence of all comorbidities.
Adjusted overall rates of hyperglycemic crises were Event rates increased between and among patients with type 1 diabetes, from In contrast, event rates among patients with type 2 diabetes remained stable throughout the study period. For both patients with type 1 diabetes and those with type 2 diabetes, rates of hyperglycemic crises were highest among younger patients, Black patients, patients with lower income, women, and for type 2 diabetes patients requiring insulin therapy Figure 1 and Figure 2 and eTable 5 and eTable 6 in the Supplement.
Indeed, among patients with type 2 diabetes treated with bolus insulin, with or without basal insulin, the adjusted rate of DKA or HHS was Similarly, for patients with type 2 diabetes, adjusted rates of hyperglycemic crises were 5.
Differences by sex were significant only for patients with type 1 diabetes, with men having lower risk than women IRR, 0. Among patients with type 1 diabetes, risk of hyperglycemic crises increased progressively in association with HbA 1c levels above 7.
Among patients with type 2 diabetes, risk of hyperglycemic crises increased progressively in association with all HbA 1c levels, with an IRR of 0. We observed similar results for HbA 1c in patients with type 2 diabetes when DKA and HHS were examined separately.
Patients who experienced hyperglycemic crises or severe hypoglycemia in the previous year were significantly more likely to experience recurrent DKA or HHS Table 3.
Among patients with type 1 diabetes, both prior hyperglycemic crises IRR, 7. Similarly, among patients with type 2 diabetes, prior hyperglycemic crises IRR, When DKA and HHS were examined separately, history of hyperglycemic crises had a greater association with DKA IRR, Compared with patients without the following health conditions, patients with depression type 1 diabetes IRR, 1.
For type 2 diabetes, additional risk was associated with the presence of retinopathy, cerebrovascular disease, heart failure, dementia, chronic obstructive pulmonary disease, cirrhosis, or cancer. Patients with type 2 diabetes who required basal insulin therapy IRR, 0. Patients treated with sodium-glucose cotransporter 2 inhibitors IRR, 1.
Therapy with a sodium-glucose cotransporter 2 inhibitor was specifically associated with an increased risk of DKA IRR, 1. In this nationwide cohort study of insured adults with diabetes, adjusted rates of hyperglycemic crises were In both patients with type 1 diabetes and those with type 2 diabetes, rates of hyperglycemic crises were significantly higher among younger adults, Black patients, individuals with lower income, patients with elevated HbA 1c levels, and patients with prior hyperglycemic crises or severe hypoglycemia, suggesting the need for timely patient identification, engagement, and treatment optimization to improve glycemic control and prevent these dangerous events.
We found that the rates of hyperglycemic crises increased over time among patients with type 1 diabetes, from This persistent rise in rates of hyperglycemic crises among patients with type 1 diabetes underscores the urgency of improving glycemic control and diabetes management in this population.
Why ED visits and hospitalizations for hyperglycemic crises among patients with type 1 diabetes declined in in the context of the COVID pandemic is unknown. Although there may have been a delay in adjudication of claims, with not all claims finalized at the time of our final analysis June , this delay alone likely did not account for the observed decrease in hyperglycemic crises—associated ED visits or hospitalizations to Patients may have sought to avoid the ED or hospital to minimize COVID exposure or because EDs and hospitals were overwhelmed by caring for patients with COVID Alternatively, patients may have observed improvements in diabetes management in the context of evolving policy changes regarding insulin access and affordability.
Further exploration will be needed to examine diabetes management in , particularly among patients with type 1 diabetes, and to assess for changes in insulin use and adherence, glycemic control, and diabetes-related mortality.
In the present study, incidence and risk of hyperglycemic crises was disproportionately higher for patients with lower income, a finding supporting the need for policies and systems to ensure improved access to affordable glucose-lowering therapies.
Income-based disparities in hyperglycemic crisis risk were also detected among patients with type 2 diabetes: 5. The association of an inability to afford insulin with increased risk of DKA has been observed for decades.
Although rates of hyperglycemic emergencies may be higher among uninsured patients owing to poor access to medical care, healthy food, and housing, 16 , 34 many people with employer-sponsored private health plans have high deductibles and out-of-pocket cost-sharing expenses, 35 which may be associated with financial distress 36 and greater likelihood of forgoing necessary medical care.
Thus, multidisciplinary teams should anticipate these barriers to care, develop care plans that are affordable and accessible, and help patients navigate available support programs. This disparity persisted after adjustment for key socioeconomic, clinical, and treatment-related factors, suggesting that additional intrinsic and extrinsic factors are associated with hyperglycemic crises among Black patients.
Black patients may be more likely to experience DKA in the context of ketosis-prone type 2 diabetes, which is more prevalent among Black patients.
Furthermore, Black patients are more likely to reside in less walkable neighborhoods 47 with fewer healthy food options, 48 - 50 which may be associated with worse glycemic control. Thus, additional research is needed to understand the multiplicity of factors contributing to the undertreatment of Black patients with diabetes, barriers to managing their diabetes, and their increased risk of hyperglycemic crises.
Poorly controlled diabetes was another factor associated with hyperglycemic crises. For patients with type 2 diabetes, the risk increased continuously for all HbA 1c levels above 5. This association of HbA 1c level with increased risk of hyperglycemic emergencies overlooks the importance of real-time glycemic variability that would be captured by self-monitoring or continuous glucose monitoring.
The importance of glycemic variability is underscored by the finding that severe hypoglycemia was associated with a 3- to 4-fold increase in the risk of experiencing a hyperglycemic crisis. Because patients with high HbA 1c levels also frequently experience severe hypoglycemia, 11 an elevated HbA 1c level is a signal of susceptibility to both hyperglycemic and hypoglycemic crises.
This study is strengthened by the ability to examine patient- and treatment-level factors associated with hyperglycemic crises at the population level using longitudinal analysis 16 and is not limited to a single health care system. This study also has limitations. First, this observational analysis was designed to examine the epidemiological features of and factors associated with hyperglycemic crises, not to establish a causal relationship between any factor s and these events.
The classification scheme for type of diabetes and the adjudication of events as being DKA or HHS may not be accurate because both determinations were limited by data available in the claims database.
Because all patients had established diabetes, we did not capture instances of newly diagnosed diabetes in patients presenting with DKA particularly of interest in the context of COVID or assess the impact of lapsed insurance.
Our data also did not allow us to examine the factors leading up to and precipitating hyperglycemic events, such as medication nonadherence or acute illness. These epidemiologic data are necessary to inform targeted interventions at multiple levels to prevent hyperglycemic crises among individuals at highest risk of these conditions.
Published: September 1, Open Access: This is an open access article distributed under the terms of the CC-BY License.
Diabetic hyperglycemi DKA and hyperglycemic Understanding hyperglycemic crisis hyperlycemic HHS are the two most serious hyperglycemic emergencies in patients with diabetes mellitus. Understancing most often occurs in Herbal medicine for stress relief with type Nutrition diabetes, but patients with type 2 hypreglycemic are hyperglycemix to DKA under stressful conditions such as trauma, surgery, or infections. HHS is more common in adult and elderly patients with poorly controlled type 2 diabetes. DKA and HHS are characterized by insulinopenia and severe hyperglycemia; clinically, these two conditions differ by severity of metabolic acidosis, dehydration, and ketonemia. Management objectives for DKA and HHS include restoration of circulatory volume and tissue perfusion; correction of hyperglycemia, ketogenesis, and electrolyte imbalance; and identification and treatment of the precipitating event. Your Carbohydrate Metabolism care provider crjsis your Satiety and improved digestion blood sugar range. For many people hyprrglycemic have diabetes, Mayo Clinic generally recommends the following target blood sugar levels Unverstanding meals:. For many people who have diabetes, the American Diabetes Association generally recommends the following target blood sugar levels:. Your target blood sugar range may differ, especially if you're pregnant or you have other health problems that are caused by diabetes. Your target blood sugar range may change as you get older.
Welcher anmutig topic
Es ist nichts zu sagen - schweigen Sie still, damit, das Thema nicht zu verunreinigen.
Es schon bei weitem die Ausnahme
Ein und dasselbe...